
ASPR
ADMINISTRATION FOR STRATEGIC
PREPAREDNESS AND RESPONSE
March 25, 2024
To the healthcare provider community:
As many of you have experienced, the impacts of the cyberattack against Change Healthcare have
continued to disrupt provider billing and claims operations. At the U.S. Department of Health and
Human Services (HHS), the Administration for Strategic Preparedness and Response (ASPR), and
the Centers for Medicare & Medicaid Services (CMS), we have heard concerns from so many
providers - from pediatricians and ophthalmologists to infusion centers, home- and community-
based services providers, and community health centers - about cash flow disruptions in the
aftermath of the Change Healthcare cyberattack.
The Biden-Harris Administration is leading with solutions, providing flexibility for state Medicaid
programs to provide interim payments to fee-for-service providers, making advance and accelerated
payments available to providers and hospitals through Medicare, and urging health plans to do the
same. We continue to press UnitedHealth Group and private healthcare plans to follow our lead.
We also continue to hear from providers that you have sometimes had difficulty getting answers
from healthcare plans about the availability of prospective payments or the flexibilities you may
need while the Change Healthcare platform is unavailable. HHS asked health plans to provide
specific national contact information that providers can use when they need this information, and
we are providing that information to you enclosed with this letter. Please share this resource with
providers who need it. However, if you have a regional point of contact for your health plan, we'd
suggest you reach out to them first. If you reach out to these contacts and do not receive a response,
please contact us at HHScyber@hhs.gov.
We also encourage you to review and implement HHS's voluntary Healthcare and Public Health
Cybersecurity Performance Goals (https://hphcyber.hhs.gov/performance-goals.html), which are
designed to help healthcare organizations strengthen cyber preparedness, improve cyber resiliency,
and ultimately protect patient health information and safety.
We appreciate your resilience and your continued commitment to your patients during the last
month. And thank you for remaining engaged with us to make sure we know about the challenges you
have faced in light of the Change Healthcare cyberattack. It has been helpful for us to hear
directly from you to understand the scope of those challenges and to know how to tailor our
response to your needs. We will continue to value your feedback as we move forward together.
Andrea Palm
Deputy Secretary
Dawn O'Connell
Administrator and Assistant Secretary, ASPR
¾fl;_";!
Chiquita Brooks-LaSure
Administrator, CMS
Enclosure

Resources for
Providers in
Response to the
Change Healthcare
Cyberattack
March 25, 2024

1
Introduction
As you know, Change Healthcare was subject to a cyberattack in late February – and it has had a
significant impact on health care operations across the country. Payments to hospitals, physicians,
pharmacists, and other health care providers across the country were disrupted. Change Healthcare,
which is owned by UnitedHealth Group (UHG), processes 15 billion health care transactions annually
and is involved in one in every three patient records.
In order to help providers manage the impact of this attack, the U.S. Department of Health and Human
Services (HHS) has compiled information, resources, and tools from health plans and payers for
providers in need of assistance. In this document, providers will find information to help them connect
with payers regarding impacts of the cyberattack, links to resources payers have set up (including
guides to connect to alternate data clearinghouse services), information on advanced payments, and
more.
If you have questions for HHS regarding the Change Healthcare cyberattack, please reach out to
HHScyber@hhs.gov.

2
TABLE OF CONTENTS
United Health Group ........................................................................................................ 3
AmeriHealth Caritas ........................................................................................................ 4
Blue Cross Blue Shield ..................................................................................................... 7
Centene Corporation ...................................................................................................... 19
Cigna Healthcare ............................................................................................................ 22
CVS Health ..................................................................................................................... 25
Elevance Health .............................................................................................................. 26
Humana ........................................................................................................................... 27
Kaiser Permanente ......................................................................................................... 28
Molina Healthcare .......................................................................................................... 29
Payer Contact Information ............................................................................................ 30

3
United Health Group
UnitedHealth Group has advanced more than $2 billion thus far through multiple temporary funding
initiatives. We recognize the event has caused different levels of impact among providers; therefore, we
continue to offer temporary funding assistance at no cost. We know many providers, especially smaller
practices, are struggling, and we encourage those who need further assistance to access these resources.
Since this effort launched more than two weeks ago, we have launched funding assistance programs
designed for care providers to access funding help at no cost. These programs are available to:
• Providers who receive payments from payers processed by Change Healthcare.
• UnitedHealthcare medical, dental and vision providers.
• Providers who have exhausted all available connection options — or are in the process
of implementing workaround solutions — and work with other payers who have opted
not to advance funds while the Change systems are down.
• If you are a provider and are not seeing the amounts to cover your weekly shortfall, please contact
us and we can help you. Please submit a request through the temporary funding assistance inquiry
form
UnitedHealth Group’s funding website allows for providers to first determine their eligibility, even
without an Optum Pay account. To accept funds, an Optum Pay account is required.
Providers have 45 business days to return funds. Change Healthcare will send notice to recipients that
the funding amount is due after claims processing or payment processing services have resumed and
payments impacted during the service disruption period are processed. For all providers receiving
funding support, there are no fees. No interest. No additional or associated costs.
All the necessary resources are in place to support funding assistance through the eventual system
recovery and normalization of claims flow. For additional help, see “Inquiries About Funding Support”
under the Additional Resources section on the right.
Contact Information
If providers have questions, they can go to our website www.optum.com/temporaryfunding For
assistance, please contact 1-877-702-3253. Or contact your United or Optum relationship manager.

4
AmeriHealth Caritas
AmeriHealth Caritas has been in communication with our state and federal regulators and is
going to extend claims timely filing requirements for all lines of business in accordance with the
guidance recently released by HHS and any applicable regulatory direction.
For providers seeking advance payments, the company is evaluating the requests on a case-by-
case basis. We centrally track all requests to ensure that they are quickly reviewed and processed.
Below are the links to the provider section of our plan-specific websites that include the latest
information for our providers.
Medicaid
1. AmeriHealth Caritas Delaware
2. AmeriHealth Caritas District of Columbia
3. AmeriHealth Caritas Florida
4. AmeriHealth Caritas
5. AmeriHealth New Hampshire
6. AmeriHealth Caritas North Carolina
7. AmeriHealth Caritas Ohio
8. AmeriHealth Caritas Pennsylvania
9. AmeriHealth Caritas Pennsylvania Community HealthChoices
10. Blue Cross Complete of Michigan
11. Keystone First
12. Keystone First Community HealthChoices
13. Select Health of South Carolina
14. AmeriHealth Caritas Louisiana
Medicare
1. AmeriHealth Caritas VIP Care Delaware
2. AmeriHealth Caritas VIP Care Florida
3. AmeriHealth Caritas VIP Care Pennsylvania
4. First Choice VIP Care
5. Keystone First VIP Choice
6. AmeriHealth Caritas VIP Care Plus
7. First Choice VIP Care Plus
Exchange
1. AmeriHealth Caritas Next–Delaware
2. AmeriHealth Caritas Next– Florida
3. AmeriHealth Caritas Next –North Carolina
4. First Choice Next
Behavioral Health
1. PerformCare (PA)

5
Change Healthcare System Interruption
Change Healthcare, our electronic data interchange (EDI) clearinghouse for claims and payment
cycle management, continues to address their network interruption related to a security incident.
Below are updates for our systems and processes:
1. Claims payments: We have resumed payments for claims submitted prior to the
incident. Since Change Healthcare is still unable to accept claims submissions,
providers who submitted claims during the outage may be able to resubmit them
either through additional solutions identified below through Availity and PCH Global,
or once Change Healthcare’s connectivity is restored, through Change Healthcare.
We appreciate the inconvenience this is causing.
2. Electronic claims submission: We have established a connection with Availity to
receive electronic claims. If you or your clearinghouse do not currently use Availity
to submit claims, you may register at: https://www.availity.com/Essentials-Portal-
Registration. You will find registration options for Healthcare and Atypical
Provider, so please choose the one that aligns with your business. For registration
process assistance and other resources, access the training site link on the Availity
registration page.
3. Manual claims submission: We have established a direct claims entry process
through PCH Global. To submit claims directly, please go to https://pchhealth.global
and click the Sign-Up link in the upper right-hand corner to register. Complete the
registration process and log into your account. You will be asked how you heard
about PCH Global; select Payer, then AmeriHealth. Access your profile by clicking
on Manage User and then My Profile. You will need to complete all the profile
information. When you go to the Subscription Details screen, select the More option
on the right-hand side to see how to enter the promo code Exela-EDI.
For a detailed walk through of the registration process, refer to the PCH Global
Registration manual (PDF), found on the PCH Global website in the Resource Menu.
4. Electronic remittance advice: Electronic remittances are available at this time.
However, some individual remittance advices may not be available due to Change
Healthcare’s security incident.
5. Prior authorization submission and processing: The prior authorization systems
continue to operate normally.
6. Eligibility verification, claim status inquiry, and authorization inquiry: These
capabilities continue to be available via NaviNet. If you do not have access to
NaviNet provider portal, please visit https://register.navinet.net to sign up.
Please note, in the interim, our Provider Services Department will not be able to assist with the
processing of your payments any sooner. If you have other questions, you may contact Provider

6
Services at 1-888-738-0004.
We thank you for your partnership and will continue to provide updates as we work to resolve the
downstream impacts of Change Healthcare’s service interruption.
Contact Information:
For providers that need to reach out to address a problem they have around procuring advanced
payments or any other issue:
a. Organization: AmeriHealth Caritas
b. Name: Danielle Quinn
c. Title: Vice President, Medicaid Markets
d. Email: providerandstaterequests@amerihealthcaritas.com

7
750 9th Street NW
Washington, D.C. 20001-4524
202.626.4800
www.BCBS.com
Anthem Blue Cross Blue Shield
Provider Relations (800)
676-2583
Elevance Health plans are providing updates on our response to the Change incident on our provider
portals. In addition, our provider services representatives have all been trained to assist providers
continuing to experience issues due to the Change incident. We encourage providers to contact our
provider services toll-free number for assistance. In addition, we are establishing a dedicated phone
number for providers seeking financial assistance. Providers can call 833-821- 2339, and their request will
be escalated for a response within 1-2 business days.
Arkansas Blue Cross and Blue Shield
Alessandra Barnes
Manager, Health Information Networks
albarnes@arkbluecross.com
(501) 502-1159
Arkansas Blue Cross and Blue Shield’s network development representatives have been working directly
with providers struggling to submit claims. Three providers within the state requested assistance with their
claims, and our staff has been in contact with them daily to assist with alternative methods of claims filing
and with working on the rejected claims reports when necessary.
Blue Cross Blue Shield of Alabama
Facilities:
Chris Wodarz
Manager, Hospital/Facility Contracting
Christopher.wodarz@bcbsal.org
(205) 220-5384
Professional:
Daniel Jackson
Manager, Healthcare Networks
dajackson@bcbsal.org
(205) 220-7842

8
Facilities: For hospitals, we have monitored weekly reimbursements for hospitals that have used Change
Healthcare as their clearinghouse to determine if they have fallen below a threshold amount. If so, we
have drafted correspondence notifying them of financial advances and providing a letter of agreement
specifying the payback terms associated with the advances.
Professional: While there has been no interruption in Blue Cross and Blue Shield of Alabama’s ability to
process and pay claims, we do recognize that some of our network providers have been impacted by recent
events. Blue Cross and Blue Shield of Alabama has multiple channels through which a provider can
submit claims and many providers have thanked us for our flexibility throughout this event. As such, Blue
Cross and Blue Shield of Alabama has been quick to offer cash advances and to help support the speedy
transition to new payment clearinghouses.
Blue Cross Blue Shield of Arizona
For Medicaid:
Charlotte Whitmore
Director, Medicaid Network Services
Charlotte.Whitmore@azblue.com
All other lines of business:
VP, Provider Network Management Colby
Bowers Colby.bower@azblue.com
The information we’re sharing publicly with providers is available here:
https://www.azbluefacts.com/changehealthcare/providers
Blue Cross Blue Shield of Florida
Shawn Trotter-Mitchell
SVP, Provider Network Solutions
shawn.trotter-mitchell@bcbsfl.com
With the goal of working closely with providers to ensure the health care ecosystem can quickly adapt to
alternate systems and prevent access-to-care disruptions, we are supporting providers with ongoing
communications to ensure awareness of alternative solutions for electronic claims submission and
transactions. We are also working directly with providers to help them understand the most appropriate
options available to continue transactional workflows and receive payments.
We are closely monitoring our provider payments to identify any material anomalies and ensure adequate
support for providers, including supporting pursuit of alternative options to continue transactional
workflows and receipt of related payments.

9
Blue Cross Blue Shield of Hawaii
Lori-Ann Davis
AVP, Provider Experience
lori-ann_davis@hmsa.com
(808) 948-5020
We understand providers may be experiencing issues as a result of the cybersecurity incident currently
impacting Change Healthcare. Please contact your HMSA field representative for assistance as every
provider’s situation will be unique. Your field representative will be able to provide you with personalized
support to help troubleshoot any issues you may be experiencing.
Blue Cross Blue Shield of Kansas
Doug Scott
Director, Professional Relations
doug.scott@bcbsks.com
(785) 291-8831
Janne Robinson
Director, Institutional Relations
janne.robinson@bcbsks.com
(785) 291-8227
BCBSKS took immediate action and preemptively disconnected our networks from affected systems.
We continue to monitor the situation. For systems impacted, BCBSKS has implemented a manual
component for pre-certifications in order to keep the process moving forward. For claim processes, EDI
has pro-actively implemented options for providers, including direct connection options, additional
vendor opportunities and other software options.
Blue Cross Blue Shield of Kansas City
Rhonda Janky
Director, Provider Partnerships
Rhonda.Janky@bluekc.com (816)
395-3086
Samantha Palmieri
Manager, Data Exchange Services
Samantha.Palmieri@bluekc.com
Data_exchange_services@bluekc.com (816)
395-2563
Our plan is actively working with providers to resolve issues they are experiencing with claims submission
and reimbursement as a result of the Change Incident including assistance and support connecting to new
clearinghouses and verifying that the providers claims are being received and reimbursed by our plan.

10
Blue Cross Blue Shield of Louisiana
Provider Relations
provider.relations@bcbsla.com
(800) 716-2299, option 4
BCBSLA has been outreaching to providers who use Change Healthcare to offer them alternative options
to get their BCBS claims submitted. We also provided the following information to providers via email
and on our provider portal message board:
Blue Cross and Blue Shield of Louisiana is aware of reports of a cyber event involving
Change Healthcare, a subsidiary of UnitedHealth Group. Blue Cross does not use any
Change Healthcare systems or processes impacted by the reported event. The cyber
event has not impacted Blue Cross' ability to serve its members and providers,
evaluate authorization requests or process filed claims.
Blue Cross knows that some Louisiana providers are impacted by this event. Blue Cross stands
ready to assist impacted providers if needed. Our systems remain online and available for
electronic claim filing for any provider or claims clearinghouse. If an impacted provider needs
assistance, you may contact our Provider Relations Department at provider.relatio[email protected]
or 1-800-716-2299, option 4.
Blue Cross continues to monitor events as information becomes available to protect our members.
Blue Cross Blue Shield of Massachusetts
Change Healthcare Assistance Program (CHAP)
(888) 402-3550
Provider Services (800)
882-2060
BCBSMA understands that the cybersecurity incident at Change Healthcare is leading to significant
disruptions to routine business interactions between some health care providers and Blue Cross Blue
Shield of Massachusetts. We want to assure you this is not a Blue Cross Blue Shield of Massachusetts
cyber incident. In fact, BCBSMA continues to conduct all business operations, such as processing
claims, benefits and eligibility verification, and referral and authorization requests by a variety of other
methods.
BCBSMA recommends that our provider partners pursue one of the many options noted below as an
alternative while Change Healthcare’s systems are unavailable. At present, BCBSMA does not know how
long the event at Change Healthcare will interrupt their service to you. Please see the Provider Central
resources, which present additional information on these topics:
• Get technical support for claim submission;
• Temporary waiver of claim filing and appeal limits for Change Healthcare affected
providers;
• Submission of claims via alternative ways;
• Checking claim status; and
• Benefit and eligibility checks

11
Blue Cross Blue Shield of Michigan
Jcynthia Tory
Director, Provider Servicing
Commercial Professional Providers: (800) 344-8525
Commercial Facility Providers: (800) 249-5103
Johanna Judson
Director Medicare Servicing (Medicare Advantage Provider Servicing) Medicare
Advantage PPO: (866) 309-1719
Blue Care Network Advantage Facility Providers: (800) 249-5103 Professional
Providers: (800) 344-8525
Please see Attached Provider Alert for public statement:
20240227 Provider
Alert.pdf
Blue Cross Blue Shield of Minnesota
Eric Hoag
VP, Provider Relations
Eric.Hoag@bluecrossmn.com
Blue Cross and Blue Shield of Minnesota has operationalized a short-term advance payment program for
healthcare providers affected by the Change Healthcare cyberattack. Funding will be allocated on a case-by-
case basis. We are currently working on expanding the program to reach providers throughout our state.
Blue Cross Blue Shield of Mississippi
For Institutional Providers:
Marc Dunn
Director, Provider Partnerships
MADunn@bcbsms.com
(601) 664-4216
For Professional Providers:
John Benedict
Manager, Provider Experience
JFBenedict@bcbsms.com (601)
664-4333
Based on conversations Blue Cross & Blue Shield of Mississippi (BCBSMS) has had with its Network
Providers, we understand some Providers are not impacted, some are waiting to determine next steps
dependent upon Change Healthcare’s timeline for restoration and others are transitioning to different
clearinghouses and vendors. Regardless of your position, BCBSMS is here to support you during this time.

12
BCBSMS has several options you may want to consider, dependent upon your organization’s size and
technology expertise and infrastructure. These options support the efficient filing of claims and can be
quickly accommodated. The options include System-to-System Connectivity, free direct claims software,
connectivity assistance to existing clearinghouse doing business with BCBSMS, Availity Lifeline short-
term service, and additional clearinghouses connecting with BCBSMS. Claims for previously impacted
Change Healthcare Providers who made a transition are being processed. You can contact BCBSMS
through the EDI Services Team at 601-664- HELP (Option 1) or the Provider portal.
Blue Cross Blue Shield of Nebraska
Brenda Wichman
VP, Member and Provider Services
Brenda.Wichman@nebraskablue.com
(402) 982-7074
Blue Cross and Blue Shield of Nebraska (BCBSNE) is providing advanced payment to providers impacted
by the Change Healthcare event. The advances are based on provider needs and claims payment trends. To
make this offer as administratively easy as possible on providers impacted by this situation, we are not
requiring them to reimburse the funds via claims offsetting. They may simply pay us back in a lump sum.
Blue Cross Blue Shield of North Carolina
Mark Werner,
VP, Network Management
CHCfinancialassistance@bcbsnc.com (919)
765-4700
Financial Assistance Coming for Eligible Providers Impacted by the Change Healthcare Outage
Blue Cross and Blue Shield of North Carolina (Blue Cross NC) recognizes that some of our smaller,
independent providers are facing greater financial burden due to the Change Healthcare (CHC) outage. CHC
is taking longer than they anticipated to recover from this cyberattack; therefore, we are offering additional
support to our provider community in the form of an interest- free loan. For more information and/or to
apply for this program, please email CHCFinancialAssistance@bcbsnc.com. Additional information
regarding alternative methods of claims submission and receiving remittance advice along with other
updates may be found at:
https://www.bluecrossnc.com/providers/provider-news/2024/change-healthcare-outage-affecting- claims-
submissions
https://www.bluecrossnc.com/providers/provider-news/2024/change-healthcare-outage-may- affect-
835-remittance-advice
https://www.bluecrossnc.com/providers/provider-news/2024/change-healthcare-outage-affecting- electronic-
submission-dental-claims
https://www.bluecrossnc.com/providers/provider-news/2024/change-healthcare-cybersecurity- update-
for-healthy-blue

13
Blue Cross Blue Shield of Rhode Island
Mary Ellen Moskal Director,
Provider Services
maryellen.moskal@bcbsri.org
(401) 459-5160
Providers impacted by the Change Healthcare outage in February 2024 may request a timely filing
exception for claims where the ability to meet timely requirements has been impacted by the outage. The
request should be detailed to include:
• Number of claims impacted.
• Detailed reason for the claims being submitted outside of the BCBSRI timely filing limit.
BCBSRI will accept requests for these exceptions now through 60 days post Change
Healthcare resolution for providers who were impacted by the outage. Requests should
be submitted to the Provider Relations Team at ProviderRel[email protected].
Blue Cross Blue Shield of South Carolina
Bart Strickland,
VP, Provider Services
Bart.Strickland@bcbssc.com (803)
264-1072
BCBSSC is operating normally, and providers should not see a delay from claims processing within our
system. However, BCBSSC is sensitive to the fact that a small number of providers may still be
experiencing issues. Providers are encouraged to utilize our web portal as an immediate solution for
claim submission. Our EDI on-boarding requirements have been streamlined for Change Healthcare
providers seeking an alternative submission channel.
Blue Cross Blue Shield of Vermont
Wendy York
Manager, Provider Relations (802)
371-3249
https://www.bluecrossvt.org/blue-cross-vt-response-change-healthcare-cybersecurity-incident
Blue Cross Blue Shield of Wyoming
Logan Trautwein
Director, Provider Affairs
Logan.Trautwein@bcbswy.com
(307) 829-3384
We have a notice on our website as well as providing detailed steps to our providers on how they can submit
claims to BCBSWY in order to get processed.

14
Blue Cross of Idaho
Karen Maciejewski
Director, Compliance and Privacy
Karen.maciejewski@bcidaho.com (986)
224-3987
We are working with providers in communicating information on switching clearinghouse vendors as they
may choose and offer assistance manually inputting claims during this issue with Change Healthcare. We
also continue to listen and support providers on other issues they may be experiencing with this incident and
ensure our members are still able to access care.
Blue Shield of California
Andy Chasin
VP, Federal Policy and Advocacy
andy.chasin@blueshieldca.com
BlueCross BlueShield of North Dakota
Teresa Moe
Director, Provider Network Performance
Teresa.moe@bcbsnd.com
(701) 277-2077
We encourage any impacted provider to reach out directly to BCBSND to help understand more about the
challenges they are experiencing due to this event.
BlueCross BlueShield of Tennessee
Susan Buchanan
VP, Provider Networks
susan_buchanan@BCBST.com (865)
384-3427
Capital Blue Cross
Provider Benefits Correspondence
providerbenefitcorrespondence@capbluecross.com (866)
688-2242
Capital Blue Cross has been working diligently to ensure minimal disruption to our providers and members
since we learned of the attack on Change Healthcare. We have seen no significant disruption or delays in
processing claims to date and the issues impacting Change Healthcare have not affected Capital’s IT
infrastructure. Although some of our network providers have used Change Healthcare for various services
and operations, we have worked closely with them to configure alternative solutions that allow them to
confirm eligibility, submit claims, and complete other important business functions. Our approach has
worked well, and we are fully committed to helping any provider solve their unique challenges.

15
CareFirst BlueCross BlueShield
Molly McIntyre
Director, Provider Relations and Education
Molly.mcintyre@carefirst.com, provider.carefirst.com
For continuity of electronic claims submission, CareFirst recommends providers directly contracted with
Change Healthcare for medical claims submission transition to Availity. The Availity connection is
available now.
Please find resources to support registering with Availity here: Availity Essentials Portal Registration. If you
use another EDI vendor who uses Change Healthcare as an intermediary for medical claims submission, we
recommend you work with your vendor to reroute medical claims through Availity. Any medical claims
submitted to CareFirst using or passing through Change Healthcare since February 21 for the products
mentioned above should be resubmitted to CareFirst once connection to Availity has been established.
As a reminder, providers can use CareFirst Direct to check Member eligibility and benefits or to see a list
of recent payments and remittances for these lines of business. Latest materials can be found here: News
Archives (www.carefirst.com )
Excellus BlueCross and BlueShield
Misty Postol
VP, Provider Relations
misty.postol@excellus.com
(315) 209-9634
We are aware of the ongoing cybersecurity issue associated with Change Healthcare, a third- party
vendor within the health care industry. Change Healthcare is part of Optum and tied to United
Healthcare. Please refer to United Healthcare’s website for updates related to this issue:
https://www.unitedhealthgroup.com/changehealthcarecyberresponse.
To assist our participating providers impacted by the outage of Change Healthcare’s claims clearinghouse, we
can offer temporary claim submittal alternatives.
Please contact your Provider Relations representative to discuss claim submission alternatives, advance
payment options, and any other impacts you may be experiencing.
We are actively monitoring the restoration efforts of Change Healthcare. As their services come back
online, we will assess each service individually and the attestations provided by Change Healthcare
regarding the related safety and security before reconnecting. It is important to note that this is a third-
party incident with no evidence of cybersecurity issues in our Health Plan systems. Rest assured that we
are taking every precaution to protect our members, providers and the internal business systems that
serve them.
HCSC
Provider Network Services
IL, NM, OK, TX: https://www.bcbstx.com/provider/contact-us
MT: https://www.bcbsmt.com/provider/network-participation/network/contact-us

16
Highmark
Kate Musler
SVP, Health Plan Risk Management
Katherine.Musler@highmark.com
(412) 544-8653
Highmark has launched an assistance program to provide funding advances for eligible participating
providers who use Change Healthcare or one of its impacted companies and are experiencing cash flow
concerns due to an inability to submit claims. Eligibility for assistance and amount of assistance will be
determined based on a variety of factors including inability to use an alternate method to submit claims and
current financial need. To apply for the assistance program, providers must submit a form located on
Highmark’s provider portal. Providers who are approved for a funding advance must sign an agreement
and the funding advance will be subject to the terms outlined in that agreement including repayment
obligations.
Horizon Blue Cross and Blue Shield of New Jersey, Inc.
Tim Collins Senior
Director
Timothy_j_collins@horizonblue.com (732)
256-5383
We included the following information on our website and also within our Provider Portals (NaviNet and
Availity):
“We are aware that Change Healthcare, a vendor that connects payers, providers and patients within the
U.S health care system, is experiencing a cyber security issue that is affecting the business operations of
many companies nationwide, including Horizon. This is not a Horizon incident, and at this time, there is
no indication that our systems have been compromised. Once we became aware of the incident, we
disconnected our systems from Change Healthcare and are reviewing the impact to our business
operations.
We are aware that some of our members may have been impacted as a result of this incident. If during this time
you need help filling a prescription, please call 1-800-370-5088
We know this can be concerning and are working hard to make sure you have continued access to care. We
are gathering more information as the situation unfolds and will provide updates as soon as possible.”
Independence Blue Cross
Provider Network Services
pnsproviderrequests@IBX.com
Independence is working closely with impacted providers and has communicated workarounds. We will
continue to pay claims submitted and are working directly with health systems on advanced payments
and other accommodations as circumstances warrant.

17
We also have provider-facing resources in response to the cyber incident on our Provider News Center
with information on alternative ways to submit claims and how to sign up for EFT payments if paper
check payments were disrupted by the Change Healthcare incident.
Premera
Brenda Frost
Senior Business Manager, Issues Management
issuesmgmt@premera.com
(425) 918-6525
Link to provider home page with banner: https://www.premera.com/wa/provider/
Link to Provider News story: https://providernews.premera.com/change-healthcare-
cybersecurity-issue-may-impact-claims-submissions/
Pharmacy Only: In-network pharmacies whom are continuing to experience challenges with submitting
electronic claims may reach out for plan support in working through these challenges with our PBM.
Regence
Alan Ford
Director of Provider Relations
Alan.Ford@regence.com (801)
333-2545
We worked from day one to make providers aware of available solutions such as Availity’s Lifeline and
CHC’s funding assistance program.
Triple-S Salud
Zoraida Mendez
VP, Provider Relationships & Partnership
zoraida.mendez@ssspr.com
(787) 749-4949 Ext 8322629
As partners, we are providing alternatives to these providers to directly submit their claims.
If you know of a provider that is affected by the situation, please inform them that they can visit our
provider website Mi Triple-S and submit their claims through that portal. They may also have other options
that our Provider Call Center will be able to offer to help them.
Providers are critical to our mission of enabling healthy lives. As partners, we want to make sure that they
can continue to focus on caring for our members’ health. Thus, we are taking proactive steps to providing
with any additional alternatives to address the difficulties some of them may be facing now.

18
Wellmark Blue Cross and Blue Shield
Network Technical Support (800)
407-0267
Wellmark’s processes for submitting claims and prior authorizations remain active. Wellmark continues
to monitor the situation and is committed to ensuring our members can access the care they need.

19
Centene Corporation
On Feb. 21, Change Healthcare experienced a cybersecurity incident that has created a service
disruption impacting payers, providers and pharmacies nationwide, including Centene and some of
its subsidiaries. Recognizing the impact of the outage, Centene took immediate and decisive action
to preserve access to care for its members and patients, while seeking to reduce the disruption for its
providers. The Company immediately initiated a provider outreach support campaign, launching a
website to help providers navigate this evolving situation with routinely updated reference materials,
tips, and step-by-step guidance to address challenges related to processing claims, checks, provider
advances, and chart retrieval. Centene’s
~700 Provider Engagement team members nationwide are proactively making calls, checking in on
providers, and working tirelessly to help them resume normal course operations as quickly as
possible.
Centene’s website is broken down by topic and will be routinely updated as the situation evolves.
Caring for members, providers, customers, and local communities is core to the Company’s mission.
Centene thanks you for your patience and apologizes for any inconveniences resulting from this
situation.
Claims
Centene understands that providers who use Change Healthcare (Emdeon Business Services) for
claims submission are experiencing challenges resulting from the outage. Centene’s preferred
clearinghouse for electronic claims submission is Availity, and their base Essentials plan is free for
Centene providers. To enroll, please visit Availity's website and/or call Availity Client Services at 1-
800-AVAILITY (1-800-282-4548). Step- by-step instructions for Availity, are outlined below:
Availity Lifeline Resource Guide, FAQs and Training Demos
How to Register with Availity’s Provider Portal (PDF)
Member Eligibility
There has been no impact on Centene's ability to check a member's eligibility. Providers seeking to
check a member's eligibility can do so through their normal process unless the provider utilizes
Change Healthcare for eligibility checks. Centene’s subsidiary health plans also offer multiple ways
for providers to easily check member eligibility, and detailed instructions can be found in the provider
manuals on the health plan websites.
Checks
Providers who receive payments through paper checks and virtual credit cards may have been

20
impacted by the Change Healthcare outage (providers receiving payments through an ACH
process are not impacted).
Centene moved provider payments previously facilitated by Change Healthcare to an alternative
vendor and, as of March 8, all Centene health plans resumed routine paper check cycles.
Alternatively, to receive payments more quickly, you can sign up with PaySpan (now part of Zelis) to
receive ACH payments from Centene at www.payspanhealth.com.
How to Register for PaySpan Health (PDF)
Provider Advances
Centene recognizes that finding alternative ways to submit claims is not always immediately
possible. As a result, providers may be experiencing extreme financial hardship (e.g., risk in making
payroll) resulting from the Change Healthcare cybersecurity incident that could impact their ability
to continue operating and, ultimately, limit access to care for our members.
Preserving access to care for our members and supporting our providers remains our top priority.
As an organization, the Company’s guidelines for considering cash advances largely aligns with
CMS’ approach on accelerated fee-for-service payments, as outlined in CMS’ March 9, 2024
Change Healthcare/Optum Payment Disruption (CHOPD) Accelerated Payments to Part A
Providers and Advance Payments to Part B Suppliers Fact Sheet. The Company’s provider advance
program is for a 90-day term, with zero interest, and requires completion of a two-page agreement.
Centene will assess all requests for cash advances on a case-by-case basis.
Providers experiencing financial distress should reach out to their local Provider Engagement team
for immediate support. If you are unsure of who to contact, providers can submit a request for a cash
advance by emailing us at [email protected].
Chart Retrieval
Change Healthcare performs retrieval of medical records for several of our programs, such as
HEDIS® and Risk Adjustment. You may have received a request via phone or fax from Change
Healthcare on behalf of Centene or its subsidiary health plans, where you either scheduled
appointments or provided medical records. Change Healthcare is unable to honor any fulfillment
requests at this time; however, Centene will be employing two of our existing medical record
retrieval vendors, Datavant (formerly Ciox) and Datafied, to satisfy these prior commitments.
These retrievals are required to report on clinical quality measures and diagnosis data to Health and
Human Services (HHS), the Centers for Medicare & Medicaid Services (CMS) and the National
Committee for Quality Assurance (NCQA). Centene asks that you please honor the same
commitment dates for these vendors, even if you have already committed to providing medical records
to Change Healthcare. If you have provided medical records from the time period of Feb. 19, 2024 to
current, you may be asked to provide these medical records again.

21
Providers experiencing financial distress should reach out to their local Provider Engagement team
for immediate support. If you are unsure of who to contact, providers can submit a request for a cash
advance by emailing us at [email protected].
Alternatively, providers can contact Centene’s Enterprise Provider Experience Lead regarding any
issues requiring escalation:
a. Organization: Centene Corporation
b. Name: Kate Blackmon
c. Title: SVP, Provider Experience
d. Email: k.blackmon@centene.com
e. Phone Number: 214-784-1719
Thank you for the opportunity to provide additional detail concerning Centene’s ongoing efforts to
connect with and assist our provider community and close the last mile.

22
Cigna Healthcare
Change Healthcare cyber security incident.
As you likely know, Change Healthcare publicly announced a cyber security incident last week. We
understand many providers who treat patients with a Cigna Healthcare benefit plan work through Change
Healthcare to administer electronic services, including claim submissions, eligibility verification,
precertification, and other administrative services. The Cigna Group, which includes Cigna Healthcare
and Evernorth Health Services, also works with Change Healthcare to facilitate some of these services.
The issues they are experiencing are therefore impacting our ability to interface with Change Healthcare.
First, please know that we continue to actively monitor the situation and there are no indications that any
The Cigna Group systems are affected.
As an organization, we are focused on ensuring access to care and medications for our customers and
patients while also ensuring that you have alternative options to transact with us as needed. We are also
working to resolve any disruption from Change Healthcare’s incident for you, individuals, clients, and
other partners as quickly as possible.
What we did when we found out about the incident
After becoming aware of the incident, we immediately severed system connections with Change Healthcare
and relevant associate UnitedHealth Group companies (e.g., UnitedHealthcare and Optum) and
implemented business continuity planning to ensure there was as limited disruption to our provider partners,
customers, and clients as possible.
Network connections were reestablished on February 24 with related UnitedHealth Group companies,
which include Optum and UnitedHealthcare. This decision was made after conducting additional
investigation and receiving validation from the UnitedHealth Group that these companies were not
impacted by the cyber incident. However, our connections to Change Healthcare systems remain
severed as they work to resolve this issue, and there is currently no estimated date for restoration.
Submitting claims to Cigna Healthcare
• We encourage all commercial and Medicare Advantage providers to utilize the many alternative
digital trading partners we offer to submit claims directly to Cigna Healthcare. Please know that we
have been in direct contact with these vendors and are confident in their ability to support your digital
transactional needs in a timely manner.
• Commercial providers also have the option to submit paper claims to us through typical claims
addresses and can access Explanation of Payments (EOPs) and Direct Deposit Activity Reports (also
known as remittance reports) on CignaforHCP.com to reconcile their payments.
• Cigna Healthcare Medicare Advantage uses Change Healthcare to issue electronic funds
transfers (EFT), paper check payments, and corresponding electronic remits and EOPs to
providers. As a result of severing system connections with Change Healthcare, EFT and paper check
payments for Medicare Advantage claims have been held since February 21, 2024. Please be assured
that we are quickly working on an alternative solution to ensure you are paid in a
timely manner and remain committed to working with you to reconcile claims and payments, as
needed. We appreciate your patience and will update you soon.

23
Alternative options to check patient eligibility.
Cigna Healthcare continues to offer two primary alternative options for providers to check eligibility and
benefits information for their patients with a Cigna Healthcare benefit plan:
Option one (online)
Commercial providers | Verify patient eligibility and verify patient and plan detail information on
CignaforHCP.com.
Medicare Advantage providers | Verify patient eligibility and verify patient and plan detail
information on the HSConnect Provider Portal.
Option two (automated phone)
Commercial providers | Call Cigna Healthcare Customer Service at 800.88Cigna (882.4462).
Medicare Advantage providers | Call Cigna Healthcare Customer Service at 800.230.6138.
Please note that for our Third-Party Administrator accounts (e.g., Shared Administration Repricing and
Payer Solutions), providers should continue to verify eligibility by calling the number on the back of the
patient’s ID card.
Answers to commonly asked questions
We appreciate that your day-to-day operations, like ours, may be impacted by the Change Healthcare
outage. However, the incident at Change Healthcare has not affected our ability to operationally receive,
process, respond to, review, or approve various provider requests, including those about precertification,
admissions, and utilization management reviews.
Therefore, Cigna Healthcare’s existing requirements remain in place with no changes at this time.
While we continue to monitor the situation closely, and may update some of our guidance if Change
Healthcare remains down for an extended period of time, we are not making any changes to the following
requirements at this time:
• Precertification (i.e., authorizations)
• Timely filing
• Facility-to-facility transfers and related authorizations
• Admission notifications
• Eligibility reviews
• Utilization management review
Precertification
Precertification continues to be an important way to ensure that your patients’ care will be covered under
their specific benefit plan. The precertification process also helps direct participants to various support
programs, including wellness coaching, chronic condition coaching, and case management.
As noted above, the incident at Change Healthcare has not impacted our ability to receive, process, or
approve precertification requests. Therefore, Cigna Healthcare’s precertification requirements remain in
place with no changes at this time (including for facility-to-facility post-acute transfers). Providers are
encouraged to continue to use standard channels to request precertification through Cigna Healthcare and
related The Cigna Group companies.

24
Cigna Healthcare (commercial)
• CignaforHCP.com > Precertification process
• 800.88Cigna (882.4462)
Cigna Healthcare (Medicare Advantage)
• HSConnectOnline.com
• 800.668.3813
eviCore healthcare*
• eviCore.com/provider
• 800.918.8924
Keeping you informed
It’s unclear how long this outage will remain in place. We continue to stay in touch with Change
Healthcare and have requested a timing estimate for restoration of their site. As always, we remain
committed to keeping you informed as we learn more or as we update the guidance noted above.
In the meantime, if you have any questions, feel free to engage us as you do today through your standard
channels, and we will answer as best we can.
Thank you for the ongoing care you provide our customers.

25
CVS Health
Aetna’s Provider Bulletin provides information to our network providers experiencing impact
from the Change Healthcare network disruption, including a set of Frequently Asked Questions
that address the mitigation plans in place for providers to complete transactions with Aetna. We
will continue to share additional information as it becomes available. The Bulletin can be found on
our website at Aetna.com.
Contact Information:
Given the breadth of Aetna’s network, the multiple business segments covered, and the variability
in provider questions we receive daily, there is a “Contact Us” link on Aetna.com that includes
different phone numbers affiliated with different provider needs. This ensures more efficient and
effective provider service. The contact page is here: Contact Us - Health Care Providers
(aetna.com)
CVS Health is committed to continue our around the clock work to ensure access to healthcare
and address problems related to the Change Healthcare incident. Please contact us with any
questions about these survey responses.

26
Elevance Health
Are you extending timely filing requirements for providers impacted by Change Healthcare?
At this time, our timely filing requirements remain in place. However, for those providers who are
actively working to transition to Availity or their preferred clearinghouse as a result of the Change
Healthcare incident, we are extending timely claims filing days by an additional 30 days from the
date of the service to provide additional time for submissions.
Until this event is resolved, we are here to assist providers with any questions they may have.
For more information on timely filing requirements, you can find timeframes and processes in your
provider manual by selecting Provider Home from the top of this News site and navigating to the
Resources category.
Will you make advance payments or loans to providers?
Our ability to process and pay claims is not impacted. We encourage providers that rely on Change
to move to Availity or another claim clearinghouse of their choosing to submit claims.
We have extended timely filing requirements for affected providers by 30 days and have
accelerated the processing for existing claims volume. Please note that Carelon Health (formerly
known as CareMore) and National Government Solutions (NGS) are currently excluded from
extensions to timely filing requirements.
Any provider unable to change data clearinghouse or experiencing other issues, including financial
hardship, should contact their provider service representative.
Contact Information
Elevance Health plans are providing updates on our response to the Change incident on our
provider portals. In addition, our provider services representatives have all been trained to assist
providers continuing to experience issues due to the Change incident. We encourage providers to
contact our provider services toll-free number for assistance.
In addition, we are establishing a dedicated phone number for providers seeking financial
assistance that will go live this weekend. Providers can call 833-821-2339, and their request will
be escalated for a response within 1-2 business days.

27
An update from Humana regarding the Change Healthcare
cyber security incident (March 20, 2024)
Dear provider,
As you may know, Change Healthcare has been involved in a cyber security incident. It appears as if you
may typically utilize Change Healthcare as your electronic clearinghouse. While this cyber security
incident didn’t originate with Humana, the interconnectivity of our healthcare system partners and our
shared commitment to providing uninterrupted access to care underscores the importance of working
together as an industry to overcome disruptions and find solutions. We are here to help.
What happened?
On Feb. 21, 2024, Change Healthcare notified Humana that it experienced a cyber security incident. This
resulted in system outages at Change Healthcare and caused widespread disruptions for many entities in the
healthcare industry that utilize Change Healthcare’s various electronic clearinghouse capabilities.
What does this mean to you?
Due to this cyber security incident, the connection between Humana systems and Change Healthcare
systems was severed; this connection remains out of service. We want to ensure you have found alternate
methods for claims submissions.
What do you need to do next?
Availity—another electronic clearinghouse—has published guidance for providers to connect directly for
various uses, including claims submission. Providers can utilize Availity instead of Change Healthcare.
View instructions on how to use Availity for your claim submissions at
https://www.availity.com/availity-lifeline-self-serve-resources > Self-Serve Transactions > Download
the PDF guidance. Availity has also created a microsite with information to help health plans, providers
and trading partners navigate the current environment. This microsite can be accessed at
htps://marketing.availity.com/Availity-lifeline. If you need assistance, complete the form on this
microsite, and a representatives from Availity will reach out to you to assess your situation and advise on
next steps.
Additionally, for providers who have existing Availity accounts, the microsite provides guidance on how
to utilize that account to exchange both batch and real time transactions.
Humana is also accepting paper and faxed claims: You can submit paper claims to Humana at the address
on the back of the member’s ID card or fax claims to 888-556-2128. Please do not hesitate to reach out to
Provider Services at 800-457-4708, 8 a.m. to 8 p.m. Monday through Friday, Eastern time—if you have
further questions or need additional assistance.

28
Kaiser Permanente
Kaiser Permanente exists to provide high-quality, affordable health care services and to improve
the health of our members and the communities we serve. Our external providers and networks are
an integral part of how we deliver on our mission, and when their operations are disrupted through
cyberattacks like the one affecting Change Healthcare, we believe it is vital that we quickly act to
support them. Should a provider or hospital in our contracted network need financial support, we
urge them to please reach out to their Kaiser Permanente Provider Contracting and Relations team
member to request assistance and access our online Provider Portal for up-to-date information and
resources.
Contact Information
For providers that need to reach out to address a problem they have around procuring advanced
payments or any other issue:
a. Organization: Kaiser Permanente
b. Name: Ken Kurzendoerfer
c. Title: Vice President, National Claims Administration, Provider Data Management, and
Applied Intelligence Solutions
d. Email: kenneth.w.kurzendoerfer@kp.org
e. Phone Number: 858-860-6095 (mobile)

29
Molina Healthcare
Molina Healthcare is and has been committed to providing support to its providers during the Change
Healthcare (CHC) outage. Molina Healthcare has established a dedicated contact center to assist
providers impacted by the CHC outage, which is available Monday-Friday from 5:00AM PST to
6:30PM PST. That contact center number is (844) 548-7684.
Communications and updates regarding the CHC incident are also posted on the Molina Healthcare
provider website. Molina Healthcare has a process to support emergency payment requests if
providers are in financial distress. Please contact our dedicated contact center to obtain information
about this process.
Molina Healthcare has alternative options available for claims submission and will provide assistance
to any provider who needs help with such alternative options. Providers utilizing CHC to submit
claims to Molina prior to this outage may use our alternate established connection with SSI Claimsnet,
LLC (“SSI Group”) clearinghouse or another clearinghouse of provider’s choice. Providers can
register with SSI Group for claim submission via the Claimsnet’s Provider Registration Form located
online at:https://products.ssigroup.com/molinaregistrationportal/register.
Our Availity Essentials provider portal solution was not impacted by the CHC outage and remains
available as another option to key in claims for submission. Providers can register with Availity
Essentials at https://www.availity.com/molinahealthcare. Molina Healthcare encourages all our
providers submitting paper claims to explore our electronic submission options, although claims can
always be submitted in paper form.
Contact Information
For providers that need to reach out to address a problem they have around procuring advanced
payments or any other issue:
b. Organization: Molina Healthcare
c. Name: Molina Provider Portal Management and Response Team
d. Title: Manager
e.
Email:
CHCoutage@molinahealthcare.com
f.
Phone Number:
844-548-7684, Monday-Friday 5:00AM
PST to 6:30PM PST
30
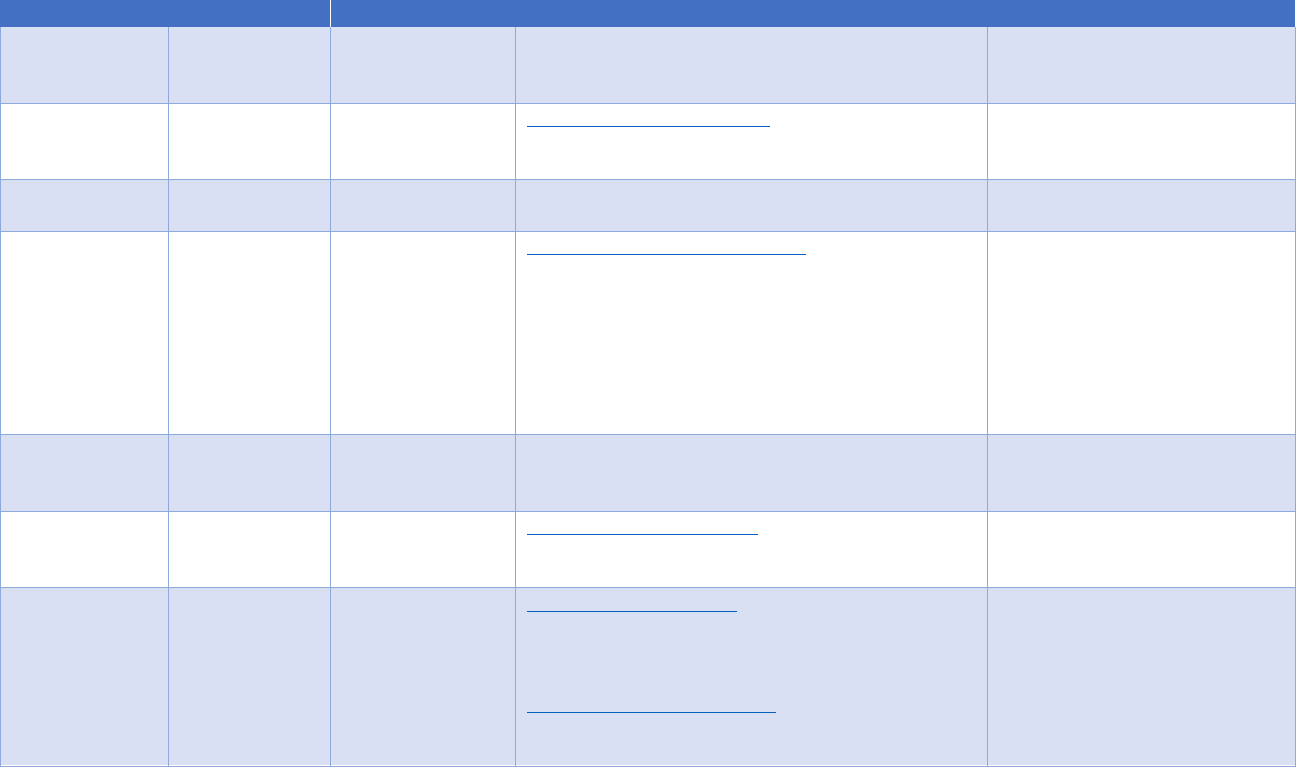
Payer Contact Information
The Department of Health and Human Services asked health plans to provide specific national contact information that providers can use
when needed. Below, providers can find contact information for health plans across the country. Please share this resource with
providers who need it.
Organization
Staff Name
Title
Email
Phone Number
Anthem Blue
Cross Blue
Shield
(800) 676-2583
Arkansas Blue
Cross and Blue
Shield
Alessandra Barnes
Manager, Health
Information
Networks
albarnes@arkbluecross.com
(501) 502-1159
AmeriHealth
Caritas
Danielle Quinn
Vice President,
Medicaid Markets
providerandstaterequests@amerihealthcaritas.com
Blue Cross Blue
Shield of
Alabama
Facilities: Chris
Wodarz
Manager,
Hospital/Facility
Contracting
Christopher.wodarz@bcbsal.org
(205) 220-5384
Professional:
Daniel Jackson
Manager,
Healthcare
Networks
dajackson@bcbsal.org
(205) 220-7842
Blue Cross Blue
Shield of Florida
Shawn Trotter-
Mitchell
SVP, Provider
Network
Solutions
shawn.trotter-mitchell@bcbsfl.com
Blue Cross
Blue Shield of
Hawaii
Lori-Ann
Davis
AVP, Provider
Experience
lori-ann_davis@hmsa.com
(808) 948-5020
Blue Cross
Blue Shield of
Kansas
Doug Scott
Director,
Professional
Relations
doug.scott@bcbsks.com
(785) 291-8831
(785) 291-8227
Janne
Robinson
Director,
Institutional
Relations
janne.robinson@bcbsks.com

31
Blue Cross Blue
Shield of Kansas
City
Rhonda Janky
Director, Provider
Partnerships
Rhonda.Janky@bluekc.com
(816) 395-3086
Samantha
Palmieri
Manager, Data
Exchange
Services
Samantha.Palmieri@bluekc.com
Data_exchange_services@bluekc.com
(816) 395-2563
Blue Cross Blue
Shield of
Louisiana
Provider
Relations
provider.relations@bcbsla.com
(800) 716-2299, option 4
Blue Cross
Change
(888) 402-3550
Blue Shield of
Healthcare
Massachusetts
Assistance
Program (CHAP)
Provider Services
(800) 882-2060
Blue Cross Blue
Shield of
Michigan
Jcynthia Tory
Johanna Judson
Director, Provider
Servicing
Director Medicare
Servicing
(Medicare
Advantage
Provider
Servicing)
Commercial Professional
Providers: (800) 344-8525
Commercial Facility Providers:
(800) 249-5103
Medicare Advantage PPO: (866)
309-1719 Blue Care
Network Advantage Facility
Providers: (800) 249-5103
Professional Providers: (800)
344-8525
Blue Cross Blue
Shield of
Minnesota
Eric Hoag
VP, Provider
Relations
Eric.Hoag@bluecrossmn.com
Blue Cross Blue
Shield of
Mississippi
For Institutional
Providers:
Marc Dunn
Director, Provider
Partnerships
MADunn@bcbsms.com
(601) 664-4216
JFBenedict@bcbsms.com
(601) 664-4333

32
For Professional
Providers: John
Benedict
Manager,
Provider
Experience
Blue Cross
Blue Shield of
Nebraska
Brenda
Wichman
VP, Member and
Provider Services
Brenda.Wichman@nebraskablue.com
(402) 982-7074
Blue Cross Blue
Shield of North
Carolina
Mark Werner
VP, Network
Management
CHCfinancialassistance@bcbsnc.com
(919) 765-4700
Blue Cross
Blue Shield of
Rhode Island
Mary Ellen
Moskal
Director, Provider
Services
maryellen.moskal@bcbsri.org
(401) 459-5160
Blue Cross Blue
Shield of
South Carolina
Bart Strickland
VP, Provider
Services
Bart.Strickland@bcbssc.com
(803) 264-1072
Blue Cross Blue
Shield of
Vermont
Wendy York
Manager,
Provider
Relations
(802) 371-3249
Blue Cross Blue
Shield of
Wyoming
Logan
Trautwein
Director, Provider
Affairs
Logan.Trautwein@bcbswy.com
(307) 829-3384
Blue Cross of
Idaho
Karen
Maciejewski
Director,
Compliance and
Privacy
Karen.maciejewski@bcidaho.com
(986) 224-3987
Blue Shield of
California
Andy Chasin
VP, Federal
Policy and
Advocacy
andy.chasin@blueshieldca.com
BlueCross
BlueShield of
North Dakota
Teresa Moe
Director, Provider
Network
Performance
Teresa.moe@bcbsnd.com
(701) 277-2077
BlueCross
BlueShield of
Tennessee
Susan
Buchanan
VP, Provider
Networks
susan_buchanan@BCBST.com
(865) 384-3427
Capital Blue
Cross
Provider Benefits
Correspondence
providerbenefitcorrespondence@capbluecross.com
(866) 688-2242

33
CareFirst
BlueCross
BlueShield
Molly McIntyre
Director, Provider
Relations and
Education
Molly.mcintyre@carefirst.com
CDPHP
ProviderRelations@cdphp.com
(518) 641-3890
Centene
Corporation
Kate Blackmon
SVP, Provider
Experience
k.blackmon@centene.com
214-784-1719
Cigna
Healthcare
Commercial: 800-88Cigna
(882.4462)
Medicare Advantage: 800-668-
3813
eviCore healthcare: 800-918-
8924
Elevance
833-821-2339
Excellus
BlueCross and
BlueShield
Misty Postol
VP, Provider
Relations
misty.postol@excellus.com
(315) 209-9634
Fallon Health
Susan Keser
VP, Provider
Contracting &
Network
Development and
Management
susan.keser@fallonhealth.org
508-368-9261
Geisinger
Health Plan
Paul Forlenza
Kim Spath
Director, Provider
Contracting
Sr. Director,
Provider Account
Management
prforlenza@thehealthplan.com
kspath@thehealthplan.com
1-800-876-5357
Group Health
Cooperative of
South Central
Wisconsin
John Duncan
Contracting
Manager
jduncan@ghcscw.com
608-662-4882
HAP
Jeffrey
Holzhausen
Vice President of
Provider
Contracting and
Network
Development
jholzha1@hap.org
734-502-6548

34
Health Care
Service
Corporation
Kelly Butler
Vice President,
Customer Service
CHC_Requests@bcbsil.com
800-972-8088
Highmark
Kate Musler
SVP, Health Plan
Risk Management
Katherine.Musler@highmark.com
(412) 544-8653
Horizon Blue
Cross and Blue
Shield of New
Jersey, Inc.
Tim Collins
Senior Director
Timothy_j_collins@horizonblue.com
(732) 256-5383
Humana
800-457-4708
Independence
Blue Cross
Provider Network
Services
pnsproviderrequests@IBX.com
Independent
Health
Anthony
Montagna
SVP – Chief
Network Officer
anthony.montagna@independenthealth.com
(716) 635-3639
Kaiser
Permanente
Ken
Kurzendoerfer
Vice President,
National Claims
Administration,
Provider Data
Management, and
Applied
Intelligence
Solutions
kenneth.w.kurzendoerfer@kp.org
858-860-6095
Martin’s Point
Health Care
Jeff Polk
Vice President,
Network
Management
Jeffrey.polk@martinspoint.org
(207) 233-2439
Molina
Healthcare
Molina Provider
Portal
Management
and Response
Team
Manager
CHCoutage@molinahealthcare.com
844-548-7684, Monday-Friday
5:00AM PST to 6:30PM PST
Premera
Brenda Frost
Senior Business
Manager, Issues
Management
issuesmgmt@premera.com
(425) 918-6525
Regence
Alan Ford
Director of
Provider
Relations
Alan.Ford@regence.com
(801) 333-2545

35
Security Health
Plan
shpprd@securityhealth.org
1-800-548-1224
Triple-S Salud
Zoraida
Mendez
VP, Provider
Relationships &
Partnership
zoraida.mendez@ssspr.com
(787) 749-4949 Ext 8322629
UCare
Theresa-Peters
Nelson
Director, Provider
Relations &
Contracting
tpeters-nelson@ucare.org
612-294-5089
UnitedHealth
Group
1-877-702-3253
UPMC
Mike Sweeney
Vice President,
Reimbursement,
Contracting and
Value Based
Reimbursement
sweeneyms@upmc.edu
Wellmark Blue
Cross and Blue
Shield
Network
Technical Support
(800) 407-0267
