
Gregory P. Beeler, Ph.D., M.A.,
Jennifer L. Murphy, Ph.D.,
Paul R. King, Ph.D., &
Katherine M. Dollar, Ph.D.
U.S. Department of Veterans Affairs
VA Western New York Healthcare System
Buffalo, NY 14215
November 1, 2016
Veterans Health Administration
Washington, DC 20420
Gregory P. Beehler, Ph.D. , M.A.
Jennifer L. Murphy, Ph.D.
Paul R. King, Ph.D.
Katherine M. Dollar, Ph.D., ABPP
Brief Cognitive Behavioral Therapy for
Chronic Pain: Therapist Manual
Version 2.0
ii
BRIEF CBT-CP IS FOR USE BY QUALIFIED CLINCIANS ONLY. THIS
PROTOCOL SHOULD BE REVIEWED IN ITS ENTIRETY BEFORE
BEING APPLIED TO PATIENT CARE.
THIS MANUAL AND RELATED MATERIALS SHOULD NOT BE
USED FOR RESEARCH WITHOUT PRIOR PERMISSION.
FOR ADDITIONAL INFORMATION
AND UPDATES PLEASE CONTACT:
Gregory P. Beehler, Ph.D., M.A.
Associate Director for Research
VA Center for Integrated Healthcare
VA Western New York Healthcare System
3495 Bailey Avenue
Buffalo, NY 14215
Phone: 716-862-7934
Email: [email protected]
Homepage: www.mirecc.va.gov/cih-visn2/
Suggested citation: Beehler, G. P., Murphy, J. L., King, P. R., & Dollar, K. M. (2021). Brief Cognitive
Behavioral Therapy for Chronic Pain: Therapist Manual, Ver 2.0. Washington, DC: U.S. Department
of Veterans Affairs.
iii
ACKNOWLEDGEMENTS
Support for developing this treatment manual was provided by the Department of Veterans
Affairs (VA) Center for Integrated Healthcare (CIH). Use of the facilities and resources were
provided by the VA Western New York Healthcare System at Buffalo and James A. Haley VA
Medical Center (Tampa, FL). The information provided in this document does not represent the
views of the Department of Veterans Affairs or the United States Government.
We wish to expressly thank Jennifer L. Murphy, Ph.D., John D. McKellar, Ph.D., Susan D. Raffa,
Ph.D., Michael E. Clark, Ph.D., Robert D. Kerns, Ph.D. and Bradley E. Karlin, Ph.D., the authors of
the original Cognitive Behavioral Therapy for Chronic Pain among Veterans: Therapist Manual,
who laid the foundation for this adaptation.
We also thank Drs. Thomas Farrington and Denise Mercurio-Riley who assisted in reviewing and
providing feedback in the development of this manual.
Most importantly, we wish to offer sincere thanks to the dedicated clinicians and Veterans who
inspired us to adapt this intervention.
iv
PREFACE
BACKGROUND
This manual includes information regarding the development of Brief Cognitive Behavioral
Therapy for Chronic Pain (Brief CBT-CP). The project is being led by contributors from CIH and
James A. Haley Veterans’ Hospital and developed for use by behavioral health providers who: a)
identify the need for a brief, focused intervention for chronic pain, or b) are not working in a
setting that can accommodate a full-length CBT-CP protocol. Incorporation of a Brief CBT-CP
treatment may be most appropriate for (but not limited to) providers working in the following
settings: Primary Care-Mental Health Integration (PCMHI), home-based primary care (HBPC),
outpatient/specialty mental health, or individuals working in consultation-liaison roles with
medical clinics (e.g., oncology, endocrinology, etc.). Individuals who are experienced in
delivering specialty pain interventions may also find benefit in this protocol, particularly if
briefer alternatives are needed based on setting-specific demands or patient preferences.
ORGANIZATION OF THE MANUAL
This manual is organized into multiple chapters. The initial chapters provide a rationale for
developing the brief intervention and an overview of foundational material about chronic pain.
The structure and components of Brief CBT-CP are summarized, and key contextual and clinical
considerations for addressing chronic pain are reviewed. Two case examples illustrate
indications for Brief CBT-CP. An approach to addressing measurement-based care with Brief
CBT-CP is described in depth as well as a chapter regarding how to engage new patients in
treatment.
Next, each treatment module is presented. The protocol requires that modules one and six are
stable anchors to begin and end the protocol. However, modules two through five can be
presented in any order, depending on the preference of the patient and clinical judgment of the
therapist. An important feature of each chapter is the inclusion of Therapist Guides. Each
module guide provides an overview of each appointment, including the key elements and
general recommended structure. They provide suggested language to introduce topics and key
talking points with patients. Module Outlines are one-page summaries of required steps to be
conducted in each appointment. These can be referenced in real time during your
appointments to keep you on track during your 30-minute appointment. Patient handouts are
an integral part of this treatment and in the first appendix for easy printing or duplication.
Several additional appendices include detailed information about pain conditions, specialty
pain treatments, and relevant mobile apps that can be used as an adjunct to Brief CBT-CP.
v
TABLE OF CONTENTS
1. RATIONALE FOR DEVELOPMENT OF BRIEF CBT-CP……………………………………………..1
2. FACTORS TO CONSIDER WHEN SELECTING BRIEF CBT-CP……………………………………4
3. INTRODUCTION TO CHRONIC PAIN……………………………………………………………………7
4. CLINICAL CONSIDERATIONS WHEN WORKING WITH PATIENTS WITH CHRONIC
PAIN…………………………………………………………………………………………………………………..14
5. AN OVERVIEW OF BRIEF CBT-CP MODULE STRUCTURE…………………………………….18
6. MEASUREMENT-BASED CARE (MBC) WITH THE PEG………………………………………..21
7. THE HOOK: OFFERING PATIENTS BRIEF CBT-CP………………………………………………..27
● BRIEF CBT-CP PROTOCOL AND THERAPIST GUIDE ●
MODULE 1: EDUCATION AND GOAL IDENTIFICATION………………………………………….35
MODULE 2: ACTIVITIES AND PACING…………………………………………………………………..47
MODULE 3: RELAXATION TRAINING……………………………………………………………………59
MODULE 4: COGNITIVE COPING 1……………………………………………………………………….71
MODULE 5: COGNITIVE COPING 2……………………………………………………………………….80
MODULE 6: THE PAIN ACTION PLAN……………………………………………………………………88
REFERENCES……………………………………………………………………………………………………….98
APPENDIX 1: PATIENT HANDOUTS BY MODULE…………………………………………………101
APPENDIX 2: PAIN CONDITIONS………………………………………………………………………..142
APPENDIX 3: TREATMENT OPTIONS FOR CHRONIC PAIN……………………………………148
vi
APPENDIX 4: MOBILE APPS FOR PAIN AND RELATED CONCERNS…………………...….156
APPENDIX 5: GUIDED IMAGERY SCRIPT……………………………………………………………..159
1
1. RATIONALE FOR DEVELOPMENT OF BRIEF CBT-CP
The full course of CBT-CP treatment typically requires eleven 50-minute sessions delivered by
therapists with specialty training in behavioral medicine or those providers specially trained as
part of the VA’s EBP program. This approach of treating chronic pain as a specialty mental
health intervention is time and resource intensive. Because of the widespread occurrence of
chronic pain among the Veteran population, there is increased interest among VA providers to
be able to offer briefer versions that can be used in more flexible formats in a wider variety of
settings. Thus, this manual serves the goal of making CBT-CP more widely available in a
briefer format. Our hope is that by offering Brief CBT-CP, the overarching goal of improving
Veteran outcomes through chronic pain self-management will be met more effectively.
1.1. EVIDENCE THAT BRIEF TREATMENTS MAY WORK FOR CHRONIC PAIN
Research on briefer psychological treatments for addressing chronic pain are growing. There
are multiple factors and corresponding lines of research that underlie the development of Brief
CBT-CP. First, because chronic pain is a common condition, multiple types of interventions are
necessary to treat pain in a sufficiently patient-centered way across diverse settings and
populations. A brief treatment may be especially well suited for addressing pain early in the
trajectory of care with the goal of preventing functional disability and distress. Second, prior
research suggests that briefer versions of CBT-CP offered in primary care and various other non-
mental health settings are effective (Ahles et al., 2006; Buszewicz et al., 2006; S.K. Dobscha et
al., 2009; Lamb et al., 2010; Martinson, Craner, & Clinton-Lont, 2020; Moore, Von Korff,
Cherkin, Saunders, & Lorig, 2000; Smith & Torrance, 2011; Von Korff et al., 1998; Wetherell et
al., 2011). Since first developing Brief CBT-CP in 2017, subsequent evaluation has indicated that,
on average, participating in Brief CBT-CP is associated with clinically significantly improvement
in a composite measure of pain intensity and pain-related functional impairment (Beehler et al.,
2019). Additionally, patients report high levels of satisfaction and acceptability of Brief CBT-CP
(Beehler et al., in press). Third, providing psychological treatment in primary care is especially
important given that over half of patients in primary care report chronic pain (Kerns, Otis,
Rosenberg, & Reid, 2003). Primary care providers find pain management especially challenging
(Matthias et al., 2010) and, according to Dobscha and colleagues, have reported dissatisfaction
with their ability to provide optimal pain relief for their patients (2008). Fourth, chronic pain
commonly co-occurs with mental health conditions such as depression, anxiety, and PTSD.
Thus, mental health providers may be especially well-suited for addressing chronic pain and
associated distress given the common CBT-based model of intervention. Finally, local
availability of pain resources and interventions may vary considerably across clinics. Thus, Brief
CBT-CP provides an additional, more accessible alternative.
2
1.2. BRIEF CBT-CP: ADAPTED FROM THE VA EBP
Brief CBT-CP as described in this manual has been adapted from the full-length VA treatment
(Murphy et al.). The authors of Brief CBT-CP, who are subject matter experts in the areas of
chronic pain management and integrated care, developed the protocol with several factors in
mind. Research indicates that CBT-CP is an effective treatment for chronic pain, but dismantling
studies do not provide sufficient guidance to suggest which specific components of CBT are
responsible for effective treatment outcomes. Thus, Brief CBT-CP includes an adapted version
of each key CBT-CP element: psychoeducation/goal setting; behavioral skills: activities,
pacing, and relaxation training; cognitive coping; and relapse prevention. Brief CBT-CP mirrors
the full-length CBT-CP currently disseminated throughout the VA as part of the EBP initiative
(Stewart et al., 2015).
1.3. BRIEF CBT-CP EMPHASIZES PATIENT-REPORTED OUTCOMES
A key component of this protocol is the use of patient-reported outcome measures
throughout the intervention. Use of brief validated measures to capture patient-reported
outcomes (e.g., routine assessment of pain intensity, distress, functional interference, and
others) at each module are strongly recommended in order to inform both patient and provider
about patient response to treatment. Previous research has indicated that routine outcome
monitoring is important for identifying patients who are not responding to treatment, with
continued monitoring useful for capturing patients’ response to treatment modifications
(Carlier et al., 2012; Scott & Lewis, 2014). Routine outcome monitoring will also aid the provider
in identifying patients who need a “step up” to a higher level of care. Specific instruction in
conducting measurement-based care as part of Brief CBT-CP is provided in a later chapter.
1.4. BRIEF CBT-CP IS DESIGNED FOR A DIFFERENT SETTING AND PURPOSE
Although Brief CBT-CP is not designed exclusively for primary care settings, efforts were made
to adapt CBT-CP to the PCMHI service delivery platform that has relatively unique features,
such as sessions of 30 minutes or less, highly focused brief assessments, an emphasis on
improving functional outcomes, and an emphasis on early detection and prevention.
Brief CBT-CP is designed to introduce patient self-management, improve pain self-efficacy,
reduce functional limitations, and potentially reduce self-report ratings of pain and negative
impacts of pain. Brief CBT-CP may be a used in a variety of ways depending on the clinical
context, provider, and patient. For example, a PCMHI provider may wish to use Brief CBT-CP for
patients with distress and functional limitations that stem from chronic pain. Specialty mental
health providers, behavioral medicine providers, or those in consultation-liaison roles may wish
to use Brief CBT-CP alone or as an adjunct to other medical or psychological therapies. Similarly,
even a pain specialist who usually provides full-length CBT-CP may wish to use the brief version
to meet the needs of patients who prefer or need a shorter treatment.
3
After a course of Brief CBT-CP, there are several potential options for disposition of the patient.
For some, no additional treatment will be necessary. Other patients may benefit from
occasional follow-up or booster sessions over the subsequent months to help with fine-tuning
the application of skills developed in Brief CBT-CP. Some patients may choose to continue with
their routine mental health treatment focused on depression, anxiety, or other psychiatric
concerns. Other patients may ultimately benefit from continuing on with a full course of CBT-CP
or additional pain-related psychosocial and rehabilitative interventions.
4
2. FACTORS TO CONSIDER WHEN SELECTING BRIEF CBT-CP
2.1. BEFORE BEGINNING BRIEF CBT-CP
Selection of this protocol assumes that providers have identified that brief intervention for
pain-related issues is clinically indicated. Because detailed training in the foundational and
functional elements of CBT clinical skills are beyond the scope of this manual, we recommend
that providers who wish to implement Brief CBT-CP have completed prior training in the basic
principles of CBT.
NOTE: Brief CBT-CP assumes that the patient has completed at least one appointment with a
mental health provider who has conducted an initial assessment appropriate to the practice
setting (e.g., functional assessment and mental health screenings typical of the PCMHI
setting; psychosocial history for a specialty mental health clinic).
2.2. ADDING BRIEF CBT-CP TO YOUR CURRENT PRACTICE: PROVIDER AND
SETTING FACTORS
Adopting a patient-centered stance is essential for conducting CBT-CP, including this brief
version. Following the biopsychosocial model, a patient-centered approach is required so that
the therapist can use patient-identified goals to direct the course of care. Patients are likely to
have a variety of concerns that are impacted by their experience of chronic pain. Thus, it is
essential to elicit from them their primary concerns. In this way, patient-centeredness is not
only a general approach to engaging the patient, it is critical for ensuring Brief CBT-CP is being
applied in a way that will be most useful.
This protocol has been designed to meet the needs of generalist mental health providers. It is
therefore important to consider that, at times, additional support from specialists may be
necessary. We advise that you identify your clinic or facility’s behavioral medicine or chronic
pain specialist(s) who can provide additional clinical support to you or act as an additional
referral source should your patient wish to engage in longer-term treatment or require a
higher level of care. It may also be helpful to coordinate care with the patient’s prescriber who
will play a key role in medical management of pain. The prescriber may find it valuable to know
that the patient is working toward better self-management.
5
2.3. DETERMINING WHO MIGHT BENEFIT FROM BRIEF CBT-CP
Brief CBT-CP will not be suitable for all patients, so clinical judgment must be used when
determining who might be best served by Brief CBT-CP. Patients who are particularly likely to
benefit from Brief CBT-CP include those with one or more of the following characteristics:
• Mild to moderate functional impairment and distress
• No severe mental health disorder or substance use disorder impacting overall function
or suggesting imminent safety risk
• Patient receptiveness to non-pharmacological self-management approaches for pain
Note: The above characteristics are comprised of suggestions only and should not be
interpreted as a list of inclusion criteria.
Finally, we provide two prototypical examples of patients who are appropriate for Brief CBT-CP
below:
2.4. BRIEF CBT-CP CASE EXAMPLE 1: PCMHI SETTING
Jeff is a 26-year-old White Veteran who recently enrolled in VA primary care services after
separating from active service in the Marine Corps six months ago. Routine mental health
screening by his primary care provider resulted in a referral to PCMHI staff for concerns related
to mood. Further evaluation by the clinic’s psychologist uncovered that chronic low back pain
stemming from his combat deployment is a significant contributor to his feeling irritable, and
that over-the-counter analgesics have offered limited pain relief. Jeff noted that his back pain,
rated as a five on the Numeric Rating Scale, has increasingly interfered with his sleep, ability to
sit through college classes, and interactions with his young son. He has become increasingly
concerned that pain will impact his long-term goal of operating his own business. He is
frustrated by what he describes as a near constant dull ache over the past two years, and
wonders if it will improve. Considering Jeff’s endorsement of moderate chronic pain and its
interference with daily activities, the clinic psychologist discusses both mood and pain
management options with Jeff and his primary care provider. Though Jeff has never attempted
cognitive behavioral self-management of his pain symptoms, he appeared eager to learn more
about managing pain, particularly through implementation of techniques that he can use on his
own. Further, he wishes to receive the bulk of his medical and mental health care in his primary
care clinic. Therefore, Jeff and his treatment team agree to incorporate Brief CBT-CP into their
collaborative approach to care.
2.5. BRIEF CBT-CP CASE EXAMPLE 2: BEHAVIORAL MEDICINE SETTING
Paulette is a 65-year-old African American Navy Veteran who is finishing treatment for colon
cancer. Her level of fatigue has increased as she completes her course of chemotherapy, which
has contributed to decreased mood and limited engagement in hobbies and social activities.
6
She has a relatively new post-surgical abdominal pain following her initial cancer surgery six
months ago. Additionally, she was diagnosed with moderate arthritis of the right knee over 10
years ago which has become more bothersome in the last several months. The infusion clinic
nurse identified that Paulette’s Numeric Rating Scale for pain is a seven, suggesting clinically
significant pain in need of additional intervention. Upon further discussion with the infusion
nurse, Paulette also reported increased frustration with her multiple sources of pain that are
clearly interfering with daily routines. The infusion nurse informs the oncologist who suggests a
new course of NSAIDs with the option of as-needed hydrocodone for more significant pain
flare-ups. Paulette agrees to try the NSAIDs, but is disinclined to use opioids due to concerns
over side effects. The oncologist also requests a referral from the behavioral medicine
consultant who contacts Paulette during her last chemotherapy treatment the following week.
Paulette reports that her pain is slightly better using the new medication but continues to be
disruptive. She also reports moderate depressive symptoms on the PHQ-9. Paulette does not
use any non-prescription drugs, but reports that she has been consuming more alcohol recently
in the evenings to help with sleep. As Paulette has been reporting to the VA frequently over the
last nine months since first diagnosed with cancer, she is eager to finish her treatment but does
not want to engage in extended sessions of psychotherapy. She is, however, willing to try the 6-
week course of Brief CBT-CP to help with pain management.

7
3. INTRODUCTION TO CHRONIC PAIN
3.1. WHAT IS PAIN?
According to the International Association for the Study of Pain (IASP), pain is defined as an
unpleasant sensory and emotional experience associated with actual or potential tissue
damage, or described in terms of such damage (IASP, 1994). This definition stresses that pain is
both a subjective physical experience (i.e., unpleasant bodily sensations) and emotional
experience (i.e., distress related to bodily sensations).
3.2. THE DIFFERENCE BETWEEN ACUTE AND CHRONIC PAIN
Pain can be either acute or chronic in nature (Institute of Medicine, 2011) as described below:
Acute pain has a short duration and is typically characterized by an identifiable injury or
disease. Some acute pain is expected to occur in response to health events, such as childbirth
or following surgery. Acute pain usually subsides over time as the body heals, and often
responds to standard medical treatments.
Chronic pain is an ongoing or recurrent pain lasting beyond the usual course of acute illness or
injury. Chronic pain typically lasts more than three to six months and adversely affects the
individual’s well-being. There may not be a clear underlying physiological cause to chronic pain.
Table 1. COMMON SOURCES OF PAIN
Common Sources of Pain
Acute
Chronic
Infection
Migraine/headache
Dental conditions
Arthritis
Burns
Fibromyalgia
Trauma
Irritable Bowel Syndrome
Surgery, other procedures
Trauma
Childbirth
Shingles
Musculoskeletal disorders (e.g., low
back pain)
Note: A detailed listing of additional pain conditions is located in the appendices.

8
Although it is important to adequately treat both acute and chronic pain, this manual focuses
only on the treatment of chronic pain. Psychosocial treatment of chronic pain is especially
important because of the well-established connection between chronic pain and diminished
quality of life, functional limitations, and psychological distress.
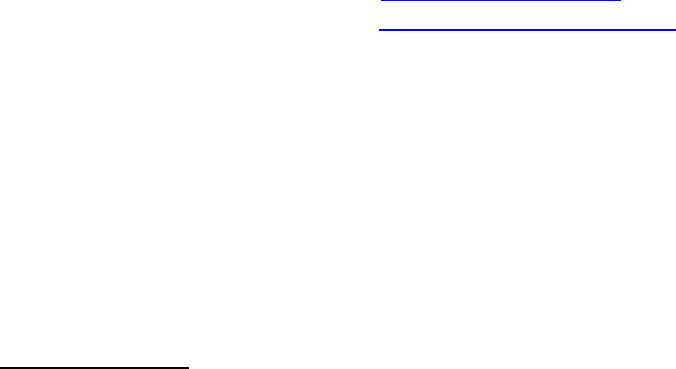
3.3. ADDRESSING CHRONIC PAIN IN THE VA: THE STEPPED CARE MODEL FOR
PAIN MANAGEMENT
There is a wide array of treatments for individuals with chronic pain. As shown in Figure 1, the
VA has adopted a stepped care model for pain. Stepped care is designed to adjust the intensity
of intervention based on patient presentation and response to care. The foundational step of
the VA model reflects the importance of routine self-care, from weight management to being
engaged in a safe and supportive social and physical environment. Step 1 includes care from
Patient Aligned Care Teams, or PACTs, who manage the majority of patients with chronic pain.
In the event that additional intervention is needed beyond services offered in PACTs, the
second step of this model includes referral to chronic pain specialists. The third step of care is
reserved for the most complex patients who require treatments such as coordinated
interdisciplinary programs. At all levels, stepped care for chronic pain stresses the importance
of a biopsychosocial perspective which considers not only traditional biomedical factors
(underlying pathology, pharmacological treatment, brief advice administered by a medical
provider) but also the psychological, behavioral, and social factors that impact Veterans with
chronic pain. Furthermore, stepped care at all levels endorses team-based approaches to care
with an increasing emphasis on patient self-management approaches.
Although the VA stepped care model suggests certain services for each step, the actual
availability of these services may vary by location. For example, Step 1 includes support from
the PCMHI provider in variety of ways, including Brief CBT-CP. PCMHI providers at a given
facility may or may not be prepared to provide support specifically for chronic pain
management. However, most are likely able to assist patients in adjusting to their pain
condition or by addressing comorbid mental health conditions. Alternatively, some PCMHI
providers will have behavioral medicine backgrounds that will allow them to take a more
diverse role in chronic pain management. This manual is well-suited to PCMHI providers who
are either new to chronic pain management or who desire to implement a brief treatment for
pain adapted from an evidence-based protocol.
9
Figure 1. VA's Stepped Care Model for Pain Management
3.4. UNDERSTANDING CHRONIC PAIN
Chronic pain is a complex phenomenon. As such, there are a number of conceptual models that
have been developed to explain the etiology and nature of pain. Currently, the biopsychosocial
model (Engel, 1977) is the most widely accepted approach to understanding chronic pain. The
biopsychosocial model (see Figure 2 below) suggests that the experience of pain is
multifactorial, with a wide array of physical, psychological, social, and other environmental
factors that may play a role in perpetuating pain.
For example, the biopsychosocial model suggests that in addition to the physiological basis of
their pain, an individual’s thoughts, behaviors, and social relationships are all important
contributors. Importantly, this model suggests that there are multiple points of intervention for
addressing chronic pain, from medical treatments, to psychological interventions, to
modifications in one’s social environment.

10
Figure 2. The Biopsychosocial Model
3.5. TREATING CHRONIC PAIN
Chronic pain can be treated through a wide array of modalities. Some of the most common
biomedical approaches are summarized in Table 2, with additional details and descriptions of
these approaches available in the appendices. Although treatments that address the
physiological contributors to pain are important to pain management, individual responses to
these treatments may vary considerably. Often, patients and providers will need to work
together to identify the best approaches for optimal pain care.
In addition to these biomedical-based treatments that address the physical domain, applying
self-management and relevant psychological and physical therapies are essential since all
dimensions of the biopsychosocial model must be addressed.

11
Table 2: BIOMEDICAL MODALITIES FOR TREATING CHRONIC PAIN
3.6. COGNITIVE BEHAVIORAL THERAPY FOR CHRONIC PAIN (CBT-CP)
There are several evidence-based psychological therapies that have been shown to improve
outcomes for patients with chronic pain. Among these, Cognitive Behavioral Therapy (CBT) is a
widely researched, time-limited psychotherapeutic approach applied to numerous mental and
behavioral conditions. CBT involves a structured approach that focuses on the relationships
among cognitions (or thoughts), emotions (or feelings), and behaviors. Treatments based on
cognitive behavioral theory have been successfully applied to the management of chronic pain,
either delivered alone or as a component of an integrated, multimodal, and interdisciplinary
pain management program. Evidence suggests that CBT-CP improves functioning and quality of
life for a variety of chronic pain conditions (Williams, Fisher, Hearn, & Eccleston, 2020).
CBT-CP is an approach rooted in the development of a strong therapeutic relationship that
encourages clients to adopt an active, problem-solving approach to cope with the many
challenges associated with chronic pain (Burns et al., 2015). Currently, the VA has endorsed
CBT-CP and developed a full-length treatment currently available as part of the Evidence-Based
Psychotherapy program (Murphy et al.). Use this link to download the manual.
Biomedical Modalities for Treating Chronic Pain
Pain-relieving medications (i.e., analgesics)
• Non-opioid analgesics
• Opioid analgesics
• Topical analgesics
• Muscle relaxants
• Adjuvant analgesics
• Headache-specific analgesics
Invasive medical treatments
• Epidural steroid injections
• Nerve blocks
Non-invasive treatments
• Physical therapy
• Cold/heat
• TENS
• Complementary and Integrative Treatments

12
The value of CBT-CP is its focus on improving patient self-management to positively impact
the chronic pain cycle shown below. The pain cycle (see Figure 3) illustrates how the
experience of pain can lead to maladaptive changes in behavior that ultimately lead to
increased distress, decreased activity, and a chronic course of pain. The experience of pain
often leads to decreased activity out of fear of increased pain associated with movement.
Limiting one’s otherwise beneficial activities can lead to physical deconditioning and
disengagement from pleasurable or otherwise meaningful activities and life events. The
persistence of chronic pain and disengagement from valued activities can lead to increased
emotional distress, negative thinking, and decreased motivation that result in further
disengagement. The resulting state of disability is reinforced by ongoing maladaptive coping.
Figure 3. The Chronic Pain Cycle
CBT-CP can provide patients with both a new perspective and new coping skills to increase
self-efficacy and break the cycle of chronic pain. The goal of CBT-CP is to identify and modify
maladaptive cognitions and behaviors that perpetuate pain-related distress and dysfunction.
CBT-CP is based on cognitive behavioral theory which focuses on the impact of cognitive
processes on affective states and resulting behaviors (Beck, 1995). The suffering associated
with chronic pain often leads to a maladaptive disengagement from people, places, and events.
Like all CBT approaches, CBT-CP draws from both behavioral theory and cognitive theory.
Behavioral theory is based on the premise that distressed individuals get a very low rate of
positive reinforcement from their environment. Because they experience few benefits of
engaging in activities (and engaging in certain activities may lead to more pain), they tend to
disengage. As they disengage from activities and people, they become more distressed and
enter a cycle of inactivity and spiraling depression. A key target of behavioral intervention is
13
behavioral activation (i.e., helping people to re-engage in pleasurable events or find new
activities).
In the case of chronic pain, certain physical movements or activities can lead to increased pain.
Pain may also be interpreted as a warning sign that certain movements or activities are unsafe
and result in harm or damage. It is not difficult to see why people with chronic pain stop
participating in certain events. Thus, we must find new ways of engaging in favorite activities
that will be less likely to produce pain. Ways of addressing physical inactivity, such as pacing,
are a key behavioral component of CBT-CP.
According to cognitive theory, the way we perceive, think about, or interpret an event impacts
our emotional experiences. Therefore, monitoring and understanding our thoughts is essential
to facilitating change. Automatic thoughts are those that occur immediately in response to an
event/situation, but often go unnoticed. Sometimes automatic thoughts occur in relation to
internal events, such as increased pain. If the automatic thought is unhelpful or maladaptive,
we may experience an unpleasant reaction at the emotional, physiological, and/or behavioral
level.
A particularly common type of these automatic negative thoughts around pain is known as
catastrophizing. Catastrophizing is a distorted thought process of imagining or assuming that
pain will lead to the worst or most intolerable outcome, such as “My pain will never go away”
or “My pain will ruin my life.” Treating the cognitive components of chronic pain includes
teaching patients to self-monitor and ultimately modify their maladaptive negative cognitions
in favor of more balanced thinking.
3.7. SUMMARY
The key operational components of CBT-CP involve breaking the chronic pain cycle by:
• Increasing engagement in healthy and pleasurable activities
• Enhancing positive pain coping skills, such as pacing and relaxation activities
• Correcting faulty assumptions and thoughts about pain
• Improving self-efficacy regarding management of pain symptoms
14
4. CLINICAL CONSIDERATIONS WHEN WORKING WITH PATIENTS WITH
CHRONIC PAIN
4.1. INTRODUCTION
Veterans who have chronic pain present with various levels of functional impairment and all
have their own pain story. In addition to the physical strain of managing chronic pain each day,
their suffering may have significant emotional and social dimensions as well. Often times,
Veterans with pain have seen numerous healthcare providers regarding their condition and
may feel frustrated with not receiving answers that they find satisfying regarding the etiology
or treatment of their pain. Perhaps most importantly, those with chronic pain may feel as if
they have not been “heard” adequately by providers. Various patient reactions can be driven
by the perception that insufficient time, attention, or care has been paid by healthcare
professionals when they are suffering each day.
As with all therapies, using CBT for the management of chronic pain requires the development
of a strong rapport. While Veterans may resist being introduced to another provider, especially
one in the mental health field, creating an environment where the Veteran is heard and
believed fully is a key to success. It is not the role of the therapist to determine the veracity of
the physiology of the pain complaint - pain is a subjective experience that is affected by
various factors. The functional impacts experienced by the Veteran should be the focus of
treatment, with clear education and direction offered as ways to positively alter the pain
experience.
While there are many challenges that may arise when treating Veterans with chronic pain,
some common topics that may impede therapeutic progress (with ideas for how to address
these complex issues) are reviewed in this section.
4.2. LOSS, GRIEF, AND ACCEPTANCE
Those with chronic pain may display certain responses to their condition and it can be
beneficial to help them identify and understand what they are feeling. For many, adjusting to
pain-related losses is one of the biggest barriers to treatment progress. Loss of identity,
confidence, well-being, and relationship/vocational roles are frequently recurring issues. Since
it is challenging to cope with and accept that the “old me” is gone, it is important to normalize
this response when working with patients since they have experienced a difficult and
unexpected shift.
It may be useful for both patient and therapist to conceptualize the advent and experience of
chronic pain as a significant loss. Kubler-Ross’ well-known and non-linear five stages of grieving
(Kubler-Ross, 1972) can be applied to better process the emotional process. The denial stage
may involve being “stuck” in the biomedical model with cognitions such as, “there must be
something to fix this.” Anger is common throughout the chronic pain experience. Individuals
15
may feel frustrated with the perception that doctors are not helping them or loved ones do
not understand. They may also feel anger about the perceived injustice of their situation -
dealing with pain every day that is not their fault, not being able to do what they want, finding
little relief in treatments. Those reactions may be even more extreme in those that are
younger since it feels particularly unfair. Bargaining and “if only” thoughts as well as feelings of
depression around the reality of living with pain are often present.
Acceptance, the final “stage,” does not imply that it is “okay” to have chronic pain or that the
person is “fine with it.” Patients may react negatively to the word “acceptance” and it is
important to differentiate an active acceptance versus a passive giving up. Quite the opposite,
actively accepting that life has changed and may be very different than what was previously
hoped for or planned is critical in moving forward. There is no suggestion in these stages that
one should “get over it” but instead be able to eventually ask themselves, “now what?”
Acceptance is a process and it takes time. While there is no right way to grieve the losses that
accompany life with a chronic medical condition, it may be helpful to encourage patients to
concentrate on living the life they have instead of focusing on the one that used to be. These
are difficult concepts to discuss, but being open about them helps individuals feel better
understood, less alone in their experience, and better able to take steps toward self-
management. Life can still be meaningful and fulfilling even when someone has pain, even if it
looks different than what was originally imagined.
Use of measures, such as the Chronic Pain Acceptance Questionnaire (McCraken, Vowles, &
Eccleston, 2004), may provide helpful information regarding where someone is in the grieving
process as well as evidence of positive progress during treatment.
4.3. MEDICATION MANAGEMENT
When treating individuals with chronic pain, issues frequently arise around medications and
medical procedures. Some Veterans may be highly focused on obtaining a particular
medication or treatment or they may be frustrated by pills being “pushed” on them without
alternatives offered. Regardless, because medications are typically a first line treatment for
pain, they are often an integrated part of daily life.
One frequent medication-related issue that arises in the context of treating individuals with
chronic pain involves the use of opioid analgesics. Opioids have increasingly been prescribed to
treat chronic pain in recent years, but an increased risk of adverse events (including accidental
overdose) has led to heightened regulation around their use. A lack of evidence supporting
long-term opioid therapy as well as side effects such as sedation, constipation, and the
possible need for tolerance-related dose escalation are all areas of concern. Veterans who
have had opioids decreased or discontinued may be opposed to these changes, upset, and
angry. When this is the case, medications may become a focus area by the patient, leaving
clinicians feeling a sense of helplessness and desire to “resolve” the issue.
16
Not specific to opioids is the more general belief by Veterans that "there must be something"
that can reduce their pain. This manifests in many forms, from a medication that they have
seen advertised on television to a firmly held conviction that they “need” surgery because a
physician mentioned it many years ago. Regardless of the details, this supports a belief that
pain is unidimensional and that a medically driven “fix” exists.
Educating patients about the biopsychosocial approach to pain and the many factors that can
impact the pain experience can be helpful. Allowing Veterans to vent about their medical
frustrations may be necessary, but allowing sessions to be derailed by these tangents is
problematic. Clinicians should acknowledge patient frustrations, encourage them to speak to a
prescriber, and then redirect the focus back to the skills that can be addressed in this
treatment. While therapists sometimes feel as if they are being insensitive or unsupportive by
providing such clear redirection, it is most therapeutic for patients to focus on what they can
change and control versus external factors.
4.4. OPIOID USE DISORDER
Opioid Use Disorder (OUD) is a DSM-5 diagnosis signifying a problematic pattern of opioid use
associated with impairment and distress. In addition, at least two of a group of other
symptoms must be present, including taking more or using more for than intended, ongoing or
repeated attempts to control use, related physical or psychological problems, and spending
excessive time in opioid-related activities. Due to the nature of opioid analgesics, developing
physiological dependence over time as one does with nicotine is expected and does not
indicate problematic use by patients. However, once opioids become a focus of attention with
various related adverse consequences, patients should be evaluated for OUD.
Some Veterans on opioids may struggle with suggested changes in their medication regimen.
They may resent feeling labeled as “drug seeking” when they request increased doses to feel
better, often a result of tolerance. They may be angered with suggestions to decrease or
discontinue opioids for risk mitigation when they are pleased with opioids’ effects, even if
those do not include significant pain reduction. Furthermore, since opioids were typically
initiated by a prescriber, they may feel “punished” with alterations in dosing schedules. In
these cases, it is again important to acknowledge and normalize Veterans’ feelings. The focus
should then return to the message that pain is multidimensional and must be addressed from
various approaches. While medication may provide limited relief, the skills being reviewed in
Brief CBT-CP can help improve overall quality of life. When Veterans are fixated on idealizing
medications, it may be useful to return to the facts that have been gathered from them
regarding their less than ideal level of functioning. Finally, it may be helpful to remind patients
that they are in control of using the skills in this treatment - they do not need to rely on a
provider and can self-manage their symptoms.
17
4.5. SLEEP
Sleep problems are among the most common complaints voiced by individuals with chronic
pain and the relationship between sleep and pain is complex. The presence of pain may make
falling and staying asleep more difficult, and disturbed. Insufficient sleep may increase next
day pain. Sleep conditions such as insomnia are linked with inflammatory processes, which
may also impact the bidirectional relationship between sleep and pain. It is not unusual for
poor sleep to be identified as the most frustrating issue for those with chronic pain due to its
negative physical and emotional effects. Therefore, it is important to discuss sleep and
evaluate the needs of the Veteran related to this topic.
While basic education around sleep hygiene may be conveyed and incorporated into
treatment, as it often would be in the primary care setting, it is important to determine if
triage is necessary. For example, if sleep disordered breathing may be present and has not
been assessed, a consult for a formal sleep study is likely in order, particularly as the
prevalence of sleep apnea is significant in the chronic pain population. If sleep issues are
severe enough to meet the diagnostic criteria for insomnia, a referral for local Cognitive
Behavioral Therapy for Insomnia (CBT-I) treatment is indicated. Use of the Insomnia Severity
Index (ISI) may be helpful in differentiating whether a consult for more intensive sleep
intervention is appropriate. Completion of CBT-I prior to engaging in CBT-CP may increase
successful outcomes, but determining the preferred order should be evaluated and
determined individually with the patient’s preferences in mind.
4.6. WORKING WITH RESISTANCE
Those with chronic pain may be resistant to psychological interventions for pain for a variety of
reasons. One strategy that may be beneficial when encountering resistance is the use of
Motivational Interviewing (MI) techniques which are highly patient-centered. MI can be used
to facilitate Veterans’ motivation to make positive health behavior changes. Because it
assumes that individuals are ambivalent about change, it seeks to help them uncover their
own internal motivation. Using open-ended questions so that they can share about pain
openly, affirming their strengths, reflecting empathically, and summarizing their perspective
and the next logical steps may help minimize resistance to treatment.
As always, it is important to remember that Veterans with chronic pain are hurting, often
emotionally as well as physically. Although they may exhibit defensive attitudes initially,
acknowledging the difficulty of their situation, including potential lack of compassion by
providers, can help establish a more open and trusting working alliance.

18
5. AN OVERVIEW OF BRIEF CBT-CP MODULE STRUCTURE
5.1. TREATMENT MODULES
Brief CBT-CP assumes that a standard initial PCMHI session following the 30-minute schedule
has been completed prior to starting Module 1. Brief CBT-CP consists of six modules. The brief
protocol requires that modules one and six are stable anchors to begin and end the protocol.
However, modules two through five can be presented in any order, depending on the
preference of the patient or best clinical judgment of the therapist. If there is no alternative
order preference identified, the modules should be delivered as listed in Table 3.
Table 3: BRIEF CBT-CP MODULES
Because CBT-CP is based on a model of intervention that emphasizes education and skill
development, educational handouts have been developed for use within the modules and to be
applied during homework modules. Patient handouts are an integral component of this
protocol and included in the appendices.
5.2. MODULE STRUCTURE
The structure of the Brief CBT-CP protocol is similar across modules and includes:
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
4. Introduce the new material and answer questions
5. Discuss new home practice opportunity
6. Module wrap-up
Brief CBT-CP Modules
Module
Content
1
Education and Goal Identification: Pain education and development of treatment
goals
2
Activities and Pacing: Importance of engagement in activities using a thoughtful
approach
3
Relaxation Training: Relaxation benefits and techniques
4
Cognitive Coping 1: Recognize unhelpful thoughts that negatively impact the pain
experience
5
Cognitive Coping 2: Modify thoughts that are unhelpful when managing pain
6
The Pain Action Plan: Plan for independent implementation of CBT-CP skills and
identify additional follow-up needs
19
5.2.1. Introduce the module and confirming the agenda (1-2 minutes)
Offering a brief introduction to the module helps orient the Veteran to the topics that will be
covered while also providing the opportunity to ask Veterans if they have anything to add to or
modify about the topic. This allows the Veteran to influence the agenda and emphasizes the
collaborative nature of Brief CBT-CP. Because the Brief CBT-CP protocol is highly structured and
works under time-limited modules, it is important to acknowledge that events may occur that
warrant discussion and that may result in adjusting content covered in a specific module.
5.2.2. Ask about mood, complete the PEG, and discuss findings (3-4 minutes)
In addition to briefly and informally asking about current mood, completion of patient-reported
outcome measures is an essential component of this protocol. The next chapter of this manual
provides detailed instruction in how to engage in measurement-based care using the PEG (Krebs
et al., 2009). Briefly, the PEG is a well-validated three-item measure that assesses pain intensity
(P), interference in enjoyment of life (E), and interference with general activity (G). Because the
PEG is so brief, it should be administered at each session as part of measurement-based care.
Additional measures can be added at the discretion of the provider.
5.2.3. Review material from the previous module, including home practice (3-5 minutes)
Providing a brief review of material covered in the prior module can create continuity between
modules and allow the Veteran to raise questions as needed. Taking a moment to discuss
potential questions reinforces the collaborative nature of the intervention and reduces the
chance of important messages being misconstrued. Review of home practice is an essential
component of Brief CBT-CP and serves to build competency in the use of adaptive pain coping
strategies. It should also enhance Veterans’ sense of self-efficacy to manage their chronic pain
condition by implementing acquired skills in the “real world”.
5.2.4. Introduce the new material and answer questions (12-15 minutes)
The majority of time in each module should be spent introducing and discussing the new
material for the module. Provide a clear rationale to the Veteran for each topic. To ensure
understanding, elicit reactions from the Veteran to material covered. Through discussion that
involves active listening, cuing, and reinforcing learning in a supportive and collaborative
environment, the Veteran is able to acquire adaptive pain management skills.
5.2.5. Discuss new home practice opportunity (2-3 minutes)
After a new topic has been reviewed in the module, it is important for the Veteran to be able to
practice building and implementing the skill independently. Discuss helpful areas for home
practice with the patient. It is important that the Veteran understands the potential benefits of
engaging in the coping technique and how it is related to better managing the effects of chronic
20
pain. Practice should be discussed collaboratively to ensure that it is manageable for the
Veteran.
5.2.6. Module wrap-up (1-2 minutes)
Each module should include a concise summary of key points that emphasizes the value of
outside practice. This wrap-up also signals the end of the module and allows for the patient to
ask any remaining questions about content addressed or next steps.
21
6. MEASUREMENT-BASED CARE (MBC) WITH THE PEG
6.1. WHY MBC?
Limiting excessive use of assessment tools in the context of everyday integrated care practice is
critical given time constraints; however, outcomes measurement is essential. Measurement
allows the clinician to better understand the Veteran’s experience of pain and the functional
domains that are impacted. Measurement also allows assessment of progress throughout
treatment and information generated can indicate when a change in practice is indicated. MBC
refers to the use of screening and ongoing symptom monitoring to guide treatment selection
and treatment modifications to improve outcomes for chronic health conditions (Morris, Toups,
& Trivedi, 2012). The aims of MBC are to rapidly and precisely diagnose conditions and to
evaluate patients’ response to intervention in order to improve treatment planning between
providers and patients (Harding, Rush, Arbuckle, Trivedi, & Pincus, 2011). Furthermore, it offers
patients a mechanism by which to track their progress and identify quantifiable goals for
treatment. The information from MBC can facilitate shared decision-making which includes
exploring options with the patient, weighing pros and cons of potential choices, and making
informed decisions in line with patient preference. MBC typically guides treatment for common
medical conditions in primary care, such as hypertension and diabetes, and has demonstrated
effectiveness in improving patient outcomes for these and other disorders (Klonoff et al., 2011;
Pickering et al., 2005). Similarly, routine monitoring of patient outcomes for mental health
conditions is associated with improvement in provider documentation of diagnosis, more rapid
treatment modifications, improved communication between patients and providers, and
improvement in patient mental health symptoms (Carlier et al., 2012). The VA strongly
endorses MBC for mental and behavioral health concerns and has been promoting the use of
MBC across mental health treatment settings since 2016 as part of a national initiative.
6.2 ADMINISTERING THE PEG
For Brief CBT-CP, the PEG (Krebs, et al., 2009) should be administered at every session, as
indicated in the module structure outline. The PEG includes three items. One item of the PEG
assesses pain intensity, and two items assess pain-related interference (i.e., enjoyment of life
and general activity). The PEG usually takes just a few minutes for patients to complete. The
measure can be completed on paper by the patient or administered verbally by the provider.
Scores should, however, be entered into the progress note for documentation. (Note that the
PEG is not included in this manual but is available as a supplemental .pdf document.) As a
helpful point of reference, research with primary care samples has estimated an average PEG
score of 6.1 (SD = 2.2) in this population, indicating a moderate level of overall pain and pain-
related interference (Krebs, et al. 2009).
6.3 CASE EXAMPLE: USING THE PEG IN EVERYDAY PRACTICE
A case example will be used to illustrate how to administer the PEG as part of Brief CBT-CP. Jeff
is a 26-year-old White Veteran who recently enrolled in VA primary care services after
separating from active service in the Marine Corps one year ago. Routine mental health
screening by his PACT provider and subsequent referral to PCMHI staff determined that chronic

22
low back pain stemming from his combat deployment is a significant contributor to his
irritability and depressed mood. Jeff’s back pain was rated as a 7 out of 10 on the Numeric
Rating Scale. He reports that pain negatively impacts his sleep, ability to sit through college
classes, and interactions with his young son. He is concerned that pain will impact his long-term
goal of operating his own business.
6.3.1. Establishing a baseline PEG and communicating findings
At Jeff’s first session of Brief CBT-CP with his PCMHI provider, his PEG scores were as follows:
Item
Score
Pain Intensity
7
Interference with life enjoyment
6
Interference with general activity
7
To determine Jeff’s baseline PEG score, simply compute an average score using the following
formula: (Item 1 + Item 2 + Item 3)/3 = average score. For convenience during clinical use, round
decimal points to the nearest whole number. This procedure is illustrated below:
To compute an average PEG score
Formula
(Item 1 + Item 2 + Item 3)/3
Example
(7 + 6 + 7)/3 = 6.6 = 7, if rounding
up
In this case, Jeff’s score is a 7 out of a possible 10, with 10 indicating the greatest severity. A
general guideline for interpreting 0-10 pain scales like the PEG is listed here:
PEG score
ranges
Qualitative description of level of
pain/interference
1-3
Mild
4-6
Moderate
7-10
Severe
In this case, Jeff was reporting severe overall pain and pain-related interference. Keep in mind
that scores of ≥4 indicate pain/interference that could benefit from intervention. Optionally,
consider reviewing the three PEG items separately, especially if they vary greatly (e.g., Pain
intensity = 8, Interference (life enjoyment) = 2, Interference (general activity) = 3). This
variability in items should be discussed to explore with the patient why there is a difference
between intensity and interference.

23
Part of establishing a useful baseline for Jeff is to utilize the score to enhance communication
with both the patient and the PCP. Scores at baseline (or any point in time) can convey current
status:
“Jeff, your score of seven on the PEG is in the severe range. This
score, along with the information you provided during our
discussion, indicates that you could benefit from starting Brief CBT-
CP…”
A discussion that incorporates patient-reported outcomes can also help fuel motivation to
engage in treatment:
“Over the next several weeks, we will use the PEG again to
monitor any changes in your pain ratings. These scores will help us
plan our next steps together. We will aim to have your score go
down over time as you apply new skills as part of Brief CBT-CP…”
This discussion can set a norm of using measurement as part of shared decision-making
between the patient and provider, while maintaining the focus of care on pain management and
restoring functioning.
In addition to discussing scores with the patient, conveying PEG scores to the primary care
provider (PCP) is also important. This type of communication not only improves flow of
information between providers, but ideally prompts the PCP to reinforce your plan for using
Brief CBT-CP when he or she interacts with the patient (e.g., motivating the patient to re-engage
in balanced, structured physical activity to avoid de-conditioning). The PCP may also consider
adjusting his/her own treatment plan (e.g., medication changes, adding adjunctive services such
as referral to physical therapy) depending on the information you convey.
6.3.2. Assessing for change over time
As mentioned previously, a primary reason for engaging in measurement at each session is to
be able to assess for meaningful changes in scores over the course of treatment. Stability of or
changes in scores are important for assessing response to treatment and can suggest times
when modification to a treatment plan is necessary. Assessing for change between two time
points is simple and can be computed quickly as follows:
To compute change in PEG scores
Formula
(Average PEG score at time 1 – Average PEG score at time 2)
Average PEG score at time 1
Multiplying the resulting figure by 100 will provide an estimate of percentage change in scores.
As a general rule, a 30% change (improvement) in pain-related scores, including the PEG, is
considered clinically significant in response to a course of treatment. Although a 30% decrease
24
is ideal, other meaningful patterns are also important to consider given the relatively short time
frame inherent to integrated care settings.
In Brief CBT-CP, less dramatic but potentially meaningful changes have been identified in our
pilot work (Beehler et al., 2019). Previously, as part of a clinical demonstration project, we
found, on average, a statistically significant 1-point decrease in PEG scores between session 1
and session 3. Although additional research is needed to replicate these findings under the
conditions of a rigorous randomized controlled trial, initial support for Brief CBT-CP is
encouraging.
Assessing for change can be done at any time frame, including when comparing the first and
third required modules. For example, note Jeff’s PEG scores below:
Module
PEG score
Module 1 (Education and Goal Setting)
7
Module 2 (Activities & Pacing):
7
Module 3 (Relaxation)
6
(7-6)/7 = 0.14 * 100 = 14% improvement
During this relatively short time frame common in PCMHI, these measures suggest no dramatic
changes, but a decreasing trend. This trend is encouraging in that there are no large
fluctuations in PEG scores that would suggest worsening of symptoms. If Jeff were to continue
on this course with additional Brief CBT-CP modules, the following pattern may emerge:
Module
PEG
score
Module 1 (Education and Goal Setting)
7
Module 2 (Activities & Pacing):
7
Module 3 (Relaxation)
6
Module 4 (Cognitive 1)
7
Module 5 (Cognitive 2)
6
Module 6 (Pain Action Plan)
5
(7-5)/7 = 0.29 * 100 = 29% improvement
In this case, additional improvement in PEG scores was realized by continuing with the
remaining Brief CBT-CP modules. Having reached a 29% decrease in PEG scores suggests a clear,
clinically significant improvement in outcome.
Of course, this is only one example of what you might find with the PEG. Below we discuss how
to address three different situations (i.e., beneficial change, no change, or worsening of
symptoms) over time. It is important to then discuss these changes with both the patient and
PCP in determining next steps.
25
6.4 USING THE PEG TO IMPROVE SHARED DECISION-MAKING
Discussing PEG scores, including changes in scores over time, can facilitate shared decision-
making in which the provider (or providers) work collaboratively with the patient to determine
the best course of treatment. Although a full description of the nature of shared decision-
making is beyond the scope of this chapter, there are a few general principles that should be
considered. According to Elwyn and colleagues (2012; 2017), shared decision-making is a
process that includes three general areas: 1) working as a team to identify choices in light of
patient goals; 2) discussing alternatives, such as the advantages and disadvantages of each
option; and 3) making an informed decision that aligns with patient preference. PEG scores can
help initiate the process of decision-making when the data indicate that change (or lack of
change) in symptoms is evident during or at the conclusion of treatment. Outlined below are
some general guidelines for using PEG scores to generate options for treatment decisions.
When PEG scores show sufficiently meaningful improvement over time, first confirm if the
patient concurs with this assessment. If the patient’s experience of pain or disability does not
appear to be reflected by the PEG scores, additional assessment may be necessary to
determine why there is a discrepancy. However, if the patient feels that sufficient improvement
has been achieved and treatment goals have been met, no additional treatment may be
necessary. Explore with the patient what an end to Brief CBT-CP means in terms of follow-up
options.
“One of the options for us to consider includes wrapping up your
treatment at this time. Based on the improvement we’ve seen in
your PEG scores and the fact that you’re meeting your main goal
of getting through your classes at college, you’re likely in a good
position to begin applying these skills on your own. If we decide to
end for now, my door remains open should you need to reconnect
with me, or another provider, regarding your pain or any other
concern that impacts your wellness...”
For many patients, knowing that they can return to PCMHI as-needed is sufficient. Other
patients may prefer to address additional concerns with you or another provider outside of
PCMHI now that their pain-related interference is under control.
In situations where PEG scores suggest that no meaningful change is evident, again confirm if
this finding is consistent with the patient’s experience. Additional discussion may be necessary
if the patient’s verbal report of response to treatment differs from PEG scores. If the patient
agrees that insufficient progress is being made, first discuss potential treatment barriers and
other factors that could have impacted patient adherence (e.g., not engaging in home practice,
change in patient goals for treatment). If the patient has had a difficult time with treatment
receipt (i.e., learning CBT skills) or enactment (i.e., using CBT skills outside of session), consider
if revisiting prior modules would be valuable for enhancing skills development.
26
“Let’s talk a little bit amore about what might be getting in the
way of moving forward. It sounds like it’s been a challenge to find
the time to apply the strategies we’ve discussed in session. One
option for us to consider is spend a moment to find times during
the day that might be best to apply one or more skills…”
Also consider if optional modules of Brief CBT-CP are appropriate. If additional discussion
suggests that Brief CBT-CP was not effective despite adequate patient adherence and interest,
consider stepping up the level of care for the patient to include referral to a pain specialty
provider or behavioral medicine expert.
When PEG scores suggest the patient is getting significantly worse over time, be certain to
confirm if this trajectory is consistent with the patient’s experience. Discrepancies should be
explored with the patient to determine why declines in PEG scores may not be reflective of the
patient‘s experience. Depending on the extent of the decline, first consider issues related to
patient safety and well-being. Additional suicide risk assessment should be conducted with
appropriate follow-up action taken as needed. Further assessment should be focused on
determining the cause of increased pain and disability, which may be transient (e.g., temporary
but repeated pain flare-ups due to overexertion) or stable (e.g., significant re-injury, new
medical or mental health diagnoses, negative life event/psychosocial factors).
“As you know, your PEG scores show that your pain and its
negative impact has become more significant since we first started
working together. I’d like to take a minute and talk with you a bit
more about what might be contributing to this situation from your
perspective. I’d also like to ask some questions about your safety
and well-being given how down you’ve been feeling. We might
want to consider adding some additional help alongside Brief CBT-
CP. Alternatively, we might consider whether or not services with
another provider who can offer more intensive support might be a
good option…”
Such factors likely suggest that stepping up to a higher level of care (e.g., referral to the
specialty pain clinic) or adding additional services (e.g., psychiatry) to the current course of
treatment may be indicated.

27
7. THE HOOK: OFFERING PATIENTS BRIEF CBT-CP
7.1. INTRODUCTION
The goal of offering an orientation to Brief CBT-CP is to provide the Veteran with a roadmap for
what can be expected during treatment and to establish clear expectations for both the
therapist and the Veteran. Brief CBT-CP can be introduced to patients any time chronic pain
management surfaces as a key concern for the patient’s wellbeing, provided that safety-related
concerns (e.g., lethality, significant neurocognitive disorder, psychosis) are absent or otherwise
addressed. Regardless of when Brief CBT-CP is introduced, it is helpful to provide a persuasive
but honest portrayal of the nature of the intervention and its potential to benefit the patient
The Therapist Guide that follows was designed to illustrate how to engage in a conversation
with the patient that can be addressed in 10 minutes or less as part of a brief, 30-minute
standard initial appointment or intake (Figure 4). We strongly recommend using this guide to
enhance motivation for treatment engagement. Of course, conversations about Brief CBT-CP
may need to be modified based on the level of patient receptivity.
The 5-A’s module
structure for initial
PCMHI appointments
(Figure 4) provides an
excellent approach for
how to introduce and
educate patients about
Brief CBT-CP. In short,
after conducting a
routine assessment of
patient functioning and
summarizing your
understanding of the
patient’s concerns (that
include the need for
chronic pain
management), the
remaining time can be
used to introduce the
patient to Brief CBT-CP,
answer questions, and
address potential barriers to full participation. If your treatment setting allows for
appointments of longer than 30 minutes, then the remaining time can be devoted to beginning
the first module of Brief CBT-CP.
Figure 4. Phases of a 30-Minute Appointment
28
If the patient ultimately decides not to engage in Brief CBT-CP, it is valuable to consider other
options that may be available. Some patients simply need more time to consider their
treatment options. For this kind of situation, we include a two-page patient handout entitled
Before You Go: Additional Information about Chronic Pain Treatment Options. This handout
includes the following: a quick summary of Brief CBT-CP; a short relaxation exercise; links to
freely available mobile apps that can address health and wellness topics; space for the provider
to summarize next steps regarding chronic pain management, such as referrals to other clinical
services; and a space for the provider’s contact information.
29
Offering Patients Brief CBT-CP:
Therapist Guide
Although adopting an empathic stance is not unique to CBT, it is nonetheless important when
working with patients experiencing chronic pain. Often, patients will be referred to you for
treatment when their pain is most distressing or when biomedical treatments have been
insufficient. Empathy is especially useful for building rapport and trust.
What is Brief CBT-CP?
• Brief CBT-CP targets thoughts, emotions, and behaviors in order to improve pain-related
functioning.
• Brief CBT-CP promotes the adoption of self-managed tools by patients so that they can
take an active role in effectively addressing chronic pain and its negative effects.
• Use the Brief Cognitive Behavioral Therapy for Chronic Pain handout to illustrate the
CBT-CP model.
Scripting includes:
1. “Living with chronic pain can be very challenging. It can negatively impact how we live
our lives, including our ability to participate in activities and important relationships with
others. Individuals with chronic pain often struggle to find ways to manage their pain
and feel that they lack the know-how to move forward with their lives.”
2. “Brief cognitive behavioral therapy, or CBT, for chronic pain is designed to help us
respond to chronic pain in a way that will help us live a more fulfilling life. Patients learn
new pain management skills that can keep us connected to the people and daily routines
that we value.”
3. “An important piece of Brief CBT for chronic pain is the teamwork between the patient
and therapist. My goal is to work closely with you in a way that you find supportive and
empowering.”
4. “This intervention is designed to be brief so it’s not a long-term commitment. Of course,
if we decide that additional support will be beneficial, then I will help connect you to
additional services.”
30
What does Brief CBT-CP Include?
• The treatment structure of Brief CBT-CP includes six appointments that last about 30
minutes each.
• Topics covered reflect the key components of full-length CBT for pain:
• Pain education and goal setting
• Activities and pacing
• Relaxation training
• Cognitive coping (covered in two sessions)
• The Pain Action Plan
• Treatment is structured, but decision making is collaborative between patient and
therapist.
Scripting includes:
1. “Brief CBT for chronic pain includes six modules of 30 minutes each. We will cover a new
pain management skill each week based on your preference. This means that we will
work closely and stay focused to make the most of our time together.”
2. “Our first module will provide some important background information about chronic
pain itself and setting new goals for moving forward. Then we will decide together about
the order of our remaining topics. We will choose from the following: activity planning
and pacing, which will help us avoid a common pitfall of overexerting ourselves and
causing a pain flare up; relaxation training which will cover several ways to reduce
tension in our bodies and feeling distressed; and cognitive coping, which helps us
address unhelpful thought patterns -we learn to feel better by changing the way we
think about pain and ourselves. Our final module will focus on reviewing the skills we
learned and developing a plan for how best to use those skills.”
3. “At the end of each module, we will talk about ways you can begin to practice each skill.
Practice is very important as we want these new approaches to become good habits. We
will find a way to make practice doable even during a busy day.”
31
What are the Advantages of Brief CBT-CP?
• There are number of advantages to applying Brief CBT-CP, both practical and research-
supported. Based on what you know about the patient, it’s helpful to emphasize the
match between patient needs/goals and what Brief CBT-CP can offer.
Scripting includes:
1. “CBT for pain has been studied by researchers for many years. Overall, these studies
show that patients experience less distress and disability after using what they learn in
CBT. Some patients even report that their pain intensity has decreased.”
2. “CBT for pain is safe for almost anyone. There are no known negative side effects and
the focus is educational and skill-building.”
3. “The brief version of CBT for pain that we will use is less than three hours of treatment
time and is spread out over several weeks. This minimizes the amount of travel and time
you spend in treatment.”
What are the Limitations of Brief CBT-CP?
• Discussing the limitations of Brief CBT-CP can be helpful in setting realistic expectations
about what treatment can and cannot accomplish.
Scripting includes:
1. “Brief CBT-CP can be very helpful, and it requires that we work together as a team to
help manage your pain more effectively. Part of your treatment will include assessing
your pain and distress using one or more brief, easy to complete surveys. These will help
us determine what is going right in treatment and other areas that may need more
focus.”
2. “Brief CBT for pain is primarily about helping with pain management. This does not
mean eliminating your pain but responding to your pain in a more helpful way so that it
feels less overwhelming.”
3. “Sometimes during treatment we will need to talk about some difficult experiences you
have had in relation to pain so that you are able to respond in beneficial ways in the
future. Over the course of treatment, the goal will be to use the skills we learn to address
distressing pain-related experiences.”

32
Before You Go: Additional Information about
Chronic Pain Treatment Options
Today we discussed some of the challenges of living with chronic pain. We also discussed some
options available to help manage chronic pain. One option that may be a good fit for you is
Brief Cognitive Behavioral Therapy for Chronic Pain, or Brief CBT-CP. Some key information
about Brief CBT-CP is summarized here, in case you would like to begin this treatment at a
future time:
1. Brief CBT-CP can help decrease distress and disability from pain and is safe for almost
anyone.
2. Brief CBT-CP includes six, one-to-one meetings of about 30 minutes each. Treatment can
be spread out over 6 to 12 weeks.
3. A new pain management skill is covered each week based on the order you prefer. Key
topics and skills include:
• Activity pacing, which helps with avoiding a common pitfall of overexertion that
causes a pain flare-up.
• Relaxation training, which will help to reduce tension in your body and manage
distress.
• Cognitive coping, which will help with managing unhelpful thought patterns.
• Developing an action plan, which will help you move forward with meeting
important personal goals based on new pain management skills.
Here’s a quick deep breathing exercise to consider that can help manage the stress that comes
with living with chronic pain:
1. Find a safe, quiet place to sit or lie in a comfortable position for at least five minutes.
Use soothing music to block out distracting noises, if necessary.
2. Breathe in deeply, but comfortably, taking a moment to focus your thoughts on your
breathing.
3. Count to yourself “one” at your next inhale, and exhale at your own pace. Continue to
count (e.g., “two”…, “three”…, “four”…) each time you inhale until you get to ten.
4. Take a moment to notice your breathing as it slows and develops a new rhythm. If
disruptive thoughts enter your mind, re-focus on counting each inhalation.
5. Count in sets of ten breaths for as long as you feel comfortable. Practicing two to three
times a day for short periods can be helpful when first learning this skill.

33
Visit the VA mobile app store (https://mobile.va.gov/appstore) to download free apps to help
with stress management and healthy lifestyles. These are a few examples of the health topics
these apps address:
• Chronic pain
• Sleep
• Weight loss
• Smoking cessation
• Stress management
• Coping with depression, anxiety, PTSD, and other mental health concerns
We discussed several options that can help you with better pain management and overall
wellness. Here is a summary of next steps to follow:
Provider: Include helpful information below on referrals to other services initiated today.
1._______________________________________________________________________
2._______________________________________________________________________
3._______________________________________________________________________
Living with chronic pain can be very challenging. It can negatively impact how we live our lives,
including our ability to participate in activities and important relationships with others.
Treatment options are available that can lead to new ways of coping with pain to maintain
connections to the people and daily routines that we value. My goal is to work with you in a
way that you find supportive and empowering.
If you would like more information about your treatment options for chronic pain or related
concerns, please contact me at the number below:
Provider/Clinic name: ____________________________________________________________
Phone number:_________________________________________________________________
Additional information: __________________________________________________________
34
BRIEF CBT-CP PROTOCOL AND THERAPIST
GUIDES
35
1. BRIEF CBT-CP MODULE ONE: EDUCATION AND GOAL IDENTIFICATION
In the context of primary care and other settings, the first contact with the Veteran is typically
used for the collection of information and to determine an appropriate treatment plan. At the
point of engaging in Brief CBT-CP, it is assumed that the initial functional and symptoms
assessment have been completed and that the Veteran has pain-related concerns that can be
best served in primary care.
1.1. Module Agenda
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
4. Introduce the new material and answer questions
5. Discuss new home practice opportunity
6. Module wrap-up
1.2. Module Materials
• PEG self-report measure
• Patient handouts (see appendix):
o Factors That Impact Pain
o The Chronic Pain Cycle
o Brief Cognitive Behavioral Therapy for Chronic Pain
o SMART Goal Setting
1.3. Module Content for the Provider
1. Chronic Pain Education
Understanding the difference between acute and chronic pain is the beginning of effective
management of persistent pain. While acute pain is a symptom and requires adjustments in
behavior so that appropriate healing can take place, chronic pain is an ongoing condition that
no longer signifies that damage or harm is actively occurring. Even though these two different
types may feel exactly the same, the meaning has changed. While withdrawing from what
causes pain is adaptive in acute pain as it allows the healing process to occur, that response is
maladaptive in chronic pain. Even in the case of conditions such as arthritis where there is a
gradual degeneration occurring, pain is not a sign of an acute injury and there are no
expectations of resolution or healing. Thus, it must be addressed in the same way.
36
Because of these differences, chronic pain must be managed as a chronic condition in much of
the same way as other disorders such as diabetes or heart disease. The biomedical model,
which works well with problems that resolve such as a broken arm, does not work well with
chronic pain. Since chronic pain has not responded adequately to treatment and resolution is
no longer expected, a different model for understanding it must be applied: the biopsychosocial
model.
Figure 5. Acute and Chronic Pain
Figure 6. Biomedical and Biopsychosocial Approaches to Pain
Acute Pain
Lasts less than 3 months
Responds to medical treatment and
diminishes with healing
Has an identified cause; body's
response to injury
Is a symptom
Chronic Pain
Lasts more than 3 months
Persists despite treatment
May develop after incident; cause
may or may not be known
Is a condition
Biomedical Model
Focuses on purely biological factors of
illness/disease
Is a symptom; assumed that resolution or
cure is possible
Works well with acute pain
Biopsychosocial Model
Focuses on biological, psychological, and
social factors of pain that interact
Is a condition; assumed that management
is key since resolution is not possible
Is necessary for chronic pain

37
2. Effects of Pain
Chronic pain affects many different areas of life. The interaction between biological/physical
(pain and medical issues), psychological (cognition, affect/emotion, behavior), and social
influences helps to explain the variability between individuals and their reports of pain. Figure 7
shows the overlap between these areas.
Figure 7. The Biopsychosocial Model
Use the Factors That Impact Pain Handout to review some of most important biological,
psychological/behavioral, and social variables that may influence chronic pain. Discuss with
Veterans how pain has impacted their lives from all aspects:
• Biological or medical factors (e.g., pain condition, comorbidities)
• Psychological factors (e.g., negative mood, lowered self-esteem, activity engagement)
• Social factors (e.g., relationships, employment)
Explain that since chronic pain is a complex problem, it must be approached in a
comprehensive way. While some factors such as previous injuries cannot be changed,
emphasize that many of the factors that impact pain can be adapted with the assistance of Brief
CBT-CP. This treatment helps Veterans change the way that they react to pain so that it has less
of a detrimental impact on their lives.
Now that the various areas of life that pain affects have been identified, use the Chronic Pain
Cycle handout (see Figure 8) to discuss the process and stages that may occur over time for
Biological
Factors
Social
Factors
Psychological
Factors

38
those with chronic pain. As the figure illustrates, the onset of chronic pain often leads to a
decrease in activities, which leads to physical deconditioning. Dealing with constant pain may
also lead to negative thoughts (i.e., “I can’t do anything when I have pain like this”) and
emotions such as frustration and depression. These factors contribute to increased avoidance
of family and friends and anything that involves movement since it hurts to move. This
combination means more distress and disability, leading to increased pain. Many Veterans will
be able to recognize this pattern in their own lives.
Figure 8. Chronic Pain Cycle

39
3. Goal Identification
The general objectives of Brief CBT-CP are to improve quality of life through the steps listed in
Table 5:
Table 5. OBJECTIVES OF BRIEF CBT-CP
Reducing the negative effects of pain on daily life by engaging in more activities, improving
mood, and increasing coping skills should be highlighted. While decreased pain intensity may
occur, try to help Veterans shift their preoccupation away from pain and towards functioning.
The hope is to make life more fulfilling so that pain feels less overwhelming.
The identification of individualized, Veteran-centric goals is critical for tailoring modules and for
helping the patient increase motivation for treatment engagement. Developing personally
meaningful treatment objectives that are achievable provides a framework to guide therapy. It
can be introduced to the Veteran with a simple statement such as:
• Let’s get you back to doing more of what is important to you.
It is sometimes difficult for individuals to produce specific goals on their own, so it can be
helpful to ask questions to guide the discussion, such as:
• What is something specific that you would like to see change in your life in the weeks to
come?
• What would you like to be able to do (better, more of, etc.)?
• If this treatment were successful, how would that look in your day-to-day life?
• Are there relationships that you would like to improve?
In order to assist in goal setting, the SMART model will be used to develop individualized goals
that are outlined in Table 6.
Reducing the negative impact of pain on daily life
Improving physical and emotional functioning
Increasing effective coping skills for managing pain
Reducing pain intensity

40
Table 6. INDIVIDUALIZED SMART GOALS
Specific
Identifies a specific action or event that will take place.
Measurable
Should be quantifiable (countable) so progress can be tracked.
Achievable
Should be attainable and realistic given resources.
Relevant
Should be personally meaningful.
Time-Bound
State the time period for accomplishing the goal.
Adapted from Doran, 1981
The SMART Goal Setting worksheet should be used with the Veteran in session. This worksheet
includes both short-term goals that can be accomplished over the course of the Brief CBT-CP
treatment timeline, as well as long-term goals that may span over the next year but are
important in serving as a motivator. While engaging in Brief CBT-CP requires time and effort,
these goals should help illuminate why the long-term benefits outweigh the short-term
investment.
Once individualized treatment goals are established, they should be monitored on an ongoing
basis for positive reinforcement and to adjust goals and treatment as indicated. It is
recommended that both the Veteran and therapist have a copy of the goals sheet available
throughout the course of treatment so that it can be referred to regularly.
4. Home Practice
Ask Veterans to continue to contemplate both short- and long-term goals. Stress the
importance of following the SMART formula reviewed during the session. Remind Veterans that
the general Brief CBT-CP objectives will be the framework for all modules, while the
individualized objectives will help motivate Veterans to engage in activities that will improve
the quality of their life and reduce the negative consequences of pain. The SMART Goal Setting
worksheet should be completed at home prior to the next module.
41
Brief CBT-CP Module 1 Therapist Guide:
Education and Goal Identification
Note to provider: Scripted statements are provided below as suggestions, rather than rules, of
how to introduce topics to patients. Scripting can be especially helpful for those providers
who are new to the content of Brief CBT-CP. Feel free to modify the scripting as needed as you
become more comfortable with core elements of each module.
1. Introduce the module and confirm the agenda
Scripting includes:
1. “Today we will begin brief cognitive behavioral therapy for chronic pain. This treatment
will help you develop new skills to use at home between modules and in the future. One
of the first things we will do at each appointment is work together to establish an
agenda for our time together. I have found that having this agenda helps to ensure that
we both get to talk about the items that we would like to discuss.”
2. “First, I would like you to complete a brief pain measure, and I will also check in on your
mood. Next, we will discuss some background on chronic pain itself and develop a plan
for how we will address some of your goals related to pain management. How does that
sound to you? Are there other things relevant to our pain work that you want to be sure
to cover today?”
Note to provider: If the patient is inclined to add items to the agenda that are not related to
pain management, the first effort on behalf of the therapist may be to link the topic back to
pain. For example, a statement such as the following may be helpful to refocus the patient:
“That sounds like it was stressful. Did you notice that your pain worsened during that time?”
2. Ask about mood, complete the PEG, and discuss findings
Scripting includes:
1. “First off, how are you feeling today and how has your mood been?”
2. “Next, I would like you to complete these three quick questions today. These items will
help us track your progress over the course of treatment. They can also help us identify if
we need to provide additional help along the way. After you complete the measure, we’ll
review the results.”

42
Note to provider: Informally checking on mood will give you a sense of how the patient is
currently coping while also providing the patient with the opportunity to express any
significant distress that might need immediate attention. Do not hesitate to further assess
for significant safety concerns, such as suicidal ideation, when indicated and by using
standard local procedures for your clinic. Assuming no safety concerns are present, briefly
review the PEG scores with patient as described in the chapter on measurement-based care.
3. Review material from the previous module
Although this is the first module of Brief CBT-CP, it is a good time to check in with patients
about any final questions or concerns they have about this treatment before getting started.
Scripting includes:
1. “Before we get started on new material, do you have any questions?”
4. Introduce the new material and answer questions
4.1. Chronic pain education
Scripting includes:
1. “To get started, I want to talk a bit about what makes chronic pain different from acute
pain, or pain that goes away after an injury heals.”
• Compare and contrast chronic pain with acute pain.
• Explain why these pains may feel the same but must be treated differently.
4.2. Effects of pain
• Use the Factors that Impact Pain handout to explain the 1) biopsychosocial model and
2) review the variety of factors that can negatively or positively impact chronic pain
Scripting includes:
1. “Chronic pain impacts many areas of our lives. You can see in this diagram that the
chronic pain you experience can be impacted by the interaction of biological or medical
factors, psychological factors, or social factors.“
2. “These factors can impact our chronic pain in either a negative way, a beneficial way, or
both and vary from person to person. They can turn up the volume on pain or turn down
the volume. What factors impact you the most?”

43
Key Point: Asking patients about what factors impact them the most will help you to identify
potential treatment targets (e.g., for SMART goal development).
Key Point: Emphasize that Brief CBT-CP is designed to help patients manage the impact of
chronic pain across these three domains.
• Use The Chronic Pain Cycle handout to explain how chronic pain may negatively impact
life over time.
Scripting includes:
1. “Chronic pain can take a toll on our behaviors, thoughts, and feelings. It’s shown here
how pain may lead us to stop participating in activities that we enjoy which leads to
negative thoughts and feelings. As our mood gets worse, we might withdraw from
routine activities and even our relationships. The less engaged we are in life, the more
distress we may feel. And without enough physical activity, we might become
deconditioned or disabled, making our pain worse.”
Key Point: Review the costs of inactivity noted on the handout.
Note to provider: Be aware that some patients may not be avoiding or under-engaging in
activities, but may be dealing with negative ramifications of pain nonetheless. Some
individuals may also be overactive, which can exacerbate their pain. The primary goal, in this
regard, is to achieve balance in activities. The module regarding Activities and Pacing will
address this concern in greater detail.
Key Point: Brief CBT-CP can help break the chronic pain cycle.
4.3 Goal Identification
• Use the Brief Cognitive Behavioral Therapy for Chronic Pain handout to provide an
overview of the objectives of Brief CBT-CP
Scripting includes:
1. “Brief CBT for chronic pain will provide you with several new strategies to help you
manage your chronic pain. Overall, these tools are designed to help reduce the negative
impact of pain on daily life, improve your physical and emotional functioning, and
increase effective coping skills. This treatment may also reduce your pain over time.”
• Use the SMART Goal Setting handout to identify Veteran-specific goals for change.
Identify at least one short-term goal and supporting rationale during this appointment
(with additional goals completed as home practice.)
44
2. “It’s important that we make sure that Brief CBT for chronic pain is addressing the areas
of your life that you find important. So, let’s get you back to doing more of what is
important to you. The first step will be to identify some short-term goals and then some
long-term goals. We’ll use the SMART goals format you see here.”
Key Point: Be certain that goals identified are relevant to chronic pain management.
Key Point: Goals should include as many of the SMART elements as possible.
Key Point: It is sometimes difficult for individuals to produce specific goals on their own, so it
can be helpful to ask questions to guide the discussion, such as:
1. “What is something specific that you would like to see change in your life in the
weeks to come?”
2. “What would you like to be able to do (better, more of, etc.)?”
3. “If this treatment were successful, how would that look in your day-to-day life?”
4. “Are there relationships that you would like to improve?”
5. Discuss new home practice opportunity
5.1. Clearly specified goals
Emphasize the value of identifying clearly specified goals (using SMART elements) for ensuring
that Brief CBT-CP will address areas of concern for the patient.
5.2. Short and long-term goals
Any short- or long-term goals not identified during this appointment should be completed by
the patient as home practice.
Scripting includes:
1. “Today we’ve identified a few SMART goals that will guide our future appointments.
Since we have already determined that you have a number of strengths, such as (X) and
(Y), I am confident that you will be able to complete the remaining short-term (and/or
long-term) goals at home. By completing this at home and bringing them with you to our
next appointment, we will be able to review them together and move more quickly into
learning new skills for chronic pain management.“
45
6. Module wrap-up
6.1. Summary of key points
This module includes considerable educational information about chronic pain and ends with
identifying patient goals for treatment. The following scripting can provide a concise summary
of key points and emphasizes again the value of goal setting and home practice.
Scripting includes:
1. “Today we discussed the difference between acute and chronic pain, including why
chronic pain is best treated from a biopsychosocial perspective. This approach
emphasizes treating pain from several angles, including developing new coping skills. We
identified some of the areas in your life that have been negatively impacted by pain and
discussed how we must avoid getting caught in the chronic pain cycle. To help us become
more active and break this cycle, we began to identify some short- and long-term goals
that will guide the rest of our appointments together. Completing the SMART goals sheet
before the next module will ensure that the remainder of our appointments are geared
towards your top priorities.”

46
Brief CBT-CP Module 1 Outline: Education and Goal Identification
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
• Although this is the first module of Brief CBT-CP, it is a good time to check in with
patients about any final questions or concerns they have about this treatment before
getting started.
4. Introduce new material and answer questions
4.1. Chronic pain education
• Compare and contrast chronic pain with acute pain.
• Explain why these pains may feel the same but must be treated differently.
4.2. Effects of pain
• Use Factors that Impact Pain handout to explain the 1) biopsychosocial model and
2) factors that impact pain.
• Use The Chronic Pain Cycle handout to explain how chronic pain may negatively
impact life over time.
4.3. Goal identification
• Use the Brief Cognitive Behavioral Therapy for Chronic Pain handout to provide an
overview of the objective of Brief CBT-CP.
• Use the SMART Goal Setting handout to identify Veteran-specific goals for change.
Identify at least one short-term goal and supporting rationale within this in-session
(with additional goals completed as home practice.)
5. Discuss new home practice opportunity
• Emphasize the value of identifying clearly specified goals (using SMART elements) for
ensuring that Brief CBT-CP will address areas of concern for the patient.
• Any short- or long-term goals not identified during this appointment should be
completed by the patient as outside practice.
6. Session wrap-up
• Provide a concise summary of key points and emphasize the value of home practice.
47
2. BRIEF CBT-CP MODULE TWO: ACTIVITIES AND PACING
This module focuses on the importance of engaging in activities and how to safely do so
through the use of time-based pacing. Unlike many other mental health interventions,
behavioral activation and guidance on how to properly pace activities is particularly important
with managing chronic pain so it is typically introduced early in the intervention.
2.1. Module Agenda
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
4. Introduce the new material and answer questions
5. Discuss new home practice opportunity
6. Module wrap-up
2.2. Module Materials
• PEG self-report measure
• Patient handouts (see appendix):
o The Chronic Pain Cycle
o Pleasant Activities List
o Pleasant Activities Schedule
o Pacing Activities
2.3 Module Content for the Provider
1. Hurt versus Harm
Often, one of the greatest challenges for those with chronic pain is the belief that they no
longer can engage in life fully or do the things that they want to do. Veterans with chronic pain
may believe that activity will lead to increased pain while also causing physical damage. This
belief, while typically true in acute pain, is inaccurate in chronic pain and may lead to
maladaptive responses such as avoidance. By avoiding activity, chronic pain worsens over time.
Inactivity leads to issues such as decreased flexibility and stamina, increased weakness and
fatigue, and even spasms from tight muscles. The problems related to deconditioning often
lead to increased risk of injury and weight gain (adding strain to the body) as well as feelings of
sadness, frustration, or boredom, which only encourage more general withdrawal from people
and places.
The avoidance response has been termed kinesiophobia (Miller, Kori, & Todd, 1991), or fear of
movement, and may develop to varying degrees in those with chronic pain. Unfortunately, it
creates a self-fulfilling cycle – not moving only makes patients’ next attempts to engage in

48
activity more difficult and painful, reinforcing this fear. For Veterans who have lower levels of
kinesiophobia and are more active, the manner in which they approach situations (e.g.,
overdoing) may also have detriments, such as new injuries. Flare-ups (relatively brief increases
in pain intensity) are a central concern of those with chronic pain. They do not want to induce a
flare-up with movement and are concerned with how to manage flare-ups when they occur.
Lack of movement, avoidance, or approaching activities without thoughtful planning makes the
occurrence of flare-ups more likely. Another common response is avoiding an area that hurts by
favoring another area. If a patient has pain in the right knee, they may begin compensating by
adding additional pressure to their left side when ambulating. In these cases, the initial area of
pain become deconditioned, and the area that is now absorbing additional stress may begin to
develop new pain.
Use The Chronic Pain Cycle handout, introduced in module one, to discuss the negative
consequences that often result from responding in a maladaptive manner to pain.
Figure 10. Chronic Pain Cycle
2. Pleasant Activities
For those with chronic pain, decreasing fear and engaging in activity is a key to improved
functioning but can be challenging. One way to increase re-engagement and decrease
kinesiophobia is to participate in pleasant activities. Many with pain may have stopped
participating in hobbies, spending time with others, or engaging in physical outings. For those
that do engage in activities more regularly, they may have given up some of their favorite
hobbies or be less comfortable when around friends and family. Many may feel that they
physically cannot do the things they want, are “no fun” to be with because of pain, or are

49
worried about experiencing a pain flare-up that might interfere with plans. The benefits of
engaging in pleasant activities are included in Figure 11.
Figure 11. Pleasant Activities
Identifying pleasurable activities for those with chronic pain may be challenging for several
reasons. Pain-related negative mood such as depression and irritability may lessen the ability to
identify such activities or diminish the motivation to engage in them. Psychosocial challenges,
such as limited resources, may be a barrier. Chronic pain and poor sleep may leave patients
feeling too tired or fatigued to participate in activities. Primarily, however, Veterans may
mention things that they would like to do but “can’t” because of pain limitations. Use the
Pleasant Activities List and Pleasant Activities Schedule to explore options. This discussion will
likely generate a forum for examining creative alternatives for previously enjoyed hobbies. For
example, if Veterans report that they used to enjoy bowling but are now unable to, inquire
about their willingness to teach bowling to children or adolescents or to play an adapted
version of bowling through a gaming system.
3. Time-Based Pacing
Some people are prone to “pushing through” pain in the name of accomplishing a task and will
not stop until it is complete, while others may be preoccupied with fears about harming
themselves and avoid activity altogether. Often, those with chronic pain use a “good pain day”
when they are feeling better to try and complete one or more rigorous activities that have
fallen by the wayside. For example, they clean the garage or mow the grass without excessive
pain – but wake up the next day feeling like they cannot move and thus are “laid up” for several
days in a row. This cycle of overactivity, increased pain, and increased rest seen in Figure 12
often happens on a recurring basis. This boom-bust pattern can lead to various negative
consequences such as pain flare-ups, increased stress and anxiety, decreased efficiency,
lowered self-esteem, and avoidance of any activity.
Positive distraction from pain
Improved mood and self-esteem
Increased socialization
Enhanced attention and concentration skills
Enhanced sense of purpose and direction

50
Figure 12. Overactivity Cycle
Overdoing or not planning activities carefully beforehand can lead to flare-ups lasting from
minutes to weeks. Minimizing the occurrence of flare-ups as well as knowing how to manage
them when they do occur is a critical component of successful Brief CBT-CP.
Engaging in a moderate, safe level of activity on a regular basis is how to avoid this maladaptive
cycle. Using the skill of pacing, where time is the guide for activity engagement, can be a helpful
strategy. It allows Veterans to consistently and thoughtfully engage in activities without causing
detrimental consequences. Pacing is often about balancing activities and planning ahead, or
working “smarter not harder.” Breaking tasks into “chunks” such as painting a room for 45
minutes per day over four days instead of for three hours on a single day is one example of
pacing. Alternating between standing to do dishes for ten minutes and sitting to fold laundry
for five minutes may be a way to avoid standing longer than is comfortable, avoiding a flare-up,
but also engaging in an “active rest” period where something is still being accomplished. Being
more thoughtful about activity allows Veterans to get more done on a more consistent basis,
which also encourages mood improvements brought about by accomplishment. Without
pacing, the cycle of being sedentary or over-active with pain flare-ups can be very discouraging.
During this module, use the Pacing Activities worksheet to explore how to pace an activity with
the Veteran. Use examples to illustrate how pacing can enable Veterans to consistently carry
out activities while minimizing the likelihood of increased pain. It is the middle ground between
doing nothing and overexertion that enables Veterans with chronic pain to engage in
reasonable amounts of activity and improve quality of life. It is important to remember to take
a break before an exacerbation occurs, and not wait until the pain is increasing. Asking a
Overactivity
Increased PainIncreased Rest
51
Veteran how long they can engage in an activity before they begin to experience an increase in
discomfort should be the guide.
Once the concept of pacing has been reviewed, it is important to discuss in this module how
Veterans will apply it to their own lives. Ask the Veteran to choose an activity where they can
use pacing over the next week, such as washing the dishes or doing yard work. With the
worksheet and sample provided, use the steps to develop a plan for incorporating the activity
into the week. Pacing is a primary means to avoid flare-ups which should be emphasized. While
pacing may be a difficult concept to implement, highlight its critical role in effective pain
management and the need for practice.
52
Brief CBT-CP Module 2 Therapist Guide:
Activities and Pacing
Note to provider: Scripted statements are provided below as suggestions, rather than rules, of
how to introduce topics to patients. Scripting can be especially helpful for those providers
who are new to the content of Brief CB-CP. Feel free to modify the scripting as needed as you
become more comfortable with core elements of each module.
1. Introduce the module and confirm the agenda
Scripting includes:
1. “Today we will discuss how to safely engage in activities through pacing. This topic is
important because it helps us to keep active but avoid “overdoing it.” As you may have
experienced, over activity can often lead to pain flare-ups that can last for days. It’s also
very important for individuals with pain to stick with enjoyable or pleasant activities, or
find new ones, because this helps lower our level of distress and makes life more
fulfilling.”
2. “First, I will ask you to complete our usual measure about your pain and functioning so
we can continue to track your progress. Next, I would like to do some follow-up from our
last module, then move into our new topic about activity pacing. How does that sound to
you? Are there other things relevant to our pain work that you want to be sure to cover
today?”
Note to provider: If the patient is inclined to add items to the agenda that are not related to
pain management, the first effort on behalf of the therapist may be to link the topic back to
pain. For example, a statement such as the following may be helpful to refocus the patient:
“That sounds like it was stressful. Did you notice that your pain worsened during that time?”
2. Ask about mood, complete the PEG, and discuss findings
Scripting includes:
1. “First off, how are you feeling today and how has your mood been?”
2. “I would like you to complete this brief measure, the PEG, again today to help with
tracking your progress. After you complete it, we’ll review the results.”
Note to provider: After the patient completes the measure, briefly review the score of the PEG
with patient in comparison to prior scores to identify any areas of significant concern/distress.
53
3. Review material from the previous module
Note to provider: The key purpose of reviewing prior module’s content is to 1) answer
questions/concerns about the topics and skills addressed, and 2) follow-up on home practice
for addressing skill acquisition and clarifying content.
Scripting includes:
1. “Before we get started on new material, do you have any questions about what we
covered last time?”
2. “Last time we discussed <previous topic> which included some home practice for you to
complete. Do you have your practice work from last time?”
Note to provider: It is not uncommon for patients to have not completed their home practice.
It is therefore important to briefly explore barriers to completion and re-state the importance
of home practice for developing and strengthening CBT skill development.
4. Introduce the new material and answer questions
4.1. Hurt versus harm
Use The Chronic Pain Cycle handout introduced in Module 1 to explain that acute and chronic
pain may feel the same but must be addressed differently
Scripting includes:
1. “It is important to remember that the pain we experience with our chronic pain condition
does not indicate that we are harming ourselves. Rather, this pain is like an annoying
alarm we can’t trust: unpleasant but not an indication of damage. Similarly, like leaving
bread in the toaster too long, smoke may set off the smoke detector. Even though the
alarm is going off and some action on our part is required, it’s not an emergency.
There’s no need to call the fire department.”
2. “Individuals with chronic pain often stop participating in certain activities out of fear
that they will experience a pain flare-up. Although we probably can’t avoid all flare-ups,
finding a balance between activity and rest is important when managing chronic pain.”
3. “As you can see in the chronic pain cycle, when we experience pain, we often decrease
our activity too much. This leads to lack of strength and flexibility, as well as an increase
in distress. As we feel worse, we might withdraw from even more activities. This cycle
can be broken by finding a balance in safe activities and rest.”
54
4. “Chronic pain can take a toll on our behaviors, thoughts, and feelings. It’s shown here in
the chronic pain cycle how pain often leads us to stop participating in activities that we
enjoy which leads to negative thoughts and feelings. As our mood gets worse, we might
withdraw from routine activities and even our relationships. The less engaged we are in
life, the more distress we may feel. And without enough physical activity, we might
become deconditioned or disabled, making our pain worse.”
Key Point: Review the costs of inactivity noted on The Chronic Pain Cycle handout.
Key Point: Brief CBT-CP can help break the chronic pain cycle.
Key Point: Managing chronic requires balance between safe, appropriate activity and rest to
avoid both inactivity that leads to deconditioning and overuse that typically results in pain flare-
ups.
4.2. Pleasant activities
Use the Pleasant Activities List and Pleasant Activities Schedule to help identify enjoyable or
meaningful activities, particularly if the patient has a difficult time generating ideas without
assistance. Explain that pleasant activities take many shapes and forms, including those that
require varying levels of physical activity, from walking to playing board games.
Start by asking the Veteran to identify activities on their own but use the Pleasant Activities List
if they have a difficult time or need to expand their list of potential activities. When several
activities are identified, record them on the Pleasant Activities Schedule as instructed in the
handout.
Scripting includes:
1. “One of the best ways to avoid inactivity is to get reconnected with your hobbies or
social activities. Pleasant activities are very helpful because they can distract us from
pain, improve our mood, give us a chance to socialize, and even help give us a sense of
purpose.”
2. “Often individuals stop certain activities because they no longer seem possible when
living with chronic pain. While this is true in some cases, other times we can modify the
activity itself, or how we participate. What pleasant activities or hobbies would you like
to go back to?
3. “It’s clear that chronic pain has had a negative impact on your activities lately.
Sometimes it’s nice to also explore some new options for the first time. Is there anything
on this list of Pleasant Activities that we might talk about further?”
55
Key Point: If the patient is highly committed to an activity that is no longer feasible, engage in a
conversation about what they found enjoyable about the activity (e.g., did they enjoy running
because of being outside, a running group, etc.) and go from there. The “essence” of that
activity that they enjoyed might be found in other more feasible activities. Alternatively, help
them find ways to remain active in a similar activity in a new capacity.
4. “It sounds like one of the parts about your jogging group that you loved was the
opportunity to meet with friends on a weekly basis. Even though you are no longer able
to jog with them for the full time, how might you continue to see your friends?”
5. “It’s clear that you really enjoyed the teamwork aspect of playing basketball. Is there a
way to keep helping the team, even if you don’t play as frequently?”
Key Point: It is often helpful to identify a range of activities, including those that may require
fewer resources (e.g., activities inside the home), can be completed alone (e.g., gardening), with
friends (e.g., lunch at a favorite restaurant), those where physical activity is the main focus (e.g.,
playing sports), and those that are important because they are personally meaningful (e.g.,
volunteering for a charitable organization.)
4.3. Time-based pacing
Use the Pacing Activities worksheet to describe the goals of planning activities and to illustrate
the process of planning activity and rest.
Scripting includes:
1. “The goal of activity planning, or pacing, is to take a larger job and break it into smaller
pieces to make it more manageable. For example, an individual might plan to paint a
room in their house. Trying to paint the room in one day may be too strenuous whereas
making progress each day for several days may help avoid overexertion that can cause a
pain flare-up.”
2. “Balance applies to everyday activities as well. For example, take a break from standing
every 10 minutes while doing the dishes. During a 5-minute break, you can remain active
with other tasks that don’t require standing, like folding laundry or paying your bills on-
line.”
3. “Whatever the activity, the main goal of pacing is to engage in routine moderate
activity. Using a bit of planning to guide our activities helps us avoid situations where we
‘push through’ the pain throughout the day, which often leads to several days of being
‘laid up’ due to a pain flare-up.”
4. “This worksheet will help us break down a larger activity into pieces to ensure that we
are finding a balance between activity and rest. It may seem unusual at first to make an
56
activity longer than you are used to, but it will help to avoid unnecessary pain in the long
run.”
5. “Pacing helps us stay balanced because it reminds us to start being active as well as to
stop or take breaks. Relying on a pre-determined schedule means we do not need to rely
only on our internal signals about the need for movement and rest.”
Key Point: To find the optimal balance of activity and rest, it’s important to estimate the degree
of active time and rest time ahead of time. The active v. rest time will vary depending on the
task. These time estimates can be adjusted as needed.
Key Point: Be sure to identify at least one activity to illustrate pacing, with attention to including
a pleasurable or personally meaningful activity (e.g., playing games with grandchildren) in
addition to others (e.g., washing dishes).
6. “Let’s use the worksheet to sketch out how to apply principles of pacing using active and
rest time. What activity should we focus on first?”
5. Discuss new home practice opportunity
With at least one activity identified, patients should record their engagement in pacing cycles,
noting both their active time and rest time. Additional activities can be identified by the patient
as part of outside practice.
Scripting includes:
1. “Today we’ve discussed the importance of pacing to keep active while reducing the
likelihood or overexertion. We’ve identified (one, two, three, etc.) activities and
estimated the amount of rest and active time for each. The next step will be for you to
record the number of cycles you complete for each activity. By completing this at home
and bringing them with you to our next appointment, we will be able to review the sheet
together, identify any areas of concern, and move into learning the next skills.“
6. Module wrap-up
This module included information about a key chronic pain management skill: time-based
activity pacing. The following scripting can provide a concise summary of key points and
emphasizes again the value of pacing and at-home practice.
Scripting includes:
1. “Today we discussed how chronic pain is like an unreliable alarm rather than an
indication that we are doing harm. Our topic emphasized finding balance between
57
activities that are pleasurable and helpful to us and avoiding overexertion that can bring
on a pain flare-up. Planning ahead and pacing out our activities is an important
approach to finding that balance and avoiding the risks of too little or too much activity.
Try out the pacing schedule we identified for your activities we discussed and record your
progress on the handout for discussion at our next module.
58
Brief CBT-CP Module 2 Outline: Activities and Pacing
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
• Reviewing the prior module’s content to 1) answer questions/concerns about the topics
and skills addressed, and 2) follow-up on outside practice or homework. Briefly explore
barriers to completion of outside practice and possible solutions (as necessary).
4. Introduce new material and answer questions
4.1. Hurt versus harm
• Use the Chronic Pain Cycle handout to explain that acute and chronic pain may feel
the same but must be addressed differently, and that chronic pain is like a “broken
alarm”.
• Use the Chronic Pain Cycle handout to explain how chronic pain negatively impacts
life over time unless we find a balance between activity and rest.
4.2. Pleasant activities
• Use the Pleasant Activities List to help identify enjoyable or meaningful activities,
particularly if the patient has a difficult time generating ideas without assistance.
• Explain that pleasant activities take many shapes and forms, including those that
require varying levels of physical activity, from walking to playing board games.
• Schedule identified activities on the Pleasant Activities Schedule handout.
4.3. Time-based pacing
• Use the Pacing Activities worksheet to describe the goals of planning activities and
to illustrate the process of planning activity and rest.
5. Discuss new home practice opportunity
• With at least one activity identified, patients should record their engagement in pacing
cycles, noting both their active time and rest time. Additional activities can be identified
by the patient as part of home practice.
6. Session wrap-up
• Provide a concise summary of key points and emphasize the value of home practice.
59
3. BRIEF CBT-CP MODULE THREE: RELAXATION TRAINING
This module introduces Veterans to the pain management benefits of relaxation and then
reviews two specific techniques: diaphragmatic or deep breathing and progressive muscle
relaxation. Since these interventions are used in the management of various mental health and
medical conditions, many providers may already be familiar with them. Emphasize that
practicing these techniques regularly between modules is critical to mastery and effective
application.
3.1. Module Agenda
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
4. Introduce the new material and answer questions
5. Discuss new home practice opportunity
6. Module wrap-up
3.2. Module Materials
• PEG self-report measure
• Patient handouts (see appendix):
o Relaxation Benefits and Tips Handout
o Deep Breathing Training
o Progressive Muscle Relaxation
o Relaxation Practice Record
3.3. Module Content for the Provider
1. Relaxation Rationale
Relaxation techniques are fundamental skills for managing chronic pain. However, the notion of
relaxation in the service of pain management is an unfamiliar concept to most individuals with
chronic pain. The rationale behind the use of relaxation techniques for pain management can
be explained most easily by focusing on chronic pain as a chronic stressor, both physically and
psychologically.
When patients experience chronic pain, their bodies react with a “fight or flight” response. This
stress response, controlled by the sympathetic nervous system, is critical to survival when
individuals face a dangerous or threatening situation. While in acute pain the response is
adaptive, with chronic pain the response is ‘stuck on’ and creates additional wear and tear on
the body. Since the body is chronically stressed due to persistent pain, it does not have the
chance to recuperate (Benson & Klipper, 1975).

60
Veterans may hold certain areas of their bodies rigidly to brace or protect against pain. They
may tense their necks or shoulders in anticipation of or in response to pain. These types of
reactions, while perfectly natural, only increase tension levels and pain intensity, but are often
done unconsciously. In addition, coping with the chronicity of the pain condition, not feeling
understood by others, reduced involvement in enjoyable activities, and negative thoughts may
also increase the stress related to pain. Since stress and pain have a bidirectional relationship –
pain influences stress and stress influences pain – gaining greater control over the response to
stress can help to better manage pain.
The good news is that the opposite physiological process, known as the relaxation response,
slows down and stops the fight or flight reaction. This parasympathetic nervous system has the
effect of reversing physiological arousal and bringing the body back to a calm state. Human
beings are capable of developing control over this relaxation response and engaging it as a
means of managing physical and emotional stress. With practice, the skill of using relaxation
techniques to return the body to a relaxed state can be developed, thereby closing the pain
gate and reducing the intensity of pain. We are retraining the body and mind to respond in a
more adaptive way to stress and tension.
2. Implementation
As with any new skill, practice of relaxation techniques should be performed daily to gain
mastery. It can be helpful to offer an analogy such as learning to play the guitar. While at first it
may be difficult and uncomfortable with little noticeable improvement, regular practice helps a
person become a skilled musician over time. In fact, fingers may begin to play certain songs on
“autopilot” as the body develops a memory for the movements. This is the case with practicing
and learning relaxation as well. Over time, relaxation exercises become easier to implement,
require less thought, result in greater benefit. Daily practice is required to develop these skills.
Some hints that may be helpful are included in Figure 13.
Figure 13. Hints for Adding Relaxation Strategies to Daily Routines
Use the handout on Relaxation Benefits and Tips in this module which further outlines the
advantages to developing the skill of relaxation and ways to implement it successfully.
Pair relaxation with a daily activity such as having a meal or making coffee/tea.
Use a relaxation "app" on a smart phone (See Appendix for examples).
Select a phrase or mantra that serves as a cue such as "calm, peace, or positivity."

61
3. Techniques
While there are various relaxation techniques that are effective, all involve a unique mental
state of passive attention to a stimulus that decreases the inner dialogue and the sympathetic
nervous system arousal. They combine a focusing tool (e.g., breath, area of body, image) with a
quiet and accepting disregard of everyday thoughts when they occur in order to return to the
focus of attention. Steps to help achieve this mental state are illustrated in Figure 14.
Two relaxation techniques will be introduced and demonstrated in this module. A brief review
of deep breathing, the foundation of all options, will be followed by an overview of brief
progressive muscle relaxation. Information regarding guided imagery, another common
relaxation technique, is included in the appendix for those who would prefer this approach.
Guided imagery can be used as a substitute for brief progressive muscle relaxation or as an
additional relaxation skill.
Figure 14. Steps to Being Prepared for Relaxation Training and Practice
1. Sit in a comfortable chair or on a mat. (If you get in bed you may fall
asleep so it is not recommended, unless you are using the technique to
aid in sleep initiation).
2. Lower the lights.
3. Take off your shoes and loosen tight clothes.
4. Close your eyes. (If you want to keep your eyes open, then focus them
on one spot).
5. Turn off your phone, TV, and radio.
6. Put pets in another room.
7. Let others in the house know you need some time alone to focus on
your health.
62
Deep Breathing
The first relaxation technique is diaphragmatic breathing, often called “deep breathing”, and it
is the foundation for all other relaxation techniques. It uses deep breathing to contract the
diaphragm by expanding the chest cavity and allowing more room for the lungs to fill with air.
This serves the purposes of slowing breathing, increasing oxygen intake, and even increasing
energy.
Diaphragmatic breathing is a brief and portable strategy that can be done anywhere, at any
time, and usually without others becoming aware that it is being done. It involves normal
breathing, but uses breaths that are intentionally smoother, slower, and deeper than the
breaths usually taken throughout the day. It is one of the easiest, most effective ways to
decrease tension in the body.
The steps for teaching this exercise are detailed here. The clinician can help model effective
technique by engaging in the exercise along with the Veteran.
Steps for Deep Breathing
1. Establish good posture.
2. Explain chest/shallow versus belly/deep breathing.
3. Have Veteran place one hand on chest and one hand on abdomen.
4. Determine if the Veteran is “chest breathing” or “belly breathing.”
5. Close eyes completely or look downward and fix gaze on one spot.
6. Observe the hands and ensure they are free of tension.
7. Have the Veteran keep one hand on chest and one hand on abdomen and keep eyes
closed or fixed on one spot.
8. Have the Veteran inhale slowly through the nose (if possible), causing the abdomen to
expand, extending inhale to three to five seconds in duration.
9. Instruct the Veteran to exhale slowly and completely through mouth, extending exhale
to three to five seconds in duration.
10. Continue this exercise for three to five minutes.

63
During the exercise, the clinician may wish to coach the Veteran with statements such as: “Feel
your body become more and more relaxed with each exhalation,” or “Each time you exhale,
think of the word relax,” or “Breathe in feelings of relaxation and breathe out any tension.”
Refer to Figure 15 and to the Deep Breathing Training handout for a sample script of this
exercise.
Figure 15. Mini-Breathing
Brief Progressive Muscle Relaxation
The second technique is progressive muscle relaxation (PMR). This exercise is focused on
systematically tensing and relaxing specific muscle groups. The underlying explanation for the
utility of this technique is that a muscle group cannot be both tense and relaxed at the same
time. By deliberately tensing the muscles and then relaxing them, patients can learn to observe
the difference between these two sensations; the body can then learn to notice tension in
muscles and to automatically release that tension.
Gentle contraction (i.e., mild to moderate tension) of each muscle group is required, not severe
tension. Tensing the muscle should not hurt, but it may feel unfamiliar and thus slightly
uncomfortable on the first practice of PMR. Muscle groups that are particularly tense may be
repeated, if desired.
MINI BREATHING EXERCISE
One idea is to try and use mini-sessions of deep breathing during the day. Incorporating brief
sessions of breathing will help with frequent practice. Because this exercise is so portable
and easy, it can help any time you are “on the go.”
For example, when you are standing in a line at the store, you may find yourself becoming
increasingly tense or impatient. Instead of focusing on that:
1. Take a deep breath in. As you breathe out, imagine the tension and negativity leaving
your body.
2. On your next breath, imagine breathing in feelings of calm and relaxation.
3. Count to six taking a slow, deep breath. Breathe out slowly, again to a count of six.
Before you know it, you will feel less tense and more in control. What are some other
situations where you might be able to do a mini-session during the day?
64
For Veterans who fear that contracting a particular muscle will increase pain in that location,
encourage them to approach that area gently. If there is a spasm or any undesirable effect,
Veterans can visualize the muscle and imagine tensing that area when they get to that part of
the body. Veterans should continue to contract the other muscles as the PMR exercise
continues.
Given the time limitations of primary Care, it is recommended to provide an overview of the
concept behind PMR and demonstrate this approach with one area/muscle group during the
module, such as wrist and arm. Demonstrate other muscle groups if time allows.
Major Muscle Groups
Please also refer to the handout entitled Progressive Muscle Relaxation for a sample script of
this exercise. The following are the muscle groups to be tensed and relaxed:
• Lower arms/upper arms
• Lower legs
• Upper legs/buttocks/lower back
• Abdomen
• Chest
• Neck/shoulders/upper back
• Mouth/jaw/throat
• Eyes/upper forehead/scalp
Steps for Brief Progressive Muscle Relaxation
1. Start with relaxed, deep breathing.
2. Systematically tense and relax each major muscle group.
3. Tension should last 5-10 seconds then relax for 10-20 seconds.
4. Spend additional time on muscles that are difficult to relax.
5. Mentally scan the body in systematic order of muscle groups, looking for remaining
tension.
6. Allow Veteran to relax any residual tension.
65
4. Practice
Encourage Veterans to practice relaxation techniques at least once per day over the next week,
more if possible. In addition, ask them to use the Relaxation Practice Record to track practice
and progress. Ask the Veteran to write down a tension rating before starting the exercise and
then return to the record afterward to self-assess and rate tension again – clarify that they are
rating tension not pain intensity. Remind patients that as the skill develops, the techniques will
become easier and benefits will increase.
66
Brief CBT-CP Module 3 Therapist Guide:
Relaxation Training
Note to provider: Scripted statements are provided below as suggestions, rather than rules, of
how to introduce topics to patients. Scripting can be especially helpful for those providers
who are new to the content of Brief CBT-CP. Feel free to modify the scripting as needed as you
become more comfortable with core elements of each module.
1. Introduce the module and confirm the agenda
Scripting includes:
1. “As I mentioned last time, today we will review the benefits of relaxation training in
managing chronic pain, and practice two specific relaxation techniques: deep (or
diaphragmatic) breathing and progressive muscle relaxation. Going over these
techniques during our appointment today is important because this will help you learn
the basics. However, practicing these techniques on your own at home is critical to
mastering the techniques, and promoting your ability to apply them in an effective
manner.
2. “First, I will ask you to complete our usual measure about your pain and functioning so
we can continue to track your progress. Next, I would like to do some follow-up from our
last module, then move into our new topic about relaxation. How does that sound to
you? Are there other things relevant to our pain work that you want to be sure to cover
today?”
Note to provider: If the patient is inclined to add items to the agenda that are not related to
pain management, the first effort on behalf of the therapist may be to link the topic back to
pain. For example, a statement such as the following may be helpful to refocus the patient:
“That sounds like it was stressful. Did you notice that your pain worsened during that time?”
2. Ask about mood, complete the PEG, and discuss findings
Scripting includes:
1. “First off, how are you feeling today and how has your mood been?”
2. “I would like you to complete this brief measure, the PEG, again today to help with
tracking your progress. After you complete it, we’ll review the results.”
Note to provider: After the patient completes the measure, briefly review the score of the PEG
with patient in comparison to prior scores to identify any areas of significant concern/distress.
67
3. Review material from the previous module
Note to provider: The key purpose of reviewing prior module’s content is to 1) answer
questions/concerns about the topics and skills addressed, and 2) follow-up on home practice
for addressing skill acquisition and clarifying content.
Scripting includes:
1. “Before we get started on new material, do you have any questions about what we
covered last time?”
2. “Last time we discussed <previous topic> which included some outside practice for you to
complete. Do you have your practice work from last time?”
Note to provider: It’s not uncommon for patients to have not completed their home practice.
It is therefore important to briefly explore barriers to completion and re-state the importance
of home practice for developing and strengthening CBT skill development.
4. Introduce the new material and answer questions
4.1. Relaxation training education
Scripting includes:
1. “I’d like to provide a little bit of background on why relaxation techniques are valuable
tools to manage chronic pain.”
Discuss that chronic pain is a stressor for both the body and mind that triggers and
subsequently maintains the fight or flight response.
Explain that relaxation skills are more than just resting or enjoying a hobby. Relaxation training
is specifically designed to counteract the fight or flight response by reducing both bodily and
psychological tension/stress.
1. “These skills can be good for your health for a variety of reasons, including that
relaxation can help improve your mood, energy level, sleep, blood pressure, as well as
pain. Though there are many different types of relaxation skills, they each have common
features, and importantly, all require practice.”
Use the Relaxation: Benefits and Tips handout to 1) explain the benefits of relaxation training,
and 2) provide an overview of basic tips to enhance relaxation skill practice.
68
4.2. Provide a brief overview of two types of relaxation training:
4.2.1. Deep breathing:
Scripting includes:
1. “Deep breathing is the foundation for all other relaxation techniques. Very deep breaths
expand the chest cavity, contract the diaphragm, and make more room for your lungs to
fill with air. This helps to slow your rate of breathing and increase oxygen intake, among
other things. It is a brief, easy to learn, and portable strategy, but is also one of the most
effective ways of quickly decreasing tension in your body.”
Use the Deep Breathing Training handout to guide the patient through in-vivo practice of the
scripted exercise.
4.2.2. Progressive muscle relaxation:
Scripting includes:
1. “Progressive muscle relaxation involves purposely tensing and relaxing specific muscle
groups, one at a time. Naturally, a muscle cannot be both tensed and relaxed at the
same time. By intentionally focusing on these alternating tensed and relaxed states, you
can train yourself to notice when you are tense, and then help to alleviate it.”
Using the Progressive Muscle Relaxation handout, provide a verbal overview of the exercise.
Demonstrate tensing and relaxation of at least one muscle group (e.g., lower arms/wrists) and
confirm that the patient understands the general technique. Demonstrate on additional muscle
groups if time allows, but it is unlikely that you can complete the full in-vivo exercise in session
due to time constraints.
Note to provider: If you or the patient believes that guided imagery should be used instead of
Progressive Muscle Relaxation, this information is available in the appendices. Guided
imagery may be considered a viable alternative to deep breathing in particular if there are
risks or limitations associated with breathing retraining (e.g., patients with COPD or other
pulmonary dysfunction).
Key Point: Emphasize that relaxation training is used to retrain the body and mind to respond
differently to stressors so that it becomes automatic and more helpful.
Key Point: When using progressive muscle relaxation, Veterans may approach a currently
painful area gently to avoid a flare-up. Alternatively, they may skip an area or use visualization
to imagine tension and relaxation.
69
Key Point: Reinforce the importance of at-home practice, and practicality of mini-sessions brief
of practice throughout the day (e.g., mini-breathing exercise).
5. Discuss new home practice opportunity
Scripting includes:
1. “Earlier I mentioned that practicing these skills is important. But it is also important to
track progress in using these skills. One way we can do that is by rating our overall level
of tension before starting the exercise, and then again when we are through.”
Review Relaxation Practice Record handout and encourage patient to practice and track
progress using the form provided.
6. Module wrap-up
Scripting includes:
1. “Today we discussed the value of training our bodies and minds to relax. Relaxation skills
can be used to directly address the stress of living with chronic pain. The techniques we
reviewed are ones that you can use daily to help with feeling less tense and more in
control of your pain. These skills work best when we apply them routinely, so I’d
recommend practicing at least once per day over the next week (more if possible).”
70
Brief CBT-CP Module 3 Outline: Relaxation Training
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review previous module
• Reviewing the prior module’s content to 1) answer questions/concerns about the topics
and skills addressed, and 2) follow-up on outside practice or homework. Briefly explore
barriers to completion of outside practice and possible solutions (as necessary).
4. Introduce the new material and answer questions
4.1. Relaxation training education
• Discuss that chronic pain is a stressor for both the body and mind that triggers and
subsequently maintains the fight or flight response.
• Explain that relaxation skills are more than just resting or enjoying a hobby, but are
designed to counteract the fight or flight response
• Use the Relaxation: Benefits and Tips handout to 1) explain the benefits of
relaxation training, and 2) provide an overview of basic tips to enhance relaxation
skill practice.
4.2 Deep breathing
• Use the script in the Deep Breathing Training handout to guide the patient through
an in-vivo exercise.
4.3 Progressive Muscle Relaxation
• Use the Progressive Muscle Relaxation handout to provide an overview of the
technique and demonstrate tension and relaxation of one (or more) muscle groups.
5. Discuss new home practice opportunity
• Review the Relaxation Practice Record handout and encourage patient to practice and
track progress using the form provided.
6. Session wrap-up
• Provide a concise summary of key points and emphasize the value of home practice.
71
4. BRIEF CBT-CP MODULE FOUR: COGNITIVE COPING 1
This is the first of two modules that target the cognitive component of the Brief CBT-CP model
by helping Veterans to 1) recognize thoughts that are unhelpful, and 2) develop skills for coping
with those thoughts. By understanding the dynamic interplay between thoughts and pain and
recognizing common maladaptive cognitions, Veterans will be better equipped to manage their
chronic pain and the difficult emotional reactions that often accompany it.
This module will focus on identifying unhelpful thoughts while the second coping module
focuses on challenging those unhelpful thoughts. Cognitive Coping 1 should be addressed
before moving to Cognitive Coping 2. Although these have been divided into two modules, if
you find your patient masters this content quickly, it may be feasible to address both modules
in a single appointment.
4.1. Module Agenda
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
4. Introduce the new material and answer questions
5. Discuss new home practice opportunity
6. Module wrap-up
4.2. Module Materials
• PEG self-report measure
• Patient handouts (see appendix):
o Brief Cognitive Behavioral Therapy for Chronic Pain
o Pain Thoughts
o Catching ANTs
4.3. Module Content for the Provider
1. Relationship Between Thoughts and Pain
For those with chronic pain, the impact of their thoughts on how they experience pain can be
powerful. If pain fails to disappear or improve significantly over time, Veterans’ thoughts may
become increasingly negative and exert a greater influence on pain. Research shows that
negative thoughts are directly associated with pain perception (Lawrence, Hoeft, Sheau, &
Mackey, 2011). Often, these thoughts are automatic and outside of a person’s awareness but
may still impact emotions and behaviors.

72
Return to the Brief Cognitive Behavioral Therapy for Chronic Pain handout to review the
relationships between thoughts, pain, mood, and behaviors. Veterans will often recognize that
with increased stress or negative emotions, they also notice an increase in pain intensity.
Explain to Veterans that all human beings have automatic thoughts that may be helpful or
unhelpful. The presence of pain, however, sets the stage for an increase in negative thinking
since uncomfortable stimuli is always present. It may be important to tell Veterans that this is
not suggesting that their thoughts have caused their pain; some patients may be sensitive to
this notion as they may feel they have been accused of exaggerating pain in the past.
Assure them that while their pain is real, it is also accurate that unhelpful thoughts can
negatively impact their pain experience in direct and indirect ways; conversely, having more
adaptive thoughts can have a positive impact and turn down the volume of their pain
experience.
Figure 16. Interactions among Chronic Pain, Thoughts, Emotions, and Behaviors
2. Pain Thoughts
Another method for discussing unhelpful thinking patterns and their potentially automatic
nature is through a discussion of common maladaptive cognitions, or pain thoughts, that many
people have. In this module, these will be introduced to Veterans using the Pain Thoughts
handout. While it is not necessary to review this entire list with Veterans, applying the
appropriate labels to the examples on the handout as well as those provided by patients may
be helpful.
73
It is important to make note of one cognitive distortion in particular: catastrophizing.
Catastrophizing, or believing the worst, is particularly salient in the treatment of pain as it has
consistently been associated with important pain-related outcomes. Catastrophizing is
characterized by the tendency to magnify the threat value of pain and to feel helpless in the
context of pain.
3. Recognizing Unhelpful Thoughts
Once Veterans have explored the role of unhelpful cognitions in the Brief CBT-CP model, they
must now begin the process of increasing their awareness of the frequency of maladaptive
thoughts associated with pain or negative mood. Use the Catching Automatic Negative
Thoughts (ANTs) Worksheet to facilitate this process. Clarify to Veterans that since many of
these thoughts happen without conscious awareness, this initial process requires some effort.
Explain that the first step in improving thoughts is to increase recognition of those that are not
helpful. Use time in this module to generate an example of a pain-related thought that the
patient has had recently that did not serve them in a positive way. If the Veteran is unable to
identify one, use an example that has arisen in previous modules. At this point in treatment, it
is likely that the Veteran has expressed various pain thoughts, so it is recommended to take
note of a few over the course of treatment. Identify how the thought impacted their mood as
well as their experience of pain. The focus should not be on whether there is a grain of truth in
the thought but rather on whether it is helpful – does it serve the Veteran? Does it make their
experience better or worse? Turn up the volume or turn down the volume? Indicate whether
the thought has been helpful or harmful to their pain experience on the Catching ANTs
Worksheet.
Note that the next module, Cognitive Coping 2, will address finding alternative ways to respond
to negative stimuli by challenging these thoughts and using coping statements.
4. Practice
Encourage Veterans to review the Pain Thoughts handout on their own to facilitate the
understanding and identification of their own unhelpful thoughts, stressing the importance of
completing as many examples as possible on the Catching ANTs worksheet. Circling whether
the thought had a helpful/positive or unhelpful/negative effect on their pain and/or mood will
help to connect the important role of thoughts in pain management.
74
Brief CBT-CP Module 4 Therapist Guide:
Cognitive Coping 1
Note to provider: Scripted statements are provided below as suggestions, rather than rules, of
how to introduce topics to patients. Scripting can be especially helpful for those providers
who are new to the content of Brief CBT-CP. Feel free to modify the scripting as needed as you
become more comfortable with core elements of each module.
1. Introduce the module and confirm the agenda
Scripting includes:
1. “Today we will focus on the relationships between our thoughts and how we experience
pain. We will discuss how some thoughts can be helpful, while others can make things
worse. We will also start to apply strategies to identify negative thoughts so that we can
learn to cope with them better.”
2. “First, I will ask you to complete our usual measure about your pain and functioning so
we can continue to track your progress. Next, I would like to do some follow-up from our
last module, then move into our new topic about pain-related thoughts. How does that
sound to you? Are there other things relevant to our pain work that you want to be sure
to cover today?”
Note to provider: If the patient is inclined to add items to the agenda that are not related to
pain management, the first effort on behalf of the therapist may be to link the topic back to
pain. For example, a statement such as the following may be helpful to refocus the patient:
“That sounds like it was stressful. Did you notice that your pain worsened during that time?”
2. Ask about mood, complete the PEG, and discuss findings
Scripting includes:
1. “First off, how are you feeling today and how has your mood been?”
2. “I would like you to complete this brief measure, the PEG, again today to help with
tracking your progress. After you complete it, we’ll review the results.”
Note to provider: After the patient completes the measure, briefly review the score of the PEG
with patient in comparison to prior scores to identify any areas of significant concern/distress.
3. Review material from the previous module
75
Note to provider: The key purpose of reviewing prior module’s content is to 1) answer
questions/concerns about the topics and skills addressed, and 2) follow-up on home practice
for addressing skill acquisition and clarifying content.
Scripting includes:
1. “Before we get started on new material, do you have any questions about what we
covered last time?”
2. “Last time we discussed <previous topic> which included some outside practice for you to
complete. Do you have your practice work from last time?”
Note to provider: It’s not uncommon for patients to have not completed their home practice.
It is therefore important to briefly explore barriers to completion and re-state the importance
of home practice for developing and strengthening CBT skill development.
4. Introduce the new material and answer questions
4.1. Relationship between thoughts and pain
Use the Brief Cognitive Behavioral Therapy for Chronic Pain handout to discuss the
relationships between thoughts and pain. (Some patients may also benefit from reviewing The
Chronic Pain Cycle handout to discuss the role of unhelpful thoughts in perpetuating the
chronic pain.)
Key Point: Explain that all people have automatic thoughts that may be helpful or unhelpful.
Scripting includes:
1. “Everyone has thoughts that can be either helpful or unhelpful. Sometimes, we don’t
even realize that our thoughts are related to how we are feeling and acting. As you can
see in this diagram, our thoughts, including negative beliefs, are linked to how we feel,
our behaviors, and even how we experience pain. These thoughts are called automatic,
meaning that they usually happen quickly and we often experience them as being out of
our control. However, with practice we can identify these thoughts and replace them
with alternative thoughts that can be more positive or helpful.”
Key Point: It may be important to tell Veterans that this is not suggesting that their thoughts
have caused their pain or that “pain is in their head.”
Key Point: Assure them that while their pain is real, it is also accurate that unhealthy thoughts
can negatively impact their pain experience in direct and indirect ways; conversely, having more
76
adaptive thoughts can have a positive impact and turn down the volume of their pain
experience.
Scripting includes:
1. “Your thoughts have not caused your pain and your pain is very real. When we
experience pain for a long time, we may be more likely to have negative pain-related
thoughts. Although our thoughts do not cause the pain, they can influence how we cope
with pain. The more skilled we are at creating helpful, balanced thoughts, the better we
are at coping with pain. Then we have more control over whether our thoughts turn up
or turn down the volume of our pain experience.”
4.2. Pain thoughts
Use the Pain Thoughts handout to review 1) common pain thoughts, 2) examples of unhelpful
thoughts, and 3) examples of helpful alternative thoughts
Scripting includes:
1. “There are some common types of thoughts that people with chronic pain report. This
worksheet provides examples of some common pain thoughts that are unhelpful and
others that are helpful. Although most people experience these pain thoughts as
automatic, with practice you can become aware of them. Once you are aware of them,
you can start to replace them with thoughts that are more helpful.”
Key Point: It is important to make note of one cognitive distortion in particular: catastrophizing.
Catastrophizing, or believing the worst, is particularly relevant in the treatment of pain as it has
consistently been associated with important pain-related outcomes.
Note to provider: Pick at least three examples to review with the Veteran, one of which
should be catastrophizing, to review both the unhelpful and alternative helpful thought.
Attempt to elicit from the Veteran if there are certain types of unhelpful thoughts that they
experience more than others as these are likely targets for cognitive restructuring.
4.3. Recognizing unhelpful thoughts
Use the Catching ANTs handout to help the Veteran learn to 1) identify (catch) negative
thoughts, 2) determine if the thought is helpful or harmful, and 3) challenge automatic negative
thoughts
Key Point: Clarify to Veterans that since many of these thoughts happen without conscious
awareness, this initial process requires some effort.
77
Scripting includes:
1. “Now that we have explored the relationship between negative thoughts and pain, the
next step is to learn how to identify some of the specific unhelpful thoughts you might
have. At first, this can be difficult to do and takes some practice to do it well. Remember
that these thoughts often occur quickly and outside of our awareness, making them hard
to identify. The first step is learning to accurately recognize and identify your thoughts.
Let’s look at this example and then we’ll create one that is specifically for you.”
Key Point: Review the example and use time in module to generate an example of a pain-related
unhelpful thought that the patient has had recently. If the Veteran is unable to identify one, use
an example that has arisen in previous modules.
Key Point: Using the Catching ANTS handout, identify how the thought impacted their mood as
well as their experience of pain.
Scripting includes:
1. “Can you think of a recent time when you had an unhelpful pain-related thought? What
was happening? What was the thought? Was that thought helpful or harmful?”
Key Point: Work with the patient to identify several unhelpful thoughts and clarify the impact on
mood or behavior. This skill is essential before moving on to the next module (Cognitive Coping
2) which will introduce ways to challenge negative cognitions and to use coping self-statements.
5. Discuss new home practice opportunity
Encourage Veterans to review the Pain Thoughts handout on their own to facilitate the
understanding and identification of their own unhelpful thoughts.
Scripting includes:
1. “We have talked about a number of new concepts today. There are a few things that I
am going to ask you to review on your own and practice before you come back. This is
critical to mastering the skills and getting the most benefit from our time together. First,
I would like you to take some time on your own to review the Pain Thoughts Handout. As
you review, think about each type of thought and ask yourself if you have these types of
thoughts or similar ones.”
Stress the importance of completing as many examples as possible on the Catching ANTs
worksheet as possible, including circling whether the thought had a helpful/positive or
unhelpful/negative influence.
78
Scripting includes:
1. “Second, I would like you to work on part of the Catching ANTs Worksheet. It would be
great if you could “catch” at least one unhelpful thought a day. The earlier we can catch
those unhelpful thoughts, the less potentially negative impact they have on our life. Just
like we did today, write down the situation, and the thought, and determine if it is
helpful or harmful. You do not need to complete the final column ‘Challenge it!’ as we
will review your examples at the next appointment.
6. Module wrap-up
This appointment includes information about how thoughts influence the experience of pain.
The goal of the appointment is for the patient to understand this relationship and be able to
identify and challenge negative pain-related cognitions. The following scripting can provide a
concise summary of key concepts.
Scripting includes:
1. “Today we focused on how our thoughts influence our experience of pain. We identified
how negative thoughts can make us feel worse while more balanced thoughts can be
helpful. We worked to “catch” specific negative thoughts, rated if they were helpful or
harmful, and started working to create more accurate and adaptive thoughts. This is the
first step to learning to cope with these unhelpful thoughts.”
2. “Next time, we will learn about how to modify these thoughts to make them more
balanced and helpful in our everyday lives. Although these skills can be difficult at first to
learn and apply, many people find them extremely helpful as they practice the skills.
Practicing these skills before our next appointment will help to improve your ability to
use positive thinking in your everyday life.”
79
Brief CBT-CP Module 4 Outline: Cognitive Coping 1
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review previous module
• Review the prior module’s content to 1) answer questions/concerns about the topics
and skills addressed, and 2) follow-up on outside practice or homework. Briefly explore
barriers to completion of outside practice and possible solutions (as necessary).
4. Introduce the new material and answer questions
4.1. Relationship between thoughts and pain
• Use the Brief Cognitive Behavioral Therapy for Chronic Pain handout to discuss the
relationships between thoughts and pain.
4.2. Pain thoughts
• Use the Pain Thoughts handout to review 1) common pain thoughts, 2) examples of
unhelpful thoughts, and 3) examples of helpful thoughts.
• Pick at least three examples to review with the Veteran, one of which should be
catastrophizing, to review both the unhelpful and alternative helpful thought.
4.3. Recognizing unhelpful thoughts
• Use the Catching ANTs handout to help the Veteran learn to 1) identify (catch)
negative thoughts, 2) determine if the thought is helpful or harmful, and 3)
challenge automatic negative thoughts.
5. Discuss new home practice opportunity
• Encourage Veterans to review the Pain Thoughts handout on their own to facilitate the
understanding and identification of their own unhelpful thoughts.
• Stress the importance of completing as many examples as possible on the Catching
ANTs worksheet as possible, including circling whether the thought had a
helpful/positive or unhelpful/negative influence.
6. Session wrap-up
• Provide a concise summary of key points and emphasize the value of home practice.
80
5. BRIEF CBT-CP MODULE 5: COGNITIVE COPING 2
This is the second of two modules that target the cognitive component of Brief CBT-CP. This
module focuses on modifying unhelpful thoughts identified in the previous module and during
the patient’s home practice. Cognitive Coping 2 is briefer in terms of its content to
accommodate sufficient review from Cognitive Coping 1 as well as in-session practice regarding
the key skill of challenging unhelpful thoughts. Taken together, the goal of these two modules is
to prepare patients to identify, evaluate, and modify unhelpful thoughts related to chronic pain.
5.1 Module Agenda
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
4. Introduce the new material and answer questions
5. Discuss new home practice opportunity
6. Module wrap-up
5.2 Module Materials
• PEG self-report measure
• Patient handouts (see appendix):
o Brief Cognitive Behavioral Therapy for Chronic Pain (as needed)
o Pain Thoughts (as needed)
o Catching ANTs
o Coping Statements
5.3 Module Content for the Provider
1. Review of Progress - Pain Thoughts
Depending on the degree of skill or comfort the patient demonstrates with identifying
unhelpful thoughts, it may be useful to briefly review the content from the prior module. One
method for discussing unhelpful thinking patterns is by reviewing the Catching ANTS worksheet
in comparison to the Pain Thoughts handout. This process can help patients to identify if they
tend to experience certain types of negative thinking more often than others, such as a
preponderance of “should statements” or emotional reasoning. Even if no specific pattern
emerges, this is a good opportunity to link the patient’s thoughts to the variety of unhelpful
thoughts about pain that can occur. While it is not necessary to review their entire list, it can be
helpful to discuss with Veterans which of the thoughts they found most frequent and/or
distressing versus less so. This process can illustrate how thoughts can impact our mood and
behavior in different ways (i.e., helpful, neutral, unhelpful).
81
2. Recognizing and Challenging Unhelpful Thoughts
Using the examples listed by the patient on Catching ANTS worksheet, introduce the concept of
challenging unhelpful thoughts. Review one of the examples in detail, including how the
thought impacted their mood as well as their experience of pain. Recall that the focus should
not be on whether there is a grain of truth in the thought but rather on whether it is helpful –
does it serve the Veteran? Does it make their experience better or worse? Turn up the volume
or turn down the volume?
Once the Veteran understands and can identify unhelpful pain-related cognitions, work with
them on alternative ways to respond to negative stimuli. The objective is not to create an
unrealistic picture of situations but a more accurate and balanced perspective. If possible,
propose a statement that reflects the role of the Veteran that increases self-efficacy. Review
the full example on the Catching ANTS worksheet and determine if patients understand the
process and rationale. It may be helpful to remind them that this is not suggesting that
thoughts cause their pain, but rather that we may be able to decrease the negative impact of
pain by making small changes to how we interpret situations.
3. Coping Statements
Another technique that can be helpful in managing pain flare-ups or negative mood is to use
positive coping statements. The ideal coping statement helps patients remain calm during
stressful situations. Coping statements provide “go-to” phrases that can replace unhealthy
thoughts or help Veterans cope with specific difficult situations, especially ones that may be
unanticipated. A key element to the success of coping statements involves finding phrases that
strongly resonate with the individual Veteran. While these could be pain-specific, they might
also be quotations, verses (e.g., song, scripture), or a phrase that a friend has delivered – the
key is personal relevance and easy access.
The Coping Statements handout helps Veterans choose statements that may be effective for
them. Patients may have their own phrases or statements that they have used in the past and
have served them well. Encourage them to add such statements to the list provided. One
advantage of formulating effective coping statements is that they can be portable and kept
handy for use at any time. They can be written on a small piece of paper and kept in a wallet or
placed into a smartphone that is carried routinely.
4. Practice
Encourage Veterans to complete the process of challenging unhelpful thoughts using the
remaining examples on the Catching ANTs worksheet. Patients should make adaptations to
unhealthy thoughts by creating a more balanced and accurate cognition. Finally, ask the
Veteran to identify several statements that they find calming and reassuring which can be used
before the next module.
82
Brief CBT-CP Module 5 Therapist Guide:
Cognitive Coping 2
Note to provider: Scripted statements are provided below as suggestions, rather than rules, of
how to introduce topics to patients. Scripting can be especially helpful for those providers
who are new to the content of Brief CBT-CP. Feel free to modify the scripting as needed as you
become more comfortable with core elements of each module.
1. Introduce the module and confirm the agenda
Scripting includes:
1. “Today we will continue to focus on the relations between our thoughts and how we
experience pain. Last time, we discussed how some thoughts can be helpful, while others
can make things worse. Today, we will review strategies to identify unhelpful thoughts
but also find ways to challenge and cope with these negative thoughts.
2. “First, I will ask you to complete our usual measure about your pain and functioning so
we can continue to track your progress. Next, I would like to do some follow-up from our
last module, then move into our topic about pain-related thoughts. How does that sound
to you? Are there other things relevant to our pain work that you want to be sure to
cover today?”
Note to provider: If the patient is inclined to add items to the agenda that are not related to
pain management, the first effort on behalf of the therapist may be to link the topic back to
pain. For example, a statement such as the following may be helpful to refocus the patient:
“That sounds like it was stressful. Did you notice that your pain worsened during that time?”
2. Ask about mood, complete the PEG, and discuss findings
Scripting includes:
1. “First off, how are you feeling today and how has your mood been?”
2. “I would like you to complete this brief measure, the PEG, again today to help with
tracking your progress. After you complete it, we’ll review the results.”
Note to provider: After the patient completes the measure, briefly review the score of the PEG
with patient in comparison to prior scores to identify any areas of significant concern/distress.
83
3. Review material from the previous module
Note to provider: The key purpose of reviewing prior module’s content is to 1) answer
questions/concerns about the topics and skills addressed, and 2) follow-up on home practice
for addressing skill acquisition and clarifying content.
Scripting includes:
1. “Before we get started on new material, do you have any questions about what we
covered last time?”
2. “Last time we discussed <previous topic> which included some outside practice for you to
complete. Do you have your practice work from last time?”
Note to provider: It’s not uncommon for patients to have not completed their home practice.
It is therefore important to briefly explore barriers to completion and re-state the importance
of home practice for developing and strengthening CBT skill development.
4. Introduce the new material and answer questions
4.1. Pain thoughts
It may be useful to first briefly review the concepts presented in the previous module with the
help of the Pain Thoughts handout. Key areas to review (as needed) include 1) common pain
thoughts, 2) examples of unhelpful thoughts, and 3) examples of helpful thoughts. This is also a
good time to compare the patient’s responses to the Catching ANTS worksheet to the
prototypes in the Pain Thoughts handout.
Scripting includes:
1. “As we discussed last time, there are some common types of thoughts that people with
chronic pain report. This worksheet provides examples of some common pain thoughts
that are unhelpful and others that are helpful. Let’s compare your examples to those
from the Pain Thoughts handout. Looking at your examples, which thoughts have
impacted you the most?”
Key point: The amount of review and discussion about the prior module’s content will vary
depending on the needs of the patient. When the patient can identify unhelpful thoughts,
introduce the new content below about challenging these thoughts.
84
4.2. Recognizing and challenging unhelpful thoughts
Use the Catching ANTs handout to begin the process of challenging or modifying unhelpful
thoughts.
Scripting includes:
1. “The next step is to learn how to challenge some of the specific unhelpful thoughts you
might have. At first, this can be difficult to do, and it takes some practice to do it well.
Which of the examples you provided should we start with? Let’s work to see if we can
come up with a more positive or balanced thought. What might you have thought that
would be more positive or helpful in that situation?”
Key Point: Work with the patient to challenge the cognition. If possible, propose a statement
that reflects the role of the Veteran and increases self-efficacy. Review the full thought record
and determine if patients understand the process and rationale.
4.3. Coping statements
Use the Coping Statements handout to help the Veteran 1) become familiar with positive
coping statements and 2) chose statements that may be effective for them.
Scripting includes:
1. “Another technique that can be helpful in coping with pain or managing negative mood
is to use positive coping statements. Coping statements help you remain calm during
stressful situations. Coping statements are your “go-to” phrases that can replace
unhealthy thoughts or help you cope with specific difficult situations. For example, telling
yourself that, I’m going to focus on what I can do, not what I can’t do, is an example of a
powerful coping statement.”
Key Point: A key element to the success of coping statements involves finding phrases that
strongly resonate with the individual Veteran. Patients may have their own phrases or
statements that they have used in the past and have served them well. Encourage them to add
such statements to the list provided.
Key Point: For patients who struggle after repeated trials of challenging unhelpful thoughts,
developing coping statements can provide an alternative approach to coping with negative
thoughts.
85
5. Discuss new home practice opportunity
Scripting includes:
1. “We’ve covered some important material today. There are a few things that I am going
to ask you to review on your own and practice before you come back. This is critical to
mastering the skills and getting the most benefit from our time together. I would like you
to continue to work on the Catching ANTs Worksheet. It would be great if you could
“catch” at least one unhelpful thought a day. Just like we did today, write down the
situation, and the thought, and determine if it is helpful or harmful. Then, take a few
moments and challenge it. Work to identify a more positive and helpful thought that
would turn down the volume on pain. We will review this at our next appointment.”
Stress the importance of completing as many examples as possible on the Catching ANTs
worksheet as possible, including circling whether the thought had a helpful/positive or
unhelpful/negative influence and creation of a more balanced and accurate cognition.
Finally, ask the Veteran to identify several statements that they find calming and reassuring
which can be used before the next module.
Scripting includes:
1. “Finally, I’d like to ask you to review the list of coping statements and identify any that
you find calming or helpful. I would also like you to think about other statements that
you may find beneficial. These could be parts of songs or poems, or even encouraging
words from a close friend. Basically, these can be any statements that help to calm or
soothe you, if you are feeling anxious or upset.”
6. Module wrap-up
Several cognitive strategies are reviewed in this module. The goal of the cognitive coping
modules is for the patient to understand the relationship between thoughts and pain, be able
to identify and challenge negative pain-related cognitions, create more helpful thoughts, and
work to identify additional coping statements.
Scripting includes:
1. “Our last two appointments have focused on how our thoughts influence our experience
of pain. We identified how negative thoughts can make us feel worse while more
balanced thoughts can be helpful. We worked to “catch” specific negative thoughts,
rated if they were helpful or harmful, and started working to create more accurate and
adaptive thoughts. We also reviewed common helpful coping statements and worked to
86
identify some statements that are meaningful to you. Although these skills can be
difficult at first to learn and apply, many people find them extremely helpful as they
practice the skills. Practicing these skills before our next appointment will help to
improve your ability to use positive thinking in your everyday life.
87
Brief CBT-CP Module 5 Outline: Cognitive Coping 2
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review Previous Module
• Review the prior module’s content to 1) answer questions/concerns about the topics
and skills addressed, and 2) follow-up on outside practice or homework. Briefly explore
barriers to completion of outside practice and possible solutions (as necessary).
4. Introduce the new material and answer questions
4.1. Pain thoughts
• Briefly review the concepts presented in the previous module with the help of the
Pain Thoughts handout.
• Key areas to review, as needed, include 1) common pain thoughts, 2) examples of
unhelpful thoughts, and 3) examples of helpful thoughts.
4.2. Recognizing and challenging unhelpful thoughts
• Use the Catching ANTs handout to begin the process of challenging or modifying
unhelpful thoughts.
4.3. Coping statements
• Use Coping Statements handout to help the Veteran 1) become familiar with
positive coping statements, and 2) chose statements that may be effective for them.
5. Discuss new home practice opportunity
• Stress the importance of completing as many examples as possible on the Catching
ANTs worksheet, including circling whether the thought had a helpful/positive or
unhelpful/negative influence and creation of a more balanced and accurate cognition.
• Ask the Veteran to identify several coping statements that they find calming and
reassuring which can be used before the next module.
6. Session wrap-up
• Provide a concise summary of key points and emphasize the value of home practice.
88
6. BRIEF CBT-CP MODULE 6: THE PAIN ACTION PLAN
This is the final module that focuses on relapse prevention. While functioning, mood, and pain
intensity have likely improved, chronic pain remains a part of daily life and pain flare-ups are
expected in the future. This module focuses on developing a plan for implementing the skills
from prior modules. This appointment should also include making appropriate referrals as
indicated should additional treatment be warranted.
6.1 Module Agenda
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review material from the previous module, including home practice
4. Review all progress/obstacles to date and develop a plan for future pain management
5. Discuss new home practice opportunity
6. Module wrap-up
6.2 Module Materials
• PEG self-report measure
• Patient handouts (see appendix):
• Anticipating Obstacles: Plan for Coping
• Weekly Activities Schedule
• SMART Goal Setting
6.3 Module Content for the Provider
1. Review of Progress
Begin the module by reminding Veterans of where they were when they entered treatment and
how much progress they have made. Be specific in the feedback provided, as patients may have
lost sight of their gains. Obtain feedback from Veterans about areas where they feel they have
made the most progress and what has worked best for them.
Asking questions, such as the following, may facilitate discussion and help Veterans identify
their own progress:
• Have you become more active?
• Has your mood improved?
• Do you feel like your life is more fulfilling, even though you still have pain?
• Have you noticed a difference in your pain intensity?
• What about how you react to your pain?
• Have others commented on positive changes they have seen in you?
89
Before examining the things that may get in the way of pain management in the future, it is
important to reflect on what the Veteran has already accomplished as a means of motivation.
2. Anticipating Obstacles
The best way to prevent a relapse to previous poor functioning is to be prepared for pain
exacerbations and difficult days. Planning ahead will make it easier to cope during challenging
times. Discuss anticipated obstacles that are likely to arise in the future as well as how those
issues will be addressed.
Use the Anticipating Obstacles: Plan for Coping worksheet to identify Veterans’ triggers for
pain increases.
Common triggers are:
• Emotional stress
• Weather changes
• Lack of sleep
• Sitting or standing “too long”
When completing the handout, encourage Veterans to be as specific as possible. For example,
instead of listing “stress”, define it further by listing the source of stress such as, “kids fighting
with each other.” Similarly, if there is a particular kind of weather that increases pain, identify
“weather under 50 degrees.” Find out how many minutes of sitting or standing is “too long.” If
the patient is unable to think of potential barriers, suggest barriers identified in prior sessions
related to coping with pain or even completing the home practice assignments. While
identifying triggers may be challenging, increasing attention to any emotional and physical signs
that may indicate an imminent flare-up can be beneficial.
Once personal triggers are identified, determine the best approaches for coping. This process is
an opportunity to review all the ways to manage pain that have been explored over the last five
modules. Engage in a discussion about all of the Brief CBT-CP techniques, from the role of
pacing, to relaxation exercise, to monitoring and modifying pain-related thoughts. Reviewing
options for managing each specific stressor can help make the exercise more realistic and
facilitate implementation.
3. Action Planning
Now Veterans are ready to develop a specific daily plan. Having a clear schedule helps patients
feel more prepared for several reasons. First, it can assist in mitigating difficult situations and
minimizing the triggers previously discussed. Second, it shows Veterans how to incorporate
various positive coping techniques into their everyday lives. Third, creating a plan promotes a
structured and purposeful approach to daily life, something that is valuable for everyone.
90
Working through a plan will help reveal how all of the pieces fit together and increase
confidence moving forward.
Using the Weekly Activities Schedule collaborate with Veterans to develop a schedule of
activities for a typical week in their words. If they prefer to use their electronic device for the
schedule, then defer to their preference. Ask about specific behaviors that they want to avoid
and use these to develop items for the schedule that will combat maladaptive habits. For
example, if someone wants to avoid isolating from others, perhaps “Meeting my friend John for
coffee” can be scheduled for every Tuesday morning, and encourage Veteran to include where
they will meet. Noting specific distractions to help keep the Veterans’ minds occupied such as
“garden (if nice weather)/puzzles (if bad weather)” or “play catch with my dog” will help create
a concrete plan for the future. It is important that the schedule is realistic, since setting
unreasonable plans will only make self-disappointment more likely if goals are not achieved.
Rewarding oneself for engaging in all scheduled activities for one week may be another
incentive to stay the course.
In all settings, but especially in primary care, it is critical to identify future needs and place
referrals as indicated. For example, if the work thus far with Brief CBT-CP has been helpful but
there is still significant progress to be made, perhaps a consult to pain psychology or a
behavioral medicine specialist for continued services (such as group or individual treatment)
may be in order. If the Veteran has increased activities and would be aided by participation in a
rehabilitation modality, such as physical or aquatic therapy, these options should be discussed.
Similarly, if in the course of treatment other more general mental health needs have emerged,
consider connecting the patient to additional mental health services, such as psychiatry or a
therapist in the mental health clinic.
4. Goals
The final task in session is to explore goals for the future. There may be accomplishments made
in recent weeks that can be expanded or new ideas that the Veteran now feels comfortable
considering. For example, if the patient has largely overcome a fear of movement, they may
want to incorporate bicycling or another adapted sport into their routine. If negative cognitions
have kept Veterans from considering dating, they may now feel confident enough to begin
exploring ways to meet others. Discuss what the individual Veteran is motivated to accomplish
in the future and tailor goals to meet specific interests and needs.
5. Practice
Provide positive feedback about all that has been accomplished so that Veterans leave feeling
supported and confident. Assure them that even if obstacles or setbacks are encountered, they
now have foundational tools necessary to manage their chronic pain.
91
Brief CBT-CP Module 6 Therapist Guide:
The Pain Action Plan
Note to provider: Scripted statements are provided below as suggestions, rather than rules, of
how to introduce topics to patients. Scripting can be especially helpful for those providers
who are new to the content of Brief CBT-CP. Feel free to modify the scripting as needed as you
become more comfortable with core elements of each module.
1. Introduce the module and confirm the agenda
Scripting includes:
1. “Today is our final appointment for addressing chronic pain as part of Brief CBT for
chronic pain. Today we will review the progress we’ve made over the last several
modules and think about next steps. It’s important that we take some time to look back
on what we’ve learned to both consider the progress we’ve made as well as plan for how
to continue to use the skills learned in the future.
3. “First, I will ask you to complete our usual measure about your pain and functioning so
we can continue to track your progress. Next, I would like to do some follow-up from our
last module, then move into our final topic about planning for the future. How does that
sound to you? Are there other things relevant to our pain work that you want to be sure
to cover today?”
Note to provider: If the patient is inclined to add items to the agenda that are not related to
pain management, the first effort on behalf of the therapist may be to link the topic back to
pain. For example, a statement such as the following may be helpful to refocus the patient:
“That sounds like it was stressful. Did you notice that your pain worsened during that time?”
2. Ask about mood, complete the PEG, and discuss findings
Scripting includes:
1. “First off, how are you feeling today and how has your mood been?”
2. “I would like you to complete this brief measure, the PEG, again today to help with
tracking your progress. After you complete it, we’ll review the results.”
Note to provider: After the patient completes the measures, review the score of the PEG with
patient in comparison to baseline to identify any areas of significant concern/distress. As this
is the final module of this treatment protocol, it is also an excellent time to compare current
92
ratings to baseline ratings to draw some summary conclusions about progress made or areas
to address in next steps.
3. Review material from the previous module
Note to provider: The key purpose of reviewing prior module’s content is to 1) answer
questions/concerns about the topics and skills addressed, and 2) follow-up on home practice
for addressing skill acquisition and clarifying content.
Scripting includes:
3. “Before we get started on new material, do you have any questions about what we
covered last time?”
4. “Last time we discussed <previous topic> which included some outside practice for you to
complete. Do you have your practice work from last time?”
Note to provider: It’s not uncommon for patients to have not completed their home practice.
It is therefore important to briefly explore barriers to completion and re-state the importance
of home practice for developing and strengthening CBT skill development.
4. Introduce the new material and answer questions
4.1. Review of progress
It is important to first emphasize substantive gains in functioning or mood that have occurred
during the course of treatment. Identifying improvement (or stabilization) is accomplished in
part by reviewing the change in patient measures, particularly from baseline to current status.
If the patient is unable to spontaneously identify areas of improvement, asking open-ended
questions may help guide them through likely areas that have improved.
Scripting includes:
1. “I’d like to start by identifying either symptoms or larger areas of life that might have
improved during the course of this treatment. Thinking back to when we first started
Brief CBT for chronic pain, what changes have you seen in your life related to chronic
pain?”
2. “One way to help identify areas of change is to take another look at the information you
reported in the measures we completed at the beginning of each module. When we
compare your score on the PEG, it looks like there’s a trend for improved functioning in
everyday activities over the course of this treatment. Have you noticed that you’ve been
93
more active or better able to engage in routines? How has that impacted other areas of
your life?”
3. “Tell me about ways that you have become more active.”
4. “Have you noticed any difference in your pain intensity or frequency? How has it
changed? Do you respond to pain differently now?
5. “Have others commented on positive changes they’ve seen in you?”
Key Point: Identify progress first (and before addressing barriers to progress) to bolster
motivation and acknowledge the results of the patient’s efforts to use CBT skills.
4.2. Anticipating obstacles
Having identified areas of growth or improvement, there are likely still areas that may need
attention in the future should they arise again. Use the Anticipating Obstacles worksheet to
identify triggers for pain and appropriate responses.
Explain that now is good time to plan for how skills learned in this treatment can be applied in
the future when triggers for pain are present.
Scripting includes:
1. “One of the best ways to help maintain our progress (or continue to move toward
achieving our goals) is to take a moment to think about likely situations or other triggers
that might bring on a difficult pain episode. By thinking of these triggers now, we might
be able to avoid some difficult situations or match the coping skills that we’ve learned to
the area of concern. Planning ahead may help us feel more confident in our ability to
manage pain the future.”
2. “Sometimes it’s difficult to identify very specific triggers for pain. As a rule of thumb,
consider times when your emotions, thoughts, or physical sensations may be hinting that
a pain flare-up is close. Do you recall our last conversation when you found that ______
was a trigger for your pain? Of the skills that we’ve talk about in our modules, which was
the most effective?”
Key Point: As a chronic condition, pain will need to be managed well into the future. Planning
ahead provides the opportunity for the patient to identify the most likely predictors of future
pain episodes and matching the CBT skill to that situation that they have found to be most
effective.
4.3. Action planning
94
Use the Weekly Activities Schedule to schedule important activities over a typical week. This
process helps minimize the impact of triggers, ensures meaningful goals/activities are attended
to, and adds structure and beneficial routines to otherwise unstructured time.
Scripting includes:
1. “There are several benefits to developing this typical weekly schedule. For one, adding
structure to our weeks can help with pacing, making sure we avoid inactivity or
overactivity. By planning ahead, we are most likely to make sure that the activities or
routines that are most important to us are really part of our day. This is also a great way
to find time in the week to practice some prevention, such as using relaxation skills, to
keep our stress and muscle tension levels down.”
2. “Let’s be sure to be as realistic as possible as we develop this plan. We can include
obligations as well as pleasurable events. For example, we can include both your hours
required at your part-time job, as well as the time you want to spend with your social
club.”
In addition to completing the Weekly Activities Schedule, the final module is a time to make a
determination if additional services are warranted. If the patient is requesting additional
services, consider if these are best addressed by you or another provider. The options are
potentially many depending on the needs of the patient and resources available in your clinic
and health care system. Some patients may require additional psychosocial interventions for
pain management in settings, such as pain clinics, that allow for longer treatment protocols.
Other patients may benefit from additional services such as physical therapy, nutrition
counseling, or specialty mental health.
Key Point: Weekly activity planning is an important final step of this treatment. Scheduling
ensures that patient-identified goals and preferences are clearly included in future activities and
routines.
Key Point: Concluding Brief CBT-CP is a highly personalized process in which additional referrals
(e.g., more intensive pain management services, mental health, or other rehabilitation-focused
services) should be considered based on patient need and local resources.
4.4. Future goals
Following weekly activity scheduling, it is valuable to briefly consider future long-term goals
that are potentially feasible now that CBT skills have been introduced. Although the weekly
scheduling will address a number of routine activities, discussing long-term goals once again
can offer an opportunity to further enhance motivation for the patient to engage in additional
realistic goals to achieve. Use the SMART Goal Setting handout to write down the short and
long-term goals identified. The patient’s short-term goals might have changed from the
95
beginning of treatment, which could indicate progress that can be emphasized. Provide
encouragement for continuing long term goals after treatment ends.
Scripting includes:
1. “Now that we’ve taken a look at what your typical weekly schedule will look like, it’s also
a good time to consider future goals. You’ve made progress in your pain management,
so what other goals for the future should we discuss briefly? Let’s write them down using
the SMART Goal Setting handout. For example, early on in our modules we discussed
that you had to quit the softball league because of your chronic pain. Now that you’ve
made progress in addressing activity pacing and identifying triggers for flare-ups, maybe
there’s a way to return to playing softball or helping out with coaching.”
5. Discuss new home practice opportunity
Although it is very helpful to acknowledge the patient’s progress throughout the course of
treatment, it is especially important to provide positive feedback about small and large gains.
This time is also good for reminding patients that they can continue to master their skills with
additional practice, even when faced with setbacks.
The patient should complete (and continue to modify as needed) the Anticipating Obstacles:
Plan for Coping and the Weekly Activities Schedule for application in the future.
Scripting includes:
1. “Today we’ve discussed the importance of continued practice of the skills discussed over
the course of our time together. We’ve identified the techniques that have worked best
for you (or identified those in need of additional practice) as well as a plan for how to use
those skills into the future. Be sure to keep the materials provided in these modules
readily available as they can be an ongoing resource well into the future. I recommend
that you come back to the worksheets we completed today to update and revise your
goals as you move forward (or complete any unaddressed worksheet items at home).
Returning to these worksheets from time-to-time can be a good ‘tune-up’ or reminder of
how to practice these skills.”
6. Module wrap-up
This module emphasized progress made and the need for continued application of these skills
into the future. It allowed time to arrange for any additional pain (or related) services that
could not be addressed by Brief CBT-CP. This is also the perfect time to add any additional
personal messages to the patient that acknowledges the value of their efforts, end of the
focused therapeutic interaction, as well as options (pending how services are delivered at your
site) for re-engaging with you as necessary.
96
Scripting includes:
1. “As the final module of Brief CBT-CP, we review the progress you’ve made over the
course of treatment. We started a few new worksheets that will be important for you to
complete outside of this module because they will act as a guide for putting the skills
into practice on daily basis. We also identified that it would be helpful to try a course of
physical therapy to promote physical fitness. We’ve arranged for that service through
your primary care provider. Finally, this is an opportunity for me to express my
appreciation for the opportunity to work with you over this course of treatment as well
as the service you have provided to our country.”
97
Brief CBT-CP Module 6 Outline: The Pain Action Plan
1. Introduce the module and confirm the agenda
2. Ask about mood, complete the PEG, and discuss findings
3. Review previous module
• Review the prior module’s content to 1) answer questions/concerns about the topics
and skills addressed, and 2) follow-up on outside practice or homework. Briefly explore
barriers to completion of outside practice and possible solutions (as necessary).
4. Introduce the new material and answer questions
4.1. Review of progress
• First emphasize substantive gains in functioning or mood that have occurred during
the course of treatment. Review the change in the PEG, particularly from baseline to
current status.
4.2. Anticipating obstacles
• Use the Anticipating Obstacles: Plan for Coping to identify triggers for pain and
appropriate responses.
• Explain that now is good time to plan for how skills learned in this treatment can be
applied in the future when triggers for pain are present.
4.3. Action planning
• Use the Weekly Activities worksheet to schedule important activities over a typical
week.
• This module is a time to make a determination if additional services (from you or
another provider) are warranted.
4.4. Future goals
• Briefly consider future short and long-term goals using the SMART Goal Setting
handout to write down the short and long-term goals identified.
5. Discuss new home practice opportunity
• The patient should complete (and continue to modify as needed) the Anticipating
Obstacles: Plan for Coping and the Weekly Activities worksheet.
6. Session wrap-up
• In addition to providing a general summary, add an additional personal message to the
patient that acknowledges the value of their efforts, end of the focused therapeutic
interaction, as well as options for re-engaging with you as necessary in the future
(pending how services are delivered at your site).
98
REFERENCES
Ahles, T. A., Wasson, J. H., Seville, J. L., Johnson, D. J., Cole, B. F., Hanscom, B., . . . McKinstry, E.
(2006). A controlled trial of methods for managing pain in primary care patients with or
without co-occurring psychosocial problems. Ann Fam Med, 4(4), 341-350.
doi:10.1370/afm.527
Beck, J. S. (1995). Cognitive Therapy: Basics and beyond. New York: Guilford Press.
Beehler, G. P., Loughran, T. A., King, P. R., Dollar, K. M., Murphy, J. L., Kearney, L. K., &
Goldstein, W. R. (in press). Patients’ perspectives of Brief Cognitive Behavioral Therapy
for Chronic Pain: Treatment satisfaction, perceived utility, and global assessment of
change. Families, Systems, & Health.
Beehler, G. P., Murphy, J. L., King, P. R., Dollar, K. M., Kearney, L. K., Haslam, A., . . . Goldstein,
W. R. (2019). Brief Cognitive Behavioral Therapy For Chronic Pain: Results From a Clinical
Demonstration Project in Primary Care Behavioral Health. Clin J Pain, 35(10), 809-817.
doi:10.1097/AJP.0000000000000747
Benson, H., & Klipper, M. Z. (1975). The RelaxationRresponse. New York: Harper Collins.
Burns, J. W., Nielson, W. R., Jensen, M. P., Heapy, A., Czlapinski, R., & Kerns, R. D. (2015).
Specific and general therapeutic mechanisms in cognitive behavioral treatment of
chronic pain. Journal of Consulting and Clinical Psychology, 83(1), 1-11.
doi:10.1037/a0037208
Buszewicz, M., Rait, G., Griffin, M., Nazareth, I., Patel, A., Atkinson, A., . . . Haines, A. (2006). Self
management of arthritis in primary care: randomised controlled trial. BMJ, 333, 879-
882. doi:10.1136/
Carlier, I. V. E., Meuldijk, D., Van Vliet, I. M., Van Fenema, E., Van der Wee, N. J. A., & Zitman, F.
G. (2012). Routine outcome monitoring and feedback on physical or mental health
status: evidence and theory. Journal of Evaluation and Clinical Practice, 18, 104-110.
Dobscha, S. K., Corson, K., Flores, J. A., Tansill, E. C., & Gerrity, M. S. (2008). Veterans affairs
primary care clinicians' attitudes toward chronic pain and correlates of opioid
prescribing rates. Pain Med, 9(5), 564-571. doi:10.1111/j.1526-4637.2007.00330.x
Dobscha, S. K., Corson, K., Perrin, N. A., Hanson, G. C., Leibowitz, R. Q., Doak, M. N., . . . Gerrity,
M. S. (2009). Collaborative care for chronic pain in primary care: a cluster randomized
trial. JAMA, 301(12), 1242-1252.
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science,
196(4286), 129-136. doi:10.1126/science.847460
Harding, J. K. J., Rush, A. J., Arbuckle, M., Trivedi, M. H., & Pincus, H. A. (2011). Measurement-
based care in psychiatric practice: A policy framework for implementation. Journal of
Clinical Psychiatry, 72(1136-1143).
IASP. (1994). Part III: Pain terms: A current list with definitions and notes on usage. In H.
Merskey & N. Bogduk (Eds.), Classification of Chronic Pain, Second Edition (pp. 209-214).
Seattle: IASP Press.
Institute of Medicine. (2011). Relieving Pain in America: A Blueprint for Transforming
Prevention, Care, Education, and Research. Washington, D.C.: The National Academies
Press.
99
Kerns, R. D., Otis, J., Rosenberg, R., & Reid, M. C. (2003). Veterans' reports of pain and
association with ratings of health, health-risk behaviors, affective distress, and use of
the healthcare system. Journal of Rehabilitation Research and Development, 40(5), 371-
380.
Klonoff, D. C., Buckingham, B., Christiansen, J. S., Montori, V. M., Tamborlane, W. V., Vigersky,
R. A., & Wolpert, H. (2011). Continuous glucose monitoring: an endocrine society clinical
practice guideline. The Journal of Clinical Endocrinology & Metabolism, 96(10), 2968-
2979.
Krebs, E. E., Lorenz, K. A., Bair, M. J., Damush, T. M., Wu, J., Sutherland, J. M., . . . Kroenke, K.
(2009). Development and initial validation of the PEG, a three-item scale assessing pain
intensity and interference. Journal of General Internal Medicine, 24(6), 733-738.
doi:10.1007/s11606-009-0981-1
Kubler-Ross, E. (1972). On death and dying. JAMA, 211.2, 174-179.
Lamb, S. E., Hansen, Z., Lall, R., Castelnuovo, E., Withers, E. J., Nichols, V., . . . Underwood, M. R.
(2010). Group cognitive behavioural treatment for low-back pain in primary care: a
randomised controlled trial and cost-effectiveness analysis. Lancet, 375, 916-923.
doi:10.1016/s01406736(09)62164-4
Lawrence, J., Hoeft, F., Sheau, K., & Mackey, S. (2011). Strategy-dependent dissociation of the
neural correlates involved in pain modulation. Anesthesiology, 115(4), 844-851.
doi:10.1097/ALN.0b013e31822b79ea
Martinson, A., Craner, J., & Clinton-Lont, J. (2020). Outcomes of a 6-week Cognitive-Behavioral
Therapy for Chronic Pain Group for veterans seen in primary care. Translational
Behavioral Medicine, 10, 254-266. doi:10.1093/tbm/iby127
Matthias, M. S., Parpart, A. L., Nyland, K. A., Huffman, M. A., Stubbs, D. L., Sargent, C., & Bair,
M. J. (2010). The patient-provider relationship in chronic pain care: providers'
perspectives. Pain Medicine, 11, 1688-1697.
McCraken, L. M., Vowles, K. E., & Eccleston, C. (2004). Acceptance of chronic pain: component
analysis and a revised assessment method. Pain, 107, 159-166.
Miller, R. P., Kori, S., & Todd, D. (1991). The Tampa Scale: A measure of kinesiophobia. Clinical
Journal of Pain, 7(1), 51-52.
Moore, J. E., Von Korff, M., Cherkin, D., Saunders, K., & Lorig, K. (2000). A randomized trial of a
cognitive-behavioral program for enhancing back pain self care in a primary care setting.
Pain, 88, 145-153.
Morris, D. W., Toups, M., & Trivedi, M. H. (2012). Measurement-based care in the treatment of
clinical depression. Focus 10, 428-433.
Murphy, J. L., McKellar, J. D., Raffa, S. D., Clark, M. E., Kerns, R. D., & Karlin, B. E. Cognitive
behavioral therapy for chronic pain among veterans: Therapist manual. Washington, DC:
U.S. Department of Veterans Affairs.
Pickering, T., Hall, J., Appel, L., Falkner, B., Graves, J., Hill, M., . . . Roccella, E. (2005).
Recommendations for blood pressure measurement in humans and experimental
animals part 1: blood pressure measurement in humans: a statement for professionals
from the Subcommittee of Professional and Public Education of the American Heart
Association Council on High Blood Pressure Research. Circulation, 11, 697-716.
100
Scott, K., & Lewis, C. C. (2014). Using measurement-based care to enhance any treatment.
Cognitive and Behavioral Practice, 22, 49-59.
Smith, B. H., & Torrance, N. (2011). Management of chronic pain in primary care. Curr Opin
Support Palliat Care, 5(2), 137-142. doi:10.1097/SPC.0b013e328345a3ec
Stewart, M. O., Karlin, B. E., Murphy, J. L., Raffa, S. D., Miller, S. A., McKellar, J., & Kerns, R. D.
(2015). National dissemination of cognitive-behavioral therapy for chronic pain in
veterans: therapist and patient-level outcomes. Clin J Pain, 31(8), 722-729.
doi:10.1097/ajp.0000000000000151
Von Korff, M., Moore, J. E., Lorig, K., Cherkin, D. C., Saunders, K., Gonzales, V. M., . . . Comite, F.
(1998). A randomized trial of a lay person-led self-management group intervention for
back pain patients in primary care. Spine (Phila Pa 1976), 23(23), 2608-2615.
Wetherell, J. L., Afari, N., Rutledge, T., Sorrell, J. T., Stoddard, J. A., Petkus, A. J., . . . Atkinson, J.
H. (2011). A randomized, controlled trial of acceptance and commitment therapy and
cognitive-behavioral therapy for chronic pain. Pain, 152(9), 2098-2107.
doi:10.1016/j.pain.2011.05.016
Williams, A. d. C., Fisher, E., Hearn, L., & Eccleston, C. (2020). Psychological therapies for the
management of chronic pain (excluding headache) in adults. Cochrane Database of
Systematic Reviews, (8).
101
Appendix 1:
Patient Handouts
102
Module 1 Patient Handouts:
Education and Goal Identification

103
Brief Cognitive Behavioral Therapy for Chronic Pain
This treatment focuses on how you think, feel, and behave in relation to your pain. As
shown in the picture below, these things are all related:
For example, chronic pain could lead to:
• Thoughts like, “I’m never going to feel better”
• Avoiding activities, even ones that you enjoy
• Feeling sad, angry, or worried
The goal of this treatment is to help you address these common reactions to chronic
pain so that you feel more confident in your ability to do things you enjoy and live a
full and meaningful life despite having pain.
Behaviors:
Not spending
time with friends
or family
Emotions:
Sadness,
Anger, Worry
Chronic
Pain
Thoughts:
Assuming the
worst or
focusing on pain
Treatment Goals
• Learn new strategies to cope with pain
• Improve your physical and emotional functioning
• Decrease how often you experience flare-ups as well as how
much they impact you
• Reduce the intensity of your pain

104
The Chronic Pain Cycle
Many people with chronic pain fear that movement will increase pain or cause physical damage/injury. This fear often
leads a decrease in activities which then leads to physical deconditioning (e.g., less strength and stamina, weight gain).
Dealing with constant pain may also lead to negative thoughts and
emotions such as frustration and depression. All of these factors
contribute to increased avoidance of people and activities.
THE COSTS OF INACTIVITY
While this cycle is understandable for those
with chronic pain, it is not helpful! In fact,
getting stuck in this cycle actually makes things
worse over time:
• More pain
• Poor physical fitness
• Less time with family and friends
• Depressed mood or increased irritability
• Lower self-esteem
• Increased strain on relationships
• Decreased quality of life

105
Factors That Impact Pain
Below are just a few examples of factors
that may impact your pain:
Factors That May Increase Pain
Factors That May Decrease Pain
Physical Factors
Illness or new injuries
Seeking medical treatments
Muscle tension
Using relaxation techniques
Thoughts
Expecting the worst
Balancing positive and negative thinking
Focusing on pain
Distracting yourself
Emotions
Depression or anger
Appropriate emotional expression, seeking
social support, engaging in pleasant
activities
Chronic pain is impacted by many factors. The interactions among these factors (shown
below) influence how you feel overall:
1. Biological factors
• Pain, medical issues
2. Psychological factors
• Emotions, attention, thoughts
3. Social factors
• Relationships, job, hobbies
The good news is that while some factors may increase your pain, others may decrease it.
You can decide how to manage many of these factors.
Biological
Factors
Social
Factors
Psychological
Factors

106
Factors That May Increase Pain
Factors That May Decrease Pain
Stress/worry/anxiety
Exercising safely and using relaxation
techniques
Behaviors
Too much (or too little) activity
Pacing yourself
Lack of involvement in hobbies
Doing more of what you enjoy
Social Interactions
Social isolation
Spending time with family and/or friends
Lack of (or too much) support from others
Volunteering/staying involved with
community
What are some things that have helped make your experience with
pain better?
1. ________________________________________________________________
2. ________________________________________________________________
3. ________________________________________________________________
What are some things that have made your experience with pain
worse?
1. ________________________________________________________________
2. ________________________________________________________________
3. ________________________________________________________________

107
SMART Goal Setting
A SMART goal uses the following guidelines:
Adapted from Doran, 1981
SMART Goal Versus Non-SMART Goal
Non-SMART Goal:
I want to get into physical shape.
SMART Goal:
I want to be more active by walking twice a week for 30
minutes for the next three months so that I can keep up with my
grandchildren when I see them during the holidays.
Non-SMART Goal:
I want to be more social.
SMART Goal:
I want to go watch a movie and eat dinner with my friends
once a week for the next three months so I spend less time alone while I
manage my chronic pain.
S
Specific
M
Measurable
A
Attainable
R
Relevant
T
Time-bound
Should identify a specific action or event that will take
place. In other words, “What specifically do I want to
do?”
Should be able to track progress. In other words,
“How will I know I have met my goal?”
Should be attainable and realistic. In other words, “Is
this really something that I can do?”
Should be personally meaningful and really matter.
In other words, “How important is this to me?”
Should state the time period for accomplishing the
goal. In other words, “By when do I want to achieve
this goal?”

108
Short-term goals can be accomplished over the course of this treatment (about 3
months). For each goal, consider if it fits the SMART criteria listed above. These should
be personally meaningful goals that motivate you to complete the program and improve
your pain management skills. Once goals are identified, track them on a weekly basis to
ensure that progress is occurring. If it is not, make adjustments as needed.
Short-Term Goals
In the space below, write down SMART goals you would like to achieve in the next three
months.
1. ________________________________________________________________
2. ________________________________________________________________
3. ________________________________________________________________
Accomplishing short-term goals keeps us motivated to achieve long-term goals. Long-
term goals are those for the next 6–12 months (or even longer). They will not be
accomplished fully during this program, but you can continue to work towards them
using the skills you have developed.
Long-Term Goals
In the space below, write down SMART goals you would like to achieve in the next 6 –12
months.
1. ________________________________________________________________
2. ________________________________________________________________
3. ________________________________________________________________
109
Module 2 Patient Handouts:
Activities and Pacing

110
The Chronic Pain Cycle
Many people with chronic pain fear that movement will increase pain or cause physical damage/injury. This fear often
leads a decrease in activities which then leads to physical deconditioning (e.g., less strength and stamina, weight gain).
Dealing with constant pain may also lead to negative thoughts and emotions such as frustration and depression. All of
these factors contribute to increased avoidance of people and activities.
THE COSTS OF INACTIVITY
While this cycle is understandable for those
with chronic pain, it is not helpful! In fact,
getting stuck in this cycle actually makes things
worse over time:
• More pain
• Poor physical fitness
• Less time with family and friends
• Depressed mood or increased irritability
• Lower self-esteem
• Increased strain on relationships
• Decreased quality of life

111
Pleasant Activities List
Try different activities to distract yourself from pain and improve your mood.
Which of the following are activities that have helped you feel better in the past
or are some new things that you would like to try? Check off any that apply!
Adapted with permission from K.M. Phillips, Ph.D.
□ Repair or fix something
□ Start or finish a project
□ Go to the pool or beach
□ Plan something nice for others
□ Go for a drive
□ Decorate or re-arrange your home
□ Knit or sew
□ Sing or play an instrument
□ Do hobbies (e.g., building models)
□ Visit with family or friends
□ Enjoy a hot bath or shower
□ Chat with your neighbor
□ Write or journal
□ Play games or do puzzles
□ Go shopping
□ Meditate or pray
□ Other activities/ideas?
_____________________________
_____________________________
□ Go fishing
□ Text, email, or call friends/family
□ Get your hair cut or nails done
□ Take a walk, exercise, or stretch
□ Do yard work or gardening
□ Read a book or magazine
□ Watch or participate in sports
□ Go to the park
□ Organize
□ Woodwork
□ Surf the internet
□ Look into classes you’d like to take
□ Plan a trip
□ Draw or paint
□ Walk your dog/play with your pet
□ Listen to music
□ Watch a movie or your favorite
show
□ Take or edit pictures

112
Pleasant Activities Schedule
List some activities that you enjoy doing:
1. ______________________________________________________________________
2. ______________________________________________________________________
3. ______________________________________________________________________
4. ______________________________________________________________________
Choose at least two pleasant activities that can be scheduled over the course
of the week and write them on your personalized pleasant activity schedule on the
next page.
Place an “X” to schedule your pleasant activity (example shown below).
Activity
Sun
Mon
Tues
Wed
Thu
Fri
Sat
Gardening
X
X
X
Circle the “X” when completed (example shown below).
Activity
Sun
Mon
Tues
Wed
Thu
Fri
Sat
Gardening
X
X
X
113
Pleasant Activities Schedule, continued
Now schedule your own pleasant activities. The example from above is shown in
the shaded area.
Activity
Sun
Mon
Tues
Wed
Thu
Fri
Sat
Gardening
X
X
X
Remember to not overdo it when engaging in activities! This is an important
concept that will be discussed in more detail later.

114
Pacing Activities
Some people with chronic pain may be fearful about harming themselves and avoid
activity altogether. Others are prone to pushing through pain on a “good pain day” to
accomplish a strenuous task and will not stop until it is complete. The next day, they
wake up with a pain flare-up and must rest for a day or more to recover!
The example above describes the Overactivity Cycle. If the Overactivity Cycle happens
on a recurring basis, it can lead to negative consequences such as increased stress and
anxiety, decreased efficiency, lowered self-esteem, and avoidance of any activity.
Engaging in a moderate, safe level of activity on a regular basis helps you avoid this cycle
of being underactive or overactive. Using the skill of pacing, where time is the guide for
activity engagement, can be a helpful strategy. Pacing is about balancing activities,
planning ahead, and working “smarter not harder.”
How to Pace
1. Estimate how long you can safely do one of your regular activities (e.g., yardwork,
dishes) without causing a severe pain flare-up.
2. Set the length of time you’ve chosen minus one minute as your "active" goal time
for the activity.
3. Approximate the amount of "resting" time you will need in order to safely
resume activity or continue your day.
Overactivity
Increased
Pain
Increased
Rest

115
Pacing Activities, continued
Remember
You might discover that the amount of time you can stay active may need adjusting
after you practice pacing for the first time. It is important to stick with the time-based
pacing goals, even if you are having a “good” or “bad” pain day. Sticking to the pacing
schedule prevents you from getting stuck in the overactivity or inactivity cycle.
Spread out activities during the week and be reasonable with the schedule so you can
succeed.
Use the table on the next page to record how you pace activities this week. Use the
sample below as your guide where each period of activity and rest equals one cycle.
Examples
In the first example, one cycle of pacing was completed on Day 1 (working for 10
minutes and resting for 15 minutes). Two cycles of pacing were completed on Day 2
(working for 10 minutes and resting for 15 minutes).
Activity 1: Gardening
Active Goal
(Minutes)
Rest Goal
(Minutes)
Number of Cycles
Day 1
10
15
1
Day 2
10
15
2
Activity 2: Washing dishes
Active Goal
(Minutes)
Rest Goal
(Minutes)
Number
of Cycles
Day 1
15
10
1
Day 2
15
10
2

116
Pacing Activities, continued
Schedule Your Own Activity 1: _________________________________
Active Goal
(Minutes)
Rest Goal
(Minutes)
Number
of Cycles
Day 1
Day 2
Day 3
Day 4
Day 5
Day 6
Day 7
Schedule Your Own Activity 2: _________________________________
Active Goal
(Minutes)
Rest Goal
(Minutes)
Number
of Cycles
Day 1
Day 2
Day 3
Day 4
Day 5
Day 6
Day 7
117
Module 3 Patient Handouts:
Relaxation Training
118
Relaxation: Benefits & Tips
The goal of relaxation is to reduce the effects of stress on your health. Since chronic pain
produces chronic stress on the body, it is important to regularly practice relaxation
techniques that can help your mind and body recover. Relaxation is more than resting or
enjoying a hobby – it involves using specific strategies to reduce tension.
Benefits of Relaxation
Relaxation is important for good health. When you are relaxed, your muscles are loose,
your heart rate is normal, and your breathing is slow and deep. Learning how to relax
can help especially when you feel pain. Relaxation prompts your body to release
chemicals that reduce pain and produce a sense of well-being.
Relaxation won't cure pain or other chronic symptoms, but skills that relax the body and
the mind may help decrease muscle tension, prevent muscle spasms, and relieve the
stress that can aggravate pain and other symptoms.
Taking time to relax and refuel your energy provides benefits such as:
• Improved mood
• Increased energy and productivity
• Improved concentration and focus
• Improved sense of control over stress and daily demands
• Improved nighttime sleep
• Increased self-confidence
• Greater ability to handle problems
• Decreased anxiety and other negative emotions such as anger and frustration
• Increased blood flow to muscles and reduced muscle tension
• Lower blood pressure, breathing rate, and heart rate
• Decreased pain, such as headaches and back pain
Relaxation Practice Tips
Relaxation is a skill that requires practice. You may not feel the benefits immediately, so
don't give up! Remain patient and motivated and you’ll reduce the negative impacts of
stress. And remember: If relaxation feels foreign or unnatural, that likely means you are
a person who needs it most!
119
Establish a routine
1. Set aside time to practice relaxation at least once or twice a day. Pairing
relaxation with a regular activity may help you remember to practice (for
example, take ten relaxed breaths before bed or whenever you sit down to eat).
2. Practice at various times throughout the day until relaxation becomes natural
and you can use it readily when you feel stressed. You may want to leave
"reminders" for yourself to relax (for example, sticky notes on the bathroom
mirror, kitchen cabinets, or car dashboard with the words "relax" or "breathe").
Be comfortable
1. Practice on a comfortable chair, sofa, mat, or bed. Dim the lights.
2. Loosen tight clothing and remove shoes, belt, glasses or contact lenses, if you
like.
Concentrate
1. Eliminate disruptions. Turn off the TV, radio, or telephone.
2. Practice in a quiet, calm environment.
3. Close your eyes to reduce distractions and improve concentration. If you prefer,
keep your eyes open and focus on one spot.
4. Move your body as little as possible, changing positions only for comfort. Don't
worry if you have some distracting thoughts—it happens to everyone. Just notice
that your thoughts have wandered and then gently, without judgment, return
your attention to your breath.
Relax
1. Begin and end relaxation practices with relaxed breathing techniques.
2. Use a relaxation CD if it helps. Gradually, learn to relax without a CD so that you
can use relaxation techniques anywhere.
120
3. Let relaxation proceed naturally and spread throughout your body. Do not try to
resist.
Be patient
1. Give yourself time to learn relaxation skills. Practice is required for these
techniques to become automatic.
2. Try not to become upset if you have trouble concentrating. A wandering mind is
normal and expected. Keep bringing your attention back to your breath.
3. Don't worry about how well you are practicing.
4. After a few weeks, select a word, such as "calm," "relax," “peace," or “patience”
that you can say during relaxation practices. Eventually, simply saying that word
may help you relax.
Incorporate relaxation into daily life
1. Over time, move relaxation practices from planned, quiet settings to "real life."
The goal is to be able to calm yourself when necessary, no matter where you are.
2. Use relaxation whenever you notice yourself feeling stressed or anxious, such as
waiting in line, at a doctor’s appointment, or during a difficult meeting.
121
Deep Breathing Training
1. Start by becoming aware of your breathing. Place one hand on your abdomen at the
waistline just over the bellybutton and the other hand on the center of your chest.
Without trying to change anything, simply notice how you are breathing. Notice where
you are breathing from, whether your shoulders are rising and falling, whether your chest
is rising and falling, or perhaps whether your belly is rising and falling. Notice how your
hands move as you breathe. Pay attention to whether one hand is moving more than the
other. (PAUSE 5 seconds)
2. Now notice the rate of your breathing. Pay attention to whether you are breathing rapidly
or slowly. Your breathing may be deep or shallow. (PAUSE 5 seconds)
3. Now as you slowly inhale, imagine the air flowing deeper into your belly. Feel your belly
fill with air as your lower hand rises. Pause briefly at the top of your breath, and then
follow your breath out as you completely exhale. Slowly take a breath in…two, three,
four, and slowly exhale…two, three, four. Let any tension melt away as you relax more
deeply with each breath. (PAUSE 5 seconds)
4. Notice the feeling of cool fresh air entering through your nose, through your nasal
passage, to the back of your throat, and descends deep into your lungs. Notice what
happens as you are inhaling… and then exhaling... Feel the temperature of each breath
cool as you inhale, and warm as you exhale. Count your breaths as you breathe in and
out. (PAUSE 10 seconds)
5. Notice your breath becoming smooth and slow. Feel your belly and ribcage expand
outward with each breath. Feel yourself become more relaxed with each exhale. Allow
your shoulders to become heavier with each exhale. (PAUSE 15 seconds)
6. Continue breathing slowly and gently. (PAUSE 15 seconds)
7. Again, slowly take a breath in…two, three, four, and slowly exhale…two, three, four. Feel
yourself become more and more relaxed with each exhale. (PAUSE 15 seconds)
8. Continue breathing slowly and gently. (PAUSE 15 seconds)
9. Now, as I count from five to one, feel yourself become more alert. Five…bringing your
attention to this room. Four…feeling calm and relaxed. Three…start to wiggle your fingers
and toes. Two…slowly start to move and stretch your muscles. One…open your eyes,
feeling refreshed.
122
Progressive Muscle Relaxation
Noticing the difference between tensed and relaxed muscles is important. This skill
reduces anxiety by promoting relaxation and helps you to recognize when your body is
tense. In order to master this skill, you will be asked to tense certain muscle groups as
hard as you can without hurting yourself. After 5 seconds of holding the tension, you
will be instructed to relax your muscles and release the tension.
1. Tense your lower arms by making fists with your hands and pulling your fists up
by bending your wrists. Focus on the tension. (PAUSE 5 seconds)
2. Now release the tension. Let your hands and lower arms relax onto the chair or
bed beside you. Feel the release from tension as you relax the muscles fully.
(PAUSE 10 seconds)
3. Create tension in the upper arms by pulling the arms back and in toward your
sides. Feel the tension in the back of the arms and radiating towards the
shoulders and into the back. Focus on the tension and hold. (PAUSE 5 seconds)
4. Now, release the arms and let them relax – almost feeling heavy at your sides.
Notice the difference between the previous tension and the new feelings of
relaxation. Your arms might feel heavy, warm, and relaxed. (PAUSE 10 seconds)
5. Now bring your attention to your lower legs. Build tension by extending your legs
in front of you and pointing your toes toward your upper body. Feel the tension
as it spreads through your feet, ankles, shins, and calves. Hold this tension.
(PAUSE 5 seconds)
6. Release all of the tension in your lower legs. Let your legs relax onto the chair or
bed. Feel the difference in these muscles as they relax. Feel the release from
tension, the sense of comfort, the heaviness of relaxation. (PAUSE 10 seconds)
Continue working through the various muscle groups, alternating between tension and
release. Remember to feel the tightness when holding the tension, and to notice the
difference between tension and relaxation upon release.
7. Upper legs and buttocks: Tense by pressing knees together and lifting legs
slightly off the bed or chair. (PAUSE 5 seconds). Release tension by letting legs
sink into chair or bed. (PAUSE 10 seconds)
123
8. Abdomen: Tense by pulling your abdomen in towards your spine. (PAUSE 5
seconds). Release tension by relaxing your abdomen to its normal position.
(PAUSE 10 seconds)
9. Chest: Build tension in your chest by taking in a deep breath and holding it.
(PAUSE 3-5 seconds). Release tension by slowly letting the air escape, and
resume normal breathing, letting air flow in and out smoothly and easily. (PAUSE
10 seconds)
10. Neck and shoulders: Create tension by pulling your shoulder blades back and up
towards your ears. (PAUSE 5 seconds). Release tension by letting your shoulders
drop down, sinking further and further until they are completely relaxed. (PAUSE
10 seconds)
11. Mouth, jaw, and throat: Create tension by clenching your teeth and turning the
corners of your mouth back into a forced smile. (PAUSE 5 seconds). Release the
tension by letting your jaw drop down and relaxing the muscles around your
throat and jaw. (PAUSE 10 seconds)
12. Eyes and lower forehead: Build tension by squeezing your eyes tightly shut and
pulling your eyebrows down. (PAUSE 5 seconds). Now release all the tension in
your eyes and lower forehead. (PAUSE 10 seconds)
13. Upper forehead and scalp: Build tension by raising your eyebrows as high as
possible. Feel the wrinkling and pulling across the forehead and top of the head.
(PAUSE 5 seconds). Now release all the tension in your forehead, letting the
eyebrows gently rest down. (PAUSE 10 seconds)
Now, you will work towards a state of relaxation.
14. Your whole body is feeling relaxed and calm. Scan your body for any last bits of
tension and if you notice any, let that tension go. Enjoy the feelings of relaxation.
(PAUSE 5 seconds)
15. As I count from one to five, feel yourself become more and more relaxed.
One…let all tension leave your body. Two…sink further and further into
relaxation. Three…feel more and more relaxed. Four…feel very relaxed.
Five…deeply relaxed. (PAUSE 30 seconds)
124
16. As you spend a few minutes in this relaxed state, think about your breathing. Feel
the cool air as you breathe in and the warm air as you breathe out. Your
breathing is smooth and regular. Every time you breathe out, think to yourself
"relax, relax, relax." You are feeling comfortable and relaxed. (PAUSE 1-3
seconds)
17. Now, as I count from five to one, feel yourself become more alert. Five…bringing
your attention to this room. Four…feeling calm and relaxed. Three…start to
wiggle your fingers and toes. Two…slowly start to move and stretch your muscles.
One…open your eyes, feeling refreshed and rejuvenated.

125
Relaxation Practice Record
Use the record below to chart your relaxation practice over time.
• Before you begin your practice, use the scale below to rate your level of tension.
• After you complete the practice, use the same scale again to rate your level of
tension.
• Noting any differences will help you figure out if the exercises are helping you
relax.
But remember, these exercises take practice and it might take several tries before
you start to see results!
Date
How long did you
practice?
(minutes)
Level of tension
before practice
(0-10)
Level of tension
after practice
(0-10)
What did I notice?
Extremely
Tense
Slightly
Tense
Slightly
Relaxed
Very
Relaxed
Totally
Relaxed
0
1
2
3
4
5
6
7
8
9
10
126
Module 4 Patient Handouts:
Cognitive Coping 1
127
Brief Cognitive Behavioral Therapy for Chronic Pain
This treatment focuses on how you think, feel, and behave in relation to your pain. As
shown in the picture below, these things are all related:
For example, chronic pain could lead to:
• Thoughts like, “I’m never going to feel better”
• Avoiding activities, even ones that you enjoy
• Feeling sad, angry, or worried
The goal of this treatment is to help you address these common reactions to chronic
pain so that you feel more confident in your ability to do things you enjoy and live a
full and meaningful life despite having pain.
Behaviors:
Not spending
time with friends
or family
Emotions:
Sadness,
Anger, Worry
Chronic
Pain
Thoughts:
Assuming the
worst or
focusing on pain
Treatment Goals
• Learn new strategies to cope with pain
• Improve your physical and emotional functioning
• Decrease how often you experience flare-ups as well as how
much they impact you
• Reduce the intensity of your pain
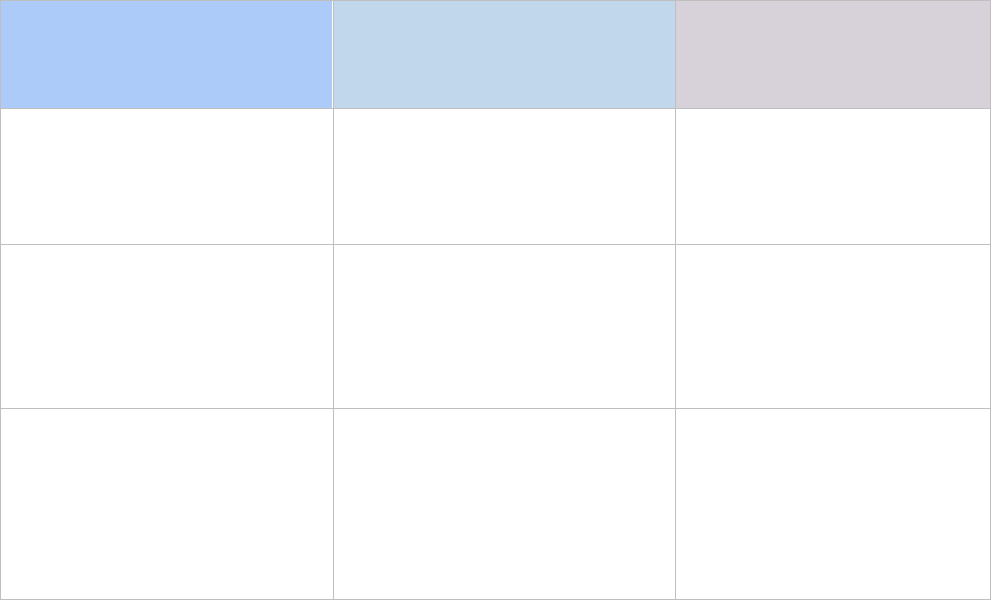
128
PAIN THOUGHTS:
Identifying and Replacing Thoughts That Are Not Helpful
Thinking about how much pain you are in does not help you cope with the pain. As pain
increases, thoughts may become more negative; as thoughts become more negative,
pain often increases further. Negative thoughts can lead to:
• Worsening mood
• Avoiding activities
• Isolating/avoiding others
Although pain thoughts can be automatic, with practice you can become more aware
when you have them. Then you can replace unhelpful thoughts with ones that are
helpful. Here are some examples of unhelpful pain thoughts and some coping
statements that you can use to replace them:
Common Pain Thoughts
Types of
Unhelpful Thoughts
Examples of
Unhelpful Thoughts
Examples of
Helpful Thoughts
Catastrophizing
Believing something is the
worst it could possibly be.
When my pain is bad, I can’t
do anything.
Even when my pain is bad,
there are still some things I
can do.
Should Statements
Thinking in terms of how
things should, must, or
ought to be.
My doctor should be able to
cure my pain.
There is no cure for chronic
pain, but I can use skills to
cope with my pain.
All or None Thinking
Seeing things as “either or”
or “right or wrong” instead
of in terms of degrees.
I can only be happy if I am
pain free.
Even if I am in pain, I can
still be happy. There is
always something that I
can do to have a better
quality of life.

129
Types of
Unhelpful Thoughts
Examples of
Unhelpful Thoughts
Examples of
Helpful Thoughts
Overgeneralization
Viewing one or two bad
events as an endless pattern
of defeat.
I tried doing exercises for my
back pain before and it didn’t
help. So, it isn’t going to help
now.
Although physical therapy
didn’t help much before,
maybe this time it will help.
I might as well try.
Jumping to Conclusions
Drawing negative
conclusions of events that
are not based on fact.
When I move my back hurts,
so it must be bad for me to
move.
Hurt does not equal harm.
Emotional Reasoning
Believing how you feel
reflects how things really
are.
I feel useless, so I am useless.
Even though I can’t do all
the things I used to do, it
doesn’t mean I can’t do
anything.
Disqualifying the Positive
Focusing on only the bad
and discounting the good.
So what if I am doing more, I
am still in pain.
Doing more is important
for me to live the life I want
to live.
Used with permission from KM. Phillips, Ph.D.
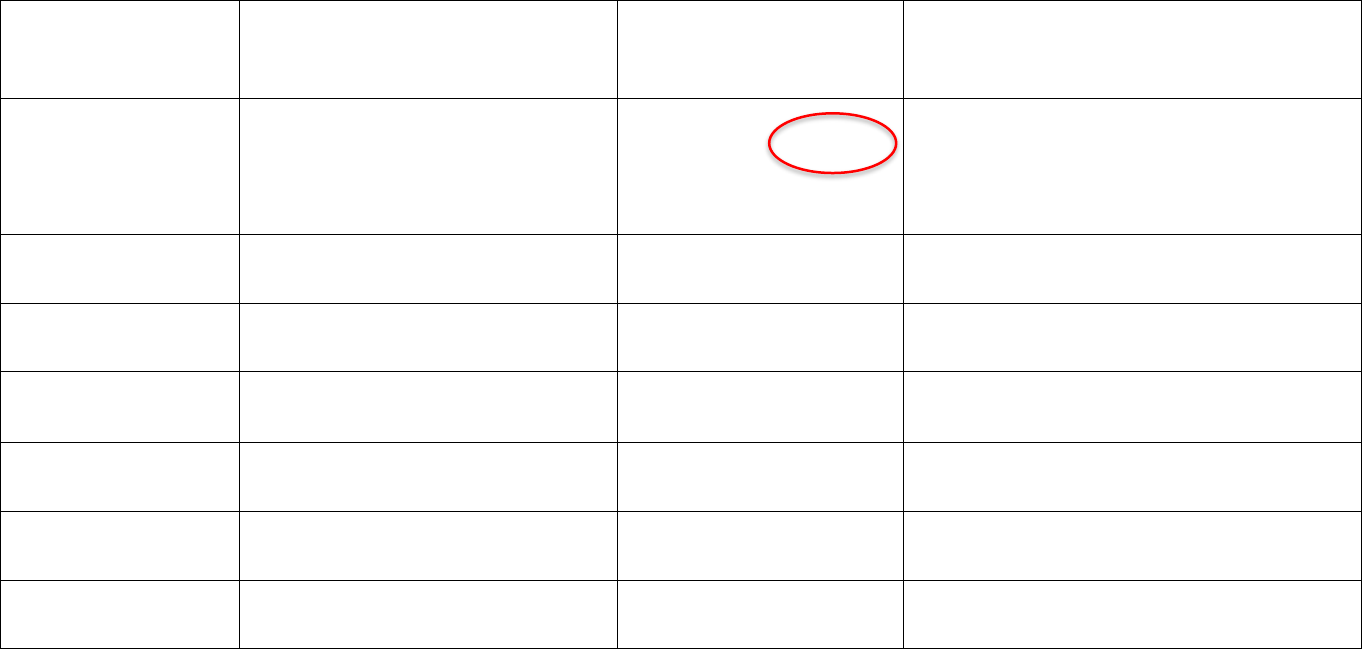
130
CATCHING ANTs: How to Catch, Check, & Challenge Automatic Negative Thoughts
When we feel upset or angry, most often we also have negative thoughts. These thoughts may happen automatically and
increase your pain and negative mood. You can feel better physically and emotionally by “catching” ANTs when they
occur, noticing how they make you feel, and challenging them with more balanced thoughts. Using the chart below,
record at least one ANT each day. Evaluate the thought and generate a new helpful one.
Day/Situation
Catch It!
Identify ANT
Check It!
Effect on your
pain/mood
Challenge It!
Positive/balanced coping
statement
Tuesday/Cleaning
garage and pain
flares
This pain is killing me. I can’t
do anything anymore.
Helpful or Unhelpful
I am hurting right now because I
overdid it, but I know that I will feel
better soon. Then I will pace myself
to get the job done.
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Adapted with permission from S. Palyo, Ph.D. & J. McQuaid, Ph.D.
131
Module 5 Patient Handouts:
Cognitive Coping 2
.

132
Brief Cognitive Behavioral Therapy for Chronic Pain
This treatment focuses on how you think, feel, and behave in relation to your pain. As
shown in the picture below, these things are all related:
For example, chronic pain could lead to:
• Thoughts like, “I’m never going to feel better”
• Avoiding activities, even ones that you enjoy
• Feeling sad, angry, or worried
The goal of this treatment is to help you address these common reactions to chronic
pain so that you feel more confident in your ability to do things you enjoy and live a
full and meaningful life despite having pain.
Behaviors:
Not spending
time with friends
or family
Emotions:
Sadness,
Anger, Worry
Chronic
Pain
Thoughts:
Assuming the
worst or
focusing on pain
Treatment Goals
• Learn new strategies to cope with pain
• Improve your physical and emotional functioning
• Decrease how often you experience flare-ups as well as how
much they impact you
• Reduce the intensity of your pain

133
PAIN THOUGHTS:
Identifying and Replacing Thoughts That Are Not Helpful
Thinking about how much pain you are in does not help you cope with the pain. As pain
increases, thoughts may become more negative; as thoughts become more negative,
pain often increases further. Negative thoughts can lead to:
• Worsening mood
• Avoiding activities
• Isolating/avoiding others
Although pain thoughts can be automatic, with practice you can become more aware
when you have them. Then you can replace unhelpful thoughts with ones that are
helpful. Here are some examples of unhelpful pain thoughts and some coping
statements that you can use to replace them:
Common Pain Thoughts
Types of
Unhelpful Thoughts
Examples of
Unhelpful Thoughts
Examples of
Helpful Thoughts
Catastrophizing
Believing something is the
worst it could possibly be.
When my pain is bad, I can’t
do anything.
Even when my pain is bad,
there are still some things I
can do.
Should Statements
Thinking in terms of how
things should, must, or
ought to be.
My doctor should be able to
cure my pain.
There is no cure for chronic
pain, but I can use skills to
cope with my pain.
All or None Thinking
Seeing things as “either or”
or “right or wrong” instead
of in terms of degrees.
I can only be happy if I am
pain free.
Even if I am in pain, I can
still be happy. There is
always something that I
can do to have a better
quality of life.

134
Types of
Unhelpful Thoughts
Examples of
Unhelpful Thoughts
Examples of
Helpful Thoughts
Overgeneralization
Viewing one or two bad
events as an endless pattern
of defeat.
I tried doing exercises for my
back pain before and it didn’t
help. So, it isn’t going to help
now.
Although physical therapy
didn’t help much before,
maybe this time it will help.
I might as well try.
Jumping to Conclusions
Drawing negative
conclusions of events that
are not based on fact.
When I move my back hurts,
so it must be bad for me to
move.
Hurt does not equal harm.
Emotional Reasoning
Believing how you feel
reflects how things really
are.
I feel useless, so I am useless.
Even though I can’t do all
the things I used to do, it
doesn’t mean I can’t do
anything.
Disqualifying the Positive
Focusing on only the bad
and discounting the good.
So what if I am doing more, I
am still in pain.
Doing more is important
for me to live the life I want
to live.
Used with permission from KM. Phillips, Ph.D.

135
CATCHING ANTs: How to Catch, Check, & Challenge Automatic Negative Thoughts
When we feel upset or angry, most often we also have negative thoughts. These thoughts may happen automatically and
increase your pain and negative mood. You can feel better physically and emotionally by “catching” ANTs when they
occur, noticing how they make you feel, and challenging them with more balanced thoughts. Using the chart below,
record at least one ANT each day. Evaluate the thought and generate a new helpful one.
Day/Situation
Catch It!
Identify ANT
Check It!
Effect on your
pain/mood
Challenge It!
Positive/balanced coping
statement
Tuesday/Cleaning
garage and pain
flares
This pain is killing me. I can’t
do anything anymore.
Helpful or Unhelpful
I am hurting right now because I
overdid it, but I know that I will feel
better soon. Then I will pace myself
to get the job done.
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Helpful or Unhelpful
Adapted with permission from S. Palyo, Ph.D. & J. McQuaid, Ph.D.

136
Coping Statements
Here are some statements that can be used to replace unhelpful thoughts. Put an “X”
next to the ones that you think may be helpful for you. What things have you told
yourself in the past to get through a pain flare or difficult situation? Add your helpful
statements to the list.
X
Coping Statement Checklist
The pain flare passes in a while.
I can handle this. I just have to make it through this moment.
I’ve gotten through it before and I can get through it again.
I don’t have to suffer. I have skills I can use to cope.
What would I tell a friend who was in pain?
How can I set a good example for my kids about coping with
life’s challenges?
How would someone I admire cope with this?
I just have to focus on something else.
There may be no cure, but I can still live my life.
I’m going to focus on what I can do, not what I can’t do.
Adapted with permission from K.M. Phillips, Ph.D.
Remember: It’s easy to think of positive statements when you’re feeling okay. But, if
you are in a bad mood or having a pain flare, it’s more difficult. Keep a list of these or
other helpful statements in a place where you can easily find them when you need them
most (e.g., in your wallet, on your refrigerator, in your phone).
137
Module 6 Patient Handouts:
The Pain Action Plan
.

138
Anticipating Obstacles: Plan for Coping
People have many challenging situations in their lives and it is expected that certain
obstacles will arise. A difficult day may involve life stressors and increased pain
symptoms. The best time to plan for how you will cope with and manage your pain
during one of these days is now.
Below, identify the specific things in your life that may be triggers for pain flare-ups, as
well as how you may cope with challenges using the skills that you have learned.
Potential Obstacles/Triggers/Stressors: (Example: Kids fighting, Cold weather)
1. ______________________________ 2. ______________________________
3. ______________________________ 4. ______________________________
5. ______________________________ 6. ______________________________
Ways to Cope: (Example: Walking, Deep breathing, Pleasant activity)
1. ______________________________ 2. ______________________________
3. ______________________________ 4. ______________________________
5. ______________________________ 6. ______________________________
Remember:
BE PREPARED! Consider all the tools you have learned and do not undersell yourself or
let automatic negative thoughts (ANTs) sabotage you. Contact friends, family, and VA
providers who are there to provide support as needed.

139
Weekly Activities Schedule
Use the schedule provided to plan your activities for the upcoming week. Be as
specific as possible and include items such as doing the dishes as well as the pain
management strategies you will employ regularly such as using relaxation techniques.
Be realistic in your planning so that you are able to follow the schedule.
Time
Sun
Mon
Tues
Wed
Thurs
Fri
Sat
7:00 a.m.
8:00
9:00
10:00
11:00
12:00 p.m.
1:00
2:00
3:00
4:00
5:00
Evening

140
SMART Goal Setting
A SMART goal uses the following guidelines:
Adapted from Doran, 1981
SMART Goal Versus Non-SMART Goal
Non-SMART Goal:
I want to get into physical shape.
SMART Goal:
I want to be more active by walking twice a week for 30
minutes for the next three months so that I can keep up with my
grandchildren when I see them during the holidays.
Non-SMART Goal:
I want to be more social.
SMART Goal:
I want to go watch a movie and eat dinner with my friends
once a week for the next three months so I spend less time alone while I
manage my chronic pain.
S
Specific
M
Measurable
A
Attainable
R
Relevant
T
Time-bound
Should identify a specific action or event that will take
place. In other words, “What specifically do I want to
do?”
Should be able to track progress. In other words,
“How will I know I have met my goal?”
Should be attainable and realistic given resources. In
other words, “Is this really something that I can do?”
Should be personally meaningful and really matter.
In other words, “How important is this to me?”
Should state the time period for accomplishing the
goal. In other words, “By when do I want to achieve
this goal?”

141
Short-term goals can be accomplished over the near future, or about 3 months from
now. For each goal, consider if it fits the SMART criteria listed above. These should be
personally meaningful goals that motivate you to complete the program and improve
your pain management skills. Once goals are identified, track them on a weekly basis to
ensure that progress is occurring. If it is not, make adjustments as needed.
Short-Term Goals
In the space below, write down SMART goals you would like to achieve in the next three
months.
1. ________________________________________________________________
2. ________________________________________________________________
3. ________________________________________________________________
Accomplishing short-term goals keeps us motivated to achieve long-term goals. Long-
term goals are those for the next 6–12 months (or even longer). They will not be
accomplished fully during this program, but you can continue to work towards them
using the skills you have developed.
Long-Term Goals
In the space below, write down SMART goals you would like to achieve in the next 6–12
months.
1. ________________________________________________________________
2. ________________________________________________________________
3. ________________________________________________________________
142
Appendix 2:
Pain Conditions

143
PAIN CONDITIONS
From Murphy, J. L., McKellar, J. D., Raffa, S. D., Clark, M. E., Kerns, R. D., & Karlin, B. E.
Cognitive behavioral therapy for chronic pain among veterans: Therapist manual.
Washington, DC: U.S. Department of Veterans Affairs.
Low Back Pain. Low back pain (LBP or lumbago) is the most common form of pain and the
most fiscally costly worldwide in terms of medical visits and loss of work productivity (Deyo &
Weinstein, 2001). Most people with acute LBP recover in a matter of weeks, but for about
10% the pain will become chronic (Costa et al., 2012). Many individuals who experience
chronic LBP report high levels of fear of movement and consequently are prone to
deconditioning of the muscles leading to greater disability. LBP may be due to factors such as
herniated discs, degenerative disc disease, spinal stenosis, or arthritis, but the vast majority of
back pain is due to muscle strain (Deyo & Weinstein, 2001).
Middle and Upper Back Pain. Middle and upper back pain is less common than LBP because
the bones in these areas do not move as often. As in the lower area of the back, pain is most
often related to muscle sprain or overuse, herniated discs, or arthritic processes.
Neck Pain. Neck pain (i.e., cervicalgia) is a common issue with about 65% of the population
experiencing it at some point in their lives. It is generally caused by activities that strain the
neck such as poor posture or sleeping, muscle tightness, or whiplash from a motor vehicle
accident. Neck pain may also be associated with headache pain.
Osteoarthritis. Osteoarthritis (OA) is the most common form of arthritis (Prieto-Alhambra &
Judge, 2013) and occurs when cartilage that cushions the ends of bones and joints
deteriorates. Because of this, OA is often referred to as the “wear and tear” disease and is
common among Veterans given engagement in military and non-military occupations that
often involve physical labor (Morgenroth, Gellhorn, & Suri, 2012). The most common areas of
the body affected include hands, feet, neck, low back, knees, and hips.
Rheumatoid Arthritis. Rheumatoid arthritis (RA) is a chronic, systemic inflammatory disorder
that primarily affects the joints. White blood cells accumulate in the joints causing swelling
and pain. Progression of the disease can lead to destruction of cartilage, ligaments, and
tendons. RA typically impacts functional status to a greater degree than OA and is twice as
prevalent in women than men.
Tendonitis/Bursitis. Tendonitis and bursitis involve inflammation of one of the tendons and
bursae, respectively. Tendons are thick cords that join muscles to bones and inflammation
causes pain and tenderness in the joints. Tendonitis is commonly associated with sports
involving repetitive motion, such as swimming or throwing a ball, but can result from any

144
repetitive movement involving the joints. Bursae are fluid-filled sacs found in joints that
surround areas where tendons, skin, and muscle tissues meet. Bursae provide essential
lubrication to the hips, knees, elbows, and heels. Damage can cause pain, swelling, and
redness.
Pelvic Floor Disorders. Pelvic floor disorders occur when the area that supports the pelvic
organs becomes weak or damaged. These may result in urinary or fecal incontinence, as well
as persistent pain in the pelvic walls. Some of the common causes are endometriosis, pelvic
floor tension myalgia, pelvic inflammatory disease, fibroids, surgeries, and irritable bowel
syndrome. Pelvic pain is much more common among women, with one in seven experiencing
some form of this chronic condition.
Gout. Gout is a type of arthritis that is characterized by inflammation, tenderness, and
stiffness in joints. The disorder is more common in men than women and often affects the big
toe. Symptoms are episodic and flare-ups are typically associated with increased levels of uric
acid. Uric acid levels are influenced by genetic factors but also by diet and lifestyle (Gheita, El-
Fishwawy, Nasrallah, & Hussein, 2012).
Peripheral Neuropathic Pain. Peripheral neuropathy typically affects the hands and feet. It
involves microvascular lesions in small blood vessels and its development is often associated
with high blood sugar secondary to diabetes. Pain is commonly, but not universally,
associated with peripheral neuropathy. Pain quality is often described as numb and tingling,
pins and needles, electric, or burning, as opposed to being characterized as “pain.”
Radicular Pain. Radicular pain is most commonly associated with LBP or neck pain, referred to
as lumbar radiculopathy and cervical radiculopathy, respectively. It radiates along a nerve due
to inflammation or irritation of the nerve root and extends from the spinal cord to areas such
as the buttocks and down the legs in the case of back pain, or down the arms in the case of
neck pain. The sudden appearance of radicular pain, new muscular weakness, or the
identification of radicular pain that is not noted by medical providers is cause for immediate
medical evaluation (Gilron, Watson, Cahill, & Moulin, 2006). Radicular pain is typically
described as burning, shooting, or shock-like (Atlas et al., 1996).
Phantom Limb Pain. A phantom limb is the sensation that an amputated or missing limb is
still attached to the body. Between 60 and 80% of individuals with an amputation experience
phantom limb sensations and the majority of these sensations are painful (Sherman,
Sherman, & Parker, 1984). In addition, pain at the site of the amputation, or stump, caused by
nerve damage in the stump region is also common. Pain is variable from a dull ache to
shooting and severe.

145
Fibromyalgia. Fibromyalgia (FM) is a disorder of unknown etiology associated with
widespread pain, sleep disturbance, fatigue, and psychological distress among other
symptoms. FM pain typically includes tender “trigger” points found in soft tissue of the back
of the neck, shoulders, low back, hips, shins, and knees, and the pain is often described as a
deep aching or burning. FM is about 7 times more common in women than men (Haviland,
Banta, & Prezekop, 2011) and individuals with FM are 3 times more likely to have a comorbid
diagnosis of major depression than individuals without FM.
Complex Regional Pain Syndrome. Complex regional pain syndrome (CRPS), previously
known as reflex sympathetic dystrophy syndrome, or RSD, is a poorly understood pain
condition that often starts after a minor injury or complication, usually to a hand, arm, foot,
or leg, and often spreads. Type 1, the form most commonly seen, has no demonstrable nerve
lesions, while there is nerve damage in Type 2. Pain is described as severe and changes in the
appearance and texture of the skin are often noticeable.
Types of Headaches
The most common types of headaches are listed below. It is important to remember,
however, that patients may have more than one kind of headache (e.g., tension-type
headaches a few times per week and migraines a few times per month). In addition, in the
same way that other pain locations may be difficult to classify, Veterans may present with
mixed symptoms that do not fall neatly into one category.
Tension-type. Tension-type headaches (TTH) are by far the most common type,
accounting for over half of all headaches (ICHD, 2nd edition, 2004). The primary sensation
associated with TTH is the feeling of a tight band wrapped around one’s head. These
range in intensity from mild to moderate and also range in frequency from episodic to
chronic. Criterion for chronic TTH is met when an individual experiences headaches for 15
days a month for at least 6 months (ICHD, 2nd edition, 2004).
Migraine. Migraine headaches occur in about 10% of the population at some point in their
lifetime (Rasmussen, Jensen, Schroll, & Olesen, 1991). They are classified as either with or
without aura, defined by symptoms such as sensory or motor disturbance that precede or
accompany the headache. Migraine headaches tend to be recurrent and are associated
with a number of autonomic nervous system symptoms. The typical migraine headache is
unilateral and pulsing in nature, lasts from 2 to 72 hours, may be associated with nausea,
vomiting, sensitivity to light and sound, and aggravated by physical activity. Migraines are
2 to 3 times more common in women than men (ICHD, 2nd edition, 2004).
Cluster. Cluster headaches involve severe unilateral pain that is orbital, supraorbital, or
temporal, lasting 15 to 180 minutes, and occurring in frequency from every other day to
up to 8 times per day (ICHD, 2nd edition, 2004). Painful episodes may be accompanied by
tearing, nasal congestion, sweating, a drooping eyelid, or a contracted pupil. These all
occur on the affected side of the face. The intense pain of cluster headaches is due to

146
dilation of blood vessels creating pressure on the trigeminal nerve. However, the
underlying cause of the dilation is not understood. This type of headache is much less
common, affecting .1% of the population, and is 3 to 4 times more common in men than
women (ICHD, 2nd edition, 2004).
Post-traumatic. Headaches associated with head trauma (e.g., mild to severe traumatic
brain injury) is common immediately following an injury, with a prevalence up to 90%. Up
to 44% of patients report continued headaches 6 months following an injury (Nicholson &
Martelli, 2004). The three most common presentation patterns are tension-type, migraine
type, or cervicogenic (Gironda et al., 2009). Exposure to blasts and concussions while
deployed make this type of headache more common among Veterans and military Service
members.
Medication Overuse. Medication overuse headaches, previously known as rebound
headaches, are a secondary cause of chronic daily headaches due to the overuse of acute
headache analgesics. Overuse is defined by treatment days per month and depends on
the drug. Overuse is often motivated by the desire to treat headaches or a fear of future
headaches, but regardless can make headaches refractory to preventative medications
(Silberstein, Lipton, & Saper, 2007).
REFERENCES
Atlas, S. J., Deyo, R. A., Patrick, D. L., Convery, K., Keller, R. B., & Singer, D. E. (1996). The
Quebec Task Force classification for spinal disorders and the severity, treatment, and
outcomes of sciatica and lumbar spinal stenosis. Spine, 21(24), 2885-2892. doi:
10.1097/00007632-199612150-00020
Costa, L. C. M, Maher, C. G., Hancock, M. J., McAuley, J. H., Herbert, R. D., & Costa, L. O. P.
(2012). The prognosis of acute and persistent low-back pain: A meta-analysis. Canadian
Medical Association Journal, 184(11), 613-624. doi: 10.1503/cmaj.111271
Deyo, R. A., & Weinstein, J. N. (2001). Low back pain. New England Journal of Medicine,
344(5), 363-370. doi: 10.1056/NEJM200102013440508
Gheita, T. A., El-Fishawy, H. S., Nasrallah, M. M., & Hussein, H. (2012). Insulin resistance and
metabolic syndrome in primary gout: Relation to punched-out erosions. Internal Journal
of Rheumatic Diseases, 15(6), 521-525. doi: 10.1111/1756-185X.12007
Gilron, I., Watson, C. P., Cahill, C. M., & Moulin, D. E. (2006). Neuropathic pain: A practical
guide for the clinician. Canadian Medical Association Journal, 175(3), 265-275.
doi:10.1503/cmaj.060146
Gironda, R. J., Clark, M. E., Ruff, R. L., Chait, S., Craine, M., Walker, R., & Scholten, J. (2009).
Traumatic brain injury, polytrauma, and pain: Challenges and treatment strategies for
the polytrauma rehabilitation. Rehabilitation Psychology, 54(3), 247-258. doi:
10.1037/a0016906
Haviland, M. G., Banta, J. E., & Przekop, P. (2011). Fibromyalgia: Prevalence, course, and co-
morbidities in hospitalized patients in the United States, 1999-2007. Clinical and
Experimental Rheumatology, 29(6 Suppl 69), 79-87.

147
International Headache Society Classification Subcommittee. (2004). International
classification of headache disorders, 2nd edition. Cephalalgia, 24(Suppl 1), 1–160.
Morgenroth, D. C., Gellhorn, A. C., & Suri, P. (2012). Osteoarthritis in the disabled
population: A mechanical perspective. Osteoarthritis, 4(5 Suppl), 20-27.
http://dx.doi.org/10.1016/j.pmrj.2012.01.003
Nicholson, K., & Martelli, M. F. (2004). The problem of pain. The Journal of Head Trauma
Rehabilitation, 19(1), 2-9. doi: 10.1097/00001199-200401000-00002
Prieto-Alhambra, D., Judge, A., Javaid, M. K., Cooper, C., Diez-Perez, A., & Arden, N. K. (2013).
Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis:
Influences of age, gender and osteoarthritis affecting other joints. Annals of the
Rheumatic Diseases, 73(9), 1659-1664. doi: 10.1136/annrheumdis-2013-203355
Rasmussen, B. K., Jensen, R., Schroll, M., & Olesen, J. (1991). Epidemiology of headache in a
general population: A prevalence study. Journal of Clinical Epidemiology, 44(11), 1147-
1157. doi: 10.1016/0895-4356(91)90147-2
Sherman, R. A., Sherman, C. J., & Parker, L. (1984). Chronic phantom and stump pain among
American Veterans: Results of a survey. Pain, 18(1), 83-95. doi:10.1016/0304-
3959(84)90128-3
Silberstein S. D., Lipton R. B., & Saper J. R. (2007). Chronic daily headache including
transformed migraine, chronic tension-type headache, and medication overuse headache.
In: Silberstein, S. D., Lipton, R. B., & Dodick, D. W. (Eds). Wolff’s Headache and Other
Head Pain. New York, NY: Oxford University Press.
148
Appendix 3:
Treatment Options for Chronic
Pain

149
TREATMENT OPTIONS FOR CHRONIC PAIN
From Murphy, J. L., McKellar, J. D., Raffa, S. D., Clark, M. E., Kerns, R. D., & Karlin, B. E. Cognitive
behavioral therapy for chronic pain among veterans: Therapist manual. Washington, DC: U.S.
Department of Veterans Affairs.
The intent of this section is to familiarize non-medical providers with common treatment modalities
by providing basic information that does not include data on efficacy.
Analgesic Medications
The following section is an introduction to analgesic, or pain relieving, medications. It is not meant to
guide prescription of medications but instead to help providers understand the likely uses of
medications taken by Veterans with chronic pain. A table of medications including both generic and
brand names is also included below.
Non-Opioid Analgesics. Aspirin and other related compounds constitute a class of drugs known
as nonsteroidal anti-inflammatory drugs (NSAIDS). This class of medication produces three
desirable effects including anti-inflammatory, analgesic, and antipyretic (fever reducing).
Commonly used medications in this category include aspirin, ibuprofen, naproxen, etodolac,
meloxicam, and piroxicam. The most common adverse effects of NSAIDs are gastrointestinal and
renal (kidney). Acetaminophen is also a non-opioid analgesic but is not an NSAID because, though
possessing pain relieving and antipyretic properties, it lacks an anti-inflammatory component.
Opioid Analgesics. Opioid analgesics (or narcotics) refer to compounds that act by binding to
opioid receptors in the brain. Though often used interchangeably, the term opiate refers only to
the naturally occurring resin found in opium poppy while opioids also include synthetically
produced substances and thus is the preferred general term.
This class of medications can either be short- or long-acting. Commonly used opioids include
morphine, hydrocodone, oxycodone, codeine, methadone, and hydromorphone. The analgesic
effects of opioids are due to decreased perception of pain, decreased reaction to pain, and
increased pain tolerance. The most commonly cited side effects of opioids (in order of frequency
reported) include nausea, constipation, drowsiness, dizziness, and vomiting (Eisenberg, McNicol,
& Carr, 2006). Opioids may be associated with risk of misuse (Comptom & Volkow, 2006) and
physiological dependence.
Measuring the risk to benefit ratio of opioid therapy for patients with chronic pain is complicated
and prescribing providers are encouraged to follow the 2010 VA/Department of Defense (DoD)
Clinical Practice Guideline for the Management of Opioid Therapy for Chronic Pain Of note,
concurrently prescribing opioids and sedatives/hypnotics (e.g., benzodiazepines) should be done
with extreme caution based on increasing evidence of risk of accidental overdose-related deaths
(Jones, Mack, & Paulozzi, 2013).

150
Tramadol. Tramadol does not fit neatly into a single category because it is dual acting. It
interferes with the transmission of pain signals like an opioid, but it also releases norepinephrine
and serotonin like an antidepressant. It is used for moderate to severe chronic pain and the most
common side effects are dizziness, sedation, constipation, nausea, and headaches. Because it is
not a pure opioid, risk of physiological dependence is lower but is still present.
Topical Analgesics. Topical analgesics are applied to the skin for delivery of medication to
targeted pain areas. They block the generation and transmission of nerve signals to the brain
through a local numbing effect. Topical products are available in various creams, gels, lotions,
patches, and plasters. Since they are applied to a localized area externally, topical agents afford a
lower risk for systemic adverse events and side effects. They are frequently used in the VA and
the most commonly prescribed topicals are capsaicin, lidocaine, diclofenac, and menthol-
methylsalycylate.
Muscle Relaxants. Muscle relaxants (or spasmolytics, antispasmodics) are most commonly
prescribed for LBP, neck pain, fibromyalgia, and tension headaches in situations where muscular
contractions appear to be a prominent component of pain.
Muscle relaxants used most commonly in VA include cyclobenzaprine, tizanidine, baclofen, and
methocarbamol. Muscle relaxants work by inhibiting the central nervous system, which
contributes to the commonly reported side effect of sedation and the recommendation against
driving or operating heavy machinery. Other common side effects include dizziness, headache,
nausea, irritability, and nervousness. Muscle relaxants also pose a risk of physiological
dependence.
Adjuvant Analgesics. Adjuvant analgesics, or co-analgesics, are medications that were originally
developed and marketed for uses other than analgesia and are also used in pain management.
The two most common classes of medications that fall into this category are certain types of
antidepressants and anticonvulsants. Antidepressants commonly used for analgesic purposes
include duloxetine, venlafaxine, and nortriptyline. Common side effects of antidepressants
include nausea, vomiting, insomnia, decreased sex drive, and constipation. Anticonvulsants,
primarily used to relieve neuropathic pain, include gabapentin, pregabalin, topiramate, and
lamotrigine. Common side effects of anticonvulsant medications include dizziness, fatigue, weight
gain, and drowsiness.
Headache Analgesics. Analgesics used to treat headaches vary widely and do not fall into a single
class. Migraine medications are generally categorized by nature of their action into those that are
preventative (e.g., propranolol, topiramate or Topamax), abortive (e.g., sumatriptan or Maxalt),
and rescue (butalbital/acetaminophen/caffeine or Fioricet). Of note, medication overuse
headaches, or rebound headaches, may occur when excessive analgesics are taken for headache
relief, leading to chronic daily headaches of a different type.
151
Examples of Common Analgesics, By Class
Opioid Analgesics
oxycodone
Oxycontin
oxycodone + acetaminophen
Percocet
oxymorphone
Opana
Opioid and Antidepressant
tramadol
Ultram
Muscle Relaxants
baclofen
cyclobenzaprine
Flexeril
methocarbamol
Robaxin
tizanidine
Zanaflex
Topical Analgesics
capsaicin cream/patch
diclofenac gel
Voltaren
lidocaine
gel/cream/ointment/
patch
Lidoderm
menthol-methylsalicylate cream
Adjuvant Analgesics:
Anticonvulsants
carbamazepine
Tegretol
gabapentin
Neurontin
pregablin
Lyrica
topiramate
Topamax
lamotrigine
Lamictal
Adjuvant Analgesics:
Antidepressants
amitriptyline
Elavil
duloxetine
Cymbalta
nortriptyline
Pamelor
venlafaxine
Effexor
Headache Analgesics
butalbital + acetaminophen + caffeine
Fioricet
rizatriptan
Maxalt
sumatriptan
Imitrex
zolmitriptan
Zomig
INVASIVE MEDICAL TREATMENT OPTIONS FOR CHRONIC PAIN
Epidural Steroid Injections. Epidural Steroid Injections (ESIs) are used for back pain complaints
associated with conditions such as spinal stenosis or spinal disc herniation. ESIs include a
combination of corticosteroids and local anesthesia that is injected into the epidural space around

152
the spinal cord and nerves. The injection may be guided by fluoroscopy or x-ray. The effects of the
injection last from one week to six months.
Nerve Blocks. Nerve blocks (aka, regional nerve blockade) are used for pain in the neck, back, feet or
even the head. Nerve blocks may include local anesthetic and epinephrine, with corticosteroids,
and/or opioids that are injected directly into the nerve group associated with reported pain. Nerve
blocks can be used to treat painful conditions, to determine sources of pain, or to judge the benefits
of more permanent treatments such as surgery.
Trigger Point Injections. Trigger point injections (TPI) are used to relieve muscles where knots form
when muscles do not relax. TPI is used in many muscle groups ranging from arms, legs, low back, and
neck and is most often associated with treatment of fibromyalgia and tension headache. The
injection contains a local anesthetic that may include a corticosteroid.
Facet Injections. Facet injections are used for those with chronic neck or back pain caused by
inflamed facet joints, which are located between each set of vertebrae in the spine from the neck to
the tailbone. A mixture of local anesthetic and corticosteroid medication is injected into the facet
joint to reduce swelling and inflammation around the facet joint space.
Radiofrequency Ablation. Radiofrequency ablation (RFA) is used to treat severe chronic low back
pain. Radiofrequency waves produce high heat on specifically identified nerves surrounding the facet
joints in the lumbar spine, ablating the nerves and destroying their ability to transmit pain signals.
RFA is an outpatient procedure using local anesthesia. While the procedure may provide pain relief,
in most patients the nerves regenerate.
OnabotulinnumtoxinA (Brand name: Botox). Botox injections are typically used for relief of frequent
migraine headaches. Botox received approval from the FDA as a treatment for chronic migraines in
2010.
Spinal Cord Stimulator. The most common use of spinal cord stimulators (SCS) is with patients
diagnosed with failed back syndrome (see definition under Surgery below). A SCS includes electrodes
implanted in the epidural space, an electrical pulse generator implanted in the lower abdominal area
of gluteal region, connecting wires to the generator, and a generator remote control.
Intrathecal Pump. An intrathecal pump is an implantable device that delivers pain medication
directly to the spinal fluid. Common medications used in pumps include baclofen or morphine. The
pumps deliver medications at higher dosages than possible with oral medications.
Surgery. Surgery may be offered for various pain locations such as back, neck, knee, shoulder, or
ankle. Surgery for chronic pain is usually considered only after conservative treatments have failed or
if seen as medically necessary. Individuals who have undergone one or more unsuccessful back
surgeries may receive the diagnosis or label of “failed back syndrome” or “failed back surgery

153
syndrome.” Causes for failure of surgery vary, but the results can lead to frustration and distrust of
medical providers, increased depression, and increased perceptions of disability (Onesti, 2004).
NON-INVASIVE TREATMENT OPTIONS FOR CHRONIC PAIN
Physical Therapy. Reduction in bodily movement that can be related to fear of pain or re-injury is
common in chronic pain and often leads to physical deconditioning and, subsequently, increased
pain. Physical therapy is an integral part of chronic pain interventions as it helps restore physical
functioning and re-engagement in rewarding life activities. Physical therapy involves a range of
activities including stretching exercises, strengthening exercises, and use of graded exercise
techniques such as therapeutic pools or stationary bikes, in addition to a range of palliative therapies
such as spinal manipulation and ultrasound, among others.
Cold/Heat. Application of cold and heat are often used for the management of chronic pain. Cold and
heat may decrease sensitivity to pain and provide competing sensory central nervous system input
that can reduce pain sensations.
Transcutaneous Electrical Nerve Stimulation (TENS). TENS units stimulate nerves by introducing a
mild electrical current. The electric current is not strong enough to cause muscle contraction, but
instead is thought to interfere with the transmission of pain signals to the brain. Electrodes are
placed on the skin and a battery-powered unit is carried or worn on the person. No surgical
procedures are involved in the use of a TENS unit.
Chiropractic. These interventions primarily focus on spinal adjustment or adjustment to other joint
areas. Spinal or other joint manipulations involve a dynamic thrust that causes an audible release and
attempts to increase range of motion.
Chiropractic care may also involve soft tissue therapy, strength training, dry needling, functional
electrical stimulation, traction, or nutritional recommendations.
Acupuncture. Acupuncture involves the insertion of needles into acupuncture points in the skin in an
effort to relieve pain. Acupuncture produces physiologic effects that are relevant to analgesia;
however, the mechanism for how acupuncture affects chronic pain remains unclear (Vickers, et al.,
2012).
Yoga/Tai Chi. Yoga and Tai Chi may provide a source of graded physical exercise combined with
relaxation to improve chronic pain.
Biofeedback. Biofeedback involves increasing awareness of physiological functions or processes such
as muscle tone, skin conduction, heart rate, or brainwaves. Awareness of different physiological
processes is gained through use of a variety of types of monitoring devices specific to the process
being monitored, such as an electromyography (EMG) to measure muscle activity or
electrodermograph to register skin conductance or resistance.

154
Information on a specific process is gathered, amplified, and displayed (fed back) to the patient who
then uses the visual or auditory feedback to gain control over the targeted behavior. Biofeedback has
been used to treat a variety of chronic pain disorders but is most often used in the management of
headaches.
Relaxation Training. Relaxation training, which may be done in the context of biofeedback, focuses
on identifying tension within the body and applying systematic techniques for decreasing that
tension. The most common techniques include diaphragmatic (or deep) breathing, progressive
muscle relaxation, and visualization.
SELECTED PSYCHOLOGICAL APPROACHES
Operant Behavioral Therapy. The operant-behavioral formulation of chronic pain by Fordyce (1976)
marked a significant development in the understanding and treatment of chronic pain by introducing
the concept of pain behaviors. These refer to forms of communication that are observable
expressions of pain and suffering such as moaning, clenching, grimacing, sighing, or limping. The
model suggests that reinforcement of such behaviors, often by those in one’s social environment,
could lead to maintenance of subjective reports of pain and increased self-perceptions of disability.
Cognitive Behavioral Therapy (CBT). CBT helps individuals resolve their problems concerning
maladaptive emotions, behaviors, and cognitions through a goal-oriented, systematic process. While
it was originally used for treatment of those with depression and anxiety disorders, it has been
implemented with a variety of other conditions from insomnia to substance abuse.
Acceptance and Commitment Therapy (ACT). Acceptance and Commitment Therapy, (ACT: Hayes et
al., 1999) is an acceptance- and mindfulness-based intervention that teaches patients to observe and
accept thoughts and feelings without judgment and without trying to change them. It focuses on
identifying core values and behaving in accordance with those values. As applied to chronic pain, ACT
emphasizes that while the physical sensation may be painful, the patient’s struggle with pain is what
causes suffering and emotional distress (Dahl & Lundgren, 2006). The aim of therapy, therefore, is to
develop greater psychological flexibility in the presence of thoughts, feelings, and behaviors
associated with pain.
Hypnotherapy. Hypnotherapy utilizes suggestive statements made by a therapist to alter the
patient’s attention and focus away from pain. Deep breathing is often used as a behavioral cue in an
effort to alter the subjective experience of pain. However, there is significant variation in specific
techniques.
Mindfulness. Mindfulness meditation is another approach combining elements of relaxation and
hypnotherapy, which seeks to increase focused attention and facilitate relaxation. Based in
Theravada Buddhism, it seeks to increase intentional self-regulation to what is occurring in the

155
present without attaching negative associations. As applied to pain management, a primary goal is to
separate the pain sensation from unhelpful thoughts.
APPENDIX 3 REFERENCES
Compton, W. M., & Volkow, N. D. (2006). Major increases in opioid analgesic abuse in the United
States: Concerns and strategies. Drug and Alcohol Dependence, 81(2), 103-107.
http://dx.doi.org/10.1016/j.drugalcdep.2005.05.009
Dahl, J. C., & Lundgren, T. L. (2006). Living beyond your pain: Using Acceptance and Commitment
Therapy to ease chronic pain. Oakland, CA: New Harbinger.
Eisenberg, E., McNicol, E., & Carr, D. B. (2006). Opioids for neuropathic pain. Cochrane Database of
Systematic Reviews, Issue 3. Art. No.: CD006146. doi:10.1002/14651858.CD006146
Fordyce, W. E. (1976). Behavioral methods for chronic pain and illness. St. Louis, MO: Mosby.
Hayes, S. C., Strosahl, K. D, & Wilson, K. G. (1999). Acceptance and commitment therapy: An
experiential approach to behavior change. New York, NY: Guilford Press.
Jones, C. M., Mack, K. A., & Paulozzi, L. J. (2013). Pharmaceutical overdose deaths, United States,
2010. Journal of the American Medical Association, 309(7), 657-659.
doi:10.1001/jama.2013.272
Onesti, S. T. (2004). Failed back syndrome. The Neurologist, 10(5), 259-264.
doi:10.1097/01.nrl.0000138733.09406.39
Vickers, A. J., Cronin, A. M., Maschino, A. C., Lewith, G., MacPherson, H., Foster, N.E., … & Linde, K.
(2012). Acupuncture for chronic pain: Individual patient data meta-analysis. Archives of Internal
Medicine, 172(19), 1444-1453. doi:10.1001/archinternmed.2012.3654
156
Appendix 4:
Mobile Apps for Pain and
Related Health Concerns

157
MOBILE APPS FOR PAIN AND RELATED CONCERNS
Below you will find several examples of mobile apps that can assist you with management of
important health topics, including chronic pain. They can be used with (or without) Brief
Cognitive Behavioral Therapy for Chronic Pain to help address wellness goals. All of the apps
below are available at the VA AppStore (https://mobile.va.gov/appstore) where there is a full
listing of additional free mobile apps:
Topic
App Image
Description
Pain
Management
Pain Coach is a mobile application for Veterans that
offers helpful tools to track and manage pain. You
can reference educational information about pain;
track your pain using a daily pain diary and a
monthly check-in; monitor your progress managing
your pain and see tables and graph of changes in
your pain level over time and; and use techniques
and tools to manage pain.
Self-care (Annie
App for Veterans)
Annie is a VA service that sends automated text
messages to Veterans to help them stay focused on
their self-care. This might include health related
notifications, reminders, or motivational messages.
Annie also empowers Veterans to play an active role
in their care, by prompting them to provide health
data such as weight or blood pressure. Anyone with
a phone that can send and received text messages
can use Annie.
Insomnia/Sleep
CBT-i Coach is for people who are engaged in
Cognitive Behavioral Therapy for Insomnia with a
health provider, or who have experienced
symptoms
of insomnia and would like to improve their sleep
habits.
Smoking/Tobacco
Cessation
Stay Quit Coach is intended to serve as a source of readily
available
support and information for adults who are
already in treatment to quit
smoking and to help them stay
quit after treatment ends.
158
Topic
App Image
Description
Weight
Management
MOVE! Coach provides self-managed weight management
allowing Veterans to monitor, track, and receive tailored
feedback regarding their progress with weight and exercise
goals while controlling relapse triggers and forming coping
plans.
PTSD
PTSD Coach is designed for Veterans and military Service
Members who have, or may have, Post-traumatic Stress
Disorder (PTSD). This app provides users with education
about PTSD, information about professional care, a self-
assessment for PTSD, opportunities to find support, and
tools that can help users manage the stressors of daily life.
PTSD
CPT Coach is for Veterans, Service members, and others
with PTSD who are participating in Cognitive Processing
Therapy (CPT) with a professional mental healthcare
provider. This app contains support materials for a
complete course.
PTSD
ACT Coach is designed for Veterans and military Service
Members in Acceptance and Commitment Therapy (ACT)
with a professional mental healthcare provider and
provides additional assistance with unpleasant thoughts,
feelings, and impulses without avoiding them or being
controlled by them.
Emotional
Distress
Mindfulness Coach is for people who may be experiencing
emotional distress, and for those wanting to maintain
healthy coping practices. The app can be used on its own
by those who would like mindfulness tools, or to enhance
face-to-face care with a healthcare professional. It is not
recommended for PTSD. Available for iOS only.
TBI
Concussion Coach is designed for Veterans, Service
Members, and other individuals who experience physical,
cognitive, and emotional symptoms that may be related to
mild to moderate traumatic brain injury. App provides a
self-assessment and information on managing TBI.
Available for iOS only.
159
Appendix 5:
Guided Imagery Script
160
GUIDED IMAGERY SCRIPT
This technique is designed to train the Veteran to create mental images that foster a relaxed
state. The Veteran should choose a location to mentally visit during the exercise; the only “rule”
is that the Veteran must pick a place that is peaceful and calm, with positive associations.
Encourage a focus on detailed images that take the Veteran away from stressful thoughts and
bodily tension.
The key to developing a deeply immersive experience where the Veteran completely engages in
the imagery exercise is to give full attention to all the specific details of the scene. It is crucial to
involve all five senses; to consider specifically what would be seen, heard, smelled, felt, and
tasted in this location. Provide examples such as smelling fresh-baked cookies in the air, feeling
warm sand in the hand, or hearing the crush of leaves underfoot.
Once the mental scene and the details of the patient’s relaxing place are gathered, guide
Veterans through the steps below. A sample for the therapist is presented below. Please refer
to the Guided Imagery Handout for a sample script of this exercise.
OVERVIEW OF STEPS FOR ANY GUIDED IMAGERY
1. Begin with comfortable posture and relaxed breath with eyes closed or gaze fixed.
2. Imagine the “entryway” into the location (e.g., path, door, staircase, lake dock).
3. Enter the relaxing place (focus on five senses).
4. Spend 5-10 minutes in the relaxing scene.
5. Have the Veteran “leave” the location through the same “entryway.”
SCRIPTING FOR INTRODUCING GUIDED IMAGERY TO THE PATIENT
“Guided imagery is designed to help us create mental images that promote a state of
relaxation. Essentially, guided imagery involves creating a detailed, imaginal location to
mentally visit and attune your thoughts and senses to. For some people, this might involve
things like smelling fresh-baked cookies, listening to birdsongs, or imagining the sensation of
walking through warm sand. But no two people will create the same mental scene. The image
or images that you select are up to you; the only rule is that you must create a calm and
peaceful scene.”
161
GUIDED IMAGERY EXERCISE
1. Imagine yourself walking slowly down a path toward your special place. This path can be
inside or outside. The path is comforting and peaceful. As you walk down this path,
imagine all of your stresses, worries, and tension are leaving you. Enjoy this journey to
your special place.
2. As you walk down this path, notice the ground beneath you…how it feels as you walk.
Notice the sounds…the comfortable temperature of the air. Take a breath in, feeling all
your tension leave you as you exhale. Notice any fragrance that may be here. Notice the
view around you. Reach out and touch something around you. Feel its textures.
3. You feel calm and safe. All your worries and anxieties being left behind as you move
toward your special place… (PAUSE 30 sec).
4. Walk down this path until you arrive at your own special place…and when you have
reached this special place, go ahead and enter… (PAUSE 10 sec).
5. You have arrived at this relaxing and peaceful place. Notice the ground underneath
you… whether it is hard or soft. Notice how the ground feels below your feet. Listen to
the sounds in this place, both close and distant. Smell the air, the fragrances. Notice the
temperature of the air around you.
6. Look above you… Notice the colors and sights above you. Look out into the distance… as
far as you can see… Take in all of the sights, fragrances, and sounds around you.
7. Reach out and touch something in this place… Notice its texture and how it feels against
your skin. Notice the different objects around you… their shapes, textures, and colors.
Notice the light and shade of this place and how it reflects off of these objects.
8. There is a comfortable place for you to sit or lie here as you take in all the smells,
sounds, sights, and textures… As you sit or lie in this place, away from it all, you feel
calm and secure, refreshed and renewed, strong and at peace. As you enjoy this place
for a few minutes, you know that you can come here whenever you please, and that this
place will always be waiting for you… (PAUSE 3-5 min).
9. Now it's time to come back… leave by the same way you came, enjoying the path… and
as you return on this path, you start to also notice the room in which you are sitting…
start to wiggle your fingers and toes… and when you are ready, slowly open your eyes
and stretch your muscles.
162
United States Department of Veterans Affairs
