
COVID-19 Vaccination Field Guide:
12 Strategies for Your Community
U.S. Department of
Health and Human Services
Centers for Disease
Control and Prevention

Table
of Contents
4
Introduction
4 About This Guide
5 Using this Guide
6
Common Barriers
6 Structural Barriers
6 Behavioral Barriers
7 Informational Barriers
8
Understanding
Your Community
8 The Social Vulnerability
Index (SVI)
9 Walk a Mile Exercise
11 Diagnostic Tool to
Identify Factors and
Strategies
12 Rapid Community
Assessment (RCA)
13
Vaccine
Confidence and
Uptake Strat
egies
15 Strategy 1:
Vaccine Ambassadors
17 Strategy 2:
Medical Provider
Vaccine Standardization
18 Strategy 3:
Medical Reminders
20 Strategy 4:
Motivational Interviews
21 Strategy 5:
Financial Incentives
22 Strategy 6:
School-Located
Vaccination Programs
23 Strategy 7:
Home-Delivered
Vaccination
24 Strategy 8:
Workplace
Vaccination Programs
25 Strategy 9:
Vaccine Requirements
27 Strategy 10:
Eective Messages
Delivered by Trusted
Messengers
29 Strategy 11:
Provider
Recommendation
30 Strategy 12:
Combating
Misinformation

4
T
he COVID-19 pandemic has affected millions of lives in communities across the world,
including in the United States. COVID-19 is unique in many ways, including its global impact,
its politicization, and the need for universal vaccination to combat the virus. When COVID-19
vaccines became available in the United States, millions of Americans eagerly sought out
and received them. Many see vaccination as the key to a post-pandemic life, yet millions of Americans
have still not been vaccinated despite eligibility and plentiful supply. Desire for receiving a COVID-19
vaccine among some minority populations, particularly Black or African American and Hispanic or
Latino populations, is high though uptake is lagging
12
. This indicates barriers related to access and
equity may be at play. For other populations, there is more hesitancy about getting vaccinated.
Communities with vaccination rates much lower than the national average may need to further
investigate and address barriers to COVID-19 vaccination.
People encounter barriers that can hinder or facilitate vaccinations. Barriers and facilitators range from
logistical and access issues, to personal beliefs and risk perception, to community beliefs and social
norms. Insights from behavioral health research can help determine strategies to help people get
vaccinated and promote near-universal uptake.
Health departments, community organizations, faith-based communities, and leaders from all sectors
of public life are making great efforts to promote COVID-19 vaccination. No single approach will work
for every community; in fact, as the research included here demonstrates, a combination of strategies
is generally most effective and will increase chances for success. This field guide highlights several
strategies derived from evidence-based practices that are being applied in communities across the
country to promote vaccine confidence and uptake.
About this Guide
This field guide offers intervention strategies to promote COVID-19 vaccine confidence and uptake
based on a rapid assessment of evidence that identified research-proven methods. This guide is
intended to support the work of health departments and community- and faith-based organizations
across the United States. It highlights some common barriers that communities experience in vaccine
confidence and uptake. Not all barriers are relevant in all communities; therefore, the second section
of this guide helps you understand the various needs of different communities and offers tools to help
you assess barriers and find potential solutions for your community of focus.
The final section describes 12 intervention strategies drawn from historical vaccination efforts that
have demonstrated positive outcomes through evaluation research. While most of the guide focuses
on increasing vaccine uptake, several strategies address increasing vaccine confidence. Each strategy
highlights the approach, population(s) served, location, barriers addressed, basis in research, and an
example of how the strategy is currently being applied to address COVID-19 vaccination.
Vaccine Confidence is the trust
that people have in recommended
vaccines and how they are
administered and developed.
Without some level of confidence,
people will not move toward
receiving a vaccine.
Vaccine Uptake refers to the
proportion of the population
that has received a vaccine.
1 PPRI Sta. (July 27, 2021). Religious Identities and the Race Against the Virus: (Wave 2: June 2021). Retrieved at:
https://www.prri.org/research/religious-vaccines-covid-vaccination/.
Ndugga, N., Hill, L., Artiga, S., and Parker, N. (August 18, 2021). Latest Data on COVID-19 Vaccinations by Race/Ethnicity. 2
Retrieved at: https://www.k.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/

5
Using this Guide
This resource consists of three primary sections:
1. Common Barriers
This section of the guide tells about common barriers to vaccine confidence and uptake.
2. Understanding Your Community
This section offers tools you can use to identify and understand what barriers and facilitators may
be factors in your community of focus. You may need only one of these tools, or several to increase
your understanding of your community.
3. Vaccine Confidence and Uptake Strategies
Here you will find recommended strategies to increase vaccine confidence and uptake. The research
that supports the strategy is provided along with case study examples. More information about the
strategies, including guidance and implementation resources, are linked within the document
and provided in Appendix A.
Factor in cost of implementing the strategy
including dollars, time, level of effort, staffing.
Implement the strategy to have the most success
by having relevant community members involved in
planning and execution; obtain leadership buy-in.
Consider piloting the effort on a small scale
to measure success before attempting wider
implementation, especially if you are unsure
about a strategy.

6
Common Barriers
There are several common barriers to COVID-19 vaccine confidence and uptake. Leaders should
consider which barriers the people in their community are experiencing. Understanding the barriers
can help identify strategies most likely to increase vaccine uptake. The Behavioral and Social Drivers
(BeSD) framework described in Appendix D offers another way to view what drives or motivates
COVID-19 vaccine uptake.
Structural Barriers
Equity: COVID-19 vaccines may not be equally distributed, administered, or accessed in
communities nationwide, especially among under-resourced communities in urban and rural areas.
Cost: While COVID-19 vaccination is currently free, it requires time and resources. This includes figuring
out where to get vaccinated, making an appointment (if necessary), traveling to the vaccination site,
possibly taking time off from work, and recovery times for those who experience side effects. Some
people will need childcare or transportation, or are unable to take time off work to get vaccinated or
recover from side effects.
Access: Proximity and travel convenience to a vaccination site plays a large part in an individual’s
ability to get vaccinated. Vaccination clinic hours of operation may limit access for some as well.
Some people do not have transportation access, internet access, or the technical skills required to
search online for vaccination sites or appointments. People with disabilities, who are confined to
their homes, or who live in a long-term care or correctional facility, cannot travel to get a vaccine.
Policy: Existing policies, such as health insurance requirements for most medical services and
service restrictions for non-citizens and undocumented residents, can influence understanding of
vaccine access. People may not know they are eligible to receive a vaccine for free or be aware of
their employer’s policies on paid and unpaid leave for vaccination purposes. Also, employers are
encouraged, but not required, to have policies allowing employees to take paid leave to get
vaccinated and to recover if they have temporary side effects.
Behavioral Barriers
Inertia: Getting vaccinated takes planning and effort. Many individuals have difficulty making
decisions—especially large decisions—so instead of deciding, they do nothing. This tendency to
do nothing leaves people unvaccinated.
Prevailing Social Norms: Community norms often drive individuals’ actions. If trusted friends
or leaders in one’s community are against getting vaccinated, others will likely follow suit.
Forgetfulness: People may forget non-routine activities and procedures. They may forget to book their
vaccination appointments or to keep them.
Friction: Complex, inconvenient, or effort-provoking processes often lead people to fulfill immediate
wants and needs. If the process of booking or attending a vaccination appointment is too complicated,
they will not do it.
Misperception: Individuals may have vaccine opinions and beliefs based on scientific inaccuracies,
including that they are at low risk of getting severely sick with COVID-19, that the pandemic is being
exaggerated, or that vaccines are not effective. These inaccuracies are often spread in communities and
lead to fear, resistance, or mistrust.

7
Behavioral Barriers (Continued)
Mistrust: Lack of trust in institutions including government, medical institutions, and media, is
sometimes based on individual or communal experiences, and affects decisions about vaccination.
Uncertainty: Due to the novelty of the vaccines, many individuals feel uncertain about the short- and
long-term side effects, causing them to take a cautious “wait-and-see” approach to getting vaccinated.
With the course of the pandemic uncertain, people may believe it will soon be over. So, they may
believe they do not need a vaccine or want to wait to see if a different option will be approved to
address COVID-19 variants. Changes in official guidance can also make people feel uncertain about
their actions or decisions.
Politicization: COVID-19 vaccines have been politicized, making political affiliation a strong
determinant of vaccination beliefs and behaviors.
Informational Barriers
Cultural Relevance: Information about the vaccines is not always communicated in ways that reflect
sociocultural norms, beliefs, and realities. This can make information less relevant and confusing to
some individuals. Language may also be a barrier for non-native English speakers, especially given the
complexity and novelty of some vaccine information.
Health Literacy: Individuals may not fully understand the complex vaccine information being shared,
such as the multiple types of vaccines offered or lack of a clear and simple call to action. Adding to
confusion is changing guidance. People may lose trust or become confused when new information is
conveyed frequently; possibly not understanding that changing data impacts guidelines. People may
also have difficulty telling the difference between factual and false health information.
Mis- and Disinformation: Most mis- and disinformation that has circulated about COVID-19 vaccines
has focused on vaccine development, safety, and effectiveness, as well as minimizing the severity of the
pandemic and COVID-19 denialism.
Lack of Adequate Information: Some individuals lack the information they need to understand the
risks, benefits, and background of vaccine development to make an informed decision about getting
vaccinated. Information overload can also be a form of inadequate information as it can become
difficult for people to know what is relevant or current.
Misinformation is false information
shared by people who do not intend
to mislead others.
Disinformation is false information
deliberately created and
disseminated with malicious intent.

8
Understanding Your Community
To effectively address common barriers, it is important to identify and understand your community of
focus. Existing community data and previously conducted assessments, such as a health equity impact
assessment, may be available and useful in this process. Several tools are available to help with this,
including the Social Vulnerability Index, the “Walk a Mile” Exercise, the diagnostic tool, and the Rapid
Community Assessment (RCA) Guide.
The Social Vulnerability Index
The Social Vulnerability Index (SVI) is a Centers for Disease Control and Prevention (CDC) database
designed to help emergency response planners and public health officials identify and map
communities that will most likely need support before, during, and after a public health emergency,
including the COVID-19 pandemic. Data from the SVI can help local leaders identify and decide which
populations to focus on.
About
Several factors, including poverty, lack of access to transportation, and crowded housing may weaken a
community’s ability to prevent human suffering and financial loss in a disaster. These factors are known
as social vulnerability. Reducing social vulnerability can decrease human suffering and economic loss.
The SVI ranks each county and census tract based on four themes:
1. Socioeconomic status
2. Household composition and disability
3. Minority status and language
4. Housing type and transportation
The higher the ranking, the more socially vulnerable the community is compared to other communities.
How to Use
The SVI data are displayed on an interactive map and can also be downloaded for a more granular look
into what determines a county or census tract’s SVI.
Applying the Data
Communities with higher SVI values have been disproportionately affected by COVID-19 both in terms
of new cases and deaths. Often these communities face greater structural barriers to vaccination. Early
in the vaccine rollout, counties with high social vulnerability had lower COVID-19 vaccination coverage
than did counties with low social vulnerability. Efforts to increase vaccine access, confidence and
demand can be prioritized for these communities to decrease inequities.

Walk a Mile Exercise
The Walk a Mile (WAM) interactive exercise invites participants to “walk a mile” in the shoes of the
population of focus in their journey to vaccination, recognizing that each population may have
unique context and experiences. Barriers and facilitators to COVID-19 vaccination for specific
populations are identified.
About
The WAM exercise identifies these key steps in the vaccination process:
1. Knowledge, awareness, and beliefs
2. Intent
3. Preparation, cost, and effort
4. Point of service
5. Experience of care
6. After service
Factors at the individual, community, societal, and political level impact vaccine access, confidence
and demand at each of these stages and should be considered throughout the exercise.
FIGURE 1: Walk a Mile Graphic
Modified from UNICEF Journey to Health,
ESARO Network Meeting 2019
9
How to Use
The exercise is designed to be completed in small groups that are familiar with the population of
focus. This may include health department staff, community- or faith-based organizations, community
leaders, and others. A facilitator guides a group conversation while people play the roles of members
of the community of focus; brainstorming their enablers and barriers at each point along
the vaccination journey. If you would like a guide to conduct the WAM exercise, please email
confidenceconsults@cdc.gov.

10
FIGURE 2: Example of Completed WAM Exercise
Applying the Data
The responses from the WAM exercise give insight into how the vaccination journey is unique to
each population. For each population, the exercise generates a list of perceived and actual barriers
and facilitators. Understanding this can lead to identifying appropriate strategies to try to increase
vaccine confidence and uptake.

11
Diagnostic Tool to Identify Factors and Strategies
About
The diagnostic tool (see Appendix C) can be used for guided conversations to assess factors related to
vaccine confidence and uptake in a specific population and identify strategies to address challenges.
FIGURE 3: Example of Diagnostic Tool Questions
How to Use
The factors that build vaccine confidence, intention, and demand are located in the left column of the
tool. Questions related to the assessment of the factors are provided for each. If the answer to
the assessment question is yes, move to the next factor. If the answer to the question is no, proceed to
the “Considerations” column. If sufficient information is available to talk through the considerations,
proceed to the “Recommended Strategies” column.
This tool is designed to be used by anyone working to increase vaccination in a specific population.
The participants in the guided conversations could include health department staff, community- or
faith-based organizations, community leaders, and others.
The tool can be used with large or small groups. The key is to have people involved in the discussion
who know the most about the population of focus and the vaccination process.
Applying the Data
Once the recommended strategies have been identified, teams can think through how to design,
implement, and evaluate these interventions.

12
Rapid Community Assessment
In attempting to apply the tools above, an organization might find that they do not have enough
information to identify barriers and facilitators related to vaccine confidence or demand. An
organization might also consider it necessary to conduct a more in-depth community assessment to
determine the status of vaccine confidence or demand in their communities. In either case, the Rapid
Community Assessment (RCA) Guide can help identify and address these challenges.
About
The RCA can be used by staff of any organization working to increase COVID-19 vaccine uptake who
wish to better understand the needs of the population of focus.
Use of this tool will help an organization to:
• Identify populations of focus at risk for low COVID-19
vaccine uptake.
• Gain an understanding of what people in the community
think about COVID-19 vaccines, as well as plan for
potential solutions to increase confidence and uptake.
• Identify community leaders, trusted messengers, and other
important channels to reach populations of focus.
• Identify areas of intervention and prioritize potential
intervention strategies to increase confidence in and
uptake of COVID-19 vaccine.
How to Use
The RCA consists of five steps:
1. Identifying objectives and community(ies) of focus
2. Planning for the assessment
3. Collecting and analyzing data
4. Reporting findings and identifying solutions
5. Evaluating your efforts
Given the urgency of the COVID-19 pandemic, the suggested
timeframe to complete the assessment is three weeks. The
RCA guide provides a step-by-step process for the assessment
as well as tools and scripts. The guide is available in English
and Spanish.
Applying the Data
The data collected through the RCA will increase your
understanding of what communities are thinking about COVID-19 vaccines, and help you plan
potential solutions to increase vaccine confidence and uptake. The data can also reveal previously
unrecognized leaders and trusted messengers through whom you can reach community members.

13
Vaccine Confidence
and Uptake Strategies
Below are selected strategies to increase
vaccine confidence and uptake drawn from
historical vaccination efforts and supported
by positive outcomes from evaluation
research. Examples from communities
currently using the strategies to increase
COVID-19 vaccine confidence and uptake
are included.
State and local health departments,
community- and faith-based organizations,
and local nonprofits are encouraged to try a
combination of these strategies to increase
vaccination rates.
Links to learn more about
how communities have
addressed challenges and
implemented the strategies
are included in Appendix A.

Vaccine
Ambassadors
Medical
Provider Vaccine
Standardization
Medical
Reminders
Motivational
Interviewing
Financial
Incentives
School-Located
Vaccination
Programs
Home-Delivered
Vaccination
Workplace
Vaccination
Vaccination
Requirements
Effective Messages
Delivered by Trusted
Messengers
Provider
Recommendation
Combating
Misinformation
14

Strategy 1
Vaccine Ambassadors
Vaccine ambassadors are a derivative of the lay health advisor (LHA)
model, which trains community members to disseminate important
health information in their communities. Ambassadors are most
effective when they are trusted community members and share
similar beliefs and characteristics with their peers.
Barriers Addressed: Equity, access, prevailing social norms, mistrust,
misinformation, cultural relevance.
Research Base: Framing vaccine uptake as a prevailing social norm
has a positive impact. A survey study showed that when people
think that most people around them want to be vaccinated, they are
more likely to be vaccinated as well. Discussing with peers the risk
of contracting disease and the decision to vaccinate impacts one’s
decision. Endorsements from peers in one’s own social network can
also help spread credible information about the vaccines.
COVID-19 Application Examples
Location: San Francisco, CA
Population of Focus: Latino Persons
The “Motivate, Vaccinate, and Activate” campaign
encouraged residents of the under-resourced,
predominantly Latinx Mission District of San Francisco,
California, to be vaccinated against COVID-19. The culturally
tailored initiative was organized through a community-
academic-city public health partnership among Unidos en
Salud (United in Health), the University of San Francisco, and
the City of San Francisco. They engaged trusted messengers,
social networks, and used a convenient vaccination site
to increase vaccination uptake and overcome hesitancy
due to misinformation, distrust of institutions, and access
to the vaccines. Community health workers educated the
community about the vaccines, texted people to let them
know of their eligibility, and used public media to spread
the word about vaccination locations.
Vaccinated community members became ambassadors
to recruit friends and family members to get vaccinated.
Important steps in this strategy included:
15
Combating
Misinformation
Vaccination
Requirements
School-Located
Vaccination
Programs
Medical
Reminders
• Two dedicated staff shared their personal experiences
modeling how this could be done.
• Staff then encouraged others to share their own
vaccination experiences with their unvaccinated friends
and family to encourage them to become vaccinated.
• Staff provided tips on how to handle difficult
conversations, provided myth-busting information,
and role played.
Outcome: Of those who were fully vaccinated, 91% of
survey respondents reported that they later recommended
vaccination to one or more unvaccinated people they
knew; 83% stated that they motivated one or more others
to be vaccinated; and 19% reported that they motivated
six or more others. During a 16-week period, the campaign
administered 20,792 vaccines at the neighborhood site.
Where to Start: Learn more about how the community implemented this strategy to use social
networks to boost vaccination coverage.

16
Location: Philadelphia, PA
Population of Focus: African American or Black Adults
A partnership between two health systems and community leaders in Philadelphia established COVID-19
vaccination clinics to overcome equity barriers among communities of color. Faith and other community
leaders were engaged as vaccine ambassadors who helped design the intervention, activated their
networks, and were trusted messengers to increase vaccinations. The strategy used other components
in addition to the vaccine ambassadors including a no- to low-tech approach to vaccine scheduling,
text or phone reminders of future vaccine appointments, and personal outreach.
Outcome: The program was designed and launched with just 2 weeks of planning. Three 7-hour clinics
vaccinated 2,821 people, 85% of whom were Black. Second dose clinics operated with an overall 0.6%
no-show rate.
Key components of this effort included:
• Health system leaders met virtually with area pastors to ensure they felt comfortable recommending
the COVID-19 vaccines.
• The pastors led by example and received their first doses at the clinic.
• During a virtual event held by two faith leaders for their congregations, Black physicians shared
their vaccination stories, provided scientific information about the vaccines, and answered
people’s questions and concerns. The event was recorded for future use by new partners, including
community organizations and health workers, senior centers, salons and barbershops with
predominantly African American or Black customers and staff, as well as WURD, a Black-owned
and operated talk radio station that aired segments about the COVID-19 vaccines and the
community clinic initiative.
Where to Start: Learn how this effort was implemented in Philadelphia including details on all the
components and lessons learned.

17
Strategy 2
Medical Provider
Vaccine Standardization
Medical provider vaccine standardization refers to offering
vaccination as a default option during patient visits and
integrating vaccination into medical practice procedures.
Barriers Addressed: Policy, mistrust, health literacy
Research Base: Medical practices and hospitals can take steps
to increase vaccine uptake through standard practice measures,
including default scheduling and presumptive announcements. In one
study, scheduling patients by default increased u vaccination by 10
percentage points. Another study showed patients with standing orders
received u and pneumococcal vaccines signicantly more often than
those with reminders. For patients with standing orders, the hospital’s
computerized system identied eligible patients and automatically
produced vaccine orders directed to nurses at the time of discharge.
Even standardizing what the doctor says when entering the room can
impact vaccine uptake. Doctors trained to announce human papilloma
virus (HPV) vaccines during visits with a brief statement that assumed
parents were ready to vaccinate (the presumptive approach) increased
uptake by 5.4% over the approach of engaging parents in open-ended
conversations about vaccinating their child.
COVID-19 Application Examples
Location: Arizona
Population of Focus: Adults
In Arizona, a local 10-physician practice received detailed
guidance from their county health department that helped
them obtain vaccine supply and establish a protocol for
administration. The county health department provided
both supplies and instructional webinars on a weekly
basis to guide practices through the process of becoming
vaccinators. The Arizona physician office trained their staff
to provide accurate information to patients who call with
questions and developed a new scheduling system to
standardize outreach and scheduling for eligible patients.
Because their office space was too small to monitor patients
for post-vaccine allergic reactions during normal business
hours, they organized special weekend vaccination clinic
hours. Yet, the groundwork has been laid for integrating
vaccination into routine practice.
Standardization measures could become routine
practice. Currently, many primary care and specialty
physician offices are not offering COVID-19 vaccines.
That is expected to change as logistical barriers are
overcome and more physician practices become
involved in the “last mile” effort to vaccinate everyone
eligible, particularly in states where state and local
health departments provide support. As the vaccines
become more available in medical practices and
hospitals, standardizing COVID-19 vaccination into
routine practice will help reduce missed opportunities
for vaccination, which are encounters during which a
person eligible for a vaccine receives health services
that do not result in them getting vaccinated.
Where to Start: The Arizona Department of Health
Services Immunization Program in partnership with
The Arizona Partnership for Immunization, a non-
profit coalition, has a free training series to improve
vaccination practices in providers’ offices. Trainings
cover areas including vaccine friendly office practices,
vaccine handling and storage, shot administration.

18
Strategy 3
Medic al Reminders
Medical reminders are messages sent to patients to remind them
of recommended or upcoming treatment. Messages can be sent by
autodialed phone calls, text messages, or post-cards, for example.
Barriers Addressed: Equity, access, forgetfulness, friction, health literacy,
lack of adequate information
Research Base: Reminders of upcoming vaccination appointments can
increase vaccination rates. This intervention is often part of a multi-pronged
approach combined with removing access barriers to optimize uptake. Duval
County Health Department in Florida successfully increased vaccination
rates by using data from the Florida Shots Registry to identify families with
upcoming vaccinations due or who were behind on their child’s vaccinations
and sending them reminders and educational materials through phone calls,
letters, and home visits.
A study in Rochester, New York, showed that when interventions were
combined to include patient reminders, provider reminders, and telephone
outreach, older adults in the intervention group were up to six times as likely
to be vaccinated against u.
A University of Pennsylvania study found that simple reminder text messages
sent to 47,306 patients in two health systems increased u vaccinations by
around 5%. Of the 19 dierent messages tested, those most likely to “nudge”
patients to be vaccinated were presented in a professional format and
tone—not casual, surprising, or interactive. The most successful messages
reminded patients twice to get their shot at their upcoming doctor’s
appointment and stated that a vaccine was already reserved for them.
COVID-19 Application Examples
Location: Multiple U.S. Locations
Population of Focus: Adults
Several state and local health departments, including in
Michigan, Oklahoma, and Baltimore, Maryland, are using
text messages to:
• Help people schedule their vaccine appointments
• Provide education and vaccination site information
• Gauge views on vaccination
Certain populations can be reached with messaging,
either based on race, ethnicity, or age, or used in geogr
aphic
locations with lower vaccination uptake. In most cases, texts
are provided in English and Spanish, but health departments
or other entities sending texts can translate and customize
to any language spoken in their community of focus.
This can also be used to remind people of their second
vaccination appointment, if applicable.
Many text-based services are available. Some, like
CareMessage, offer a free model for nonprofits to help
with COVID-19 vaccination. CDC recommends that
providers without a text-message system offer their

19
patients the COVID-19 text reminder service, VaxText℠, which is free to providers and patients.
After enrolling in VaxText℠, people who have received the first COVID-19 vaccine dose receive
weekly text reminders in English or Spanish about their second dose or a reminder that they are
overdue, if applicable.
Well-crafted emails containing behavioral nudges can also be used as reminders to get vaccinated.
A large Pennsylvania health system found that after a five-week effort to have employees
vaccinated against COVID-19, 41% still had not scheduled their vaccination. They found through
a study that individually addressed emails containing behaviorally informed messages increased
vaccination registration.
The emails had three important components:
• Told the healthcare worker that vaccines would soon be available more broadly, thus, reducing
employees’ access and emphasizing scarcity.
• Contained a message either about social norms, saying that many fellow employees had already
chosen to be vaccinated; or about risks, comparing the risk of vaccination with the risk of COVID-19.
• Asked employees to make an active choice by clicking through to schedule their vaccination
appointment.
Where to Start: Learn the details on how this reminder effort was implemented.

20
Strategy 4
Motivational
Interviewing
Motivational interviewing refers to patient-centered conversations
designed to increase patient motivation and likelihood of health
behavior uptake.
Barriers Addressed: Misperception, health literacy, uncertainty
Research Base: Motivational interviewing aims to support decision
making by strengthening a person’s intention to vaccinate based
on their own arguments. The healthcare professional informs about
vaccination in alignment with the individual’s specic informational
needs and with respect for their beliefs. Motivational interviewing has
been shown to decrease parental vaccine hesitancy. A pilot study of
using motivational interviewing in maternity wards during postpartum
stays found the strategy led to a 15% increase in mothers’ intention to
get their child vaccinated, a 7% increase in infants’ vaccination coverage
at seven months, and a 9% greater chance of complete vaccination
at 2 years. Motivational interviewing was also found to signicantly
improve HPV vaccination completion among adolescent patients in a
study that employed an intervention of using a presumptive vaccine
recommendation with motivational interviewing follow up for parents
who remained resistant. Some healthcare providers have concerns that
this approach takes too long and that such a conversation is not billable.
COVID-19 Application Examples
Location: Western Pennsylvania
Population of Focus: Adults
Motivational interviewing can be a strategy to promote
COVID-19 vaccine uptake. A demonstration project in the
Pittsburgh area showed that innovative notification and
motivational interviewing strategies at a regional chain
supermarket pharmacy increased the number of herpes
zoster, flu, pertussis, and pneumococcal vaccines given to
adults. Community pharmacies are accessible and able to
provide COVID-19 vaccinations to many customers, along
with their other patient-centered products and services
and may be able to model programs similar to this.
Pharmacy staff identified the patient, who then received
an automated notification about their vaccination status.
The staff used motivational interviewing techniques face-
to-face or by telephone to engage patients in conversation
about getting vaccinated.
Outcome: The 99 pharmacies in western Pennsylvania that
took part in the project saw a 33% increase in vaccinations
over the prior year: 45% for flu, 31% for pertussis, and
7% for pneumococcal vaccinations, while herpes zoster
vaccinations dropped by 5%.
Where to Start: Scripts for using motivational interviewing with those who may be COVID-19 vaccine
hesitant are available.

21
Strategy 5
Financial Incentives
Financial incentives aim to motivate people to participate in a health
behavior by providing a tangible reward, or a chance at a tangible
reward, for completion of the behavior.
Barriers Addressed: Inertia
Research Base: While evidence supporting the use of incentives to increase
vaccine uptake is overall limited, the type that appears eective is of a
guaranteed gift incentive. For example, oering a $30 incentive increased
vaccination rates at college campus clinics according to one study. Recent
studies of the Ohio COVID-19 vaccine lottery have been less positive,
showing the likelihood that the approach has not increased vaccine uptake.
Clearly, these are two dierent approaches—one is a guaranteed gift and the
other a chance at winning. Also, the audiences dier with the rst comprised
of young adult college students and the latter a general population.
COVID-19 Application Examples
Location: Multiple U.S. Locations
Population of Focus: Adults and Youth
• West Virginia state government is offering residents
ages 16 to 35 who have been vaccinated a choice of
receiving either a $100 savings bond or a $100 gift card.
The governor estimates this might cost the state up to
$20 million.
• California offered $50 in the form of a virtual Mastercard
or grocery gift card to residents who started their
vaccination series between May 27 and July 18. The
money is limited to the first 2 million requests, which
limits the total cost to the state.
• Employers are also offering cash incentives to their staff.
Maryland state employees will receive $100 and the
Colorado Department of Corrections will provide $500
to staff who elect to get vaccinated.
• Many large private corporations are also providing cash
incentives to employees, often ranging from $75 to
$500 including Amazon, Kroger, PetCo, AutoZone, and
Bolthouse Farms.
• Many businesses are offering free products to those who
have been vaccinated, including the well-publicized
free Krispy Kreme donut. Several states are offering
free admission to state parks or similar incentives for
vaccinated visitors. Offers like these non-monetary
guaranteed incentives have not been well-studied for
effectiveness.
Where to Start: The Equal Employment Opportunity Commission (EEOC) provides
guidance to employers on offering incentives to employees for becoming vaccinated.
For ideas on incentives to offer, see the list of state and local government incentives
maintained by the National Governors Association.

22
Strategy 6
School-Located
Vaccination Programs
School-located vaccination programs are events held at a school
campus to remove logistical barriers and increase vaccine uptake.
These can be open to students only, or offered to faculty, families,
and the greater community as well.
Barriers Addressed: Access, friction, prevailing social norms,
uncertainty, lack of adequate information
Research Base: Voluntary school-located vaccination programs have
demonstrated high coverage, though they are not without challenges.
One of the major challenges is obtaining informed parental consent
when needed. School-located programs can be eective even with
“controversial” vaccinations such as for HPV. The setting also has been
shown to yield higher completion rates of multi-dose vaccine series as
compared to community health center settings.
COVID-19 Application Example
Location: St. Louis County, Missouri
Population of Focus: School-age Youth
School districts of many sizes across the country are holding
COVID-19 vaccination events. One of the first school districts
to do so was the Parkway School District in St. Louis County,
Missouri, which held their event on April 26, 2021. The event
was held in partnership with a local pharmacy. In a survey,
350 parents said they were interested, and the 204 students
who were vaccinated at the event represented about 5% of
eligible students in the district.
Timing of the event may have affected turnout because
some expressed concern about the second dose occurring
during the week of finals for some students, according to
the Interim Health Services Director who led the effort. The
director also noted that school nurses are trusted sources of
health information and play an important role in educating
students and families about the COVID-19 vaccines. Two
additional vaccination clinics have been held, one just days
after the U.S. Food and Drug Administration authorized the
Pfizer-BioNTech vaccine for those 12 years and older.
While this strategy has focused on vaccinating students
through school-located vaccination programs, school
settings may also be ideal locations for community
vaccination events. Much for the same reason schools are
often used as voting locations, they generally are easily
accessible, have ample parking, have both indoor and
outdoor spaces available, and are familiar places.
Outcome: So far, Parkway School District has vaccinated
nearly 3,000 students through their three on-site clinic
events. This was made possible, in part, due to their
excellent relationship with a local pharmacy, which
will pave the way for possible future student vaccination
events should a vaccine be approved for younger
school-age children.
Where to Start: The school district documented their
lessons learned as guidance for other school districts
noting the importance of details such as:
• Ensuring Ample Parking
• Working Around Educational Schedules
• Obtaining Consent
• Training Staff
• Managing Vaccine Delivery and Storage

23
Strategy 7
Home-Delivered
Vaccination
Home-delivered vaccination efforts reach populations where
they are; traditionally used when barriers to transportation
and access exist.
Barriers Addressed: Equity, access, inertia, friction
Research Base: Bringing vaccines to where people are, including
in their homes, is an eective means to reach several hard-to-reach
populations. This strategy can be applied to people who are bound to
their homes as well as to neighborhoods with low vaccination rates.
In an eective eort in New York City, individuals canvassed specic
communities to educate people about the u vaccine and oered
it to people on the spot. They focused on those with substance use
disorders, immigrant populations, older adults, sex workers, and
people experiencing homelessness. Both appointment-based home
delivery and canvassing methods may be eective ways to deliver
COVID-19 vaccines.
COVID-19 Application Example
Location: Multnomah County, Oregon
Population of Focus: Adults
As the COVID-19 vaccination effort progresses, shifts are occurring from mass vaccination sites to
smaller neighborhood and community clinics, and now to home-based efforts to do everything
possible to give all individuals the opportunity to get vaccinated. The Emergency Operations Center in
Multnomah County, Oregon, has partnered with the Public Health Division and County Human Services
to provide COVID-19 vaccinations through a mobile program reaching people where they live. Initially
vaccinating those in adult care homes, they have expanded the project’s scope to include other adults
who are homebound.
The county’s mobile door-to-door COVID-19 response team pairs Medical Reserve Corps volunteers,
who are licensed medical practitioners, and other volunteers to assist in providing COVID-19
vaccinations to people in their homes. The goal of the response, launched in February 2021, is to
vaccinate up to 5,000 people. “Getting to meet people ‘where they are at’ and administering a life-
saving vaccine is an incredibly powerful experience. It truly brought people hope. The coordination
it takes to make this kind of outreach happen is no small feat – but it’s precisely the kind of work we
need to do in order to respond quickly to inequalities and gaps in vaccine distribution, especially for
those who are most vulnerable,” said Dr. Sharon Meieran, a Medical Reserve Corps volunteer.
Where to Start: CDC provides guidance for implementing home-bound and residential living
COVID-19 vaccination including consideration for training requirements, planning, storage and
handling, and administration.

Strategy 8
Workplace
Vaccination Programs
24
A vaccination event held on-site at a workplace to remove logistical barriers and create norms.
This can be open to emplo
yees only or extended to family members or the greater community.
Barriers Addressed: Access, cost, prevailing social norms, friction
Research Base: Numerous studies have shown that vaccination programs at the worksite can increase
vaccination rates among workers and their families. In one study, where u vaccination rates increased
signicantly after the intervention, 90% of vaccinated employees received a vaccine at employer-sponsored
events. The most important reasons employees reported for being vaccinated at work were not related to
health, but that the vaccine was free, convenient, and would help them avoid being absent from work.
There is evidence on-the-job COVID-19 vaccines may have similar uptake success. A recent Kaiser Family
Foundation study found that 23% of Americans would be more likely to get a vaccine if it was available
at their workplace. Another recent survey of employees by McKinsey & Company found an even greater
potential return with 83% of those surveyed saying oering on-site vaccinations would signicantly (49%)
or moderately (34%) increase the likelihood that they would get a COVID-19 vaccine. According to a 2020
Gallup poll, small businesses are one of the most trusted institutions in the U.S.
COVID-19 Application Example
Location: Midwest; Jackson, Mississippi
Population of Focus: Adults
Tyson Foods is offering on-site vaccination at many of their
facilities. In Iowa and Illinois, the company partnered with
the Midwest grocery chain Hy-Vee and state and local public
health departments to vaccinate food processing workers
at four locations in the two states. Workers in that industry
have been hit hard by COVID-19 and were extremely excited
for the opportunity. The workers are diverse, with one
facility requiring vaccine education information translation
in 18 languages. Tyson Foods also offered workers up to four
hours of regular pay if they needed to get their vaccine(s)
outside of a normal shift or away from the jobsite.
Outcome: By early March 2021, Hy-Vee staff had vaccinated
over 2,400 employees in one of the states.
Small businesses can also support on-site vaccination
efforts. In Jackson, Mississippi, the Broad Street Baking
Company partnered with the Mississippi State Department
of Health and the G.A. Carmichael Family Health Center to
hold mobile vaccination events in a parking lot near the
restaurant in April and June 2021.
Outcome: At both events, vaccines were given to all
employees and other attendees who requested them.
Where to Start: CDC offers guidance to state, tribal, and local jurisdictions on reaching out to worker
populations to increase vaccine uptake. This includes how to talk with small businesses and special
considerations for rural communities and migratory workers. CDC also has information for employers
on how they can support vaccination of their workforce.

Strategy 9
Vaccination
Requirements
Vaccination requirements are policies that require employees, students,
or patrons to be vaccinated and provide proof of vaccination in order to
be in compliance.
Barriers Addressed: Policy, inertia, prevailing social norms, politicization
Research Base: Vaccine requirements at the organizational level may be an
eective way to increase vaccination rates and decrease disease incidence.
Requirements by employers or schools ask that employees or students provide
proper documentation of vaccination to comply with the organization’s
vaccination policy. Exemptions can be oered for specic circumstances,
such as medical and religious reasons. Vaccination requirements have not often
been used for adult populations, with the exception of military requirements
and for healthcare workers to receive u shots. There is evidence showing
school mandates positively impact uptake for routine childhood vaccines
and some studies suggest that vaccination for children and workers, including
mandatory vaccination, decreases absenteeism.
COVID-19 Application Example
Location: Multiple U.S. Locations
Population of Focus: Adults
Many employers and institutes of higher education such as universities
are requiring staff and students to be vaccinated against COVID-19. Large
companies have most recently required staff to be vaccinated to return
to the office. A number of federal, state and local governments are also
requiring vaccination for employees; some with an alternate option for
weekly testing for COVID-19 and some without that option. Examples of
early adopters of vaccination requirements are provided below.
Houston Methodist Health System: Houston Methodist was the first health
system in the country to mandate COVID-19 vaccination for all employees
to protect their patients and workforce. The health system is made up of an
academic medical center and six community hospitals employing over 26,000
people. The first phase of the policy included managers and new hires and
was gradually rolled out to all staff. Those not in compliance received a two-
week suspension during which they could get vaccinated. Several employees
pushed back on the requirement and took the hospital system to federal court.
The Texas court dismissed the lawsuit and upheld the vaccine requirement
stating that the requirement does not break any laws and is in line with
public policy.
Outcome: Houston Methodist achieved nearly 100% compliance with 24,947
workers being vaccinated. Medical and religious exemptions were granted to
over 600 employees and only 153 employees out of 26,000 (.5%) resigned or
were fired for not complying.
25

Morgan Stanley Office Vaccine Policy: Morgan Stanley created a policy requiring all employees returning
to their offices to be vaccinated. It also extends to clients and visitors to their two New York offices. The
company views this policy as a way to create a safe and normal office environment that allows employees
to forgo masks and social distancing. Employees who remain unvaccinated have the option of working
from home, but the company is strongly encouraging employees to come back into the office.
Where to Start: The policy and procedures Houston Methodist put in place is publicly available and can
be used as a model for other employers wanting to require COVID-19 vaccines. Other legal organizations
also have templates available online as found in Appendix A.
26

27
Strategy 10
Effective Messages
Delivered by Trusted Messengers
Effective messages are messages that have undergone testing with
the intended population and were shown to produce the desired
outcome. Trusted messengers are people seen as credible sources
of information by specific populations. Trusted messengers can be
trained to be vaccine ambassadors (see Strategy 1) and may include
experts.
Barriers Addressed: Mistrust, health literacy, misinformation, lack
of adequate information
Research Base: The messengers and messages used to convey
information about vaccines are important to improving vaccine
condence.
The COVID-19 States Project Report evaluates results from two
experiments designed to test eective communication strategies for
increasing COVID-19 vaccine condence and intent. The rst experiment
tested ve messages and a control message for the eect it had on
participants’ willingness to receive a COVID-19 vaccine. The messages
involved themes of patriotism, harm reduction, social norms, scientist
recommendation, and physician recommendation. The study found
that messages involving a personal physician or a scientist
recommending vaccination were the most compelling. The second
experiment looked at messenger eectiveness and found that messages
delivered by politicians increased resistance to vaccination while
those delivered by physicians or scientists showed increased vaccine
condence and intent.
Messages and messengers should be continually evaluated
for eectiveness and tested across populations with dierent
demographics. Continued evaluation of messages allows
communication campaigns to tailor messages to specic concerns
and demographic populations, which is shown to be more eective
than generalized messaging.

28
COVID-19 Application Example
Location: Multiple U.S. Locations
Population of Focus: Adults
The Black Coalition Against COVID, The Kaiser Family Foundation, and Esperanza Hope for All created
a COVID-19 vaccine communications campaign called “The Conversation,” which uses the hashtag
#BetweenUsAboutUs. The campaign features 50 videos of Black and Latino doctors, nurses, and scientists
talking about vaccine facts and dispelling misinformation. In addition to the videos, the campaign oers
graphics, print media, social media content, and TV and radio PSAs. The content is free for educational
use and communities and organizations are invited to download and utilize their materials in English and
Spanish. Some content features doctors sharing why they got vaccinated. One graphic shows a female
Black doctor with the quote, “When we get enough people vaccinated, we’re going to see the death rates
go down. Then we’re going to see the hospitalization rates go down.” Currently, the campaign’s videos have
over 21,000,000 views on YouTube.
Where to Start: For specific messaging language tips based on COVID-19 messaging research, see the
deBeaumont Foundation’s Tip Sheet.

Strategy 11
Provider
Recommendation
Provider recommendation refers to healthcare professionals
suggesting that a patient receive a COVID-19 vaccination.
Barriers Addressed: Inertia, friction, mistrust, uncertainty,
mis- and disinformation, lack of adequate information
Research Base: Provider recommendations have strong support for increasing
vaccination. The Advisory Committee on Immunization Practices includes
this strategy in their recommendations for improving vaccination rates.
Some people may have more trust in their own doctor than in the medical
community in general. Research on vaccinations in pregnant people found
that provider recommendation shows increases in vaccination rates and when
coupled with oering the vaccination during doctor’s oce visits, doubles
the likelihood of uptake. In a study of u vaccination in adults, patients who
received provider recommendations with an oer of vaccination were 1.76
times more likely than those who did not receive a recommendation to be
vaccinated. Those receiving only a recommendation were 1.72 times more
likely than those who did not receive a recommendation to be vaccinated.
The HPV vaccine, which relies on healthcare professionals for distribution,
depends on provider recommendations for adequate coverage. A study
on low HPV vaccination rates in North Carolina, found that lack of provider
recommendations contributed to under vaccination in the population.
COVID-19 Application Example
Location: New York, New York; Philadelphia, Pennsylvania
Population of Focus: Adults
The New York City Department of Health and Mental
Hygiene created a resource called Vaccine Talks that
emphasizes the importance of healthcare professional
recommendations in increasing COVID-19 vaccination rates.
Vaccine Talks offers resources for healthcare providers and
their staff to recommend and offer COVID-19 vaccination
at multiple points of interaction with patients. The health
commissioner released a statement promoting Vaccine
Talks that places emphasis on the trust patients have
in their healthcare providers and says that their strong
recommendations for COVID-19 vaccines will help drive
vaccination rates in the city.
Vaccine Talks includes a resource called the “Use Every
Opportunity” tool instructing healthcare offices on how
to integrate COVID-19 vaccine education and offers into
all healthcare settings. Vaccine Talks also includes a link
to a form the provider can complete to request that the
public health system contact the patient to schedule their
vaccination at a clinic or in their home if needed.
29
Emergency departments and urgent care facilities are
important locations for COVID-19 vaccine provider
recommendations due to the high number of patients seeking
routine care in these settings. The Philadelphia Department
of Public Health put out a call to emergency facilities in the
city to begin recommending and administering COVID-19
vaccines to patients upon discharge. The notice focused on
postpartum discharges and patients being discharged to
long-term care facilities as key demographics for provider
recommendations and offers. They provided best practices
for vaccination during patient discharge.
Where to Start: The Vaccine Talks resources include
scripts for physicians to talk to their patients about
COVID-19 vaccines, including talking to parents of
eligible children, and other tools for physicians
to support vaccine confidence building with staff
and patients.

30
Strategy 12
Combating
Misinformation
Tactics used to address and dismantle misinformation and disinformation. Misinformation refers to the
sharing of false information and disinformation refers to information that is deliberately misleading and
intended to manipulate a narrative.
Barriers Addressed: Misperception, mis- and disinformation, lack of adequate information
Research Base: Believing incorrect information can act as a barrier to vaccine uptake. Vaccine myths are
particularly dicult to combat, in part because people tend to believe information that is in line with their
existing attitudes and worldview. Fact-checking and debunking appear to be eective tools to counteract
the eects of misinformation, particularly when the correct information sources are universities and health
institutions. Debunking incorrect information with messages that reect the worldview and arm the values
of the intended audience may be the most successful approach. Debunking misinformation is challenging.
Misinformation is often simple and more cognitively attractive than fact, and refuting a falsehood often
requires repeating it, which reinforces the falsehood in the believer. Techniques that help dispel falsehoods
include warning the audience upfront that misleading information is coming, using fewer arguments to
refute the myth, and keeping the factual statements simple.
Everyday social media users can play an important part in correcting misinformation. While the person
originally expressing the misinformation may not be moved because the correction does not align with
their world view, others see the correct information and are impacted by it. Responding with empathy
and providing facts, rather than simply saying something is wrong, are tips for eective corrections.
COVID-19 Application Examples
Location: Multiple U.S. Locations
Population of Focus: Adults
Public Good Projects (PGP) is a public health non-profit
organization with a mission to stop the spread of vaccine
misinformation through evidence-based media monitoring,
behavioral interventions, and cross-sector initiatives. In
the beginning of the COVID-19 pandemic, PGP created a
misinformation tracking system to monitor misinformation
being shared about COVID-19 and later about the vaccines.
Using this tracking system, PGP pinpointed ideas that could
pose a threat to public health measures and worked with
scientists to create evidence-based responses. To combat
the misinformation, PGP identifies micro-influencers with
audiences who have high rates of vaccine hesitancy and
equips them with science-backed messages to share with
their social networks. Their vaccine-hesitant followers are
more likely to accept this information when it comes from
someone they trust rather than from a health expert.
Where to Start: Dissemination of factual and
easy to understand information comba
ts mis- and
disinformation. This can be done in a variety of
ways including identifying and training social media
micro-influencers in your community as PGP is doing
nationally or using your own social media to promote
accurate information. To keep your finger on the pulse
of social media misinformation nationally you can
refer to the Virality Project’s weekly briefing. To
monitor your local social media, you can utilize
the RCA’s Social Listening and Monitoring Tool.
31
Conclusion
Reaching universal COVID-19 vaccination coverage
in the United States is a monumental challenge.
There are barriers impeding both vaccine confidence
and uptake. Structural barriers, such as time costs
and transportation, lead to inequitable vaccine
distribution, often negatively affecting populations
that have been disproportionately affected by the
pandemic. People’s behaviors and beliefs, often
based on misinformation or low health literacy,
can obstruct their willingness to get vaccinated,
while other human nature factors make it difficult
to motivate people to do something difficult, new,
or unfamiliar. COVID-19 vaccination and pandemic-
related information can be perceived as complex and
sometimes contradictory, adding yet another barrier.
Compounding all of this is the current politicization
of getting vaccinated.
Understanding the specific barriers your community
of focus faces will help you identify and initiate
activities that will help overcome those barriers.
Tools, including the SVI, WAM Exercise, and the
diagnostic tool, can help to identify populations
disproportionately affected by the pandemic and
the barriers and facilitators to vaccination they face.
The RCA Guide offers in-depth resources to help you
quickly learn more about needs related to COVID-19
vaccination in your community of focus.
While the COVID-19 vaccination effort is unique
in many ways, applying best practices and lessons
learned from previous vaccination efforts increases
the likelihood of overcoming vaccine hesitancy and
improving vaccine uptake. There is no magic formula
to addressing vaccination barriers—communities
need to employ multiple tailored strategies and
tactics. The examples offered in this guide can serve
as inspiration as well as practical guidance. Each
community will need to customize its approaches to
harness available resources to meet local needs.

32
Appendix A
References and Resources
To learn more about each of the strategies discussed in this guide, the research supporting them,
and information on how to implement them in your community, see the resources below.
Common Barriers
The Behavioral and Social Drivers (BeSD) of COVID-19 Vaccination Uptake
The Behavioral and Social Driver (BeSD) expert working group.
https://journals.sagepub.com/doi/full/10.1177/1529100618760521
Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing vaccination:
Putting psychological science into action. Psychological Science in the Public Interest, 18(3), 149-207.
Understanding Your Community
Social Vulnerability Index
The CDC/ATSDR Social Vulnerability Index (CDC/ATSDR SVI) uses 15 U.S. census variables to help local
officials identify communities that may need support before, during, or after disasters.
https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
SVI data is displayed on an interactive map.
https://svi.cdc.gov/map.html
RCA Guide and Tools
COVID-19 Vaccine Confidence Rapid Community Assessment Guide and tools.
https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence/rca-guide/index.html
Vaccine Confidence and Uptake Strategies
Strategy 1: Vaccine Ambassadors
Research Base
The influence of social norms on flu vaccination among African American and White adults.
https://doi.org/10.1093/her/cyx070
Quinn, S. C., Hilyard, K. M., Jamison, A. M., An, J., Hancock, G. R., Musa, D., & Freimuth, V. S. (2017). The
influence of social norms on flu vaccination among African American and White adults. Health education
research, 32(6), 473-486.
Attention, intentions, and follow-through in preventive health behavior: Field experimental evidence on flu
vaccination.
https://www.swarthmore.edu/sites/default/files/assets/documents/user_profiles/ebronch1/JEBO_2015.pdf
Bronchetti, E. T., Huffman, D. B., & Magenheim, E. (2015). Attention, intentions, and follow-through in
preventive health behavior: Field experimental evidence on flu vaccination. Journal of Economic Behavior &
Organization, 116, 270-291.
More Information About the COVID-19 Examples
A multi-component, community-based strategy to facilitate COVID-19 vaccine uptake among
Latinx populations: from theory to practice
https://www.medrxiv.org/content/10.1101/2021.06.07.21258230v1.full.pdf
Marquez, C., Kerkhoff, A. D., Naso, J., Contreras, M. G., Castellanos, E., Rojas, S., ... & Havlir, D. V. (2021).
A multi-component, community-based strategy to facilitate COVID-19 vaccine uptake among Latinx
populations: from theory to practice. MedRxiv.

33
Operationalizing Equity: A rapid-cycle innovation approach to COVID-19 vaccination in Black neighborhoods.
https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0094
Lee, K. C., Al-Ramahi, N., Hahn, LO., Donnell, T., Schonewolf, L. J., Khan, N., O’Malley, C., Ghatri, U. G.,
Pearlman, E., Balachandran, M., et al. (April 7, 2021). Operationalizing Equity: A rapid-cycle innovation
approach to COVID-19
vaccination in Black neighborhoods. NEJM Catalyst.
Additional Resources for Implementing this Strategy
San Francisco Department of Public Health’s community COVID-19 vaccine communication training for
ambassadors slide presentation.
https://www.sfdph.org/dph/files/ig/vaccine/vaccine-ambassador-training-pdf.pdf
Strategy 2: Medical Provider Vaccine Standardization
Research Base
Default clinic appointments promote influenza vaccination uptake without a displacement effect.
https://behavioralpolicy.org/wp-content/uploads/2017/06/chapman-web.pdf
Chapman, G. B., Li, M., Leventhal, H., & Leventhal, E. A. (2016). Default clinic appointments promote
influenza vaccination uptake without a displacement effect. Behavioral Science & Policy, 2(2), 40-50.
Inpatient computer-based standing orders vs physician reminders to increase influenza and pneumococcal
vaccination rates: a randomized trial.
https://jamanetwork.com/journals/jama/article-abstract/199810
Dexter, P. R., Perkins, S. M., Maharry, K. S., Jones, K., & McDonald, C. J. (2004). Inpatient computer-based
standing orders vs physician reminders to increase influenza and pneumococcal vaccination rates: a
randomized trial. Jama, 292(19), 2366-2371.
Announcements versus conversations to improve HPV vaccination coverage: a randomized trial.
https://pediatrics.aappublications.org/content/pediatrics/139/1/e20161764.full.pdf
Brewer, N. T., Hall, M. E., Malo, T. L., Gilkey, M. B., Quinn, B., & Lathren, C. (2017). Announcements versus
conversations to improve HPV vaccination coverage: a randomized trial. Pediatrics, 139(1).
More Information About the COVID-19 Examples
The Room Where It Happens: Primary Care and COVID-19 Vaccinations.
https://www.commonwealthfund.org/publications/2021/jul/room-where-it-happens
Klein, S., Hostetter, M. (7 July 2021). The Room Where It Happens: The role of primary care in the next
phase of the COVID-19 vaccination campaign. The Commonwealth Fund.
The Arizona Department of Health Services Immunization Program in partnership with TAPI, a non-profit
coalition, has a free training series to improve vaccination practices in providers’ offices. Trainings cover areas
including setting up vaccine friendly office practices, vaccine handling and storage, shot administration.
https://whyimmunize.org/covid-19-vaccine-t-i-p-s/
Additional Resources for Implementing this Strategy
The Community Guide: Vaccination: Provider Reminders
The Community Guide: Vaccination: Standing Orders
Standing orders templates for administering vaccines
https://www.immunize.org/standing-orders/
CDC COVID-19 Vaccination Program Provider Requirements and Support
https://www.cdc.gov/vaccines/covid-19/vaccination-provider-support.html
Appendix A

34
Appendix A
The COVID-19 Vaccine Use Every Opportunity implementation tool provides strategies for ensuring COVID-19
vaccination is offered to every eligible patient during their encounters with your organization. The Use Every
Opportunity framework is an adaptable tool for implementing workflows to achieve the highest level of
COVID-19 vaccine coverage possible in all health care settings.
https://www1.nyc.gov/assets/doh/downloads/pdf/covid/providers/covid-19-vaccine-use-every-
opportunity-tool.pdf
Strategy 3: Medical Reminders
Research Base
The Community Guide in Action - A Good Shot: Reaching Immunization Targets for two-year-old’s in Duval
County, Florida.
https://www.thecommunityguide.org/sites/default/files/assets/Vaccinations-FL_0.pdf
Increasing inner-city adult influenza vaccination rates: a randomized controlled trial.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3113429/pdf/phr126s20039.pdf
Humiston, S. G., Bennett, N. M., Long, C., Eberly, S., Arvelo, L., Stankaitis, J., & Szilagyi, P. G. (2011).
Increasing inner-city adult influenza vaccination rates: a randomized controlled trial. Public Health
Reports, 126(2_suppl), 39-47.
A megastudy of text-based nudges encouraging patients to get vaccinated at an upcoming doctor’s
appointment.
https://www.pnas.org/content/118/20/e2101165118
Milkman, K. L., Patel, M. S., Gandhi, L., Graci, H. N., Gromet, D. M., Ho, H., ... & Duckworth, A. L. (2021).
A megastudy of text-based nudges encouraging patients to get vaccinated at an upcoming doctor’s
appointment. Proceedings of the National Academy of Sciences, 118(20).
More Information about the COVID-19 Examples
Pennsylvania health system email reminders
Santos HC, Goren A, Chabris CF, Meyer MN. Effect of Targeted Behavioral Science Messages on COVID-19
Vaccination Registration Among Employees of a Large Health System: A Randomized Trial. JAMA Netw
Open. 2021;4(7):e2118702. doi:10.1001/jamanetworkopen.2021.18702
Additional Resources for Implementing this Strategy
VaxText is a free text messaging platform that providers can offer to their patients. Patients can opt in to
conveniently receive text message reminders to get their second dose of COVID-19 vaccine.
https://www.cdc.gov/vaccines/covid-19/reporting/vaxtext/index.html
Strategy 4: Motivational Interviewing
Research Base
Motivational interviewing: A promising tool to address vaccine hesitancy.
https://pubmed.ncbi.nlm.nih.gov/32281992/
Gagneur, A., Gosselin, V., & Dubé, È. (2018). Motivational interviewing: A promising tool to address vaccine
hesitancy. Vaccine, 36(44), 6553-6555.
Effects of a Health Care Professional Communication Training Intervention on Adolescent Human
Papillomavirus Vaccination: A Cluster Randomized Clinical Trial.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5875329/
Dempsey, A. F., Pyrznawoski, J., Lockhart, S., Barnard, J., Campagna, E. J., Garrett, K., Fisher, A., Dickinson,
L. M., & O’Leary, S. T. (2018). Effect of a Health Care Professional Communication Training Intervention
on Adolescent Human Papillomavirus Vaccination: A Cluster Randomized Clinical Trial. JAMA pediatrics,
172(5), e180016. https://doi.org/10.1001/jamapediatrics.2018.0016

35
More Information about the COVID-19 Examples
Increasing adult vaccinations at a regional supermarket chain pharmacy: A multi-site demonstration project
Increasing adult vaccinations at a regional supermarket chain pharmacy: A multi-site demonstration
project - ScienceDirect
Coley, K.C., Gessler,C., McGivney, M., Richardson, R., DeJames, J., Berenbrok, L. A. (2020). Increasing adult
vaccinations at a regional supermarket chain pharmacy: A multi-site demonstration project. Vaccine,
38(24), 4044-4049. https://doi.org/10.1016/j.vaccine.2020.02.040.
Additional Resources for Implementing this Strategy
Communication Skills for Talking About COVID-19 Vaccines - These communication skills are designed for
clinicians to use with patients and families, using an approach adapted from motivational interviewing and
research on vaccine hesitancy.
https://www.capc.org/covid-19/communication-skills-for-talking-about-covid-19-vaccines/
Strategy 5: Financial Incentives
Research Base
Attention, intentions, and follow-through in preventive health behavior: Field experimental evidence on flu
vaccination.
https://www.sciencedirect.com/science/article/abs/pii/S0167268115001079?via%3Dihub#abst0005
Bronchetti, E. T., Huffman, D. B., & Magenheim, E. (2015). Attention, intentions, and follow-through in
preventive health behavior: Field experimental evidence on flu vaccination. Journal of Economic Behavior
& Organization, 116, 270-291.
Lottery-Based Incentive in Ohio and COVID-19 Vaccination Rates.
https://jamanetwork.com/journals/jama/fullarticle/2781792
Walkey, A. J., Law, A., & Bosch, N. A. (2021). Lottery-Based Incentive in Ohio and COVID-19 Vaccination
Rates. JAMA.
Did Ohio’s Vaccine Lottery Increase Vaccination Rates? A Pre-Registered, Synthetic Control Study.
https://osf.io/a6de5/
More Information about the COVID-19 Examples
The Equal Employment Opportunity Commission (EEOC) provides guidance to employees regarding offering
COVID-19 vaccine incentives.
https://www.eeoc.gov/wysk/what-you-should-know-about-covid-19-and-ada-rehabilitation-act-and-
other-eeo-laws#K
The National Governors Association maintains a list of state and local government incentives being offered for
COVID-19 vaccination.
https://www.nga.org/center/publications/covid-19-vaccine-incentives/
Additional Resources for Implementing this Strategy
Vaccination Programs: Client of Family Incentive Rewards
https://www.thecommunityguide.org/findings/vaccination-programs-client-or-family-incentive-rewards
Strategy 6: School-Located Vaccination Programs
Research Base
Voluntary school-based human papillomavirus vaccination: an efficient and acceptable model for achieving
high vaccine coverage in adolescents.
https://www.jahonline.org/article/S1054-139X1000318-6/fulltext
Skinner, S. R., & Robbins, S. C. C. (2010). Voluntary school-based human papillomavirus vaccination: an
efficient and acceptable model for achieving high vaccine coverage in adolescents. Journal of Adolescent
Health, 47(3), 215-218.
Appendix A

36
HPV vaccine uptake in a school-located vaccination program.
https://www.tandfonline.com/doi/full/10.1080/21645515.2016.1208326
Middleman, A. B., Won, T., Auslander, B., Misra, S., & Short, M. (2016). HPV vaccine uptake in a school-
located vaccination program. Human vaccines & immunotherapeutics, 12(11), 2872-2874.
Addressing adolescent immunization disparities: a retrospective analysis of school-based health center
immunization delivery.
https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2009.176628
Federico, S. G., Abrams, L., Everhart, R. M., Melinkovich, P., & Hambidge, S. J. (2010). Addressing adolescent
immunization disparities: a retrospective analysis of school-based health center immunization delivery.
American journal of public health, 100(9), 1630-1634.
More Information about the COVID-19 Examples
Preparing for a school-located COVID-19 vaccination clinic.
https://journals.sagepub.com/doi/full/10.1177/1942602X21991643
Park, K., Cartmill, R., Johnson-Gordon, B., Landes, M., Malik, K., Sinnott, J., ... & Wallin, R. (2021). Preparing
for a school-located COVID-19 vaccination clinic. NASN School Nurse, 36(3), 156-163.
Additional Resources for Implementing this Strategy
Lessons learned about the need for careful and thorough planning for school-located vaccination programs
are shared.
Lott, J., & Johnson, J. (2012). Promising Practices for School-located Vaccination Clinics—Part I:
Preparation. Pediatrics, 129(Supplement 2), S75-S80.
Promising Practices for School-located Vaccination Clinics—Part I: Preparation | American Academy of
Pediatrics (aappublications.org)
Lessons learned about clinic operations based on experience of a school-located mass vaccination program for
influenza.
Lott, J., & Johnson, J. (2012). Promising Practices for School-located Vaccination Clinics—Part II: Clinic
Operations and Program Sustainability. Pediatrics, 129(Supplement 2), S81-S87.
Promising Practices for School-located Vaccination Clinics— | American Academy of Pediatrics
(aappublications.org)
Guidance for consideration when planning school-located vaccination clinics for COVID-19.
https://www.cdc.gov/vaccines/covid-19/planning/school-located-clinics.html#additional
Resources for school-based vaccines and immunizations for kids and teens.
https://www.sbh4all.org/resources/school-based-vaccines-and-immunizations/
Strategy 7: Home-Delivered Vaccination
Research Base
Project VIVA: a multilevel community-based intervention to increase influenza vaccination rates among hard-
to-reach populations in New York City.
https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2007.119586
Coady, M. H., Galea, S., Blaney, S., Ompad, D. C., Sisco, S., & Vlahov, D. (2008). Project VIVA: a multilevel
community-based intervention to increase influenza vaccination rates among hard-to-reach populations
in New York City. American Journal of Public Health, 98(7), 1314-1321.
More Information about the COVID-19 Examples
Door-to-door teams reach nearly all care homes within a week in Multnomah County, Oregon to distribute the
COVID-19 vaccine.
https://www.multco.us/novel-coronavirus-covid-19/news/door-door-teams-reach-nearly-all-care-homes-
within-week
Appendix A

37
Appendix A
Additional Resources for Implementing this Strategy
Guidance for implementing home-bound and residential living vaccination.
Centers for Disease Control: Vaccinating Homebound Persons With COVID-19 Vaccine
https://www.cdc.gov/vaccines/covid-19/clinical-considerations/homebound-persons.html
How the Medical Reserve Corps is assisting with COVID-19 vaccination.
https://www.phe.gov/mrc
Strategy 8: Workplace Vaccination Programs
Research Base
Effectiveness of worksite interventions to increase influenza vaccination rates among employees and families.
https://journals.lww.com/joem/Abstract/2013/02000/Effectiveness_of_Worksite_Interventions_to.8.aspx
Ofstead, C. L., Sherman, B. W., Wetzler, H. P., Langlay, A. M. D., Mueller, N. J., Ward, J. M., ... & Poland, G. A.
(2013). Effectiveness of worksite interventions to increase influenza vaccination rates among employees
and families. Journal of occupational and environmental medicine, 55(2), 156-163.
The KFF COVID-19 Vaccine Monitor is an ongoing research project tracking the public’s attitudes and
experiences with COVID-19 vaccinations, where this topic is about vaccine attitudes among essential workers.
https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-vaccine-attitudes-
among-essential-workers/
Getting to work: Employers’ role in COVID-19 Vaccination.
https://www.mckinsey.com/industries/pharmaceuticals-and-medical-products/our-insights/getting-to-
work-employers-role-in-covid-19-vaccination
More Information about the COVID-19 Examples
Hy-Vee brings mobile units directly to Midwestern food workers.
https://www.cdc.gov/vaccines/covid-19/retail-pharmacy-program/retail-stories.html
U.S. Chamber of Commerce: Small Businesses Host Vaccine Clinics to Speed Up Shots.
https://www.uschamber.com/series/above-the-fold/small-businesses-host-vaccine-clinics-speed-shots
Additional Resources for Implementing this Strategy
CDC guidance for state, tribal, and local jurisdictions on promoting workplace vaccination efforts.
https://www.cdc.gov/vaccines/covid-19/health-departments/essential-workers/index.html
CDC guidance for employers to promote employee COVID-19 vaccination.
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/toolkits/essential-workers.html
Guidance for planning Vaccination Clinics Held at Temporary, Satellite, or Off-Site Locations
https://www.cdc.gov/vaccines/hcp/admin/mass-clinic-activities/index.html
Strategy 9: Vaccine Requirements
Research Base
Increasing Appropriate Vaccination: Vaccination Requirements for Child Care, School, and College Attendance
(2009 Archived Review).
https://www.thecommunityguide.org/sites/default/files/Vaccination-Requirements-Schools-Archive.pdf
Nudges or mandates? The ethics of mandatory flu vaccination.
Nudges or mandates? The ethics of mandatory flu vaccination - ScienceDirect
Dubov, A., & Phung, C. (2015). Nudges or mandates? The ethics of mandatory flu vaccination. Vaccine,
33(22), 2530-2535.
38
Systematic review of the effect of immunization mandates on uptake of routine childhood immunizations.
https://www.sciencedirect.com/science/article/abs/pii/S0163445316300299
Lee, C., & Robinson, J. L. (2016). Systematic review of the effect of immunization mandates on uptake of
routine childhood immunizations. Journal of Infection, 72(6), 659-666.
More Information about the COVID-19 Examples
The complete list of higher education institutions requiring vaccination for the fall 2021-2022 semester.
https://universitybusiness.com/state-by-state-look-at-colleges-requiring-vaccines/
List of hospitals and health systems that are requiring vaccines for workers.
https://www.beckershospitalreview.com/workforce/hospitals-health-systems-mandating-vaccines-for-
workersjune17.html
Morgan Stanley to Require Vaccinations to Enter N.Y. Offices.
https://www.bloomberg.com/news/articles/2021-06-22/morgan-stanley-tells-staff-they-ll-need-vaccines-
to-enter-office
The deadline for Houston Methodist’s vaccine mandate was June 7. How did it go?
https://www.beckershospitalreview.com/workforce/the-deadline-for-houston-methodist-s-
vaccine-mandate-was-june-7-how-did-it-go.html#:~:text=Post%2DAcute-,The%20deadline%20
for%20Houston%20Methodist’s%20vaccine%20mandate%20was%20June,How%20did%20it%20
go%3F&text=Houston%20Methodist%20employees%20had%20a,24%2C947%20workers%20being%20
fully%20vaccinated.
Mandatory Vaccination Policy Lawsuit Update: Nurses Take a Shot Against Hospital, But Judge Jabs Back in
Texas.
https://www.natlawreview.com/article/mandatory-vaccination-policy-lawsuit-update-nurses-take-shot-
against-hospital-judge
Additional Resources for Implementing this Strategy
Several legal organizations offer guidance and templates for crafting vaccine requirement policies:
https://www.fisherphillips.com/services/emerging-issues/vaccine-resource-center/index.
html?tab=overview
https://www.shrm.org/resourcesandtools/tools-and-samples/policies/pages/vaccination-policy-
mandatory-covid19-coronavirus.aspx
https://www.themcdispatch.com/wp-content/uploads/2021/02/HUB-SAMPLE-Employee-COVID-19-
Vaccine-Policy.pdf
Houston Methodist Vaccine Requirement Policy
https://hrportal.ehr.com/LinkClick.aspx?fileticket=WbwcMj8SRPg%3d&portalid=78
Strategy 10: Effective Messages Delivered by Trusted Messengers
Research Base
Assessing the state of vaccine confidence in the United States: recommendations from the National Vaccine
Advisory Committee.
https://journals.sagepub.com/doi/abs/10.1177/003335491513000606
Committee, N. V. A. (2015). Assessing the state of vaccine confidence in the United States:
recommendations from the National Vaccine Advisory Committee: approved by the National Vaccine
Advisory Committee on June 10, 2015. Public Health Reports, 130(6), 573-595.
The COVID-19 States Project: A 50-State COVID-19 Survey Report #36: Evaluation of COVID-19 Vaccine
Communication Strategies.
https://news.northeastern.edu/wp-content/uploads/2021/01/COVID19-CONSORTIUM-REPORT-36-
VACCINE-COMM-Jan-2021.pdf
Appendix A

39
Examining the effect of information channel on COVID-19 vaccine acceptance.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0251095
Piltch-Loeb, R., Savoia, E., Goldberg, B., Hughes, B., Verhey, T., Kayyem, J., ... & Testa, M. (2021). Examining
the effect of information channel on COVID-19 vaccine acceptance. Plos one, 16(5), e0251095.
More Information about the COVID-19 Examples
Greater Than COVID helps individuals take charge of their health during the evolving COVID-19 public health
crisis. Tailored media messages and community tools will address information needs about the new vaccines.
https://www.greaterthancovid.org/theconversation/
Additional Resources for Implementing this Strategy
Resources for building vaccine confidence and CDC vaccine confidence insight reports.
https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence.html#reports
Vaccine communication tips from deBeaumont Foundation.
https://debeaumont.org/changing-the-covid-conversation/vaccineacceptance/covid-vaccine-poll-
vaccine-communications-tips/
Strategy 11: Provider Recommendation
Research Base
Recommendations and offers for adult influenza vaccination, 2011–2012 season, United States.
https://doi.org/10.1016/j.vaccine.2016.04.061
Benedict, K. M., Santibanez, T. A., Black, C. L., Ding, H., Graitcer, S. B., Bridges, C. B., & Kennedy, E. D. (2017).
Recommendations and offers for adult influenza vaccination, 2011–2012 season, United States. Vaccine,
35(9), 1353-1361.
Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk
geographic area.
https://doi.org/10.1097/OLQ.0b013e3181f12dbf
Brewer, N. T., Gottlieb, S. L., Reiter, P. L., McRee, A. L., Liddon, N., Markowitz, L., & Smith, J. S. (2011).
Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk
geographic area. Sexually transmitted diseases, 38(3), 197–204.
More Information about the COVID-19 Examples
The New York City Department of Health and Human Hygiene created a resource called Vaccine Talks which
emphasizes the importance of healthcare provider recommendations in increasing COVID-19 vaccination
rates.
https://www1.nyc.gov/site/doh/covid/covid-19-providers-vaccines-communication.page
The statement the NY health commissioner released promoting Vaccine Talks that place emphasis on the trust
patients have in their healthcare providers.
https://www1.nyc.gov/assets/doh/downloads/pdf/covid/providers/coh-letter-vaccine-
communication-04272021.pdf
COVID-19 Vaccine Use Every Opportunity Campaign Implementation Tool.
https://www1.nyc.gov/assets/doh/downloads/pdf/covid/providers/covid-19-vaccine-use-every-
opportunity-tool.pdf
Here is an example of the Philadelphia Department of Public Health putting a call out to emergency facilities in
the city to begin recommending and administering COVID-19 vaccines to patient upon discharge.
https://vax.phila.gov/index.php/notices/vaccinate-patients-upon-discharging/
Here is an example of the Philadelphia Department of Public Health using CDC Best Practices for Vaccinating
Appendix A

40
Upon Discharge in addition to Vaccine eligibility.
https://vax.phila.gov/index.php/notices/cdc-best-practices-for-vaccinating-upon-discharge/
Additional Resources for Implementing this Strategy
CDC offers 5 suggestions on how to talk to your patients about COVID-19 vaccine.
https://www.cdc.org/vaccines/covid-19/hcp/engaging-patients.html
The American Medical Association’s (AMA) COVID-19 Vaccine FAQs includes statements physicians can use
when talking with patients.
https://www.ama-assn.org/system/files/2020-12/covid-19-vaccine-physician-faqs.pdf
Strategy 12: Combating Misinformation
Research Base
Debunking: A meta-analysis of the psychological efficacy of messages countering misinformation.
https://journals.sagepub.com/doi/full/10.1177/0956797617714579
Chan, M. P. S., Jones, C. R., Hall Jamieson, K., & Albarracín, D. (2017). Debunking: A meta-analysis of the
psychological efficacy of messages countering misinformation. Psychological science, 28(11), 1531-1546.
Effects of fact-checking social media vaccine misinformation on attitudes toward vaccines.
https://doi.org/10.1016/j.ypmed.2020.106408
Zhang, J., Featherstone, J. D., Calabrese, C., & Wojcieszak, M. (2021). Effects of fact-checking social media
vaccine misinformation on attitudes toward vaccines. Preventive Medicine, 145, 106408.
Misinformation and its correction: Continued influence and successful debiasing.
https://journals.sagepub.com/doi/pdf/10.1177/1529100612451018
Lewandowsky, S., Ecker, U. K., Seifert, C. M., Schwarz, N., & Cook, J. (2012). Misinformation and its
correction: Continued influence and successful debiasing. Psychological science in the public interest, 13(3),
106-131.
The Swiss cheese model for mitigating online misinformation.
https://www.tandfonline.com/doi/full/10.1080/00963402.2021.1912170
Bode, L., & Vraga, E. (2021). The Swiss cheese model for mitigating online misinformation. Bulletin of the
Atomic Scientists, 77(3), 129-133.
More Information about the COVID-19 Examples
PGP (The Public Good Projects) is a public health nonprofit specializing in large-scale media monitoring
programs, social and behavior change interventions, and cross-sector initiatives.
https://publicgoodprojects.org/about
How data scientists and influencers are joining forces to fight against dangerous COVID-19 conspiracy theories
online.
https://www.msn.com/en-us/money/other/how-influencers-are-fighting-dangerous-conspiracy-theories-
about-covid-19-as-people-shun-experts-warnings/ar-BB1c8Zf6
Additional Resources for Implementing this Strategy
Weekly briefings highlighting trends in vaccine misinformation.
https://www.viralityproject.org/weekly-briefings
Additional Resource
The Guide to Community Preventive Services (The Community Guide) lists evidence-based interventions to
improve vaccination rates in an easy-to-use table.
https://www.thecommunityguide.org/sites/default/files/assets/What-Works-Factsheet-Vaccination.pdf
Appendix A

41
Appendix B
Strategy Matrix Table
Common Barriers
Strategy Barriers Population Location
1. Vaccine Ambassadors Equity, access, prevailing
social norms, mistrust,
misinformation, cultural
relevance
Hispanic or Latino Adults and
Black Adults
San Francisco, CA
Philadelphia, PA
2. Medical Providers
Standardize Vaccination
Policy, mistrust, health literacy Adults Multiple U.S. locations
3. Medical Reminders Equity, access, forgetfulness,
friction, health literacy, lack of
adequate information
Adults Multiple U.S. locations
4. Motivational Interviewing Misperception, health literacy,
uncertainty
Adults Western Pennsylvania
5. Financial Incentives Inertia College Students Multiple U.S. locations
6. School-Located
Vaccination Programs
Access, friction, prevailing
social norms, uncertainty, lack
of adequate information
School-aged Youth St. Louis County, MO
7. Home-Delivered
Vaccination
Equity, access, inertia, friction Adults Multnomah County, OR
8. Workplace Vaccination Access, cost, prevailing social
norms, friction
Adults Midwest; Jackson, MS
9. COVID-19 Vaccine
Requirements
Policy, inertia, prevailing social
norms, politicization
Adults Multiple U.S. locations
10. Eective messages
delivered by trusted
messengers
Mistrust, health literacy,
misinformation, lack of
adequate information
Adults Multiple U.S. locations
11. Provider
Recommendations and Oers
Inertia, friction, mistrust,
uncertainty, mis- and
disinformation, lack of
adequate Information
Adults New York, NY;
Philadelphia, PA
12. Combating Misinformation Misperception, mis- and
disinformation, lack of
adequate information
Adults Multiple U.S. locations

42
Appendix C
Diagnostic Tool

43
Appendix C
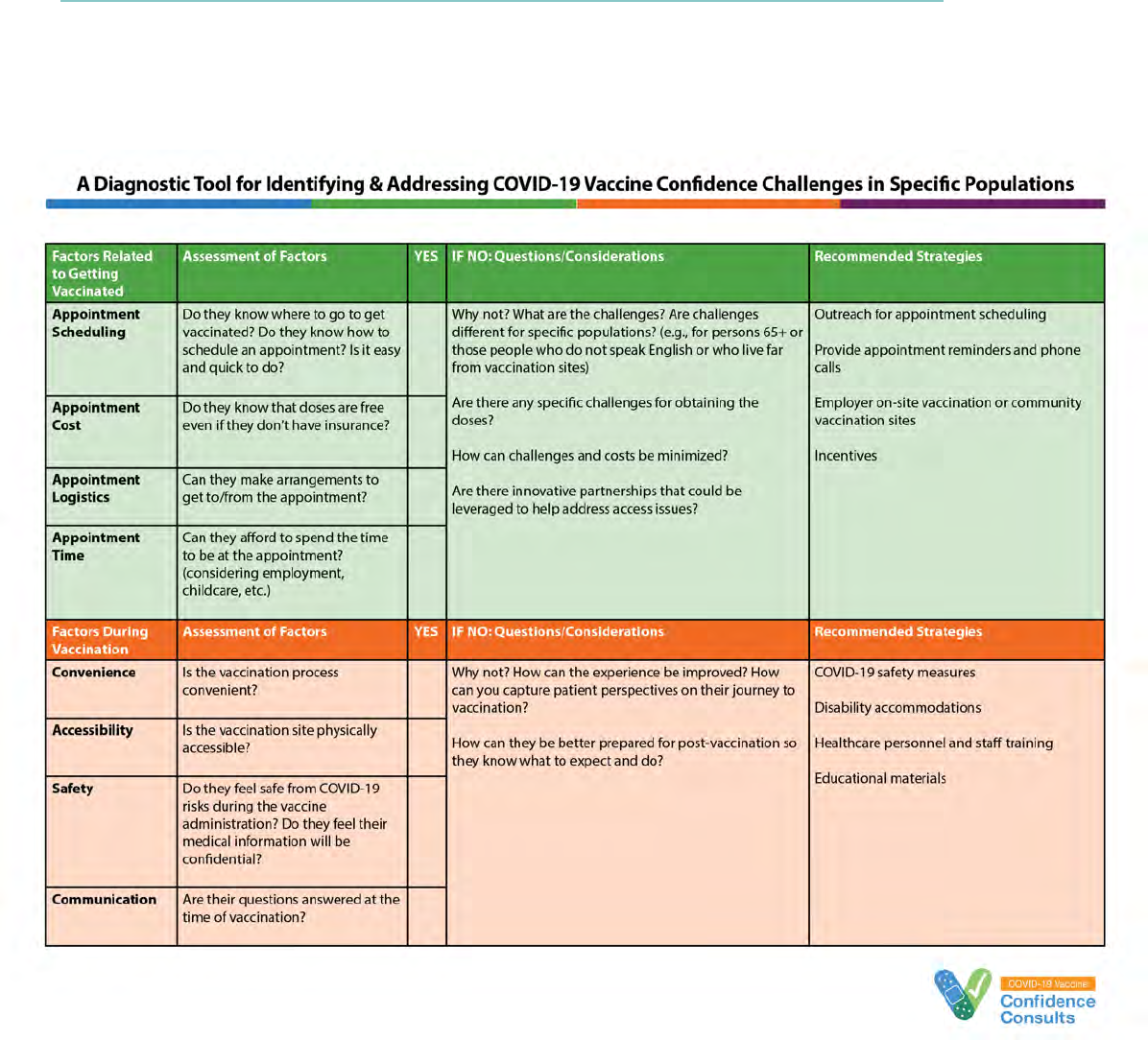
44
Appendix C

45
Appendix C

46
Appendix D
BeSD Framework
The Behavioral and Social Drivers (BeSD) Framework
Source: The WHO BeSD working group. Based on Increasing Vaccination Model (Brewer et al., 2017)
An expert working group chaired by the World Health Organization (WHO) developed a behavioral
framework specific to COVID-19 vaccination uptake titled the Behavioral and Social Drivers (BeSD)
of COVID-19 Vaccination Uptake. The framework demonstrates that the following drivers are
associated with COVID-19 vaccination:
What people think and feel
Social process
Motivation
Practical issues
Each driver can be measured through regular data collection to understand and act on individuals’
barriers and enablers to COVID-19 vaccine uptake. Factors at many levels—individual, community,
societal, and policy—affect someone’s decision to get vaccinated. Some of these factors are
within control to address, and some are not. Understanding this framework provides an additional
way to understand people’s thoughts and behaviors related to their decision about receiving
the COVID-19 vaccine.

47
Acknowledgments
Timely production of this guide would not have been possible without strong leadership from CDC
staff, insightful technical input and review from advisory committee members, and hours of work by
contractors. We gratefully acknowledge each contributor.
We are thankful to the National Association of County and City Health Officials (NACCHO) members
who reviewed the draft and provided feedback from the perspective of those we hope will use the
information in this Field Guide.
The Little Jab Book: 18 Behavioral Science Strategies for Increasing Vaccination Uptake, developed by
Busara, Common Thread, and Save the Children, was the inspiration to develop a U.S.-oriented resource
and became the template for this work.
Advisory Committee
Ann Aikin, MA
Office of Infectious Disease and HIV/AIDS Policy
U.S. Department of Health and Human Services
Washington, D.C.
Meredith Allen, DrPH
Health Security
Association of State and Territorial Health Officials
Arlington, VA
Noel T. Brewer, PhD
Department of Health Behavior
Gillings School of Global Public Health
University of North Carolina – Chapel Hill
Chapel Hill, NC
Alison Buttenheim, PhD MBA
Department of Family and Community Health
University of Pennsylvania School of Nursing
Philadelphia, PA
Michelle Cantu, MPH
Infectious Disease and Immunization
National Association of County and City Health Officials
Washington, D.C.
David Hopkins, MD
Guide to Community Preventive Services
Office of the Associate Director for Policy and Strategy
CDC
Portland, OR
Amy Lansky, PhD
Guide to Community Preventive Services
Office of the Associate Director for Policy and Strategy
CDC
Portland, OR
James Tseryuan Lee, MD
Immunization Services Division
CDC
Atlanta, GA
Saad B. Omer, PhD
Yale Institute of Global Health
Yale University
New Haven, CT
Marcus Plescia, MD
Medical Officer
Association of State and Territorial Health Officials
Arlington, VA
Elana Safran, MS
Office of Evaluation Sciences
U.S. General Services Administration
Washington, D.C.

48
Acknowledgments
CDC Leadership
Neetu Abad, PhD
Global Immunization Division
CDC
Atlanta, GA
Kimberly Bonner, PhD
Epidemic Intelligence Service
CDC
Atlanta, GA
Stephanie Griswold, MPH
National Center for Immunization and Respiratory Diseases
CDC
Atlanta, GA
Elisabeth Wilhelm, MA
Global Immunization Division
CDC
Atlanta, GA
Writing and Design Team
Kelly Clay, MS, CHES®
Karna, LLC
Alia Hiller, CHES®
Tanaq Support Services, LLC
Roderick Hopkins, MPH
Karna, LLC
Alange Jacobs
Karna, LLC
Lorraine L. Janeczko, MPH
Karna, LLC
Sarah Morris Hummer, MA
Tanaq Support Services, LLC
Carly Ng, MPH, CHES®
Tanaq Support Services, LLC
Aparna Ramakrishnan, MA, MSW
Karna, LLC
Torey Repetski, MPH
Karna, LLC
Leslie Rodriguez, PhD
Karna, LLC
Randall Simpson, MPH, PMP
Karna, LLC
Bryan Sorenson, MPH
Tanaq Support Services, LLC
Nicole Weinstein, MSW
Karna, LLC

