
WINTER 2022 Volume 18 {N
o
1} Edition 53
Resilience:
A Key t o Safe Nursing Practice
Resilience:
A Key to Safe Nursing Practice
CE Article
Also inside...
2022-2025 NCBON Strategic Plan
The Official Publication of the North Carolina Board of Nursing
Nort h Carolina's Guide to Diabetes
Prevent ion and Managem ent 2020:
Resources for Nurses to Take Action
CE Article

2
Protect the public by regulating the practice of nursing.
PRACTICE
- Practice Corner
- CE Opportunities 2022
The Bulletin is the
official publication of the
North Carolina Board of Nursing.
Office Locat ion
4516 Lake Boone Trail
Raleigh, NC 27607
Mailings
PO Box 2129
Raleigh, NC 27602-2129
Telephone
(919) 782-3211
Fax
(919) 781-9461
Websit e
www.NCBON.com
Office Hours
8:00a-5:00p
Board Chair
Ann Marie Milner, DNP, MSN, RN, CNE
Chief Execut ive Officer
Crystal Tillman, DNP, RN, CNP, FRE
Editors
Sara Griffith, PhD, RN
Angela Ellis
Paulette Hampton
Catherine Soderberg
Brad Gibson
Mission
Protect the public by regulating the
practice of nursing.
Vision
Exemplary nursing care for all.
The Bulletin is published three times a year by the NCBON. In
compliance with the Americans with Disabilities Act, this publication
may be requested in alternate formats by contacting the Board's office.
Table of Contents
GOVERNANCE
- Letter from the NCBON CEO
- Letter from the NCBON Chair
- '22-'25 NCBON Strategic Plan
- 2022 Board Member Oath of Office
- Nomination form for 2022 Election
- NC Nursecast Collaboration
- Board of Nursing Actions
APRN
- Considering Graduate Nursing Education?
- New APRN Position Statement
LICENSURE
- Licensure Corner
- Accessing NCBON Disciplinary Actions
CE Articles
Resilience:
A Key to Safe Nursing Practice (1.5 CH)
North Carolina's Guide to Diabetes
Prevention and Management 2020:
Resources for Nurses to Take Action (0.5 CH)
EDUCATION
- NCBON and NCSBN Annual Report Collaboration
- 18th Annual Education Summit
- Update: Hospice and Home Care Foundation Grant
- AHEC Collaboration: NCLEX Next Generation Courses
Click or tap link below to jump to section.

3
Protect the public by regulating the practice of nursing.
PRACTICE
- Practice Corner
- CE Opportunities 2022
letter from the
Chief Executive Officer
In January 2021, the Board convened a Strategic Planning
Committee for purposes of reviewing the Board?s Mission,
Vision, Values, and establishing a Strategic Plan for
2022-2025. The Committee received, reviewed, and
analyzed data from environmental scans, other nursing
boards, National Council of State Boards of Nursing, as
well as surveys to key stakeholders. Thank you to the 1665
respondents who participated in our on-line survey! After
a long year of intense work, the Board approved the new Strategic Plan for 2022-2025
located on page 5 of this issue. Be sure to follow us on social media and attend the
Board Business Meetings held each year in January, May, and September to follow our
progress with the new plan.
Our new Board Members, Dr. Shakira Henderson and Cheryl Wheeler, took their Oath
of Office during the January Board Meeting. The Oath of Office video is linked on page 6.
We are grateful for your service to the public. Consider submitting a nomination form
for one of the available positions: RN (ADN Nurse Educator), RN (Staff Nurse), or LPN.
The nomination form is located on page 9 and is due by April 1, 2022. The Summer
edition of The Bulletin will contain candidate information. The election will be held
between July 1st and August 15th.
In response to the ongoing COVID pandemic and the impact on nursing, the Board
approved the continuation of multiple waivers until June 31, 2022 or unless sooner
amended or rescinded by the Board or further Executive Order.
The Winter Edition of The Bulletin is packed with two free continuing education articles
and other resources pertinent to nursing. The resilience article written by Dr. Terry Ward
on page 12 is timely as nurses in North Carolina continue to be on the front lines
providing nursing care and services to all patients. Dr. Ward provides suggestions to
build and maintain resiliency.
If you are interested in writing an article for The Bulletin, please reach out to Dr. Sara
Griffith at sgriffith@ncbon.com.
Regards,
Crystal L. Tillman, DNP, RN, CNP, FRE
Chief Executive Officer
GOVERNANCE
- Letter from the NCBON CEO
- Letter from the NCBON Chair
- '22-'25 NCBON Strategic Plan
- 2022 Board Member Oath of Office
- Nomination form for 2022 Election
- NC Nursecast Collaboration
- Board of Nursing Actions
APRN
- Considering Graduate Nursing Education?
- New APRN Position Statement
LICENSURE
- Licensure Corner
- Accessing NCBON Disciplinary Actions
EDUCATION
- NCBON and NCSBN Annual Report Collaboration
- 18th Annual Education Summit
- Update: Hospice and Home Care Foundation Grant
- AHEC Collaboration: NCLEX Next Generation Courses

4
Protect the public by regulating the practice of nursing.
letter from the
NCBON Board Chair
A year to remember or perhaps these will be the years we
will never forget. As the pandemic continues with no real
end in sight, nurses are and will continue to be the front
line workers providing care for patients. Although the
public may not fully understand the extent of what a nurse
does when they hear about us on a news segment or drive
by a hospital and see one of us walking by, they do know
who cares for them in their time of need and gain better
understanding of how important this profession is. It is a remarkable testament to the
impact on our patients that nurses have been consistently voted the most ethical and
honest profession for the past 18 years in the Gallup Poll.
Nurses across the state have been caring for pandemic patients in a safe, competent, and
compassionate way since March 2020. These efforts have not come without cost.
Increased nursing shortages (that started before the pandemic), increased patient-nurse
ratios, burn-out, and physical and emotional health has taken its toll. As Dr. Terry Ward so
pointedly writes, ?The strain and stressors are unprecedented. Nurses are being faced
with a surge in nursing capacity, burnout, and moral. All these challenges to resilience
lead to alterations in well-being.? Dr. Ward?s CE article, Resilience: A Key to Safe Nursing
Practice can be found in this Bulletin. As we continue to provide compassionate care to
our patients, it is important we also care for ourselves and one another. We can use
strategies, like that shared by Dr. Ward, to promote personal resilience that will support
the nurse?s ability to cope in our ever-changing healthcare environment.
I am grateful for the dedication and care that our more than 170,000 Registered Nurses
and Licensed Practical Nurses give to the residents of our State. Even though the Year of
the Nurse was 2020, I believe that every year is the Year of the Nurse. Your commitment
and the care you show your patients ensures that they believe it too. Know you are
appreciated this year and every year. I am honored to continue to serve you as an elected
Board Member and now as Board Chair.
Sincerely,
Ann Marie Milner, DNP, MSN, RN, CNE
NCBON Board Chair
5
Protect the public by regulating the practice of nursing.
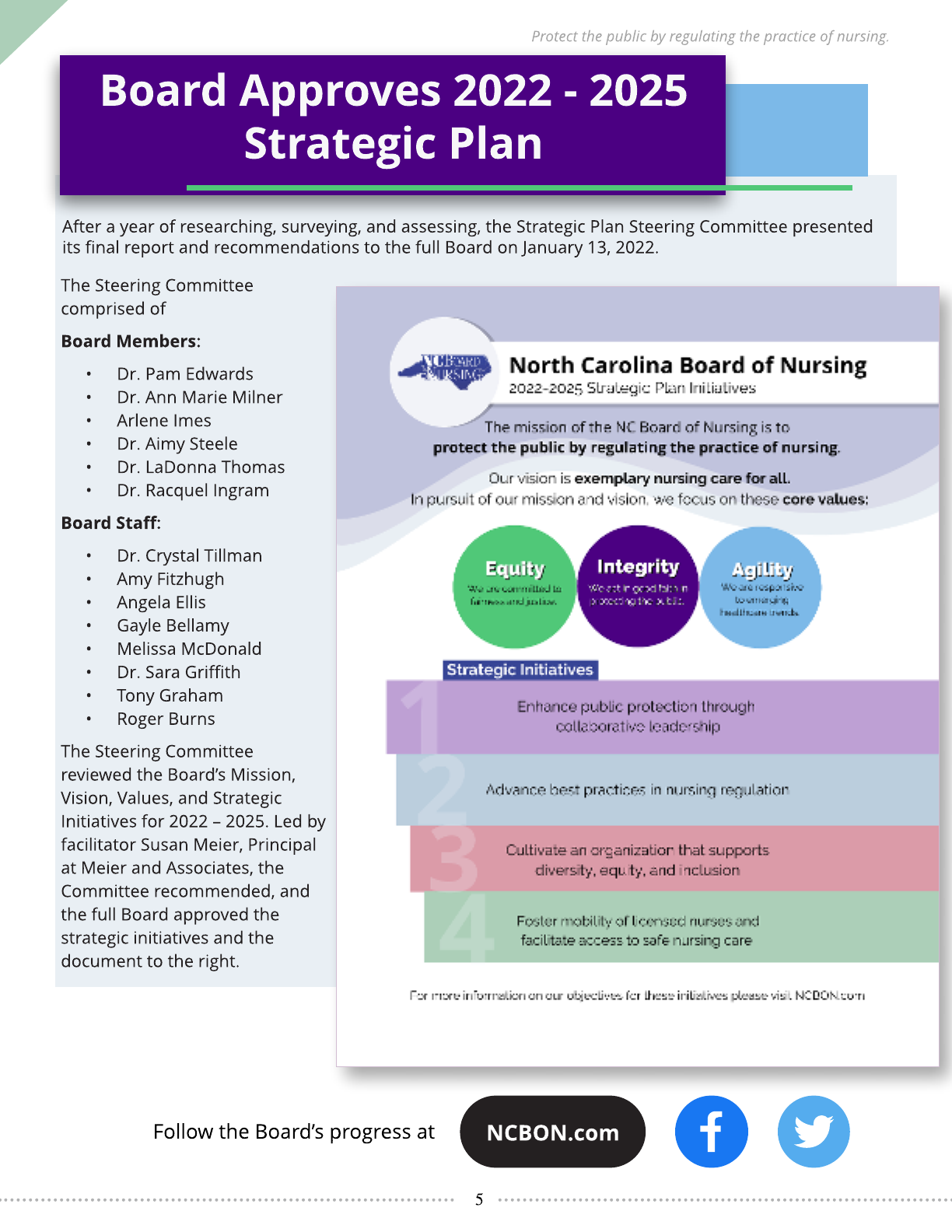
After a year of researching, surveying, and assessing, the Strategic Plan Steering Committee presented
its final report and recommendations to the full Board on January 13, 2022.
Follow the Board?s progress at
Board Approves 2022 - 2025
Strategic Plan
The Steering Committee
comprised of
Board Members:
- Dr. Pam Edwards
- Dr. Ann Marie Milner
- Arlene Imes
- Dr. Aimy Steele
- Dr. LaDonna Thomas
- Dr. Racquel Ingram
Board St aff:
- Dr. Crystal Tillman
- Amy Fitzhugh
- Angela Ellis
- Gayle Bellamy
- Melissa McDonald
- Dr. Sara Griffith
- Tony Graham
- Roger Burns
The Steering Committee
reviewed the Board?s Mission,
Vision, Values, and Strategic
Initiatives for 2022 ? 2025. Led by
facilitator Susan Meier, Principal
at Meier and Associates, the
Committee recommended, and
the full Board approved the
strategic initiatives and the
document to the right.
NCBON.com

6
Protect the public by regulating the practice of nursing.
Click here to wat ch the full
2022 January Board Business Meeting
in it s ent irety.
2022 Board Member Oath of Office
Duties of a Board Member
The major duties and responsibilities of NCBON
Board members are defined in the Nursing
Practice Act (GS 90-171.23). A portion of the duties
are listed below:
- Issue its interpretations of the Nursing
Practice Act (i.e. position statements and
decision trees). These can be found on the
NCBON website (www.ncbon.com).
- Adopt, amend, or repeal rules and
regulations as necessary to carry out the
provisions of the Nursing Practice Act
(NPA).
- Establish qualifications of, employ, and set
the compensation of an executive officer
who shall be a registered nurse and who
shall not be a member of the Board.
- Examine, license, and renew the licenses of
duly qualified applicants for licensure.
- Investigate and take appropriate action for
violations of the NPA.
- Establish standards and monitor nursing
programs that lead to initial licensure.
- Implement and monitor continuing
education of nurses.
- Appoint advisory committees.
- Appoint and maintain a subcommittee of
the Board to work jointly with the
subcommittee of the North Carolina
Medical Board to develop rules and
regulations to govern the performance of
medical acts by registered nurses.
- Recommend and collect such fees for
licensure, license, renewal, examinations,
and reexaminations.
- Implement the interstate compact.
- Establish programs for aiding in the
recovery and rehabilitation of nurses who
experience chemical addiction or abuse or
mental or physical disabilities and
programs for monitoring such nurses for
safe practice.
- Establish programs for aiding in the
remediation of nurses who experience
practice deficiencies.
Each elected or appointed Board members serve a
4-year term.
Our next Board meeting is scheduled for May 19,
2022. Follow the NCBON on social media or check
our website for a link to watch live!
Dr. Shakira Henderson and Cheryl Wheeler were
elected for terms starting in January 2022 by the
Nurses of North Carolina.
On January 13, 2022, they took the oath of office
during the Board Business Meeting.

7
Protect the public by regulating the practice of nursing.
Following @NCNursingBoard on Social Media gives you
access to up-to-dat e informat ion bet ween issues of The
Bulletin - Pract ice Changes, Renewal Reminders, Rule
Revisions, and so much more.
Click any of the icons below to find our pages.
Orient ation Session for Adm inistrat ors of
Nursing Services and Mid-level Nurse
Managers
March 22, 2022 - virtual
April 26, 2022 - virtual
Educat ion Program Director Orient ation
(EPDO)
September 14, 2022
The 18t h Annual Educat ion Summit
March 28, 2022 - virtual
Upcoming Events
Meetings may be held virtually. Please check www.ncbon.com.
Board Meet ing
May 19, 2022
Administrat ive Hearings
May 18, 2022
Hearing Committ ee
March 30, 2022
April 27, 2022
June 29, 2022
Educat ion & Practice Commit tee
March 8, 2022 - virtual
Please visit www.ncbon.com for updates to our
calendar and call-in information to attend public
meetings.

8
Protect the public by regulating the practice of nursing.
Although we just completed a successful Board of
Nursing election, we are already preparing for our
next election. In 2022, the Board will have three
openings: RN ADN/Diploma Nurse Educator, RN
Staff Nurse, and LPN. The nomination form must
be completed and received in the Board office on
or before April 1, 2022. Read the nomination
instructions and make sure the candidate(s) being
nominated meets all the requirements.
Inst ruct ions
Nominations for both RN and LPN positions shall
be made by submitting a completed nomination
form signed by at least 10 RNs (for an RN nominee)
or 10 LPNs (for an LPN nominee) eligible to vote in
the election. The minimum requirements for an RN
or an LPN to seek election to the Board and to
maintain membership are as follows:
1. Hold a current unencumbered license to
practice in North Carolina;
2. Be a resident of North Carolina;
3. Have a minimum of five years' experience in
nursing; and,
4. Have been engaged continuously in a
position that meets the criteria for the
specified Board position, for at least three
years immediately preceding the election.
Minimum ongoing-employment requirements for
both RNs and LPNs shall include continuous
employment equal to or greater than 50% of a
full-time position that meets the criteria for the
specified Board member position, except for the
RN-At Large position.
If you are interested in being a candidate for one of
the positions, visit our website at www.ncbon.com
for additional information, including a Board
Member Job Description and other Board-related
information. You may also contact Chandra Graves,
Manager, Administration, at chandra@ncbon.com
or (919) 782-3211, ext. 232. After careful review of
the information packet, you must complete the
nomination form and submit it to the Board office
by April 1, 2022.
Guidelines for Nom inat ion
1. RNs can petition only for RN nominations and
LPNs can petition only for LPN nominations.
2. Only petitions submitted on the nomination
form will be considered. Photocopies or faxes
are not acceptable.
3. The certificate number of the nominee and each
petitioner must be listed on the form.
4. Names and certificate numbers (for each
petitioner) must be legible and accurate.
5. Each petition shall be verified with the records of
the Board to validate that each nominee and
petitioner holds appropriate North Carolina
licensure.
6. If the license of the nominee is not current, the
petition shall be declared invalid.
7. If the license of any petitioner listed on the
nomination form is not current, and that finding
decreases the number of petitioners to fewer
than ten, the petition shall be declared invalid.
8. The envelope containing the petition must be
postmarked on or before April 1, 2022, for the
nominee to be considered for candidacy.
Petitions received before April 1, 2022 deadline
will be processed on receipt.
9. Elections will be held July 1 through August 15,
2022. Those elected will begin their terms of
office in January 2023.
Please submit completed
nomination form to:
2022 Board Election
North Carolina Board of Nursing
P.O. Box 2129
Raleigh, NC 27602-2129
NOMINATION FORM FOR 2022 ELECTION

9
Protect the public by regulating the practice of nursing.
NOMINATION OF CANDIDATE FOR MEMBERSHIP ON THE
NORTH CAROLINA BOARD OF NURSING FOR 2022
We, the undersigned currently licensed nurses, do hereby petition for the name of
____________________________________________________________RN / LPN (circle one),
whose Certificate Number is _______________________________, to be placed in nomination as a
Member of the NC Board of Nursing in the category of (check one):
RN (ADN/Diploma Nurse Educator) RN (Staff Nurse) LPN
Address of Nominee:
Telephone Number: Home: Work:
E-mail Address:
PETITIONER
At least 10 petitioners per candidate required.
Only RNs may petition for RN nominations. Only LPNs may petition for LPN nominations.
TO BE POSTMARKED ON OR BEFORE APRIL 1, 2022
Name Signat ure Certificate Number
Nomination Form Instructions on page 8.

10
Protect the public by regulating the practice of nursing.
A web-based tool forecasting future supply and demand of
RNs and LPNs in NC.
This project is brought to you by the Cecil G. Sheps Center
for Health Services Research at the
University of North Carolina in Partnership with the
North Carolina Board of Nursing.
For questions specific to the model,
contact the UNC Program on Health
Workforce and Research
(nchealthworkforce@unc.edu). To
discuss the partnership between the
NCBON and Cecil G. Sheps Center,
contact Catherine Moore, PhD, RN,
Chair of the NCBON Research
Committee (cmoore@ncbon.com).
NC Nursecast
Click
Here
11
Protect the public by regulating the practice of nursing.
Administrative Matters
- Approved the Mission, Vision, Values and Strategic
Initiatives for 2022-2025 (see page 5)
- Approved the proposed revisions to Fiscal Policies
Education Matters
Ratification of Determination of Program Approval Status:
- Watts College of Nursing, Durham ? BSN
- Ratification of Full Approval Status:
- Central Piedmont Community College, Charlotte ?
ADN
- Davidson-Davie Community College, Lexington ? ADN
- Mars Hill University, Mars Hill ? BSN
- University of North Carolina, Greensboro ? BSN
- University of North Carolina, Chapel Hill ? BSN
Ratification of Approved Enrollment Expansion
- Cape Fear Community College, Wilmington ? ADN,
increase enrollment by 60 for a total program
enrollment of 260 students beginning January 1, 2022
- Gardner-Webb University, Boiling Springs ? BSN,
increase enrollment by 40 for a total program
enrollment of 190 students beginning November 30,
2021
Notification of Planned Decrease in Approved Total
Enrollment
- Gardner-Webb University, Boiling Springs ? ASN,
decrease enrollment by 40 for a total program
enrollment of 100 students beginning November 30,
2021
Ratification of Approval of Refresher Course
- Lenoir Community College, Kinston ? RN
Notification of Alternate Scheduling Option
- Alamance Community College, Graham ? ADN
- Beaufort Community College, Washington ? ADN
- Blue Ridge Community College, Hendersonville ? ADN
- Caldwell Community College, Hickory ? ADN
- Carolinas College of Health Sciences, Charlotte ? ADN
- Central Carolina Community College, Sanford ? LPN
- Chamberlain University, Charlotte ? BSN
- College of the Albemarle, Elizabeth City ? ADN
- Craven Community College, New Bern ? ADN
- Gardner-Webb University, Boiling Springs ? BSN
- Mars Hill University, Mars Hill ? BSN
- Mitchell Community College, Statesville ? ADN
- Montgomery Community College, Troy ? ADN and
LPN
- Nash Community College, Rocky Mount ? ADN and
LPN
- Pfeiffer University, Misenheimer ? BSN
- Randolph Community College, Asheboro ? ADN
- Region A Nursing Consortium, Clyde ? ADN
- Rockingham Community College, Wentworth ? ADN
and LPN
- Sandhills Community College, Pinehurst ? ADN
- Surry Community College, Dobson - ADN
- Wilson Community College, Wilson ? ADN
FYI Accreditation Decisions by ACEN for Initial or
Continuing Approval & Next Visit Date
- Catawba Valley Community College, Hickory ? ADN ?
Continuing approval ? Spring 2021
- Davidson-Davie, Lexington ? ADN ? Continuing
approval with conditions ? Spring 2021
- Gardner-Webb University, Boiling Springs ? BSN and
ASN ? Continuing approval - remove conditions status
? Spring 2021
- Watts College of Nursing (Duke Regional Hospital),
Durham ? BSN ? Initial approval visit ? Spring 2021
- Wayne Community College, Goldsboro ? ADN and
LPN ? Continuing approval ? Spring 2021
NCLEX Quarterly Pass Rates
- 4th Quarter
Alternate Scheduling Option
- Northeastern University, Charlotte ? BSN Program
Option and Enrollment Expansion
- Determination of Program Approval Status ? Initial
Approval for New Program
- Belmont Abbey College, Belmont ? BSN Program
- High Point University, High Point ? BSN Program
- Isothermal Community College, Spindale ? ADN
Program
- McDowell Technical Community College, Marion ?
ADN Program
- University of Mount Olive, Mount Olive ? BSN Program
Practice Matters
NAII Programs:
Ratification of Approval NA II Courses:
- Beaufort County Community College, Washington -
Career & College Promise
- Beaufort County Community College, Washington -
Continuing Education
Board of Nursing Actions
12
Protect the public by regulating the practice of nursing.
Author: Terry Ward, PhD, RN, CNE
RESILIENCE:
A Key to Safe Nursing Practice
Disclosure St atem ent ? The following disclosure applies to the NCBON continuing nursing education article entitled
?Resilience: A Key to Safe Nursing Practice.? Participants must read the CE article, online reference documents (if
applicable), and the Reflective Questions in order to earn CE contact hours. Verification of participation will be noted by
online registration.
Provider St atem ent ? The North Carolina Board of Nursing will offer 1.5 contact hours for this continuing nursing
education activity.
The North Carolina Board of Nursing is approved as a provider of nursing continuing professional development by the
North Carolina Nurses Association, an accredited approver by the American Nurses Credentialing Center?s Commission on
Accreditation.
Introduction:
The North Carolina Board of Nursing (NCBON)
recognizes the pandemic's toll across the state.
Increased inquiries to the NCBON of nursing staff
regarding the scope of practice, staffing, and
interpretation of law and rule are evidence of the
dilemma nurses and healthcare organizations face
during these times. The difficult and turbulent
times during the COVID pandemic have created
circumstances that can prevent nurses from fully
complying with the safety goals, practices,
procedures, and nursing practice laws. This
behavior is not conducive to safe nursing practice.
Despite the burden and chaos characterizing their
work environment, the mission of nurses is to
maintain patient safety. To achieve this goal,
nurses must replace feelings of fatigue and
burnout with resilience. Encouraging nurses'
resilience can create work environments of
professionalism, mindfulness, and awareness of
errors or potential errors. Resilience is a key to
maintaining patient safety and regulatory
compliance. Some of the competencies to building
Learning Out come: Nurses completing this activity and evaluation will identify by self-assessment a gain in knowledge related
to resilience and the NCBON resources to support resilience.
Purpose: The purpose of this article is to provide knowledge regarding the definition of resilience, challenges to resilience,
strategies for enhanced resilience, and resources to support professional and personal resilience.
EARN CE CREDIT
INSTRUCTIONS
Read the article, online reference documents (if applicable), and the Reflective Questions.
EARN CONTACT HOUR CERTIFICATE
Go to www.ncbon.com and scroll over ?Education?; under ?Continuing Education,? select ?Board Sponsored Bulletin Offerings,?
scroll down to link, ?Resilience: A Key to Safe Nursing Practice.? Register. Be sure to write down your confirmation number,
complete, and submit the evaluation and print your certificate immediately.
If you experience issues with printing your CE certificate, please email paulette@ncbon.com. In the email, provide your full name
and the title of the CE offering (Resilience: A Key to Safe Nursing Practice).
Registration deadline is July 1, 2024.
CE Article

13
Protect the public by regulating the practice of nursing.
resilience are knowing when, where, and from
whom to obtain needed help. This article aims to
define resilience, discuss challenges to resilience,
provide strategies for enhanced resilience, and
provide resources to support professional and
personal resilience, which lead to safe nursing
practice.
Background
On March 10, 2020, Governor Roy Cooper issued
an executive order declaring a state of emergency
in North Carolina (NC Governor Roy Cooper, 2020).
The declaration activated a response from nursing
professionals in all sectors of the profession.
Nurses had to address the need to protect the
health of the public. Fear of infection, lack of
capacity, work overload, and insufficient
preparation are all causes of psychological distress
(Lorente et al., 2021). The COVID-19 pandemic has
increased demands and exerted tremendous
stress on the lives of healthcare workers (Jo et al.,
2021). As the adversities of the pandemic continue
to unfold, nurses need resources to mitigate
distress. Resilience is a characteristic that can help
nurses to better cope during crises and function
more effectively in their roles.
Definition of Resilience
The American Psychological Association (2014)
defines resilience as "the process of adapting well
in the face of adversity, trauma, tragedy, threats, or
even significant sources of stress (para. 4)." In an
integrative literature review, Aburn et al. (2016)
state that no universal definition of resilience
exists. However, key definitions or concepts of
resilience were identified, such as rising above to
overcome adversity, adaptation and adjustment,
good mental health as a proxy for resilience, and
the ability to bounce back (Aburn et al., 2016).
Resilience is a construct that includes a cluster of
concepts. In an extensive literature review, Morse
et al. (2021) identified associated concepts to
describe resilience as a state and a process.
Concepts of maintenance (Stewart & Yuen, 2011),
equilibrium (Bonanno, 2004; Wagnild & Young,
1990), hardiness (Wilks et al., 2011), psychosocial
well-being (Bekhet & Avery, 2017; Fletcher &
Sarkar, 2013; Gillespie et al., 2007; Shaw et al.,
2009), and stability (Wagnild, 2003) were included
when viewing resilience as a state.
Resilience as a process reiterates "the action or an
act of rebounding or springing back; rebound,
recoil" ("Resilience," OED, 2020, Entry 163619).
Securing internal and external resources to
manage illness flexibly articulates this process of
resilience (Haase et al., 2017). Competency (Greene
et al., 2004; Haase et al., 2017; Masten, 1994),
adaptation (Kimura et al., 2019), and positive
adjustment during adversity outline actions taken
during a changed life trajectory (Alizadeh et al.,
2018; Black & Dorstyn, 2015).
Resilience is seen as a positive and sustaining
outcome, often allowing individuals to flourish
despite their present life circumstances (Molina et
al., 2014). Mancini and Bonanno (2009) further
considered resilience a particular trajectory or
mechanism of positive adaptation that changes
over time and protects against psychological
distress. However, most authors agree that
resilience commences with adversity (Ungar, 2003).
Some recognize that this adversity is an event (e.g.,
a natural disaster or global pandemic); others
might consider it the result of a long-term stressor
(e.g., mental health issues) (Morse et al., 2021).
1. Review the definitions of resilience above.
Reflect on or create an individual definition
which can be adapted for nursing practice in
its current state.
Challenges to Resilience
As of July 2021, nurses have experienced four
waves of COVID-19 surges. The strain and stressors
are unprecedented. Nurses are being faced with a
surge in nursing capacity, burnout, and moral
distress. All these challenges to resilience lead to
alterations in well-being.
In developing a nursing diagnosis taxonomy, Ward
and Eisbach (2013) identified three alterations in
resilience: risk for compromised resilience,
impaired individual resilience, and readiness for
enhanced resilience. Risk for compromised
resilience is defined as a potential decreased
ability to sustain a pattern of positive responses to
an adverse situation or crisis. Impaired resilience is

14
Protect the public by regulating the practice of nursing.
an actual decreased ability to sustain a positive
response to an adverse situation or crisis.
Readiness for enhanced resilience is a pattern of
positive responses to adverse situations or crisis
that is sufficient for optimizing human potential
and can be strengthened (Ward & Eisbach, 2013).
Impaired or compromised resilience is defined as a
decreased ability to sustain a pattern of positive
responses to an adverse situation or crisis (Ward &
Eisbach, 2013). Defining characteristics include
decreased interest in activities, depression, guilt,
isolation, low self-esteem, the renewed elevation of
distress, and the use of maladaptive coping skills
(Ward & Eisbach, 2013). It is vital to explore deeper
the challenges associated with impaired or
compromised resilience.
Surge in Nursing Capacity
The COVID-19 pandemic is a surge-generating
event. The critical components of the surge include
staff, stuff, structure, and systems (Adams, 2009).
Staff refers to personnel, stuff consists of supplies
and equipment, structure refers to facilities, and
systems include integrated management policies
and processes (Adams, 2009; Barbisch & Koenig,
2006; Phillips, 2006; Schultz & Koenig, 2006).
Nurses report feeling the effects of the surge in
nursing capacity physically, emotionally, and
psychologically (Walsh, 2021). The World Health
Organization (WHO) declared 2020 as the Year of
the Nurse and Midwife, intending to raise
awareness of the need for "nine million more
nurses and midwives to achieve universal health
coverage by 2030" (WHO, 2020b, para. 1). The
nursing community could not have fathomed the
coming of a global pandemic or the significant
impact on the nursing workforce. The COVID-19
pandemic placed a substantial increase in demand
for nurses and their need to perform. This surge in
nursing capacity has overwhelmed the profession.
The surge in capacity is relevant to the nursing role
in various settings, and nurses must become aware
of the concept, implications, and how it relates to
public protection. The Joint Commission (2008) has
defined surge capacity as "the ability to expand
care capabilities in response to sudden or more
prolonged demand" (p.19). It can also be described
as the ability to obtain adequate staff, supplies and
equipment, structures, and systems to provide
good care to meet the immediate health needs of
the public amid a crisis (Adams, 2009).
The North Carolina Board of Nursing in
collaboration with the North Carolina Healthcare
Foundation (NCHF), the North Carolina
Organization of Nurse Leaders (NCONL), and the
North Carolina Directors of Nursing Administration
in Long Term Care (NC DONA/LTC) acknowledge
the surge in nursing capacity across the state of
North Carolina (NCBON, 2021).
These organizations' collaborative efforts resulted
in resources supporting the surge in nursing
capacity. The document highlights how limited
numbers of well-qualified staff cause short staffing
and extended work hours to pose considerable
challenges for RNs, LPNs, and other healthcare
providers. Changes in care delivery models and
team composition were also identified as
challenges. During widespread emergencies, there
is a high likelihood that the type of care delivery
will change. In addition, care teams may consist of
team members unfamiliar with one another.
Another challenge is unintended barriers to
nursing practice in the organization by facility
policies which may be more restrictive than the
legal scope requires. Nurse leaders are
encouraged to acknowledge the stress the changes
may cause.

15
Protect the public by regulating the practice of nursing.
Burnout
Burnout is a syndrome that results from chronic
workplace stress that has not been managed. It is
characterized by exhaustion, negative feelings or
cynicism related to one's job, and reduced
professional efficacy (Janeway, 2020; Maslach et al,
2017). Burnout is a significant threat to the stability
of the nursing workforce (Janeway, 2020). Studies
before the pandemic indicate the prevalence of
burnout among US registered nurses (RNs) ranges
from 35 to 45% (Dyrbye et al., 2017; Li, 2018; Moss
et al., 2016). Nurses experiencing burnout are
more likely to have higher stress levels, get less
sleep, and are more likely to be overweight than
the general population (Eanes, 2015; Lee et al.,
2011; Melnyk et al., 2013; Thacker et al., 2016).
Letvak et al. (2012) studied depression among RNs
and found almost twice the rate of depression
compared with those in other professions. Burnout
has been shown to have a negative impact on
patient satisfaction, worsen patient outcomes or
increase rates of safety events, and increase
mortality (Magtibay & Chesak, 2017).
National Council of State Boards of Nursing's
(NCSBN) Environmental Scan (2021) reported on
the issues of patient safety, healthcare quality, and
healthcare delivery. The report shared findings
from (Garcia et al., 2019), which revealed a more
than 60% association between burnout and patient
safety. Factors influencing burnout included
teamwork climate, work environment, workload,
professional tiredness, workplace safety, job
satisfaction, and personal and professional life
imbalance (Garcia et al., 2019). A positive safety
culture, which includes open communication,
management support, professional suitability,
mutual learning, teamwork, good interpersonal
relationships, and organizational workflow
improvements, prevents professional fatigue
(Garcia et al., 2019).
Moral Distress
The COVID-19 pandemic has caused moral distress,
which is pervasive in health care settings where
nurses work in a diverse number of nursing roles
(Lake et al., 2021; Whitehead et al., 2015). The
pandemic has created a crisis state in professional
nursing practice. Shifting standards of care,
interrupted patient relationships, triaging limited
resources, working in unfamiliar environments,
and uncertainty about disease progression, and
transmission are only a few of the potential
sources of moral distress during the pandemic.
The American Nurses Association's Code of Ethics
for Nurses with Interpretive Statements (2015)
defines moral distress as "the condition of knowing
the morally right thing to do, but institutional,
procedural, or social constraints make doing the
right thing nearly impossible." Moral distress, the
code emphasizes, "threatens core values and
moral integrity." (Rushton et al., 2017). Moral
distress is characterized by feeling powerless and
unable to speak up or be heard (Hamric, 2014). It is
associated with the individual's duty to uphold
professional and ethical standards or
responsibilities. When an individual experiences
moral distress, they feel compromised in their
ability to practice as moral agents according to
professional values and standards (Lake et al.,
2021). According to the National Academies of
Sciences, Engineering, and Medicine (2021) Future
of Nursing 2020?2030 report, nurses' well-being is
affected by the demands of the job, which in turn
affects their work.
Strategies For Enhanced Resilience
Resilience is often deployed to tackle the
adversities faced by nurses. Therefore, nurses
need to implement strategies to enhance their
professional and personal resilience. Increasing
resilience takes time and intentionality.
Implementing strategies for enhanced resilience,
along with resources to support professional and
personal resilience, will allow nurses some reprieve
from emotional distress, rendering nurses more
capable of coping, complying with professional
standards, and delivering quality and safe nursing
care (Henshall et al., 2020, & Hamric, 2014).
The American Psychological Association (APA)
outlines four core components of resilience:
connection, wellness, healthy thinking, and
meaning. Focusing on these four core components
can empower nurses to withstand and learn from
complex and traumatic experiences (APA, 2020).

16
Protect the public by regulating the practice of nursing.
These core components have been further
contextualized, making them actions nurses can
take to enhance personal resilience.
- Connection: Prioritize healthy relationships
with empathetic and understanding people
so that you are reminded you are not alone
in the midst of difficulties. Having
trustworthy and compassionate individuals
who validate your feelings will support the
skill of resilience. Be sure to accept support
from those who care about you.
- Wellness: Take care of your body by
practicing self-care, including proper
nutrition, exercise, sleep, hydration,
mindfulness, etc.
- Healthy Thinking: Maintain healthy thought
patterns by keeping things in perspective,
accepting that change is inevitable, avoiding
negative outlets, and striving to maintain a
positive attitude.
- Meaning: Find your purpose; help others, be
a proactive problem solver during hard
times, and set and work towards realistic
goals to identify tangible signs of growth and
self-discovery (APA, 2020).
These strategies for personal resilience can be
developed to enhance the individual nurse's ability
to cope with stressful and chaotic healthcare
environment challenges. Personal resilience should
be combined with efforts to build resilient teams to
effectively address the root causes of moral distress
and burnout, which often stem from
organizational/systems failures and ineffective
leadership (Stephens, 2019). Professional resilience
is the capacity to thrive in demanding situations,
with choices made when responding to difficult
situations, attitude, and willingness to act.
Elements of professional resilience include
maintaining positive collegial relationships,
professional networks, professional development,
and service or participation. Professional resilience
is not a passive concept. It involves active
engagement on the part of the individual. Jo et al.
(2021), in a study examining factors associated with
nurses' resilience during the COVID-19 pandemic,
found that nurses participating in policy and
procedure development had higher resilience
scores.
Resources For Professional and
Personal Resilience
Enhanced resilience is demonstrated when nurses
can identify available resources, support systems,
and adapt to adversities and challenges (Ward &
Eisbach, 2013). The primary resources for nurses
needed to manage the complexities of nursing
practice are the ANA Code of Ethics, State Nursing
Practice Act and Rules, and the regulatory
guidance of their state board of nursing.
ANA Code of Ethics
The American Nurses Association (ANA) Code of
Ethics is a dynamic and robust anchor for
professional nursing practice. During these
turbulent times in nursing, nurses need to tap into
this timeless resource. The Code of Ethics consists
of two components: the provisions and
accompanying interpretive statements. There are
nine provisions. The first three describe the nurse's
most fundamental values and commitments; the
next three address boundaries and duty of loyalty;
and the last three address duties beyond the
individual patient encounters. For each provision,
there are interpretive statements that provide
greater specificity for practice and are responsive
to the contemporary context of nursing. Position
statements from constituent members are
included for additional detailed guidance to
address clinical, research, administrative,
educational, and public policy issues (ANA, 2015).
A copy of the Code of Ethics and Interpretive
Statements are available in a view-only format for
members and non-members of ANA at
The American Nurses Association (ANA) Code of
Ethics for Nurses with Interpretive Statements
during the pandemic may help nurses shift our
focus and decrease moral distress. During a
pandemic, we move away from a focus on
NursingWorld.org
https://www.nursingworld.org/practice-policy/
nursing-excellence/ethics/
code-of-ethics-for-nurses/coe-view-only/

17
Protect the public by regulating the practice of nursing.
relationship-centered care (Provision 2,
Commitment to Patient) and adopt an
outcome-based framework (Provision 8, Promotion
of Community and World Health). In an
outcome-based framework the nurse focuses on
strategies to avoid entering crisis standards of care
and when crisis is unavoidable, works to fairly save
the greatest number of people possible (Webster &
Wocail, 2020). While this shift in thinking can be
exceptionally challenging, the code of ethics
provides necessary guidance to assist nurses in
maintaining compliance with standards for
professional practice.
North Carolina Board of Nursing
The NCBON role is to bring attention to the issues
impacting safe nursing practice, such as burnout
and resilience in professional nursing practice.
Furthermore, the Board's role is to work
collaboratively with nurses, healthcare
organizations, and state agencies to identify
guidance and meaningful resources to support
safe nursing practice. This positions the Board to
achieve its mission of public protection and vision
of exemplary nursing care for all. The North
Carolina Nurse Practice Act (NPA) is a law that
works together with the North Carolina
Administrative Code (NCAC) in the state to govern
safe nursing practice. This act provides the
framework for safe, competent nursing practice.
The NPA defines nursing practice for both
registered and licensed practical nurses. The
registered nurse has ten components of nursing
practice, and the licensed practical nurse has seven
components of practice. These components are
further explained in NCAC. Position Statements are
also available to interpret further and clarify law
and rule. Like the ANA Code of Ethics Interpretive
Statements, the NCBON Position Statements
provide guidance and direction related to common
practice issues experienced by nurses. (NCBON,
2020a; NCBON 2020b; NCAC, 2022). These
resources, along with consultation from NCBON
staff, serve as a support resource for nurses who
may be experiencing impaired resilience resulting
in stress, burnout, and moral distress. These tools
are most effective when nurses know and utilize
them to make decisions regarding safe nursing
practice. Expert staff well versed in nursing law
and rule, licensure, education, practice, and
compliance are available to assist nurses with
related matters. By engaging the NCBON staff,
nurses can assist the NCBON in carrying out its
strategic plan to enhance public protection,
advance best practices in nursing regulation, and
facilitate access to safe nursing care.
Nursing Surge in Capacity Document
As mentioned earlier, the Nursing Surge Capacity
document by the (NCBON), (NCHF), (NCONL), (NC
DONA/LTC) (NCBON, 2021) captures the current
state of nursing practice as a result of the
biological event COVID-19. It serves as a resource
to provide solutions for nurses to combat the
challenges faced due to the pandemic. The
document provides an overview of the nurse's
accountability for safe nursing practice and laws
and rules which mandate that practice. The paper
offers examples of care delivery models that
support appropriate staffing and nursing care
capabilities during infectious disease epidemics.
The resource highlights NCBON resources to
support scope of practice barriers. It includes
contact information for consultation from Board
staff and links to additional resources in the list
below (NCBON, 2021; NCBON, 2020c). The Nursing
Surge in Capacity document has a plethora of
information to assist and support nurses during
the pandemic. Nurses must use the knowledge in
resources such as these to build their capacity to
adapt well in the face of adversity, trauma, tragedy,
and significant sources of stress.
- Nursing Practice Act GS 90-171.20 (7) and (8)
- Administrative Rule 21 NCAC 36.0224
- Administrative Rule 21 NCAC 36.0225

18
Protect the public by regulating the practice of nursing.
- Current NC NCBON temporary waivers and
guidance
- Position Statements and Decision Trees:
- Scope of Practice Decision Tree for the RN
and LPN
- Delegation and Assignment of Nursing
Activities
- LPN Scope of Practice Clarification
- RN Scope of Practice Clarification
- Delegation of Immunization Administration
to UAP
- Infusion Therapy- Insertion/Access
Procedures
- Delegation: NAII Credentialed as EMT-I/P
- Delegation of Medication Administration to
UAP
- Important Information About COVID-19
Vaccines
Finally, additional community resources are
available, such as the NC Area Health Education
Centers (AHEC), Centers for Disease Control,
American Association of Critical Care Nurses, The
Society of Critical Care Medicine, and the American
Association of Colleges of Nursing.
2. Review the Nursing Practice Act GS 90-171.20
(7) and (8), Administrative Rule 21 NCAC 36.0224,
Administrative Rule 21 NCAC 36.0225, and
Position Statements and Decision Trees: Scope of
Practice Decision Tree for the RN and LPN. Reflect
on how these resources can assist in the delivery
of safe patient care.
3. Review the Nursing Surge in Capacity Resource.
Reflect on situations in practice for which this
resource can be used to provide solutions.
4. Reflect on opportunities for which practice
consultation may be beneficial.
Professional and Personal Resilience
Nurses must recognize the Governor's formal
declaration of a state of emergency enables the
NCBON legal and regulatory power to govern safe
nursing practice and implement protections for
public health. Guidance statements which the
Board developed, support professional practice.
Nurses should access guidance statements,
recommendations, and provisions of rules. A nurse
can access these resources on the NCBON website
(NCBON, 2020 d). To maintain professional
resilience, nurses must be aware of these critical
resources during a crisis.
Nurses can find themselves operating in crisis
during a pandemic. The ANA Crisis Standard of
Care is a resource that can build professional
resilience. This resource provides guidance that
applies to care decisions made during extreme
circumstances, such as those resulting from
emergencies, disasters, or pandemics like
COVID-19 (ANA, 2020). The resource defines crisis
standard of care as a substantial change in regular
healthcare operations and the level of care it is
possible to deliver, which is made necessary by a
pervasive (e.g., pandemic influenza) or catastrophic
(e.g., earthquake, hurricane) disaster (ANA, 2020).
The crisis standard discusses the change in ethical
frameworks nurses face. It also offers answers to
frequent challenges nurses and their colleagues
address during a crisis. Guidance for institutions is
also included.
Being ready to adapt and provide essential care
under crisis conditions is a professional
responsibility (ANA 2020). Resilience often results
in personal growth (APA, 2020; Stephens, 2019).
Personal resilience can be defined as a person's
ability to cope with stress and adversity and
continue to function effectively (Rice and Lui, 2016).
Individual resilience involves behaviors, thoughts,
and actions that promote personal well-being (US
DHHS, 2020). Stephens (2019) defines personal
resilience as an individual's use of personal
protective factors (PPFs) to navigate stressful
situations or perceived adverse events to cope
effectively and reach a higher level of well-being.
When a nurse desires individual or personal
resilience, it is vital to have a plan. Stephens Model
of Resilience (2019) for building resilience begins
with assessing PPFs that may need to be
strengthened or enhanced. These PPFs are defined
as coping skills that help defend us against the
effects of stress. Examples of PPFs are
competence, faith/spirituality, flexibility, hope,
humor, meaning in life, optimism, perseverance,
positive emotions, self-awareness, self-efficacy,

19
Protect the public by regulating the practice of nursing.
self-esteem, and social support. An assessment of
strengths and areas of improvement in these areas
will help nurses conceptualize PPFs individually.
Nurses should identify two or three of the factors
they desire to enhance. The model proposes
developing and enhancing PPFs strengthens efforts
to handle adversity and improve well-being.
Stephens (2019) further asserts four central
themes are vital to building resilience. The four
themes or 4 Ps are priorities, purpose, perspective,
and personal responsibility. Priorities means what
matters most to the individual; purpose means
recognizing meaning in life experiences;
perspective means striving to see the big picture,
and personal responsibility means being
accountable for one?s own well-being.
Nurses should ask themselves the
following questions:
- Priorit ies - What are my priorities? What
matters most to the individual? How do you
define ?doing what is right?? Does the way
you spend your time and energy accurately
reflect your priorities? If not, what?s taking
their place?
- Purpose - Why are you here? Do you
believe there?s a reason for everything that
happens to you? Do you seek to learn from
failure, disappointment, or ?bad?
experiences?
- Perspect ive - Do you strive to see the
?bigger picture? when you?re faced with a
difficult situation? How do you remain
informed? Who/what do you consult before
making decisions?
- Personal responsibilit y - Do you believe
you?re accountable for your actions? Do you
consider the effects of your behavior on
others when choosing your response to a
situation? Are you willing to ?change your
mind? or admit your mistakes for the good
of your team or colleagues? (Stephens,
2019).
Nurses can apply this model immediately into daily
life to strengthen personal resilience. When
implementing this model nurses should recognize
resilience building is an active process.
5. Access Stephens Model for Building personal
resilience available in the link below. Conduct the
?What are your PPF's? self-assessment.
https://www.myamericannurse.com/
wp-content/uploads/2019/08/
ant8-Resilience-729a.pdf
6. Identify 2-3 personal protective factor (PPF?s)
or coping skills for enhancement.
7. Reflect on the questions related to the
?Building resilience with the 4 Ps? from Stephens
Model of Resilience. How did it increase or
improve self-awareness?
The stress of the COVID-19 pandemic on nurse?s
well-being is duly noted in the literature. Resilience
is a mediating factor for nurse?s well-being.
Resources and support presented here are tools
nurses can use to achieve resilience, both
professionally and personally.
8. Consider your previous thoughts related to
professional and personal resilience. Reflect on
the ways in which the information provided in this
article enhanced your knowledge of a nurse?s
individual professional and personal resilience.
Conclusion
This article defined resilience, discussed
challenges to resilience, enhanced resilience
strategies and resources to support professional
and personal resilience. This knowledge can
increase nurse?s ability to face current and future
challenges. When a nurse makes choices anchored
in strategies to enhance personal and professional
resilience, it strengthens their abilities to engage in
safe patient care, resulting in positive patient
outcomes.
About the Aut hor
years of experience. Her areas of expertise include,
oncology, orthopedics, mental health nursing
(resilience), nursing education with a focus in program
evaluation and curriculum. She actively engages in
service and scholarship within the nursing community.
Terry Ward, PhD, RN, CNE
Dr. Ward is an Education
Consultant at the North Carolina
Board of Nursing, in Raleigh, NC.
She is a registered nurse with 34

20
Protect the public by regulating the practice of nursing.
References
Aburn, G., Gott, M., & Hoare, K. (2016). What is resilience? An Integrative Review of the empirical literature.? Journal of Advanced
Nursing,?72(5), 980?1000. https://doi.org/10.1111/jan.12888
Adams, L., Berry, D., (March 26, 2012) "Who Will Show Up? Estimating Ability and Willingness of Essential Hospital Personnel to
Report to Work in Response to a Disaster"?OJIN: The Online Journal of Issues in Nursing?Vol. 17 No. 2.
Alizadeh, S., Khanahmadi, S., Vedadhir, A., & Barjasteh, S. (2018). The Relationship between Resilience with Self- Compassion,
Social Support and Sense of Belonging in Women with Breast Cancer.?Asian Pacific Journal of Cancer Prevention: APJCP,?19(9),
2469?2474. https://doi.org/10.22034/APJCP.2018.19.9.2469
American Nurses Association.?Crisis Standard of Care: COVID-19 Pandemic.?2020.?
nursingworld.org/~496044/globalassets/practiceandpolicy/work-environment/health?safety/coronavirus
/crisis-standards-of-care.pdf
American Nurses Association (ANA). (2015)?Code of ethics for nurses with interpretive statements. Silver Springs, MD:
Nursesbooks.org.
American Psychological Association. (2020, February 1)?Building your resilience. https://www.apa.org/topics/resilience
Barbisch, D.F., & Koenig, K.L. (2006). Understanding surge capacity: Essential elements.?Academic Emergency Medicine, 13,
1098-1102.
Bekhet, A. K., Avery, J. S. (2017).?Resilience from the perspective of caregivers of persons with dementia. Archives of Psychiatric
Nursing, 32(1), 19 23.?https://doi.org/10.1116/j.apnu.2017.09.008.
Black, R., & Dorstyn, D. (2015). A biopsychosocial model of resilience for multiple sclerosis.?Journal of Health Psychology,?20(11),
1434-1444.
Bonanno, G. A., Kennedy, P., Galatzer-Levy, I. R., Lude, P., Elfström, M. L. (2012).?Trajectories of resilience, depression, and anxiety
following spinal cord injury. Rehabilitation Psychology, 57(3),?236.?https://doi.org/10.1037/a0029256
Dyrbye L.N., Shanafelt T.D., Sinsky C. National Academy of Medicine-Perspectives; Washington, D.C.: 2017. Burnout among health
care professionals.
Eanes, L. (2015). CE: The potential effects of sleep loss on a nurse's health.?AJN The American Journal of Nursing,?115(4), 34-40.
Fletcher, D., Sarkar, M. (2013).?Psychological resilience: A review and critique of definitions, concepts, and theory. European
Psychologist, 18(1),?12?23.?https://doi.org/10.1027/1016-9040/a000124
Garcia, C. D. L., Abreu, L. C. D., Ramos, J. L. S., Castro, C. F. D. D., Smiderle, F. R. N., Santos, J. A. D., & Bezerra, I. M. P. (2019).
Influence of burnout on patient safety: systematic review and meta-analysis.?Medicina,?55(9), 553.
Gillespie, B. M., Chaboyer, W., Wallis, M. (2007).?Development of a theoretically derived model of resilience through concept
analysis. Contemporary Nurse, 25(1?2),?124?135.?https://doi.org/10.5172/conu.2007.25.1-2.124
Greene, R. R., Galambos, C., & Lee, Y. (2004). Resilience theory: Theoretical and professional conceptualizations.?Journal of Human
Behavior in the Social Environment,?8(4), 75-91.
Haase, J. E., Kintner, E. K., Robb, S. L., Stump, T. E., Monahan, P. O., Phillips, C., Stegenga, K. A., & Burns, D. S. (2017). The Resilience
in Illness Model Part 2: Confirmatory Evaluation in Adolescents and Young Adults with Cancer.?Cancer Nursing,?40(6), 454?463.
https://doi.org/10.1097/NCC.0000000000000450
Hamric, A. B. (2014). A case study of moral distress.?Journal of Hospice & Palliative Nursing,?16(8), 457-463.
Henshall, C., Davey, Z., & Jackson, D. (2020). Nursing resilience interventions ? A way forward in challenging healthcare territories.
Journal of Clinical Nursing, 29(19-20), 3597?3599. https://doi.org/10.1111/jocn.15276
Janeway D. (2020). The Role of Psychiatry in Treating Burnout Among Nurses During the Covid-19 Pandemic.?Journal of Radiology
Nursing,?39(3), 176?178. https://doi.org/10.1016/j.jradnu.2020.06.004
Jo, S., Kurt, S., Bennett, J. A., Mayer, K., Pituch, K. A., Simpson, V., Skibiski, J., Takagi, E., Karaaslan, M. M., Ozluk, B., & Reifsnider, E.
(2021). Nurses' resilience in the face of coronavirus (COVID-19): An international view. Nursing & Health Sciences, 23(3), 646?657.
https://doi.org/10.1111/nhs.12863
Kimura, N. R., Neto, J. P. S., Santos, R. L., Baptista, M. A. T., Portugal, G., Johannessen, A., ... & Dourado, M. C. (2019). Resilience in
carers of people with young-onset Alzheimer disease.?Journal of Geriatric Psychiatry and Neurology,?32(2), 59-67.

21
Protect the public by regulating the practice of nursing.
Lake, E. T., Narva, A. M., Holland, S., Smith, J. G., Cramer, E., Rosenbaum, K. E. F., ... & Rogowski, J. A. (2021). Hospital nurses' moral
distress and mental health during COVID-19.?Journal of Advanced Nursing.
Lee, W. L., Tsai, S. H., Tsai, C. W., & Lee, C. Y. (2011). A Study on Work Stress, Stress Coping Strategies, and Health Promoting
Lifestyle among District Hospital Nurses in Taiwan.?Journal of Occupational Health, 53(5):377?383.
Letvak S.A. (2012). Depression in hospital-employed nurses.?Clinical Nurse Specialist, 26(3):177?182.
Li H. (2018). Quantification of burnout in emergency nurses: A systematic review and meta-analysis.?International Emergency
Nursing, 39:46?54.?
Lorente, L., Vera, M., & Peiró, T. (2021). Nurses´ stressors and psychological distress during the COVID-19 pandemic: The
mediating role of coping and resilience. Journal of Advanced Nursing, 77(3), 1335?1344. https://doi.org/10.1111/jan.14695
Maslach, C., & Leiter, M. P. (2017). Understanding burnout: New models. In C. L. Cooper & J. C. Quick (Eds.),?The handbook of
stress and health: A guide to research and practice?(pp. 36?56). Wiley Blackwell.?https://doi.org/10.1002/9781118993811.ch3
Magtibay, D. L., Chesak, S. S., Coughlin, K., & Sood, A. (2017). Decreasing stress and burnout in nurses: efficacy of blended
learning with stress management and resilience training program.?JONA: The Journal of Nursing Administration,?47(7/8), 391-395.
Melnyk, B. M., Hrabe, D. P., & Szalacha, L. A. (2013). Relationships among work stress, job satisfaction, mental health, and healthy
lifestyle behaviors in new graduate nurses attending the nurse athlete program: a call to action for nursing leaders.?Nursing
Administration Quarterly,?37(4), 278-285.
Molina, Y., Jean, C. Y., Martinez-Gutierrez, J., Reding, K. W., Joyce, P., & Rosenberg, A. R. (2014). Resilience among patients across
the cancer continuum: diverse perspectives.?Clinical Journal of Oncology Nursing,?18(1), 93.
Morse, J. M., Kent-Marvick, J., Barry, L. A., Harvey, J., Okang, E. N., Rudd, E. A., ... & Williams, M. R. (2021). Developing the resilience
framework for nursing and healthcare. Global Qualitative Nursing Research, 8, 23333936211005475.
Moss, M., Good, V. S., Gozal, D., Kleinpell, R., & Sessler, C. N. (2016). Collaborative Statement-Burnout Syndrome in Critical Care
Health-care Professionals: A Call for Action.?Chest,?150(1), 17-26.
National Council of State Boards of Nursing. (2021). NCSBN?s Environmental Scan COVID-19 and Its Impact on Nursing and
Regulation.?Journal of Nursing Regulation,?11(4), S1.
National Academies of Sciences, Engineering, and Medicine. (2021). The future of nursing 2020-2030.
North Carolina Board of Nursing. (2021, February) Strategies to Support Nursing Surge Capacity During Biological Events.
https://www.ncbon.com/myfiles/downloads/coronavirus/nursing_surge_capacity_resource_2021.pdf
North Carolina Board of Nursing. (2020a, August) Article 9A. Nursing Practice Act.
https://www.ncleg.net/enactedlegislation/statutes/html/byarticle/chapter_90/article_9a.html
NCBON. (2020b). Position Statements and Decision Trees. Retrieved December 3, 2021 from
https://www.ncbon.com/practice-position-statements-decisions-trees
NCBON.? (2020c).??Important information about COVID-19:? Temporary waivers.??Retrieved December 3, 2021 from?
https://www.ncbon.com/news-publications-statistics-important-information-about-covid-19?
NCBON.? (2020d).??Homepage.??Retrieved December 3, 2021 from?https://www.ncbon.com/
North Carolina Office of Administrative Hearings. (2022) NCAC Table of Contents. Retrieved January 3, 2022 from
https://www.ncleg.net/enactedlegislation/statutes/html/byarticle/chapter_90/article_9a.html
NC Governor Roy Cooper. (2020, March 10) Governor Cooper Declares State of Emergency To Respond To Coronavirus COVID-19.
Department of Health and Human Services Issues Recommendations to Slow Spread. Retrieved December 3, 2021 from
https://governor.nc.gov/news/governor-cooper-declares-state-emergency-respond-coronavirus-covid-19
Phillips, S. (2006). Current status of surge research.?Academic Emergency Medicine, 13, 1103- 416.
Resilience. (2020).?In Oxford English dictionary.?https://www-oed-com.ezproxy.lib.utah.edu/view/Entry/163619
Rice, V., & Liu, B. (2016). Personal resilience and coping with implications for work. Part I: a review. Work, 54(2), 325-333.
Rushton, C. H., Schoonover-Shoffner, K., & Kennedy, M. S. (2017). A collaborative state of the science initiative: Transforming
moral distress into moral resilience in nursing.?AJN The American Journal of Nursing,?117(2), S2-S6.
Schultz, C.H., & Koenig, K.L. (2006). State of research in high-consequence hospital surge capacity.?Academic Emergency Medicine,
13,?1153-1156.

22
Protect the public by regulating the practice of nursing.
Shaw, L. M., Vanderstichele, H., Knapik-Czajka, M., Clark, C. M., Aisen, P. S., Petersen, R. C., Blennow, K., Soares, H., Simon, A.,
Lewczuk, P., Dean, R., Siemers, E., Potter, W., Lee, V. M., Trojanowski, J. Q., & Alzheimer?s Disease Neuroimaging Initiative (2009).?
Cerebrospinal fluid biomarker signature in Alzheimer?s disease neuroimaging initiative subjects. Annals of Neurology, 65(4),?
403?413.?https://doi.org/10.1002/ana.21610
Stephens, T. M. (2019). Building personal resilience: Develop skills to overcome daily challenges and prepare for the future.?
American Nurse Today,?14(8), 10-16.
Stewart, D. E., Yuen, T. (2011).?A systematic review of resilience in the physically ill. Psychosomatics, 52(3),?199?209.
https://doi.org/10.1016/j.psym.2011.01.036
Thacker, K., Stavarski, D. H., Brancato, V., Flay, C., & Greenawald, D. (2016). CE: Original research: An investigation into the
health-promoting lifestyle practices of RNs.?AJN The American Journal of Nursing,?116(4), 24-30.
The Joint Commission. (2008).?The Joint Commission Accreditation Program: Hospital emergency management. Retrieved
December 6, 2021 from?www.jointcommission.org/NR/rdonlyres/DCA586BD-1915-49AD-AC6E-C88F6AEA706D/0/HAP_EM.pdf
Ungar, M. (2003). Qualitative contributions to resilience research.?Qualitative Social Work,?2(1), 85-102.
US Department of Health and Human Services (2020). Individual resilience. phe.gov. (n.d.). Retrieved December 17, 2021, from
https://www.phe.gov/Preparedness/planning/abc/Pages/individual-resilience.aspx
Wagnild, G. (2003).?Resilience and successful aging: Comparison among low and high income older adults. Journal of
Gerontological Nursing, 29(12),?42?49.?https://doi.org/10.3928/0098-9134-20031201-09
Wagnild, G., Young, H. M. (1990).?Resilience among older women. The Journal of Nursing Scholarship, 22(4),?252?255.?
https://doi.org/10.1016/j.gerinurse.2016.02.014
Walsh, C.?(2021, November 2).? Love, death, fear, guilt, pride, hope, friendship, alienation, and to much sorrow. Through it all, they
kept showing up. Harvard Gazette.? https://news.harvard.edu/gazette/story/2021/11/14-nurses-on-life-and-work-during-covid/
Ward, T., & Eisbach, S. (2013). Impaired individual resilience. In B.J. Ackley & G.B. Ladwig (Eds.), Nursing diagnosis handbook: An
evidence-based guide to planning care (10th ed., pp. 654-657). Maryland Heights, MO: Mosby Elsevier
Whitehead, P. B., Herbertson, R. K., Hamric, A. B., Epstein, E. G., & Fisher, J. M. (2015). Moral distress among healthcare
professionals: Report of an institution-wide survey.?Journal of Nursing Scholarship,?47(2), 117-125.
Webster, L., & Wocial, L. D. (2020). Ethics in a pandemic: Nurses need to engage in self-care to reduce moral distress.?American
Nurse Journal,?15(9), 18-23.
World Health Organization (WHO). (2020a).?State of the world's nursing 2020: Investing in education, jobs and leadership. Web
Annex: Nursing roles in 21st-century health systems.?World Health Organization. Retrieved December 3, 2021 from:?
https://apps.who.int/iris/handle/10665/332852
World Health Organization (WHO). (2020b).?Year of the nurse and the midwife 2020. Campaigns. Retrieved from December 3,
2021:
https://www.who.int/campaigns/annual-theme/year-of-the-nurse-and-the-midwife-2020#:~:text=The%20world%20needs%209%
20million,the%20Nurse%20and%20the%20Midwife
Wilks, S. E., Little, K. G., Gough, H. R., Spurlock, W. J. (2011).?Alzheimer?s aggression: Influences on caregiver coping and resilience.
Journal of Gerontological Social Work, 54(3),?260?275.?https://doi.org/10.1080/01634372.2010.544531

23
Protect the public by regulating the practice of nursing.
Authors: Chris E. Memering, MSN, RN, CDCES, FADCES
Laura Edwards, RN, MPA
Disclosure St at ement ? The following disclosure applies to the NCBON continuing nursing education article entitled
?North Carolina?s Guide to Diabetes Prevention and Management 2020: Resources for Nurses to Take Action.? Participants
must read the CE article, online reference documents (if applicable), and the Reflective Questions in order to earn CE
contact hours. Verification of participation will be noted by online registration. Neither the author nor members of the
planning committee have any conflicts of interest related to the content of this activity.
Provider Statem ent ? The North Carolina Board of Nursing will offer .5 contact hours for this continuing nursing
education activity.
The North Carolina Board of Nursing is approved as a provider of nursing continuing professional development by the
North Carolina Nurses Association, an accredited approver by the American Nurses Credentialing Center?s Commission on
Accreditation.
Learning Out come: Participants will gain increased knowledge of the burden and impact of diabetes in North Carolina, and
how to access tools and resources within the NC Guide to Diabetes Prevention and Management 2020.
EARN CE CREDIT
INSTRUCTIONS
Read the article, online reference documents, and the Reflective Questions (if applicable).
EARN CONTACT HOUR CERTIFICATE
Go to www.ncbon.com and scroll over ?Education?; under ?Continuing Education,? select ?Board Sponsored Bulletin
Offerings,? scroll down to link, ?North Carolina?s Guide to Diabetes Prevention and Management 2020: Resources for Nurses
to Take Action.? Register. Be sure to write down your confirmation number, complete and submit the evaluation, and print
your certificate immediately.
If you experience issues with printing your CE certificate, please email paulette@ncbon.com. In the email, provide your full
name and the title of the CE offering (North Carolina?s Guide to Diabetes Prevention and Management 2020: Resources for
Nurses to Take Action).
Registration deadline is July 1, 2024.
Many nurses work daily with people with chronic disease. In North Carolina, one of the most common
chronic diseases is diabetes. In 2020, almost one half of North Carolinians have diabetes or are at risk for
developing diabetes (CDC, 2020). The rate of diabetes in NC is 11.3%, which is a 33% increase over the last
10 years (ADA, 2020). Over a third (34.5%) of North Carolinians have prediabetes and of those, 80% are
not aware they have the condition (ADA, 2020). It is projected that over 3,000 people will die directly or
indirectly annually because of diabetes and its complications, ranking NC as seventh in the nation for
diabetes related deaths (NCHS: CDC, 2020).
This burden of chronic disease adds to the overall burden of annual health care costs in the state. The
annual healthcare costs of diabetes in NC are estimated to surpass $17 billion by 2025 (Konen & Page,
2011). These include direct and indirect costs; 72% of national diabetes costs are attributed to direct
healthcare costs, while 28% of costs are attributed to indirect healthcare costs (work-related absenteeism,
unemployment, and premature death) (ADA, 2020). Of the $11 billion of direct and indirect care costs in
NC, $7.79 billion was direct healthcare cost and $2.90 billion was indirect cost (NCDHHS, 2020). Diabetes
North Carolina's Guide to Diabetes
Prevention and Management 2020:
Resources for Nurses to Take Action
CE Article

24
Protect the public by regulating the practice of nursing.
is associated with an elevated hospital admission rate of 1.9 per 1000 with an average length of stay of
4.7 days (Powers et al., 2020). In 2018, the average cost per hospitalized person with diabetes was
$33,000 (Powers et al., 2020).
As a nurse in North Carolina, there are many areas that we can influence within our practices and
communities for the health of all. The North Carolina Diabetes Advisory Council (NC DAC), which is an
advisory group to the NC Division of Public Health, works to reduce the burden of diabetes through
coordination among the many stakeholders in diabetes prevention and control in North Carolina. The NC
DAC was created in 1984 and connects health professionals, providers, community and business leaders,
persons with diabetes, advocacy groups, coalitions, stakeholders, and partners who are all committed to
reducing the burden of diabetes in North Carolina (Diabetes NC, 2021).
The DAC?s core responsibilities (Diabetes NC, 2021) are to:
- Educate and publicly validate early detection, treatment, and self-management training for
diabetes prevention and control, as a health priority for all North Carolinians.
- Provide scientific credibility and public validity for new service priority areas and interventions
based on evolving clinical and epidemiological studies and technology.
- Foster interagency collaboration and networking for identification, utilization, and expansion of
resources for diabetes control services.
- Evaluate, present, and propose strategies for the prevention and control of diabetes in North
Carolina in terms of assessed need, estimated costs, potential benefits, and probability of success
of each strategy.
With this charge, the DAC creates a strategic plan every few years. In recent years, this strategic plan has
turned into the North Carolina Guide for Diabetes Prevention and Management. The latest of these
guides was updated and launched in 2020. The focus of the guide is to reduce NC?s diabetes burden. To
that end, the focus must be to alleviate the gap in health access/outcomes of care among different
groups of people, address health equity inclusive of strategies that address social determinants of health,
and address ?upstream? issues that contribute to health disparities and exist for our society and our most
vulnerable populations. Examples of ?upstream? factors include housing stability, neighborhood
conditions, education, food access, and income and financial security.
Figure 1: Socio-Ecological Model of Health in the North Carolina?s
Guide to Diabetes Prevention and Management 2020
[Click image to enlarge]

25
Protect the public by regulating the practice of nursing.
The NC Guide to Diabetes Prevention and Management offers a working guide for communities,
healthcare providers and insurers, employers, and advocates and policymakers. Within the guide, there
are strategies for primary, secondary, and tertiary prevention in diabetes care for each of these groups
(Institute for Work & Health, 2015). Primary prevention includes strategies for diabetes prevention,
including coordinated referrals with local Diabetes Prevention Programs (DPP). Secondary prevention
refers to once diagnosis has occurred (Type 1, Type 2, or gestational) for the prevention of complications
(ADA, 2021). For an employer, this might include creating a disease specific wellness program for those
with diabetes that provides education or resources. For the healthcare team, this includes referral and
access to diabetes self-management education and support (DSMES) services (Powers et al., 2020). This
may include collaborative practice agreements with a local DSMES service provider, if there is not one
located within your practice. Tertiary prevention includes management of complications of diabetes.
Nurses play a large role in all stages of prevention.
As a reminder, there are three primary types of diabetes: Type 1, caused by an autoimmune destruction
of ?-cells in the pancreas that produce insulin; Type 2, starting with insulin resistance progressing to a
loss of insulin secretion by ?-cells; and gestational, diagnosed during the 2nd or 3rd trimester without
underlying diabetes prior to pregnancy (ADA, 2021). Other forms of diabetes are related to other
conditions, genetic changes, or drug and chemical induced diabetes. Nursing needs to be somewhat
familiar with all types of diabetes, but especially Type 1 (5-10% of the population) and Type 2 (90-95% of
the population) and to understand the differences therein (ADA, 2021). One thing to remember is that
with advances in medical treatments and technology, people with Type 1 diabetes are living much longer
(Banion & Valentine, 2021). And with the changes to access and social determinants of health, as well as
environmental impacts, there are more youth being diagnosed with Type 2 diabetes (Vivian, 2021).
Figure 2: from the North Carolina?s Guide for Diabetes Prevention and Management 2020
[click image to enlarge]
The NC Guide to Diabetes Prevention and Management offers a refresher on prevention strategies along
the continuum of diabetes care that all healthcare providers can utilize. This includes recommendations
on lifestyle modifications including healthful eating habits, incorporation of more physical activity,
adequate sleep, maintaining a healthy weight, and living tobacco free. Resources, including mobile apps
and professional organizations, are also included in the guide as one area for nursing and others in
healthcare to help reduce the burden of living with a chronic disease. The adoption and utilization of
diabetes technology for all those affected by diabetes to better understand their disease may also be of

26
Protect the public by regulating the practice of nursing.
benefit. As such, nursing would benefit from understanding information from these devices, beyond our
standard lab values of an A1c. Diabetes prevention and management is a joint responsibility between an
individual and their healthcare team. There are many other healthcare providers who are important in
diabetes care including all nurses (LPN, RN, APRN, DNP), physicians, podiatrists,
ophthalmologists/optometrists, dentists, registered dieticians, behavioral health/mental healthcare
providers, community pharmacists, community healthcare workers, and diabetes care and education
specialists. All play a role in care and optimizing the health of individuals with diabetes.
References
American Diabetes Association. (2021). Standards of Medical Care in Diabetes ? 2021. Diabetes Care, 44(Supplement 1). DOI:
10.2337/dc21
American Diabetes Association. (2020). The Burden of Diabetes in North Carolina.
http://main.diabetes.org/dorg/docs/state-fact-sheets/ADV_2020_State_Fact_sheets_NC.pdf
Banion, C. and Valentine, V. (2021). Type 1 Diabetes Throughout the Life Span. In Cornell, S., Halstenson, C., and Miller, D.K. (Eds.),
The Art and Science of Diabetes Care and Education Desk Reference, 5th Edition (pp. 403-430). Chicago, IL: American Association
of Diabetes Educators.
Centers for Disease Control and Prevention. (2020). National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease
Control and Prevention, U.S. Department of Health and Human Services. 2020; page 10.
https://www.cdc.gov/diabetes/data/statistics-report/
Diabetes North Carolina. (2021). North Carolina Diabetes Advisory Council.
https://www.diabetesnc.com/diabetes-advisory-council/
Institute for Work & Health. (2015). What Researchers Mean by ? Primary, Secondary and Tertiary Prevention. At Work. 80.?
Retrieved at: https://www.iwh.on.ca/wrmb/primary-secondary-and-tertiary-prevention?
Konen J, Page J. (2011). The state of diabetes in North Carolina. North Carolina Journal of Medicine. 72(5): 373-378.
classic.ncmedicaljournal.com/ wp-content/uploads/2011/09/72505-web.pdf.
National Center for Health Statistics (2020). Diabetes Mortality by State.
https://www.cdc.gov/nchs/pressroom/sosmap/diabetes_mortality/diabetes.htm Accessed July 9, 2020.
North Carolina Department of Health and Human Services (NCDHHS), Division of Public Health, State Center for Health Statistics.
Data produced upon request on 10/20/2020.
Powers, M.A., Bardsley, J. K., Cypress, M., Funnell, M. M., Harms, D., Hess-Fischl, A., et al. (2020). Diabetes self-management
education and support in adults with Type 2 Diabetes: A consensus report of the American Diabetes Association, the Association
of Diabetes Care & Education Specialist, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the
American Academy of Pas, the American Association of Nurse Practitioners, and the American Pharmacists Association. The
Diabetes Educator, 46(4); 350-369. DOI: 10.1177/0145721720930959
Vivian, E.M. (2021). Type 2 Diabetes Throughout the Life Span. In Cornell, S., Halstenson, C., and Miller, D.K. (Eds.), The Art and
Science of Diabetes Care and Education Desk Reference, 5th Edition (pp. 431-450). Chicago, IL: American Association of Diabetes
Educators.
United Health Foundation. (2019). Annual Report: North Carolina Summary 2019. America?s Health Rankings, United Health
Foundation. https://www.americashealthrankings.org/explore/annual/measure/Diabetes/state/NC Accessed July 9, 2020.

27
Protect the public by regulating the practice of nursing.
Returning to school is a big decision with
significant costs and lifelong career
implications. Is this in your future plans?
Many are applying now for programs
starting in the fall. Planning ahead and
doing your homework before you hit the
classroom will help prepare you to make
the right decision.
How do you see your career progressing and what do you want to do? The answer to
these questions will impact the rest of your career. Clinical practice, education,
informatics, research, leadership, or a combination? For the purposes of this article, the
roles regulated by the North Carolina Board of Nursing (NCBON) will be reviewed.
Masters and doctoral programs are offered for the four Advanced Practice Registered
Nurses (APRNs) roles. These include: Certified Registered Nurse Anesthetists (CRNAs),
Certified Nurse Midwives (CNMs), Clinical Nurse Specialists (CNSs) and Certified Nurse
Practitioners (NPs).
APRNs are educated in one of the four roles, and in at least one of the six population foci:
family/individual across the lifespan, adult-gerontology, pediatrics, neonatal, women?s
health/gender-related or psych/mental health. The 2008 Consensus Model for APRN
Regulation (Licensure, Accreditation, Certification, & Education) was developed by the
APRN Consensus Work Group and the National Council of State Boards of Nursing APRN
Advisory Committee to provide guidance to states in developing uniformity in APRN
regulation. The model defines APRN practice and describes the APRN regulatory model.
The Consensus Model has been fully adopted by accreditation, certification, and
education bodies and by some regulatory bodies. NC law prevents full adoption of the
Consensus Model for practice. Modernization of the NC Nursing Practice Act is required
before the Consensus Model may be adopted.
When a student selects a program of study, their education will be tailored to the specific
population foci, and the national certification will match that educational preparation.
Scope of practice is defined by education, certification, and maintained competence.
Many times, practice lines are very clear. A recent position statement from NCBON for
APRN Scope of Practice may be helpful in thinking through the four APRN roles. A CNS
wouldn?t provide anesthesia and a CRNA would not provide primary care. However, for
some APRNs the lines may not be as clear and understanding those lines prior to taking
on a course of study is important.
Are you Considering
Graduate
Nursing Education?
Melanie Mabrey, DNP, ACNP-BC, BC-ADM, FAANP
APRN Consultant, NCBON
Choosing a Program of Study

28
Protect the public by regulating the practice of nursing.
References
APRN Consensus Work Group, National Council of State Boards of Nursing APRN
Advisory Committee. (2008). Consensus Model for APRN Regulation: Licensure,
Accreditation, Certification & Education. July 7, 2008.
https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_
July_2008.pdf
Gonzalez, J. & Gigli, K. (2021). Navigating population foci and implications for
nurse practitioner scope of practice. Journal for Nurse Practitioners, 17(7), 846-50.
https://doi.org/10.1016/j.nurpra.2021.04.008
Valiga, T. M. & Thornlow, D. (2018). What to consider when choosing a graduate
nursing program. Nursing2018, 48(1), 11-14.
https://doi.org/10.1097/01.nurse.0000527614.67902.8e
The first step in determining the program that is right for you involves selecting an APRN
role: CNM, CRNA, CNS, or NP. The next is determining the population foci. CNMs and
CRNAs have the population predetermined by the role. CNSs and NPs must select a
population foci. The potential adult gerontology or pediatric NP student must then also
indicate if they will be prepared in acute or primary care.
Too often nurses say, ?I am doing the FNP program so I can work anywhere.? Or students
may have been told that an FNP will be the most versatile program. It is not the case that
an FNP can work anywhere. The FNP program does provide education in primary care
across the lifespan education, but that doesn?t prepare the FNP to work in acute care. If
you know where you want to practice as an NP, look at which population foci best matches
that practice.
Once you have determined your program of study, begin looking at schools that will meet
your needs and goals. The NCBON gets regular calls from students looking for preceptors.
The NCBON does not have a list of preceptors. When choosing a school, find out if the
school provides preceptors or if it is the responsibility of the student. Also, be prepared to
travel to clinical sites. Some students have reported traveling 200 miles to their clinical site.
The travel can add significant time and costs to your program of study. Ask the school that
provides clinical sites how far you may be expected to travel. Also note, preceptors within
health systems may not be allowed to take students outside of their own program
students and/or employees. After completing your core classes (Physical Assessment,
Pharmacology, and Pathophysiology) the last thing you want to find is that you are unable
to find preceptors for your various clinical rotations.
Questions about APRN practice, please email me at mmabrey@ncbon.com.
Experience Precepted Clinical
Melanie Mabrey
DNP, ACNP-BC, BC-ADM, FAANP
APRN Consultant
30
Protect the public by regulating the practice of nursing.
In collaboration with the North Carolina Board of Nursing (NCBON), the National Council of State Boards
of Nursing (NCSBN) is assisting with the collection of data for the 2021-2022 Annual Report for
pre-licensure nursing education programs.
NCSBN Core Annual Report Project: What is it ?
The NCSBN survey was designed based on the core data results of a large, mixed-methods study of
nursing program quality indicators and warning signs.
This is the first-ever core nursing education database that has been developed.
Questions regarding COVID-19 are included to analyze its impact within your program.
The NCSBN has reported more than 20 Boards of Nursing are participating.
NCBON Annual Report
Fulfills program director responsibility for report submission consistent with 21 NCAC 36 .0323(f)(1) by
11:59 pm on October 31.
Data results will continue to be disseminated via the NCBON Trends Report.
Data results will continue to assist the Sheps Center for Health Services Research and NCSBN in
projecting the future workforce needs to be met by the nursing education programs in North Carolina.
How does this impact you?
The process of completing the Annual Report will not change. The NCBON will provide a Qualtrics
hyperlink via email granting access to the report the morning of October 1, 2022.
Access will close at 11:59 pm on October 31, 2022.
Please be on the lookout for more detailed information in the upcoming months.
NCBON Educat ion Departm ent
education@ncbon.com
(919) 782-3211, ext. 238
NCBON and NCSBN
Annual Report Collaboration
A New Opportunity!

31
Protect the public by regulating the practice of nursing.
North Carolina Board of Nursing
18th Annual Education Summit
Presenters
The North Carolina Board of Nursing is approved as a provider of?nursing
continuing professional development by the North Carolina?Nurses
Association, an accredited approver by the American?Nurses Credentialing
Center?s Commission on Accreditation.
Resilience: Who, What, When, Why, & How
Teresa M. Stephens, PhD, MSN, RN, CNE
Interim Dean, Professor of Nursing
School of Nursing
King University
The Nursing Workforce Model and Faculty Short ages
Erin P. Fraher, PhD, MPP
Director of the Program on Health Workforce?Research and Policy
University of North Carolina at Chapel Hill??
Cecil G.?Sheps?Center for Health Services Research
Next Generation NCLEX Update
Karin J. Sherrill, RN, MSN, CNE, ANEF, FAADN
Faculty Educator, Nursing Education Consultant
Event Fee: $50
Registration Ends: March 14, 2022
Register Now!
Contact Hours will be awarded.
March 28, 2022
Virtual Event
8:30 am ? 12:45 pm EST

32
Protect the public by regulating the practice of nursing.
The Hospice and Home Care Foundation of North
Carolina, affiliated with the Association for Home
and Hospice Care of North Carolina, is in the third
year of a 3-year grant funded project to: Address
the Serious Shortage of RNs in Home Health and
Hospice. Funded by the State Employees Credit
Union Foundation and the Golden LEAF
Foundation, key project components include
developing and piloting a clinical rotation model
to provide ?real life? exposure to home health and
hospice care; and developing and piloting an
on-boarding model to enable home health and
hospice agencies to successfully integrate newly
graduated/licensed RNs into their organizations.
Models were developed with input from key
stakeholders, including the NC Board of Nursing.
Seven pilot partnerships comprised of a nurse
education program and one or more home
health/hospice agencies are participating
including: 1) Surry Community College, Mountain
Valley Hospice and Palliative Care, and Yadkin
Valley Home Health/Rehab Services; 2)
Appalachian State University and Trellis
Supportive Care; 3) East Carolina University and
3HC Home Health and Hospice Care; 4) Cape Fear
Community College and Lower Cape Fear
LifeCare; 5) UNC-Pembroke and HealthKeeperz; 6)
Gardner-Webb University and Hospice of
Cleveland County; and 7) UNC-Chapel Hill and
Transitions LifeCare.
The clinical rotation model developed is
structured in an 11-clinical day, chart format,
Susan L. Harmuth, MS and Kathy B. Turner, RN, BSN
including daily objectives, content to be covered,
preceptor guide, etc. The model can be adapted for
shorter rotation frameworks. On-boarding model
content is broken into phases based on the new
nurse?s readiness and it is expected to take up to
one year to successfully integrate newly graduated
RNs into home health and hospice work.
In spite of challenges resulting from COVID-19,
through summer of 2021, a total of 80 nursing
students participated in the full clinical rotation
model and 161 participated in shorter ?mini?
rotations. Seven newly graduated RNs were
employed by home health/hospice pilot project
agencies. Overall feedback from students,
preceptors, faculty, and agencies has been very
positive. The models will be available to interested
nurse education programs and home
health/hospice agencies beginning April/May 2022.
The Association for Home and Hospice Care of
North Carolina will assume on-going program
efforts after the conclusion of the pilot project.
To provide a sense of project impacts thus far,
below are several quotes from pilot project
participants.
??this opportunity has been amazing. We have
been able to showcase all the wonderful things a
career in home health has to offer. We have hired
one LPN to RN graduate that participated in the
program, and she has thrived in her roll. She has
been elevated to a lead position in record time
because of the preparation she had coming into
Hospice and Home Care Foundation Grant
to Address the Serious Shortage
of RNs in Home Health and Hospice Agencies
Update

33
Protect the public by regulating the practice of nursing.
this position. We have recently hired another RN
that is currently training and exceeding
expectations daily??
Lauren Ledford, MBA, Executive Director, Yadkin
Valley Home Health/Rehab Services
?This collaboration has provided opportunities for
our students to be involved in all aspects of home
health and hospice care in various courses
throughout the curriculum, which has opened
their eyes to the care and career opportunities
within that.?New educational tools have been
introduced into the curriculum, such as ELNEC
modules, in addition to the clinical experiences
facilitated by our partnership. It has also given
way to opportunities within the department of
nursing, specifically in the simulation setting, in
order to better prepare our students and engage in
meaningful dialogue related to the unique care
that takes place in the home health and hospice
setting..."
Kristen Morgan, MSN, RN, CNE ? Clinical Course
Coordinator, Appalachian State University; Whitney
Hicks MSN, RN, BMTCN -Clinical Instructor,
Appalachian State University
?... I feel sentimental toward my experience in
home health. It gave me new perspective of the
community we serve here in ENC; it is a perspective
that you cannot gain in the hospital alone. The
privilege to enter the homes of patients painted
vivid detail of many social determinants that have
made health an impossible dream, an
unattainable goal. The intimacy of home visits
provides a nurse-patient relationship very different
from the hospital setting. You see the whole
person, not merely a patient in a hospital bed, but
the surrounding environment that shapes the
person they have come to be??
ECU Student Participant -Excerpt from Student
Journal Entry
Board Member Nominations
Now Open
Open Positions for 2022 Election:
- RN - Staff Nurse
- RN - ADN/ Diploma Nurse
Educator
- Licensed Practical Nurse
See Pages 8-9 for more information and
Nomination Form
As a licensed nurse in NC, it
is your responsibility to keep
the NCBON updated on your
contact information to
ensure that you can be
reached in a timely manner.
Having a current, valid email
address on file with the
NCBON will facilitate
communications.
Important Info!
If you have recently changed employers or are
recently licensed after graduation from nursing
school, update your email address. Changes can be
made easily by logging into the NC Board of Nursing
Gateway at www.ncbon.com
21 NCAC 36 .0208
(b) In the event of an address, email, or telephone change, the
licensee shall submit the change online on the Board's website
at www.ncbon.com within 30 calendar days of the change.

34
Protect the public by regulating the practice of nursing.

35
Protect the public by regulating the practice of nursing.
Joyce Winstead, MSN, RN, FRE - Director, Practice
Nurses practice in complex healthcare systems that are constantly evolving and changing to meet the
growing healthcare needs of the public. To maintain professional competency in the ever changing
healthcare systems, nurses must acquire new nursing practice knowledge and skills on an ongoing basis
throughout their careers. As healthcare systems continue to evolve and nurses acquire new practice
knowledge, skills, and responsibilities questions often arise regarding whether a specific procedure or
activity would be within the legal scope of practice for the registered nurse (RN) or licensed practical nurse
(LPN).
Enacted in 1903, the North Carolina (NC) Nursing Practice Act (NPA), General Statute (GS) 90-171.20,
legislates the Board of Nursing (NCBON) the authority to regulate nursing practice in NC. The NPA is
promulgated in the NC Administrative Code (Rules). The General Statue mandates the protection of the
public. For this reason, the mission of the NCBON is to protect the public by regulating the practice of
nursing.
The NPA and Rules define the legal scope of practice for the nurse, both RN and LPN. The NPA GS
90-171.20 (7) defines the RN scope. Section(8) of GS 90-171.20 defines the LPN scope. Both the RN and
LPN scope of practice are further defined in Administrative Rules 21 NCAC 36.0224 for RNs and 21 NCAC
36.0225 for LPNs. Provided below is a comparison table that list the scope of practice components for the
RN and LPN. The term ?participating? is central for the LPN scope of practice. Participating is defined in
Practice Corner
RN
Component s of Scope of Pract ice
LPN
Component s of Scope of Pract ice
Accepting Responsibilities/Assignments Accepting Responsibilities/Assignments
Assessment Participate in Assessment
Planning Participate in Planning
Implementation Participate in Implementation
Evaluation Participate in Evaluation
Reporting and Recording Reporting and Recording
Collaboration Participate in Collaboration
Teaching and Client Counseling Participate in Client Teaching and Counseling
Managing Nursing Not within LPN Scope of Practice
Administration of Nursing Services Not within LPN Scope of Practice
Accepting Responsibility for Nursing Actions Accepting Responsibility for Nursing Actions
Scope of Practice Decision Tree for the RN and LPN
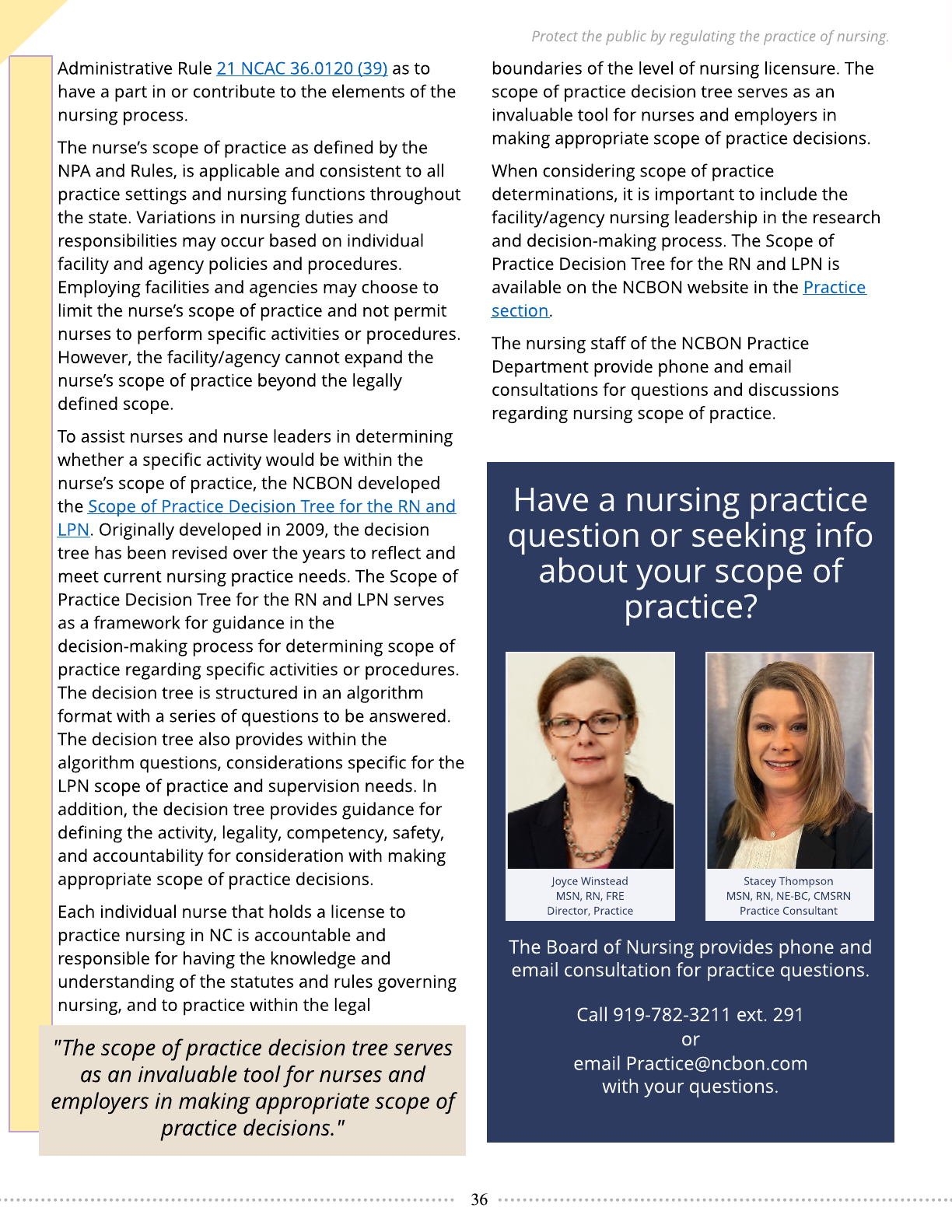
36
Protect the public by regulating the practice of nursing.
Administrative Rule 21 NCAC 36.0120 (39) as to
have a part in or contribute to the elements of the
nursing process.
The nurse?s scope of practice as defined by the
NPA and Rules, is applicable and consistent to all
practice settings and nursing functions throughout
the state. Variations in nursing duties and
responsibilities may occur based on individual
facility and agency policies and procedures.
Employing facilities and agencies may choose to
limit the nurse?s scope of practice and not permit
nurses to perform specific activities or procedures.
However, the facility/agency cannot expand the
nurse?s scope of practice beyond the legally
defined scope.
To assist nurses and nurse leaders in determining
whether a specific activity would be within the
nurse?s scope of practice, the NCBON developed
the Scope of Practice Decision Tree for the RN and
LPN. Originally developed in 2009, the decision
tree has been revised over the years to reflect and
meet current nursing practice needs. The Scope of
Practice Decision Tree for the RN and LPN serves
as a framework for guidance in the
decision-making process for determining scope of
practice regarding specific activities or procedures.
The decision tree is structured in an algorithm
format with a series of questions to be answered.
The decision tree also provides within the
algorithm questions, considerations specific for the
LPN scope of practice and supervision needs. In
addition, the decision tree provides guidance for
defining the activity, legality, competency, safety,
and accountability for consideration with making
appropriate scope of practice decisions.
Each individual nurse that holds a license to
practice nursing in NC is accountable and
responsible for having the knowledge and
understanding of the statutes and rules governing
nursing, and to practice within the legal
"The scope of practice decision tree serves
as an invaluable tool for nurses and
employers in making appropriate scope of
practice decisions."
boundaries of the level of nursing licensure. The
scope of practice decision tree serves as an
invaluable tool for nurses and employers in
making appropriate scope of practice decisions.
When considering scope of practice
determinations, it is important to include the
facility/agency nursing leadership in the research
and decision-making process. The Scope of
Practice Decision Tree for the RN and LPN is
available on the NCBON website in the Practice
section.
The nursing staff of the NCBON Practice
Department provide phone and email
consultations for questions and discussions
regarding nursing scope of practice.
Joyce Winstead
MSN, RN, FRE
Director, Practice
Stacey Thompson
MSN, RN, NE-BC, CMSRN
Practice Consultant
Have a nursing practice
question or seeking info
about your scope of
practice?
The Board of Nursing provides phone and
email consultation for practice questions.
Call 919-782-3211 ext. 291
or
email Practice@ncbon.com
with your questions.

37
Protect the public by regulating the practice of nursing.
TO ACCESS ONLINE CE ARTICLES, SESSION REGISTRATION, AND THE PRESENTATION REQUEST FORM,
GO TO WWW.NCBON.COM AND LOOK FOR CONTINUING EDUCATION OFFERINGS.
QUESTIONS? EMAIL PAULETTE@NCBON.COM
Resilience: A Key to Safe Nursing Practice (1.5 CH)
North Carolina?s Guide to Diabetes Prevention and Management 2020: Resources for Nurses to Take
Action (.5 CH)
Negligent Nursing Practice: What You Need to Know (1 CH)
Patient Care and Documentation: The Balancing Act (1 CH)
Nursing Regulatory Agencies and Advocacy Organizations: What is the Difference? (1 CH)
For more articles, click here or follow instructions above.
CE Opportunities 2022
The 2022 sessions are listed below as follows:
March 22 - Virt ual
April 26 - Virtual
Septem ber 13 - Format to be Announced
October 4 - Format to be Announced
$40.00 fee (non-refundable) (Note: You will be notified of any date or format changes.)
Register online at www.ncbon.com. Registration at least two weeks in advance of a scheduled
session is required. Seating is limited.
If you are unable to attend and do not have a substitute to go in your place, please provide this
information via email to Paulette@ncbon.com so someone on the waiting list can attend.
Learn about the functions of the Board of Nursing
and how these functions impact the roles of the
nurse administrators and the mid-level nurse
managers in all types of nursing services. (4.5 CHs).
Orientation Session for
Administrators of Nursing Services
and Mid-Level Nurse Managers
Online Bulletin Articles

38
Protect the public by regulating the practice of nursing.
Legal Scope of Pract ice Online Course (1.5 CH)
The purpose of this offering is to provide information and clarification of the components of the legal
scope of practice for licensed nurses (RN and LPN) practicing in North Carolina.
Just Culture in Nursing Regulation Booklet (1.0 CH)
The booklet provides an introduction to the basic principles of Just Culture and the use of these
concepts in evaluating the reportability of untoward events to the Board using the NCBON Complaint
Evaluation Tool (CET).
NCBON Practice Consultants are available upon request to
provide continuing education presentations regarding
nursing practice. To request a Practice Consultant, please
complete the Presentation Request Form online and submit
it per form instructions. The NCBON will contact you to
arrange a presentation. A minimum of 25 - 30 licensed
nurses (APRN, RN or LPN) are required for presentations.
NCBON Practice Consultant
Presentation
Standard Presentat ion Offerings
Continuing Competence (1 CH) - 1 hour ? Presentation is for all nurses with an active license in NC
and is an overview of continuing competency requirements.
Legal Scope of Pract ice (2 CHs) - 2 hours ? Defines and contrasts each component of the RN and
LPN scope of practice including nursing accountability for delegation of tasks to unlicensed assistive
personnel. Potential violations are discussed.
Delegation: Responsibility of the Nurse (1 CH) - 1 hour ? Provides information about delegation
that would enhance the nurse?s knowledge, skills, and application of delegation principles to ensure
the provision of safe competent nursing care. Discussion includes the role and responsibilities of the
nurse for delegation to unlicensed assistive personnel.
Understanding the Scope of Practice and Role of the LPN (1 CH) - 1 hour ? Assists RNs, LPNs, and
employers of nurses in understanding the LPN scope of practice.
Nursing Regulat ion in NC (1 CH) - 1 hour ? Describes an overview of the NC Board of Nursing
authority, composition, vision, function, activities, strategic initiatives, and resources.
Int roduct ion to Just Cult ure and NCBON Complaint Evaluation Tool (1.5 CHs) - 1.5 hours ?
Provides information about Just Culture concepts, role of nursing regulation in practice errors,
instructions in use of NCBON CET, consultation with NCBON about practice errors, and mandatory
reporting. Suggested audience is nursing leadership: director, administrator, manager, supervisor,
etc.
Int roduct ion to the NCBON Complaint Evaluation Tool (1 CH) - 1 hour ? Provides brief
information about Just Culture concepts and instructions for use of the NC Board of Nursing?s
Complaint Evaluation Tool, consultation with the NCBON, consultation with NCBON about practice
errors and mandatory reporting. Suggested for leadership familiar and unfamiliar with Just Culture.
Available Online

39
Protect the public by regulating the practice of nursing.
The licensure department is home to Licensure by Examination and
Endorsements, APRN privilege to practice, NAII listing,
Licensure/listings renewal/reinstatement and criminal background
checks. Each month we process over 3,000 new applications and over
6,000 renewal applications.
For your convenience, all our applications are online and easily
accessible via our website. By navigating to our homepage,
www.ncbon.com, on the far-left side of the screen, there is a ?I want to? ? drop down. Select your
area of interest and proceed. The website was developed with you in mind. Due to the high volume
of calls, it?s not always feasible to immediately speak with a member of the Licensure team. We
process applications in the order they are received. Additionally, you can always log into your
Gateway account and check the status of your application. The information in your Gateway is
?real-time?.
North Carolina is a member of the National Licensure Compact (NLC). If you are applying for
licensure in NC with an NC address you will be issued a multi-state licensure if you meet the
eligibility requirements. Temporary licenses are available to qualified endorsement applicants
from non-compact states. The temporary license is a non-renewable, once in a lifet ime, license
issued for a period not to exceed six months.
Multi-state licenses will not be issued to applicants with an out of state address. If an applicant
wishes to obtain multi-state licensure, you must provide evidence NC is your primary state of
residence along with a written request for the status change. We recommend signing up for Nursys
e-notify for free notifications and alerts to changes in your licensure status to include upcoming
expiration dates.
NCBON?s list of Frequently Asked Questions may address many questions.
Receive email alerts for changes in your license
and expiration dates.
Sign up for Nursys e-Notify.
Licensure Corner
Tony Graham, MS, CPM
Chief Operations Officer

40
Protect the public by regulating the practice of nursing.
Accessing NCBON Disciplinary Actions
The mission of the NCBON is to protect the public by regulating the practice of nursing.
When the NCBON takes disciplinary action, the information is readily accessible on the
NCBON website. In addition, the NCBON reports disciplinary actions to NURSYS®, National
Practitioner Data Bank (NPDB), and Office of the Inspector General (OIG).
The NCBON?s electronic database serves as the primary source for licensure verification
for Registered Nurses, Licensed Practical Nurses, Advanced Practice Registered Nurses,
and Nurse Aide IIs in NC. To conduct a license verification, click here.
Looking for Disciplinary Actions?
To review the continuously
updated list of nurses who have
received disciplinary action, go to
www.ncbon.com, click on
?Discipline and Compliance,? and
then ?Discipline Actions Log? (click
red box). The Discipline Action Log
will automatically list the last 100
disciplinary actions.
If there is a specific nurse or
time frame you would like to
search, enter the information in
the search section at the top of
the webpage. The publicly
available documents associated
with a nurse who has had
disciplinary action are uploaded
to the website.

41
Protect the public by regulating the practice of nursing.
?The brick walls are there for a reason. The brick walls are not there to keep us
out. The brick walls are there to give us a chance to show how badly we want
something. Because the brick walls are there to stop the people who don?t want it
badly enough. They?re there to stop the other people.?
Randy Pausch
The Last Lecture
The next issue of
will be released in late June 2022.
What to expect...
- Slate of Candidates
- Names and Faces
- Biographies
- Voting Information
- Fresh CE Opportunities
Reflect ion on "Resilience"
After learning of his terminal pancreatic cancer, Randy Paucsh, an American educator, a professor
of computer science, human?computer interaction, and design at Carnegie Mellon University
(CMU) in Pittsburgh, Pennsylvania, gave an upbeat lecture in which resilience was a common
theme.
Dr. Terry Ward's article, "Resilience: A Key to Safe Nursing Practice", echos the above sentiment
and guides nurses on how to apply resilience to their daily lives.

