
Recommendations to Strengthen the Resilience of New
Jersey’s Nursing Homes in the Wake of COVID-19
June 2, 2020

PROJECT BACKGROUND
2

Rapid Assessment of NJ’s COVID-19 Response for LTC
• In response to the growing impact of COVID-19 on nursing home residents and staff, in early May, the New Jersey Department of Health (DOH)
engaged Manatt Health (Manatt) to undertake a rapid assessment of the state’s COVID-19 response targeted toward the long-term care (LTC)
system.
• Manatt was charged with providing the state with a set of actionable recommendations over the near-term and intermediate to longer-term
aimed at improving the quality, resilience and safety of the state’s LTC delivery system now and for the future.
• Over the three-week project, Manatt undertook a review of relevant literature, conducted a data review, evaluated national best practices and
actions taken in other states, and conducted over fifty interviews with stakeholders from:
• New Jersey state government
• New Jersey associations
• New Jersey labor representatives
• New Jersey nursing homes
• New Jersey consumer and advocacy groups
• National experts
• Other states
• Based on this assessment, this report presents a series of recommendations over the near-term (next 4 months) and intermediate to longer-
term (5+ months) to:
• Strengthen emergency response capacity
• Stabilize facilities & bolster workforce
• Increase transparency & accountability
• Build a more resilient & higher quality LTC system
Context
3
This report was updated on 6/4/2020 to correct minor typos. The content of the report did not change.

Comment on Limitations
• This report was developed over a three-week period when the COVID-19 landscape in New Jersey was changing rapidly. The
recommendations in this report are informed by the most up-to-date information at that point in time, but Manatt recognizes that
week to week – and often day by day – there are new developments and information relating to the COVID-19 crisis.
• The primary focus of this report is skilled nursing facilities (SNFs), nursing facilities and special care nursing facilities (collectively
referred to in this report as nursing homes) licensed by the state of New Jersey, rather than the full range of congregate care settings
that operate in the state. Additional work may be done to identify which of these recommendations can be extended to those care
settings. The term “LTC facilities” is used when recommendations apply to facilities beyond nursing homes.
• While this report is about nursing homes, the people who reside in nursing homes have diverse needs. They include people with both
short- and long-term stays, and people with dementia, serious mental illness, traumatic brain injury and intellectual/developmental
disabilities.
• Because this report was developed during statewide “stay-at-home” orders and while nursing home visitation was restricted, Manatt
did not conduct any in-person visits to nursing homes. Instead, Manatt held video and telephonic calls with many stakeholders,
including a sampling of facilities, as well as trade associations, labor representatives, consumer advocates and many others. In the
future, in-person visits could further inform these recommendations.
• This report highlights a set of recommendations deemed to be high-impact actions that the State can take. It does not represent the
full spectrum of actions and improvements that the state may want to consider. Many of the recommendations in this report are
interdependent.
• Importantly, implementation of many of these recommendations will require further planning, and statutory or regulatory changes,
and many of these recommendations will require additional funding.
4

CONTEXT
5

COVID-19 Has Shone a Light on Heroes
Throughout COVID-19, we have seen unsung heroes who have stepped
up to an extraordinary degree—including many government leaders and
staff and nursing home administrators. Most notably, the front-line staff
in nursing homes, who placed their own health and the health of their
families at risk, deserve our recognition and gratitude.
6

Despite efforts to manage spread of coronavirus in NJ and elsewhere, COVID-19 fed on and exposed
weaknesses in our health care system, perhaps most notably in our nursing homes.
How Did We Get Here?
• As the outbreak unfolded, the situation was rapidly
changing on the ground, which impacted both the federal
and state responses.
• Similar to other states, New Jersey’s initial preparedness
coordination was more focused on external threats to the
state, with an emphasis on responding to the risk from
international travel.
• New Jersey quickly pivoted to focusing on the health care
delivery system response focus, though—as was true in
many states—with greater emphasis on inpatient hospital
surge capacity planning and support. The focus on
hospitals prompted the prioritization of the distribution of
supplies, personal protective equipment (PPE) and other
resources to that sector.
• DOH released a series of
guidance directed toward LTC
facilities beginning on March 3* and began to distribute
some PPE to nursing homes later in the month.
The Situation and Challenges
Are Not Unique to New Jersey
New Jersey Was Hit Early and Hard
• New Jersey had its first diagnosed COVID-19 case on March 4; at that time, testing was
scarce and the
testing and spread-risk was focused on symptomatic people. Along with the
broader New York City metropolitan area, cases rapidly increased in March.
• Likely due to its proximity to New York City and density, New Jersey ranks second nationally
behind New York in cases (160,918) and deaths (11,721) as of June 2.
*See Appendix on state actions addressing COVID-19 in nursing homes.
NY
376,520
(21%)
NJ
160,918
(9%)
Rest of US
1.16
million
(70%)
COVID-19 Cases
Share of US Population
NY
6%
NJ
3%
Rest of US
91%
7

Source: Manatt analysis of COVID-19 infection and death data file received from NJ DOH received on May 26, 2020; U.S. Census, Population Reference Bureau, “Annual
Estimates of the Resident Population for Counties in New Jersey: July 1, 2019”, data.census.gov
New Jersey’s outbreak peaked in late March through early April, with a substantial portion of the
population affected.
How Did We Get Here? (cont.)
8

Residents of nursing homes were particularly vulnerable.
Most tragically, high community spread in New Jersey brought
COVID-19 into New Jersey’s nursing homes.
How Did We Get Here?
(cont .)
• The state’s Wanaque Center for Nursing and
Rehabilitation had a serious, widely covered
viral outbreak among a particularly vulnerable,
specialized community of children using
ventilators just over a year ago.
• The Life Care Center in Kirkland, Washington,
was the center of the first major U.S. COVID-19
outbreak, and nursing homes in Europe were
ravaged by the virus.
Nursing homes are hotspots for
infectious disease outbreaks and
were quickly hit by COVID-19
• New Jersey has many old facilities, many
with 3- and 4-bedded rooms.
• A large percentage of nursing homes in New
Jersey have documented infection control
deficiencies and citations.
• Nursing homes are staffed by workers who
are also subject to community spread; many
of whom came from communities with large
outbreaks.
Certain characteristics of New Jersey
nursing homes—which are not
unique to the State—put them at
particularly high risk of an outbreak
Nursing homes are
congregate settings
that are the home for
people prone to
infection with
weakened capacities
to fight back.
9

Why It Matters: Protecting our Families, Neighbors and Caretakers
People living in nursing homes are our mothers and fathers, our sisters and brothers, our aunts and
uncles, our grandparents and great-grandparents, our former teachers, our veterans and our neighbors.
Nursing Home Demographics
People Living in Nursing Homes
• On an average day, over 45,000 New Jerseyans—approximately 0.5% of the state
population—are residing in a nursing home.
• People living in nursing homes have their own preferences and must have agency in
decisions that impact their homes and lives.
• Nursing home residents are among our most vulnerable community members. Many
are over 85 years of age, and they may be disabled, medically frail or have mental
impairments.
• Nursing homes provide crucial medical, skilled nursing and rehabilitative care for
both short stays (such as on a post-operative basis) and LTC. People receiving short-
term v. long-term care in nursing homes have very different needs.
• In New Jersey, two or three individuals often share nursing home rooms. There is a
growing movement in New Jersey and throughout the country to modernize nursing
homes to make them more home-like and less institutional.
• People living in nursing homes long term are often without means and/or have spent
down most of their resources before turning to Medicaid, which is the primary payer
for nursing home services.
New Jersey Nursing Home Demographics 2018
Medicaid Medicare Other Total
Average Daily
Census
26,570 6,823 12,455 45,847
Average Length
of Stay (days)
365 31 81 102
As of February 2020, about 20,500 Medicaid beneficiaries residing in
nursing homes were enrolled in managed long term services and
supports (MLTSS) and 6,500 were in fee-for-service.
Note: Underlying data is state reported totals (methodologies may vary; as such should be considered illustrative only). This analysis excludes New York due to discrepancies with its data.
50%
60%
62%
67%
43%
New Jersey
Connecticut
Massachusetts
Pennsylvania
US
Share of COVID-19 Deaths in Nursing Homes and Assisted Living Facilities
as of 5/22
*Includes deaths of residents in all LTC facilities
As of 6/2:
5,965
10

Why It Matters: Protecting our Families, Neighbors and Caretakers cont.
Nursing home staff working on the front lines, who continue to place their own health and the health
of their families at risk throughout COVID-19, deserve support and protection.
Nursing Home Staff
• 54,361 staff work in New Jersey nursing homes, including nursing staff, food, cleaning, and administrative
staff.
• Certified nursing assistants (CNAs) and licensed practical nurses (LPNs) provide most of the care in nursing
homes. CNAs are the backbone of the staff and provide close to
90% of direct care, including bathing,
lifting, toileting and assistance with daily activities, to New Jersey’s nursing home residents.
• Chronic staffing shortages of CNAs and LPNs put additional pressure on overworked staff.
• Further, due to the low wages, many nursing home staff nationally and in New Jersey work
more than one
job
, sometimes across multiple nursing homes, sometimes shifting between hospitals and nursing homes
or other part-time jobs.
o In New Jersey,
CNAs make an average of $15/hour and LPNs make an average of $27.65/hour.
• Some facilities pay higher wages in lieu of benefit packages; some facilities pay lower wages with benefits.
13% of workers have no
health insurance.
• The overwhelming majority of the New Jersey nursing home direct care workers are women who are racial
or ethnic
minorities. Half are immigrants.
• CNAs have experienced the same childcare and family care obligations during the pandemic that are
exacerbated when schools and child care are closed and family members are ill as everyone else – but like
all frontline responders, they cannot work from home.
Spotlight on NJ Direct Care Workforce
• CNAs: 15,606
• LPNs: 5,603
• RNs: 4,900
• Women: 91%
• Racial or Ethnic Minorities: 84%
o Black or African American: 61%
o Hispanic or Latino: 14%
o Asian or Pacific Islander: 7%
o Other: 2%
• Immigrants: 50%
NJ LTC Workers’ COVID-19 Status as of June 2
Cases 10,895
Deaths 107
11

COVID-19 Amplified Existing Systemic Issues
You cannot invent a system that works when a crisis hits; the system must already be in place.
Critical Themes
COVID-19 didn’t create the problem – it exacerbated the long-standing, underlying systemic
issues affecting nursing home care in New Jersey.
• Nursing homes were largely underprepared for the threat of a widespread infection and under-resourced due to long-standing staffing
shortages or low staffing ratios. Many had previously been cited for infection control deficiencies.
• There was room for improvement in bidirectional communications between nursing homes and DOH. Lapses on both sides may have
contributed to inconsistent compliance with DOH guidance.
• Nursing homes generally were not adequately tied into the larger system of care and typically do not have strong communications and
consult relationships and protocols with emergency departments. Further, there is often poor communication between nursing homes and
hospitals at the point of hospital admissions and discharges. In addition, there is a lack of interoperability between nursing home and hospital
electronic health records.
• Under-resourced state agencies did not have sufficient staff to deploy to facilities and conduct meaningful oversight prior to COVID-19.
o No LTC-focused preparedness plan was in place in the state prior to COVID-19 with respect to PPE, staffing back up plans or
communications from facilities to hospitals or families.
o Much of the oversight of nursing homes is highly prescribed by federal rules; the federal requirements are rigid, often resulting in paper
compliance and limited improvements.
• New Jersey’s LTC industry and its regulatory agencies were not equipped with the technological systems or the practiced processes to rapidly
collect and share data in support of the state’s public health response.
12
Person-Centered
Communication +
Collaboration
High Quality, Safe
Facilities
Aligned Regulatory
Oversight + Support
Emergency
Preparedness
Strong sense of purpose, mission and value
Technology-enabled and data-driven
Viable financial model(s)
Critical
enablers:
Regular communication
among and between patients,
families, employees, care
delivery partners, facilities
and regulators
Meaningful choice, with
access to supports to enable
living at home/preferred
residence as long as possible
Goals of care plans and
ongoing dialogue
Use of telehealth and
consumer-convenient
services and supports
Resident empowerment
and active engagement
around wellness
Key
elements:
Formal cross-agency
collaboration centered on LTC
Adequate staffing levels –
both overall and by skill level
Enhanced wages and benefits
to reduce turnover and
moonlighting and ensure
consistency
Modernized facilities with
more single rooms, updated
HVAC, broadband and IT
infrastructure
Strong infection control
policies and procedures.
Access to clinical expertise;
engaged clinical relationships
High degree of
transparency across system
Sufficient staff,
resources and expertise
state-level
Real-time use of data to
inform interventions,
educate public and hold
industry accountable
Payment aligned with
desired system outcomes
Clear emergency plans
at facility, regional and
state levels and defined
roles and responsibilities
Clear communications
plan
Ongoing training and
drills; learning system
with access to technical
assistance
Strong community
relationships
Culture of safety
Culture of quality
Meaningful forums for
stakeholders to provide input
and to participate in industry-
wide improvement
Culture of caring and
respect
Culture of problem-solving
Culture of accountability
More home-like and non-
institutional nursing homes
Clear bi-directional
family/caregiver channels
Elements of a High-Functioning, Resilient LTC System
Meaningful consequences
for consistently poor
performance
13

A Galvanizing Moment
While COVID-19 has shone a light on the structural deficiencies in how we provide and fund
LTC, it also presents an opportunity for meaningful change:
• LTC workers and facilities are on the frontline of the pandemic response.
• COVID-19 exposed weakness and vulnerabilities in the system that represent a tough—but not
insurmountable—set of challenges.
• Stakeholders across New Jersey have mobilized to support their neighbors and have collaborated in
new ways, demonstrating opportunities for greater alignment across the system.
• Policymakers and regulators have developed a clearer view of the key priorities for reform going
forward.
• Recovery from this crisis should be a catalyst for change, bringing together policymakers, providers,
community members and others to create a high-functioning, resilient LTC system.
14

Landscape Review
15

New Jersey’s Nursing Homes: Key Characteristics
Spotlight on New Jersey Nursing Homes
Total number of nursing homes 370
For-profit ownership 74%
Non-profit ownership 23%
Government owned 3%
Average number of residents per day per
nursing home
119
Bed occupancy rate 82%
Average number of beds per nursing home 145
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020
Although New Jersey has a wide range of congregate care settings, including assisted living
facilities, veterans memorial homes, developmental centers, and group homes, this report
focuses primarily on nursing homes.
16
Infection Control Deficiencies in Nursing Homes
Approximately one-third of nursing homes surveyed by New Jersey in 2017 were cited for an infection
prevention and control deficiency.
Infection Prevention and Control Deficiencies Cited, by State, 2017
State Number of Surveyed
Nursing Homes
Number With an Infection
Prevention and Control Deficiency
Cited
Percentage of Surveyed Nursing Homes With an Infection
Prevention and Control Deficiency Cited
New Jersey 334 105 31.4%
Total Across U.S. 14,550 5,755 39.6%
Nursing Homes with Infection Prevention and Control Deficiencies Cited, by State, Aggregate of Surveys from 2013 through 2017
State Total Surveyed
Nursing Homes
2013-2017
Nursing Homes With
No Infection
Prevention and
Control Deficiencies
Cited
Nursing Homes With
Infection Prevention
and Control
Deficiencies Cited in
Only One Year
Nursing Homes With Infection
Prevention and Control
Deficiencies Cited in Multiple
Non-Consecutive Years
Nursing Homes With Infection
Prevention and Control
Deficiencies Cited in Multiple
Consecutive Years
New Jersey 374 95 (25%) 133 (36%) 55 (15%) 91 (24%)
Total Across U.S. 16,266 2,967 (18%) 4,309 (26%) 2,563 (16%) 6,427 (40%)
Source: Infection Control Deficiencies Were Widespread and Persistent in Nursing Homes Prior to COVID-19 Pandemic, GAO. https://www.gao.gov/assets/710/707111.pdf
17

Distribution of COVID-19 Across New Jersey Nursing Homes: Early Observations
Based on available data, strong and consistent patterns between nursing home COVID-19 cases and deaths and potential predictive characteristics were
not immediately evident. Early observations included:
• The Central East, Central West, and South regions had fewer COVID-19 cases per 1,000 people and fewer nursing home cases per licensed bed
compared to the North East and North West; in other words, with some exceptions, the intensity of COVID-19 cases in nursing homes largely
mirrored their surrounding communities.
• Larger nursing homes have not had a higher rate of confirmed COVID-19 cases or deaths on a per licensed bed basis than smaller nursing homes.
• For-profit and not-for-profit nursing homes have had similar rates of COVID-19 cases and deaths per licensed bed (additional in-depth analysis
recommended); however, data were not available to consider for-profit and not-for-profit subgroups.
• An observed relationship has not been identified between the Centers for Medicare and Medicaid Services’ (CMS) Nursing Home Compare overall Star
rating or quality star ratings and total COVID-19 nursing home deaths per licensed bed in New Jersey. (Continuing evaluation is happening across the
industry, including new reporting requirements for direct reporting to CMS, and these issues are anticipated to receive much scrutiny in the coming
months.)
• Weak relationships – if any – have been observed between number of COVID-19 deaths per licensed bed and nursing home health and infection
control deficiencies given available data.
Key Takeaways
The early analytic results are based on Manatt’s analysis of available data, including the sources listed below.
• Nursing Home Compare data (https://www.medicare.gov/nursinghomecompare/search.html? – accessed, May 12, 2020)
• U.S. Census data (https://data.census.gov/cedsci/ - accessed, May 12, 2020)
• New Jersey LTC COVID-19 infection and death data
(
https://www.state.nj.us/health/healthfacilities/documents/LTCFacilitiesOutbreaksList.pdf - accessed, May 12, 2020)
• New Jersey COVID-19 dashboard data (https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml – accessed, May
22, 2020)
Manatt Health conducted an analysis of COVID-19 cases and deaths in New Jersey nursing homes reporting to CMS. These facilities were selected for in-depth review due to the availability
of information regarding Star ratings, survey results, licensed beds, health deficiencies, ownership status and staffing. The facility data from CMS were cross-walked to the New Jersey
COVID-19 dashboard for confirmed COVID-19 cases and deaths in LTC facilities as of May 22, 2020. See Appendix for additional details.
Note: On June 1, 2020, CMS released a first tabulation of survey data from the Nursing Home COVID-19 Data Source: CDC National Healthcare
Safety Network (NHSN). This data reflects data entered into the NHSN system by nursing homes as of May 24, 2020 and is anticipated to be
updated on a weekly basis. CMS reports this initial data tabulation is incomplete; only approx. 80% of facilities reported by the deadline. CMS
also notes that, as with any new reporting program, some of the data from their early submissions may be inaccurate as facilities learn a new
system. Of note, facilities may opt to report cumulative data retrospectively back to January 1, 2020, though no facility is required to report
prior to May 8, 2020. Therefore, some facilities may be reporting higher numbers of cases/deaths compared to other facilities, due to their
retrospective reporting. The availability of testing may impact the number of confirmed COVID-19 cases facilities report. Deaths in this data set
are only counted if they include a lab confirmation for COVID-19.
18

Notes: Chart presented for directional purposes only. Deaths reported by LTC facilities to DOH; deaths may not be lab confirmed. Total and nursing home-only deaths collected from separate data sources that may have
differences in data collection, compilation, and presentation methodologies resulting in slight deviations in totals by date when compared. Nursing home deaths only includes COVID-19 deaths attributable to nursing home
residents and nursing homes listed in the CMS Nursing Home Compare database. All other COVID-19 deaths, including nursing home staff deaths and those attributed to assisted living and non-Medicare/Medicaid certified
nursing homes are counted as “not nursing home.” Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey
as of May 22, 2020:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22, 2020
By county, the percentage of total COVID-19 deaths that has occurred among nursing home residents
has ranged from 14% to 69%.
High Percentage of NJ COVID-19 Deaths Have Been in Nursing Homes
19

Anecdotes From the Field: Responses Were Inconsistent During COVID-19
Some facilities with 3- and 4-bedded rooms moved
patients closer together because they were so seriously
short-staffed. Their intention was to improve safety and
deploy workforce more strategically but in hindsight, it was
the opposite of what should have happened.
“
”
A nursing home began lowering its daily census in
February, restricting congregate meals, increased wages of
nursing home staff and limited their ability to work at
multiple facilities, stockpiled PPE and brought in a nurse
educator on infection control. She did rounds with them to
see how staff was using PPE and made suggestions on how
they could improve their use of PPE.
“
”
A nursing home began to disseminate COVID-19
information to staff and residents/families, to screen
visitors and test and train staff on hygiene procedures in
the facilities in January. The nursing home also isolated
residents and staff upon a positive test, and paid workers a
bonuses to retain workforce.
“
”
A large, isolated facility operates van carpools to bring staff
in from a large city in Northern New Jersey (which happens
to be a high community outbreak region). Even if staff
isolated and practiced good infection control in the facility,
social distancing in large van carpools is impossible
.
“
”
Nursing homes had to quickly adapt their everyday operations to respond to the challenges presented by
COVID-19. In hindsight, some may have exacerbated outbreaks.
At the beginning of the crisis, the feelings among most staff were fear and panic. They weren’t provided training on infection control and use
of PPE, and guidance kept changing. Some employers were opting out of the paid sick leave made available under the federal emergency
legislation. So people were going to work even if they were sick because they needed to get paid. Some facilities loosened their attendance
policies, but some did not.”
”
“
Note: These anecdotes are drawn from Manatt interviews with stakeholders.
20

Recommendations
21

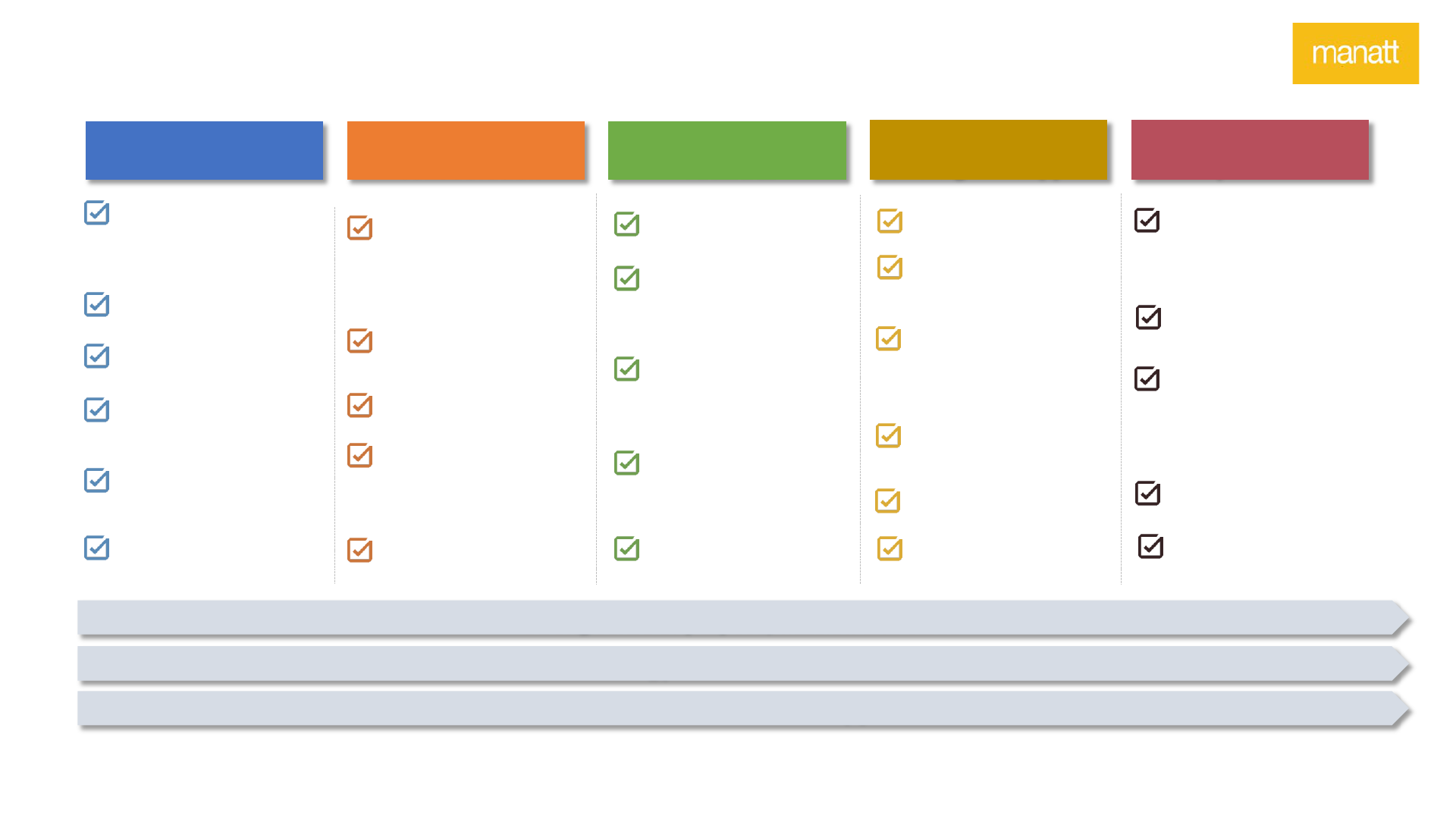
Recognize, Stabilize &
Resource the Workforce
Improve Oversight of and
Increase Penalties for Nursing
Homes
Consolidate and Strengthen
Response Through a Central
LTC Emergency
Operations Center
Implement “Reopening” Plan
and Forward-Looking Testing
Strategy
Strengthen Emergency
Response Capacity
Stabilize Facilities &
Bolster Workforce
Strengthen the ability to plan, coordinate
and execute effective responses to the
emergency and potential surges
Increase the responsibilities of and
support for New Jersey’s nursing homes
and their workers in the short and
longer-term
Increase Transparency &
Accountability
Build More Resilient &
Higher Quality System
Implement stronger mechanisms to
ensure a greater degree of accountability
and increase transparency through data
and reporting
Implement structures for stronger
collaboration and advance payment and
delivery reforms, including increasing
reliance on home- and community based
services (HCBS)
Institute COVID-19 Relief
Payments for Facilities &
Review Rates
Implement Strategy for
Resident & Family
Communications
Institute New Procedures to
Regulate and Monitor Facility
Ownership
Rationalize and Centralize LTC
Data Collection and Processing
Improve Safety and Quality
Infrastructure in Nursing
Homes
Strengthen State Agency
Organization and Alignment
Around LTC
Create Governor's Task Force
on Transforming New Jersey’s
LTC Delivery System
Core Recommendations
1
2
3
4
5
6
7
8
9
10
11
Note: Many of these recommendations are interrelated; the order of recommendations does not indicate relative priority.
22

Consolidate Response Effort Through a Central LTC Emergency
Operations Center: Context
• To manage reopening and potential future surges, New Jersey will need a tightly managed, unified
response and “true north” to coordinate resources and communications particularly in light of a
large fragmented LTC industry.
• New Jersey’s emergency management central command structure is widely seen as organized and
effective. It is unique in its organization under the State Police, but like many states, it more
frequently focuses on incident/hazard response and natural disasters, coordinating through a
network of county offices and a large number of highly decentralized public health offices.
• In support of the COVID-19 response, New Jersey reactivated a regional medical coordination
center (MCC) model, which has been effective in managing hospital capacity.
• However, in spite of an expanded emergency response focus on LTC facilities, there are many
moving parts and alternative mechanisms for nursing homes and other LTC facilities related to
reporting, seeking supplies (PPE and testing equipment) and addressing urgent issues. Facilities
have varying capacities to absorb and appropriately respond to the information and direction.
• With sufficient resources, DOH could mount a central infrastructure or capacity that coordinates
all activity and communications for nursing homes and LTC, which have proven to be the “eye of
the storm” in the COVID-19 pandemic.
Examples From Other States
• Delaware activated its State
Health Operations Center
(SHOC), which provides
command and control for all
public health emergencies.
SHOC operations include
“Points of Dispensing,”
alternate care sites, and a
joint centrally located
information center that
includes workers from
multiple state agencies.
• Colorado’s Unified Command
Center launched a Residential
Care Task Force which rapidly
implemented actions to
mitigate COVID-19 spread.
1
Context
23

Near-Term Recommendations
1. Establish New Jersey Long-Term Care Emergency Operations Center (LTC EOC) as the centralized command and resource for LTC COVID-
19 response efforts and communications.
• The LTC EOC would build on proven regional infrastructure and supplement (but not duplicate) and work in concert with the current
statewide COVID-19 emergency response efforts, as led by the Coronavirus Task Force, and supported by the New Jersey State Police’s
Office of Emergency Management (OEM).
• The LTC EOC would be led by DOH and staffed by DOH, Department of Human Services (DHS), or other agency staff (or through
contract support) as determined by DOH and DHS leadership. The LTC EOC team could also include clinicians, public health experts,
elder affairs and disability services representatives, emergency response/ New Jersey OEM representative(s), and other stakeholders
as DOH deems appropriate.
• The LTC EOC would have ongoing, direct communication mechanisms and feedback loops, including an advisory counsel, to obtain real-
time input from facility owners and staff, unions, resident/family advocacy representatives, and experts in the needs of special
populations, among other stakeholders, as appropriate.
• In addition, the LTC EOC would have a DOH staff person as the designated liaison to the industry.
• The LTC EOC would be charged with providing guidance to the State/OEM team to ensure that supplies are secured and distributed
rationally, critical staffing shortages are identified and solutions developed, problems are quickly surfaced and addressed, the
operational aspects of planned policies are vetted with industry and key stakeholders, and that policies and guidance are effectively
communicated to all stakeholders in order to ensure coordination and effectiveness.
Consolidate Response Effort Through a Central LTC Emergency
Operations Center: Recommendations
1
Indicates that a recommendation requires statutory or regulatory change.
24

Near-Term Recommendations
Consolidate Response Effort Through a Central LTC Emergency
Operations Center: Recommendations
1
• A dashboard could be developed (expanding on the current emergency data sources) to provide a real-time line of sight into on-
the-ground challenges and emerging issue areas and to proactively, for example, where and when a facility may need more than
30-days of PPE on hand.
• In addition to coordinating resource distribution, the LTC EOC would develop additional state guidance and federal guidance and
emerging best practices related to COVID-19-related infection control, symptom monitoring, use of telehealth and other. As with
the resource distribution guidance, the operational aspects of planned state guidance—including guidance suggested in other
recommendations—would be vetted with key stakeholders to ensure successful implementation.
2. Evaluate Regional Coordination Aligned with Hospital MCC Model
• New Jersey had a legacy regional medical coordination center (MCC) model* for disaster response (akin to the Federal Emergency
Management Agency (FEMA) Medical Operations Coordination Cells (
MOCCs)) to help facilitate regional capacity coordination and
communication across hospitals in the event of an emergency. DOH reactivated three regions to support the COVID-19 inpatient
response. A similar structure would be beneficial for LTC facility coordination, but is more challenging to stand up.
• One option is to expand on the existing regional MCCs and pair hospitals with nursing homes for infectious disease and infection
control consultation and emergency resource coordination, including potentially testing support as needed. This would require
additional funding and should be discussed as a potential model with FEMA among others.
*New Jersey consolidated its MCC operations from five into one center in 2018.
25

Design and Implement a “Reopening” Plan and Forward-Looking Testing
Strategy for Nursing Homes: Context
• Nursing homes support short stay (such as post-acute care rehabilitation) and long stay
(residential) needs and are critical providers of palliative care and end-of-life care for many. Most
of the short stays have stopped with the COVID-19 outbreak, but, as the health system resumes so-
called elective cases, patients will require high-quality, safe nursing home services and New
Jersey’s facilities will need to accept patient transfers.
• The nursing home ecosystem relies on many individuals from outside the facility, from medical
providers, to therapists, social workers, faith-based leaders, and health plan care managers, as well
as ancillary service providers. Family and other visitors and volunteers are also essential,
providing social visits and supplemental support services, including feeding, bathing, dressing,
personal care and other functions.
• In order to “reopen” nursing homes and resume normal operations, however, critical steps are
needed to fully prepare for a possible second wave and/or isolated outbreaks and protect
residents and staff to the fullest extent possible.
• New Jersey will need to provide clear guidance, direction and protocols, including on testing and
supplies, and facilities must act accordingly to ensure that nursing homes can safely reopen to
key providers such as hospice as well as visitors and new residents, that potential infections can be
identified and interventions swiftly implemented, and that there are sufficient contingencies in
place in the event of new crises. New Jersey has made progress in these areas, but additional work
is necessary.
2
Context
New Federal Guidance
• On May 18, the U.S. Department of
Health and Human Services (HHS)
issued nursing home reopening
guidance for states focused on a
phased approach:
o Criteria for relaxing certain
restrictions and mitigating risk
of resurgence and factors to
inform decision-making
o Considerations allowing
visitation and services
o Recommendations for
restoration of survey activities
• On May 19, the Centers for Disease
Control and Prevention (CDC)
updated and expanded its
guidance
for nursing homes, related to tiered
requirements by phase, testing
plans, and infection control.
26

Near-Term Recommendations
1. Develop a plan and provide guidance for how New Jersey nursing homes can comply with and implement
federal guidance on reopening. Through the LTC EOC, seek and incorporate feedback from stakeholders including
nursing homes, hospitals, and other providers on feasibility and clinical considerations.
• The guidance should provide, as a condition of reopening, that every facility have the following:
o Adequate isolation rooms/capabilities and the ability to cohort both staff and patients;
o An adequate minimum supply of PPE and test kits; and
o Sufficient staffing and a staffing contingency plan and appropriate staff training to carry out its responsibilities.
• The guidance should define acceptable models of cohorting (e.g., single rooms, separate wings/floors), the
staffing levels that must be in place, and how PPE and testing will be made available to facilities that are
unable to obtain them on their own.
• Implement a centralized FAQ resource, education sessions and focus groups to support nursing homes in
implementing this guidance.
• Require facilities to attest to meeting all requirements before opening their facility to new residents and
others, including family members, and if – at any time after opening – the circumstances change, they are
obligated to report any gaps that need to be addressed through the emergency center communications
mechanism.
• Do not permit hospitals to discharge patients to nursing homes unless such attestations are in place.
• The LTC EOC, with support or “strike” teams, will regularly check in on facilities’ capacity to reopen or stay
open, and where necessary, provide assistance to the facility during the public health emergency.
• Plan for the changes in policy and operations that may be needed if the flexibilities currently authorized
under federal 1135 waivers expire before future waves.
Design and Implement a “Reopening” Plan and Forward-Looking Testing
Strategy for Nursing Homes: Recommendations
New Federal Guidance
On May 18, the U.S. Department of
Health and Human Services issued
nursing home reopening guidance
(
link) for States focused on a phased
approach:
o Criteria for relaxing certain
restrictions and mitigating the
risk of resurgence and factors
to inform decision-making.
o Considerations allowing
visitation and services in each
phase
o Recommendations for
restoration of survey activities
On May 19, the CDC updated and
expanded its guidance for nursing
homes, related to tiered
requirements by phase, testing
plans, and infection control (
link).
Examples From Other States
• Maryland has three types of statewide
strike teams support nursing homes:
testing teams (test and provide
instruction on cohorting), assistance
teams (assess equipment and supply
needs, triage residents), and clinical
teams (provide medical triage and
stabilize residents in the nursing home
to prevent transport to hospitals).
• Pennsylvania deployed a Medical
Assistance Team to provide staffing
support to facilities in need. The State
also developed detailed
guidance on
cohorting in response to test results.
• Minnesota designated nearly a dozen
LTC facilities as “COVID support sites.”
Facilities must be vetted by the state to
ensure they have adequate staffing,
supplies and infection-control
standards to accept COVID-19 patients,
including the ability to cohort
residents.
2
27

Near-Term Recommendations
2. Back-up Plan for Patient Placement in Event of Regional Outbreak or Surge
• The state should be prepared to support and quickly stand up at least three regional hub facilities for COVID-positive patients who do
not require hospitalization to manage capacity and centralize expertise in the event of future waves or case surges that overly tax the
system’s capacity to manage care.
• The LTC EOC and facilities should regularly monitor current capacity and intervention or patient redirection needs.
3. Forward-Looking Comprehensive Testing Plan
• New Jersey issued a mandatory testing Executive Directive on May 12 for nursing home residents and staff, which will provide a
baseline. The Executive Directive permits monetary penalties for non-compliant facilities; DOH should impose these penalties as
appropriate once there are sufficient testing kits available.
• Going forward, New Jersey will need a practical, feasible and flexible forward-looking testing policy:
Capacity to evolve over time:
• Should account for both advances in saliva testing, point-of-care
and serological testing and the ability to pivot to individualized
testing over frequent broad testing at the appropriate time.
• Future testing policies should consider the risk of spread by
group or setting, as well as the relationship to local infection
rates, which will change over time.
• Should include a combination of symptom screening and testing
for visitors with flexibilities for frequent visitors who were
previously tested and attest to certain infection control
protocols.
• In the event recurring testing is needed, the protocols should
prioritize the least invasive, most expedient methods available.
Centralized supports should include:
• Clear guidance for nursing homes that are able to
implement and manage a robust testing process in-house or
with their own system resources and associated funding
information.
• A mechanism by which nursing homes can partner with
select “hub” hospitals, based on the regional coordination
structure (as was successful in the Southern New Jersey
testing pilot) or preferred vendors.
• A network of preferred labs.
• Capability to quickly stand up state/hospital-supported
mobile testing units in the event of a surge.
Guidance on staff, supplies and funding:
• Facilities should provide on-site testing
opportunity to staff.
• Protocols should be developed related to staff
who work at multiple locations and
communication of testing results.
• Support for overall funding and supplies should be
developed through LTC EOC to ensure rational
allocation; nursing homes should be prioritized for
testing supplies.
• Long-term and ongoing reimbursement needs to
be further worked out at state and federal levels.
2
Design and Implement a “Reopening” Plan and Forward-Looking Testing
Strategy for Nursing Homes: Recommendations (cont.)
28

Near-Term Recommendations
4. Back-up Staffing Plan
• With ongoing testing, it is likely that staff – potentially on a rolling basis – will need to be quarantined or take sick leave due to exposure to
the virus (and/or for asymptomatic staff to be moved to COVID-19 wings/units).
• Each nursing home must develop a staffing back up plan, using the LTC EOC communication mechanism to alert the state to staffing
shortages. Options for ensuring adequate staffing will include a combination of (among others):
o “Bridge teams” (which could be formed in collaboration with hospitals, for example) to provide immediate temporary support;
o Staffing back up contracts negotiated by facilities, with encouragement to contract on a regional basis and potentially in partnership
with hospitals to achieve advantages of scale;
o National Guard deployments;
o Improved operations of the “Call to Serve” (volunteer) registry to improve vetting of volunteers qualifications and willingness to
volunteer in certain settings.
• Require nursing homes to report on staff quarantined or taking sick leaves to identify new or looming shortages.
Design and Implement a “Reopening” Plan and Forward-Looking Testing
Strategy for Nursing Homes: Recommendations (cont.)
Intermediate to Long Term Recommendations
• Given the financial challenges and costs faced by health care providers due to the pandemic, some nursing home operators in New Jersey may file for
bankruptcy or indicate an inability to continue operations.
• New Jersey should plan for such economic distress scenarios and evaluate options for receivership, management support and other mechanisms to
support distressed facility operators to ensure continuity of high-quality services to residents if needed.
2
29

Implement Strategy for Resident & Family Communications: Context
Examples From Other States
• New York strongly encourages nursing
homes to develop a communication
protocol for family, loved ones and
residents when visitation is suspended
that includes notification of suspected
cases of COVID-19 and regular updates.
• Massachusetts launched a family
resource line that is staffed seven days
a week from 9 a.m. to 5 p.m. Staffers
coordinate with state agencies to find
answers to callers’ questions, in
addition to directing them to the state’s
nursing home resource site.
• Florida is partnering with the
Alzheimer’s Association and other
stakeholders to distribute tablets
statewide and provide training to
nursing home and assisted living facility
residents to enable communication
with family.
Context
• Restricting visitation at the peak of the COVID-19 pandemic was necessary to
protect nursing home residents; however:
o It cut residents off from regular communication with loved ones, and
o It prevented family members from playing a role in caring for residents and
monitoring the day-to-day operations of nursing homes.
• DOH has taken steps toward addressing these issues, such as issuing a
directive
to nursing homes in early April (in line with state statute and regulations) prior to
related federal guidance to notify all residents and staff members of suspected or
confirmed cases of COVID-19.
• Additional protocols and resources should be put in place to ensure frequent and
regular communications between families and residents and facility staff during
periods of restricted visitation.
• In addition, support is needed to ensure residents are able to leverage telehealth
opportunities and ensure continuity of care.
3
30

Near-Term Recommendations
• Develop guidance establishing expectations for nursing homes’ communications with residents and staff, families, and other representatives,
including Medicaid managed care plans and care managers, covering:
o Frequency of communications between (1) nursing homes and families, and (2) residents and their families.
o Content of communications, including updates on the resident, the facility, and COVID-19 cases.
• Disseminate guidance to residents, families, and representatives on the process for elevating concerns to nursing home staff, Medicaid
managed care plans, and relevant branch of the state (e.g., DOH or LTC Ombudsman).
• Strengthen MLTSS contractual requirements for care manager responsibilities at times when visitation is restricted.
• Further publicize process for nursing homes to request up to $3,000 to purchase communicative technology (e.g., iPads, Amazon Echo, etc.)
paid for using civil monetary penalty funding pools.
• Require nursing homes to dedicate a staff member to manage communications across residents, their families, and other representatives,
including supporting residents with using technology for personal calls and telemedicine.
Implement Strategy for Resident & Family Communications:
Recommendations
Intermediate to Long Term Recommendations
3
31

Recognize, Stabilize & Resource the Workforce: Context
Examples From Other States
• Illinois nursing home workers
secured a new contract that includes
an additional $2/hour for employees
working during the COVID-19 stay-at-
home order. The contract also
increased base pay rate to at least
$15/hour and expanded sick leave.
• Massachusetts funded a $1,000
signing bonus to workers who
registered through its LTC staffing
portal to work a minimum number of
hours at a nursing facility. Eligible
staffing types include: RN, LPN,
CNA/Patient Care Tech, OT, OTA, PT,
PTA, LICSW, and activities staff.
1
Neither New Jersey’s progressive paid sick leave policies (N.J. Stat. Ann. § 34:11D-8 (West)) nor the federal Families First Coronavirus
Response Act provisions relating to sick leave extend to all nursing home workers
Context
• Nursing home staff face a high risk of contracting and/or transmitting COVID-19
while caring for vulnerable residents.
• Nursing home staff earn close to minimum wage, have inconsistent access to
health coverage and sick leave
1
and are often not recognized or valued as part
of the health care workforce, factors that contribute to chronic staffing
shortages and turnover, and training gaps.
• Many nursing home staff work across multiple facilities to support their families.
• While some nursing homes in New Jersey have independently extended wage
enhancements to staff during the emergency, the state has not instituted wage
pass-throughs or other forms of supplemental pay to workers.
• Wage enhancements can help mitigate the need for staff to continue to work
across multiple facilities, decreasing the risk of exposure for themselves and
residents.
4
32

Near-Term Recommendations
Recognize, Stabilize, & Resource the Workforce: Recommendations
• Ensure all nursing home staff have access to paid sick leave.
• Institute wage enhancements for staff who work a minimum number of hours in a single nursing home, now and for future
COVID-19 waves (could be funded through Medicaid or Coronavirus Aid, Relief, and Economic Security (CARES) Act funding).
Intermediate to Longer-Term Recommendations
• Work with legislature to create a workforce development and appropriations package to:
o Design and implement minimum staffing ratios for RNs, LPNs, and CNAs that are aligned with differential needs of
nursing home residents (e.g., residents with dementia). Prohibit professional staff serving in administrative roles from
counting toward these ratios.
o Establish a wage floor and wage pass-throughs for future Medicaid rate increases. Wage increases should be linked to
expectations for additional training for workers to strengthen quality of care.
• Strengthen training and certification requirements and opportunities, including annual in-service education requirements to
build skills and expand scopes of practice.
• Seek federal and state funding to develop a direct care workforce career development program focused on recruitment,
training and career advancement.
4
33

Institute COVID-19 Relief Payments for Nursing Homes & Review
Rates Going Forward: Context
Relevant Federal Guidance
• In March, CMS released a Disaster
Relief State Plan Amendment
template, permitting states to
temporarily increase rates for
services covered through Medicaid
fee-for-service
• In mid-May, CMS released
guidance to states on ways to
effectuate temporary provider rate
increases through Medicaid
managed care.
Context
• To respond to COVID-19, nursing homes have additional costs related to cleaning, facility
reconfiguration, PPE, testing and staffing, while they are losing revenue from the lack of
rehabilitation stays after elective procedures. Nursing homes have a short-term need to fund these
new costs to promote safety.
• To date, approximately one-third of states have made COVID-19 relief payments to nursing homes to
offset increased costs and to ensure sufficient liquidity to maintain full operations; New Jersey has not
done so.
• Medicaid is the largest payer for LTC services. While DHS has instituted multiple rate increases since
fiscal year 2016, current Medicaid rates do not anticipate wage increases and state-of-the-art
equipment, among other expenses.
• Some nursing homes across the country, however, have generated large profits.
o For example, nationwide in
2016, for-profit SNFs had an average Medicare profit of 14%, with
one-quarter of facilities having a profit of over 20.2%. However, Medicaid is the largest payer
for nursing homes and individual facility potential profitability also depends in part on whether
and to what extent the home serves Medicaid-covered residents.
o These profits may represent funds that are diverted from the provision of care and facility
upgrades. DOH and DHS have limited insight into how nursing homes are using their publicly-
funded revenues.
5
34

Institute COVID-19 Relief Payments for Nursing Homes & Review
Rates Going Forward: Recommendations
Near-Term Recommendations
• Rely on federal coronavirus relief and stimulus funding, including
CARES Act funding, and/or Medicaid to provide temporary relief
payments to nursing homes. Any new disbursements should net out
previously received CARES Act funding. (See Appendix for description of
CARES Act funding.)
• New Jersey may want to consider whether temporary relief payments
should be tied to compliance with reporting and other requirements.
Examples From Other States
• Connecticut increased nursing home
provider rates by 10% to cover:
o Staff retention bonuses, overtime,
and shift incentive payments
o New costs related to screening
visitors, PPE, and cleaning and
housekeeping supplies
o Other COVID-related costs
• Massachusetts temporarily enacted a 10%
Medicaid rate increase for nursing homes
to support additional staffing, infection
control and supply costs. Facilities that
create dedicated COVID-19 wings and
units and follow necessary safety
protocols are eligible for an additional
15% rate increase.
5
35

Institute COVID-19 Relief Payments for Nursing Homes & Review
Rates Going Forward: Recommendations (cont.)
1. Review Rates and Link Any Increases to Quality and Safety
• Contract with a vendor to conduct a rate study to assess: (1) sufficiency of Medicaid nursing home rates to cover direct care and administrative costs (e.g.,
reporting); (2) the distribution of nursing home spend between direct care, administrative costs, and other expenses; (3) nursing home resident acuity levels; (4)
potential to apply acuity adjustments to rates; and (5) rate implications of staffing recommendations in this report. Vendor should have experience working with
at least 10 other states and/or health insurance carriers on health rating and have expertise on rates for nursing homes.
• If rate modifications are recommended, seek legislative authorization for increases. Require a portion of any rate increase be passed through to nursing home
workers, similar to state legislation passed for personal care services, and tie increases to quality and safety improvements. For example, require facilities to:
o Meet new staffing level requirements;
o Have staff participate in a state direct care workforce career development program; or
o Implement policies for improved coordination with MLTSS and care managers.
• Review DHS’s multi-year Medicaid value-based payment strategy, including the Quality Incentive Payment Program, to ensure incentives focus on key priorities
for quality improvement and consider whether incentives are enough of a “carrot” to impact behavior.
2. Create a Direct Care Ratio (DCR) Reporting and Rebate Requirement
• To ensure payments to nursing homes–including any increases–are used for resident care, seek legislative authorization to develop a nursing home DCR—similar
to the medical-loss ratio (MLR) requirements that apply to insurance plans—that requires facilities to use no more than a certain percentage of revenues for
administrative costs and profits. Insurance MLRs range from 80-89%. Set DCR based on historical cost reports and adjust as needed based on new financial
reporting requirements.
o Audit cost reports and recover payments in excess of the DCR requirements.
o Monitor performance of nursing homes to inform adjustments to DCR.
Intermediate to Longer-Term Recommendations
5
36

Institute New Procedures to Regulate and Monitor Nursing Home
Ownership: Context
Examples From Other States
• Massachusetts provides
an opportunity for public
input on any proposed
CHOW or notice of intent
to sell or close a SNF.
Applicants must
submit
three years of projected
profit and losses, and
projected three years’
capital budget.
• New York requires a CON
review process, including
a public hearing, for
CHOWs.
Context
• Nationally and in New Jersey, the ownership of facilities has become heavily for-profit and is frequently changing
hands. A facility may change ownership multiple times in a single week.
• For-profit facilities have opaque financials and can use complex ownership and management structures to obscure
the entities responsible for delivering care, curtailing the ability of the state and residents to hold them accountable.
• Rigorous change of ownership (CHOW) requirements are critical for ensuring accountability and promoting quality
and stability of the workforce. Current DOH processes fall short:
o DOH currently collects information from anyone with a 10% director or indirect ownership interest; however,
many states require the disclosure of anyone with a 5% (or less) interest.
o CHOWs are not public, and DOH has not historically disapproved a CHOW.
o Facilities that change ownership are not subject to any additional oversight or reporting following the change.
• The certificate of need (CON) process provides a more rigorous review of new facilities; however, a loophole in the
CON process allows new facilities to acquire previously approved but not utilized “paper beds” from other owners.
o Every five years, a facility may request approval of up to 10 beds or 10% of its licensed bed capacity, whichever
is less, without CON approval. Some facilities never actually add the beds, but holds approval or gives
approved beds to a “paper bed” broker. New owners can acquire “paper beds” (the beds acquired through the
add-a-bed process but never used) through the CHOW process, allowing them to skip the CON process
entirely.
6
37

Institute New Procedures to Regulate and Monitor Nursing Home
Ownership: Recommendations
• Increase transparency in CHOWs.
o Require disclosure of all direct and indirect owners having any or a 5% or more (states vary in their approaches) ownership interest and
all related parties that will be providing services to the facility.
o Require a proposed budget to be submitted with the CHOW application.
o Publicly post proposed CHOWs and solicit constituents’ feedback.
o Require closer scrutiny of quality and compliance with MLR requirements in the 2-3 years following a CHOW; including annual licensure
surveys.
o Impose a waiting period following a CHOW during which another CHOW cannot occur.
• Do not approve CHOWs when DOH has concerns regarding the prospective owner; instead, if necessary to protect residents, propose
temporary receivership or solicit a temporary manager. To the extent permitted by law, DOH could have a standing contract with a vendor that
can be triggered if the need arises.
• Close loopholes that allow significant changes without DOH oversight.
o Require prior approval before allowing a facility to delegate facility management to a third party.
o Revise the regulation to clarify that all beds added through the “add-a-bed” process solely be used by the facility and make these beds
nontransferable.
Intermediate to Longer-Term Recommendations
6
38

Improve Oversight of and Increase Penalties for Non-Compliant Facilities:
Context
Examples From Other
States
• Nebraska commenced
receivership against Skyline, and
Minnesota has been a receiver
and engaged a managing agent
for a facility at least three times
in the last ten years.
• Massachusetts creates and
publishes its own performance
report for each facility, which
includes changes of ownership.
It also performs state licensure
surveys biannually. Its Center for
Health Information and Analysis
collects significant data about
the quality, affordability,
utilization, access, and
outcomes of the health care
system in the state.
Context
• Survey and complaint processes are primary mechanisms for protecting residents who are unable to
advocate for themselves.
• DOH’s certification and survey and complaint investigatory arm has been historically under-resourced and
understaffed.
o DOH is unable to perform all of its CMS-mandated activities. It has 4,000 backlogged complaints, 700
of which are high priority due to the nature of the complaint. Some complaints are over two years old.
• DOH performs CMS-required facility surveys timely; however, there is broad agreement that the CMS survey
process is flawed. For instance, nursing homes are subject to the same survey intensity regardless of
historical compliance, and while the surveys are unannounced, facilities are often able to predict when they
will occur and ramp up staffing and alter existing procedures to produce better outcomes.
• CMS has authority over the sanctions and penalties imposed for CMS survey deficiencies. Penalties are
frequently reduced by CMS through the appeals process. Even when financial penalties are imposed, they do
not deter bad behavior. Nationally and in New Jersey, facilities have the same problems year-over-year.
• DOH has independent authority to impose penalties, revoke a license, appoint a receiver or temporary
manager or cease new admissions for violations of New Jersey requirements. Historically, DOH has not
exercised this authority.
• Complaints and other quality data are reported to several different entities, including the LTC Ombudsman,
DHS, Medicaid managed care plans and DOH, but are not aggregated. No one has a full picture of the quality
of care or recurring issues.
7
39

Improve Oversight of and Increase Penalties for Non-Compliant Facilities:
Recommendations
• Increase DOH funding and staff so that surveys can be performed and complaints can be investigated timely; perform licensure surveys of poor
performing facilities at least every two years that focus on fewer areas and validate through observation that the facility actually complies with its
policies. Require DOH to perform a survey of infection control and sanitation compliance of each facility every six months.
• Impose more serious sanctions—using New Jersey’s independent authority as needed—for top priorities.
o Impose more serious sanctions for infection control deficiencies.
o Exercise existing authority to impose more serious sanctions for non-compliance with state licensure requirements. Penalties should escalate
when the same deficiency is found on a subsequent survey or during a complaint investigation.
o Revise the regulations to increase the financial penalties for non-compliance.
• Terminate, revoke the license of, require temporary management of, or prohibit new admissions to poorly performing facilities (e.g., ones that have
repeat serious deficiencies, such as reusing single use equipment with multiple residents, or have a One Star Rating for consecutive years).
• Evaluate whether any willing provider requirement should continue – i.e., whether managed care plans should be empowered to end or suspend their
contracts with troubled facilities – and identify any other ways DHS can enhance Medicaid managed care plans’ role in monitoring quality as part of
network management and in coordination with DOH’s quality oversight.
• Leverage data obtained by CMS, DHS, DOH, Medicaid managed care plans, and the LTC Ombudsman to develop more robust reporting to identify
consistently poor performing facilities and those with a high number of substantiated complaints.
• Produce a nursing home report card for each facility that includes quality, complaint, and other information.
Intermediate to Longer-Term Recommendations
7
40

Rationalize and Centralize LTC Data Collection and Processing: Context
8
Examples From Other
States
• Massachusetts published its first
statewide nursing facility industry
report in 2019, highlighting
occupancy, operating expense,
utilization and staffing data, and
leveraged this data reporting
infrastructure to quickly collect
data from nursing homes on their
COVID-19 needs.
• Minnesota publicly provides
information on nursing home
staffing, rates, and quality.
• California collects and releases
comprehensive LTC facility
financial
data and utilization data
in machine-readable and easily-
analyzable formats as part of its
transparency efforts.
Context
• New Jersey’s LTC industry, DOH, DHS and DOH’s Division of Public Health Infrastructure,
Laboratories & Emergency Preparedness are not equipped with the technology, data, or analytic
staff to support ongoing data-driven oversight or to rapidly respond to public health
emergencies:
o LTC facilities struggle to understand and submit reliable data to satisfy a patchwork of
ever-changing federal, state and Medicaid managed care plan reporting requirements.
o State regulators are challenged to meaningfully collect, curate, analyze and use the
limited data received to support their core regulatory and program oversight functions
(e.g., capacity to measure and monitor population health/acuity).
• Industrywide underinvestment in modern technological and analytic infrastructure and
reporting has created an opaque, data-poor regulatory ecosystem that lacks nimbleness to
scale to regulatory need.
• Similar to other states, during the pandemic, New Jersey has relied on contractors and
associations to scale its information sharing capacity and deploy the most expedient system to
stand-up in some ways “makeshift” systems to quickly respond to the crisis, but will need to
migrate that data capacity and management in-house or cement a longer-term solution.
41

Rationalize and Centralize LTC Data Collection and Processing:
Recommendations
Near-Term Recommendations
1. Take actions to improve exchange of and access to critical information:
o Consolidate state and federal LTC COVID-19 reporting through the New Jersey Hospital Association (NJHA) PPE, Supply & Capacity portal; assess
current LTC facility COVID-19 reporting demands and standardize and consolidate them, where possible.
o Migrate NJHA portal onto DOH infrastructure; clearly communicate changes to LTC facilities.
o Establish centralized state LTC facility communication protocols to reduce duplicative outreach and increase information sharing; centralize
internal COVID-19 and LTC facility data reporting and storage to support cross-governmental information sharing (e.g., DOH, DHS, county OEM,
local health departments); establish automatic “alerts” to governmental points-of-contact, generated from LTC facility COVID-19 data
submissions that exceed established thresholds.
o Provide smaller LTC facilities with support (e.g., financial, staffing, technical assistance) to improve their health information technology (HIT)
capabilities, including data reporting.
o Compile complaints received across state agencies and review on a regular basis at the central emergency response system.
2. Implement new data reporting requirements:
o Focus should be on increasing market transparency and facilitating ability to enhance regulatory oversight.
o Require LTC facilities to publicly post (i.e., on websites) policies otherwise required to be compliant with state law, including outbreak response
plans, and have designated staff available to answer questions on policies.
8
42

Rationalize and Centralize LTC Data Collection and Processing:
Recommendations (cont.)
1. Develop centralized, rationalized, and scalable data and information-sharing infrastructure and protocols.
o Identify opportunities to eliminate duplicative reporting and/or standardize reporting requirements.
o Establish a centralized, cross-agency workgroup to monitor LTC-related data reporting.
o Assess state HIT needs to support technology-enabled and data-driven regulatory oversight across departments and
prospective uses (e.g., New Jersey Health Information Network, DHS risk adjustment); identify opportunities to centralize
and modernize state health data infrastructure, processes, and analytic capabilities.
o Assess LTC facility HIT needs to support population health management, interoperability, and modernized reporting
requirements.
o Identify and apply for federal funding to support infrastructure development.
2. Implement new data reporting requirements to increase market transparency and enhance regulatory oversight.
o Identify new data required from LTC facilities to support priority, cross-departmental regulatory needs; solicit nursing home
and managed care plan feedback on draft requirements, obtaining input on most efficient method of data collection and
specification; evaluate duplication of reporting across federal government, state agencies and managed care plans that might
be streamlined or automated; promulgate reporting requirements.
o Analyze data for oversight purposes, and make results public when possible.
o Produce public, annual report on the performance of New Jersey’s LTC system.
Intermediate to Longer-Term Recommendations
8
43

Improve Safety and Quality Infrastructure in Nursing Homes: Context
Context
• Promoting a safe and effective LTC system is a shared goal. Nursing homes must be safe, but they also must raise the bar
and improve quality.
• Infection control deficiencies are the most common type of deficiencies cited for nursing homes; Approximately
one-
third
of nursing homes surveyed by New Jersey were cited for an infection prevention and control deficiency in 2017.
Lessons learned from an infection
outbreak in a New Jersey facility in 2018 that resulted in the mortality of 11 children
could have been more widely implemented and leveraged as a catalyst for cultural change for other facilities and the
state.
• Quality improvement has multiple dimensions including structural (i.e., appropriate staffing, infection control expertise,
access to clinical consults as needed); process (i.e., protocols for infection control, training on use of PPE, etc.) and
outcomes (i.e. reduction in adverse events like falls with injury, bed sores, onset of pneumonia, increase in social
connectedness, functioning level, satisfaction with service and support by residents and families, among others).
• Level of clinical engagement and oversight (including role of the medical director), ensuring continuity of care during an
emergency (including review of care plans, advance directives, palliative care, coordination of medical care, and
transitions across care settings), and competency-based staffing and training are also important factors in building a
culture of quality.*
• Federal and state LTC oversight processes focus almost exclusively on citing and penalizing facilities. These are critical
functions but there are few opportunities for facilities to receive support and technical assistance to improve their
quality. Those that need help may be hesitant to disclose challenges for fear of penalties.
o New Jersey’s Infection Control Assessment & Response (ICAR) program provides consultations to facilities to
strengthen infection prevention, but funding for ICAR is dwindling, its capacity is limited, and its services do not
extend to broader quality improvement.
Examples from CMS and
Other States
• CMS has a targeted Probe
and Educate program that
helps providers reduce
claims denials and appeals
through one-on-one help.
• Florida deploys Rapid
Emergency Support Teams
to 200+ LTC facilities to
train staff on infection
controls and augment
clinical patient care.
• Missouri has a Quality
Improvement Program that
offers individual nurse
consultation and technical
assistance for the
completion of certain
assessments, quality
improvement, as well as
support groups and
workshops.
9
*DOH has provided financial support for nursing home workers to attend training programs , such as those through Association for Professionals in Infection Control and Epidemiology and Rutgers Project ECHO,
but further training initiatives are needed.
44

Improve Safety and Quality Infrastructure in Nursing Homes:
Recommendations
Near-Term Recommendations
• Infection Control
o Mandate that every facility have a senior-level Infection Control Preventionist (ICP)* who reports to
the CEO and the Board of Directors. For facilities with over 100 beds, this position should be full-time
and the person should not have any other responsibilities.
o Request additional funding for the ICAR program (e.g., via civil monetary penalty funding pools).
o In addition, contract with a vendor or other entity able to rapidly assist in training and technical
assistance on infection control. For example, Rutgers University and NJHA have relevant experience to
rely on.
• Broader Quality Improvement
o Provide resources (e.g., civil monetary penalty funding pools) for a program either within DOH (but
outside of the enforcement arm) or a vendor to provide technical assistance to facilities on quality
improvement, best practices, or compliance with specific requirements, and that periodically reviews
whether the technical assistance is indeed improving quality of the nursing homes it supports.
o Consider a pilot program whereby a reviewer follows a cohort of residents for a period of time to see
how the facility’s quality of care is improving (as the survey focus is oriented to review at a given
point in time).
* Despite federal and state mandates for an infection prevention and control program, many facilities lack a culture of infection prevention: staff receives minimal infection control training, and much of it is ineffective
because it is part of long, slide-based training or is simply a handout. There is a federal requirement that each nursing facility have a part-time infection preventionist (IP) at least part-time. 42 CFR § 483.80 (b)). CMS has
proposed to revise this requirement so that a facility only has to ensure that the IP has sufficient time at the facility to meet the objectives of its infection prevention and control program. New Jersey mandates each facility
have an employee who is designated as an infection control coordinator. N.J.A.C. 8:39-19.1
Proposed Responsibilities of ICP
• Developing robust policies and
procedures and a training curriculum for
the nursing home, which should be
informed by best practices and clinical
expertise, and includes training on use of
PPE.
• Evaluating whether the CNA training
curriculum provides sufficient hands-on
training in infection control and
prevention.
• Implementing routine monitoring of
infection prevention activities and initiate
discipline for those who routinely violate
prevention policies.
• Reporting to the CEO and Board of
Directors, at least quarterly, on the
effectiveness of such activities and
number of infections/quarter.
• Requiring nursing homes to perform
quarterly emergency and infection
control drills, i.e. activating their plans to
ensure they are actionable and effective.
9
45

• Infection Control
o Perform targeted surveys every six months to assess whether the facility implemented effective infection control and prevention
measures.
• Quality Improvement
o Require targeted surveys if policies and protocols appear ineffective as evidenced by concerning metrics that do not decrease over time,
such as number of falls, onset of pneumonia, increase in social connectedness, functioning level, satisfaction with service and support by
residents and families.
o Institute a “probe and educate model” to help identify quality of care risks and deficiencies and provide the tools for education and
improvement. This would include a non-punitive review of the facility focusing on viewing policies and procedures in action and access
and use of clinical consults. Resident outcomes information would not be shared with the surveyors. The probe and educate model would
perform a baseline review, then return to the facility to assess improvement following education, and continue the loop until
improvement is made or other action needs to be taken.
o In concert with recommendations from the proposed Governor’s Task Force, evaluate staffing levels and competency by resident acuity
and complexity and impose greater responsibility and accountability on the medical director for quality outcomes.
o Continue to expand DHS’s Quality Incentive Payment Program for nursing homes.
Intermediate to Longer-Term Recommendations
Improve Safety and Quality in Infrastructure Nursing Homes:
Recommendations
9
46

Strengthen State Agency Organization and Alignment Around LTC:
Context
Examples From Other States
Massachusetts’ LTC
licensing, survey, regulatory,
policy and rate-setting
agencies are all housed
under the Executive Office of
Health and Human Services
(EOHHS). While multiple
agencies, such as
MassHealth (Medicaid), the
Department of Public Health,
Elder Affairs and several
disability and community
services agencies, regularly
collaborate on LTC strategies
and activities, ultimate
decision-making and
accountability for LTC
leadership and strategy lies
with the Secretary of EOHHS.
• Today, oversight of the LTC system is spread across DOH and various divisions within
DHS. No single department or division is responsible and accountable for overseeing
the LTC system as a whole.
• The pandemic has shed light on the need for strong cross-agency alignment and
communication to ensure that the state has a cohesive LTC policy, financing,
licensing, oversight and regulatory strategy and that LTC activities are aligned and
coordinated across the departments.
• From 2008 to 2019, combined staffing at DOH and DHS decreased by approximately
30% and key DOH positions remain open. To help the state be more responsive to the
LTC system during regular operations and emergencies, DOH should focus on
expanding its leadership team to bring in additional LTC expertise.
• Similarly, DHS through the Medicaid program has primary responsibility for care
delivery and financing but lacks the resources to develop essential data analytic
capacity and other expertise needed to move delivery and payment reforms
forward.
Context
10
47

Strengthen State Agency Organization and Alignment Around LTC:
Recommendations
• Consider designating one of the existing Deputy Commissioners or establish a new Deputy Commissioner-level position
at DOH to be responsible for overseeing and coordinating all activity across the LTC system.
• Develop a formal workplan for DOH and DHS to align and troubleshoot on LTC issues and coordinate on key ongoing
priorities impacting both departments, such as data-driven monitoring, quality, and payment methodology.
• Continue effort to fill vacant position for DOH Deputy Commissioner of Public Health Services as soon as possible.
Near-Term Recommendations
• Review current DOH and DHS staffing structures to identify additional positions and LTC expertise that may be needed,
including:
o Ongoing regulatory and licensing oversight at DOH.
o Data analytics at DHS.
Intermediate to Longer-Term Recommendations
10
48

Create Governor's Task Force on Transforming New Jersey’s LTC Delivery
System: Context
Examples From Other States
Massachusetts created the Nursing Facility Task Force
in 2019 via legislation, charged with evaluating ways
to ensure the financial stability of SNFs; considering
the role of SNFs within the continuum of elder care
services; and addressing current workforce
challenges.
California. Governor Newsom issued an executive
order directing the Secretary of Health and Human
Services to convene a cabinet-level workgroup to
develop a “Master Plan for Aging.” The Master Plan
will be a blueprint for state and local government and
the private and philanthropy sectors to “promote
healthy aging” in light of an aging and diversifying
state population. Priorities for the Master Plan
include independence and choice for seniors and will
include recommendations for coordinating federal,
state, and local government programs and services,
and 10-year targets for implementing
recommendations.
• COVID-19 has exposed long-standing nursing home staffing and workforce
challenges, outdated care models that do not reflect the diverse needs of
residents, outdated physical plants of facilities, and other structural
deficiencies in New Jersey’s LTC system. At the same time, the provider
landscape has changed significantly in recent years.
• Most people prefer to remain in their homes as long as possible, supported
by HCBS instead of institutional settings. While New Jersey lagged far behind
with respect to the proportion of LTC provided in the home, it has greatly
increased its provision of HCBS in recent years and is seeking to further
augment its efforts to allow people needing long-term services and
supports (LTSS) to remain in the community.
• New Jersey has an opportunity to be a leader in developing a forward-
looking vision and approach to redesigning institutional and community-
based care models, services, payment, staffing, and best practices for
modernizing facilities to not only better guard against potential future
infections but to transform care for the high-risk individuals who use LTC.
Context
11
49

Create Governor's Task Force on Transforming New Jersey’s LTC Delivery
System: Recommendations
• Establish a Governor’s Task Force charged with developing actionable recommendations to reform the LTC system centered
around person-centered care, safety, quality improvement, workforce engagement and sustainability.
• The Task Force could be comprised of a diverse panel of policymakers, nursing and medical professionals, labor
representatives, experts on LTC and aging and disability policy, consumer/resident representatives, and representatives from
nursing homes (among potentially other providers) appointed by the Governor.
• The Task Force would consider factors related specifically to create the optimal balance of services and supports, including
continued expansion of HCBS, nursing home reforms and broader system reforms.
o Nursing home reforms could consider new care models for nursing homes, optimal nursing home size and configuration
for both resident wellness (e.g., create smaller internal communities that foster on-going relationships with staff) and
infection control, policies for increasing clinical presence in nursing homes, and nursing home staffing levels and ratios
based on acuity or special population needs.
o Broader system reforms could consider technology requirements for all LTC providers to more easily enable telehealth,
career laddering or other models for LTC workforce engagement and advancement, the role of Medicaid managed care
in quality improvement and oversight of nursing homes, and acuity adjustments for Medicaid managed care payments
to nursing homes.
Intermediate to Longer-Term Recommendations
11
50

• Appendix A. Additional Considerations: Federal Collaboration
• Appendix B. Timeline of Key State Actions Addressing COVID-19 At LTC Facilities
• Appendix C. Summary of Federal Actions Addressing COVID-19 At LTC Facilities
• Appendix D. Overview of Selected Federal Funding
• Appendix E. New Jersey Nursing Home Profile
• Appendix F. Analyses of COVID-19 by Region, Quality Ratings, Staffing and
Ownership Type
• Appendix G. Other State and Local Responses
• Appendix H. References
Appendices
51

APPENDIX A. ADDITIONAL CONSIDERATIONS: FEDERAL COLLABORATION
52

Nursing home residents are among the most susceptible to severe illness and adverse outcomes from COVID-19. The national experience and emerging data (not only New
Jersey’s) indicate that the nursing home environment is conducive to the rapid spread of the virus, almost certainly from many of the same underlying systemic issues
discussed in this report.
Responsibility for regulations, oversight, and funding of nursing homes is shared between states and the federal government. While the scope of recommendations in this
report are limited to action by the State of New Jersey and/or the nursing homes under its jurisdiction, several opportunities for federal support of the state’s efforts and/or
closer federal-state partnership around industry transformation are evident. Select examples (by no means comprehensive) include:
Prioritization of COVID-19 Testing for Nursing Home Residents and Staff. Nursing home residents and staff should be prioritized for testing
kits and supplies, with clear direction related to payment responsibility, at both the federal and state level - particularly in the near-to-mid
term as our collective understanding of prevention and treatment options evolves. One option could be for Medicare Part A to cover
recommended testing for nursing home residents. Given the acute need for ongoing testing and monitoring, a national plan for nasal as well
as alternate collection and serological testing for nursing homes should be developed as/if those testing approaches become more reliable.
Stronger Role of Infection Preventionist. Prior to the pandemic, CMS proposed to
lessen requirements for the infection preventionist.
Learnings from the pandemic demonstrate a need for continuous vigilance, and there may be an opportunity to elevate and strengthen that
role, as part of a broader effort to further foster a culture of safety and continuous quality improvement in our nation’s nursing homes.
More Flexible, Targeted Oversight. Effective, targeted state oversight and appropriate intervention for struggling nursing homes is critical –
and all the more tenuous as states face challenging finances and
budget cuts in the wake of sharp economic declines. CMS’s current nursing
home survey requirements (temporary flexibilities for the pandemic not withstanding) are highly prescribed and standardized. Flexibilities
around frequency are needed, including consideration of a model whereby struggling facilities receive more comprehensive surveys more
frequently and stronger performers alternate between full and limited surveys. This could free up resources for the state to focus on and
provide interventions and support for areas that are low performing across all nursing homes nationally, such as infection control.
Increased Funding for Oversight and Technical Assistance. In concert, increased funding for survey and oversight as well as technical
assistance for safety and quality improvement furnished at the federal and
state level is likely warranted.
Additional Considerations – States Need a Federal Partnership
53

54
Availability of HIT Funding. Nursing homes, along with other post-acute and LTC providers, largely have been excluded from federal
efforts to expand the use of electronic health records and health information exchange (HIE). Evaluation of opportunities to enhance
health IT and HIE funding for nursing homes to enable better data analytics, sharing and reporting and to allow nursing homes to
take advantage of the implementation of new Fast Healthcare Interoperability Resource (FHIR)-based application programming
interface (APIs) and expanded trusted information exchange frameworks should be prioritized in the wake of the pandemic.
Better Targeting of PPE. Given the ongoing national shortages of PPE, in its planning for potential future waves or case surges, the
federal government should use FEMA and other resources to both direct most acutely needed PPE for nursing homes and give more
specific guidance on specific types and uses of PPE for nursing home staff and visitors.
Reforms to Nursing Home Staffing and Care Model. A national conversation is needed on staffing ratios, clinical acuity-based
staffing and competencies, and high quality services for distinct sub-patient populations, among other important issues. CMS has
announced the formation of an independent commission to address safety and quality in nursing homes. Further opportunity exists
to reconsider the nursing home model and develop recommendations for forward-looking care transformation.
Increased Flexibility in Care Delivery. The federal government has granted many flexibilities under the public health emergency
period, including expanded use of telemedicine and flexibilities related to staffing. Consideration should be given as to the
flexibilities that should be retained in whole or in part after the pandemic ends.
Additional Considerations – States Need a Federal Partnership (cont.)

APPENDIX B. TIMELINE OF KEY STATE ACTIONS ADDRESSING COVID-19 AT LTC
FACILITIES
55

Key State Actions Addressing COVID-19 at LTC Facilities
Week of February 3
• Facilitated a discussion at the New Jersey Hospital Association on preparing for a novel coronavirus.
Week of March 2
• Guidance issued to LTC facilities on preparing for COVID-19, based on available CDC guidance.
• Memo issued to LTC facilities reminding them of their statutory responsibility to have a disaster response plan.
Week of March 9
• DOH held Coronavirus Preparedness Briefing call with LTC facilities.
Week of March 16*
• Visitors restricted from nursing homes except for end-of-life visits, with screening and protection requirements. Staff monitoring and screening requirements put in place.
• Additional and updated recommendations provided to all LTC facilities, including information on resource planning, resident and staff education, screening protocols,
developing an infection control plan, and surveillance and tracking.
• DOH and DHS submitted to CMS two 1135 waiver requests.
Week of March 23**
• Series of action taken to support and supplement LTC workforce, including extending recertification deadlines, allowing facilities to use certified nurse assistants (CNAs)
certified in another state, and allowing registered medical technicians and certified home health aides to function as CNAs in LTC facilities.
• Executive Order requires all health care facilities, including LTC facilities, to report daily data on their capacity and supplies of PPE to the New Jersey Office of Emergency
Management. Reporting is done through a portal currently hosted by the New Jersey Hospital Association.
Week of March 30
• Guidance issued on statutorily mandated notification of residents, families, visitors and staff in the event of contagious disease outbreak in a facility.
• Infection prevention and mitigation guidance issued on restricting visitors, active screening, cohorting within a facility, ending communal dining, universal masking,
“optimizing” PPE, and reviewing staff contingency plans.
• Guidance issued on hospital discharges and admissions to post-acute settings.
February and March Activity
*Beginning March 19, the New Jersey Hospital Association began hosting weekly infection control conference calls, with DOH participation. These calls continue to date.
**During the week of March 23, DOH also
assisted St. Joseph’s in Woodbridge in relocating all of its residents to a different nursing home that became a COVID-only facility.
56

Key State Actions Addressing COVID-19 at LTC Facilities cont.
Week of April 6
• Outbreak management checklist distributed to nursing homes.
Week of April 13
• State Attorney General announces investigation into nursing home deaths.
• Guidance issued curtailing admissions order.
• Expanded pool of CNAs by allowing personal care assistants and certified medical assistants to function as CNAs, and allowing nursing homes to
hire temporary nurse aides who complete a state-approved online course offered by the American Health Care Association.
Week of April 20
• Statewide list of cases in nursing homes released to the public.
• Following PPE has been distributed to facilities based on self-reported need: 458,000 N95 masks, 2.1 million surgical masks, 58,000 face shields,
27,000 surgical gowns, 1.7 million gloves.
• “Volunteer” portal launched for health care professionals. At least 25 nurses registered through the portal are sent to work in veterans homes.
• Outbreak reporting and response guidelines for LTC facilities issued to local health departments.
• With Rutgers Medical School, hosted a Project ECHO teleconference for LTC providers about infection prevention and control in LTC settings.
Week of April 27
• National Guard medics deployed to two state veterans homes to supplement facility staff.
• With Rutgers Medical School, hosted a Project ECHO teleconference for LTC providers about end-of-life planning in LTC settings.
April Activity
57

Key State Actions Addressing COVID-19 at LTC Facilities cont.
Week of May 4
• Online portal established for the public to anonymously report misconduct in LTC.
• Announcement made that the state’s three veterans homes are offering universal testing. Private consortium of nursing homes and hospitals
announce it will test 10,000 residents and 20,000 staffers at 74 facilities in the state over the course of two weeks.
• State allows temporary emergency licenses to be granted to recent graduates of nursing, physician assistant, pharmacy and respiratory care
therapy programs.
• At least 300 National Guards are deployed to nursing homes across the state.
Week of May 11
• All LTC facilities are required to add a COVID-19 testing plan to their current disease outbreak plan. The testing plan must include:
o Baseline molecular testing of all staff and residents by May 26 (deadline was later extended to May 30).
o Retesting all negative staff and residents within 3-7 days of baseline testing.
o Further retesting in accordance with CDC guidance.
• CMS approved New Jersey’s Medicaid Appendix K: Emergency Preparedness and Response submission.
Week of May 18
• As testing continues, state announces 650 residents at the three veterans homes have been tested (more than half found positive), and 14,000
residents and 42,000 staff at 100 privately run LTC facilities have been tested.
• Issued FAQ on testing plan Executive Directive (see above).
Week of May 25
• Expanded testing plan FAQs issued.
May Activity
58

APPENDIX C. SUMMARY OF KEY FEDERAL ACTIONS ADDRESSING COVID-19
AT LTC FACILITIES
59

Summary of Federal Policy Guidance and Select Additional Actions in
Response to COVID-19 in Nursing Homes
• HHS sent additional provider relief payments directly to nursing homes
(
May 22)
• CDC released updated resources and tools for nursing homes (May 19)
• CDC updated Interim Testing Guidance in Response to Suspected or
Confirmed COVID-19 in Nursing Home Residents and Healthcare Personnel
(
May 19)
• CMS issued phase reopening guidance FAQs (May 18)
• CMS published informational tool kit to reduce prevalence of COVID-19 in
nursing homes, cataloguing state practices and state directives (
May 13)
• FEMA coordinated two shipments totaling a 14-day supply of PPE directly
to approx. 15,000 nursing homes nationwide (
May 4)
• CMS announced it will form an independent commission to address safety
and quality in nursing homes (
April 30)
• CMS published COVID-19 Long Term Care Facility Guidance Sheet (April 2)
• In addition, on a rolling basis, CMS has provided several waiver flexibilities
in effect during the public health emergency period related to workforce
capacity, telehealth expansion, surge capacity planning, and other, with
some broadly applicable to providers and some specific to
LTC facilities
CMS Quality Safety & Oversight memoranda, guidance, clarifications and instructions to State Survey
Agencies and CMS Regional Offices for Nursing Homes (all policy memos can be accessed
here):
• COVID-19 Survey Activities, CARES Act Funding, Enhanced Enforcement for Infection
Control deficiencies, and Quality Improvement Activities in Nursing Homes (June 1)
• Nursing Home Reopening Recommendations for State and Local Officials (May 18)
• Interim Final Rule Updating Requirements for Notification of Confirmed and Suspected
COVID-19 Cases Among Residents and Staff in Nursing Homes (May 6)
• Nursing Home Five Star Quality Ratings System update; Nursing Home Staff Counts;
and Frequently Asked Questions (April 24)
• Upcoming Requirements for Notification of Confirmed COVID-19 (or COVID-19 Persons
under Investigation) Among Residents and Staff in Nursing Homes (April 19)
• 2019 Novel Coronavirus Long-Term Care Facility Transfer Scenarios (April 13)
• Prioritization of Survey Activities (March 23)
• Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19)
in Nursing Homes (REVISED) (March 13)
• Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19)
in Nursing Homes (March 4)
• Suspension of Survey Activities (March 4)
• Release of Additional Toolkits to Ensure Safety and Quality in Nursing Homes (Feb. 14)
• Information for Healthcare Facilities Concerning 2019 Novel Coronavirus Illness (Feb. 6)
Policy & Memos to States and Regions
Recent Additional Agency Actions:
60

The CDC continues to update its guidance and resources for nursing homes and long-term
care:
https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
• CDC suggests that critical PPE shortages at the facility level are less than one week supply
remaining, despite use of PPE conservation strategies, of: N95 masks • Surgical masks •
Eye protection, including face shields or goggles • Gowns • Gloves • Alcohol-based hand
sanitizer. (CDC also offers a free PPE burn rate calculator for nursing homes). An
acceptable minimum coupled with reliable supplies must be defined by facility.
CDC details extensive “Core Practices,” which should remain in place even as nursing homes
resume normal activities, related to a wide-ranging set of issues (including cohorting, testing,
PPE protocols, training, among others) for infection control during the COVID-19 emergency
Compilation of CMS guidance related to COVID-19:
https://www.cms.gov/About-
CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page
There is no one-size-fits-all formula for all nursing home reopening. There are clear foundational elements: strong bidirectional communications mechanisms, an effective infection control plan (with
enough and the right kind of PPE, sufficient disinfectant supplies, a consistent handwashing protocol, and the ability to cohort residents and staff, among other elements) and a rational, regular testing
plan for residents and staff.
In addition, clinical input, the acuity of residents’ health status (including underlying chronic conditions and mental status), local/regional community outbreak trends, capacity for local/regional
contract tracing, level of training on infection control protocols, familiarity of staff with protocols and individual residents (especially in times of temporary staffing), potential adjustments to symptom
and vitals checks (such as frequency, addition of pulse-oximetry, for example) and the specifics of an individual facility’s design, layout, room configuration and age are also factors that have to be
taken into account.
In concert with “reopening” plans must be contingency plans to quickly restrict access and/or impose greater infection control measures and to ensure robust ongoing monitoring and
communications. CMS and CDC have recently issued new guidance, which they continue to update:
In its
May 18 guidance, CMS recommends nursing homes follow a staged or phased
reopening process. CMS does not recommend opening facilities to visitors (
except for
compassionate care situations
) until phase three when:
• At least 28 days without a new COVID-19 case originating on-site (as opposed to
accepting a patient with COVID-19 transferred from a hospital, for example)
• The nursing home is not experiencing staff shortages
• The nursing home has adequate supplies of PPE and essential cleaning and
disinfection supplies
• The nursing home has adequate access to testing for COVID-19 (which also requires
an arrangement with laboratories to process tests)
• Local hospital(s) have capacity
Additional related considerations: community case status, ability for universal source control
(e.g., residents, staff and visitors wearing masks or face coverings), ability to ensure social
distancing and other measures for visitors, an ability to monitor changes in testing results
against a baseline; a policy or procedure for residents and staff who decline tests or cannot be
tested.
Additional Considerations – Nursing Home “Reopening”
Reopening to Visitors
Infection Control
61

APPENDIX D. OVERVIEW OF SELECTED FEDERAL FUNDING
62

Federal COVID-19 Funding Sources – Provider Relief Fund
Funding Background Funding Description and Relevance to Nursing Homes Links
Public Health
and
Social Services
Emergency
Fund (PHSSEF)
Administered
by HHS
Congress has appropriated $175 billion for
health care providers to prevent, prepare
for, and respond to COVID-19 to be
distributed through grants and other
payment mechanisms. Eligible expenses
include lost revenues, building new
structures or retrofitting existing buildings,
purchasing supplies, training staff, and other
COVID-19-related costs.
The CARES Act provided an initial $100
billion for this fund.
Under the “CARES 3.5” Act - the Paycheck
Protection Program Increase Act of 2020 –
Congress appropriated an additional $75
billion to the fund.
April 2020: HHS allocated $50 billion to providers via a “General
Distribution Fund” based on 2018 net patient revenue. Only providers who
billed Medicare fee-for-service in 2019 are eligible for this funding. This
funding was directly distributed based on the assumption of COVID-related
costs or lost revenues.
• HHS initially released $30 billion based on a provider’s proportionate
share of 2019 Medicare fee-for-service total payments.
• HHS has distributed an additional $20 billion to providers allocated
such that, when added to the initial distribution, it will equal a
provider’s proportionate share of 2018 net patient revenues.
• Providers must sign an attestation and agree to a specific set of Terms
& Conditions (T&Cs) within 90 days of receiving payment.
• Nursing homes in New Jersey that billed Medicare FFS in 2019 would
be eligible for funds from this pool; the amount will vary by facility and
all total allocations have not been disclosed yet.
On May 22, 2020: HHS announced it will make additional relief fund
distributions to SNFs based on both a fixed basis and variable basis. Each
SNF will receive a fixed distribution of $50,000, plus a distribution of $2,500
per bed. All certified SNFs with six or more certified beds are eligible for
this targeted distribution.
NJ SNFs will receive $170,215,000. SNFs must comply with a set of T&Cs
related to this funding. Funding can be used to offset lost revenues and/or
COVID-related expenses after January 31, 2020.
Provider Fund overview:
https://www.hhs.gov/coronavirus/care
s-act-provider-relief-fund/index.html
Database of providers that have
attested to receiving Provider Relief
Fund monies (from $50 Billion General
Distribution Fund) updated weekly,
based on provider attestations:
https://data.cdc.gov/Administrative/H
HS-Provider-Relief-Fund/kh8y-3es6
New SNF distribution:
https://www.hhs.gov/about/news/202
0/05/22/hhs-announces-nearly-4.9-
billion-distribution-to-nursing-facilities-
impacted-by-covid19.html
State by state breakdown of SNF
distribution:
https://www.hhs.gov/sites/default/files
/skilled-nursing-facility-provider-relief-
payment-state-breakdown.pdf
May 22 SNF-specific funding T&Cs:
https://www.hhs.gov/sites/default/files
/terms-and-conditions-skilled-nursing-
facility-relief-fund.pdf
63

Federal COVID-19 Funding Sources – Loans
Funding Background Funding Description and Relevance to Nursing Homes Links
Medicare
Accelerated and
Advanced
Payment
Program
Administered by
CMS
(CARES Act)
The CMS Accelerated and Advance
Payment (AAP) Program is designed to
increase cash flow to Medicare providers
and suppliers impacted by the pandemic.
Note: On April 26, CMS announced that, effective immediately, it is no longer
accepting new applications for the Advance Payment Program (which applies
to Part B suppliers) and that it is “reevaluating” the amounts that will be paid
via the Accelerated Payment Program (which applies to Part A providers).
Eligible facilities were able to request loans in the form of advance payments,
funded from the Medicare Hospital Insurance (Part A) and Supplementary
Medical Insurance (Part B).
While there is a deferred repayment period, the loans must be repaid.
https://www.cms.gov/newsroom/press
-releases/trump-administration-
provides-financial-relief-medicare-
providers
https://www.cms.gov/newsroom/press
-releases/cms-reevaluates-accelerated-
payment-program-and-suspends-
advance-payment-program
Small Business
Administration’s
(SBA) Paycheck
Protection
Program
Administered by
the Department
of Treasury
(CARES Act and the Paycheck Protection
Program Increase Act of 2020)
Expands the SBA’s current loan program
and eligibility requirements in order for
businesses to pay employees and keep
them on payroll during the current
COVID-19 crisis and provides for loan
forgiveness, with certain limits.
Some small nursing homes may be eligible. Businesses must have no more
than 500 employees to be eligible. In determining whether a business has less
than 500 employees, affiliates must be aggregated.
The maximum amount any eligible business may borrow is the lesser of (i) the
business’s average total monthly payroll costs during the one-year period prior
to the loan being made multiplied by 2.5, plus the outstanding amount of an
SBA disaster loan that was made between January 31, 2020, and the date that
such loan is financed with a loan under the Act; or (ii) $10 million.
https://www.sba.gov/funding-
programs/loans/coronavirus-relief-
options
Main Street
Lending
Program
Administered by
the Department
of Treasury
(CARES Act) $75 billion program
Lending program to enhance support for
small and mid-sized businesses that were
in good financial standing before the
crisis by offering 4-year loans to U.S.
companies.
Not in effect yet. Program launching early June.
Eligible business with less than 15,000 employees or $5 billion in annual
revenue are eligible for loans of as much as $500,000. Main Street loans are
full-recourse loans and are not forgivable.
https://www.federalreserve.gov/monet
arypolicy/mainstreetlending.htm
64

Federal COVID-19 Funding Sources – State Funds
Funding Background Funding Description and Relevance to Nursing Homes Links
Testing Funding –
PHSSEF
Administered by
HHS
(Paycheck Protection Program Increase Act of
2020)
The Act appropriates $25 billion to the PHSSEF
to address expenses related to expanded
COVID-19 testing. The fund is intended to
“prevent, prepare for, and respond to
coronavirus, domestically or internationally, for
necessary expenses to research, develop,
validate, manufacture, purchase, administer,
and expand capacity for COVID-19 tests to
effectively monitor and suppress COVID-19.”
$10.25 billion for states, localities, territories sent within 30 days of enactment for
“necessary expenses to develop, purchase, administer, process, and analyze COVID-
19 tests,” including:
• Support for workforce;
• Epidemiology;
• Use by employers or in other settings;
• Scaling up of testing by public health, academic, commercial, and hospital
laboratories, and community-based testing sites, health care facilities, and other
entities engaged in COVID-19 testing;
• Conducting surveillance and contact tracing; and
• Other related activities related to COVID-19 testing.
The governor or designee of each state must submit to the Secretary a plan for
COVID-19 testing within 30 days of the enactment of the Act. The plan must
incorporate goals for the remainder of calendar year 2020, including (i) the number
of tests needed, month-by-month; (ii) month-by-month estimates of laboratory and
testing capacity; and (iii) a description of how the state will use its resources for
testing.
While some of the balance of the fund is allocated to specific agencies, health clinics
and the uninsured, HHS has discretion over a portion of remaining funding.
https://www.congress.gov/116/bills/hr266
/BILLS-116hr266eas.pdf
Coronavirus
Relief Fund
Administered by
the Department
of Treasury
(CARES Act)
$150 billion to states and local governments,
distributed largely in proportion to state
population
The CARES Act included broad guidelines for the Fund, which provide that this
funding may only be used to cover costs that:
• Are necessary expenditures incurred due to the public health emergency with
respect to COVID-19;
• Were not accounted for in the budget most recently approved as of March 27
(the date of enactment of the CARES Act) for the state or government; and
• Were incurred between March 1 and December 30.
Additional guidance on use has been published through a series of FAQs.
https://home.treasury.gov/system/files/13
6/Payments-to-States-and-Units-of-Local-
Government.pdf
https://home.treasury.gov/system/files/13
6/Coronavirus-Relief-Fund-Frequently-
Asked-Questions.pdf
65
Federal COVID-19 Funding Sources – State Funds
Funding Background Funding Description and Relevance to Nursing Homes Links
Enhanced
Federal Medical
Assistance
Percentage
(FMAP)
Families First Coronavirus Relief Act (FFCRA)
6.2 percentage point in FMAP, the federal
Medicaid matching rate for each state
The Medicaid program is jointly funded by the federal government and
states. The federal government pays states for a specified percentage of
program expenditures, called the FMAP.
FFCRA applies a 6.2 percentage point increase in federal Medicaid
matching rate for every state, retroactive to January 1, 2020, through the
last day of the calendar quarter in which the emergency ends. The
increased matching rate applies only to expenditures typically matched
at the state’s regular Medicaid matching rate and not to the enhanced
matching rate for the expansion population under the Affordable Care
Act.
While the federal portion of Medicaid expenditures will increase with
the increase in the federal Medicaid matching rate, allowing states to
use the portion of the money they would have spent on Medicaid for
other uses, Medicaid enrollment is expected to increase as
unemployment increases, meaning that overall Medicaid costs are
expected to increase. In addition, as a condition of receiving the 6.2
percentage point increase, states must maintain most current
beneficiaries in their programs.
https://www.medicaid.gov/state-
resource-center/downloads/covid-19-
section-6008-faqs.pdf
66

APPENDIX E. NEW JERSEY NURSING HOME PROFILE
67

62%
56%
70%
63%
62%
65%
13%
17%
11%
12%
12%
9%
25%
27%
19%
25% 27%
26%
0%
25%
50%
75%
100%
United States New Jersey Connecticut Massachusetts New York Pennsylvania
Distribution of Certified Nursing Facility Residents by Primary
Payer Source (2017)
Medicaid Medicare Private/Other
Source: Distribution of Certified Nursing Facility Residents by Primary Payer Source, 2017, kff.org,
https://www.kff.org/other/state-indicator/distribution-of-
certified-nursing-facilities-by-primary-payer-source/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
Nursing Home Payer Mix
A smaller proportion of New Jersey nursing home residents have Medicaid as their primary
payer compared to other states in the region and the nation.
68

72%
22%
6%
United States
77%
17%
6%
New Jersey
Source: Manatt analysis of Nursing Home Compare data as of May 12, 2020. Based on standard surveys reported 2016 to 2019. Analysis excludes 7 hospitals where daily average resident
totals are not available.
Note: In New Jersey, 74% of nursing homes are for profit, 23% are non-profit and 3% are government-owned. Nationally, 70% of nursing homes are for profit, 23% are non-profit and 6%
are government-owned.
Percentage of Nursing Home Residents Per Day by Ownership Status
Nursing Home Ownership Type
A greater proportion of New Jersey nursing home residents reside in for profit nursing homes
than in the nation as a whole.
69

80%
82%
86%
85%
91%
86%
0%
25%
50%
75%
100%
United States New Jersey Connecticut Massachusetts New York Pennsylvania
Percentage of Nursing Home Beds Occupied
Nursing Home Occupancy
Source: Manatt analysis of Nursing Home Compare data as of May 12, 2020. Based on standard surveys reported 2016 to 2019. Analysis excludes hospitals where daily average resident
totals are not available.
Prior to COVID-19, New Jersey’s nursing home occupancy rate was slightly higher than the
national rate, but lower than in other states in the region.
70

Nursing Home Capacity
Source: Manatt analysis of Nursing Home Compare data as of May 12, 2020. Based on standard surveys reported 2016 to 2019. Analysis excludes hospitals where daily average resident
totals are not available.
Prior to COVID-19, New Jersey had comparable nursing home bed capacity to that of other
states in the region.
106
86
31
145
119
37
120
103
42
116
99
39
187
169
36
127
109
38
-
50
100
150
200
Average Beds per Nursing Home Average Residents per Day, per
Nursing Home
Beds per 1,000 Individuals Aged
65+
Nursing Home Bed Capacity
United States New Jersey Connecticut Massachusetts New York Pennsylvania
71

Sources:
Occupational Employment Statistics Query System, Bureau of Labor Statistics, May 2019, https://data.bls.gov/oes/#/home
Occupational Outlook Handbook: Nursing Assistants, May 2019, bls.gov, https://www.bls.gov/OOH/healthcare/nursing-assistants.htm
Occupational Outlook Handbook: Licensed Practical Nurses, May 2019, bls.gov, https://www.bls.gov/OOH/healthcare/licensed-practical-and-licensed-vocational-nurses.htm
$23.32
$27.65
$27.59
$29.01
$23.97
$23.65
$0
$5
$10
$15
$20
$25
$30
$35
Licensed Practical Nurse
$14.77
$15.00
$16.52
$16.84
$18.66
$15.19
$0
$5
$10
$15
$20
$25
$30
$35
Certified Nursing Assistant
Hourly Mean Wage by State (2019)
Nursing Home Staff Wages
New Jersey licensed practical nurses earn wages that are comparable to peers in neighboring
states. New Jersey certified nursing assistants earn less than other states in the region.*
72
*Header revised for clarity on 6/4/20.

Note: Further investigation is recommended on cost of living and sufficiency of wages for full-time and part-time equivalents. Components may
not sum to 100 percent due to rounding.
Source: Workforce Data Center, PHI, https://phinational.org/policy-research/workforce-data-center/
Nursing Home Employment Status and Health Insurance Coverage Rates
A higher proportion of New Jersey nursing home employees are full time compared to other
states in the region and the nation, yet 13% are uninsured.
60%
66%
63%
54%
68%
71%
25%
22%
29%
40%
25%
18%
11%
13%
8%
6%
6%
11%
0%
25%
50%
75%
100%
US New Jersey Connecticut Massachusetts New York Pennsylvania
Health Insurance Coverage Source (2017)
Insurance Through Employer or Union Public Coverage (includes Medicare and Medicaid) Uninsured
81%
93%
64%
67%
85%
77%
0%
25%
50%
75%
100%
% Full-Time
Nursing Home Employment Status (2018)
US New Jersey Connecticut
Massachusetts New York Pennsylvania
73

Provision of LTSS by Setting
Initiatives to increase the utilization of HCBS in New Jersey’s Medicaid program continue to
be a high priority. Substantial progress has been made in recent years to grow utilization.
Source: Long Term Care Trend, NJ Family Care, http://www.njfamilycare.org/analytics/LTC_trend.html
71%
67%
61%
55%
51%
47%
29%
33%
39%
45%
49%
53%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Jul-14 Mar-15 Mar-16 Mar-17 Mar-18 Mar-19
HCBS vs. Nursing Home LTSS Utilization
Nursing Homes HCBS
74

Payer Mix by Ownership Type
Source: New Jersey Nursing Home Profile, 2019, njha.com, http://www.njha.com/media/1190328/snf-2019-report.pdf
62%
44%
57%
15%
15%
6%
23%
41%
37%
0%
25%
50%
75%
100%
For Profit Nonprofit Government-owned
New Jersey Nursing Home Payer Mix, by Ownership Type (2019)
Medicaid Medicare All Other
Medicaid is the largest payer across all nursing home ownership types in New Jersey,
although it provides a substantially smaller share of reimbursement for nonprofit facilities as
compared to other ownership types.
75

APPENDIX F. ANALYSES OF COVID-19 BY REGION, QUALITY RATINGS, STAFFING,
AND OWNERSHIP TYPE
76

Parameters of NJ Nursing Home Analysis
• On May 22, Manatt completed an analysis of COVID-19 cases and deaths in New
Jersey nursing homes by region, quality ratings, staffing, and ownership using the
following data:
o Nursing Home Compare data
(
https://www.medicare.gov/nursinghomecompare/search.html – accessed,
May 12, 2020)
o U.S. Census data (https://data.census.gov/cedsci/ - accessed, May 12, 2020)
o New Jersey LTC COVID-19 infection and death data
(
https://www.state.nj.us/health/healthfacilities/documents/LTCFacilitiesOutbre
aksList.pdf
- accessed, May 12, 2020)
o New Jersey COVID-19 dashboard data
(
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml – accessed,
May 22, 2020)
• Regional analyses included in this report were conducted based upon the State’s five
historic Medical Coordination Center regions, which are defined by county as shown
below.
North West
• Passaic
• Morris
• Sussex
• Warren
North East
• Bergen
• Essex
• Hudson
South
• Atlantic
• Burlington
• Camden
• Cape May
• Cumberland
• Gloucester
• Salem
Central East
• Middlesex
• Monmouth
• Ocean
• Union
Central West
• Hunterdon
• Mercer
• Somerset
Sussex
Warren Morris
Passaic
Essex
Somerset
Middlesex
Union
Mercer Monmouth
Burlington
Ocean
Camden
Gloucester
Salem
Cumberland
Atlantic
Cape
May
Hunterdon
Bergen
77

Total and Nursing Home COVID-19 Cases by Region
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility
COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey
COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Geography
Population
(2019 Census)
Total Cases
Total Nursing Home Cases
Total Nursing
Homes Licensed
Beds
North East
2,403,000 52,643 4,604 13,020
North West 1,239,000 23,998 2,463 7,947
Central East 2,607,000 46,436 4,961 16,451
Central West 820,000 11,714 1,471 4,600
South 1,811,000 17,202 2,747 11,436
North East 353.61
North West 309.93
Central East 301.56
Central West 319.78
South 240.21
Regions ranked in descending order by deaths per 1,000 people
Nursing Home Cases Per
1,000 Licensed Beds
Cases Per 1,000 People
21.91
19.37
17.81
14.29
9.50
78

Note: Based on available data, strong, consistent, and reliable patterns between nursing home COVID-19 cases and deaths
and nursing home size are not evident. Further investigation is recommended as more data becomes available, and data
reliability increases.
<= 125
126 to 174 175+
All Certified (Medicaid and/or Medicare) Nursing Homes 370 181 72 117
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 152 66 111
Total COVID-19 Cases (Residents Only) 16,246 5,261 3,225 7,760
Total COVID-19 Deaths (Residents Only) 4,317 1,354 900 2,063
Total Licensed Beds 49,525 14,357 9,619 25,549
COVID-19 Cases Per Licensed Bed 0.328 0.366 0.335 0.304
COVID-19 Deaths Per Licensed Bed 0.087 0.094 0.094 0.081
Total Licensed Beds
Any Nursing Home
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
COVID-19 Cases and Deaths by Nursing Home Size
79

For Profit Non Profit Government
All Certified (Medicaid and/or Medicare) Nursing Homes 370 274 85 11
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 244 76 9
Total COVID-19 Cases (Residents Only) 16,246 12,822 2,616 808
Total COVID-19 Deaths (Residents Only) 4,317 3,327 734 256
Total Licensed Beds 49,525 38,083 8,672 2,770
COVID-19 Cases Per Licensed Bed 0.328 0.337 0.302 0.292
COVID-19 Deaths Per Licensed Bed 0.087 0.087 0.085 0.092
Any Nursing Home
Nursing Homes by Ownership Status
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Note: Based on available data, strong, consistent, and reliable patterns between nursing home COVID-19 cases and deaths
and ownership status are not evident. Further investigation is recommended as more data becomes available, and data
reliability increases.
COVID-19 Cases and Deaths by Nursing Home Ownership Status
80

1 to 3*
4 5
All Certified (Medicaid and/or Medicare) Nursing Homes 370 151 81 138
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 138 70 121
Total COVID-19 Cases (Residents Only) 16,246 7,410 3,643 5,193
Total COVID-19 Deaths (Residents Only) 4,317 1,965 999 1,353
Total Licensed Beds 49,525 23,026 10,933 15,566
COVID-19 Cases Per Licensed Bed 0.328 0.322 0.333 0.334
COVID-19 Deaths Per Licensed Bed 0.087 0.085 0.091 0.087
*Note: Two facilities in New Jersey did not have a Overall Star Rating, and are grouped in the "1 to 3" category.
Nursing Homes by Nursing Home Compare Overall Star Rating
Any Nursing Home
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
COVID-19 Cases and Deaths by Nursing Home Overall Star Rating
81

1 to 3* 4 5
All Certified (Medicaid and/or Medicare) Nursing Homes 370 56 69 245
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 49 58 222
Total COVID-19 Cases (Residents Only) 16,246 2,832 2,749 10,665
Total COVID-19 Deaths (Residents Only) 4,317 724 662 2,931
Total Licensed Beds 49,525 8,343 7,951 33,231
COVID-19 Cases Per Licensed Bed 0.328 0.339 0.346 0.321
COVID-19 Deaths Per Licensed Bed 0.087 0.087 0.083 0.088
*Note: Two facilities in New Jersey did not have a Quality Star Rating, and are grouped in the "1 to 3" category.
Nursing Homes by Nursing Home Compare Quality Star Rating
Any Nursing Home
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Note: Based on available data, strong, consistent, and reliable patterns between nursing home COVID-19 cases and deaths
and nursing home Quality Star Ratings are not evident. Further investigation is recommended as more data becomes
available, and data reliability increases.
COVID-19 Cases and Deaths by Nursing Home Quality Star Rating
82

1 to 3* 4 5
All Certified (Medicaid and/or Medicare) Nursing Homes 370 216 99 55
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 193 89 47
Total COVID-19 Cases (Residents Only) 16,246 10,804 4,103 1,339
Total COVID-19 Deaths (Residents Only) 4,317 2,786 1,131 400
Total Licensed Beds 49,525 31,387 13,283 4,855
COVID-19 Cases Per Licensed Bed 0.328 0.344 0.309 0.276
COVID-19 Deaths Per Licensed Bed 0.087 0.089 0.085 0.082
*Note: Two facilities in New Jersey did not have a Staffing Star Rating, and are grouped in the "1 to 3" category.
Nursing Homes by Nursing Home Compare Staffing Star Rating
Any Nursing Home
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Note: Further investigation is recommended as more data becomes available, and data reliability increases.
COVID-19 Cases and Deaths by Nursing Home Staffing Star Rating
83

0 1 to 4 5+
All Certified (Medicaid and/or Medicare) Nursing Homes 370 4 44 322
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 2 36 291
Total COVID-19 Cases (Residents Only) 16,246 55 1,383 14,808
Total COVID-19 Deaths (Residents Only) 4,317 12 319 3,986
Total Licensed Beds 49,525 167 4,012 45,346
COVID-19 Cases Per Licensed Bed 0.328 0.329 0.345 0.327
COVID-19 Deaths Per Licensed Bed 0.087 0.072 0.080 0.088
Any Nursing Home
Nursing Home Compare Deficiencies (2017-2020)
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Note: Based on available data, strong, consistent, and reliable patterns between nursing home COVID-19 cases and deaths
and nursing home health deficiencies are not evident. Further investigation is recommended as more data becomes
available, and data reliability increases.
COVID-19 Cases and Deaths by Nursing Home Health Deficiencies
84

0 1 2+
All Certified (Medicaid and/or Medicare) Nursing Homes 370 107 154 109
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 87 139 103
Total COVID-19 Cases (Residents Only) 16,246 4,181 6,532 5,533
Total COVID-19 Deaths (Residents Only) 4,317 1,102 1,828 1,387
Total Licensed Beds 49,525 11,751 21,086 16,688
COVID-19 Cases Per Licensed Bed 0.328 0.356 0.310 0.332
COVID-19 Deaths Per Licensed Bed 0.087 0.094 0.087 0.083
Any Nursing Home
Nursing Home Compare Infection Deficiencies (2017-2020)
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Note: Based on available data, strong, consistent, and reliable patterns between nursing home COVID-19 cases and deaths
and nursing home infection-related deficiencies are not evident. Further investigation is recommended as more data
becomes available, and data reliability increases.
COVID-19 Cases and Deaths by Nursing Home Infection-Related Deficiencies
85

0 1 2+
All Certified (Medicaid and/or Medicare) Nursing Homes 370 269 76 25
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 239 68 22
Total COVID-19 Cases (Residents Only) 16,246 11,497 3,514 1,235
Total COVID-19 Deaths (Residents Only) 4,317 3,020 964 333
Total Licensed Beds 49,525 35,500 10,542 3,483
COVID-19 Cases Per Licensed Bed 0.328 0.324 0.333 0.355
COVID-19 Deaths Per Licensed Bed 0.087 0.085 0.091 0.096
Any Nursing Home
Nursing Home Compare Staffing Deficiencies (2017-2020)
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Note: Further investigation is recommended as more data becomes available, and data reliability increases.
COVID-19 Cases and Deaths by Nursing Home Staffing-Related Health
Deficiencies
86

COVID-19 Cases and Deaths by Nursing Home Staffing Hours
Note: Nursing home staffing hours only includes nurse staffing hours (registered nurse, licensed practical nurse, and nurse aids), but does not include other types of nursing
home staff including clerical and housekeeping staff.
Source: Manatt analysis of Nursing Home Compare data as of May 12th, 2020, U.S. Census data, Long Term Care Facility COVID-19 infections and deaths from New Jersey:
https://www.state.nj.us/health/healthfacilities/documents/LTC_Facilities_Outbreaks_List.pdf and the New Jersey COVID-19 dashboard
https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml ” as of May 22nd 2020
Note: Based on available data, strong, consistent, and reliable patterns between nursing home COVID-19 cases and deaths and
nursing home staffing hours are not evident. Further investigation is recommended as more data becomes available, and data
reliability increases.
<=3.33
3.34 to 3.84 3.85+
All Certified (Medicaid and/or Medicare) Nursing Homes 370 73 156 141
Among Nursing Homes With at Least 1 Confirmed Resident COVID-19 Infection
Certified Nursing Homes 329 65 138 126
Total COVID-19 Cases (Residents Only) 16,246 3,617 7,834 4,795
Total COVID-19 Deaths (Residents Only) 4,317 926 2,058 1,333
Total Licensed Beds 49,525 10,554 22,067 16,904
COVID-19 Cases Per Licensed Bed 0.328 0.343 0.355 0.284
COVID-19 Deaths Per Licensed Bed 0.087 0.088 0.093 0.079
Any Nursing Home
Nursing Home Compare Adjusted Total Nursing Home Staffing Hours
per Resident per Day
87

The following data would support additional in-depth research efforts:
• Timely, complete and verified geographic and nursing home infection and death time-series death data.
• Detailed information on LTC facility layout including configuration and age of facilities (e.g., number of homes and
proportion of beds in 2, 3, and 4 resident rooms, unit size).
• Detailed information on special populations (e.g., dementia care units) and patient acuity levels.
• Additional ownership information. The majority of New Jersey LTC facilities (74%) are under for-profit ownership.
Manatt did not identify a strong correlation between ownership type (for profit, not-for-profit) and LTC COVID-19
cases or deaths, though overall trends may mask significant differences among specific ownership scenarios and
parent company owners, data which were not publicly available.
In addition, New Jersey might consider deeper-dive research focusing on identifying the strategies most successful in:
• Reducing nursing home exposure to COVID-19.
• Slowing the rate of COVID-19 transmission among nursing home residents.
• Reducing death rates for COVID-19 infected residents with similar health profiles and acuity.
Recommendations for Future Quantitative Analysis
88

APPENDIX G. OTHER STATE AND LOCAL RESPONSES
89

Selection of State and Local Responses
California: As of the middle of May, only three of the 2,100 residents living in California’s eight veterans homes were confirmed positive for
COVID-19. News reports attribute the low infection rate to leadership, planning and infection control. The Secretary of California’s Department
of Veterans Affairs and the Director of Long-Term Care were meeting regularly with facility directors by mid-February and implementing a 38-
step plan that included: update each facility’s emergency operation plans, ensure facilities have enough PPE, and undertake infection control
measures such as using disposable dinnerware and disinfecting common areas every 30 minutes. Pre-COVID-19 factors also contributed to the
low infection rate: electronic records are used, procedures are standardized across all facilities in the system, workforce has paid sick leave, and
staff physicians are on-site daily.
Michigan: Established “regional hubs” designated by the state Department of Health and Human Services to treat individuals from congregate
care settings who are affected by COVID-19 but do not require hospital-level care. There are approximately 19 hubs serving nearly 300
patients, each with enhanced daily reporting requirements. Michigan also activated an infection prevention resource and assessment team
(iPRAT) to provide training to local health departments and facilities; review facilities’ infection control procedures and training protocols;
assist with remote contact tracing; and provide remote facilitation of the CDC’s Tele-ICAR tool.
North Carolina: The Division of Public Health and North Carolina Area Health Education Centers (AHEC) provide reoccurring virtual trainings
and updates to more than 2,000 LTC workers. In addition, sessions provide a Q&A opportunity between providers and the state. North Carolina
worked with AHEC to push out information to providers on testing, PPE, and infection control.
Paterson, NJ: Contract tracers have traced approximately 90% of the city’s 6,200 COVID-19 cases. Prior to COVID-19, the Paterson Board of
Health (BOH) had two disease detectives on staff, but an additional two dozen BOH employees had been trained in communicable disease
investigation last year using a state grant. The contract tracing team now includes 50 of BOH’s 60 employees. Contact tracers check in daily
with all cases and their contacts to see how they are feeling and to monitor compliance with quarantine restrictions. New Jersey’s electronic
communicable disease tracking system serves as the team’s master database.
90

Green House Project
• The Green House Project model was developed by a geriatrician in the early 2000s, with support from the Robert
Wood Johnson Foundation. Key elements of the model include:
• Residents live in self-contained small home-like settings. Medical equipment is tucked away in wall closets
to maintain the home-like feel.
• Each home has a low staff ratios and staff receive advanced training.
• Nursing assistants manage residents' care, with support from nurses and therapists. Unlike the traditional
nursing home model, there are not additional supervisory or administrative layers.
• The first Green House was opened in 2003 in Mississippi. In 2010, the first Green House home for short-term
rehab was opened and in 2011, the first Green House homes for veterans opened.
• There are two Green House homes in New Jersey: Morris Hall Meadows in Lawrenceville and Green Hill in West
Orange.
• There are now nearly 300 Green House homes in 32 states. As of mid-May, only 8 of 243 reporting homes have a
COVID-19 case.
• The Green House Project works with organizations, including developers and providers, to build Green House
homes by connecting them to an experienced peer network, and providing consultation services on building a
business case, financing, addressing regulatory hurdles, and designing and constructing the homes.
• Financing options for building Green House homes include grants, social impact investments, and tax credits for
Green House homes in low-income communities.
“When you know somebody
really well, you could pick
up atypical behavior. You
know someone isn't eating
as much as they normally
eat because you prepare
the meals…You can get
testing faster, make a
diagnosis and move the
patient out to the [Covid-
19-positive] cohort of units
that we have.”
-Dr. Jeffrey Farber, CEO of
the New Jewish Home,
discussing the advantages
of the Green House Project
during the pandemic
The Green House Project is a relatively new nursing home model that emphasizes resident autonomy and highly
personalized care teams in a setting that looks and feels less like an institution and more like a home.
91

APPENDIX H. REFERENCES
92

References
Slide 7:
• “Key Messaging to Long-term Care Facilities (LTCF) for COVID-19.” New Jersey Department of Health. March 3, 2020.
https://www.nj.gov/health/cd/documents/topics/NCOV/NcOv_LINCS_LTCF_Key Messages_03032020.108103.pdf
• “Updated Guidance on Evaluating and Testing Persons for Coronavirus Disease 2019 (COVID-19).” Centers for Disease Control. March 8, 2020.
https://emergency.cdc.gov/han/2020/HAN00429.asp
• “U.S. and World Population Clock." 2020. United States Census Bureau. https://www.census.gov/popclock/
• “Coronavirus in the U.S.: Latest Map and Case Count." 2020. New York Times. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html#states
Slide 9:
• “11 kids dead at N.J. nursing facility. 36 infected. Feds fine Wanaque Center $600K." March 2, 2019. Star Ledger. https://www.nj.com/news/2019/03/11-kids-dead-at-nj-nursing-facility-36-
infected-feds-fine-wanaque-center-600k.html
• “Coronavirus spread at Life Care Center of Kirkland for weeks, while response stalled." March 18, 2020. The Seattle Times. https://www.seattletimes.com/seattle-news/times-
watchdog/coronavirus-spread-in-a-kirkland-nursing-home-for-weeks-while-response-stalled/
Slide 10:
• “New Jersey Nursing Home Profile." 2018. NJHA. http://www.njha.com/media/510224/SNF-Final-Report-2018.pdf.
• “New Jersey COVID-19 Dashboard." June 2, 2020. New Jersey Department of Health. https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml
• “Long Care: Trend.” NJ Family Care http://www.njfamilycare.org/analytics/LTC_trend.html
• “Nursing Homes & Assisted Living Facilities Account for 42% of COVID-19 Deaths.” May 22, 2020. The Foundation for Research and Equal Opportunity. https://freopp.org/the-covid-19-nursing-
home-crisis-by-the-numbers-3a47433c3f70.
Slide 11
• “New Jersey Nursing Home Profile.” 2018. NJHA. http://www.njha.com/media/510224/SNF-Final-Report-2018.pdf.
• Pfefferle, Susan G., and Dana Beth Weinberg. 2008. "Certified Nurse Assistants Making Meaning Of Direct Care." Qualitative Health Research 18 (7): 952-961. doi:10.1177/1049732308318031.
• "Workforce Data Center – PHI.” 2020. PHI. http://phinational.org/policy-research/workforce-data-center/#states=34.
• “Occupational Employment Statistics: Nurses Assistants.” May 2019. U.S. Bureau of Labor Statistics. https://www.bls.gov/oes/current/oes311131.htm#st
• “Occupational Employment Statistics: Licensed Practical Nurses and Licensed Vocational Nurses.” May 2019. U.S. Bureau of Labor Statistics. https://www.bls.gov/OOH/healthcare/licensed-
practical-and-licensed-vocational-nurses.htm
• “New Jersey COVID-19 Dashboard.” June 2, 2020. New Jersey Department of Health. https://www.nj.gov/health/cd/topics/covid2019_dashboard.shtml
Slide 17:
• “Infection Control Deficiencies Were Widespread and Persistent in Nursing Homes Prior to COVID-19 Pandemic." May 20, 2020. U.S. Government Accountability Office.
https://www.gao.gov/assets/710/707111.pdf
93

References (cont.)
Slide 23:
• “Inside Look Into Delaware's Emergency Coronavirus Response Hub.” March 17, 2020. Delaware Online. https://www.delawareonline.com/story/news/2020/03/17/delaware-public-
health-experts-monitoring-coronavirus-spread/5055171002/
• "State Announces Residential Outbreak Task Force | Colorado COVID-19 Updates." May 6, 2020. Colorado Department of Public Health and Environment and Colorado State Emergency
Operations Center. https://covid19.colorado.gov/press-release/state-announces-residential-outbreak-task-force.
Slide 25:
• “Establishing Medical Operations Coordination Cells for COVID-19.” April 24, 2020. ASPR. https://asprtracie.hhs.gov/technical-resources/resource/8354/establishing-medical-operations-
coordination-cells-moccs-for-covid-19
Slide 26:
• "Nursing Home Reopening Recommendations For State And Local Officials." May 18, 2020. CMS. https://www.cms.gov/files/document/nursing-home-reopening-recommendations-state-
and-local-officials.pdf.
• "Coronavirus Disease 2019 (COVID-19) Nursing Homes & Long-Term Care Facilities." May 19, 2020. CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
Slide 27:
• "Governor Hogan Activates Statewide Strike Teams for Nursing Homes, Enacts Order to Shut Down Unsafe Facilities." April 7, 2020. Maryland Governor’s Office.
https://governor.maryland.gov/2020/04/07/governor-hogan-activates-statewide-strike-teams-for-nursing-homes-enacts-order-to-shut-down-unsafe-facilities/.
• “Wolf Administration Releases Data on COVID-19 Cases by Long-Term Care Facility.” Office of the Governor. May 19, 2020. https://www.media.pa.gov/Pages/Health-
Details.aspx?newsid=817
• “Interim Guidance for Nursing Care Facilities During COVID-19." May 12, 2020. Pennsylvania Department of Health.
https://www.health.pa.gov/topics/Documents/Diseases%20and%20Conditions/COVID-19%20Interim%20Nursing%20Facility%20Guidance.pdf
• “Advisory: Universal Message Regarding Cohorting of Residents in Skilled Nursing Facilities.” Pennsylvania Department of Health. April 14, 2020.
https://www.health.pa.gov/topics/Documents/HAN/2020-PAHAN-496-04-14-ADV-Cohorting R.pdf
• “Minnesota Nursing Homes, Already the Site of 81% Of COVID-19 Deaths, Continue Taking in Infected Patients." May 20, 2020. Star Tribune. https://www.startribune.com/minn-nursing-
homes-already-site-of-81-of-covid-19-deaths-still-taking-in-infected-patients/570601282/
Slide 28
• “Executive Directive No. 20-013: COVI-19 Testing at Licensed Long-term Care Facilities, Assisted Living Residences, Comprehensive Personal Care Homes, Residential Health Care Facilities,
and Dementia Care Homes. May 12, 2020. New Jersey Department of Health.
https://nj.gov/health/legal/covid19/05-12-2020_LTC_COVID19testing.pdf
94

References (cont.)
Slide 30:
• “Notification of Residents, Residents’ Families, Visitors and Staff in the Event of a Contagious Disease Outbreak in a Facility.” April 4, 2020. New Jersey Department of Health.
https://files.constantcontact.com/e1419ee3001/45ed2b23-2b55-4ac2-a433-6d4f76ac920d.pdf
• "Upcoming Requirements For Notification Of Confirmed COVID-19 (Or COVID19 Persons Under Investigation) Among Residents And Staff In Nursing Homes." April 19, 2020. CMA.
https://www.cms.gov/files/document/qso-20-26-nh.pdf
• "Guidance For Resident And Family Communication In Adult Care Facilities (ACFs) And Nursing Homes (NHs)." April 4, 2020. Office for People with Developmental Disabilities.
https://opwdd.ny.gov/system/files/documents/2020/04/4.10.2020-doh_covid19_acf-nh_residentfamilycommunication.pdf.
• “Baker-Polito Administration Announces New Funding, Outlines Ongoing Steps To Support Long-Term Care Facilities." April 15, 2020. Office of the Governor.
https://www.mass.gov/news/baker-polito-administration-announces-new-funding-outlines-ongoing-steps-to-support-long-term
• “The State of Florida’s “Project: VITAL” Will Connect Florida Seniors to Their Families Through Virtual Technology to Help Mitigate the Effects of Social Isolation." April 8, 2020.
Florida Department of Elder Affairs.
http://elderaffairs.state.fl.us/doea/press/2020/UPDATED%20-%20Project%20Vital%20Press%20Release-FINAL20200408.pdf
Slide 31:
• “Civil Money Penalty (CMP) Reinvestment Application Template Coronavirus Disease 2019 (COVID-19) Communicative Technology Request.” April 24, 2020. CMS.
https://ltcombudsman.org/uploads/files/support/COVID-19_APPLICATION_TEMPLATE__FINAL_508_202004161441519152.PDF
Slide 32:
• “Illinois nursing home strike averted as tentative agreement reached, including hazard pay for workers during COVID-19 outbreak." May 7, 2020. Chicago Tribune.
https://www.chicagotribune.com/coronavirus/ct-coronavirus-nursing-home-strike-averted-20200507-nwoi7rccxvcinh7ew33op6r3ou-story.html
• “MassHealth Investment to Support Signing Bonuses for Nursing Facility Staff.” April 15, 2020. Massachusetts Senior Care Association.
https://www.maseniorcare.org/sites/default/files/inline-files/MassHealth%20Signing%20Bonsues%20for%20Nursing%20Facility%20Staff_final.pdf
Slide 34:
• “States Leverage Medicaid to Provide Nursing Homes a Lifeline through COVID-19.” May 20,2020. Leading Age. https://www.leadingage.org/regulation/states-leverage-medicaid-
provide-nursing-homes-lifeline-through-covid-19
• “Increasing The Equity of Medicare’s Payments Within Each Post-acute Care Setting; And Assessing Payment Adequacy And Updating Payments for Skilled Nursing Facilities."
December 7, 2017. Medicare Payment Advisory Commission. http://www.medpac.gov/docs/default-source/default-document-library/combined-pac-and-snf-update-dec-2017-
public-handout.pdf?sfvrsn=0
• "Medicaid Disaster Relief for the COVID-19 National Emergency." March 2020. CMS. https://www.medicaid.gov/state-resource-center/downloads/medicaid-disaster-relief-spa-
template.docx
• “Medicaid Managed Care Options in Responding to COVID-19." May 14, 2020. Center for Medicare & Medicaid Services. https://www.medicaid.gov/sites/default/files/Federal-
Policy-Guidance/Downloads/cib051420.pdf
95

References (cont.)
Slide 35:
• “Nursing Facility Rate Increase Notice." April 3, 2020. Connecticut Department of Social Services. https://portal.ct.gov/-/media/Departments-and-
Agencies/DSS/Communications/DOC040320-001.pdf?la=en
• “Baker-Polito Administration Announces New Funding, Outlines Ongoing Steps To Support Long-Term Care Facilities.” April 15, 2020. Office of the Governor.
https://www.mass.gov/news/baker-polito-administration-announces-new-funding-outlines-ongoing-steps-to-support-long-term
Slide 37:
• 105 CMR 153.000 https://www.mass.gov/files/documents/2018/08/30/105cmr153.pdf
• “Department Of Public Health Division Of Health Care Facility Licensure And Certification Suitability Application Disclosure Of Additional Information”. Massachusetts Department
of Public Health.
https://www.mass.gov/doc/suitability-application-disclosure-form/download
• “How to Determine if CON Submission is Required”. May 2020. New York Department of Health. https://www.health.ny.gov/facilities/cons/more_information/
Slide 39:
• “Efforts to Strengthen Federal Enforcement Have Not Deterred Some Homes from Repeatedly Harming Residents”. March 2007. U.S. Government Accountability Office.
https://www.gao.gov/assets/260/258016.pdf
• “Chain of 21 Nebraska nursing homes placed in receivership after missing payroll." March 26, 2020. Omaha World Herald. https://www.omaha.com/livewellnebraska/chain-of-
21-nebraska-nursing-homes-placed-in-receivership-after-missing-payroll/article_013a2693-60af-5359-b258-c99a6325e30c.html
• "Minnesota Department Of Health (MDH) Seeks Nursing Home Receivership Managing Agent Candidates." 2020. MDH.
https://www.health.state.mn.us/facilities/regulation/nursinghomes/receivership.html
• “Nursing Home Search Page." 2020. Massachusetts Executive Office of Health and Human Services. https://eohhs.ehs.state.ma.us/nursehome/default.aspx
Slide 41:
• “Massachusetts Nursing Facilities." 2020. Massachusetts Center for Health Information and Analysis. https://www.chiamass.gov/massachusetts-nursing-facilities/
• “Long-stay nursing homes: Search." Minnesota Nursing Home Report Card. http://nhreportcard.dhs.mn.gov/SearchLS.aspx
• “Long-Term Care Facility Financial Data." 2020. California Office of Statewide Health Planning and Development. https://oshpd.ca.gov/data-and-reports/cost-transparency/long-
term-care-facility-financial-data/
• “Long-Term Care Facility Utilization." 2020. California Office of Statewide Health Planning and Development. https://oshpd.ca.gov/data-and-reports/healthcare-utilization/long-
term-care-utilization/
96

References (cont.)
Slide 44:
• “Not Long Before Coronavirus, Another Outbreak Ravaged a N.J. Nursing Home. Were Its Lessons Forgotten?." March 30, 2020. The Star Ledger
https://www.nj.com/coronavirus/2020/03/not-long-before-coronavirus-another-outbreak-ravaged-a-nj-nursing-home-were-its-lessons-forgotten.html
• “Infection Control Deficiencies Were Widespread and Persistent in Nursing Homes Prior to COVID-19 Pandemic." May 20, 2020.GAO. https://www.gao.gov/assets/710/707111.pdf
• “Targeted Probe and Educate (TPE)." December 2019. CMS. https://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-
Programs/Medical-Review/Targeted-Probe-and-EducateTPE
• “Protecting Florida’s Seniors: Long-term Care Facilities." 2020. Governor of Florida. https://www.flgov.com/wp-content/uploads/covid19/5.13.20%20DRAFT%20LTC%20slides%20-
%20FINAL_New.pdf
• “Nursing Home Help." Sinclair School of Nursing. https://nursinghomehelp.org/qipmo-program/team/
Slide 47:
• “Years of Disinvestment Hamper New Jersey’s Pandemic Response.” April 20, 2020. New Jersey Policy Perspective. https://www.njpp.org/budget/years-of-disinvestment-hamper-
new-jerseys-pandemic-response
• “Executive Office of Health and Human Services.“ EOHHS. https://www.mass.gov/orgs/executive-office-of-health-and-human-services
Slide 49:
• “Long Term Care: Trend." 2020. NJ Family Care. http://www.njfamilycare.org/analytics/LTC_trend.html
• “Nursing Facility Task Force." 2019. Office of the Governor. https://www.mass.gov/orgs/nursing-facility-task-force
• “Executive Order N-14-19.” June 10, 2019. California Office of the Governor. https://www.gov.ca.gov/wp-content/uploads/2019/06/6.10.19-Master-Plan-for-Aging-EO.pdf
Slide 53:
• “Proposed Rule: Medicare and Medicaid Programs; Requirements for Long-Term Care Facilities: Regulatory Provisions To Promote Efficiency, and Transparency.” July 18, 2019.
CMS.
https://www.govinfo.gov/content/pkg/FR-2019-07-18/pdf/2019-14946.pdf
• “State Budget Hits Due to Coronavirus Are Trickling In and It's Not Pretty.” May 14, 2020. USA Today. https://www.usatoday.com/story/money/2020/05/13/coronavirus-states-
reporting-steep-tax-revenue-shortfalls/3108657001/
Slide 54:
• “Coronavirus Pandemic Response: PPE Packages for Nursing Homes.” May 2, 2020. FEMA. https://www.fema.gov/news-release/2020/05/02/coronavirus-pandemic-response-ppe-
packages-nursing-homes#:~:text=Under%20direction%20of%20the%20White,nursing%20homes%20across%20the%20Nation
• “CMS Announces Independent Commission to Address Safety and Quality in Nursing Homes.” April 30, 2020. CMS. https://www.cms.gov/newsroom/press-releases/cms-
announces-independent-commission-address-safety-and-quality-nursing-homes
97

References (cont.)
Slide 56:
• “Key Messaging to Long-term Care Facilities (LTCF) for COVID-19.” March 3, 2020. New Jersey Department of Health.
https://www.nj.gov/health/cd/documents/topics/NCOV/NcOv_LINCS_LTCF_Key Messages_03032020.108103.pdf
• “Mandatory Guidelines for Visitors and Facility Staff.” March 16, 2020. New Jersey Department of Health. https://nj.gov/health/legal/covid19/3-16-
2020_MandatoryGuidelinesforVisitors_andFacilityStaff_ Supersedes3-13-2020Guidelines.pdf
• “Recommendations for Long-Term Care Facilities during COVID-19 Pandemic.” March 20, 2020. New Jersey Department of Health.
https://nj.gov/health/cd/documents/topics/NCOV/NJDOH_Recommendations_For_LTC-COVID19_3_20_2020.108137.pdf
• “Executive Order No. 111.” Office of the Governor. https://nj.gov/infobank/eo/056murphy/pdf/EO-111.pdf
• “Notification of Residents, Residents’ Families, Visitors and Staff in the Event of a Contagious Disease Outbreak in a Facility.” April 4, 2020. New Jersey Department of Health.
https://files.constantcontact.com/e1419ee3001/45ed2b23-2b55-4ac2-a433-6d4f76ac920d.pdf
• “Priority Actions for All Post-acute Care Settings in Response to COVID-19.” March 30, 2020. New Jersey Department of Health.
https://www.nj.gov/health/cd/documents/topics/NCOV/LINCS_Priority_Messaging_to_Post-acute_Care.pdf
• “All 94 Residents of New Jersey Nursing Home Presumed Positive For Coronavirus.” March 26, 2020. USA Today.
https://www.usatoday.com/story/news/nation/2020/03/25/whippany-nursing-home-takes-covid-19-seniors-woodbridge-facility/5081292002/
• “Hospital Discharges and Admissions to Post-Acute Care Setting.” March 31, 2020. New Jersey Department of Health.
https://www.nj.gov/health/healthfacilities/documents/CN/temp_waivers/HospitalDischarges_andAdmissions_toPost-AcuteCareSettings.pdf
• “State Request for 1135 Waiver Authorization.” March 16, 2020. New Jersey Department of Health.
https://nj.gov/humanservices/library/slides/1135Waiver%20signed%20by%20DOH%203-16-2020[2][2][1].pdf
• Letter to J. Glaze, CMS. March 19, 2020. New Jersey Department of Human Services.
https://nj.gov/humanservices/library/slides/NJ%201135%20Submission%203%2019%2020.pdf
Slide 57:
• “Outbreak Management Checklist for COVID-19 in Nursing Homes and Other Post-Acute Care Settings.” May 11, 2020. New Jersey Department of Health.
https://www.nj.gov/health/cd/documents/topics/NCOV/COVID_Outbreak_Management_Checklist.pdf
• “Statement of Attorney General Gurbir S. Grewal Regarding Deaths at Nursing Homes and Other Long-Term Care Facilities in New Jersey.” April 16, 2020. Office of the Attorney
General.
https://www.nj.gov/oag/newsreleases20/pr20200416c.html
• "New Jersey Nursing Homes and Assisted Living Facilities." April 13, 2020. New Jersey Department of Health. https://nj.gov/health/legal/covid19/4-13-
20_EmergencyCurtailmentOfAdmissions.pdf
• “COVID-19 Long-Term Care Facility Outbreak Reporting and Response Guidelines.” April 22, 2020. New Jersey Department of Health.
https://www.documentcloud.org/documents/6922480-NJDOH-LTCF-Outbreak-Response.html
98

References (cont.)
Slide 58:
• “Nursing Home Misconduct Reporting Form.” May 2020. State of New Jersey. https://covid19.nj.gov/forms/ltc?ourl=https://covid19.nj.gov/LTC&oref=
• “Administrative Order And Notice Of Rule Waiver Pursuant To P.L. 2020, C. 18; N.J.S.A. 45:1-29. May 5, 2020. New Jersey Department Of Law And Public Safety Division Of
Consumer Affairs.
https://www.njconsumeraffairs.gov/COVID19/Documents/DCA-AO-2020-05_DCA-W-2020-09.pdf
• “Executive Directive No. 20-013: COVID-19 Testing at Licensed Long-term Care Facilities, Assisted Living Residences, Comprehensive Personal Care Homes, Residential Health Care
Facilities, and Dementia Care Homes. May 12, 2020. New Jersey Department of Health.
https://nj.gov/health/legal/covid19/05-12-2020_LTC_COVID19testing.pdf
• “Frequently Asked Questions: Department of Health Executive Directive 20-013. Testing at Licensed Long-term Care Facilities, Assisted Living Residences, Comprehensive Personal
Care Homes, Residential Health Care Facilities, and Dementia Care Homes. New Jersey Department of Health.
https://nj.gov/health/legal/covid19/05-12-
2020_LTC_COVID19testing.pdf
Slide 60:
• “HHS Announces Nearly $4.9 Billion Distribution to Nursing Facilities Impacted by COVID-19.” May 22, 2020. HHS. https://www.hhs.gov/about/news/2020/05/22/hhs-announces-
nearly-4.9-billion-distribution-to-nursing-facilities-impacted-by-covid19.html
• “Preparing for COVID-19 in Nursing Homes.” May 19, 2020. CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
• “Interim Testing Guidance in Response to Suspected or Confirmed COVID-19 in Nursing Home Residents and Healthcare Personnel.” May 19, 2020. CDC.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/nursing-homes-testing.html
• “Nursing Home Reopening Recommendations Frequently Asked Questions.” May 18, 2020. CMS. https://www.cms.gov/files/document/covid-nursing-home-reopening-
recommendation-faqs.pdf
• “Toolkit on State Actions to Mitigate COVID-19 Prevalence in Nursing Homes.” May 13, 2020. CMS. https://www.cms.gov/files/document/covid-toolkit-states-mitigate-covid-19-
nursing-homes.pdf
• “Coronavirus Pandemic Response: PPE Packages for Nursing Homes.” May 2, 2020. FEMA. https://www.fema.gov/news-release/2020/05/02/coronavirus-pandemic-response-ppe-
packages-nursing-homes#:~:text=Under%20direction%20of%20the%20White,nursing%20homes%20across%20the%20Nation
• “CMS Announces Independent Commission to Address Safety and Quality in Nursing Homes.” April 30, 2020. CMS. https://www.cms.gov/newsroom/press-releases/cms-
announces-independent-commission-address-safety-and-quality-nursing-homes
• “Coronavirus Waivers & Flexibilities.” May 2020. CMS. https://www.cms.gov/about-cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-waivers
• “Long Term Care Facilities (Skilled Nursing Facilities and/or Nursing Facilities): CMS Flexibilities to Fight COVID-19.” May 15, 2020. CMS. https://www.cms.gov/about-
cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-waivers
Slide 61:
• "Nursing Home Reopening Recommendations For State And Local Officials." May 18, 2020. CMS. https://www.cms.gov/files/document/nursing-home-reopening-
recommendations-state-and-local-officials.pdf
• “Preparing for COVID-19 in Nursing Homes.” May 19, 2020. CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
• “Current emergencies.” May 2020. CMS. https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page
99

References (cont.)
Slide 90:
• “Meet the 73-year-old surgeon working to keep California veterans safe from COVID-10." May 10, 2020. Los Angeles Times. https://www.latimes.com/california/story/2020-05-
10/coronavirus-california-veterans-safe-homes
• “MDHHS Implementing Strategies in Long-term Care Facilities to Help Slow the Spread of COVID-19 and Protect Residents and Staff." April 20, 2020. Michigan.gov.
https://www.michigan.gov/som/0,4669,7-192-47796-526529--,00.html
• “NCDHHS Expands Measures to Prevent and Respond to COVID-19 in Long-term Care Facilities." May 18, 2020. North Carolina Department of Health and Human Services.
https://www.ncdhhs.gov/news/press-releases/ncdhhs-expands-measures-prevent-and-respond-covid-19-long-term-care-facilities
• “As the Nation Begins Virus Tracing, It Could Learn From This N.J. City." May 21, 2020. New York Times. https://www.nytimes.com/2020/05/21/nyregion/contact-tracing-paterson-
nj.html
Slide 91:
• “The Greenhouse Project." The Greenhouse Project. https://www.thegreenhouseproject.org/
• “The Green House Project." Robert Wood Johnson Foundation. https://www.rwjf.org/en/how-we-work/grants-explorer/featured-programs/the-green-house-project.html
• “As Death Toll in Nursing Homes Climbs, Calls to Redesign Them Grow.” May 12, 2020. New York Times. https://www.nytimes.com/2020/05/12/business/nursing-homes-
coronavirus.html
• "NY's Nursing Home Crisis: Facilities Chart A Path Forward." 2020. Crain's New York Business. https://www.crainsnewyork.com/health-pulse/nys-nursing-home-crisis-facilities-
chart-path-forward?utm_source=health-pulse-friday&utm_medium=email&utm_campaign=20200528&utm_content=hero-headline.
100
