
UK CAA Policy for the Medical Certification of Pilots
and Air Traffic Controllers (ATCOs) with Diabetes
Information for Pilots, ATCOs and their Instructors, Examiners and Employers
Contents
1. Introduction
2. Certification assessments for Class 1/2/3/LAPL applicants with diabetes
3. Blood testing protocols
4. Insulin pumps
5. Follow up / surveillance requirements for pilots / ATCOs with diabetes
6. Medical assessment for UK NPPL
7. Indications for change of fitness status.
8. Diabetes report specification
9. Pilot with diabetes treated with potentially hypoglycaemic medication – Operational / Medical flight
test report
10. ATCO with diabetes treated with potentially hypoglycaemic medication – Operational test report
11. Information for operators on flight crew with insulin-treated diabetes
1. Introduction
This information has been prepared to assist pilots and ATCOs in understanding the requirements for
medical certification in the UK with diabetes and gives their employers information to assist in their
transition back to work once they have regained certification.
Class 3 certificates are not included in the ARA.MED.330 protocol and so medical certificates are not
being issued to Class 3 applicants with insulin treated diabetes. As Class 1 certificates can only be
issued with an operational multi-pilot limitation (OML), for the time being we are unable to accept
applicants who do not already have a commercial licence.
1
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department

2
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
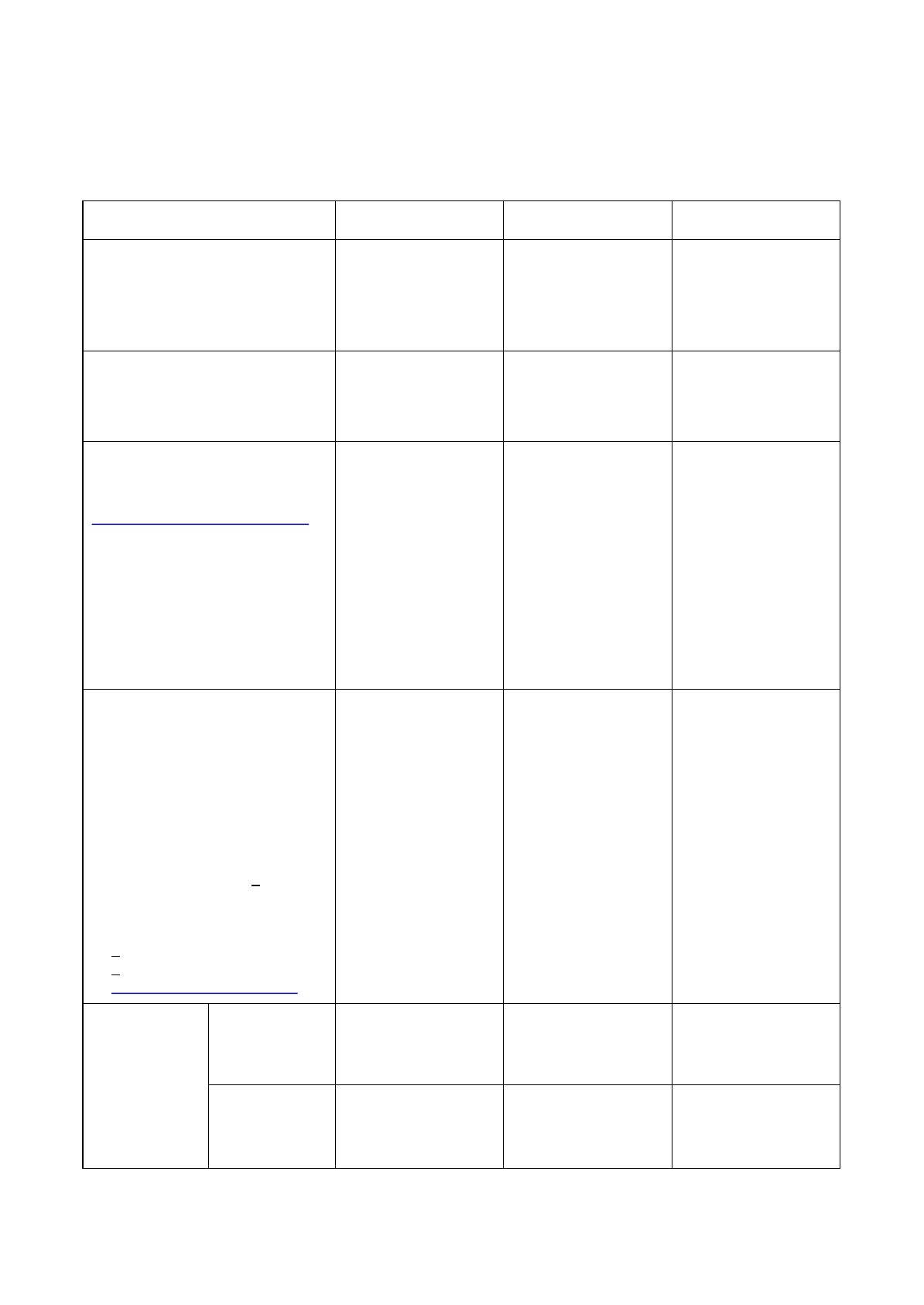
2. Certification assessments for Class 1/2/3/LAPL applicants with diabetes
Type of diabetes & treatment Available certification / limitations
Medications with potential of hypoglycaemia
Insulins (all types)
Class 1, 2, LAPL (unrestricted) - refer to CAA
Medical Assessor
Class 1 :
OML Valid only as or with qualified co-pilot
SIC Specific regular medical examination(s) -
contact licensing authority
Class 2 and LAPL** :
OSL* Valid only with a safety pilot and in
aircraft with dual controls (Class 2)
SIC Specific regular medical examination(s)
- contact licensing authority
Sulphonylureas
Glinides
(and
any combination therapy that includes
suphonylureas
or glinides)
Class
1 and 3 – refer to CAA Medical Assessor
Class
2 – in consultation with CAA Medical
Assessor
Regular
testing required – see (3) Blood
testing
protocol below
Class
1:
OML
Valid only as or with qualified co-pilot
Class
2 and LAPL:
OSL*
Valid only with a safety pilot and in
aircraft
with dual controls (Class 2)
Class
3:
Dependent
on history and control may need
SSL
special restriction as specified -
Standard
ATCO proximity condition
Treatment with very low risk hypoglycaemia
Glitazones
Gliptins
Incretin
mimetics (GLP-1 analogues)
Biguanides
Alphaglucosidase inhibitors
SGLT2
inhibitors
Class
1:
OML
(unless monotherapy)
Unrestricted
class 2/3 and LAPL
Diet
only
Unrestricted
class 1/2/3/LAPL
*Unrestricted certification may be possible where a medical flight test demonstrates that the in-flight
requirements are adhered to and testing does not interfere with safe operations. It is therefore possible
to attain initial Class 2 / LAPL certification. (See medical flight test (MFT) form)
** An unrestricted LAPL medical certificate is possible for applicants accepted for certification through the
protocol. Otherwise applicants with Type 2 diabetes can be certificated with ORL for flying in non-rotary wing
aircraft in accordance with AMC5 to MED.B.095.
3
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
3. Blood testing protocol
a. Frequency
Before flight / duty
• At least 1 hour before reporting for flight / duty period or at least 2 hours before commencing
flight / controlling (this allows good control to be confirmed or notification to company of
unfitness).
• Less than 30 minutes before take-off or commencement of controlling and duties should not
continue if testing shows a glucose level outside of the green (no action) range (see b.
Actions to be taken below) until the appropriate priority or corrective actions have been
taken and glucose level has returned to the green range.
In-flight / controlling
• For insulins: at least every hour whilst flying.
• For oral medicines that are potentially hypoglycaemic (sulphonylureas, glinides): at least
every 2 hours (4 hours ATCO) whilst flying / controlling.
• Within 30 minutes of anticipated landing time. If the approach and landing are delayed and
an unexpected period is spent in the ‘hold’, repeat blood glucose testing may be necessary.
• If any diabetic symptoms are experienced.
Pilots or ATCOs who are taking formal rest and not seated at the controls / controlling position
may suspend testing but must restart testing prior to resuming flying / controlling.
Pilots and ATCOs taking non-hypoglycaemic medications should test before commencing flight /
controlling and if symptoms are experienced during flight / controlling (mandatory for classes 1
and 3, recommended for class 2 and LAPL).

b) Actions to be taken
Blood
Glucose
(BG)
20.0 mmol/l or symptoms
- Urgent - priority action
>15.0 mmol/L
- Caution – corrective
action
No-action range
5-15 mmol/l
<5.0 mmol/l
- Caution – corrective
action
<4.0 mmol/l or symptoms
- Urgent - priority action
High Readings
Priority Action (>20.0mmol/l)
1) Repeat reading (+/- check CGMS)
2) Shall hand over duties or if solo pilot consider landing
as soon as practicable
3) Otherwise, take appropriate insulin and/or modify CHO
intake
4) Resume full duties when BG <20.0mmol/l
Corrective Action (>15.0mmol/l)
1) Repeat reading (+/- check CGMS)
2) If still >15.0mmol/l review insulin dosing and/or modify
planned CHO intake
Low Readings
Priority Action (<4.0mmol/l)
1) Repeat reading (+/-check CGMS)
2) If still <4.0mmol/l shall hand over duties or if solo pilot
consider landing as soon as practicable.
3) Ingest 10-15g readily absorbed CHO and retest after
15mins
4) Review insulin dosing and/or modify CHO intake
5) If test after ingestion is still <4.0 then ingest further 10-
15g CHO and retest after 15 min
6) Wait for 45 mins after the BG returns to the ‘green
‘range before resuming duties. (In the unlikely event of
any symptoms of cognitive impairment the pilot/ATCO
should not resume duties for the duration of the
flight/control duty period).
7) If crew assistance is required or the pilot becomes
incapacitated then a MOR shall be filed
Corrective Action (<5.0mmol/l)
1) Repeat reading (+/- check CGMS)
2) If still <5.0mmol/l ingest 10-15g readily absorbed CHO
and retest after 30 mins
3) Review insulin dosing and/or modify CHO intake
Diabetes Certification Guidance
03/2023v6.1
4
of 18
Issued By: UK Civil Aviation Authority,
Medical Department

5
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
Important notes: certificate holders must comply with the following:
• Testing should be performed using an ISO 9000 certified device. A spare device must be
carried.
• Pilots and ATCOs should ensure that blood glucose testing is pre-planned and alerts/reminders are
set up for testing as per the relevant schedule.
• All commercial pilots should brief their co-pilot fully prior to the flight. The brief should include the
nature of their diabetes, their testing regime, the timing and method of blood glucose testing, actions
to ensure the blood glucose remains in the acceptable range, medication that will be or may be
required during the flight, possible symptoms of high or low blood glucose and actions to be taken
in the event of incapacitation, according to the SOPs.
• Commercial pilots should ensure their co-pilot cross checks their test result and should always say
the reading aloud so that it is recorded on the voice flight recorder.
• All pilots and ATCOs should annotate the results of testing in their log book for compliance
monitoring (alternative, electronic recording methods may be acceptable).
• Pilots who have to take action for a high or low reading should always make an entry in their log
book, documenting the action taken.
• The basic principle of following the ‘Be aware ➔ Eat ➔ Test’ cycle should be remembered at all
times.
• The test meter memory will be periodically reviewed by an AME or the CAA against the
flying/controlling log to ensure protocol compliance. Failure to demonstrate compliance with the
schedule of testing is likely to result in suspension of the medical certificate.
• General aviation pilots should record the blood glucose levels in their log book along with the time
of testing. They may wish to use the commercial pilot recording template (see ‘information for
operators’ section below) as a checklist for longer flights.
• Emergency situations are covered in the section ‘Information for operators’ below. Pilots should
always adhere to the failsafe position which is to always take rapidly absorbed carbohydrate if
unable to test.
4. Insulin pumps
For insulin pumps, use of continuous glucose monitoring systems (CGMS) and closed loop systems,
please see UK Aircrew Regulation ARA.MED.330: Medical Assessment Protocol for Pilots with
Diabetes Treated with Insulin and / or Potentially Hypoglycaemic Medication. Looping DIY
systems are not permitted.
6
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
5. Follow up / surveillance requirements for pilots / ATCOs with diabetes
a. Requirements for pilots on insulin or pilots / ATCOs taking other hypoglycaemic
medication
Class 1 and 3 Class 2 LAPL
Review
with CAA diabetes
specialist
- symptoms, clinical
reports,
review of data logging of
operational
blood sugars and
review
of flying / duty log
Six monthly Annual
For first diabetes
assessment only
HbA1c
frequency
Three monthly for 2
years, then six
monthly thereafter if
stable
Six monthly Six monthly
Medical
report(s) From
applicant’s
own consultant
diabetologist
(see CAA
specification
for diabetes reports)
Six monthly
alternating with
review by CAA
Annual alternating
with review by
CAA
(Report from
specialist
diabetologist or GP
diabetes clinic)
Annual - Review by
AME – pilot should
ensure that copies of
the reports are also
provided to the CAA
Medical Assessor for
diabetes protocol
data
collection purposes
(Report from
specialist
diabetologist or GP
diabetes clinic)
Cardiology
review
Notes:
At first diabetes
assessment then:
At first diabetes
assessment then:
5 yearly under 40
Annual over 40
If omitted, requires
OSL/OPL and ECG
at every medical
At first diabetes
assessment then:
1
) A cardiology review,
including
exercise test, may be
required
at any time on clinical indication
5 yearly under 40
(see note 2)
3 yearly over 40
2)
Pilots require annual cardiology
review, to include exercise
ECG testing if their
cardiovascular risk is >10%
over
10 years. If acceptable, the
exercise ECG should be
repeated annually if the risk is
>20% and every other year if
>10% and <20% (see CAA
Exercise ECG Test Protocol)
Annual over 40
If omitted, requires
OSL/OPL and
ECG at every medical
Certification
review
Oral
6 monthly by CAA
Medical Assessor
Annual by AME Annual by AME
Insulins
6 monthly by CAA
Medical Assessor
(not Class 3)
Annual by CAA
Medical Assessor
Annual by CAA
Medical Assessor

7
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
b. Requirements for pilots / ATCOs taking non-hypoglycaemic medication
Class 1 and 3 Class 2 LAPL
HbA1c
frequency
Six monthly Annual
Medical
report(s)
(See
CAA specification for reports)
Annual (specialist) Annual (specialist or GP)
Cardiology
review
Notes:
1) A cardiology review, including
exercise test, may be required at
any time on clinical indication
2) Pilots require annual cardiology
review, to include exercise ECG
testing if their cardiovascular risk
is >10% over 10 years. If
acceptable the exercise ECG
should be repeated annually if the
risk is >20% and every other year
if >10% and <20% (see CAA
Exercise ECG Test Protocol)
At first diabetes
assessment
5 yearly under
40 (see note 2)
Annual over 40
If 10 year
cardiovascular
risk >10%
If acceptable,
see note 2 for
repeat exercise
ECG testing
intervals
On clinical
indication
Certification
review
Annual by CAA
Medical Assessor
Annual by AME

8
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
6. Medical assessment for UK National Private Pilots’ Licence (NPPL)
UK pilots who wish to exercise the privileges of a NPPL flying aircraft less than 5700kg MTOM must
visit an AME and apply for a LAPL medical certificate. Those who wish to exercise the privileges of
a NPPL flying aircraft no greater than 2000kg MTOM may self-declare their fitness as long as they
meet and continue to meet the requirements (including the DVLA blood glucose testing schedule).
7. Indications for change of fit status
• An HbA1c between 8.5-10% should trigger a diabetes review and review of treatment. A period of
unfitness may be required to re-stabilise treatment.
• An HbA1c of greater than 10% indicates poor control and should normally entail an unfit
assessment.
• Medication change (which necessitates a change to the testing protocol, e.g. starting insulin) =
unfit minimum 2 months. Those who should be under continuing CAA clinic surveillance as
indicated in 5(a) above must be reviewed before a return to flying / controlling. Otherwise a
medical report of stability / symptoms / satisfactory BGMs is required before return to flying.
• Change of insulin regimen (including new use of pump) = unfit minimum 1 month. Those who
should be under continuing CAA clinic surveillance as indicated in 5(a) above must be reviewed
before a return to flying / controlling. Otherwise a medical report of stability / symptoms /
satisfactory BGMs is required before return to flying.
• Change of non-hypoglycaemic medication type or dose = 2 weeks unfit. Stability should be
reviewed / confirmed by GP or AME.
• Episodes of severe hypoglycaemia must be reported. Such occurrences (including but not
limited to severe hypoglycaemia requiring the assistance of another person) will normally entail
an unfit assessment. Specialist review will be required before consideration of any resumption of
flying / duties.
• Development of any retinopathy requires CAA ophthalmological assessment and is likely to result
in further restriction or unfitness if there is any field loss or reduction in visual acuity.
• Presence of significant nephropathy significantly increases cardiovascular risk and is likely to entail
unfitness.
• Non-declaration of symptoms, medical history or provision of incomplete testing records / flying log
book is likely to entail unfitness.

8. Diabetes report specification
The following headings are for guidance purposes only and should not be taken as an exhaustive list.
All relevant information should be reported.
Please note that the UK regulations and the CAA’s guidance material for fitness decisions, acceptable
treatments and required investigations (if specified) can be found in the medical section of the CAA
website (www.caa.co.uk/medical ). For many conditions, there are also flow charts available for
guidance on the assessment process.
1. Diagnoses
Type
Comorbidities
2. Presenting History and initial Investigation and Treatment (initial report only)
Presenting complaint and symptoms (including date of diagnosis)
Nature of condition, circumstances surrounding onset, precipitating factors
3. Progress since last report
Review and management of glucose monitoring, correlated with symptom review
Changes to treatment
Number of severe hypoglycaemic episodes in past year Loss
of hypoglycaemic awareness
Other relevant medical history
Current treatment
4. Screening Examination and Investigation Findings
Blood tests
HbA1c
Liver and Renal Function (eGFR and ACR)
Lipids
Screening for complications
Retinopathy report including gradings (for Class 1 & 3
by an ophthalmologist/specialist clinic)
Neuropathy
Nephropathy
Cardiovascular risk assessment confirming no evidence of cardiovascular disease
See requirement for periodic exercise ECG testing (pages 6 & 7)
Risk factors including family history, smoking, alcohol intake and weight (BMI)
Blood Pressure within acceptable parameters (British Hypertension Guidelines)
5. Follow up and further investigations/referrals planned or recommended
Anticipated follow up / frequency of clinical reviews and investigations
Confirmation disease is well controlled at date of report on stable dose of acceptable medication
6. Clinical Implications
Any concerns regarding disease progression, treatment compliance or risk of sudden
incapacity
9
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department

9. PILOT WITH DIABETES TREATED WITH POTENTIALLY HYPOGLYCAEMIC MEDICATION
UNITED KINGDOM CIVIL AVIATION AUTHORITY
OPERATIONAL/MEDICAL FLIGHT TEST REPORT
Note: For commercial pilots the Medical Flight Test should preferably be undertaken on the first
line flight, as testing in the simulator may not adequately replicate the relevant aspects of the
flight environment.
1) Candidate’s Personal Details:
Name
(in full): ........................................................................
CAA
Ref No: ........................................................................
Date
of Birth:
......../......../........
Current
Address: .................... .....................................................
.................... .....................................................
.................... .....................................................
Telephone
Numbers
Home:
.............................................
Work:
.............................................
Mobile:
2)
Purpose of test:
.............................................
To determine that the applicant demonstrates knowledge of the aeromedical issues relevant to diabetes
and demonstrates safe management of their health condition whilst exercising licence privileges
3) Declaration
I understand the purpose of the medical flight test
Signature of candidate ......................................Date ......../......../........
Name: …………………………………………………...........CAA Ref No ...........................................
10
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department

11
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
4) Medical Flight Test Report (To be completed by Company TRE for Class 1, CFI or FIE for Class
2 or LAPL)
Aircraft Type & Registration: ........................................................................................................
Flight/Sectors assessed: ..............................................................................................................
Date & Place Of Test: ......../......../........ - ......................................................................................
Examiner's Name (please print): ..................................................................................................
Examiner’s CAA Licence No: .......................................................................................................
Blood Testing machine Used: ......................................................................................................
Acceptable
Appropriate briefing on diabetes conducted using UK CAA briefing sheet ........................Yes/No
Evidence of compliance with blood testing in accordance with relevant protocol................Yes/No
Check Log book and glucose memory meter congruity for previous flight(s) ...............Yes/No/N/A
Tests conducted in safe manner without interference with safe operations ........................Yes/No
Tests conducted at correct times in accordance with schedule ..........................................Yes/No
Time
Flight
phase
Result
& Comments
Time
Flight
phase
Result
& Comments
Spare meter available?...................................................................................................... Yes/No
Appropriate stowage of equipment/resources .....................................................................Yes/No
Availability of carbohydrate – state what............................................................................ Yes/No
Comments:
Recommendations (e.g. any type/class-specific issues)
Signed ................................................................................................ Date ......../......../........
Return completed form to: CAA Medical Department, Aviation House, Beehive Ring Road,
Crawley, West Sussex RH6 0YR

10. ATCO WITH DIABETES TREATED WITH POTENTIALLY HYPOGLYCAEMIC MEDICATION
UNITED KINGDOM CIVIL AVIATION AUTHORITY
OPERATIONAL TEST REPORT
1) Candidate’s Personal Details:
Name
(in full):
........................................................................
CAA
Ref No:
........................................................................
Date
of Birth:
......../......../........
Current
Address:
.........................................................................
..........................................................................
..........................................................................
Telephone
Numbers
Home:
.............................................
Work:
.............................................
Mobile:
2)
Purpose of
test:
.............................................
To determine that the applicant demonstrates knowledge of the aeromedical issues relevant to diabetes
and demonstrates safe management of their health condition whilst exercising licence privileges
3) Declaration:
I understand the purpose of the operational test
Signature of candidate ......................................Date ......../......../........
Name of ATCO: …………………………………………………..CAA Ref No ........................................
12
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department

13
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
4) Operational Test Report (To be completed by Watch Manager)
Job role (e.g. area, approach, tower): ..........................................................................................
Duty period(s) assessed: .............................................................................................................
Date & Place of Test: ......../......../........ - .......................................................................................
Examiner's Name (please print): ..................................................................................................
Examiner’s CAA Licence No: .......................................................................................................
Blood Testing Machine Used: ......................................................................................................
Acceptable
Appropriate briefing on diabetes conducted using UK CAA briefing sheet…………………Yes/No
Spare blood testing machine available ..............................................................................Yes/No
Where an insulin pump is used, alternative delivery method available ........................Yes/No/N/A
Availability of carbohydrate – state what............................................................................Yes/No
Appropriate stowage of medication/equipment/resources ..................................................Yes/No
Check operational blood glucose testing records and glucose memory meter congruity ....Yes/No
Evidence of compliance with blood testing in accordance with relevant protocol................Yes/No
Tests conducted in safe manner without interference with safe operations ........................Yes/No
Time
Result
& Comments
Time
Result
& Comments
Appropriate stowage of equipment/resources ....................................................................Yes/No
Availability of carbohydrate – state what............................................................................Yes/No
Comments:
Recommendations (e.g. any type/class-specific issues)
Signed ................................................................................................. Date ......../......../........
Return completed form to: CAA Medical Department, Aviation House, Beehive Ring Road,
Crawley, West Sussex RH6 0YR

14
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
11. Information for Operators on Flight Crew with Insulin-Treated Diabetes
Summary
Operators may have flight crew who develop diabetes requiring insulin who wish to return to flying
once their condition has stabilised or may recruit a pilot with this condition. This guidance provides
information for operators and should be read in conjunction with the document ‘‘The Medical Assessment
Protocol for Pilots with Diabetes Treated with Insulin and/or Potentially Hypoglycaemic Medication”.
Background
Diabetes
Insulin is a hormone produced by the pancreas which controls blood glucose (sugar) levels. Diabetes
develops when there is insufficient insulin or it cannot be effectively used by the body and blood sugar
level regulation becomes unbalanced.
Treatment is often with medicines (tablets or insulin injections) that allow the body to use the circulating
sugar, thus keeping the blood sugar level in the normal range. High levels occur if not enough medicine
is taken/used or too much carbohydrate is eaten and low levels can occur if toomuch medicine is
taken/used or not enough carbohydrate is eaten to balance the medicine.
Pilots with insulin-treated diabetes
A Class 1 medical certificate is only issued to a pilot on insulin if they fulfil stringent criteria including
demonstration of excellent control of their diabetes.
Pilots with insulin-treated diabetes have to comply with the ARA.MED.330 protocol including frequent
blood sugar testing before and during a flight duty period to ensure their blood glucose levels remain
within an acceptable range. Hazards should be identified through the operator’s safety management
system (SMS) and the operator is responsible for putting in place measures to remove, or mitigate, the
risks of the identified hazards.
Examples:
Hazard
Mitigation
Incapacitation
due to low or high
blood
sugar level
•
Multi-pilot flying only in commercial operations.
•
Adherence to blood glucose mandatory blood glucose testing
protocol.
•
Awareness of the risk of not adhering to the protocol through
training and pre-briefing.
•
Cross checking of blood glucose results by other pilot(s).
•
Immediate consumption of carbohydrate in the event of a low
reading or if operational circumstances prevent blood glucose.
Sharps
injury from blood sugar testing
equipment
Use
of a self-contained testing system or a sharps box for lancet
after
use.
Distraction
of other pilot
Full
briefing in advance of flight duty.
Pilot
incapacitation not identified
All
pilots briefed in standard operating procedures in the event of a
pilot
becoming unwell or uncommunicative.

15
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
Considerations for operations manuals
a) General (these items are likely to be included already)
Pilot responsibility - decrease in medical fitness
The operations regulations contain requirements for crew not to perform duties when unfit orif aware
of any decrease in their medical fitness that might render them unable to safely exercise licence
privileges.
Incapacitation of pilot
Any incapacitation, whether sudden or subtle, should be handled in the same way as any othermedical
incapacitation.
Training for pilot incapacitation
Training on how to recognise pilot incapacitation and the standard operating procedures to follow
in the event of pilot incapacitation should be included in the annual SEP training.
b) Specific (these items may need to be added)
Possible symptoms of low or high blood sugar
Low
blood glucose
(hypoglycaemia)
(if
level less than 3)
High
blood glucose
(hyperglycaemia)
(if
level greater than 20)
Sweaty,
pale skin
Thirst
Mood
changes
Excess
urine output
Poor
concentration / distraction
Dehydration
Confusion
Mood
changes
Excessive
tiredness / sleepy
Blurred
vision
Pilot responsibilities - insulin-treated diabetes
Flight crew members must inform their line manager if returning to flying after being re- certificated
following a diagnosis of diabetes and being treated with insulin. In this circumstance, class 1 medical
certification will be subject to an operational multi-pilot limitation; the line manager should be informed
of any other operational limitations.
The pilot must comply with the schedule of blood glucose testing required by the UK CAA.

16
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
The pilot must brief the other member(s) of the flight crew (and other members of the crew as
necessary) before each flight on:
• The reason for blood glucose tests.
• How the blood glucose test is done.
• When blood glucose tests are required (including with reference to the flight plan).
• Actions to be taken in the event of a blood glucose test outside of the
acceptable range (below 5 or above 15 mmol/l).
• Whether, when and how insulin will be used during the flight duty period.
• Possible symptoms of low or high blood glucose.
• Actions to be taken by the pilot if a test is ‘out of range’.
Blood glucose test times should be pre-planned, by time from departure, waypoints, or by setting
up alarms - an iPad, phone or in-cockpit alarm could be used.
It is the pilot’s responsibility, when on duty, to carry any medication (e.g. insulin) required, any
equipment required to deliver the medication (e.g. pens and pumps) and documentary evidence from
their general practitioner or diabetes specialist confirming the need to carry the medication and
equipment. Sufficient medication and equipment should be carried to cover the planned duty period
and additional contingency for unplanned extensions. All equipment, medication and carbohydrate for
emergency consumption should be safely stored in the cockpit and immediately accessible.
Testing should always be undertaken ensuring compliance with standard operating procedures at all
times. The pilot should avoid testing blood glucose during ground manoeuvring in the vicinity of
runway holding areas or entering or crossing a runway, or in phases of flight associated with heavy
workload including the take-off and approach and landing.
The result of the blood glucose test should be spoken aloud by the pilot so that it is captured on the
cockpit voice recorder (CVR) and the test result should be shown to and cross-checked by the other
pilot.
The blood testing schedules are described in ‘Blood glucose testing’ (Section 3 above).
Blood glucose levels should be recorded in, and a comment made in the remarks column of, the log
book.
An example template for recording blood glucose levels is shown here:

17
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
UK Civil Aviation Authority
Blood Glucose Log (for pilots with diabetes)
Pilot name: CAA reference no:
A/C type: Flight no: Route:
Date and
time:
Flight phase:
Reading
(mmoL
-1
)
X-check:
Symptoms
Comments
Pre-Report
Pre-Flight
In Flight
Pre-Landing
Other
Crew
CVR
A record should be made of any snacks or meals taken, insulin used, any bunk rest and any corrective
action that was required in the event of a low or high result.
Any crew intervention required to assist a pilot in controlling their blood glucose levels is a reportable
event and should be reported under the MOR scheme and the pilot should declare themselves unfit.
Any failure to comply with the testing schedule is a reportable event and should be reported under the
MOR scheme.
Blood glucose testing must be done after every period of prolonged rest, 30 minutes prior to resuming
flight duties.
If the testing equipment is not self-contained, the lancet, needle and any clinical waste should be
disposed of in a single use sharps box.
The pilot should always carry a spare, functioning glucose meter with memory; if both meters become
unserviceable the pilot should hand over control of the aircraft to the other pilot. In this event it is
recommended that the autopilot should be engaged to reduce workload.
Emergency situations
If operational considerations prevent the pilot from undertaking a blood glucose test at the required
time 15g of rapidly absorbable glucose/carbohydrate (e.g. 3 jelly babies, 4 glucotabs) should be
consumed immediately and blood glucose testing done as soon as possible.
In an event such as a rapid decompression there would be no time to take precautionary carbohydrate
and priority would be given to flying the aircraft. Carbohydrate should be taken once the emergency
has stabilised. If a mask continues to be required, it could be quickly lifted, carbohydrate consumed
and the mask replaced within a couple of seconds. In any other emergency situation 15g carbohydrate
should be taken as soon as practicable.
If an operational emergency is prolonged, with no opportunity for blood glucose testing, this

18
of 18
Diabetes Certification Guidance
03/2023v6.1
Issued By: UK Civil Aviation Authority,
Medical Department
consumption of 15g carbohydrate must be repeated every hour. Blood glucose testing should be
undertaken hourly or more frequently if there was any concern about the pre-emergency glucose trend
or if a lot of carbohydrate has been taken over the course of several hours without the possibility of
testing.
If the pilot has an insulin pump, in the event of a decompression, it should be switched off and 15g
carbohydrate should be taken as soon as possible.
If the pilot is awoken from their bunk for an emergency, blood glucose must be tested prior to resuming
control.
Responsibilities of other pilot(s) (whether commander or not)
The operator may wish to inform the whole fleet that they may be rostered with a pilot with insulin-
treated diabetes so that flight crew who have any concerns about flying with another pilot using a
needle and syringe on the flight deck and periodically undertaking finger prick blood tests have the
opportunity to raise these concerns. Any pilot who is uncomfortable should notify their line
management to ensure this can be addressed through appropriate rostering.
The other pilot(s) should positively cross-check each blood sugar test result during the flight duty
period and confirm the result verbally.
The other pilot should respect the confidentiality of any medical information shared by the pilot.
Responsibilities of the operator
The operator will need to ensure all additional operational procedures and information is promulgated
to all pilots in the fleet of a pilot with insulin-treated diabetes.
Flight manuals may need to be amended to include operational considerations for pilots and operators
of pilots operating with insulin-treated diabetes.
The operator will have access to confidential medical information about their pilot with insulin-treated
diabetes. The normal rules of medical confidentiality apply and must be respected at all times.
Flight crew with diabetes treated with medication other than insulin
Other medications that may lower blood sugar levels, e.g. sulphonylureas or glinides, may be used by
diabetic pilots to control their blood sugar levels. Pilots on these medications should be subject to the
same blood sugar tests, protocols and operational procedures as pilots on insulin. The only difference
is that the periodicity of the in-flight testing schedule is reduced to every 2 hours.
Pilots on glitazones, gliptins, GLP-1 analogues, biguanides, alphaglucosidase inhibitors only require
one pre-flight blood glucose check; if this is within the acceptable range, they do not need to undertake
further in-flight testing.
