
Potential Harm to Fertility
• Gonorrhea, chlamydia, syphilis and HIV can reduce fertility
• HIV can make it more likely to contract gonorrhea, chlamydia, and syphilis, which
impact fertility
• Scarring from these infections can make it hard to conceive (pelvic inflammatory
disease)
Sexually Transmitted Infections and Treatment
STIs and Threat to Fertility
• Most common viral STI
• Spread by skin-to-skin contact, oral sex, anal sex, and vaginal sex
• Condoms do not necessarily prevent HPV
• Most do not know they have the infection, since it may not show symptoms
o HPV can be spread even without symptoms
• Most people are asymptomatic and do not know they have the infection
• There are many types (strains) of HPV, which vary in symptoms:
o Some go away on their own
o Some have no symptoms
o Some cause cervical cancer
o Some cause genital warts
• Can also cause cancer of the vagina, anus, head and neck
• HPV is not curable, but symptoms can be treated
General Information and Transmission
Symptoms and Treatment
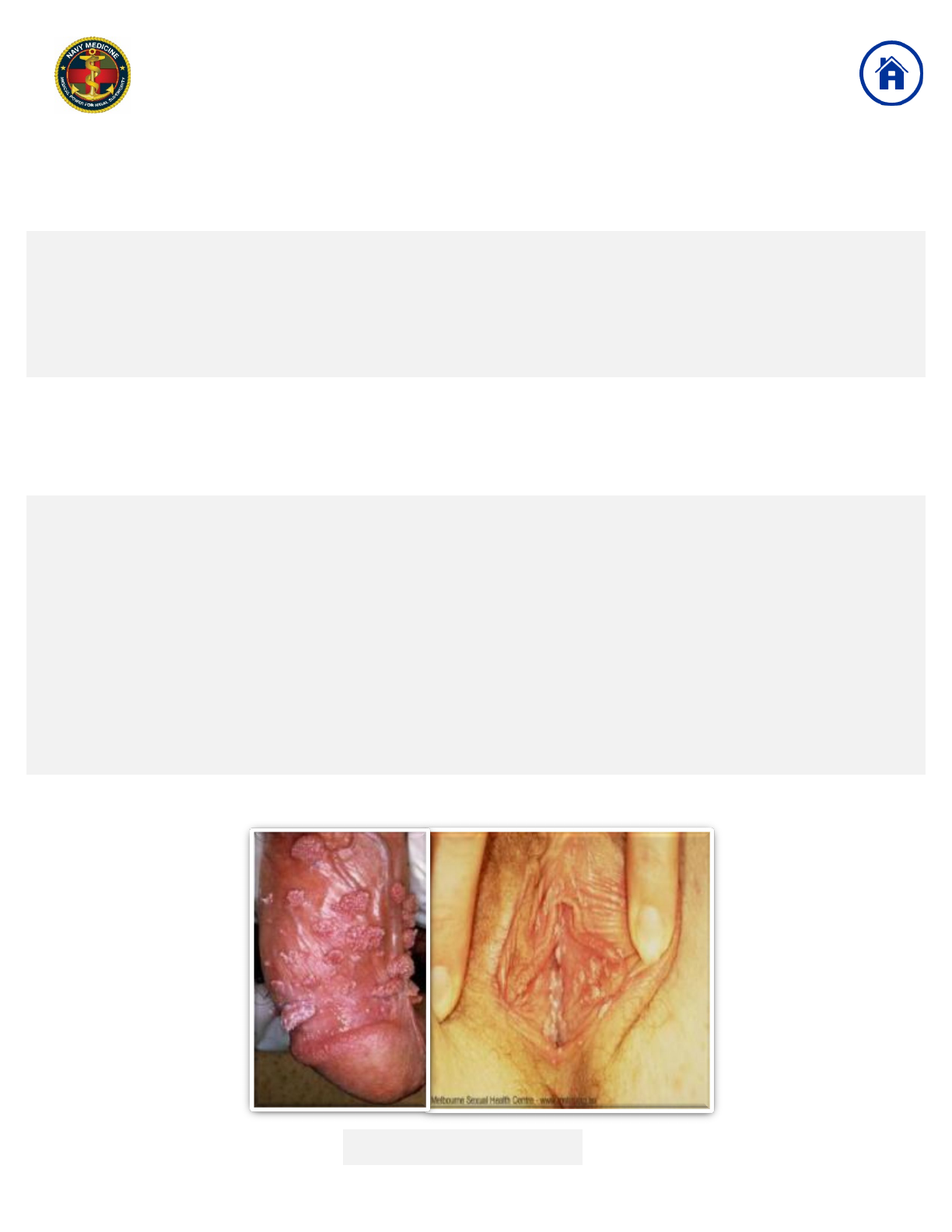
Genital warts from HPV
Sexually Transmitted Infections and Treatment
Human Papilloma Virus (HPV)

First Line Patient Applied Therapy
Imiquimod (Aldara, Zyclara)
• 3.75% Cream: Apply thin film once daily before bedtime for two weeks to the skin of the
affected area; keep on eight hours, then wash off with soap and water. Continue nightly
until the warts are gone, no more than eight weeks.
• 5% Cream: Apply a thin layer three times per week (on alternate days) prior to bedtime;
leave on skin for six to ten hours, then remove with mild soap and water. Continue until
there is total clearance of the genitals/perianal warts for a maximum duration of therapy
of sixteen weeks.
Podophyllotoxin
• Apply podophyllotoxin twice daily for three consecutive days, then withhold use for four
consecutive days. This one-week course may be repeated up to four times until warts
are no longer visible. The total treatment area should not exceed 10 cm
2
, and the total
volume of podophyllotoxin should be limited to 0.5 mL per day. The area to which
podophyllotoxin is applied should not contain any open lesions or wounds.
Podophyllotoxin should be washed off one to four hours after application in order to
minimize local irritation. If feasible, the clinician should apply the first treatment to
demonstrate the correct sites for application and proper technique. Sexual intercourse
should be avoided when podophyllotoxin is on the skin.
Sinecatechins (Veregen)
• Apply a thin layer three times daily to warts until all warts have cleared, maximum
duration sixteen weeks.
Sexually Transmitted Infections and Treatment
Medical Treatment for Genital Warts

Clinician Applied Therapy
Sexually Transmitted Infections and Treatment
Medical Treatment for Genital Warts
Cyrotherapy: Liquid nitrogen is typically applied via a spray gun device or a cotton bud,
and two freeze-thaw cycles are performed. A small margin of healthy skin (e.g., 1 mm)
should be included in the treatment area. Treat patients every two weeks for up to six to
ten weeks. If clearance has not been achieved within six to ten weeks, other treatment
should be implemented.
Electrosurgery: After the injection of a local anesthetic, warts are desiccated and are
either left to fall off or curetted. Care must be taken to control the depth of electrocautery to
minimize scarring. Similar to surgical excision, high clearance rates (94% - 100%) have
been reported but recurrence is possible. More likely to result in permanent
dyspigmentation and scarring.
Surgical Excision: Surgical excision is most beneficial for patients who have large (e.g.,
>1 cm), exophytic anogenital warts. A scissor or shave excision can remove most
anogenital warts. Excision to the depth of the superficial dermis is generally sufficient.
Laser Therapy: Carbon dioxide (CO
2
) lasers are the principal lasers used to destroy
anogenital warts. Treatment is painful; local or general anesthesia is necessary. The
surgeon must be certified and credentialed to use the laser.

What is Gardasil?
• Gardasil is an optional vaccine available for male and females age 9 – 45
• Only 5% of eligible military males are currently being vaccinated and approximately
26% of eligible military females
• The vaccine can prevent genital warts, cervical cancer, anal cancer, and oropharyngeal
cancer, so OFFER YOUR ELIGIBLE PATIENTS THE VACCINE IF THEY HAVE NOT
HAD IT!
How does it work?
• Prevents against nine most common types of HPV which cause 90% of cervical
cancer and genital warts
• This is a 3-shot series for those age 15 and above (2 shots for ages 9 - 14)
o 1
st
shot: between ages 15-45 years old
o 2
nd
shot: 2 months later
o 3
rd
shot: 6 months after first (can be completed any time after the initial vaccine)
Gardasil
Sexually Transmitted Infections and Treatment
HPV Vaccine

Types
• HSV 1: Typically appears on the mouth (i.e., cold sores)
• HSV 2: Typically appears on the genitals
o But HSV1 can be spread to the genitals if someone who gets cold sores performs
oral sex
Transmission
• Skin-to-skin contact, oral, anal, and vaginal sex
• Transmission may occur when an infected person does not have a visible sore, or
does not even know the infection is present
• Very common, many catch HSV1 during their childhood
• Condoms reduce the risk of getting/spreading genital herpes but do not eliminate
risk
Symptoms
• During the first outbreak, one may experience
o Painful, red bumps (sores)
o Blisters that rupture and spread
• Stress can trigger outbreaks
• Over time, outbreaks happen less frequently or stop
Treatment
• Herpes is not curable, but outbreaks can be treated with antivirals to lessen discomfort
• Stigma against herpes is often worse than the actual infection itself
Types and Transmission
Symptoms and Treatment
Sexually Transmitted Infections and Treatment
Herpes Simplex Virus

Primary: Initial presentation can be mild or severe with painful genital ulcers, dysuria,
fever, tender local inguinal lymphadenopathy, and headache, or may be asymptomatic.
Typical incubation is four days but can range two to twelve days. Duration nineteen days
with viral shedding for two to five days.
Non-primary first episode: Same as primary but associated with fewer lesions and less
systemic symptoms. Duration ten days with viral shedding two to five days.
Recurrent: Same as primary but associated with fewer lesions, shorter duration, and less
systemic symptoms.
No shipboard capability of testing, so treatment initiation is based upon symptoms. If not
on ship, it can be diagnosed by culturing a lesion (unroof it and obtain sample of vesicular
fluid), or by type specific serologic tests. It can also be diagnosed with polymerase chain
reaction. Obtaining the serotype (HSV 1 vs HSV 2) can help predict expected recurrence
of outbreaks.
Testing
Primary: Important to initiate treatment within 72 hours of symptoms. Treatment duration
7-10 days.
• Acyclovir: 400 mg three times daily
• Famciclovir: 250 mg three times daily
• Valacyclovir: 1000 mg twice daily
Recurrent: Important to initiate treatment within 24 hours of symptoms.
• Acyclovir: 800 mg three times daily for two days; or 800 mg twice daily for five
days; or 400 mg three times daily for five days
• Famciclovir: 1000 mg twice daily for a single day duration; or 125 mg twice daily
for five days; or 500 mg once, followed by 250 mg twice daily for two days
• Valacyclovir: 500 mg twice daily for three days or 1000 mg once daily for five
days
Treatment
Sexually Transmitted Infections and Treatment
Herpes Simplex Virus
Primary vs. Recurrent

Treatment
• Metronidazole (Flagyl): 2 grams in a single oral dose or alternatively 500 mg orally
twice daily for seven days as 2 grams is not always tolerated
• DO NOT DRINK ALCHOHOL WHILE TAKING FLAGYL: Abdominal cramps, nausea,
vomiting, headaches, and flushing have been reported with oral and injectable
metronidazole and concomitant alcohol consumption (disulfiram-like reactions)
• Alternative: Tinidazole: 2 gram single dose or 500 mg twice a day for seven days
Transmission and Symptoms
Sexually Transmitted Infections and Treatment
Trichomonas
• Also known as “trich”
• Common bacterial STI
• Transmitted through oral, anal and vaginal sex
• In most cases has no symptoms
• Men typically have no symptoms
• Symptoms for women include:
o Foul-smelling vaginal discharge
o Genital itching
o Painful urination

General Information
• Bacterial STI
• Retesting three to six months after treatment is recommended due to risk of re-
infection
• Ensure the patient’s partner is treated to avoid re-infection
• Resistant strains of gonorrhea are on the rise
Transmission
• Oral, anal, and vaginal sex
Symptoms
• Majority are asymptomatic
• Can cause infertility due to fallopian tube scarring
• Symptoms for women:
o Increased vaginal discharge
o Pain with intercourse
o Fever
o Sore throat
o Irregular bleeding
o Pain with urination
o Cervical friability or mucopurulent discharge
Types and Transmission
Symptoms and Treatment
Sexually Transmitted Infections and Treatment
Chlamydia and Gonorrhea

The rising rates of gonococcal resistance to non-cephalosporin classes of antimicrobial
agents led to the use of cephalosporins, particularly intramuscular injections of ceftriaxone
and oral cefixime. However, trends in increasing mean minimum inhibitory concentrations
(MICs) of N. gonorrhoeae for both agents, indicating decreasing susceptibility, have been
reported worldwide and have led to changes in the recommendations for use of these
agents. For patients with allergies or suspected gonococcal resistance, consult a physician
for other treatment options as these patients may require intravenous therapy.
To treat Chlamydia:
• Azithromycin: 1 gram in a single oral dose
• Alternative 1: Ofloxacin 300 mg twice a day for 7 days
• Alternative 2: Levofloxacin 500 mg orally once a day for 7 days
To treat Gonorrhea:
• Ceftriaxone 250 mg intramuscular in a single dose for treatment of gonococcal infection
• In addition to Ceftriaxone: Azithromycin (1 gram in a single oral dose) for possible
additional activity against N. gonorrhoeae and for treatment of potential chlamydia
coinfection. (Dual therapy is related to concerns regarding the early emergence of
cephalosporin resistance and the paucity of alternative first-line agents)
• Alternative: Doxycycline (100 mg orally twice daily for seven days) is not an optimal
alternative to azithromycin for uncomplicated gonococcal infections given concerns
about the increased prevalence of N. gonorrhoeae resistance to doxycycline. However,
doxycycline is used in combination with ceftriaxone for pelvic inflammatory disease (in
combination with ceftriaxone) due to its activity against C. trachomatis. Doxycycline is
also used for cases of epididymitis or proctitis, in which azithromycin has not been
studied.
Treatment
Sexually Transmitted Infections and Treatment
Chlamydia and Gonorrhea

Transmitted through direct contact with a syphilis sore.
• Can be spread through skin-to-skin contact, oral, anal, and vaginal sex
• Incidence is on the rise
• Testing: RPR (Rapid Plasma Reagin) looks for presence of antibodies. A reactive
nontreponemal test is then confirmed with a treponemal test, such as the fluorescent
treponemal antibody absorption (FTA-ABS)
• If recently infected, serologic testing may be negative; if high suspicion, treat and retest
in four weeks
Primary Symptoms
• Single, small, round painless sore; can appear from ten to ninety days after sex with
infected person. Sore can heal within three to six weeks, even without treatment (but
infection is still present).
Secondary Symptoms
• Rash on hands and feet; can appear two to ten weeks after appearance of sore.
Tertiary (Late) Symptoms
• Damage to heart, eyes, brain, nerves, bones, liver, or joints; may be years or decades
after infection.
Treatment
• Penicillin G benzathine: 2.4 million units IM once
• Alternative: Doxycycline: 100 mg orally twice daily for 14 days
• Late stages are not curable.
Symptoms and Treatment
Transmission
Sexually Transmitted Infections and Treatment
Syphilis

What is HIV?
What is AIDS?
Sexually Transmitted Infections and Treatment
Human Immunodeficiency Virus (HIV)
Acquired Immune Deficiency Syndrome (AIDS)
• Virus that attacks the immune system that can result in AIDS if left untreated.
• Transmitted through oral, anal and vaginal sex, and blood transfer (i.e. sharing
needles).
• Cannot be spread through saliva (kissing, sharing drinks) or shared toilet seats.
• Can take up to 6 months to show on a blood test.
• Early infection causes a variety of nonspecific ‘flu like’ symptoms such as fever, muscle
aches, rash, fatigue, sore throat, enlarged lymph nodes.
• HIV becomes AIDS when the body’s immune system is too weak to fight off infection
• AIDS is diagnosed when a patient develops an AIDS defining illness, such as Kaposi
sarcoma, Pneumocystis pneumonia, or toxoplasmosis (there are 27 conditions that
define AIDS).
• Can take up to 10 years to develop symptoms and full blown AIDS.
• Immediate use of antiretroviral medications can prolong life expectancy and duration in
the asymptomatic phase of HIV.

• PrEP (pre-exposure prophylaxis) is a daily medicine that can reduce your chance of
getting HIV.
• Daily PrEP reduces the risk of getting HIV from sex by more than 90%. Among
people who inject drugs, it reduces the risk by more than 70%.
• Risk of getting HIV from sex can be lowered by combining PrEP with condoms.
• Condoms are available at military pharmacies and can also be purchased for ten
cents a piece
here: (http://www.totalaccessgroup.com/condoms_for_military.html)
when you ask for public health pricing.
• Recommended for:
o People in an ongoing sexual relationship with an HIV-positive partner.
o Heterosexual men or women who do not regularly use condoms during sex with
partners of unknown HIV status who are at substantial risk of HIV infection.
o People who have injected drugs in the past 6 months.
o HIV negative women with an HIV-positive partner who are considering getting
pregnant may consider the risks and benefits of PrEP as one strategy to reduce
the risk of HIV infection for herself and her baby.
What is PEP?
What is PrEP?
Sexually Transmitted Infections and Treatment
HIV Prevention with PrEP and PEP
• PEP (post-exposure prophylaxisis) can reduce your chance of getting HIV after
potential exposure by taking antiretroviral medications.
• Must be taken within seventy-two hours of potential exposure.
• Available at military pharmacies.
• Recommended for emergency situations, such as exposure to blood from person with
an unknown HIV status or sexual assault.

• Viral infection that attacks the liver.
• Transmitted through oral, anal, and vaginal sex, and blood contact (Tattoos, IV
drug use).
• Testing:
• Hepatitis B surface antigen (HBsAg) is the serologic hallmark of HBV infection. It
can be detected using an enzyme immunoassay (EIA). HBsAg appears in serum
one to ten weeks after an acute exposure to HBV, prior to the onset of hepatitic
symptoms or elevation of serum alanine aminotransferase (ALT). In patients who
subsequently recover, HBsAg usually becomes undetectable after four to six
months. Persistence of HBsAg for more than six months implies chronic infection.
Type of Infection and Transmission
Symptoms and Treatment
Sexually Transmitted Infections and Treatment
Hepatitis B
• Most people have no symptoms
• Those who do develop symptoms may have fatigue, nausea, loss of appetite, and
yellowing of the eyes and skin.
• In most people, Hepatitis B and C cannot be cured and can cause liver failure over time
• Can be prevented by vaccine:
• Most people have already been vaccinated.
• For most patients, treatment is mainly supportive. The likelihood of liver failure from
acute HBV is less than one percent, and in immunocompetent adults, the likelihood
of progression to chronic HBV infection is less than 5%.

Are any of the following present?
• Pelvic abscesses**
• Trichomonas vaginalis infection
• Bacterial vaginosis
No
Yes
Are any of the following present?
• Severe clinical illness (high fever, nausea, vomiting, severe abdominal pain)
• Complicated PID with pelvic abscess (including tubo-ovarian abscess)
• Possible need for invasive diagnostic exploration for alternate etiology (e.g.,
appendicitis, ovarian torsion) or surgical intervention for suspected ruptured tubo-
ovarian abscess
• Inability to take oral medications due to nausea and vomiting
• Pregnancy
• Lack of response or tolerance to oral medications
• Concern for nonadherence to therapy
Are any of the following present?
• Gynecologic instrumentation in the prior 2 to 3
weeks
• Trichomonas vaginalis infection
• Bacterial vaginosis
Hospitalize and initiate a parenteral regimen*:
• Cefoxitin OR cefotetan PLUS Doxycycline
OR
• Clindamycin PLUS Gentamicin
• Continue until clinical improvement
Yes
No
Once tolerating oral intake,
add the following
medications:
• Doxycycline
PLUS
• Metronidazole to
complete a 14-day
course
Once tolerating oral intake,
add the following
medications:
• Doxycycline to complete
a 14-day course
Treat in the outpatient setting
with:
• Single IM dose of a long-
acting cephalosporin (e.g.,
ceftriaxone) PLUS
• Doxycycline for 14 days
PLUS
• Metronidazole for 14 days
Treat in the outpatient setting
with:
• Single IM dose of a long-
acting cephalosporin***
(e.g., ceftriaxone)
PLUS
• Doxycycline for 14 days)
Antibiotic doses:
• Cefoxitin 2 g intravenously every 6 hours
• Cefotetan 2 g intravenously every 12 hours
• Clindamycin 900 mg intravenously every 8 hours
• Gentamicin 3 to 5 mg/kg every 8 hours
• Ceftriaxone 250 mg intramuscularly once
• Doxycycline 100 mg orally twice daily
• Metronidazole 500 mg orally twice daily
Yes
No
IM: Intramuscular; PID: pelvic inflammatory disease.
TOA may require surgical management.
*These two regimens are both recommended by the Centers for Disease Control and
Prevention in the United States. We generally prefer cefoxitin or cefotetan plus
doxycycline for its overall safety and tolerability.
** Refer to other UpToDate content for details on additional management
considerations, including other potential antibiotic regimens, for women with a tubo-
ovarian abscess.
***We prefer ceftriaxone because it has the best and most established activity against
Neisseria gonorrhoeae. Other appropriate cephalosporins include cefoxitin (with
probenecid), cefotaxime, and ceftizoxime.
Sexually Transmitted Infections and Treatment
Antimicrobial Therapy for Pelvic Inflammatory
Disease in Adults and Adolescents
Color Key:
Treatment Plan
General Flow
Chart Pathway
Decision Factor

• Fully treatable with antibiotics, although antibiotic resistance is becoming more
common.
• Treatment for gonorrhea, chlamydia, trichomoniasis, syphilis does not protect you
against reinfection
• HPV/Herpes
o Infection remains in your immune system for life, but you can manage the
symptoms with antivirals.
o Can still have children with guidance of a provider.
• HIV
o Over 6,000 active duty Sailors and Marines have been diagnosed with HIV since
1985.
o Sailors are diagnosed with HIV at about twice the rate compared to Marines.
o Most (98%) Sailors and Marines diagnosed with HIV are men and most are aged
20-39.
o However, women can get HIV.
o If diagnosed, you can remain active duty and receive excellent care.
o You can still have a healthy child.
o Patients with HIV should disclose their status to any potential partners, use
condoms and other precautions, and their partners should use PrEP.
STI screenings are essential to know your STI status.
Disclosure to partners is key to ensure both parties can have informed, safer sex.
Curable STIs: Gonorrhea,
Chlamydia, Trichomoniasis, Syphilis
Sexually Transmitted Infections and Treatment
Living with STIs
Treatable STIs: HPV, Herpes and HIV



