
2022
Health Worker Recruitment and Retention in New York City:
What Are the Issues? What Are the Strategies?

Health Worker Recruitment and Retention in New York City:
What Are the Issues? What Are the Strategies?
December 2022
Center for Health Workforce Studies
School of Public Health, University at Albany
State University of New York
1 University Place, Suite 220
Rensselaer, NY 12144-3445
Phone: (518) 402-0250
Web: www.chwsny.org
Email: [email protected]
Center for Health Workforce Studies
TABLE OF CONTENTS
INTRODUCTION........................................................................................................................................................ 1
METHODS ................................................................................................................................................................. 1
Primary Data Sources ................................................................................................................................ 2
Secondary Data Sources............................................................................................................................ 3
Data Analysis............................................................................................................................................... 4
FINDINGS .................................................................................................................................................................. 4
Recruitment and Retention Challenges................................................................................................... 4
Strategies Used to Address Recruitment and Retention Diculties ................................................... 7
NYC Health Workforce Trends.................................................................................................................. 9
Registered Nursing Education in NYC: Preliminary Findings ..............................................................13
LIMITATIONS...........................................................................................................................................................13
DISCUSSION............................................................................................................................................................14
CONCLUSIONS .......................................................................................................................................................16
REFERENCES ...........................................................................................................................................................17
BEST PRACTICES FROM THE FIELD
The New Jewish Home Geriatrics Career Development Program ..................................................................... 6
NYC Health + Hospitals Nursing Residency Program.......................................................................................... 7
FutureReadyNYC...................................................................................................................................................... 8
Jamaica Hospital Student Nurse Summer Externship Program ........................................................................ 9
AHRC Retention Support Coordinator ...............................................................................................................10
TABLES AND FIGURES
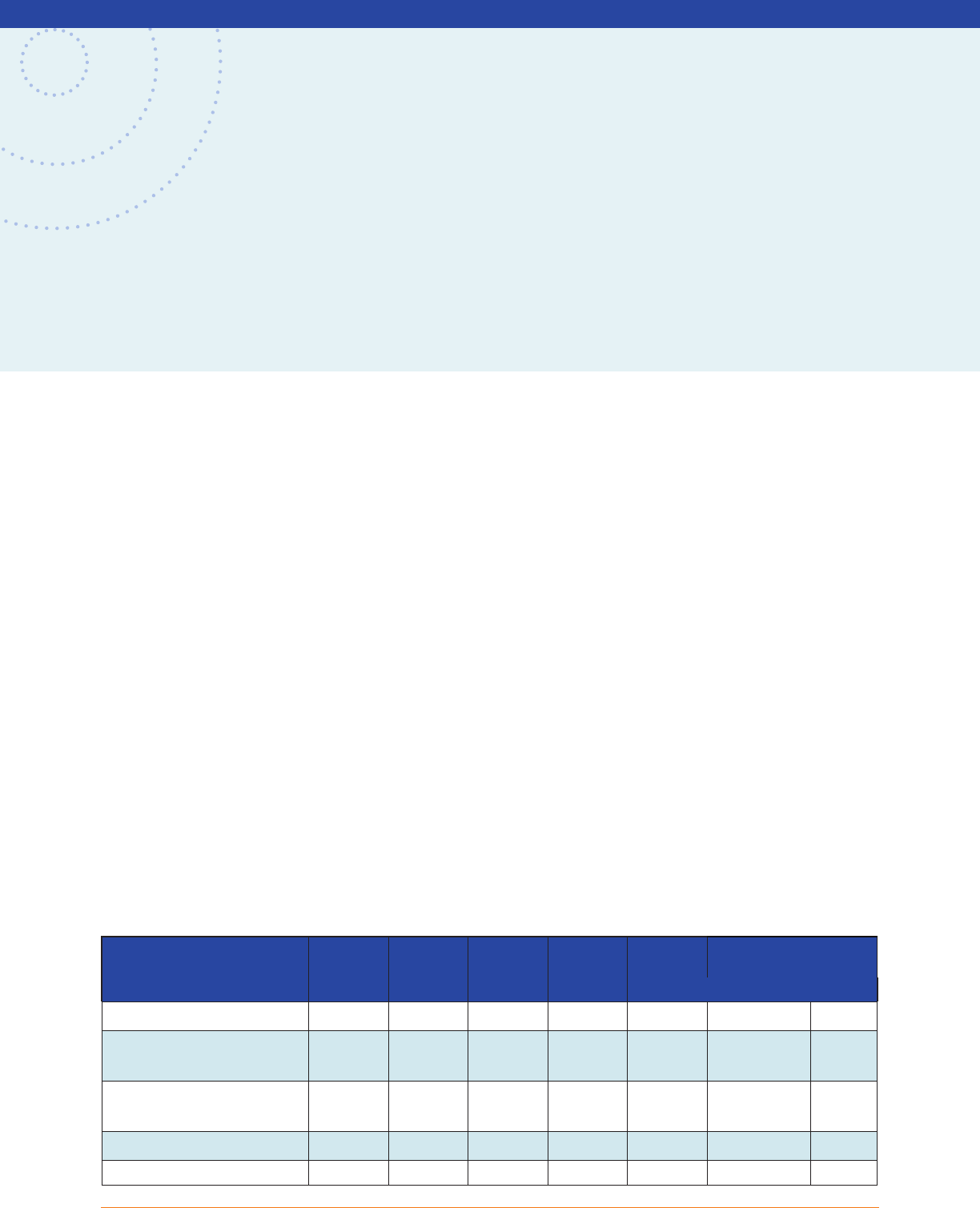
TABLE 1. Health Care Occupations with Recruitment and Retention Diculties in NYC by Setting ............. 5
FIGURE 1. Employment Growth in NYC, 2000-2021 (Standardized to 2000).................................................... 8
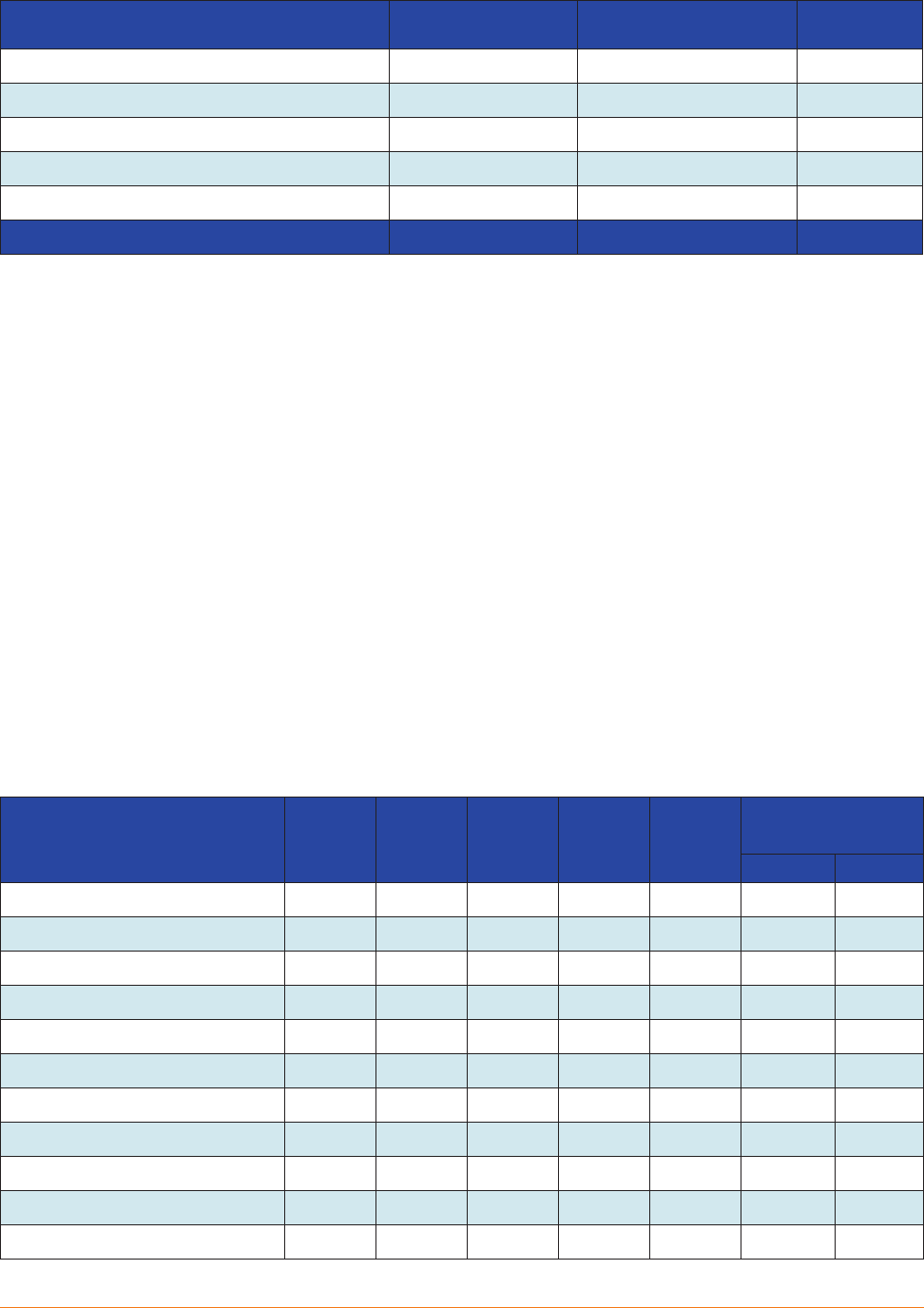
TABLE 2. Health Care Sector Employment in the New York City Region, by Setting, 2016-2020................... 9
TABLE 3. Employment Projections for NYC for Selected Occupations, 2018-2028 .......................................10
TABLE 4. Employment Projections for NYC by Setting, 2018-2028..................................................................11
TABLE 5. Count of RNs by License Address ........................................................................................................11
TABLE 6. The RN Workforce in NYC by Location of Residence and Work Setting..........................................12
TABLE 7. Number of Graduations in Selected Health Professions Education Programs in NYC,
2017-2021 ...............................................................................................................................................................12
ii

Health Worker Recruitment and Retention in New York City
INTRODUCTION
The health workforce is a vital component of New York State’s health care delivery system. Eorts to
expand access to care, improve the quality of care, or address health disparities depend on the availability
of a diverse, well-trained, and adequately sized health workforce. Many states, including New York State
(NYS), face the ongoing challenge of health worker maldistribution. For instance, while the overall supply
of health workers appears to be adequate, these workers are not evenly distributed, resulting in areas that
are underserved. Chronic workforce shortages in primary care, oral health, and behavioral health have
persisted in many rural and inner-city communities of the state. Currently, nearly 30% of New Yorkers
reside in federally designated Health Professional Shortage Areas (HPSAs), with many of these shortage
areas located in New York City (NYC).
1
The COVID-19 pandemic has had substantial impacts on the state’s health care delivery system as well as
on its health workforce. Initially, in response to surging COVID-19 cases, NYS used an array of strategies,
sometimes using executive orders to build workforce surge capacity, to make better use of the available
health workforce and to facilitate licensing health professionals from other states. In addition, health
professions education programs faced pandemic-related disruptions that jeopardized their students’ ability
to meet educational program requirements. More recently, health care providers report growing diculty
recruiting and retaining patient-care sta in all health care settings, including acute care, ambulatory care,
long-term care, and home health care.
The Center for Health Workforce Studies (CHWS) is a research center based at the University at Albany
School of Public Health. Established in 1996, the mission of CHWS is to provide timely, accurate data and
conduct policy-relevant research on the health workforce to support health workforce planning and poli-
cymaking. CHWS monitors NYS’s health workforce and has studied long-standing workforce recruitment
and retention challenges reported by the state’s health care providers.
METHODS
CHWS, in collaboration with City University of New York (CUNY) and with support from 1199 SEIU League
Training and Upgrading Fund, conducted a study to identify the workforce issues that health care providers
face in the greater NYC area (the 5 boroughs of NYC, plus Long Island and the lower Hudson Valley), including
the factors contributing to recruitment and retention challenges, COVID-19 impacts, and the strategies
used to address these challenges.
Research questions included:
● What health professions/occupations are the most dicult for NYC healthcare providers to
recruit and why?
● What health professions/occupations are the most dicult for NYC health care providers to
retain and why?
1

Center for Health Workforce Studies
● Do recruitment and retention diculties vary by provider type?
● What strategies are health care providers using to recruit and retain needed workers?
● What are recent trends in the deployment of and demand for health workers in NYC?
● What impacts has the COVID-19 pandemic had on the health professions educational pipeline,
particularly registered nursing, in relation to admissions, graduations, capacity constraints,
transition to practice, and demand for new graduates?
The study used a mixed-methods approach to assess health workforce recruitment and retention issues
currently experienced by NYC health care providers, to understand the ways in which the COVID-19 pandemic
has contributed to these issues, and to identify strategies used by providers to attract and retain workers.
Primary Data Sources
Key Informant Interviews
Semi-structured key informant interviews were conducted from May-August 2022 with approximately 15
human resources (HR) sta and Chief Learning Ocers from hospitals and hospital systems, including
safety net hospitals, academic medical centers, and community hospitals; long-term care facilities; home
health care agencies; and ambulatory care providers, including federally qualied health centers (FQHCs)
in the greater NYC area. Interview participants were selected through a convenience sample, with atten-
tion paid to location, organizational size, and sponsorship. Additionally, group interviews were held from
April-June 2022 with Chief Nursing Ocers from NYC health care organizations and in August 2022 with
HR sta from FQHCs.
Interviewees were asked about current recruitment and retention challenges; contributing factors, including
pandemic impacts; and potential strategies used to address these diculties. A team of 3-4 researchers
convened Zoom interviews, which lasted 30-45 minutes on average. Prior to the scheduled interview, a list
of questions was sent to participants that included:
● What professions/occupations are hardest to recruit?
● What professions/occupations are hardest to retain?
● What are the most common reasons for diculty in recruitment/retention?
● What strategies are used address stang challenges?
● How are gaps in transition to practice (preparation/readiness of new sta) being addressed?
● Are there any strategies in place to bolster training pipelines?
Health Care Employer Demand Surveys
Since 2000, CHWS has been surveying health care providers across NYS annually to learn more about their
recruitment and retention challenges and to determine whether there is variation by setting (hospitals,
long-term care, home care, and ambulatory care) and/or by geography. This data source supported a trend
2
Health Worker Recruitment and Retention in New York City
analysis to determine whether recruitment and retention issues have changed over time, including a better
understanding of COVID-19 impacts on attracting and retaining health workers. The employer-demand
survey ndings for nursing homes, long-term facilities, and home health care agencies were based on
surveys conducted in 2022. The employer-demand survey ndings for hospitals and FQHCs were based
on surveys conducted in 2021. The most recent report of ndings from health care employer-demand
surveys can be found at: https://www.chwsny.org/wp-content/uploads/2021/12/CHWS_RR_InfoGraphic_
Final_Updated-1-24-22.pdf and at https://www.chwsny.org/wp-content/uploads/2022/02/CHWS_FQHC_
RR_InfoGraphic_Final.pdf.
Survey of Nursing Deans of RN Education Programs in NYS
For over 20 years, CHWS has conducted an annual survey of the deans of NYS’s registered nurse (RN)
education programs. The survey asks about nursing program applications, admissions, and graduations as
well as the deans’ assessment of the local job market, barriers to expanding program capacity, and more
recently, COVID-19 impacts on their programs. The survey was conducted in the spring and summer of
2022, and it included separate surveys for associate degree RN programs and baccalaureate degree RN
programs. An analysis of data from this source was used to assess the RN educational pipeline in NYC,
including COVID-19 impacts. The most recent report based on ndings from this survey can be found at:
https://www.chwsny.org/wp-content/uploads/2022/08/NURSING-ED-REPORT-NY-UT-2022.pdf
Secondary Data Sources
The Integrated Postsecondary Data System
The Integrated Postsecondary Data System (IPEDS) is a compilation of surveys conducted annually by
the US Department of Education, National Center for Education Statistics. IPEDS includes information on
institutional characteristics, student nancial aid, faculty, and graduations by award level and by program
for educational programs from every college, university, and technical and/or vocational institution that
participates in the federal student-nancial-aid program. Data analyzed include nal data from academic
years 2016-2017 through 2019-2020 and provisional data from the 2020-2021 academic year. Data from
IPEDS were used in this study to assess trends in graduations from health professions education programs
in NYC.
The American Community Survey
The American Community Survey (ACS) is conducted each year by the US Census Bureau and is used to
provide population estimates by a variety of indicators, including age, gender, race and ethnicity, educa-
tional level, occupation, occupational setting, income, and socioeconomic status. The 5-year estimates can
be broken down by various geographic levels, including state, county, subcounty, census tract, and census
block. ACS data were used to develop estimates of RN employment in NYC. Data from the 2015-2019 5-year
estimates were used for the analysis.
3

Center for Health Workforce Studies
NYS Department of Labor employment data and 10-year projections
The NYS Department of Labor (NYSDOL) Quarterly Census of Employment and Wages (QWEC) data were
used to count the number of jobs in in health care by setting for the years 2017-2021 by NYSDOL region.
Additionally, NYSDOL developed regional projections for the 2018-2028 period by both occupation and
setting and the projections include counts of both newly created positions and annual job openings that
are a result of worker departures (retirements, job changes, departures from the eld). These data were
used to assess NYC health workforce employment trends over a 10-year period.
NYS Education Department RN licensure data
Licensure data from the NYS Education Department (NYSED) for the years 2018-2022 were used to count
the number of licensed RNs in NYC. NYSED uses licensees’ addresses to determine the county of residence.
The 5 boroughs of NYC were aggregated to obtain a regional total.
Data Analysis
All analyses were NYC-focused. IPEDS data were used to assess trends in graduations from health profes-
sions education programs. ACS data were used to estimate the number of RNs employed in health care
settings regardless of where they lived. NYSDOL employment data were used to report the number of health
care jobs in NYC. NYSDOL projections were used to identify the professions and occupations projected
to be in greatest demand over the 10-year period. NYSED licensure data were used to assess trends in
licensed RNs by geography.
The University at Albany Institutional Review Board (IRB) conducted a review of the interview protocols and
the proposed secondary data analysis and determined that the research was not human subjects research
and did not require an IRB application.
FINDINGS
Recruitment and Retention Challenges
Nurse leaders and HR sta from health care providers in all settings identied RNs as one of the occupations
most dicult to recruit and retain (Table 1). They also reported that licensed practical nurses (LPNs) were
also among the most dicult to recruit. HR sta from hospitals reported that clinical laboratory techni-
cians and technologists; MRI, ultrasound, and surgical technicians; respiratory therapists; and radiologic
technicians were also dicult to recruit and retain. HR sta from hospitals, home health care agencies, and
ambulatory care indicated that physicians, social workers, medical assistants, and clerical sta were dicult
to recruit and retain. HR sta from long-term care providers and home health care agencies reported that
home health aides were dicult to recruit and retain.
4

Health Worker Recruitment and Retention in New York City
TABLE 1. Health Care Occupations with Recruitment and Retention Diculties in NYC by Setting
Setting Most Dicult to Recruit and Retain
Hospitals Behavioral health providers
Clinical laboratory technicians
Clinical laboratory technologists
Licensed practical nurses (recruitment only)
MRI, ultrasound, and radiologic technicians
Nurse practitioners
Registered nurses
Respiratory therapists
Social workers
Surgical technicians
Long-Term Care Providers Certied nurse aides
Clerical sta
Home health aides
Licensed practical nurses
Nursing directors and managers
Registered nurses
Home Health Care Home health aides
Licensed practical nurses
Nurse practitioners
Personal care aides
Registered nurses
Social workers
Ambulatory Care Providers Clerical sta
Licensed practical nurses
Medical assistants
Nurse practitioners
Obstetricians/gynecologists
Primary care physicians
Psychiatrists
Registered nurses
Social workers
Support sta
Reasons for Recruitment and Retention Diculties
Health workforce recruitment was problematic for providers prior to the pandemic. However, the COVID-19
pandemic exacerbated health workforce shortages in NYC, dramatically increasing the number of occupa-
tions in short supply as well as the magnitude of the shortages. Some of the occupations in short supply
have been problematic for many years, even prior to the pandemic. Some are newer, eg, the recruitment
diculties of LPNs reported by hospitals. Key informant interviewees in hospitals indicated they added
more LPN positions due to the diculties recruiting and retaining RNs.
5

Center for Health Workforce Studies
The New Jewish Home Geriatrics Career Development Program
The New Jewish Home Geriatrics Career Development (GCD)
is a workforce development training program for under-
served young people. GCD bridges the gap between geri-
GCD currently partners with 10 under-resourced New York
City public high schools to serve students in grades 10-12
through a 3-year after-school or out-of-school program. GCD
BEST PRACTICES FROM THE FIELD
atric care job opportunities and underserved young people.
GCD provides hands-on experience, paid internships, job
training, and courses in healthcare certications aligned with
the needs of the industry.
Each year GCD serves approximately 275 participants ages
14-24 across 2 programs at no cost to the participants.
also trains young adults ages 18-24 who are disconnected
from education and employment through a 3-month full-
time skill development program that includes human devel-
opment, social support, foundational professional training,
healthcare career orientation, skills training for certication,
and connection to employment. There have been nearly
1,000 graduates since 2006.
Key informants generally agreed that a critical factor contributing to recruitment problems was that demand
for workers outstripped supply. As a result, there was great competition for available workers. Many
informants noted that many social-service agencies, retail stores, and fast-food restaurants are in direct
competition for the same entry-level workers. Key informants also indicated that noncompetitive salaries
contributed to the problem. An example cited frequently was that RNs were often drawn to travel or agency
nurse positions that paid much higher wages than NYC health care providers could oer them. This trend
extends beyond NYC.
2
NYC respondents to the employer-demand survey also agreed that a general shortage of workers and
noncompetitive salaries were key reasons for recruitment diculties. Long-term care respondents to the
survey also indicated that refusal to obtain a COVID-19 vaccine or booster also contributed to recruitment
and retention diculties. Home care respondents to the survey indicated that a lack of exible scheduling
and transportation challenges also contributed to recruitment diculties in home care agencies in NYC.
Most key informants noted a generational shift among prospective job candidates, indicating that younger
applicants were much more concerned with work-life balance and the need for organizational support for
worker resilience to address burnout. These younger workers seemed less mission-driven and more likely
to create boundaries that better separate work and personal life through behaviors such as “quiet quitting.”
3
These applicants were much more likely to want exible hours and, in some instances, the opportunity to
work remotely. Additionally, key informants across settings reported an increasing amount of “ghosting”
by prospective new hires who accepted jobs but never began employment. They also described new hires
who began employment but only stayed long enough to obtain the necessary experience to get a higher
paying job, often in a dierent setting.
Key informants as well as respondents to the employer-demand survey indicated that the retention of
health care workers by providers in NYC worsened during the pandemic. They attributed retention dicul-
ties to a variety of factors. Many workers experienced stressful working conditions (extremely ill patients
6

Health Worker Recruitment and Retention in New York City
BEST PRACTICES FROM THE FIELD
NYC Health + Hospitals Nursing Residency Program
NYC Health + Hospitals implemented a 12-month nurse
residency program in 2019 using evidence-based Vizient/
AACN curriculum for newly hired registered nurses (RNs)
The benets of the program include increasing retention
rates for the participating RNs who learn strategies for deliv-
ering patient care. The RNs participate in group seminars on
with less than 1 year experience or RNs who are new to their
decision-making, conict-resolution, end-of life care, health-
specialty. The sessions occur once a month over a 12-month
care quality, and patient safety, among other topics. RNs
period. The program starts at time of hire and is designed
participating in the program develop and present a poster
to build condence, build relationships, and develop leader-
on an evidenced-based practice topic that improves the
ship skills through shared learning and mentoring.
quality of patient care
and stang shortages) that resulted in attrition, often from patient-care positions. Many older workers
retired. Some workers who left their jobs were concerned about COVID-19 exposure and the potential
impact on themselves and their families. In addition, many workers found better paying jobs that were
often less stressful both in and out of health care. Some nurses pursued opportunities as travel nurses
or agency nurses, which tended to be higher paying. Other factors that contributed to attrition included
family commitments (childcare or eldercare) and transportation issues.
Strategies Used to Address Recruitment and Retention Diculties
Key informants described a variety of strategies they used to attract and retain workers. Some key infor-
mants described using incentives to attract health care professionals, particularly service-obligated schol-
arships and loan-repayment programs such as the Primary Care Service Corps, Doctors Across New York,
and the National Health Service Corps. In 2020, there were nearly 600 health care professionals who
participated in these programs and were fullling service obligations in NYC.
4
Informants also described partnerships with educational institutions to support career advancement
opportunities for new recruits as well as existing workers. Among the strategies used through these collab-
orations were standardized career-ladder programs (eg, nurse aide to LPN to RN) or internships or extern-
ships oered to health-professions students who would then go on to become employees after training.
Informants emphasized the value of local recruitment, indicating that community residents were more
likely to consider employment close to home.
Key informants discussed the urgent need to support new graduates’ transition to practice. During the
pandemic, RN students had limited access to clinical-training sites, greatly reducing direct-patient experi-
ence. According to Chief Nursing Ocers, many providers provide nurse residencies to new RN hires to help
them acclimate to patient care. However, preceptor shortages were problematic and challenged the eec-
tiveness of these residencies and oversight of clinical training for RNs and other health care professionals.
7

Center for Health Workforce Studies
BEST PRACTICES FROM THE FIELD
FutureReadyNYC
Northwell Health, a hospital-based healthcare system,
partnered with the New York City Department of Educa-
tion to create “FutureReadyNYC.” It introduces students
The aim of FutureReadyNYC is to help students visualize
their career paths by introducing earn-and-learn and profes-
sional development pathways connected directly to their
in grades 9-12 to healthcare roles and gives them a better
studies. Additionally, FutureReadyNYC aims to remove
understanding of opportunities at Northwell Health based
barriers to employment and spark interest in healthcare that
on high-demand jobs. The program is operating at 4 high
drives participants to become future innovators, leaders,
schools throughout New York City.
and clinicians, while building relevant skills to support their
readiness for economically secure careers in healthcare.
Retention strategies reported by key informants included retention bonuses, worker-resilience programs,
exible hours, and use of hybrid models when possible. Some key informants added more support sta
(LPNs and nurse aides) to ease the demands placed on RNs, while others used agency sta to reduce
the need for overtime by existing nursing sta. One focus group participant described using a “retention
coordinator” whose job entailed working with both new and existing sta to assess their satisfaction with
working conditions and to the extent possible, make changes that supported worker retention. A few key
informants indicated that they were exploring the potential for recruiting foreign-trained RNs as a strategy
but indicated that the process was both costly and lengthy and had not yet proved fruitful.
FIGURE 1. Employment Growth in NYC, 2000-2021 (Standardized to 2000)
90%
100%
110%
120%
130%
140%
150%
160%
170%
Percentage of Job Growth
Year
Health Care Employment All Other Employmetn Sectors
Source: NYSDOL, Quarterly Census of Employment and Wages.
8
Health Worker Recruitment and Retention in New York City
BEST PRACTICES FROM THE FIELD
Jamaica Hospital Student Nurse Summer Externship Program
Jamaica Hospital oers a 9-week paid externship program
each year that employs 30 nursing students during the
summer. RN students who are eligible for this program must
be currently enrolled in an accredited RN program and must
This program gives the student nurses an opportunity to
integrate theoretical knowledge with clinical skills and begin
to develop basic, critical thinking skills through the applica-
tion of the nursing process under the supervision of a nurse
have completed 2 semesters of clinical nursing rotations
preceptor. The program for 2022 began on June 26. Student
in an acute care setting and be entering their nal year of
externs were assigned to specic medical surgical units and
nursing education.
they also rotated through critical care and the emergency
department to gain more experience.
Some key informants described involvement in programs at local primary and secondary schools designed
to help students learn about health care career opportunities as well as expanded volunteer programs at
their facilities. They indicated that such programs may assure a future health workforce drawn from local
communities.
NYC Health Workforce Trends
Health Care Employment
● The Covid-19 pandemic aected both overall employment and health care employment in NYC.
Between 2019-2020, jobs in the health care sector in NYC declined by 4%, while jobs in all
other employment sectors dropped by 15%. Jobs in the health care sector in NYC, however,
rebounded in 2021, surpassing the number of jobs in 2019 (Figure 1). National trends indicate
a similar pattern of job loss in health care, with the number of jobs rebounding in 2021, though
not to the pre-COVID-19 levels.
5
● Jobs in home health care grew the fastest between 2016-2020 in NYC.
Between 2017-2021, jobs in home health care in NYC grew by 40%, jobs in ambulatory care grew
by 3%, and jobs in hospitals grew by 2% (Table 2). Jobs in nursing homes and residential-care
facilities in NYC both declined by 13% during the same period.
TABLE 2. Health Care Sector Employment in the New York City Region, by Setting, 2016-2020
Setting 2017 2018 2019 2020 2021
Change Between
2018-2022
Number Percent
Hospitals 205,662 205,108 208,304 211,577 209,483 3,821 1.9%
Ambulatory care (excluding
home health care)
129,172 129,152 134,312 122,008 132,903 3,731 2.9%
Nursing home and residential
care facilities
50,172 49,834 49,134 45,785 43,542 -6,630 -13.2%
Home health care 151,886 178,335 205,851 203,713 213,270 61,384 40.4%
Total 536,892 562,429 597,601 583,083 599,198 62,306 11.6%
Source: NYSDOL, Quarterly Census of Employment and Wages.
9

Center for Health Workforce Studies
BEST PRACTICES FROM THE FIELD
AHRC Retention Support Coordinator
AHRC, a federally qualied health center, has implemented
the new role of retention support coordinator (RSC). The
RSC focuses on retaining and engaging with rst-year direct
support professionals (DSPs). The RSC sends out onboarding
The RSC creates training plans for struggling DSPs when
requested, which are discussed and approved by managers.
The RSC also meets with program directors and human
resources business partners to identify “focus areas” at
surveys at 30-, 60-, and 90-days after the start of employ-
specic locations that have increased turnover, increased
ment, and exit surveys to the rst-year DSPs who resign. The
complaints, or reports of low morale.
RSC also conducts “stay” interviews after DSPs successfully
complete their probationary periods.
Employment Projections
● Jobs for home health aides and personal care aides are projected to grow the fastest in NYC
between 2018-2028.
Home health aide positions are projected to grow by nearly 72% between 2018-2028 in NYC,
with more than 37,000 annual openings (Table 3). There are projected to be nearly 32,000
annual openings for personal care aides during the same time period.
TABLE 3. Employment Projections for NYC for Selected Occupations, 2018-2028
Title
Number of Jobs
Projected Change
Between 2018-2028
Average
Annual
Openings
2018 2028 Number Percent
Home Health Aides 165,810 285,030 119,220 71.90% 37,185
Personal Care Aides 126,720 210,360 83,640 66.00% 31,855
Registered Nurses 78,470 97,570 19,100 24.30% 6,610
Nursing Assistants 39,790 45,570 5,780 14.50% 5,361
Medical Assistants 13,670 19,220 5,550 40.60% 2,367
Licensed Practical Nurses 15,380 19,360 3,980 25.90% 1,722
Medical and Health Service Administrators 14,440 17,920 3,480 24.10% 1,630
Healthcare Social Workers 7,040 9,600 2,560 36.40% 1,069
Clinical Lab Technologists and Technicians 7,900 9,370 1,470 18.60% 691
Nursing Practitioners 6,480 8,990 2,510 38.70% 664
Physician Assistants 5,770 8,140 2,370 41.10% 632
Radiologic Technologists 5,200 6,440 1,240 23.80% 443
Surgical Technologists 2,530 2,910 380 15.00% 258
Respiratory Therapists 2,260 2,940 680 30.10% 205
Source: NYSDOL, Jobs in Demand/Projects, Long-Term Occupation Projections, 2018-2028.
10

Health Worker Recruitment and Retention in New York City
● Driven by the growth of home health aide and personal care aide jobs, home health care
employment in NYC is projected to grow the fastest between 2018-2018.
Jobs in home health care are projected to grow the fastest in NYC between 2018-2028, increasing
by nearly 66%. Jobs in hospitals and nursing and residential-care facilities are projected to
increase by 13% and nearly 11%, respectively, during the same time period.
TABLE 4. Employment Projections for NYC by Setting, 2018-2028
Industry Title
Number of Jobs
Projected Change
Between 2018-2028
2018 2028 Number Percent
Ambulatory health care services 330,500 547,230 216,730 65.6%
Hospitals 213,450 241,210 27,760 13.0%
Nursing and residential care facilities 81,590 90,140 8,550 10.5%
Source: NYSDOL, Jobs in Demand/Projects, Long-Term Occupation Projections, 2018-2028.
Registered Nursing Employment in NYC
● Between 2018-2022, the number of licensed RNs with NYC addresses increased by nearly 8%.
Statewide, the number of total RN licenses increased by more than 17% between 2018-2022
(Table 5). The number of licensed RNs with NYC addresses increased by slightly over 9%, while
the number of RNs with other NYS addresses grew by nealry 9%. In contrast, licensed RNs with
out-of-state addresses increased by nearly 50% over the same time period.
● One in 10 RNs working in NYC lives in another state.
Based on an analysis of ACS data, 10% of RNs working in NYC live outside of NYS, including
11% of RNs working in hospitals (Table 6). In contrast, only 5% of RNs working in home health
care in NYC live outside of NYS.
TABLE 5. Count of RNs by License Address
2018 2019 2020 2021 2022
Change Between
2018-2022
Number Percent
RNs with New York City addresses 68,802 71,070 72,103 73,956 75,128 6,326 9.2%
RNs with other NYS addresses 168,642 173,420 175,237 181,132 183,315 14,673 8.7%
RNs with addresses outside NYS 64,763 72,928 80,864 90,124 96,752 31,989 49.4%
Total NYS RN licenses 302,207 317,418 328,204 345,212 355,195 52,988 17.5%
Source: NYSED.
11
Center for Health Workforce Studies
TABLE 6. The RN Workforce in NYC by Location of Residence and Work Setting
Setting NYS Addresses # (%)
Out of State Addresses
# (%)
Totals
Home health care 3,298 (95.1%) 169 (4.9%) 3,467
Ambulatory care (other than home care) 6,229 (90.5%) 653 (9.5%) 6,882
Hospitals 51,431 (89.2%) 6,254 (10.8%) 57,685
Nursing homes/LTC 5,682 (91.4%) 532 (8.6%) 6,214
Other employment sectors 6,839 (92.8%) 534 (7.2%) 7,373
Total NYC RN workforce 73,479 (90.0%) 8,142 (10.0%) 81,621
Source: ACS, 5-Year Estimates, 2015-2019.
The NYC Health Professions Educational Pipeline
● Between 2017-2021, social worker graduations in NYC grew by 650, or almost 22%.
The number of graduations from social worker education programs in NYC grew by 650, or
almost 22% between 2017-2021 (Table 7). Additionally, the number of graduates from LPN
education programs in NYC increased by 139 or by nearly 67% during the same time period.
In contrast, the number of pharmacist graduates from NYC education programs declined by 277
or by 46%. While the number of pharmacist graduates has decreased, research has indicated
that the number of pharmacy graduates is still exceeding average annual job openings.
6
The
number of RN graduates from NYC education programs also decreased, declining by 80 or by
just over 2% between 2017-2021. Finally, the number of clinical laboratory technologist grad-
uations declined by 51 or by almost 38% during the same time period. The number of surgical
technology graduations also fell between 2017-2021.
TABLE 7. Number of Graduations in Selected Health Professions Education Programs in NYC, 2017-2021
Occupational Program 2017 2018 2019 2020 2021
Change Between
2017 and 2021
Number Percent
Clinical Laboratory Technicians 34 32 26 24 26 -8 -23.5%
Clinical Laboratory Technologists 136 113 88 102 85 -51 -37.5%
Licensed Practical Nurses 208 243 334 287 347 139 66.8%
Mental Health Counselors 346 357 359 411 353 7 2.0%
Pharmacists 602 546 298 328 325 -277 -46.0%
Physician Assistants 637 665 610 608 602 -35 -5.5%
Radiation Therapists 205 239 227 231 225 20 9.8%
Registered Nurses 3612 3,322 3,197 3,376 3,532 -80 -2.2%
Respiratory Therapists 23 28 0 0 43 20 87.0%
Social Workers 3,014 2,980 3,109 3,112 3,664 650 21.6%
Surgical Technologists 113 146 104 138 94 -19 -16.8%
Source: IPEDS.
12

Health Worker Recruitment and Retention in New York City
Registered Nursing Education in NYC: Preliminary Findings
The 2022 Nursing Deans and Directors survey is currently in the eld. To date, over 30% of RN educa-
tion programs in NYC have responded to the survey (nearly a quarter of associate degree nursing (ADN)
programs and over 36% of baccalaureate degree nursing (BSN) programs. The following summarizes
preliminary ndings based on responses from NYC nursing education programs to date.
Nearly half of the deans reported that applications to their programs were comparable to last year. While
half of ADN deans indicated that applications to their programs were somewhat higher, only 18% of BSN
deans reported a higher number of applications compared to the previous year. More than 70% of the
deans indicated that the number of acceptances to their programs was comparable to last year.
Nearly three-quarters of the deans reported turning away qualied applicants for the 2021-2022 school
year. The reasons most often cited for turning away qualied applicants included faculty shortages, insuf-
cient number of clinical training sites, and program admissions caps. Over 33% of BSN deans cited lack
of classroom space as a reason for turning away qualied applicants.
More than 70% of deans indicated that they were recruiting faculty to ll vacant positions. On average, deans
reported recruiting for 3 faculty positions, and 80% of the positions were full time. More than two-thirds
of deans reported hiring adjunct faculty to ll these vacancies. When asked about the reasons for faculty
leaving their positions, the deans most commonly cited retirements, accepting nursing positions elsewhere,
making a career change in nursing, or family obligations.
When asked about COVID-19 impacts on their programs, two-thirds of deans cited reduced access to clin-
ical training sites which greatly reduced the preparedness of their graduates for entry into practice. All of
the deans reported increased use of simulation to help students complete clinical training requirements,
while some reported using alternate clinical settings to address this issue.
Nearly 80% of deans reported many job openings for their graduates. All BSN deans reported many jobs
in hospitals and in nursing homes, while all ADN deans reported many jobs for their graduates in nursing
homes. Nearly all deans agreed that the COVID-19 pandemic created more demand for newly trained RNs.
LIMITATIONS
Participants for the key informant interviews were selected using a convenience sample. Consequently,
they may not be representative of the population of health care providers in NYC, which could limit the
generalizability of ndings.
The hospital response rate to the employer-demand survey was low. This could result in selection bias,
eg, hospitals having the most dicult challenges responding to the survey which could limit the general-
izability of ndings.
13

Center for Health Workforce Studies
NYSDOL data were used to report the number of health care jobs in NYC. These data are potentially aected
by several factors, including closures, mergers, and expansions of health facilities. Consequently, large
changes in jobs in specic health sectors (ie, hospitals, nursing homes, or home health care) may reect
changes in ownership or the service delivery system rather than changes in the workforce. Additionally,
more recent changes in jobs and employment such as temporary or permanent layos or retirements due
to the COVID-19 pandemic may not be reected in the data.
NYSDOL 2018-2028 job projections include counts of both newly created positions and annual job openings
that are a result of worker departures (retirements, job changes, departures from the eld). Occupations
with a small increase in the number of new jobs but a high number of annual openings typically reect
signicant annual turnover rather than expansion of the occupation. Limitations to these projections include
unanticipated external factors such as recessions, changes in scope of work or education for specic occu-
pational titles, changes in state and/or federal reimbursement, and advances in technology. Additionally,
these projections did not account for the eects of the COVID-19 pandemic on the need for health care or
the impact the COVID-19 pandemic had on the health care workforce.
NYSED licensure counts are based on the mailing address of licensees, which could be either a home or a
practice location. Certain individuals in the le may be licensed to practice in NYS but may live and/or work
in another state. Some individuals who are licensed in a health care profession may be working part time,
may not be working in the profession at all, or may be working in the profession in another state. Conse-
quently, licensure counts tend to overestimate the number of active health professionals working in NYS.
Not all health professions graduations reect newly licensed individuals entering a profession. For example,
some RN graduates are BSN completers, ie, they are already licensed nurses who obtained a higher nursing
degree. Additionally, graduation may not make a person qualied to practice in a profession. For example,
graduating with a bachelor’s degree in social work does not qualify a person for licensure in NYS.
DISCUSSION
The COVID-19 pandemic had profound impacts on the state’s health care delivery system as well as its
workforce. Initially, as COVID-19 pandemic cases surged, demand for acute care services rose sharply.
NYS used a number of dierent strategies, sometimes through executive order s to build health workforce
surge capacity, to make better use of the available health workforce and to facilitate licensing health profes-
sionals from other states. Many hospital systems hired travel RNs to ll stang gaps. This may explain the
dramatic increase in the number of RNs licensed in NYS with out-of-state addresses. The use of travel RNs,
however, is not a long-term solution. Decreased hospital admissions, especially from elective surgeries, in
conjunction with increased workforce costs, have nancially stressed hospitals even further.
Additionally, during that time, many providers, particularly in ambulatory care, cut back or stopped services
entirely, temporarily or permanently closing oces and laying o sta. This, in part, may explain the 4%
drop in health care employment between 2019-2020. For many patients, in-oce ambulatory visits were
14

Health Worker Recruitment and Retention in New York City
replaced by telehealth or teledentistry visits. While national data have shown a rebound in health care
employment, the number of health care jobs has not returned to the pre-COVID-19 pandemic levels. This,
in combination with the increased number of retirements, has stressed the health care workforce even
further.
As acute COVID-19 cases began to subside, health care providers in all settings experienced great diculty
recruiting and retaining workers, particularly in patient care. While health worker shortages were not a new
phenomenon, the COVID-19 pandemic dramatically increased the number of occupations in short supply
as well as the magnitude of the shortages. Other employment sectors were also experiencing widespread
labor shortages at that time and were also competing for the same entry-level workers. As a result, there
was very strong competition for workers in general and in health care settings specically.
RNs, LPNs, and social workers were identied as very dicult to recruit by providers across all health care
settings. Hospitals also reported diculty recruiting behavioral health providers, radiologic technicians,
surgical technicians, respiratory therapists, and laboratory technicians and technologists. Long-term care
providers also reported diculty recruiting nursing directors, CNAs, and clerical sta. Home care providers
reported diculty recruiting and retaining home health aides and personal care aides. Ambulatory care
providers reported diculty recruiting physicians, nurse practitioners, behavioral health providers, clerical
sta, and medical assistants.
A critical factor that contributed to recruitment problems was that demand for workers outstripped supply,
resulting in greater competition for available workers. Noncompetitive salaries were also problematic.
Those occupations considered hard to recruit were also identied as hard to retain and the COVID-19
pandemic contributed to more attrition from the workforce. Many workers experienced stressful working
conditions (extremely ill patients and stang shortages) and left their jobs, including many older workers
who retired. Some workers left their jobs because they were concerned about COVID-19 exposure and
the potential impact on themselves and their families. Other workers found better paying jobs both in
and out of health care. Other factors that contributed to increased attrition included family commitments
(childcare or eldercare) and transportation issues.
Employers observed a generational shift in how younger employees view their jobs. These workers prioritize
work-life balance by engaging in behaviors such as “quiet quitting” in order to avoid burnout and maintain
better balance between their work and personal lives. Employers recognized the need to structure workers’
jobs to support resilience and help workers achieve this balance, giving them a sense of control, while
ensuring the work gets done. Eorts to address these concerns have the potential to reduce behaviors
such as “ghosting” by new employees, who may be attracted to a work culture that prioritizes resilience
and balance. One key informant described using a retention coordinator who was tasked with worker
outreach and the development of strategies to support sta retention.
15

Center for Health Workforce Studies
The COVID-19 pandemic also impacted the health professions education pipeline. While there was little
change in the number of new RN graduates between 2020-2021, there was a change in new RNs’ practice
readiness. During COVID-19, many health care providers were unable to accommodate clinical rotations for
students and as a result, nursing students had limited experience working directly with patients. According
to many of the individuals interviewed, this left them much less prepared for working in patient-care
settings. Nursing deans indicated that they cannot easily expand program capacity as they are constrained
by limited access to clinical training sites and faculty shortages.
A variety of health workforce recruitment strategies were identied and included service-obligated scholar-
ships and loan-repayment programs. Other providers reported educational partnerships to support career
advancement, including career ladders. Nurse residencies were a common strategy to support transition to
practice for new RN graduates. Retention strategies included sign-on bonuses, worker resilience programs,
and exible hours. Also, providers added more support sta or agency sta to reduce demand on patient-
care RNs. It is unclear how successful these strategies have been in the short term and what their impact is
long term. Thus, it is important to assess the eectiveness of these strategies and to identify best practices.
CONCLUSION
This study aimed to identify the workforce issues that NYC health care providers were facing, the factors
contributing to recruitment and retention challenges, including COVID-19 impacts, and the strategies used
to address these challenges. Data drawn from a variety of sources, both primary and secondary, were used
to answer the research questions posed. Findings suggest widespread workforce shortages exacerbated by
the COVID-19 pandemic. Providers identied a variety of strategies that can potentially reduce the supply/
demand imbalances currently faced by NYC health care providers. Strategies that can potentially alleviate
health workforce shortages require collaborative eorts by a wide array of stakeholders including, among
others, providers, educators, labor, management, and governmental entities.
16

Health Worker Recruitment and Retention in New York City
REFERENCES
1
US Department of Health and Human Services, Health Resources & Services Administration. Health work-
force data, tools, and dashboards. Accessed August 8, 2022. https://data.hrsa.gov/topics/health-workforce/
health-workforce-shortage-areas
2
Carbajal E, Plescia M, Gooch K. Why don’t hospitals just pay full-time nurses more? Becker’s Hospital
Review. January 21,2022. Accessed August 26, 2022. https://www.beckershospitalreview.com/nursing/
the-complexity-behind-travel-nurses-exponential-rates.html
3
Wilks C. 5 Reasons Why Quiet Quitting Is Great for Your Mental Health. Psychol Today. Accessed August
29, 2022. https://www.psychologytoday.com/us/blog/human-ourishing-101/202208/5-reasons-why-quiet-
quitting-is-great-your-mental-health
4
Harun N, Martiniano R. The Impact of Service-Obligated Providers on Healthcare in New York State. Rensselaer,
NY: Center for Health Workforce Studies, School of Public Health, SUNY Albany; September 2020.
5
Cantor J, Whaley C, Simon K, Nguyen T. US healthcare workforce changes during the rst and second years
of the COVID-19 pandemic. JAMA Health Forum. 2022;3(2):e215217. doi:10.1001/jamahealthforum.2021.5217.
6
Lebovitz L, Rudolph M. Update on pharmacist workforce data and thoughts on how to manage the over-
supply. Am J Pharm Educ. 2020;84(10):ajpe7889. doi:10.5688/ajpe7889.
17

ABOUT THE AUTHORS
Jean Moore, DrPH, FAAN
Director, Center for Health Workforce Studies
As director, Dr. Moore is responsible for administrative aspects and participates in the prepa-
ration and review of all CHWS research projects and reports, ensuring their policy relevance.
She also plays a key advisory role for CHWS, its activities, and the outcomes of its work. Dr.
Moore has served as principal investigator for more than 35 health workforce research studies
and authored nearly 70 publications, including peer-reviewed journal articles and reports.
Robert Martiniano, DrPH, MPA
Senior Program Manager, Center for Health Workforce Studies
Dr. Martiniano has an extensive background in health workforce research and program
management, including 11 years at the New York State Department of Health. He has worked
with a number of dierent communities, agencies and membership organizations on devel-
oping community health needs assessments, identifying provider and workforce shortages
based on the healthcare delivery system and the health of the population, and understanding
the impact of new models of care on the health care workforce—including the development
of emerging workforce titles.
Patricia Simino Boyce, PhD, MA, BS
University Dean for Health and Human Services, CUNY
Patricia Simino Boyce is the University Dean for Health and Human Services (HHS) at CUNY.
Dr. Boyce is responsible for the portfolio of HHS undergraduate and graduate degrees, and
credit-bearing certicate programs across CUNY’s 25 colleges and graduate schools, repre-
senting 40,000 enrolled students. Dr. Boyce provides strategic direction across CUNY’s HHS
portfolio and collaborates with academic leadership, industry partners, and key stakeholders
to mobilize resources, best practices, partnerships, and innovations to ensure distinction in
CUNY’s academic programs and clinical experiences that drive career success for students and
meet industry needs for the healthcare, allied health, public health, and human service elds.
School of Public Health | University at Albany, SUNY
1 University Place, Suite 220 | Rensselaer, NY 12144-3445
www.chwsny.org
