
INSPIRE Study
Cognitive
Behavioral Therapy
for Chronic Pain
(CBT-CP) Group
Program
Session Handouts and Worksheets
1
Table of Contents
Group Session 1. Introduction to Group, CBT-CP, and Diaphragmatic Breathing ........................................ 2
Group Session 2. Relaxation Techniques and Behavioral Activation/Pleasant Activity Scheduling ............. 7
Group Session 3. Self-Care and Wellbeing: Sleep Hygiene and Exercise .................................................... 13
Group Session 4. Automatic Thoughts, Cognitive Errors, and Pain ............................................................ 19
Group Session 5. Cognitive Re-Structuring and Cognitive Distancing (Distraction) ................................... 24
Group Session 6. Stress Management and Time-Based Pacing .................................................................. 28
Group Session 7. How To Work with Painful Emotions (e.g., Anger, Frustration) ..................................... 29
Group Session 8. Review and Trouble-shooting ......................................................................................... 34
Note:
The CBT-CP participant packet used in the INSPIRE study included materials reprinted from various
sources. We are not able to reproduce these materials here for public distribution. However, we have
cited the original source materials and provided links when available.
Group Session 1. Introduction to Group, CBT-CP, and
Diaphragmatic Breathing
• Class Guidelines
• Diagram of Biopsychosocial Model
• Homework Practice with Diaphragmatic Breathing
• Pain and Distress Cycle

INSPIRE
CBT Group Session 1
3
CBT for Chronic Pain Class Guidelines
1. Group discussions are confidential: What is said in group, stays in group!
2. We encourage you to practice ways to feel your best so you can participate actively.
a. Class time offers an opportunity to experiment with your experience.
b. We endorse creativity that increases your comfort (e.g., pillows, laying down, sitting,
comfortable posture).
3. This is a CBT skills class.
a. Group members are encouraged to practice skills and discuss their practice each week.
b. We take a proactive and focused approach (this is not a space for venting).
c. We emphasize self‐accountability.
d. You will be encouraged to set goals and monitor your progress.
e. We will teach and reinforce skills to help you work towards your goals and values.
4. We encourage fostering a safe, respectful environment for one another.
a. We encourage you to attend and participate. Experiment and see what happens.
b. Please arrive on time to group, and call if you are going to be late or miss a session.
c. Please silence all cell phones while in group.
d. Please be respectful of each other’s opinion and space.
5. We foster a positive, compassionate class environment.
a. “We are all doing the best we can.”
b. Nonjudgmental stance towards self and others.
c. Compassion vs. Caretaking.
6. For telehealth groups, we ask that you (in addition to items 1-5 above):
a. Please turn on your video (webcam). Being able to see one another helps us all get the
most out of group.
b. Attend group in a space free of distractions, where you can be alone and speak freely.
c. Attend group in a room where a nonmember (e.g. family member, roommate, etc.)
cannot see or hear the group.
d. Do not record the meeting or take screenshots of other group members.
e. Mute your audio when you are not speaking. This helps reduce extra noise so we can all
hear each other.
f. For safety reasons, please do not drive during the group session.
Others:
INSPIRE
CBT Group Session 1
5
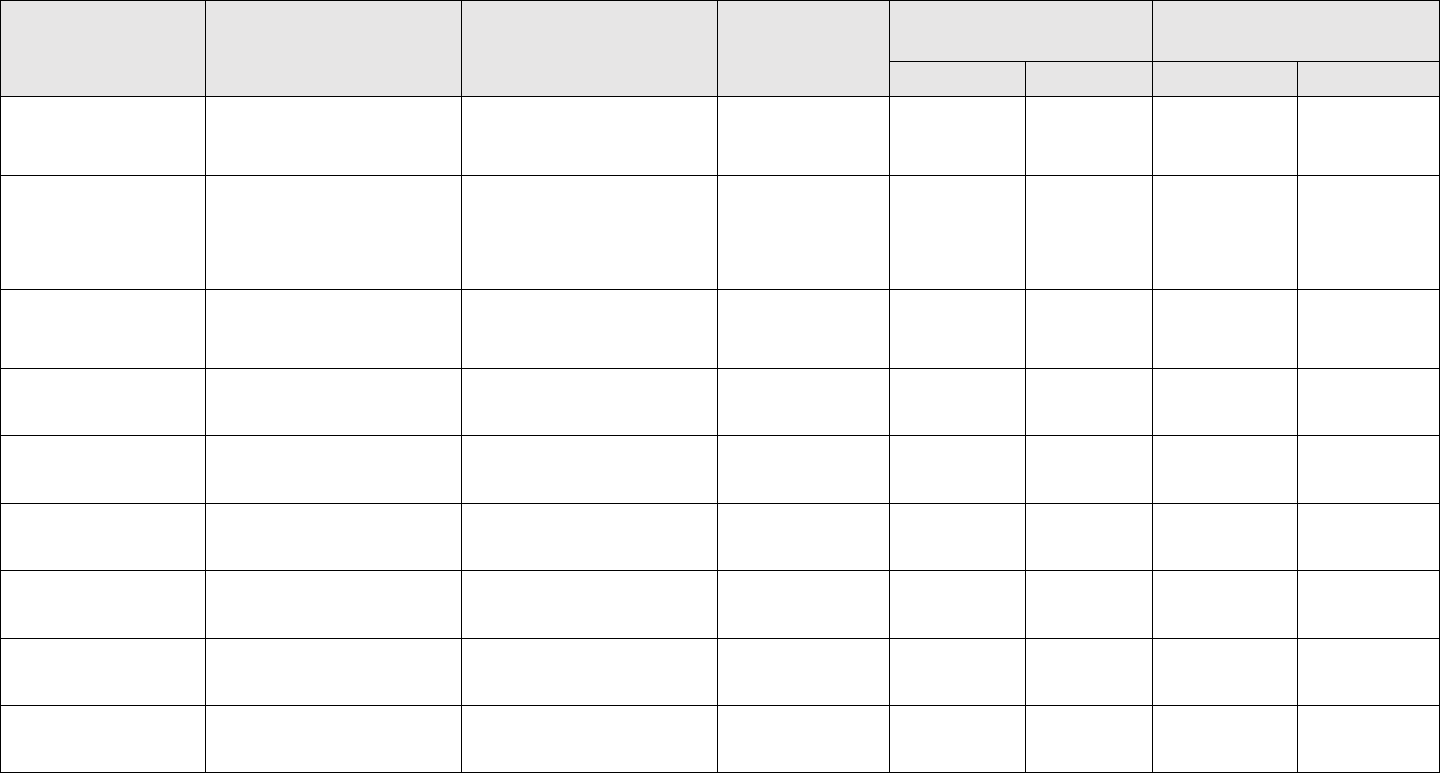
Homework Practice with Diaphragmatic Breathing
Record your experience with diaphragmatic breathing practice. The goal is to practice at least one time each day and to notice its effects. The examples below
illustrate some ways you might record your experience on this worksheet. Do what seems most helpful to you.
Date or day/time
Situation
Plan/Practice
Length of
Practice?
Level of tension (0‐
10)
Level of Pain (0‐
10)
Before
After
Before
After
7/25/18
Noticed I was holding
breath at computer
Practiced in a
breakout room
10 breaths
7
3
7
4
Wed morning
While waiting in line
at grocery and feeling
anxious
Practiced in grocery
line
3 mins
10+
6
8+
<6
Wed midday
Pain was rising
Practiced in a recliner
10 mins
Medium
Low
High
OK!

INSPIRE
CBT Group Session 1
6
Pain and Distress Cycle
Chronic Pain
Decreased activity
& Deconditioning
Distress &
Disability
Negative
Emotions
Avoidance &
Withdrawal
Group Session 2. Relaxation Techniques and Behavioral
Activation/Pleasant Activity Scheduling
• CDC Guideline for Prescribing Opioids for Chronic Pain
• Gate Control Theory of Pain
• Positive Activities for Behavioral Activation
• The Brain and Pain

INSPIRE
CBT Group Session 2
8
CDC Guideline for Prescribing Opioids for Chronic Pain
Information handout reprinted from the Centers for Disease Control and Prevention.
*
Available from:
https://www.cdc.gov/drugoverdose/pdf/infographic-
cdc_guideline_for_prescribing_opioids_for_chronic_pain-a.pdf
LEARN
*
Reference to materials on the CDC website does not constitute its endorsement or recommendation by the U.S.
Government, Department of Health and Human Services, or Centers for Disease Control and Prevention.

INSPIRE
CBT Group Session 2
9
Gate Control Theory of Pain
Ronald Melzack and Patrick Wall introduced a scientific theory to explain variation in people’s
experience of pain.
*
They identified a "neural gate," at the base of the cervical spinal column that
affects how pain signals are transmitted and interpreted by the brain in any given moment. When the
gate is wide open, pain feels more intense. When the gate closes, pain signals are blocked or muted.
Their research has provided important ways to understand and change people’s experience with chronic
pain.
Most people report that their “gate” closes (pain becomes less bothersome) when they are engaged in
something engrossing. It is also common for the “gate” to open in times of stress, when the focus is on
pain and worries, and when there’s nothing else demanding attention or providing distraction.
What opens the gate?
Stress and Tension – A particularly stressful or frustrating situation can make the pain feel worse.
Anxiety and anger often lead to tension in the body, which opens the pain gate.
Mental Factors – Focusing on pain can have the effect of magnifying it. When the brain is not otherwise
engaged, the pain gate opens. Feelings of emotional distress—anxiety, worry, dread, anger, frustration,
irritation—can also intensity pain.
Lack of activity – Inactivity can also open the pain gate and make it harder to become active.
What closes the gate?
Relaxation and Acceptance – General feelings of relaxation and acceptance of the current moment can
help close the gate.
Mental Factors – Focusing on something meaningful and feelings of gratitude, kindness, closeness,
connection, and love can all help close the gate.
Activity – Engaging in activities that are stimulating can occupy the mind and distract from pain, thus
closing the gate.
*
Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971-9.

INSPIRE
CBT Group Session 2
10
Positive Activities for Behavioral Activation
Those who suffer from chronic pain may begin to decrease their functioning in order to cope, such as
avoiding activities they fear will further pain or injury. This leads to decreased activity and physical
deconditioning. This often leads to negative thoughts about pain and oneself and diminishes
participation in pleasurable activities.
Behavioral activation is a strategy to help people to engage in things that are enjoyable, even when they
do not feel like it. The goal is to engage in something each day that you find enjoyable, engaging, or that
provide a sense of accomplishment.
Step 1: Begin by listing activities that you enjoy and find valuable:
Examples:
Gardening, yoga, seeing live music, playing board games, reading, folding laundry
At home:
With others:
Work or housework related:
For fun and creativity:
Outdoors and/or physical:
Before bed:

INSPIRE
CBT Group Session 2
11
Now you will log what you did each day and what you noticed before and after completing the activity, such as reduction in distress or an increase in vitality.
Step 2: Use the list on the front page to incorporate into your weekly activities:
Day / time
Activity
Duration
What did you notice?
Before
After
Sunday,
evening
Saw live music with friends
3 hours
Felt tense, hurting, and didn’t feel
like going
Was surprised how much fun it was!
INSPIRE
CBT Group Session 2
12
The Brain and Pain
Information handout reprinted from Cognitive Therapy for Chronic Pain: A Step-by-Step Guide, Second
Edition, by Beverly E. Thorn. New York, NY: The Guilford Press; 2017.
Group Session 3. Self-Care and Wellbeing: Sleep Hygiene and
Exercise
• Prescription Opioids: What You Need to Know
• Promoting Safer and More Effective Pain Management
• Improving Sleep through Behavior Change
• Sleep Log

INSPIRE
CBT Group Session 3
14
Prescription Opioids: What You Need to Know
Information handout reprinted from the Centers for Disease Control and Prevention (CDC) and the
American Hospital Association.
*
Available from: https://www.cdc.gov/drugoverdose/pdf/AHA-Patient-
Opioid-Factsheet-a.pdf
*
Reference to materials on the CDC website does not constitute its endorsement or recommendation by the U.S.
Government, Department of Health and Human Services, or Centers for Disease Control and Prevention.

INSPIRE
CBT Group Session 3
15
Promoting Safer and More Effective Pain Management
Information handout reprinted from the Centers for Disease Control and Prevention (CDC).
*
Available
from: https://www.cdc.gov/drugoverdose/pdf/guidelines_factsheet-patients-a.pdf
*
Reference to materials on the CDC website does not constitute its endorsement or recommendation by the U.S.
Government, Department of Health and Human Services, or Centers for Disease Control and Prevention.
INSPIRE
CBT Group Session 3
16
Improving Sleep through Behavior Change
Stimulus Control Procedures
1. Go to bed only when you are sleepy. The longer you are in bed, the more bed is
associated with a place to be awake instead of being asleep. Delay bedtime until
sleepy.
2. Get out of bed when you can't fall asleep or go back to sleep in about 15 minutes. Get
out of bed if you don't fall asleep fairly soon. Return to bed only when you are sleepy.
When you feel sleepy, return to bed. The goal is to reconnect your bed with being
asleep.
3. Use the bed for sleep and sex only. Do not watch tv, listen to the radio, eat, or read in
your bed or bedroom.
Sleep Hygiene Guidelines
1. Caffeine - Avoid caffeine 6 to 8 hours before bedtime.
2. Nicotine - Avoid tobacco near bedtime and during the night.
3. Alcohol - Avoid alcohol after dinner. Alcohol often promotes the onset of sleep but
interrupts the natural sleep pattern. Do not consume alcohol within 4 hours of going to
bed.
4. Sleeping Pills - Sleep medications are effective only temporarily. Sleep medications lose
their effectiveness after about 2-4 weeks of regular use.
5. Regular Exercise - Do not exercise within 2 hours of bedtime. It may elevate nervous
system activity and interfere with your ability o fall asleep.
6. Bedroom Environment - Your bedroom should have a moderate temperature and be
quiet and dark. Noises can be masked with background white noise (eg, fan) or with
earplugs. Bedrooms may be darkened with blackout shades or sleep masks may be
worn.
7. Eating - A light bedroom snack, such a s a glass of milk, cheese, or a bowl of cereal can
promote sleep. Avoid snacks in the middle of the night because awakening may
become associated with hunger.
8. Avoid Naps - The sleep you obtain during the day takes away from the amount of sleep
you need that night. If you must nap, schedule it before 3pm and do not sleep more
than 15 to 30 minutes.
INSPIRE
CBT Group Session 3
17
9. Allow yourself at least an hour before bedtime to unwind - Find what works for you to
wind down, and perhaps give yourself an hour to do so.
10. Regular Sleep Schedule - Keep a regular time each day, 7 days a week, to get out of
bed. Keeping a regular waking time helps set your circadian rhythm so that your body
leans to sleep at the desired time.
11. Set a Reasonable Bedtime and Arising Time and Stick to Them - Set the alarm clock and
get out of bed at the same time each morning, weekdays, and weekends, regardless of
the bedtime or the amount of sleep you obtained the previous night. The guideline is
designed to regulate your internal biological clock and reset your sleep-wake rhythm.

INSPIRE
CBT Group Session 3
18
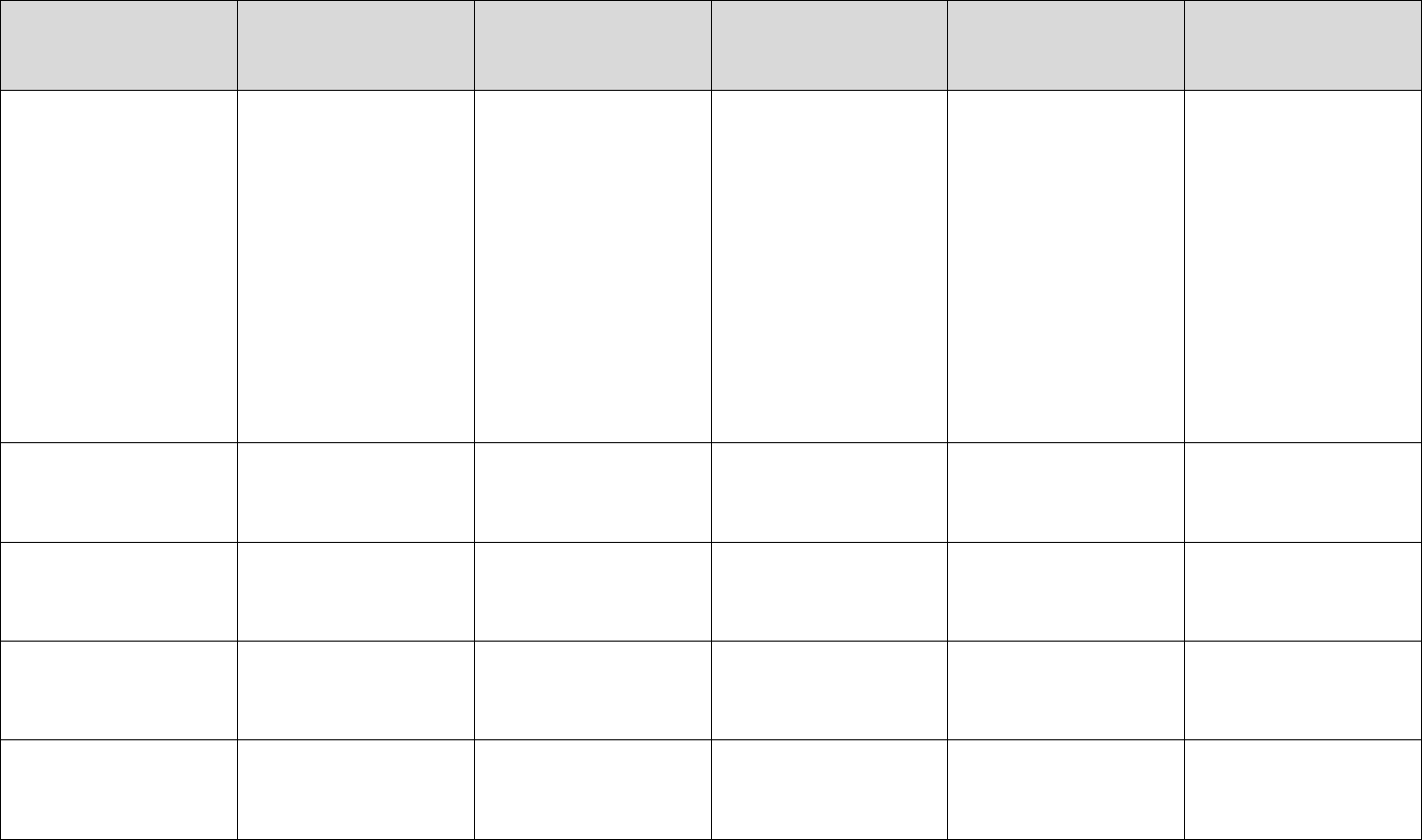
Sleep Log
Complete in the morning:
Sunday
Monday
Tuesday
Wednesday
Thursday
Friday
Saturday
Time you went to bed
How did you unwind before bed? (e.g., light
reading, breath work, meditation)
Time you woke up
Total hours of sleep
How many times you woke up
Complete in the evening:
Number of caffeinated drinks
Time of last caffeinated drink
Time of last meal
Minutes of exercise during the day
Rate your pain (0=no pain, 10=great pain)
Observations/Comments:
Group Session 4. Automatic Thoughts, Cognitive Errors, and
Pain
• ABC Model
• The Feeling Wheel
• Thought Record
• Unhelpful Thinking Styles

INSPIRE
CBT Group Session 4
22
Thought Record
Activating Event
Beliefs
(Automatic Thought)
Consequences (Emotions
and Behavior)
Balanced Thought
Bodily Sensations
Someone invited me on a
walk
I can’t do this, I can’t
do anything
I feel despondent and
hopeless, and I retreat
I appreciate that
someone invited me, and
I have options about how
I respond, I could pace
myself and take a short
walk and see how it goes
or invite them to do
something else
Sweaty palms, tension in
muscles
Group Session 5. Cognitive Re-Structuring and Cognitive
Distancing (Distraction)
• ABC Model
• Coping Statements
• Thought Record
INSPIRE
CBT Group Session 5
26
Coping Statements
Coping statements can help decrease anxiety, depression, and negative self‐judgment. When we’re
especially upset or activated it’s easy to get caught up in negative, self‐defeating thoughts. One way to
reduce their power is to come up with healthier alternatives that are true for you. Come up with a list of
coping statements that feel reasonable and believable to you. Even when coping statements feel
awkward at first, try to repeat them often. The more that you practice saying coping statements to
yourself, the easier it will become to replace negative thought habits or “loops.” It takes time and
practice to create new habits. The good news is that the human brain is quite plastic, so we can actually
re‐condition ourselves and create new neural pathways.
Use this list to get started. Choose a handful that resonate with you or write alternatives that work
better. You may want to carry a list of your top 5‐10 coping statements in your wallet, planner, or phone
so they are always handy.
“This situation is temporary, this too shall pass.”
“I’ve survived painful experiences before, I will survive this too.”
“Just for this moment this is how it is, but this moment will pass, as all moments do.”
“I can be uncomfortable, and still make it through this situation.”
“It’s okay. I can do this.”
“All I have to manage is this very moment.”
“I can choose how I want to show up in this moment.”
“This is a moment. Let me relax into it and breath.”
“I am strong enough to handle what is happening to me right now.”
“My thoughts do not control my life.”
“I am the master of my own life, and I can chose my responses and tolerate my feelings.”
“I accept all my feelings and sensations as part of myself in this moment.”
“Even though the pain is high, I am not in danger right now, I am safe.”
“This situation sucks, but it is only temporary.”
“So what?! Seriously, so what if_____??”
“God/Spirit/The Universe always takes care of me; somehow I am always taken care of.”
“If I am alive, I have been taken care of and protected by someone or something.”
“Everything is working out exactly as it should, for the good of all concerned, even if I can’t see it right
now.”
INSPIRE
CBT Group Session 5
27
Thought Record
Activating Event
Beliefs
(Automatic Thought)
Consequences
(Emotions and
Behavior)
Dispute/
Challenge Beliefs
Balanced Thought
Effective New Beliefs
Bodily Sensation
Someone invited me
on a walk
I can’t do this, I
can’t do anything
I feel despondent
and hopeless, and I
retreat
It’s not true that I
can’t do anything, I
can do some things
I appreciate that
someone invited me,
and I have options
about how I
respond, I could pace
myself and take a
short walk and see
how it goes or invite
them to do
something else
Sweaty palms, tight
muscles
Group Session 6. Stress Management and Time-Based Pacing
No additional handouts or worksheets this session.
Group Session 7. How To Work with Painful Emotions (e.g.,
Anger, Frustration)
• Anger Management Skills
• Anger Warning Signs
• Worksheet: Dealing with Painful Emotions
• Stress-Judging-Pain Worksheet

INSPIRE
CBT Group Session 7
32
Worksheet: Dealing with Painful Emotions
Situation
Emotion
Thoughts and Urges
Coping Response
(Self‐Talk, Relaxation, Action)
Observation/Outcome
My partner said
something that felt
unkind
Anger, hurt
Feel like snapping or
yelling
I paused, breathed deeply,
took a step back
I was able to reduce emotional reaction
and return to talk later about it
INSPIRE
CBT Group Session 7
33
Stress-Judging-Pain Worksheet
Information handout reprinted from Cognitive Therapy for Chronic Pain: A Step-by-Step Guide, Second
Edition, by Beverly E. Thorn. New York, NY: The Guilford Press; 2017.
Group Session 8. Review and Trouble-shooting
• Applying Your Pain Coping Skills: Problem Solving
• Dealing with a Setback
• Goal Setting and Moving Forward
INSPIRE
CBT Group Session 8
35
Applying Your Pain Coping Skills: Problem Solving
Your pain coping skills menu now includes several different skills:
Pain Coping Skills Menu
❖ Relaxation
o Diaphragmatic breathing
o Progressive muscle relaxation training
o Imagery
❖ Increasing engagement
o Distraction methods
o Activity-rest cycle (pacing)
o Pleasant activity scheduling
o Getting active (behavioral activation)
❖ Working with thoughts
o Changing self-talk
o Letting go of thoughts
o Challenging (negative) thoughts
o Calming self-statements
❖ Improving self-care
o Sleep practices
o Activity-rest cycle
o Getting active
o Stress-management toolkit
❖ Working with painful emotions
o Managing anger
o Reducing distress
o Identifying/communicating feelings
❖ Increasing positive emotions
o Getting active
o Pleasant activities
o Gratitude exercises
o Calming self-statements
As you practice with these skills you will notice many positive benefits. Sometimes bringing in one skill –
such as relaxing with diaphragmatic breathing – is enough to make a significant difference. Other times,
you may need a combination of skills. When stress levels are high, it is more difficult to think of the skills
you need. Use the following steps while you are feeling calm and relaxed as a way to be ready with skills
to use in more challenging situations.
Step 1: Describe the situation
Step 2: Think of difficulties you are likely to have in the situation
Step 3: Think of coping skills you will be able to apply that would be helpful

INSPIRE
CBT Group Session 8
36
Dealing With a Setback
Sometimes coping with a stressful situation will lead to a setback in your coping efforts. In a
setback, you might be overwhelmed by self‐defeating thoughts and feelings and stop applying
your coping skills.
Below are four steps for coping with a setback. If you apply these steps, you can ensure that the
setback is a minor one in which there is only a temporary lapse in coping efforts.
Step 1
Stop, look, listen. Your reaction to this situation can be viewed as a warning sign that
you are in danger. Find a quiet place where you can stop, rest, and review the situation
and how you might react to it.
Step 2
Keep calm. The usual reaction to a setback is to become upset and begin thinking in a
negative and distorted fashion. This emotional reaction is normal. Give yourself time to
relax and let the feelings pass. The problems you are having coping do not mean that
you are a failure or that your coping efforts are useless. Try to look at the problems as
an independent event, perhaps something that might be able to be avoided in the
future.
Step 3
Review the situation leading up to the setback in coping. Review the events leading up
to the setback. Were there any warning signals or other factors that might be
important (time of day, activities you were doing, mood)? Are there different ways that
you might have coped with the events that might have helped?
Step 4
Make an immediate plan for coping. If you can remove yourself from the stressful
situation, do so. If this is not possible, use imagery or other methods to try to distance
yourself from the problems you are confronting. Try to do something pleasant for
yourself. Use your skills in cognitive restructuring to deal with overly negative thoughts.
Ask your friends and family members to help by providing suggestions for ways of
coping or alternative activities. Call a friend and seek support.
INSPIRE
CBT Group Session 8
37
Goal Setting and Moving Forward
Take this opportunity to reflect on goals that you set earlier. What have you been able to accomplish?
How may your goals changes? Consider what you’d like to focus on currently. Remember to break your
goals into small enough pieces that you can accomplish within a week or so. You can use the action
plan below to help with this process.
Setting a Goal:
1. Identify something you want to do.
2. Is this a reasonable goal? Can you expect to accomplish it? Is it a short‐term or a long‐term
goal? Take a moment to consider if you need to modify your answer above.
Developing an Action Plan to Accomplish Your Goal:
1. Consider the following questions:
a. What would it look like if you had accomplished your goal? (i.e., how would you or how
would someone else know you had met your goal?)
b. What would be different about you and about your life?
c. How long will it take you to complete your goal?
2. Using the information above, answer the following questions to help you to state your goal in
terms of specific and observable behaviors:
a. How much?
b. When?
c. How long?
d. How often?
3. What steps do you need to take to accomplish your overall goal?
4. Rate your confidence level in your ability to complete the entire action plan (0‐10).

INSPIRE
CBT Group Session 8
38
Personal Plan for Maintaining Progress
Part 1:
Circle the 3 or 4 coping skills that helped you
the most, and that you are planning to
emphasize the most in your home practice.
Part 2:
Circle the coping skills you have found somewhat
helpful but need more practice with.
1. Diaphragmatic breathing
2. Progressive muscle relaxation training
3. Imagery
4. Distraction
5. Activity-rest cycle
6. Pleasant activity scheduling
7. Getting active (behavioral activation)
8. Changing self-talk
9. Letting go of thoughts
10. Calming self-statements
11. Sleep practices
12. Managing painful emotions
1. Diaphragmatic breathing
2. Progressive muscle relaxation training
3. Imagery
4. Distraction
5. Activity-rest cycle
6. Pleasant activity scheduling
7. Getting active (behavioral activation)
8. Changing self-talk
9. Letting go of thoughts
10. Calming self-statements
11. Sleep practices
12. Managing painful emotions
Part 3: In the space provided below, write down some goals that you are likely to achieve in the next six
months if you continue to practice your pain coping skills.
1.
2.
3.
4.
5.







