Trauma-Informed Care in
Behavioral Health Services
Treatment Improvement Protocol (TIP) Series
57
Part 3: A Review of the Literature
Contents:
Section 1—Literature Review
Section 2—Annotated Bibliography
Section 3—General Bibliography
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Substance Abuse and Mental Health Services Administration
Center for Substance Abuse Treatment
1 Choke Cherry Road
Rockville, MD 20857
Contents
Section 1—A Review of the Literature .................................................................................... 1-1
Introduction to Trauma and Traumatic Stress Reactions ....................................................... 1-1
Types of Trauma .................................................................................................................. 1-15
Extent and Effects of Trauma and Traumatic Stress Reactions in Specific Populations ..... 1-24
Responses to Trauma: Trauma and Behavioral Health ........................................................ 1-38
Screening and Assessing Trauma and Trauma-Specific Disorders ..................................... 1-65
Prevention and Early Interventions for Traumatic Stress Reactions ................................... 1-72
Trauma-Specific Treatments ................................................................................................ 1-79
Integrated Approaches for Trauma and Substance Abuse ................................................... 1-93
Other Integrated Approaches ............................................................................................... 1-95
Treating Complex Trauma/PTSD ........................................................................................ 1-96
Treatment for Specific Populations ..................................................................................... 1-97
Trauma-Informed Intervention Considerations ................................................................. 1-102
Building a Trauma-Informed Workforce ........................................................................... 1-105
References .......................................................................................................................... 1-108
Appendix—Methodology .................................................................................................. 1-153
Section 2—Links to Select Abstracts ........................................................................................ 2-1
Section 3—General Bibliography ............................................................................................. 3-1
Trauma-Informed Care in Behavioral Health Services 1-1
Section 1—A Review of the Literature
Introduction to Trauma and Traumatic Stress Reactions
Providing a comprehensive literature review on trauma, traumatic stress, trauma-informed care
(TIC), and trauma-related interventions is a daunting task when considering the quantity and
prolific production of research in this area in the past 20 years. To manage the volume of
information, this literature review mainly focuses on reviews and meta-analyses rather than
seminal work to address many of the most relevant topics.
What Is Trauma?
In this text, “trauma” refers to experiences that cause intense physical and psychological stress
reactions. “Trauma results from an event, series of events, or set of circumstances that is
experienced by an individual as physically or emotionally harmful or threatening and that has
lasting adverse effects on the individual’s functioning and physical, social, emotional, or spiritual
well-being” (Substance Abuse and Mental Health Services Administration [SAMHSA], Trauma
and Justice Strategic Initiative, 2012, p. 2). Although many individuals report a single specific
traumatic event, others, especially those seeking mental health or substance abuse services, have
been exposed to multiple or chronic traumatic events. According to the Diagnostic and Statistical
Manual of Mental Disorders, 5th Edition (DSM-5), trauma is defined as when an individual
person is exposed “to actual or threatened death, serious injury, or sexual violence” (American
Psychiatric Association [APA], 2013, p. 271).
The definition of psychological trauma is not limited to diagnostic criteria, however. In fact,
some clinicians have moved away from considering trauma-related symptoms as indicators of a
mental disorder and instead view them as part of the normal human survival instinct or as
“adaptive mental processes involved in the assimilation and integration of new information with
intense survival emphasis which exposure to the trauma has provided” (Turnbull, 1998, p. 88).
These normal adaptive processes only become pathological if they are inhibited in some way
(Turnbull, 1998), or if they are left unacknowledged and therefore untreated (Scott, 1990).
Trauma has been characterized more broadly by others. For example, Horowitz (1989) defined it
as a sudden and forceful event that overwhelms a person’s ability to respond to it, recognizing
that a trauma need not involve actual physical harm to oneself; an event can be traumatic if it
contradicts one’s worldview and overpowers one’s ability to cope.
How Common Is Trauma?
Trauma exposure is common in the United States. However, trauma exposure varies
considerably according to different demographic characteristics and is especially high among
clients receiving behavioral health services (see the discussions under the headings “Extent and
Effects of Trauma and Traumatic Stress Reactions in Specific Populations” and “Other Disorders
That May Be Related to Trauma ” for more information on relevant rates). Although the large
surveys discussed here provide data on trauma exposure for the general population, published
1-2 Part 3, Section 1—A Review of the Literature
literature often provides more specific data as well, which is one reason why differences in
exposure according to gender and race/ethnicity are highlighted here.
At one time, trauma was considered an abnormal experience. Contrary to this myth, the first
National Comorbidity Study (NCS), a large national survey designed to study the prevalence and
effects of mental disorders in the United States, established how prevalent traumas are in the
lives of the general U.S. population (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995).
Presented with a list of 11 types of traumatic experiences and a 12th “other” category, 60.7
percent of men and 51.2 percent of women reported experiencing at least one trauma in their
lifetime (Kessler, 2000; Kessler et al. 1995; 1999):
The most common trauma was witnessing someone being badly injured or killed (cited by
35.6 percent of men and 14.5 percent of women).
The second most common trauma was being involved in a fire, flood, or other natural
disaster (cited by 18.9 percent of men and 15.2 percent of women).
The third most common trauma was a life-threatening accident/assault, such as from an
automobile accident, a gunshot, or a fall (cited by 25 percent of men and 13.8 percent of
women.
The NCS also found that it was not uncommon for individuals to have experienced multiple
traumatic events (Kessler, 2000). Among men in the total sample, 14.5 percent reported two
traumatic events, 9.5 percent reported three, 10.2 percent reported four or more, and 26.5 percent
reported only one such event. Among women, 13.5 percent of the total sample reported two
traumatic events, 5 percent reported three, 6.4 percent reported four or more, and 26.3 percent
reported only one.
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is another
large national survey of behavioral health, but it only assessed posttraumatic stress disorder
(PTSD) and trauma exposure in its second wave of interviews, in which 34,653 of the original
43,093 respondents were reinterviewed (Pietrzak, Goldstein, Southwick, & Grant, 2011a). In the
Wave 2 interview, respondents were asked about 27 different types of potentially traumatic
events; the most commonly reported traumatic events were serious illness or injury to someone
close (affecting 48.4 percent of those who did not have PTSD symptoms and 66.6 percent of
those with PTSD), unexpected death of someone close (affecting 42.2 percent of those without
PTSD and 65.9 percent of those with PTSD), and seeing someone badly injured or killed
(affecting 24 percent of those without PTSD and 43.1 percent of those with PTSD; Pietrzak,
Goldstein, Southwick, & Grant, 2011a). According to the same data, 71.6 percent of the sample
witnessed trauma, 30.7 percent experienced a trauma that resulted in injury, and 17.3 percent
experienced a trauma that was purely psychological in nature (e.g., being threatened with a
weapon; El-Gabalawy, 2011).
NESARC also found that exposure to specific traumatic events varied considerably according to
race, ethnicity, or cultural group. The survey found that 83.7 percent of non-Latino White
Americans reported a traumatic event, compared with 76.4 percent of African Americans, 68.2
percent of Latinos, and 66.4 of percent of Asian Americans, Native Hawaiians, or Pacific
Islanders (Roberts, Gilman, Breslau, Breslau, & Koenen, 2011). Exposure to specific traumas
also varied considerably. White Americans were more likely to report an unexpected death of
Trauma-Informed Care in Behavioral Health Services 1-3
someone they knew (44.7 percent did) than were African Americans (39.9 percent), Latinos
(29.6 percent), and Asian Americans, Native Hawaiians, or Pacific Islanders (25.8 percent) as
well as being more likely to report having a close friend/relative who experienced a life-
threatening injury. On the other hand, African Americans were the most likely to report being the
victim of assaultive violence (29.7 percent), followed by White Americans (26.1 percent),
Latinos (25.6 percent), and Asian Americans, Native Hawaiians, or Pacific Islanders (16.3
percent). In terms of combat trauma, White Americans and African Americans were about as
likely to have been combatants (10 percent of each group reported combat trauma), and more
likely than Asian Americans, Native Hawaiians, or Pacific Islanders (5.4 percent) or Latinos (4.4
percent). However, Asian Americans, Native Hawaiians, or Pacific Islanders were the most
likely to have been unarmed civilians in a war zone (7.5 percent), followed by Latinos (3.8
percent), White Americans (2 percent), and African Americans (1.9 percent).
Across the world, according to data from the World Health Organization (WHO) surveys, which
includes the NCS and NCS replication (NCS-R) and surveys from 20 other countries, the most
commonly reported traumas are the death of a loved one (30.5 percent), witnessing violence to
others (21.8 percent), and experiencing interpersonal violence (18.8 percent; Stein et al., 2010).
As Kessler (2000) noted, trauma from assaultive violence in the United States is likely to be
more common than in most other developed countries in general. However, trauma related to
other traumatic events (e.g., automobile accidents, natural disasters) appear to be quite similar
throughout developed countries.
A longitudinal survey from New Zealand also provides useful data on trauma exposure. In this
survey, a cohort of subjects from a single town was interviewed at age 26 and again at age 32 in
order to evaluate what constituted the worst trauma those individuals had experienced (Koenen,
Moffitt et al., 2008). The types of worst experiences reported before age 26 were:
Sudden unexpected death by trauma of a close family member or friend (38 percent).
Personal assault or victimization (32 percent).
Serious accidents (14 percent).
Hearing about or witnessing a close friend or relative experiencing an assault, serious
accident, or serious injury (12 percent).
Personal illness (3 percent).
Natural disaster (1 percent)
How Common Are Traumatic Stress Reactions?
As with trauma rates, PTSD rates vary considerably across different demographic groups. The
reader should consult the section titled “Extent and Effects of Trauma and Traumatic Stress
Reactions in Specific Populations” for more specific information on PTSD rates. More general
information from major surveys is included in this section.
The DSM-5 (APA, 2013) estimates that the prevalence rate of PTSD in the U.S. adult population
is about 8 percent, but studies of populations at high risk for PTSD (e.g., combat veterans,
survivors of natural disasters) have found PTSD rates ranging from 3 to 58 percent. The NCS
(which evaluated behavioral health disorders, including PTSD) found that, for Americans ages
15 to 54, the lifetime prevalence of PTSD (based on DSM Third Edition, text revision [DSM-III-
1-4 Part 3, Section 1—A Review of the Literature
R; APA, 1987] criteria) was 7.8 percent, with women more than twice as likely as men to have
the disorder during their lives (10.4 percent of women and 5 percent of men; Kessler et al.,
1995). In the NCS-R, which interviewed 9,282 individuals ages 18 and older between February
2001 and April 2003, the lifetime prevalence of PTSD was 6.8 percent, again with a much higher
rate for women (9.7 percent) than for men (3.6 percent; Kessler, Berglund et al., 2005; NCS,
2005). The past-year prevalence rate for PTSD was 3.5 percent, with 5.2 percent of women and
1.8 percent of men having PTSD in the 12 months prior to their interviews (Kessler, Chiu et al.,
2005).
Kessler, Berglund et al. (2005) examined the issue of lifetime prevalence in the NCS-R to
determine whether the prevalence statistics of the NCS were still valid in light of changes to the
diagnostic criteria that occurred with the publication of the DSM Fourth Edition, text revision
(DSM-IV-TR; APA, 2000). The study was divided into two parts. Part I included face-to-face
diagnostic interviews of 9,282 participants who were 18 years of age or older. Part II included
factors related to diagnosis (e.g., risk factors) and was completed only with participants from
Part I who had a “lifetime disorder” and a probability sample from other Part I participants
(n=5,692). Data analysis in this study estimated a lifetime PTSD prevalence of 6.8 percent, but
the authors also analyzed the data to determine projected lifetime risk and found that at age 75,
the lifetime risk for PTSD was 28 percent higher than the lifetime prevalence estimate. However,
the authors suggested that because of certain study limitations (e.g., related to sample
parameters, reluctance to participate or to disclose diagnoses), these results should be considered
a conservative estimate.
As noted earlier, Wave 1 of NESARC did not evaluate PTSD, but Wave 2 found that 6.4 percent
of the population (8.6 percent of women and 4.1 percent of men) had PTSD at some point during
their lives (Pietrzak et al., 2011a). NESARC researchers also evaluated lifetime prevalence of
partial PTSD (defined as including at least one symptom under Criteria B, C, and D, with
symptom duration of at least 1 month) and found that 6.6 percent of the total population (8.6
percent of women and 4.5 percent of men) met criteria for partial but not full PTSD at some
point during their lives. It should be noted, however, that most large behavioral health surveys,
such as the NCS and NESARC, rely on retrospective evaluation of symptoms, and some research
indicates that they underestimate behavioral health disorders compared with prospective
longitudinal studies (Moffitt et al., 2009). Differences in prevalence estimates may also be
related both to changes in PTSD diagnostic criteria and to a variety of methodological
differences in the research (e.g., different diagnostic instruments, procedures) on which these
estimates were based (Kessler, 2000; Kessler, Chiu et al., 2005; Kessler et al., 1995; Narrow,
Rae, Robins, & Regier, 2002).
It is also worth noting that delayed PTSD may account for a considerable percentage of PTSD
cases. A meta-analytic review that included studies in which individuals were assessed 1 to 6
months after trauma exposure and again at least 6 months later found that 24.8 percent of PTSD
cases involved delayed trauma (Smid, Mooren, van der Mast, Gersons, & Kleber, 2009). Studies
included in the review found between 3.8 and 83.3 percent of their samples had delayed PTSD.
Factors that were associated with significantly greater odds of having delayed rather than
nondelayed PTSD included a Western (as opposed to non-Western) cultural background and
military combat exposure.
Trauma-Informed Care in Behavioral Health Services 1-5
More recently, Smid, van der Velden, Gersons, and Kleber (2012) conducted a study of 1,083
individuals affected by a large fireworks disaster to evaluate delayed PTSD rates at both 18
months and 4 years after the disaster. In their review of prospective studies of disaster survivors,
they found that between 2 and 19 percent of survivors developed delayed PTSD, whereas in their
own study, 3.8 percent (n=24) of the total sample (n=636) who were available for all assessments
had delayed PTSD and 13.5 percent had PTSD that was not delayed.
What Is Complex Trauma?
An individual has been exposed to complex trauma when he or she has either experienced
repeated instances of the same type of trauma over a period of time or experienced multiple types
of trauma (van der Kolk, McFarlane, & Weisaeth, 1996). Expert consensus is that people who
have complex trauma will typically require more intensive and extensive treatment as well as
possible adaptations to standard treatment (see the expert clinician survey in Cloitre et al., 2011).
This Treatment Improvement Protocol (TIP) uses a definition of complex trauma developed by
the National Child Traumatic Stress Network (NCTSN; 2003), which defines complex trauma as
a “dual problem” involving both “exposure to traumatic events and the impact of this exposure
on immediate and long-term outcomes” (p. 5). NCTSN notes that complex trauma usually
involves multiple instances of trauma (occurring either simultaneously or sequentially) and
multiple forms of trauma (e.g., experiencing emotional abuse, sexual abuse, and physical abuse).
Also, complex trauma, such as that experienced by children who sustain repeated abuse,
typically results in emotional dysregulation and a lack of appropriate coping mechanisms, which
in turn can increase the risk of further traumatic experiences. Although the NCTSN definition
was developed for explaining childhood trauma, it can be adapted to fit an adult population.
Herman (1992) was among the first to highlight the inadequacy of existing diagnostic criteria for
PTSD for people who have complex trauma by pointing out that these criteria were developed
based on a clinical consideration of symptoms experienced by individuals who had survived
relatively time-limited traumatic experiences (e.g., combat veterans, survivors of rape). Herman
proposed that many individuals with a history of prolonged and repeated trauma (as opposed to
trauma that is time-limited or related to a single traumatic event) present with clinical
characteristics that “transcend simple PTSD” (p. 379); these characteristics include physical
symptoms (including many of the symptoms listed in the diagnostic criteria for PTSD, although
they may appear more “complex, diffuse, and tenacious” [p. 379]), personality changes in which
the individual’s sense of identity is negatively affected and which may inhibit the individual’s
ability to form relationships with others, and a propensity for vulnerability to further harm (by
self or others).
In 1992, Herman published the seminal work Trauma and Recovery (revised in 1997), which
discussed proposed changes to the next DSM that would include a new term for this trauma-
related constellation of symptoms. Her suggestion was the term “complex post-traumatic stress
disorder” (complex PTSD). However, none of the proposed changes she discussed were included
in the DSM-IV (APA, 1994), DSM-IV-TR (APA, 2000), or DSM-5 (APA, 2013). Jackson,
Nissenson, and Cloitre (2010) observed that the DSM-IV classification of “associated features
and disorders” (APA, 2000) for PTSD is intended to cover symptoms of complex PTSD (e.g.,
problems with affect regulation, impaired relationships), but it does not take into account one key
aspect of complex PTSD as it was originally defined, which is that such symptoms and disorders
1-6 Part 3, Section 1—A Review of the Literature
(e.g., substance abuse) are not viewed as secondary to PTSD symptoms, but rather, as equally
important and directly related to traumatic experiences.
Complex trauma is typically interpersonal and generally involves situations in which the person
who is traumatized cannot escape from the traumatic experiences because he or she is
constrained physically, socially, or psychologically (Herman, 1992). Because of this, people who
have experienced complex trauma often have additional disturbances in their ability to self-
regulate—beyond those seen in PTSD—that are not related to complex trauma. These include
difficulties in emotional regulation, difficulties in one’s capacity for relationships, problems with
attention or consciousness (e.g., dissociative experiences), a disturbed belief system, and/or
somatic complaints or disorganization (Briere & Scott, 2012; Cloitre et al., 2011; van der Kolk,
McFarlane, & Van der Hart, 1996).
What Is Acute Stress Disorder?
Acute stress disorder (ASD), according to the DSM-5, involves a traumatic stress reaction that
occurs within 1 month of trauma exposure and includes at least nine symptoms from any of the
five categories (intrusion, negative mood, dissociation, avoidance, and arousal; APA, 2013). To
receive this diagnosis, the individual also has to display a reaction that causes significant distress
or impairment in social, occupational, or other important areas of functioning. ASD can occur at
the time of the trauma exposure or any time within 4 weeks of that event As Roberts, Kitchiner,
Kendardy, and Bisson (2010) observed, there is a large degree of overlap between ASD and
PTSD symptoms, but what distinguishes them is the timing of those symptoms relative to trauma
exposure. Cardeña and Carlson (2011) provided a history of the ASD diagnosis and discussed
the validity of the diagnostic criteria. ASD can develop into PTSD if the symptoms extend
beyond 1 month.
What Is PTSD?
PTSD is a traumatic stress reaction that develops in response to a significant trauma. It is a
mental disorder, and for behavioral health providers in the United States, the currently accepted
diagnostic criteria for the disorder are those provided by the DSM-5 (APA, 2013). For
professionals in the field of behavioral health, the definition of psychological trauma is
historically and clinically tied to the diagnostic criteria for PTSD, which made their first
appearance in the DSM-III (APA, 1980). However, over the years, the diagnostic criteria have
undergone some significant changes. These changes are important factors to consider when
reading, evaluating, and especially comparing research.
Criterion A concerns the type of trauma involved; Criterion B describes symptoms of intrusion;
Criterion C includes the presence of persistent avoidance of stimuli associated with the trauma;
Criterion D highlights symptoms of negative alterations in cognitions and mood associated with
the traumatic event(s); Criterion E includes marked alterations in arousal and reactivity as it
relates to the trauma; Criterion F addresses the duration of the symptoms; and Criterion G
includes clinical distress or impairment in important areas of functioning (e.g., occupational).
The presenting symptoms cannot be attributable to the physiological effects of a substance,
including alcohol or medications.

Trauma-Informed Care in Behavioral Health Services 1-7
The first part of the evolving PTSD definition is Criterion A (Exhibit L-1), which describes
changes in the definition of a traumatic event from that of “a recognizable stressor,” to “an event
that is outside the range of usual human experience,” to an event that is defined by two specific
descriptors, to “exposure to actual or threatened death, serious injury, or sexual violence.”
Exhibit L-1
Evolution of Criterion A for PTSD in the DSM
DSM-III (1980) DSM-III-R (1987)
DSM-IV (1994) & DSM-IV-TR
(2000) DSM-5 (2013)
“Existence of
a
recognizable
stressor that
would evoke
significant
symptoms of
distress in
almost
everyone”
(APA, 1980,
p. 238).
“The person has
experienced an event
that is outside the
range of usual
human experience
[emphasis added] and
that would be
markedly distressing
to almost anyone”
(APA, 1987, p. 250;
examples given
include serious threat
or harm to self or
others).
“The person has been exposed
to a traumatic event in which
both of the following were
present [emphasis added]:
(1) the person experienced,
witnessed, or was confronted
with an event or events that
involved actual or threatened
death or serious injury, or a
threat to the physical integrity of
self or others.
(2) the person’s response
involved intense fear,
helplessness or horror” (APA,
1994, pp. 427–428; APA, 2000,
pp. 467–468).
“Exposure to actual
or threatened death,
serious injury, or
sexual violence”
(APA, 2013, p. 271).
There are four ways
that an individual can
experience the
traumatic event(s):
directly, witnessing
the event, learning
about the event, or
through repeated or
extreme exposure to
aversive details of the
traumatic event(s).
Criterion B has also evolved. In the DSM-III (APA, 1980), it described reexperiencing a trauma
through three symptoms: intrusive thoughts, recurrent dreams, or the feeling of reexperiencing
the trauma as a result of some sort of stimulus. DSM-III-R (APA, 1987) expanded Criterion B by
adding another symptom: “intense psychological distress at exposure to events that symbolize or
resemble an aspect of the traumatic event, including anniversaries of the trauma” (p. 250). It also
added information regarding symptom presentations that may occur in children (e.g., repetitive
play expressing aspects of the trauma). DSM-IV (APA, 1994) added a fifth symptom of
“physiological reactivity on exposure to internal or external cues that symbolize or resemble an
aspect of the traumatic event” (p. 428) and additional symptom presentations that may occur in
children (e.g., nightmares that lack recognizable features, reenactments of the trauma). Likewise,
DSM-5 (2013) became more developmentally focused in diagnostic criteria and added a separate
criterion for children younger than 7 years of age. Additional changes in the DSM-5 include a
more explicit definition of the stressor criterion, an additional and separate symptom cluster
highlighting avoidance and persistent negative alterations in cognitions and mood, and the
elimination of an individual’s subjective reaction to the traumatic event (intense fear,
helplessness, or horror).
Criterion C addresses avoidance of stimuli associated with the traumatic event(s). Criterion C
evolved between DSM-III and DSM-III-R (Exhibit L-2), with only minimal changes in language

1-8 Part 3, Section 1—A Review of the Literature
in the DSM-IV and DSM-IV-TR (APA, 1994; 2000). The DSM-5 dropped the terminology of
numbing of general responsiveness in this criterion’s heading (APA, 2013).
Exhibit L-2
Evolution of Criterion C for PTSD in the DSM
DSM-III (1980) DSM-III-R (1987) DSM-5 (2013)
“Numbing of
responsiveness to
or reduced
involvement with the
external world,
beginning sometime
after the trauma, as
shown by at least
one of the following:
(1) markedly
diminished interest
in one or more
significant activities
(2) feeling of
detachment or
estrangement from
others
(3) constricted
affect” (APA, 1980,
p. 238).
“Persistent avoidance of stimuli associated
with the trauma or numbing of general
responsiveness (not present before the
trauma), as indicated by at least three of the
following:
(1) efforts to avoid thoughts or feelings
associated with the trauma
(2) efforts to avoid activities or situations
that arouse recollections of the trauma
(3) inability to recall an important aspect of
the trauma (psychogenic amnesia)
(4) markedly diminished interest in
significant activities (in young children, loss
of recently acquired developmental skills
such as toilet training or language skills)
(5) feeling of detachment or estrangement
from others
(6) restricted range of affect, e.g., unable to
have loving feelings
(7) sense of a foreshortened future, e.g.,
does not expect to have a career, marriage,
or children, or a long life” (APA, 1987, p.
250).
“Persistent avoidance of
stimuli associated with the
traumatic (event(s),
beginning after the
traumatic event(s)
occurred, as evidenced by
one or both of the
following:
(1) Avoidance of or efforts
to avoid distressing
memories, thoughts, or
feelings about or closely
associated with the
traumatic event(s).
(2) Avoidance of or efforts
to avoid external
reminders ( people,
places, conversations,
activities, objects,
situations) that arouse
distressing memories,
thoughts, or feelings
about or closely
associated with the
traumatic event(s)” (APA,
2013, p. 272).
Criterion D addresses symptoms related to negative alterations in cognitions and mood
associated with the traumatic event(s). This symptom cluster is a new addition to DSM-5 and
includes “irritable behavior and angry outbursts (with little or no provocation), typically
expressed as verbal or physical aggression toward people or objects; reckless or self-destructive
behavior; hypervigilance; exaggerated startle response; problems with concentration; sleep
disturbance (e.g., difficulty falling or staying asleep or restless sleep)” (APA, 2013, p. 272). In
prior DSM publications, criterion D related to increased arousal (e.g., difficulties with sleep and
concentration). In DSM-5, this criterion has moved to Criterion E, with no other changes in
symptoms. This criterion has also evolved from the description in the DSM-III to a more concise
description in the DSM-III-R, and it has become even more concise in the DSM-IV, DSM-IV-
TR, and DSM-5 (Exhibit L-3).

Trauma-Informed Care in Behavioral Health Services 1-9
Exhibit L-3
Evolution of Criterion E for PTSD in the DSM
DSM-III (1980) DSM-III-R (1987)
DSM-IV (1994),DSM-IV-
TR (2000), and DSM-5
(2013)
“At least two of the following
symptoms that were not present
before the trauma:
(1) hyperalertness or
exaggerated startle response
(2) sleep disturbance
(3) guilt about surviving when
other have not, or about
behavior required for survival
(4) memory impairment or
trouble concentrating
(5) avoidance of activities that
arouse recollection of the
traumatic event
(6) intensification of symptoms
by exposure to events that
symbolize or resemble the
traumatic event” (p. 238)
“Persistent symptoms of
increased arousal (not present
before the trauma), as
indicated by at least two of the
following:
(1) difficulty falling or staying
asleep
(2) irritability or outbursts of anger
(3) difficulty concentrating
(4) hypervigilance
(5) exaggerated startle response
(6) physiologic reactivity upon
exposure to events that
symbolize or resemble an aspect
of the traumatic event (e.g., a
woman who was raped in an
elevator breaks out in a sweat
when entering any elevator)” (p.
250)
“Persistent symptoms of
increased arousal (not
present before the
trauma), as
indicated by two or more
of the following:
(1) difficulty falling or
staying asleep
(2) irritability or outbursts
of anger
(3) difficulty
concentrating
(4) hypervigilance
(5) exaggerated startle
response” (p. 428, p.
468, and p. 272,
respectively).
A time criterion was added in the DSM-III-R (APA, 1987) to specify a minimum timeframe of 1
month or more for experiencing symptoms in Criteria B, C, D, and E. In the DSM-IV (APA,
1994), DSM-IV-TR (APA, 2000), and DSM-5 (APA, 2013), this criterion was retained, with the
slight change of requiring more than 1 month of symptoms (APA, 1994; 2000, 2013). The
criterion that addresses the level of distress and functioning was not included until the
publication of the DSM-IV (APA, 1994) and has remained the same in the DSM-5 (APA, 2013).
This criterion added a new defining characteristic, which specifies that “the disturbance causes
clinically significant distress or impairment in social, occupation, or other important areas of
functioning” (APA, 2013, p. 272).
Turnbull (1998) describes the historical development of the idea of PTSD up to its inclusion in
the International Statistical Classification of Diseases and Related Health Problems, 9th
Revision (1979) and the DSM-III-R. The DSM-5 recognizes certain specifiers that may further
characterize PTSD (APA, 2013). For example, a specific case of PTSD may be with delayed
expression (full criteria are not met until at least 6 months have passed since the trauma
exposure, although the onset of symptoms may immediately follow the trauma; APA, 2000;
2013).
1-10 Part 3, Section 1—A Review of the Literature
What Is Partial PTSD?
Partial PTSD is a category developed by researchers to evaluate people who have some
impairment related to elevated PTSD symptoms but do not meet full criteria for the disorder. The
term is commonly defined as either having at least one PTSD symptom from Criteria B, C, and
D that lasts at least 1 month after a traumatic event (Criterion A) or as meeting Criterion A plus
two of the other three criteria (Mylle & Maes, 2004). These authors also reviewed studies about
the prevalence of partial PTSD according to both criteria. Partial PTSD has been associated with
several of the same negative consequences associated with full PTSD, but not to the same extent
as a full PTSD diagnosis (e.g., Pietrzak et al., 2011a).
What Is TIC?
In the past 15 years, there have been many definitions of TIC and various models for
incorporating it across organizations. This TIP uses SAMHSA’s definition of TIC, which
describes this type of care involving “these key elements: (1) realizing the prevalence of trauma;
(2) recognizing how trauma affects all individuals involved with the program, organization, or
system, including its own workforce; and (3) responding by putting this knowledge into practice”
(SAMHSA, Trauma and Justice Strategic Initiative, 2012, p. 4). In a seminal article on the
development of a trauma-informed service system, Harris and Fallot (2001) proposed that such a
system is one in which administrators and staff understand how traumatic experiences negatively
affect behavioral health in multiple ways and are committed to responding to those needs
through universal trauma screening, staff education and training regarding trauma and its effects,
and willingness to review and change policies and procedures to prevent the (re)traumatization
of clients.
As part of the overall review of policies, practices, and research involving trauma-informed
services for individuals who are homeless, Hopper, Bassuk, and Olivet (2010) reviewed the
literature and organizational principles on TIC and found several common themes. These
included an awareness of how symptoms and behaviors are related to traumatic experiences, an
emphasis on safety, an opportunity for individuals to develop or regain a sense of control over
their lives, and an emphasis on strengths rather than on deficiencies. They used these themes to
develop the following definition of TIC (Hopper, Bassuk, & Olivet, 2010, p. 82):
Trauma-Informed Care is a strengths-based framework that is grounded in an understanding of
and responsiveness to the impact of trauma, that emphasizes physical, psychological, and
emotional safety for both providers and survivors, and that creates opportunities for survivors to
rebuild a sense of control and empowerment.”
Other definitions of TIC exist, and Hopper and colleagues (2010) reviewed some of the better-
known versions of these and presented them in a table (see Exhibit L-4) for easy comparison.

Trauma-Informed Care in Behavioral Health Services 1-11
Exhibit L-4
Principles of TIC
Example Definitions of Trauma-Informed Care
Common Principles Across Definitions
Community
Connections:
Five Guiding
Principles for
Trauma-
Informed
Services
NASMHPD:
a
Criteria for
Building a Trauma-
Informed Mental
Health Service
System
NCTSN:
b
Principles of
Trauma-
Informed
Care for
Children
NCFH:
c
Operating
Principles for
Trauma-
Informed
Organizational
Self-
Assessment
WCDVS:
d
Trauma-
Informed or Trauma-
Denied: Principles&
Implementation of
Trauma-Informed
Services for Women
Consensus-Based Principles
Theory-Based
Expert Trauma Panel
Experts
Theory-Based
Research-Based
1. Trauma Awareness
a. Program
philosophy
and mission
Trauma function/
focus; trauma policy
or position; financing
for best practices;
trauma- informed
services; clinical
practice guidelines for
people with trauma
histories; trauma-
informed disaster
planning; systems
integration; research
& data on trauma &
evidence-based &
best- practice
treatment models;
access to evidence-
based & best-practice
trauma treatment
Recognize the impact
of trauma on
development and
coping
b. Staff
education,
training, and
consultation
Workforce
orientation,
training, support,
competencies and
job standards
related to trauma;
promote education
of professionals in
trauma
Emphasize trauma
recovery as a primary
goal
c. Practices
Trauma screening
and assessment;
Trauma- specific
services, including
evidence-based and
emerging best-
practice treatment
models
Integration
(symptoms such
as adaptive
coping,
integrating
services,
trauma-specific
services)
d. Recognition
of vicarious
trauma and staff
self- care
2. Safety
a. Physical and
emotional
safety
Safety
(physical
and
emotional)
Maintaining
clear and
consistent
boundaries
Safety, basic
needs,
consistency,
and
predictability
Create an
atmosphere of safety,
respect, and
acceptance
b.
Relationships:
authentic,
respectful,
clear
boundaries
Trustworthiness
(clear tasks,
consistent
practices, staff-
consumer
boundaries)
[see
Delivering
services
below]
Engagement:
respectful
nonjudgmental
relationships,
clear
boundaries
Use a relational
collaboration model.
Growth is fostered by
mutual, respectful,
authentic relationships

1-12 Part 3, Section 1—A Review of the Literature
c. Avoid
retraumatization
Procedures to avoid
retraumatization and
reduce impacts of
trauma
Minimize
retraumatization
d. Acceptance of
and respect for
diversity
Trauma policies and
services that respect
culture, race
ethnicity, gender,
age, sexual
orientation, disability,
and socioeconomic
status
Delivering
services in a
nonjudgmental
and respectful
manner
Cultural
competence
Work towards cultural
competence,
understand contextual
factors
3. Choice &
Empowerment
a. Choice and
control
Choice: maximize
consumer choice
and control
Consumer/trauma
survivor/ recovering
person involvement
and trauma-informed
rights
Maximizing
choice and
control for
participants
Consumer
control, choice
and autonomy
Underscore consumers’
choice and control over
recovery
b. Empower
ment model
Empowerment:
prioritize
consumer
empowerment,
skill-building, and
growth
Avoiding
provocation
and power
assertion
Open
communication:
provide
information
openly to
consumers
Use an empowerment
model
c. Consumers
nvolved in
service
development and
evaluation
Collaboration:
maximize
collaboration and
sharing of power
between staff and
consumers
Sharing power
in the running
of shelter
activities
Shared power
and governance
Involve consumers in
design and evaluation of
services
4. Strengths- based
Focus on
strengths,
resiliency
[see
Empowerment
above]
Healing, instill-
ing hope
Highlight consumers’
strengths, adaptations,
and resiliencies
Source: Hopper, Bassuk, & Olivet, 2010. Adapted with permission.
a
NASMHPD= National Association of State Mental Health Program Directors.
b
NCTSN = National Child Traumatic Stress Network.
c
NCFH = National Center on Family Homelessness.
d
WCDVS = Women, Co-Occurring Disorders and Violence Study.
Elliott, Bjelajac, Fallot, Markoff, and Reed (2005) discussed TIC within the context of services
for women and suggested some guiding principles for such services; they also briefly reviewed
literature in support of those principles.
What Is the Relationship of Culture to Traumatic Stress Reactions?
Although cultural responses to trauma may vary, high PTSD rates have been diagnosed in a wide
range of cultures following exposure to a significant traumatic event, including Ju’hoansi (i.e.,
Kalahari Bushmen) exposed to domestic violence, Cambodians who lived through the Khmer
Rouge regime, survivors of the Rwandan genocide, and Filipinos who experienced a large-scale
natural disaster (Marques, Robinaugh, LeBlanc, & Hinton, 2011). Neurobiological research also
indicates that affect dysregulation, changes in right hemisphere functioning, and a kindling
phenomenon occurs across cultures in individuals who have PTSD or a prolonged stress reaction
as the result of trauma exposure (Wilson, 2007).
Marsella and Christopher (2004) observed that intrusive PTSD symptoms appear to be more
common cross-culturally than symptoms of avoidance or the reexperiencing of trauma and that
the occurrence of the two latter categories of symptoms may vary considerably across cultures.
Other international research indicates that the presentation and occurrence of specific PTSD
Trauma-Informed Care in Behavioral Health Services 1-13
symptoms and the rates of other mental disorders and/or symptoms following trauma vary
considerably among nations/cultural groups (Marques et al., 2011). For example, research
conducted with Vietnamese survivors of a typhoon found that both depression and panic disorder
appeared to be more common responses to the trauma than PTSD (Amstadter et al., 2009). Other
studies conducted with Vietnamese (Hinton et al., 2001) and Cambodian (Hinton, Ba, Peou, &
Um, 2000) refugees have also found high rates of panic disorder/panic attacks co-occurring with
PTSD among trauma survivors.
Members of some cultural groups may also have increased risk for PTSD, or for certain PTSD
symptoms, compared with members of other groups. Research from the United States suggests
that Latinos have greater risk for PTSD when trauma exposure is controlled for than African
Americans, White Americans, or Asian Americans (e.g., see Marshall, Schell, & Miles, 2009). A
study conducted in the Netherlands with a diverse group of individuals affected by an airline
disaster found that those who came from non-Western cultures (n=379) experienced significantly
more health-related anxieties, more severe PTSD symptoms, more fatigue, and more impaired
health-related quality of life than did those from Western cultures (n=406; Verschuur, Maric, &
Spinhoven, 2010). Other research conducted with refugees in Finland who were survivors of
torture (N=78) found that those from southeastern European cultures had significantly more
PTSD symptoms than did those from Middle Eastern, Central African, or Southern Asian
cultures (Schubert & Punamäki, 2011).
Marsella (2010), as part of a review of the ethnocultural aspects of PTSD, noted that culture may
affect individuals’ responses to trauma by providing meaning to symptoms (e.g., nightmares), by
shaping individuals’ beliefs about traumatic events (e.g., through different concepts of destiny or
fate), by affecting individuals’ beliefs about their own responsibility for the trauma and their
subsequent response, by indicating what disabilities or impairments may result from the trauma,
and by shaping the threshold for normal versus pathological levels of arousal (e.g., through
perceptions and interpretations of stressors). He also indicated that cultural beliefs may be used
to help heal maladaptive responses to trauma. Hoshmand (2007) reviewed research that
suggested the importance of understanding cultural sources of strength/resilience when
interpreting trauma from a cultural perspective.
Because of these differences, members of certain cultural groups may not present symptoms in a
manner that can be easily identified as PTSD or another behavioral health disorder. For instance,
clinicians working with Cambodian refugees have observed that traumatic memories in the form
of flashbacks or nightmares may be interpreted as attacks by dead spirits, whereas hyperarousal
symptoms may indicate a physical or spiritual weakness (Hinton, Hinton, Pich, Loeum, &
Pollack, 2009; Hinton, Park, Hsia, Hofmann, & Pollack, 2009). Hoshmand (2007) recommended
taking an ecological approach to interpreting trauma, which means that traumatic experiences
and trauma responses are interpreted within the context of the individual’s culture and with
respect to other factors (e.g., gender, age) that might shape those responses.
Role of acculturation
Another relevant concern is the degree to which acculturation affects responses to trauma.
Research in this area is limited, but the preponderance of evidence seems to indicate that greater
acculturation is associated with lower levels of PTSD symptoms (Dunlavy, 2010). This is
contrary to the evidence relating acculturation, for some immigrant groups, to certain other
1-14 Part 3, Section 1—A Review of the Literature
behavioral health problems, notably substance abuse and depressive symptoms (e.g., Alegría et
al., 2008; Gonzalez & Gonzalez, 2008; Grant et al., 2004; Xie & Greenman, 2005). In her own
data analysis concerning African immigrants to Sweden, however, Dunlavy found no significant
associations between acculturation and PTSD symptoms.
A large study in this area was conducted in the Netherlands with a group of 221 immigrants
affected by a large fireworks explosion and a matched group of 127 immigrants unaffected by
the disaster (Drogendijk, van der Velden, & Kleber, 2012). The study found that lower
acculturation (assessed with the Lowlands Acculturation Scale [LAS]) was associated with
increased behavioral health problems for individuals who had experienced this trauma but not for
those in the control group. Specifically, a greater need to keep the norms and values of one’s
original culture (measured with a subscale of the LAS) was significantly associated with more
intrusion and avoidance symptoms (indicative of PTSD), anxiety, depression, hostility, and
somatic complaints for those affected by this trauma. For those unaffected, acculturation had no
significant association with behavioral health measures, nor were other domains of acculturation
significantly associated with PTSD symptoms, although having skills to cope with a new
culture/society and feeling socially integrated into that society were associated with better
outcomes in the other areas of behavioral health measures. The authors observed that their
findings may indicate that, in the context of a disaster affecting large numbers of people, a lack
of flexibility in terms of cultural norms and values may be a source of additional stress.
The role of acculturation vis-à-vis PTSD, however, may vary according to cultural group and the
predominant culture’s relationship to that group (e.g., it may be different for immigrant and
indigenous populations). For example, a study conducted in Taiwan with members of an
aboriginal group affected by an earthquake (N=196) found that lower levels of acculturation to
mainstream Taiwanese culture were associated with significantly higher levels of PTSD
symptoms following the disaster (Lee et al., 2009). Other studies indicate that a domain from the
Demographic and Post-Migration Living Difficulty Questionnaire labeled “difficulties adjusting
to cultural life” in a new society was also associated with greater PTSD symptom severity among
refugees in studies in Australia (Schweitzer, Melville, Steel & Lacherez, 2006) and the United
Kingdom (Carswell, Blackburn, & Barker, 2011). This domain, which evaluates feelings of
isolation, loneliness, boredom, and a lack of access to preferred foods, may also represent
difficulties in acculturation, as the sense of isolation may be greater among less acculturated
refugees who are not able to establish social connections in their new culture.
For immigrants/refugees, better acquisition of the language of their new country, which may also
represent greater acculturation, has also been associated with significantly lower levels of PTSD
symptoms among Iraqi refugees living in Sweden (N=48) but not with significant differences in
rates of PTSD diagnosis (Söndergaard & Theorell, 2004). Similarly, a study of Burmese refugees
living in Australia (N=70) found a significant association between postmigration living
difficulties, of which concern about communication problems was the most often-cited example,
and PTSD symptoms (Schweitzer, Brough, Vromans, & Asic-Kobe, 2011).
Schweitzer and colleagues (2006), in their study of 63 Sudanese refugees in Australia, also found
that support from family and others within a Sudanese community was a significant resilience
factor with regard to behavioral health, whereas social support from the larger Australian society
Trauma-Informed Care in Behavioral Health Services 1-15
was not. The planned TIP, Improving Cultural Competence (SAMHSA, planned c), includes
more information on the role of acculturation in behavioral health disorders and their treatment.
Types of Trauma
There are numerous forms and types of trauma. In this section, the research reviewed explores a
wide variety of traumas; however, the sheer volume of research available precludes a thorough
review of each trauma type. In addition, the order of appearance in this document does not
denote a specific trauma’s importance or prevalence, nor is a lack of relevance implied if a given
trauma is not specifically addressed in this TIP. The intent of this section is to give the reader a
broad science-based perspective on the types of trauma.
Adverse Childhood Experiences
Adverse childhood experiences (ACEs), often referred to as early childhood or interpersonal
trauma, are childhood experiences that can have a negative effect on an individual’s well-being
that often lasts into adulthood. These experiences include child abuse and neglect as well as
substance abuse and mental illness in the family, having a family member incarcerated, and
violence directed toward a parent (usually the mother; Dube et al., 2005). ACEs are associated
with significant increases in a number of negative social, behavioral health, and physical health
outcomes, including alcohol and drug use disorders, depression, suicidality, risky sexual
behavior, sexual victimization in adulthood, domestic violence, self-harm behaviors, physical
inactivity, obesity, heart disease, cancer, liver disease, sexually transmitted diseases, teen
pregnancy, homelessness, unemployment, and being both a perpetrator and/or a victim of
interpersonal violence (Dietz et al., 1999; Felitti et al., 1998; Herman, Susser, Struening, & Link,
1997; Hillis, Anda, Felitti, Nordenberg, & Marchbanks, 2000; Lalor & McElvaney, 2010; Noll,
Horowitz, Bonanno, Trickett, & Putnam, 2003; Roberts, McLaughlin, Conron, & Koenen, 2011;
Tam, Zlotnick, & Robertson, 2003).
Childhood trauma also appears to be more likely to result in PTSD than trauma experienced in
adulthood. Wrenn and colleagues (2011), using a largely African American, inner-city sample of
people who had experienced trauma (N=767), found that childhood trauma was associated with
significantly greater PTSD risk than trauma experienced in adulthood alone. Childhood abuse
was associated with even greater risk than other trauma experienced in childhood.
A major study evaluating the effects of ACEs was conducted with 17,421 members of a large
health maintenance organization (HMO) in California in collaboration with the Centers for
Disease Control and Prevention (Dube et al., 2005). Two rounds of questionnaires were given,
with 7,641 respondents completing both assessments (Edwards, Anda, Felitti, & Dube, 2004). In
the initial assessment, 29.9 percent of men and 27 percent of women reported experiencing
physical abuse as children; 24.7 percent of women and 16 percent of men, sexual abuse; and 13.1
percent of women and 7.6 percent of men, emotional abuse (Dube et al., 2005). Also, 29.5
percent of women and 23.8 percent of men reported parental substance abuse, 23.3 percent of
women and 14.8 percent of men reported parental mental illness, and 13.7 percent of women and
11.5 percent of men reported violence directed toward their mothers.
The NCS and NCS-R evaluated a similar group of 12 experiences, labeled childhood adversities
(CAs), which included parental death, parental divorce/separation, life-threatening illness, and
1-16 Part 3, Section 1—A Review of the Literature
extreme economic hardship in addition to the experiences included in the ACE study (Green et
al., 2010). In this sample, 8.4 percent reported childhood physical abuse; 6 percent, sexual abuse;
5.6 percent, neglect; 14 percent, family violence; 10.3 percent, parental mental illness; 8.5
percent, parental substance abuse; and 5.8 percent, life-threatening illness (Green et al., 2010).
In a multivariate model, almost all of the CAs evaluated in the NCS were associated with
increased odds of having a mental disorder; the strongest associations were with parental mental
illness, parental substance abuse, family violence, childhood physical abuse, childhood sexual
abuse, and life-threatening illness (Green et al., 2010). These data also show a significant
association between certain CAs (i.e., parental mental illness, substance abuse in the family,
family violence, childhood physical/sexual abuse, childhood neglect, economic hardship) and the
persistence of mental disorders (McLaughlin, Green, Gruber et al., 2010a). The associations of
single trauma to mental disorders were modest, but multiple traumas had a cumulative effect, so
that exposure to multiple CAs further increased the strength of the association with both onset
and persistence of mental disorders. These same CAs were also significantly associated with
functional impairment related to behavioral health disorders (McLaughlin et al., 2010b).
Another large study, the Developmental Victimization Survey, investigated forms of childhood
abuse and maltreatment in 2,030 children and adolescents ages 2 to 17. The study found that 13.8
percent had sustained some form of maltreatment in the year of the survey; 10.3 percent,
psychological/emotional abuse; 3.6 percent, physical abuse; 1.4 percent, neglect; and 0.6 percent,
sexual abuse (Finkelhor, Ormord, Turner, & Hamby, 2005). However, some literature indicates
that all these data underrepresent the extent of childhood abuse and neglect, as both research and
expert opinion indicate that these traumas are generally underreported (see review by Gilbert et
al., 2009).
Gilbert and colleagues (2009) specifically reviewed data on psychological abuse, which is not
often evaluated in the literature. They found that approximately 10 percent of children in the
United States and the United Kingdom experience psychological abuse in any given year, and
between 4 and 9 percent sustain severe emotional abuse. Children who have sustained one type
of abuse or neglect are likely to have experienced other types as well, according to research
conducted with a variety of samples (see reviews by Edwards et al., 2003; Gilbert et al., 2009).
Research indicates that women are much more likely to sustain sexual abuse than men. Some
studies have found that men are more likely than women to sustain physical abuse in childhood
(e.g., Dube et al., 2005), whereas others did not find significant differences (e.g., Finkelhor et al.,
2005). Although childhood sexual abuse is more common for women than for men, research
evaluating outcomes for both genders has, for the most part, found similar long-term
consequences for men and women (Banyard, Williams, & Siegel, 2004; Dube et al., 2005).
Research also indicates that children living in households with yearly incomes of $20,000 or less
(in 2003–2004) are significantly more likely than children from other households to experience
psychological/emotional abuse, but not physical or sexual abuse (Finkelhor et al., 2005).
According to the same study, children from low-income families are also significantly more
likely to witness domestic violence and violence in their communities, and they are significantly
more likely to sustain violent assault or rape not perpetrated by a family member. Other research
has also found that children who are maltreated, especially those who sustain physical abuse, are
Trauma-Informed Care in Behavioral Health Services 1-17
more likely to be exposed to violence in their communities and to witness domestic violence;
these latter traumatic experiences have specific negative effects on children’s functioning beyond
those associated with abuse/neglect (Lynch & Cicchetti, 1998).
Different types of childhood abuse may have different behavioral health effects. In a study of
196 clients in treatment for alcohol dependence, a history of emotional abuse in childhood was
associated with a significant increase in risk for mood disorders (especially major depression)
and PTSD, physical abuse in childhood was associated with a significant increase in suicide
attempts, and sexual abuse in childhood was associated with significant increases in risk for
anxiety disorders, including PTSD (Huang, Schwandt, Ramchandani, George, & Heilig, 2012).
A study of 140 women found that those who experienced sexual abuse in childhood were
significantly more likely to engage in self-harm behaviors, those who sustained emotional abuse
were significantly more likely to be victims of sexual assault/rape in adulthood, and those who
were neglected in childhood were significantly more likely to be victims of physical abuse in
adulthood (Noll et al., 2003).
More so than other ACEs, physical and sexual abuse in childhood are associated with even
greater and more lasting problems, including significantly higher rates of depression, substance
use disorders, and PTSD in later life (see review by Gilbert et al., 2009). In addition, Gilbert and
colleagues (2009) found strong evidence linking childhood abuse with suicide attempts, high-risk
sexual behavior, criminal behavior, and obesity. As one seminal article on the effects of
childhood trauma observes, “deficits in virtually all of the major tasks of development” can
result from such abuse in childhood (Lynch & Cicchetti, 1998, p. 238). A more recent analysis of
NCS-R data that controlled for other anxiety disorders, depression, and demographic factors also
found that childhood sexual abuse was associated with significantly greater risk for social
anxiety disorder (SAD), panic disorder, and generalized anxiety disorder (GAD), in addition to
PTSD, in adulthood (Cougle, Timpano, Sachs-Ericsson, Keough, & Riccardi, 2010). Physical
abuse in childhood, however, was only associated with significantly higher risk for specific
phobias and PTSD.
Abuse during childhood also appears to predispose individuals to further abuse and trauma as
they grow older. Sexual abuse in childhood and the severity of such abuse have been shown in a
number of studies to be significantly associated with a greater risk for sexual abuse in adulthood
(see review by Classen, Palesh, & Aggarwal, 2005). Physical abuse in childhood, to a lesser
degree, is also associated with an increased risk for sexual abuse in adulthood (Classen et al.,
2005). Women who were physically abused as children are at greater risk for being victims of
domestic violence, whereas men who were physically abused are at greater risk for being
perpetrators of domestic violence (Whitfield, Anda, Dube, & Felitti, 2003). This study, which
used data from the ACE study described previously, did not assess the relationship of child abuse
to violence perpetrated by women or sustained by men.
In addition to likely contributing to behavioral health disorders, childhood abuse may also affect
behavioral health treatment outcomes. Research conducted with 146 women who were homeless
and had substance use disorders found that those who had histories of childhood abuse (physical,
sexual, and/or emotional) had significantly worse outcomes in terms psychological functioning
(assessed with multiple instruments) and substance abuse (assessed with an instrument derived
from the Addiction Severity Index [ASI]; Sacks, McKendrick, & Banks, 2008). More
1-18 Part 3, Section 1—A Review of the Literature
information on the relationship between childhood abuse/neglect and substance abuse in
adulthood can be found in TIP 36, Substance Abuse Treatment for Persons With Child Abuse and
Neglect Issues (Center for Substance Abuse Treatment [CSAT], 2000).
Ford (2009) reviewed the neurobiological and development research that helps explain how
trauma experienced in childhood can affect the brain and how those effects may continue
throughout a person’s lifetime (see also earlier work, Anda et al., 2006). More recent studies
confirm this research. As one example, Dannlowski and colleagues (2012) found strong
associations between childhood maltreatment (assessed retrospectively using the Childhood
Trauma Questionnaire) and both decreased gray-matter volume in a number of areas of the brain
and increased response in the amygdala upon seeing pictures of threatening facial expressions.
Schumm, Briggs-Phillips, and Hobfoll (2006) reviewed three theories on why sexual abuse in
childhood has extensive and lasting negative effects: these individuals develop a generalized fear
response as a result of their inability to control or predict abuse, and this leaves them unable to
emotionally engage in interpersonal relationships; they feel worthless and perceive others as
disapproving of them; and/or they become easy targets for exploitative social networks, which
further harm their ability to trust. The authors noted that these patterns together may contribute to
problems with interpersonal relationships, which in turn affect behavioral health.
Disasters/Mass Trauma
Large-scale traumatic events like natural disasters (e.g., earthquakes, hurricanes), human
disasters (e.g., chemical spills, nuclear accidents), and terrorist attacks have unique effects
because of the number of people affected and the fact that whole communities/populations may
experience consequences (Norris, Friedman, & Watson, 2002). In addition to affecting
behavioral health, such traumatic events often involve multiple losses, including the loss of lives
(of friends and family), home, occupation/employment, health/physical well-being, and even
one’s worldview (such events may affect one’s sense of security or beliefs about the justice of
the world; Walsh, 2007).
Not all disasters/mass trauma incidents appear to have the same effect on people’s behavioral
health. In their review of 160 studies of mass trauma events, Norris and colleagues (2002) found
that rates of serious psychological impairment (measured with a number of different instruments)
were significantly higher for individuals who endured trauma from mass violence (e.g., terrorist
attacks) than for those who experienced a technological or natural disaster. Severe impairment
was also more common if the event occurred in a developing (rather than developed) country,
and, in most studies, if the individual who experienced the event was female rather than male.
DiGrande, Neria, Brackbill, Pulliam, and Galea (2010) assessed PTSD symptoms for 3,271
individuals evacuated from the World Trade Center on 9/11 by phone interview (and by face-to-
face interview for 5 percent of the sample) 2 to 3 years after the event. They found that 95.6
percent had at least one PTSD symptom and 15 percent had probable PTSD according to their
scores on the PTSD Checklist (PCL), Stressor-Specific Version. Specific experiences associated
with significantly higher odds for PTSD included witnessing a horrific incident (e.g., the airplane
hitting the towers, people falling from the building, people who were injured or killed), being
injured in the attack, being exposed to the dust cloud that resulted from the building collapse,
being above the impact zone when the attack occurred, and evacuating later rather than earlier.
Trauma-Informed Care in Behavioral Health Services 1-19
Another study of people affected by the 9/11 attacks that used a national sample (n=933
respondents to the 2-month follow-up assessment; n=787 respondents to the 6-month
assessment) and a Web-based survey also found that 17 percent reported at least one ASD/PTSD
symptom 2 months after the 9/11 attack; 5.8 percent reported at least one symptom 6 months
after the attack (Silver, Holman, McIntosh et al., 2002). Individuals were significantly more
likely to report symptoms if they were female, were separated/divorced/widowed, had a
diagnosed depressive or anxiety disorder, had a physical illness, had disengaged from coping
efforts, and/or had greater exposure to the actual attacks. The authors concluded that individuals
need not be directly exposed to mass trauma events for those events to have a negative effect on
their behavioral health.
Norris and colleagues (2002) reviewed information on risk and protective factors associated with
behavioral health disorders and symptoms for survivors of natural disasters and those caused by
people drawn from 160 studies published between 1981 and 2001. For the most part, these are
the same as found with other populations of trauma survivors, with possible exceptions being the
presence of children, which is a risk factor for anxiety in mothers involved in disasters (fathers
were not studied in the four articles reviewed), and the loss of material resources, which has been
found to be a risk factor for behavioral health disorder symptoms in survivors of disasters but is
rarely evaluated in studies involving other types of trauma. Such losses also appear to have a
greater effect on older adults involved in disasters (see the “People in Specific Age Groups”
section).
Domestic Violence/Intimate Partner Violence
Domestic violence or intimate partner violence, also referred as interpersonal trauma, is a major
source of trauma for women (and can affect men as well) and carries with it a high risk for PTSD
(Coker, Weston, Creson, Justice, & Blakeney, 2005). Between 2001 and 2005, intimate partner
violence accounted for 21.5 percent of nonfatal violence against women and 3.6 percent of
violence against men (Catalano, 2012). Rates of domestic violence are high for people with
behavioral health disorders, especially people with substance use disorders.
Coker and colleagues (2005) evaluated data regarding links between intimate partner violence
and PTSD taken from the National Violence Against Women Survey, a large national household
survey of 8,000 women and 8,000 men conducted in the mid-1990s (see Tjaden & Thoennes
[2000] for more information on the study). Among a subsample of men and women who were
survivors of intimate partner violence (368 women, 185 men), PTSD rates were high, with 24
percent of the women and 20 percent of the men having moderate to severe levels of PTSD
symptoms, indicating possible current PTSD (although rates of possible PTSD were higher for
women, the difference between genders was not significant). The authors also found that higher
socioeconomic status (SES), current marriage, and the cessation of intimate partner violence
were all associated with significantly lower odds of having elevated PTSD symptoms.
Research from Spain suggests a dose–response relationship between intimate partner violence
and PTSD (Pico-Alfonso, 2005); although physical, sexual, and psychological abuse from
partners were all significantly related to PTSD, the latter had the strongest relationship.
1-20 Part 3, Section 1—A Review of the Literature
Political Violence/Torture
Trauma from political violence and torture varies considerably across the globe and is common
among some refugee groups (Johnson & Thompson, 2008). Histories of torture are also common
among smaller populations, such as former prisoners of war (Engdahl, Dikel, Eberly, & Blank,
1997). Accurate data on the prevalence of such trauma in the United States is difficult to obtain,
because most major surveys do not inquire specifically about it.
Because of the high degree of interpersonal violence involved, political violence and torture
often result in traumatic stress reactions that pose particular problems for providers in terms of
treatment and assessment. In Steel and colleagues’ (2009) meta-analysis of research on trauma
and traumatic stress among refugees and others exposed to mass conflict and political violence,
of all the experiences evaluated, torture was associated with the greatest increase in PTSD risk
(more than doubling the odds of having PTSD).
Johnson and Thompson (2008) reviewed literature on the prevalence of PTSD among survivors
of political and civilian war trauma. They cited studies involving torture survivors that found
PTSD rates ranging from 18 to 90 percent of study participants. They observed evidence of a
dose–response relationship between torture and both initiation and maintenance of PTSD. This
review suggests that protective factors for PTSD that results from torture and civilian war trauma
include being prepared for torture, having strong social and family support, and having stronger
religious beliefs.
Some theories hold that having redress for torture and other political violence may help survivors
process their traumatic experiences and thus aid in behavioral health treatment (e.g., Roht-
Arriaza, 1995). However, Başoğlu and colleagues (2005) found only a relatively weak
association between the lack of redress for war-related trauma and PTSD symptoms among a
group of 1,358 civilian war survivors in the former Yugoslavia. Fears about threats to one’s
safety and beliefs about losing control over one’s life had much stronger associations with PTSD
symptoms.
The role of forgiveness in the behavioral health of survivors of torture and other political
violence may depend on the context of the violence and the object of forgiveness. Kira and
colleagues (2009) found, among a group of 501 Iraqi refugees, that those who forgave
perpetrators of violence in general as well as those who collaborated with the regime (as
measured with a modified version of the Forgiveness Versus Refusal To Forgive Scale) had
significantly better physical and behavioral health than did those who did not forgive those
people. On the other hand, forgiveness of dictators and specific individuals who were the
principal perpetrators of the violence was associated with significantly worse physical and
behavioral health outcomes.
Sexual Assault/Rape
In 2010, 1.3 percent of women age 12 and older were victims of sexual assault/rape, and it was
estimated that, in the general population, about 0.1 percent of men were victims—although there
were not sufficient data to be certain of the accuracy of that estimate (Truman, 2011). These data
are based on a general population survey that excluded the institutionalized population, which
sustains even higher rates of sexual assault/rape. For example, from 2008 to 2009, 4.4 percent of
Trauma-Informed Care in Behavioral Health Services 1-21
prison inmates were victims of sexual assault (Beck & Harrison, 2010). Although women are
more likely than men to be sexually assaulted even in prison, there are about 13 times as many
men as women in such facilities, so a large number of incarcerated men are affected. Among
prison inmates in 2008–2009, 1.9 percent of men and 4.7 percent of women reported being
sexually victimized by other inmates in the prior year, whereas 2.9 percent of men and 2.1
percent of women reported being sexually victimized by staff members during that period.
Histories of sexual abuse among clinical populations are also likely to be considerably more
common than in the general population (e.g., see TIP 51, Substance Abuse Treatment:
Addressing the Specific Needs of Women [CSAT, 2009b], for a review of data on sexual assault
among female clients in substance abuse treatment settings). Certain other populations, including
survivors of childhood physical and/or sexual abuse, people with disabilities, and people who are
homeless, also have a higher risk for sexual assault (Luce, Schrager, & Gilchrist, 2010).
Accurate data on sexual assault among patients institutionalized for mental disorders are difficult
to locate, but rates of sexual assault should be expected to be high in this group as well.
According to a study by Teplin, McClelland, Abram, and Weiner (2005) of 936 patients with
serious mental illness (SMI) attending outpatient residential day treatment at a Chicago program,
participants were 17.2 times more likely to have been victims of sexual assault or rape in the
prior year and 22.5 times more likely to have been victims of rape than a comparable general
population sample from the National Crime Victimization Survey during the same period.
Studies have also found very high PTSD rates among survivors of sexual assault, especially
survivors of rape, and data suggest that sexual assault is more likely than most other types of
trauma to result in PTSD (see reviews in Ullman & Filipas, 2001). In addition, sexual abuse in
adulthood or childhood is also associated with high levels of other behavioral health disorders. In
a meta-analytic review of 37 studies providing data on 3,162,318 individuals, Chen and
colleagues (2010) found that a history of sexual abuse in childhood or adulthood was associated
with more than three times the risk for an anxiety disorder compared with individuals who had
no such history; more than twice the risk for depression, an eating disorder, or PTSD; and more
than four times the risk for suicide attempts.
Ullman and Filipas (2001) reviewed research identifying factors associated with increased risk
for PTSD among victims of sexual assault/rape. These include being attacked by a stranger,
being subjected to physical force or threatened with a weapon, being physically injured, having a
prior history of childhood sexual abuse, being raped in a location typically considered safe, using
wishful thinking as a coping strategy in response to the attack, and receiving fewer community
services and/or experiencing a high degree of secondary victimization following the attack. On
the other hand, the use of positive distancing (e.g., acceptance coping, optimism, cognitive
distancing) was associated with lower PTSD risk.
In their own research on 332 women who had been sexually assaulted, Ullman and Filipas
(2001) determined that, although positive social reactions following the assault were not
significantly associated with severe PTSD symptoms, more negative responses from others were
associated with more severe PTSD symptoms. In particular, being treated differently or being
discriminated against showed the strongest association with more severe PTSD, and responses in
which people tried to distract the victim (e.g., telling her to move on with her life) showed less
1-22 Part 3, Section 1—A Review of the Literature
severity but were still significantly linked with more severe PTSD. Positive social support was
not significantly related to PTSD symptom severity, but some factors were identified as
significantly associated with more positive social support—namely, lower severity of
victimization and disclosing more about the assault (discussing it at greater length and/or in more
detail). Greater injury severity and a greater perceived threat at the time of the assault were also
associated with significantly more severe PTSD symptoms.
Combat Trauma
Because of the resources available to the military (including the ability to compile accurate data
about a relatively large population), combat trauma is one of the most widely studied types of
trauma in terms of behavioral health. For more information on the impact of trauma and
deployment, see the planned TIP, Reintegration-Related Behavioral Health Issues in Veterans
and Military Families (SAMHSA, planned f). This section summarizes information available in
more detail in that TIP.
According to the largest study of PTSD among Vietnam War veterans, the National Vietnam
Veterans Readjustment Study (NVVRS), 15.2 percent of male veterans had current PTSD, and
30.6 percent met criteria for PTSD at some point during their lives (Kulka et al., 1990b). In
addition, 8.5 percent of women who were in the Vietnam theater as civilian nurses had current
PTSD, and 26.9 percent had PTSD at some point during their lives. These rates were
considerably higher than rates in veterans from that era who did not serve in Vietnam (of whom
2.5 percent of men and 1.1 percent of women had current PTSD) or a civilian comparison group
that was also included in the study.
A later reanalysis of NVVRS data, which took into account criticisms of the initial study,
provided a more conservative estimate of 9.1 percent of men having current PTSD and 18.7
percent meeting criteria for the disorder at some point during their lives (Dohrenwend et al.,
2006, 2007). These authors found that, even for individuals who had substantial impairment
relating to PTSD symptoms, PTSD diagnoses decreased over a 10- to 11-year period following
the war; for the majority, this occurred without receiving mental health services. The NVVRS
also found that war zone stress, which included combat trauma and exposure to other traumatic
events, was also significantly related to major depression, dysthymia, obsessive–compulsive
disorder (OCD), GAD, alcohol use disorders, and antisocial personality disorder (ASPD) for
men (Jordan et al. 1991). The majority (63 percent) of male veterans who had high levels of
exposure to war zone stress met criteria for at least one mental disorder during their lives, and 41
percent had at least one current disorder at the time of assessment.
Studies of military personnel who served in Operation Desert Shield/Desert Storm, Operation
Enduring Freedom (OEF), and/or Operation Iraqi Freedom (OIF) also found high rates of PTSD
and other behavioral health disorders among those exposed to combat. For instance, the National
Health Survey of Gulf War Era Veterans and Their Families, conducted 5 years after Operation
Desert Storm ended, found that the PTSD rate was three times higher for deployed troops than
for nondeployed troops during the same period, with 12.1 percent of deployed troops having
probable current PTSD according to the PCL (Kang, Natelson, Mahan, Lee, & Murphy, 2003).
This study found a correlation between a greater intensity of combat exposure and greater
likelihood of having PTSD.
Trauma-Informed Care in Behavioral Health Services 1-23
Several major studies have evaluated behavioral health disorders among individuals deployed to
OEF/OIF. For example, a review included in a RAND Center for Military Health Policy
Research report found that between 5 and 15 percent of returning service members had current
PTSD, and between 2 and 10 percent had current depression (Karney, Ramchand, Osilla,
Caldarone, & Burns, 2008). Combat duty and being wounded both significantly increased the
chances that an individual would have PTSD. Although greater numbers of women were exposed
to combat trauma in OEF/OIF than in prior conflicts, studies also continued to find higher PTSD
rates in men than in women who had been deployed, with rates of 9.3 percent and 8.4 percent,
respectively, in one large (N=163,812) study (Haskell et al., 2011).
Historical Trauma
Historical trauma refers to trauma inflicted in the past on members of a certain cultural group
that may continue to have effects on the current generation. The concept was originally
developed to help explain how generations descended from Holocaust survivors continued to be
psychologically affected by the trauma their parents and/or grandparents had experienced (Duran
et al., 1998; Sotero, 2006). Clinicians working with other populations, such as Native Americans,
observed a similar pattern with regard to how the behavioral health of more recent generations
continued to be affected by violence committed against their ancestors (Brave Heart, 2003, 2004;
Duran, Duran, Brave Heart, & Yellow Horse-Davis, 1998). Other groups who experienced large-
scale and well-remembered violence, such as attempted genocide or slavery, also have to deal
with historical trauma.
The phenomenon has been studied most often in the United States with Native American
populations, and for many Native Americans receiving behavioral health services, historical
trauma may be an important clinical issue (Brave Heart, 2004; Evans-Campbell, 2008). Some
research indicates that thinking about historical loss is associated with certain behavioral health
problems, such as increased risk for alcohol use disorders (Whitbeck et al., 2004). Although the
exact mechanism through which historical trauma works is not known, the process may be one in
which subsequent generations experience secondary trauma as the result of their parents’ PTSD.
Another explanation is that traumatic experiences harm an individual’s ability to parent
effectively and thus increase the abuse of children, causing those children to have traumatic
stress reactions themselves (Brave Heart, 1999). Some research also points to substance abuse
connected to trauma as central in the perpetuation of historical trauma (Libby, Orton, Beals,
Buchwald, & Manson, 2008).
Sotero (2006), who reviewed research on historical trauma across diverse populations, proposed
that large-scale interpersonal trauma continues to affect communities/cultural groups through
material (e.g., displacement), psychological (e.g., PTSD), economic (e.g., loss of sources of
income/sustenance), and cultural (e.g., lost knowledge of traditions and beliefs) effects. These
powerful effects of trauma cause the next generation to experience similar consequences,
resulting in worse coping skills or attempts to self-medicate distress through substance abuse.
Cumulative Trauma
Kessler (2000) observed that large epidemiological surveys typically ask about the worst or most
severe trauma an individual has endured, with the assumption that if the individual has had
PTSD, it would appear after such a trauma. This approach may undercount lifetime prevalence,
1-24 Part 3, Section 1—A Review of the Literature
however, because further trauma following the worst episode of trauma exposure may have a
kindling effect that results in PTSD a considerable length of time after the worst episode
occurred.
Thus, repeated trauma further increases risk for PTSD, and prior trauma is recognized as a PTSD
risk factor following a traumatic event (see the “Risk and Protective Factors” section). For
example, research conducted with inner-city women (N=777) found that women who had
experienced multiple traumas significantly increased their risk for PTSD (Schumm, Briggs-
Phillips, & Hobfoll, 2006). Therefore, women who had experienced child abuse and also had
been raped as adults were over 17 times more likely than others to be screened as probably
having PTSD, whereas women who had experienced only one of those two types of trauma were
about six times more likely than others to meet screening criteria for probable PTSD.
Studies conducted with other populations have also found that greater exposure to traumatic
events increases risk for a number of behavioral health disorders. For example, a seminal study
conducted with Cambodian refugees (N=993) found a significant dose–response relationship
between the number of traumatic events an individual had experienced and depression, PTSD
symptoms (including arousal, reexperiencing, and emotional numbing, but not avoidance), and
symptoms of culturally specific behavioral health disorders (Mollica, McInnes, Poole, & Tor,
1998).
Extent and Effects of Trauma and Traumatic Stress
Reactions in Specific Populations
The incidence and prevalence of trauma and of behavioral health problems related to trauma vary
across demographic groups. Some of the major demographic differences that may affect trauma
exposure and behavioral health are discussed in this section.
Members of Specific Cultural/Ethnic/Racial Groups
Rates of trauma exposure among some samples of members of certain cultural, ethnic, and racial
groups are higher than the U.S. average. To what extent this reflects socioeconomic and
geographic factors is not clear, as other data indicate that people in urban areas and those with
lower SES are also at greater risk for certain types of trauma (see “People With Lower SES”).
Researchers have found that PTSD rates vary considerably among diverse cultures and that rates
are high among people exposed to significant trauma, regardless of their culture of origin
(Marques et al., 2011).
According to data from Wave 2 of NESARC (N=34,653), which oversampled to achieve a
racially/ethnically diverse sample, non-Latino White Americans were significantly more likely to
have some trauma experience during their lives compared with members of other ethnic/racial
groups, with 83.7 percent of White Americans, 76.4 percent of African Americans, 66.4 percent
of Asian Americans, and 68.2 percent of Latinos reporting some type of trauma exposure during
their lives (Roberts et al., 2011). However, this did not hold true for every type of trauma
exposure. African Americans and Latinos were significantly more likely than White Americans
to have been exposed to childhood maltreatment, with the largest difference being the increased
likelihood of witnessing domestic violence. African Americans were significantly more likely
Trauma-Informed Care in Behavioral Health Services 1-25
than White Americans to have been violently assaulted. Asian Americans, who had significantly
lower levels of exposure than White Americans to many kinds of trauma, were significantly
more likely to have been exposed to war-related trauma (mostly as the result of being unarmed
civilians in a combat zone) and to be refugees from a region where combat was occurring.
Among certain subpopulations of major ethnic/racial groups, trauma exposure may be even more
common. For example, Goldmann and colleagues (2011) assessed trauma histories of 1,306
African American residents of Detroit, the majority of whom had annual incomes below $35,000
(34.6 percent below $15,000, and 27 percent between $15,000 and $35,000). They found that
87.2 percent reported at least one type of trauma during their lives; 51 percent reported
experiencing assaultive violence, 64.5 percent reported another type of injury or shocking
experience (e.g., witnessing someone being seriously injured or killed), and 64 percent reported
learning about trauma from a loved one. Of those who reported at least one trauma, 17 percent
likely had PTSD at some point during their lives, with a higher rate of likely PTSD for
individuals experiencing certain types of trauma (e.g., 32.8 percent of those who had been raped
and 31.2 percent of those who had been badly beaten had a lifetime PTSD diagnosis).
In Wave 2 of NESARC, African American men were significantly more likely than White
American men to have PTSD at some point during their lives, but this was not the case for
African American women (Roberts et al., 2010). According to the same research, Asian
American men and women were significantly less likely than White American men and women
to meet criteria for a lifetime diagnosis of PTSD. Asnaani, Richey, Dimaite, Hinton, and
Hofmann (2010) combined data from the NCS-R and two other surveys that use the same
methodology (the National Study of American Life and the National Latino and Asian American
Study of Mental Health) to evaluate the lifetime prevalence of PTSD. Their data indicated that,
after controlling for age, gender, and SES, both White Americans and African Americans were
significantly more likely than Asian Americans or Latino Americans to have PTSD at some point
during their lives, whereas White Americans and African Americans did not differ from one
another significantly in this regard. Latino Americans were also significantly more likely than
Asian Americans to have the disorder.
As Norris and Slone (2007) observed in their chapter on the epidemiology of PTSD, data are
inconclusive about whether there are significant differences in the likelihood that members of
diverse racial/ethnic/cultural groups within the United States will develop PTSD, especially
given differences in trauma exposure relating to both culture and SES. Marques and colleagues
(2011), in a review of cross-cultural differences in anxiety disorders, observed that the evidence
is mixed regarding differences in PTSD prevalence between African Americans and White
Americans. They concluded that the evidence is stronger regarding elevated levels of PTSD
among Latinos compared with members of other ethnic racial groups. Another review by Pole,
Gone, and Kulkarni (2008) similarly concluded that evidence fairly consistently suggests that
Latinos are more likely than members of other ethnic/cultural groups to develop PTSD but that
significant differences in PTSD rates observed among other ethnic/racial/cultural groups in the
United States tend to disappear when other factors, such as trauma exposure, are taken into
account.
Research indicating significantly higher PTSD rates among Latino populations in the United
States is worth a closer look. Research conducted with Vietnam veterans, a group for whom
1-26 Part 3, Section 1—A Review of the Literature
trauma exposure can be fairly accurately determined, identified Latinos as having greater risk for
PTSD, and this finding was confirmed in later analyses of the data. Ruef, Litz, and Schlenger
(2000) analyzed data from the NVVRS, a large, publicly mandated study that oversampled for
Latinos and African Americans. Although the NVVRS found that PTSD rates were higher
among both Latino veterans (27.9 percent of whom had PTSD at the time of the study) and
African American veterans (20.6 percent) than among White American or other veterans (13.7
percent), after controlling for combat exposure and significant predeployment variables that
affected PTSD (e.g., childhood behavioral problems, substance use disorder symptoms prior to
entering the military), only Latino veterans still had significantly higher PTSD rates.
Ruef, Litz, and Schlenger’s analysis (2000) of the extensive NVVRS data took into account
issues such as linguistic competence in English, cultural differences in reporting style,
experiences of racism during deployment, postdeployment adjustment problems, participation in
behavioral health treatment, and co-occurring disorders. Most of these factors could not explain
differences in PTSD rates between Latinos and African Americans, the latter of whom faced
many of the same stressors. Latinos in the study reported experiencing less racism than did
African Americans, but they may have also experienced less unit cohesion because of their
smaller relative numbers (unit cohesion is also believed to be a protective factor in regard to
PTSD; see the “Risk and Protective Factors” section). The authors did find that Latinos reported
significantly fewer people in their units who they believed were concerned about their welfare
than did African Americans or White Americans.
Using both NVVRS data and data from the Hawaii Vietnam Veterans Project, Schnurr, Lunney,
Sengupta, and Waelde (2003) concluded that Latino male veterans had significantly higher
PTSD rates compared with White men, whereas Asian American male veterans had significantly
lower rates. This finding suggests that the higher PTSD rates observed in Latinos in Vietnam
were not simply the result of greater identification with the Vietnamese. Also, in another analysis
of NVVRS data, Ortega and Rosenheck (2001) found that acculturation did not significantly
affect PTSD rates among Latinos, discounting the possible explanation that differences in
acculturation were responsible for higher PTSD rates in this population. They did, however, find
that in an adjusted model, Puerto Rican veterans were more likely than Mexican American
veterans to have PTSD, suggesting that cultural differences among Latinos may affect PTSD.
Wilcox, Briones, and Suess (1991) also found that Puerto Rican Vietnam veterans had more
severe PTSD symptoms than did Mexican American veterans.
Research conducted with veterans of OIF and OEF also indicates that Latinos are at greater risk
of developing PTSD than members of other ethnic/cultural groups. Researchers at the RAND
Center found that, for OEF/OIF veterans, Latino ethnicity and female gender were both
associated with increased risk for depression and PTSD, even after controlling for trauma
exposure (Tanielian et al., 2008).
Latinos have been found to have higher PTSD rates relative to members of other ethnic/racial
groups in research conducted with other populations, including New York city residents who
witnessed the 9/11 attack (Galea et al., 2004), police officers in three major cities (Pole et al.,
2001; 2005), and hurricane survivors in Florida (Perilla, Norris, & Lavizzo, 2002). However,
among a group of people who were exposed to hurricanes in Florida in 2004, Latino ethnicity
Trauma-Informed Care in Behavioral Health Services 1-27
was only a significant PTSD risk factor for those under age 60, suggesting that age may also
interact with culture in affecting PTSD (Acierno, Ruggiero, Kilpatrick, Resnick, & Galea, 2006).
Pole and colleagues (2008) reviewed possible explanations for why Latinos have elevated PTSD
rates. Two explanations appear to have the greatest support: culturally defined differences in
coping styles (Latinos appear to engage more in self-blame coping and wishful thinking coping,
generally related to religious beliefs) and increased likelihood of experiencing peritraumatic
dissociation, a possible PTSD risk factor that appears to be a more common reaction to trauma
for individuals with greater adherence to Latino cultural norms.
Marshall and colleagues (2009) evaluated differences in PTSD symptoms among a mostly male
(77.6 percent male across the study) group of Latinos (n=330), African Americans (n=171), and
non-Latino White Americans (n=135) who had sustained a sudden physical injury and were
treated at a trauma center in the Los Angeles area. As with other studies, these authors found that
Latinos reported significantly more severe PTSD symptoms (with a difference equivalent to
about a 3-point increase in PCL scores) than African Americans and non-Latino White
Americans. However, they also observed that certain PTSD symptoms were responsible for this
difference. Of the 17 symptoms included on the PCL, Latinos were significantly more likely than
non-Latino White Americans to report 11 of the symptoms, with considerable variation in the
magnitude of the differences. As Triffleman and Pole (2010) observed in a review of this study,
these findings suggest that “elevated rates of PTSD diagnosis among [Latinos] may be due to
differing symptoms, differing levels of symptom severity, and potentially differing relationships
between symptoms” compared with non-Latino White Americans (p. 492).
Particular types of trauma may have a greater or lesser impact on members of a particular
cultural group. For instance, Palinkas, Downs, Patterson, & Russell (1993) found that in the
wake of the Exxon Valdez disaster, Alaska Natives exposed to the event had significantly higher
PTSD and GAD rates than did White Americans who were also exposed. Lilly and Graham-
Bermann (2009) evaluated PTSD in 120 mothers with low incomes who were victims of intimate
partner violence, of whom 42 were African American and 78 were White American. The women
in the study had experienced multiple traumas in the prior year (an average of 36 acts of sexual
abuse, 10 acts of severe physical violence, and 17 acts of mild physical violence). The authors
found that the African American women in the study had significantly fewer PTSD symptoms
(as assessed with the Posttraumatic Stress Scale for Family Violence) than did the White
American women, even though African American women had experienced more severe violence
(although not significantly more so) than the White American women.
Research has also found that the relationship of different types of childhood abuse to PTSD
symptoms varies by cultural group. Among a group of 669 lesbian, gay, or bisexual individuals,
emotional abuse in childhood had a significantly stronger relationship to PTSD and other anxiety
symptoms for African Americans compared with White Americans, whereas physical abuse in
childhood had a significantly stronger relationship to PTSD and other anxiety symptoms for
Latinos than for White Americans (Balsam, Lehavot, Beadnell, & Circo, 2010). International
research also indicates that, in Turkey and India, childhood emotional abuse and neglect have a
greater effect on dissociation than physical or sexual abuse, which is contrary to what is found in
the United States (Lewis-Fernández, Martínez-Taboas, Sar, Patel, & Boatin, 2007).
1-28 Part 3, Section 1—A Review of the Literature
Trauma rates vary by subpopulations within these broad cultural, racial, and ethnic
classifications and may be affected more strongly by noncultural factors (e.g., amount of trauma
exposure). For instance, data suggest that PTSD rates are relatively low for Asian Americans
(e.g., Pietrzak et al., 2011a), but among Cambodian refugees, PTSD rates are considerably
higher. Marshall, Schell, Elliott, Berthold, and Chun (2005), in a telephone survey of 586
Cambodian adults living in Long Beach, CA, found that 100 percent had experienced trauma,
and 62 percent met criteria for a past-year diagnosis of PTSD.
As another example, the American Indian Service Utilization, Psychiatric Epidemiology, Risk
and Protective Factors Project (AI-SUPERPFP), which collected data from 3,084 American
Indians ages 15 to 54 who were members of either a Northern Plains Tribe or a Southwest Tribe,
found significant differences in some types of trauma exposure between American Indians from
the two different regions (Manson, Beals, Klein, & Croy, 2005). PTSD rates also varied,
although the differences were not significant; the largest difference found was between men from
the Southwestern Tribes (11.7 percent of whom met criteria for PTSD during their lifetime) and
men from the Northern Plains Tribes (8.9 percent of whom had lifetime PTSD; Beals, Manson,
Whitesell, Spicer, Mitchell et al., 2005). Larger, but still not significant, differences were found
in lifetime PTSD rates between male American Indian Vietnam veterans from the Northern
Plains Tribes (n=305) and those from the Southwestern Tribes (n=316), who had lifetime rates of
57 percent and 45 percent respectively (Beals et al., 2002). These rates, however, were
considerably higher than found in the general population sample of Beals, Manson, Whitesell,
Spicer, Novins, and colleagues (2005), indicating that factors other than cultural background (in
this case, combat exposure) likely play a greater role in trauma exposure and traumatic stress
reactions.
As suggested by the example of Cambodian American immigrants, rates of trauma are high
among immigrants from countries where military action and political violence are occurring,
regardless of their specific cultural background. Steel and colleagues (2009) conducted a meta-
analysis of trauma and traumatic stress reactions among groups exposed to mass conflict and
displacement. Although reported rates of PTSD and depression varied widely among the studies
included in the review, the authors found that, across surveys, 30.6 percent of participants had
PTSD, and 30.8 percent had depression.
Women and Men
Research generally indicates that men are more likely than women to experience a traumatic
event during their lives (Olff, Langeland, Draijer, & Gersons, 2007). However, data from
multiple sources show that women are significantly more likely than men to experience intimate
partner violence and sexual assault (both in childhood and adulthood; Pratchett, Pelcovitz, &
Yehuda, 2010). This same review found that various research suggests that between 20 and 22
percent of women experience intimate partner violence, and approximately a quarter of all
women are victims of sexual assault. Women are significantly less likely than men, however, to
experience many other types of trauma, including nonsexual assault, combat, traumatic
accidents, and witnessing the death or injury of another person.
Research has consistently found that women are more likely than men to have PTSD, and this
holds true, albeit to a lesser extent, when controlling for trauma exposure (Kimerling, Ouimette,
& Weitlauf, 2007; Olff et al., 2007). For example, data from Wave 2 of NESARC showed that
Trauma-Informed Care in Behavioral Health Services 1-29
women were significantly more likely than men to have PTSD or partial PTSD at some point
during their lives (Pietrzak et al., 2011a). Women were nearly twice as likely as men to have a
lifetime PTSD diagnosis, with 8.6 percent of women and 4.1 percent of men meeting those
criteria. Women were also more likely to meet criteria for a partial but not full diagnosis of
PTSD during their lives (8.6 percent for women compared with 4.5 percent for men). The NCS
also found that women ages 15 to 54 were about twice as likely as men in that age range to have
PTSD at some point during their lives (the rates were 10.4 percent and 5 percent, respectively;
Kessler et al., 1995). Although specific percentages differ, these relative PTSD rates among men
and women are in line with findings from other large studies in the United States and some
studies from other Western countries (see review by Olff et al., 2007).
In another analysis of NCS data, Kessler (2000) noted that a larger percentage of women
exposed to trauma (20.4 percent) than men exposed to trauma (8.1 percent) had PTSD, but he did
not find the difference to be significant. However, women were significantly more likely to have
PTSD than men exposed to the same trauma if they had experienced a sexual assault other than
rape, a physical attack, a trauma to a loved one, or threat with a weapon. Men, however, had
significantly higher PTSD rates connected to combat trauma. Additionally, McLean, Asnaani,
Litz, and Hofmann (2011) found a significant difference in both prior-year and lifetime PTSD
rates among men and women when they combined data from the NCS-R and two other large
national surveys that used the same methodology (National Study of American Life and National
Latino and Asian American Study of Mental Health). According to these data, 4.3 percent of
women and 1.7 percent of men met criteria for PTSD in the year prior to assessment, and 8.5
percent of women and 3.4 percent of men had the disorder at some point during their lives.
A large trauma study conducted in the Detroit metropolitan area (N=2,181) found that although
men were significantly more likely to experience trauma and to have experienced multiple
traumas, women were about twice as likely to develop PTSD following a traumatic experience
(13 percent of women compared with 6.2 percent of men; Breslau, 2002). However, this study,
which evaluated the relative risk for PTSD related to particular types of trauma, also found that
this difference could largely be attributed to differences in response to assaultive violence.
Although PTSD rates did not differ significantly between men and women exposed to other
types of trauma, women were almost six times more likely to develop PTSD in response to
assaultive violence than were men (35.7 percent of women and 6 percent of men exposed to such
violence developed PTSD).
In addition to research indicating that women are more likely than men to develop PTSD as a
result of assaultive violence, a study conducted with 6,697 male and 554 female veterans from
OIF and OEF found that women who sustained physical injury as a result of a traumatic
experience were significantly more likely than men who sustained such injuries to develop PTSD
(Maguen, Luxton, Skopp, & Madden, 2011). In many studies that evaluate PTSD rates by gender
for men and women exposed to the same specific trauma or type of trauma, women are more
likely than men to develop PTSD. For example, female 9/11 survivors were significantly more
likely than male survivors to have probable PTSD (DiGrande et al., 2010). In a study that
compared three different international samples (American, Mexican, and Polish) of individuals
who experienced a natural disaster, women in all three samples had significantly more PTSD
symptoms (North, Kaniasty, Conrad, Inman, & Murphy, 2002). Also, in a group of 454 college
students, women who experienced the death or illness of a loved one had significantly more
1-30 Part 3, Section 1—A Review of the Literature
PTSD symptoms than did men who experienced the same (Gold, Marx, Soler-Baillo, & Sloan,
2005).
According to data from the Trauma Recovery Project (n=627), women were also found to be
significantly more likely than men to develop prolonged PTSD (lasting for at least 18 months)
and had significantly worse ratings of quality of life as a result of prolonged PTSD (Holbrook,
Hoyt, Stein, & Sieber, 2002). In addition, studies indicate that women with PTSD, compared
with men with the disorder, are more likely to have co-occurring mood disorders but less likely
to have co-occurring substance use disorders (McLean & Anderson, 2009; McLean et al., 2011;
Olff et al., 2007). Even in the absence of PTSD, trauma exposure is associated with significantly
higher levels of depressive symptoms and lower levels of substance abuse among women than
among men (Maguen et al., 2011). Using NCS-R data, Dunn, Gilman, Willett, Slopen, and
Molnar (2012) found that higher rates of rape and sexual assault among women compared with
men were in part responsible for higher depression rates among women.
Research generally indicates that women are more likely than men to seek treatment for
behavioral health disorders (McLean & Anderson, 2009). Therefore, women are also
significantly more likely to receive treatment for PTSD. According to NESARC data, women are
approximately 34 percent more likely to be treated for PTSD than men (Roberts et al., 2011).
Women often respond differently to trauma than do men, which may contribute to higher PTSD
rates among women. For example, women are more likely to report dissociation immediately
after or in the few weeks following trauma exposure (Cardeña & Carlson, 2011). Women also
tend to report more intense emotional responses and more dissociation following trauma
exposure (see review by Olff et al., 2007). Research conducted with survivors of serious
vehicular accidents indicates that women are significantly more likely than men are to
experience certain PTSD symptoms 1 month after the accident (e.g., distress in similar situations,
physical reactions to memories, hypervigilance, trouble sleeping, avoidance of
thoughts/feelings/activities/places, exaggerated startle response; Fullerton et al., 2001).
Pratchett and colleagues (2010) reviewed some of the possible explanations for why women
have higher PTSD rates compared with men, even after accounting for trauma exposure. One
possibility was that women are more likely to experience types of trauma (e.g., sexual assault)
that have a greater propensity to lead to PTSD. Other possibilities are that, in aggregate terms,
women’s cognitive appraisals of trauma may differ from those of men and that interpersonal
violence, in particular, may be perceived as a greater threat to women’s core identity. In addition,
following from research showing significant gender differences in emotional reactivity and/or
emotional regulation, women may have more intense emotional responses than men to trauma,
which in turn may increase PTSD risk. However, increased emotional reactivity does not
necessarily mean that women are more affected by trauma, just that they are affected differently.
Research conducted with children who have histories of sexual trauma indicates that boys are
more likely to present externalizing symptoms, whereas girls more often present internalizing
symptoms. Another possible explanation is that women tend to use different coping strategies
following trauma exposure, which may make them more prone to developing PTSD (Olff et al.,
2007).
Research reviewed by Olff and colleagues (2007) also indicates that women who have
peritraumatic dissociation at the time of trauma are much more likely than men who have it to
Trauma-Informed Care in Behavioral Health Services 1-31
develop PTSD; women are also more likely to respond to acute trauma with dissociation and less
likely to respond with hyperarousal than are men (Fullerton et al., 2001). Research evaluating
physiological differences in male and female responses to trauma tends to confirm that such
differences exist. McLean and Anderson (2009) also reviewed possible explanations for higher
PTSD rates among women.
Women may also be affected differently than men by some risk and resilience factors, such as
social support. Research conducted with victims (118 male and 39 female) of violent crime
found that a negative response from others and a lower level of satisfaction with support from
others, had a significantly greater effect on women than on men, although these factors were
associated with greater PTSD symptom severity for both men and women (Andrews, Brewin, &
Rose, 2003). Similarly, research conducted with military personnel deployed in the Gulf War
found that a lack of social support had a greater relationship to depressive symptoms for women
than for men, and greater concerns about disruptions in family and personal relationships had a
more pronounced connection to anxiety symptoms for women than for men (Vogt, Pless, King,
& King, 2005). For military personnel deployed to OIF, negative changes in intimate
relationships (according to self-report) following deployment were significantly related to PTSD
for women but not men, but only when there was a high level of combat exposure (Skopp et al.,
2011).
Another PTSD risk factor that has been found to have a stronger relationship to PTSD for
women than for men includes childhood abuse history (Brewin, Andrews, & Valentine, 2000).
Conversely, both antisocial behavior in childhood and younger age at the time of the traumatic
event appear to have stronger relationships to PTSD for men than for women (King, King, Foy,
& Gudanowski, 1996). In addition, culture appears to play a role in the higher PTSD rates
observed in women, and culture can also moderate these differences (Kimerling et al., 2007).
Research by Norris, Perilla, Ibanez, and Murphy (2001) that compared PTSD rates for men and
women from either the United States or Mexico who were exposed to a natural disaster found
that the magnitude of gender differences in PTSD rates were significantly greater for Mexicans
than for Americans.
People With Lower SES
Although it is not possible to say whether lower SES is associated with increased risk for all
types of trauma, studies have found that lower SES is linked to significantly greater risk for
accidents (Cubbin & Smith, 2002), criminal victimization (Rand & Robinson, 2012; Truman,
2011), combat trauma (Prigerson, Maciejewski, & Rosenheck, 2002), and domestic violence
(Mouton et al., 2004; Vest, Catlin, Chen, & Brownson, 2002). Research from around the world,
similarly, has found that lower SES is associated with increased risk for accidents (including
motor vehicle accidents, burns, and poisoning) and interpersonal violence, including domestic
violence (see review by Laflamme, Burrows, & Hasselberg, 2009).
In a predominately African American sample of 1,256 primary care patients with low SES who
were living in an urban center, 46.2 percent met criteria for a PTSD diagnosis at some point
during their lives (Gillespie et al., 2009). The most common traumas for men in the study were
serious accident or injury (experienced by 56.1 percent), being attacked with a weapon by
someone other than an intimate partner (55.1 percent), being attacked without a weapon by
someone other than an intimate partner (40.3 percent), and sudden life-threatening illness (30.7
1-32 Part 3, Section 1—A Review of the Literature
percent). For women, the most common traumas were serious accident or injury (experienced by
42.2 percent), being attacked by an intimate partner without a weapon (33 percent), sexual abuse
before age 14 (23.9 percent), and being attacked with a weapon by someone other than an
intimate partner (21.8 percent).
Lower income has also been associated with significantly greater PTSD likelihood in other
studies with different populations, including Cambodian refugees (Marshall et al., 2005), African
Americans in a large urban area (Alim et al., 2006), and others. For some populations, however,
lower SES may not be associated with increased trauma exposure and/or traumatic stress
reactions. For example, in the AI-SUPERPFP study of two American Indian populations, both
lower SES and less education were associated with significantly lower levels of trauma exposure
(Manson et al., 2005).
Data clearly show that lower SES is linked to greater risk for PTSD in one’s lifetime than is
found in general population samples. For example, Wave 2 of NESARC found a significant
association between lower income and a higher likelihood of having PTSD at some point during
one’s life, with individuals in the $0 to $19,999 a year bracket having 2.3 times the risk and
those in the $20,000 to $34,999 bracket having 1.8 times the risk compared with others in the
survey (Pietrzak et al., 2011a). People with lower SES, again according to NESARC data, are
also significantly more likely to report lower levels of perceived social support, a significant risk
factor for both trauma exposure and PTSD (Moak & Agrawal, 2010).
The association between lower income and higher rates of trauma/traumatic stress may partly
reflect the fact that people with lower incomes can only afford to live in neighborhoods where
community violence is high (Gapen et al., 2011; Truman, 2011). Gapen and colleagues (2011)
evaluated the relationship of perceived neighborhood disorder (measured with the Neighborhood
Disorder Scale) and PTSD symptoms (assessed with the Modified PTSD Symptom Scale) among
a group of largely (95 percent) African American users of an inner-city health clinic. They found
a significant relationship between perceived neighborhood disorder and PTSD symptoms that
was partially mediated by perceived community cohesion (assessed with the Community
Cohesion Scale). The authors suggested that, in communities where high crime and other
problems exist, residents develop a lack of trust that, in turn, can exacerbate PTSD symptoms.
Less education is also associated with significantly greater risk of having PTSD (DiGrande et al.,
2011; Galea et al., 2008; Pietrzak et al., 2011a). People with lower incomes have fewer resources
with which to address trauma, face more additional stressors that may increase the likelihood of
developing PTSD, and may have learned fewer coping skills (Kelly, Merrill, Shumway,
Alvidrez, & Boccellari, 2010). The fact that losing economic resources as a result of a traumatic
event can significantly increase PTSD risk (e.g., Hobfoll et al., 2008) may also support this
explanation.
Lesbian, Gay, Bisexual, and Transgender People
Studies have documented greater exposure to trauma and higher PTSD rates among lesbian, gay,
bisexual, and transgender people compared with people who are heterosexual (Roberts, Austin,
Corliss, Vandermorris, & Koenen, 2010). Elevated PTSD rates and trauma exposure in this
population are perhaps best documented by Roberts and colleagues’ (2010) analysis of NESARC
data, which included 145 individuals who self-identified as gay/lesbian, 161who self-identified
Trauma-Informed Care in Behavioral Health Services 1-33
as bisexual, 314 who self-identified as heterosexual who reported same-sex partners, 953 who
self-identified as heterosexual who reported attraction to members of the same gender but no
partners, and 18,144 who self-identified as heterosexual who reported neither. According to
these data, women who were lesbian, bisexual, or heterosexual with same-sex partners were
significantly more likely, compared with heterosexual women (including those who had same-
sex attraction but no same-sex partners), to have experienced childhood maltreatment, to have
experienced most types of interpersonal violence, to have witnessed someone being
injured/killed, and to have learned of trauma experienced by a close friend or relative. For men,
being gay or self-identified as heterosexual with same-sex partners, but not being bisexual, was
associated with significantly more likelihood of experiencing interpersonal violence and of
having learned of trauma experienced by a close friend or relative.
For women who were exposed to traumatic events, being bisexual or heterosexual with same-sex
partners was associated with a significantly higher likelihood of having PTSD, compared with
being heterosexual with no same-sex partners. For men who were exposed to traumatic events,
being gay or heterosexual with same-sex partners was associated with a significantly higher
likelihood of having PTSD compared with being heterosexual with no same-sex partners. In a
model that adjusted for gender, race/ethnicity, education, and age at the time of interview, being
self-identified as gay/lesbian, bisexual, or heterosexual with same-sex partners was associated
with more than twice the likelihood of developing PTSD when exposed to trauma. When the
worst type of trauma experienced and the age of its occurrence were factored into the analysis,
the odds ratios fell but remained high compared with heterosexual individuals with no same-sex
partners. The greatest increase in the odds of having PTSD, 1.59 times, was found for self-
identified heterosexuals who had same-sex partners.
Roberts and colleagues (2010) found elevated rates of childhood maltreatment only among
women who were “sexual minorities,” but other studies have found high rates of childhood abuse
among both men and women who are gay/lesbian or bisexual compared with those who are
heterosexual. For example, Balsam, Rothblum, and Beauchaine (2005) found that lesbian, gay,
or bisexual individuals were significantly more likely than were heterosexual siblings to report
psychological and physical abuse by parents/caretakers during childhood and to report more
childhood sexual abuse (not necessarily from caretakers). They also were significantly more
likely to report abuse from partners in adulthood and sexual assaults in adulthood. The authors
found larger differences in sexual victimization among men in the study than among women.
Little information is available about trauma and PTSD among transgender individuals. A
German study involving 41 transgender individuals and 115 individuals receiving inpatient
treatment for mental disorders found that the transgender individuals were significantly more
likely to have experienced childhood emotional abuse/neglect but significantly less likely to have
experienced childhood sexual abuse than were the inpatients (Kersting et al., 2003). Balsam and
colleagues (2010) evaluated the relationship of culture and childhood abuse for a group of
lesbian, gay, or bisexual individuals (N=669). They found that rates of childhood physical abuse
were significantly higher for Latinos and Asian Americans than White Americans and that rates
of childhood sexual abuse were significantly higher for Latinos and African Americans than
White Americans.
1-34 Part 3, Section 1—A Review of the Literature
Other research conducted with 528 lesbian, gay, or bisexual youth (ages 15 to 19) found that 80
percent had experienced verbal victimization, 11 percent physical victimization, and 8 percent
sexual victimization outside the home because of their sexual orientation or atypical gender
behavior. Physical victimization was significantly associated with PTSD (D’Augelli, Grossman,
& Starks, 2006). In an Internet survey of 662 gay, lesbian, or bisexual adults, approximately 20
percent reported being the victim of hate crimes involving physical violence or damage to
property (Herek, 2009).
People With Physical and/or Cognitive Disabilities
People with disabilities, compared with people without disabilities, are 4 to 10 times more likely
to be victims of violence, abuse, and/or neglect (Petersilia, 2001). For example, an analysis of
school, foster care, and police records found that children with disabilities were 3.4 times more
likely than other children to be abused/neglected and were over three times more likely to
experience each specific type of abuse/neglect than children without disabilities (Sullivan &
Knutson, 2000). Govindshenoy and Spencer (2007) reviewed four studies that provide data on
childhood abuse among people with disabilities. Three of the studies found a significant
association between psychological/emotional disabilities and abuse, two between learning
disabilities and abuse, and one between physical disabilities and abuse (see also Fisher, Hodapp,
& Dykens, 2008).
Petersilia (2001) observed that studies from a number of Western countries have found that,
compared with the general population, people with developmental disabilities have a
significantly greater risk for being victims of violence and abuse (although data are limited).
Other research indicates that women with significant physical disabilities are about four times
more likely than other women to be sexually assaulted in adulthood (Casteel, Martin, Smith,
Gurka, & Kupper, 2008; Martin et al., 2006). Plummer and Findley (2012) reviewed these and
other studies discussing the heightened risk for physical and sexual abuse of women with
disabilities.
Research on resilience and traumatic stress reactions indicates that greater intelligence protects
against PTSD (e.g., see Macklin, Litz, McNally, Lasko, Orr, & Pitman, 1998); therefore,
cognitive disabilities may increase risk for developing PTSD following trauma exposure.
Mevissen and de Jongh (2010) reviewed four studies that report PTSD rates in people with
cognitive disabilities as ranging from 2.5 to 60 percent. Razza, Tomasulo, and Sobsey (2011)
also reviewed research that supports the view that people with cognitive disabilities have an
increased risk for developing PTSD following trauma exposure. They cited research indicating
that developmental level affects how an individual processes traumatic experiences and that
cognitive impairments may lead to increases in PTSD. Furthermore, they presented research
indicating that trauma itself negatively affects intellectual abilities.
People Who Are Homeless
In the NCS-R, individuals who had been homeless for more than 1 week in their adult lives were
significantly more likely than those who had remained domiciled to report being in a traumatic
environment (e.g., a combat zone, a natural disaster), having a traumatic experience (e.g., being
kidnapped, being in an automobile accident), experiencing personal violence directed toward
themselves, and/or witnessing the trauma of others (Greenberg & Rosenheck, 2010). In addition,
Trauma-Informed Care in Behavioral Health Services 1-35
those who reported at least 1 week of homelessness were significantly more likely to have had
PTSD at some point during their lives, with 17.2 percent meeting those criteria compared with
6.3 percent of those who had not been homeless for 1 week or more.
Other research indicates that people who are homeless, compared with those who are domiciled,
are significantly more likely to have experienced physical/sexual abuse in childhood (Herman,
Susser, Struening, & Link, 1997; Tam et al., 2003), to be victims of interpersonal violence as
adults (Wenzel et al. 2004), and to sustain unintentional injury (Frencher et al., 2010). People
who are homeless and have behavioral health disorders are significantly more likely than other
people who are homeless to be victims of violence (Lee & Schreck, 2005) and/or to have an
unintentional injury (Wan, Morabito, Khaw, Knudson, & Dicker, 2006).
Among people who are homeless, histories of childhood abuse are associated with significant
increases in the likelihood of having mental health impairment (Kim, Ford, Howard, & Bradford,
2010), and among individuals with mental disorders, histories of childhood abuse are associated
with significant increases in the likelihood of being homeless (Lu, Mueser, Rosenberg, &
Jankowski, 2008; Rosenberg, Lu, Mueser, Jankowski, & Cournos, 2007). In their review of the
research on trauma and homelessness, Hopper and colleagues (2010) concluded that “early
developmental trauma—including child abuse, neglect, and disrupted attachment—provides a
subtext for the narrative of many people’s pathways to homelessness” (p. 80). For more
information on homelessness and traumatic stress reactions, refer to TIP 55, Behavioral Health
Services for People Who Are Homeless (SAMHSA, 2013b).
Veterans
People who have served in the armed forces, in addition to their exposure to combat-related
trauma, also have high rates of exposure to other types of trauma before, during, and after their
service. Veterans have high rates of motor vehicle accidents, especially while driving military
vehicles (Bell, Amoroso, Yore, Smith, & Jones, 2000; Rossen, Pollack, Canham-Chervak,
Canada, & Baker, 2011) and of unintentional injuries related to activities such as exercising and
training (Jones & Knapik, 1999; Wilkinson et al., 2011).
Female veterans report high rates of sexual assault and rape, often occurring during their military
service. Surveys of large groups of female veterans receiving U.S. Department of Veterans
Affairs (VA) services include the following results:
Hankin and colleagues (1999) found that 23 percent of female veterans reported military-
related sexual assault (defined as unwanted sexual relations in which force or the threat of
force was used).
Skinner and colleagues (2000) found that 23 percent of their respondents reported being
sexually assaulted (defined as being forced to have “sexual relations”).
Sadler, Booth, Cook, and Doebbeling (2003) found that 28 percent of respondents reported
being raped while in the military.
Suris, Lind, Kashner, and Borman (2007) found that 33 percent of their sample reported a
sexual assault while in the military.
Kimerling and colleagues (2010) found that 15.1 percent of women and 0.7 percent of men
reported experiencing sexual trauma while in the military.
1-36 Part 3, Section 1—A Review of the Literature
Booth, Mengeling, Torner, & Sadler (2011) found that 24.6 percent of their sample reported
being raped while in the military. Among women who had served in a combat or war zone
(n=576), rape was most often cited (by 36 percent) as the worst trauma they had ever
experienced.
Kang, Dalager, Mahan, and Ishii (2005) interviewed 1,381 Gulf War veterans with current PTSD
and 10,060 without PTSD and found that sexual trauma (defined as sexual harassment and/or
assault) was significantly more common among both male and female veterans who had PTSD
than among male and female veterans who did not. Sexual assault during deployment was
reported by 9.5 percent of women with PTSD and 2.2 percent of other women, and it was
reported by 0.9 percent of men with PTSD and 0.1 percent of other men. The authors determined
that, for women, sexual trauma (either harassment or assault) was associated with greater risk for
PTSD than was combat exposure. Sexual trauma that occurs during a woman’s military service
may also be more likely to result in PTSD than does such trauma experienced before entering or
after leaving the military (Himmelfarb, Yaeger, & Mintz, 2006). For more detailed information
on the impact of trauma and deployment, see the planned TIP, Reintegration-Related Behavioral
Health Issues in Veterans and Military Families (SAMHSA, planned f).
People in Specific Age Groups
Among adults, trauma exposure and traumatic stress reactions vary somewhat according to age.
Norris and Slone (2007) reviewed research regarding differences in trauma exposure according
to age group. They observed that overall trauma exposure is greatest among older adolescents
and young adults (roughly ages 16 to 20), but that exposure to particular types of trauma varies
more across age groups (e.g., sudden, unexpected death of a loved one is most common among
individuals in their 40s). In the NCS, the lifetime risk of having PTSD among people who had
been exposed to trauma peaked in those ages 25 to 35, whereas the lifetime risk of having been
exposed to trauma peaked in those ages 35 to 44 (Kessler et al., 1995).
Research regarding the incidence and prevalence of trauma exposure and current PTSD among
older adults (typically defined as either ages 55 and older or ages 65 and older) in the United
States is limited, but some studies are available. For example, national crime data indicate that
older adults (age 50 and older) are much less likely than those who are younger to be the victims
of violent crime (Truman, 2011). Older adult women are also significantly less likely than other
adult women to experience recent sexual or physical assault, according to a telephone survey of
3,209 women (Acierno et al., 2002). This same study also found that older women who have
sustained physical and/or sexual assault are less likely to develop PTSD and less likely to have
certain types of PTSD symptoms than younger women who have been assaulted.
Overall, most research does indicate that current PTSD rates decline with age even for
individuals in groups with high PTSD rates, such as former prisoners of war or Holocaust
survivors. NCS-R data also indicate that PTSD is less common among older adults than in the
general population (Byers, Yaffe, Covinsky, Friedman, & Bruce, 2010). According to these data,
4.7 percent of older adults ages 55 to 64 had PTSD in the prior year, but only 0.6 percent of
those ages 65 to 74, 0.1 percent of those ages 74 to 84, and 0.7 percent of persons ages 85 and
older had PTSD in the prior year.
Trauma-Informed Care in Behavioral Health Services 1-37
However, some studies from outside the United States have associated older age with increased
PTSD risk. For example, among a group of survivors of the 2004 tsunami in Southern Asia,
being age 40 or older was associated with being significantly more likely to develop PTSD
(Pyari, Kutty, & Sarma, 2012). In largely international research conducted with survivors of
torture and civilian war trauma, older age was also associated with increased PTSD risk (Johnson
& Thompson, 2008). Böttche, Kuwert, & Knaevelsrud (2012) reviewed research on the course
and severity of PTSD among older adults, much of it from European sources, observing that
American and Swedish studies found lower lifetime PTSD prevalence for older adults compared
with middle-aged and younger adults; however, they noted that two German studies found higher
rates for older adults (this may reflect cultural differences, differences in exposure to war-related
trauma, and/or differences in assessment methods). In addition, older adults in specific
populations/groups may have even higher rates of trauma and traumatic stress reactions. One
such group is older adults who are incarcerated (for review, see Maschi et al., 2011).
Older adults may also have somewhat different responses to traumatic stress than adults who are
younger. Traumatic experiences (whether experienced in childhood or adulthood) may affect
both depression and anxiety symptoms in older adults, according to a large (N=1,216) study of
older adults in New Zealand (Dulin & Passmore, 2010). This study found that avoidance of prior
traumatic memories and situations played a large role in late-life anxiety and depression,
accounting for 49 percent of the variance between past trauma and depression and 46 percent of
the variance between trauma and anxiety.
Cook and Niederehe (2007) reviewed research that generally indicates that PTSD for older adults
is typically less severe and that their PTSD symptoms are less intense compared with other
adults. Older adults also appear to experience more arousal symptoms and fewer intrusive
symptoms, and they are less likely to experience depression and GAD in the wake of natural
disasters than are other adults (Cook & Niederhe, 2007). Grammer and Moran (2011), in another
review, observed that biological changes associated with PTSD differ between older adults and
people who are younger (e.g., less variance in cortisol levels, higher levels of serum lipids).
Cultural factors appear to play a role in how age affects PTSD risk and traumatic stress reactions.
Woodward and colleagues (2011) assessed a culturally diverse sample of adults age 55 and older
(N=3,046) using the DSM-IV Composite International Diagnostic Interview. Because they
oversampled for members of certain cultural groups, they were able to report cultural, racial, and
ethnic differences, but they only reported lifetime rates of disorders. These authors found that 4.6
percent of non-Hispanic White Americans, 4.5 percent of African Americans, 3.0 percent of
Black Caribbean Americans, 2.1 percent of Latino Americans, and 2.0 percent of Asian
Americans in this age group met criteria for PTSD at some point during their lives; differences
between the groups did not reach the level of significance.
Norris and colleagues (2002) compared PTSD symptoms following exposure to natural disasters
for individuals from different age groups and three different cultural groups (American,
Mexican, and Polish). They found that among a mixed-race/ethnicity group of Americans who
experienced Hurricane Andrew, middle-aged individuals had significantly more severe PTSD
symptoms (assessed with the Revised Civilian Mississippi Scale [RCMS]) than older adults or
younger adults; among Mexicans who experienced Hurricane Paulina, younger adults had
significantly more severe PTSD symptoms, according to the RCMS, than older or middle-aged
1-38 Part 3, Section 1—A Review of the Literature
adults; and among Poles who experienced a flood, older adults had more severe PTSD symptoms
than younger or middle-aged adults.
Among military service personnel and veterans, Brewin, Andrews, and Valentine (2000)
observed that younger age was a PTSD risk factor in military (usually combat-exposed) but not
civilian samples, which may mean that the role of age differed according to the different types of
trauma commonly experienced by these groups. Other studies of either active-duty personnel or
veterans also found that younger age (typically being age 25 and under) was associated with
significantly higher risk of having PTSD (Greiger et al., 2006; Seal et al., 2009; Tanielian et al.,
2008). However, data from the NVVRS indicated that during the Vietnam War era, younger age
was associated with significantly greater risk for PTSD for men but not women in the military
(King et al., 1996).
Data on OEF/OIF veterans indicate that older age (being 30 or older) is a PTSD risk factor for
women but not for men (Maguen, Ren, Bosch, Marmar, & Seal, 2010). Cook and Niederehe
(2007) reviewed earlier research that found relatively low PTSD rates among World War II and
Korean War veterans who were exposed to combat, suggesting that if PTSD had been present at
levels similar to those seen in more recent conflicts, it likely resolved during older adulthood.
Among older adult veterans in long-term care facilities, past PTSD symptoms were associated
with a significantly greater likelihood of engaging in aggressive behavior, and observer-reported
PTSD symptoms strongly correlated with patient anger (Carlson, Lauderdale, Hawkins, &
Sheikh, 2008).
Risk and protective factors for PTSD may also vary between age groups. Acierno, Kilpatrick,
Resnick, Saunders, & Best (2006) compared risk factors for adults ages 60 and older (n=1,130)
and adults younger than 60 (n=413) affected by the 2004 Florida hurricanes. They found that low
income and a greater number of days displaced from one’s home significantly increased PTSD
risk for older adults but not younger ones. Also, for older adults only, more days displaced also
increased risk for depression and GAD, whereas greater out-of-pocket posthurricane expenses
increased risk for GAD alone. Younger adults, however, did have significantly higher levels of
PTSD symptoms than older adults. Another concern for older adults with trauma histories is the
emergence of PTSD in older adulthood resulting from trauma experienced many years earlier.
Little research is available on this subject, but Hiskey, Luckie, Davies, and Brewin (2008)
reviewed 4 studies involving older adult male war veterans and 12 case studies that document
this phenomenon.
Responses to Trauma: Trauma and Behavioral Health
Not all traumas are equally likely to result in a traumatic stress reaction. Notably, PTSD risk is
significantly higher for trauma involving interpersonal violence (Breslau, 2002; Fetzner,
McMillan, Sareen, & Asmundson, 2011; Kessler, 2000). Kessler (2000) observed that “the
conditional risk of PTSD among trauma victims in U.S. samples varies enormously depending
on the type of trauma to which they were exposed” (p. 6). As an example, he gave data from the
NCS. For men in that survey, 65 percent of those who had experienced rape had PTSD,
compared with 38.8 percent of those who had combat exposure, 12.2 percent of those who
experienced another type of sexual assault, 6.4 percent of those who witnessed a traumatic event,
6.3 percent of those who had a life-threatening accident, 4.4 percent of those who had a loved
Trauma-Informed Care in Behavioral Health Services 1-39
one who sustained trauma, 3.7 percent of those who were in a natural disaster, and 1.9 percent of
those who were threatened with a weapon. For women, the highest rate of PTSD (45.9 percent)
was associated with rape. PTSD rates among women for other traumas were 32.6 percent for
women who had been threatened with a weapon, 26.5 percent for sexual assault other than rape,
21.3 percent for physical attack, 10.4 percent for trauma occurring to a loved one, 8.8 percent for
a life-threatening accident, 7.5 percent for witnessing a traumatic event, and 5.4 percent for
experiencing a natural disaster.
Data from Wave 2 of NESARC indicate that people who have current PTSD, compared with
people with histories of trauma exposure but no PTSD or partial PTSD, are more likely to have
experienced certain types of trauma, including being mugged/held up (4.5 times more likely),
childhood neglect (4.4 times), childhood physical abuse (4.4 times), military combat (4.3 times),
witnessing family violence in childhood (4.2 times), sexual assault (4.1 times), being stalked (4.1
times), being kidnapped/held hostage (4.0 times), being assaulted by someone other than an
intimate partner (4.0 times), and being assaulted by an intimate partner (3.2 times; Pietrzak et al.,
2011a). Trauma in which the individual fears for his or her life is also associated with increased
PTSD risk. According to data from the Trauma Recovery Project, a large (N=1,048) prospective
study of trauma and its effects, perceived threat to life significantly predicted both early
symptoms of acute stress and PTSD (Holbrook, Hoyt, Stein, & Sieber, 2001). The odds of
developing PTSD when there was a perceived threat to life were 1.6 times higher. Other
significant factors associated with PTSD risk included perceiving a greater chance of the
traumatic event occurring again, which increased the odds of developing PTSD 1.5 times;
assaultive violence, which increased the odds 1.6 times; and sustaining a penetrative wound,
which increased the odds 2.4 times. Research with military samples has also consistently found
that greater perceived threat is associated with greater PTSD risk (Maguen, Suvakm, & Litz,
2006).
Abuse in childhood often results in lasting and severe PTSD because it has physical and
behavioral effects on the developing mind (Cougle, Timpano et al., 2010). Wrenn and colleagues
(2011), using a largely African American, inner-city sample of people who had experienced
trauma (N=767), found that trauma in childhood was associated with significantly greater PTSD
risk than trauma experienced in adulthood alone. Childhood abuse was associated with even
greater risk than other childhood trauma. Sexual abuse, in adulthood or childhood, is also
associated with high PTSD levels as well as other behavioral health disorders. In a meta-analytic
review of 37 studies providing data on 3,162,318 individuals, Chen and colleagues (2010) found
that a history of sexual abuse in childhood or adulthood was associated with more than three
times the risk for an anxiety disorder compared with individuals who had no such history; more
than twice the risk for depression, an eating disorder, or PTSD; and more than four times the risk
for suicide attempts.
Brain Responses to Traumatic Stress
Neuroimaging studies demonstrate specific changes in the brains of people with PTSD, such as
increased activity in the amygdala, decreased activity in the medial prefrontal cortex, and
reduced hippocampal and anterior cingulate cortex volumes (Garfinkel & Liverzon, 2009;
Hughes & Shin, 2011). Neurochemical changes have also been found in people with PTSD,
including increased dopamine levels, increased norepinephrine levels and/or activity, decreased
1-40 Part 3, Section 1—A Review of the Literature
concentrations of serotonin in parts of the brain, decreased gamma-aminobutyric acid activity,
increased glutamate levels, decreased plasma levels of neuropeptide Y (NPY), and increased
levels of beta-endorphin in the cerebrospinal fluid (Sherin & Nemeroff, 2011). Brenner (2011),
Garfinkel and Liverzon (2009), Hughes and Shin (2011), and Sherin and Nemeroff (2011)
reviewed research on changes in brain activity, chemistry, and volume related to PTSD. Brenner
(2011) also attempted to distinguish these changes from those associated with traumatic brain
injury (TBI).
Risk and Protective Factors
A number of risk and protective factors for trauma and for traumatic stress reactions (particularly
PTSD) have been identified in the literature. Some of these factors are likely true risk/protective
factors in that they increase or decrease risk in and of themselves, whereas others (e.g., elevated
heart rate following trauma exposure) are likely indicative of other underlying risk factors, but
both types of factors are discussed together in this literature review. As Layne, Warren, Watson,
and Shalev (2007) observed in their review on PTSD-related risk and resilience, there is a lack of
general agreement in the literature as to what defines protective or resilience factors, making it
difficult to evaluate the relative importance of such factors. They noted that factors that promote
resilience to traumatic stress reactions can range from genetic biological factors (e.g., greater
levels of dehydroepiandrosterone, lower production of corticotrophin-releasing hormone), to
personal attributes (e.g., greater intelligence, a stronger internal locus of control), to processes of
adaptation to stressors/adversities, to social relationships.
Risk factors
Research has found a number of factors associated with increased risk for trauma exposure and
traumatic stress reactions. Some of these factors are demographic in nature (e.g., SES,
race/ethnicity, gender), whereas others involve individual and social characteristics (e.g., lower
intelligence, less social support). Breslau, Lucia, and Alvarado (2006) found that youth with
lower intelligence (as measured by intelligence quotient [IQ]) were significantly more likely to
have been exposed in the 10 years following their assessment to traumatic events—specifically,
nonassaultive trauma—and to have developed PTSD (conditioned upon not having anxiety
disorders or high rates of externalizing problems at their initial assessment). In terms of social
support, Moak and Agrawal (2010), using data from Waves 1 and 2 of NESARC, found a
modest but significant correlation between lower perceived social support and exposure to
traumatic events.
A number of reviews and meta-analyses provide an overview of PTSD risk factors. Brewin and
colleagues (2000) included 77 articles in their meta-analysis, which focused largely on
demographic factors. They concluded that PTSD risk following trauma exposure increased with
the following factors: female gender, lower SES, racial/ethnic minority status, less education,
prior behavioral health disorders, a history of childhood abuse, a history of other prior trauma,
other ACEs, a history of behavioral health disorders in one’s family, and a lack of social support.
They cautioned, however, that only a prior history of behavioral health disorders, childhood
abuse, and a family history of behavioral health disorders were uniformly found to increase risk
in the studies that included them as variables. The authors also observed that risk factors differed
somewhat between military and civilian samples, with female gender having no significant effect
in military samples but younger age being associated with increased PTSD risk in military
Trauma-Informed Care in Behavioral Health Services 1-41
samples. Trauma severity also had a significantly greater effect on PTSD in military than in
civilian samples (which may reflect differences in the nature of trauma typically experienced by
these two groups). Brewin and colleagues (2000) found that risk factors vary somewhat by
gender as well, so that, for example, childhood abuse has a significantly greater effect on women
than on men, and younger age has an effect for men but not women (which may explain why it
has an effect for largely male military samples but not civilian samples). These authors
concluded that there was a great deal of heterogeneity across the studies and thus cautioned
against trying to create a model in which pretrauma risk factors are considered universal rather
than mediated by particular responses to trauma or factors associated with the trauma itself.
A meta-analysis by Ozer, Best, Lipsey, and Weiss (2003) included a larger group of studies
(476) and focused on a different set of risk factors than did Brewin and colleagues’ (2000)
review, namely factors associated with “psychological processing and functioning” and “aspects
of the traumatic event or its sequelae” (p. 55). As such, they presented their review as
complementary to that of Brewin and colleagues (2000). Ozer and colleagues (2003) found seven
significant risk factors for PTSD:
1. A history of prior trauma
2. Problems with behavioral health prior to the trauma (including preexisting mental disorders)
3. A family history of behavioral health disorders
4. A perceived threat to one’s life during the traumatic event
5. Perceived social support following the trauma
6. Intensely negative emotional responses immediately following the trauma (e.g., extreme fear,
helplessness, horror, shame)
7. Peritraumatic dissociation (i.e., dissociative experiences during or immediately following the
trauma)
These authors found that stronger PTSD “predictors” were factors that were more proximal to
the traumatic event, namely perceived threat to life, perceived social support, heightened
peritraumatic emotional responses, and peritraumatic dissociation. In addition to differences in
focus, Ozer and colleagues’ (2003) review differed from that of Brewin and colleagues (2000) in
that it found social support to be a weaker predictor. The authors noted that this may reflect the
fact that social support (or the lack thereof) had a larger effect in studies in which 3 or more
years had elapsed since the trauma than in those that assessed individuals sooner after the
traumatic event; their review included more of the latter. They noted that this may indicate that
social support has a cumulative effect or is more important when individuals have more chronic
PTSD (and less important in cases of ASD). Data from NESARC also indicate that lower
perceived social support is associated with a number of other mental disorders (e.g., major
depression, GAD) and behaviors such as suicidality (Moak & Agrawal, 2009).
Vogt, King, and King’s (2007) reviewed the literature on PTSD risk factors, paying special
attention to the mechanisms through which such factors may affect PTSD. Their findings did not
differ substantially from earlier reviews, but they observed some other factors associated with
increased risk that were not included in the meta-analytic reviews cited previously, which had
more strict inclusion criteria. They cited studies that found a dose–response relationship between
severity of trauma and PTSD, as well as studies that found an increase in PTSD associated with
trauma resulting in physical injury, trauma perceived as more malicious or horrifying, trauma in
1-42 Part 3, Section 1—A Review of the Literature
which one is actively involved (rather than a participant), and trauma that resulted in
peritraumatic dissociation. The authors also observed that demographic factors (i.e., female
gender, younger age, lower SES, lower education, lower intelligence, and certain racial/ethnic
backgrounds) appeared to have a significant, but modest, relationship to PTSD risk. Prior trauma
exposure, preexisting mental disorders, a history of childhood abuse, other exposure to ACEs, a
family history of mental disorders, and lack of social support all appeared to have a somewhat
large effect on increasing PTSD risk. They also noted that research, mostly conducted with
veterans, indicated that the risk factors for onset and maintenance of PTSD appear to be
different. Risk factors that existed prior to the traumatic experience did not have as strong an
effect on the latter. However, other factors that came into play after the trauma may have
affected the course of and recovery from PTSD. Examples of these include social supports
available after the trauma (including community reactions), use of coping strategies, and
cognitive appraisals of the nature of the trauma.
Recent studies (not included in the previously discussed reviews) that evaluate risk factors
associated with PTSD symptoms not only generally confirm the prior findings; they also shed
light on how different factors affect PTSD risk following different types of trauma exposure. For
example, in a study that evaluated risk factors associated with PTSD symptoms (not PTSD
diagnosis) for 2,001 New York residents following the 9/11 attack, risk factors included seeing
the actual attack, living closer to the attack, experiencing a fear of injury/death at the time of the
attack, being involved in the rescue effort, losing a job following the attack, having a friend or
family member killed in the attack, experiencing greater media exposure to the attack, having
more stressors in the year prior to the attack, and having less social support (Lawyer et al., 2006).
However, in a multivariate model that controlled for other historical, exposure, and demographic
factors, the only risk factors that remained significant were heightened peritraumatic emotional
responses and dissociation, peritraumatic panic/physiological arousal, greater life stressors in the
year prior to the attacks, and being involved in the rescue effort.
In another study involving 527 adults admitted to a Level 1 trauma center with traumatic injuries,
greater PTSD symptom severity was associated with younger age, being unmarried, being
unemployed, having lower SES, being African American or Latino, and experiencing assaultive
rather than nonassaultive trauma (Chiu, deRoon-Cassini, & Brasel, 2011). A study of 1,386
patients at a trauma clinic found that patients were significantly more likely to screen positive for
probably developing PTSD (in a screen that occurred a mean of 24 days after the traumatic
event) if they were under 55 years old, were female, had sustained a blunt or penetrating wound
(excluding self-inflicted or accidental wounds), and/or had been in a motor vehicle crash or had
been the target of assaultive trauma (compared with all other traumas; Alarcon et al., 2012).
Developmental risk factors (e.g., childhood abuse, preexisting mental disorders, mental disorders
in one’s family), according to Koenen (2006), affect an individual’s ability to self-regulate
thoughts and feelings. The author noted that, although more research is needed, such risk factors
may play a significant role in determining whether an individual is at risk for PTSD following
trauma exposure.
Risk factors associated with material needs and losses are often ignored in research, but a
number of studies have found that such factors do affect PTSD rates. For example, research from
Israel indicates that the loss of economic resources following trauma exposure is associated with
a significantly greater likelihood of PTSD (Hobfoll et al., 2008). Loss of home and/or economic
Trauma-Informed Care in Behavioral Health Services 1-43
resources seems to affect PTSD onset and to affect specific populations differently. Research
conducted with survivors of a large fireworks explosion in the Netherlands found that individuals
whose homes were destroyed were significantly more likely than others affected by the disaster
to have late-onset PTSD (Smid et al., 2012) and were more sensitized to stressful events
occurring after the disaster (Smid et al., 2011). Material losses and lack of income appear to have
a significantly greater effect on increasing PTSD risk for adults ages 60 and older compared with
younger adults (Acierno et al., 2006)
In addition, a diagnosis of ASD following the traumatic event is a PTSD risk factor. Bryant
(2011) reviewed 22 studies that evaluated the relationship of ASD to later PTSD development,
concluding that an ASD diagnosis had a reasonable level of predictability (with at least half of
individuals who had ASD later developing PTSD), but that it had poor sensitivity as a predictive
measure (because the majority of individuals who developed PTSD did not have ASD). Cardeña
and Carlson (2011) postulated that ASD is not a robust predictor of PTSD because ASD may be
only one possible response to trauma and because protective factors that come into play after
trauma exposure may help keep some individuals who have ASD from developing PTSD.
The importance of peritraumatic dissociation as a PTSD risk factor has been debated. Meta-
analytic reviews by Breh and Seidler (2007), Lensvelt-Mulders and colleagues (2008), and Ozer,
Best, and Lipsey, & Weiss (2003) all found evidence that peritraumatic dissociation represented
a PTSD risk factor. Also, Cardeña and Carlson (2011), following Lensvelt-Mulders and
colleagues (2008), concluded that peritraumatic dissociation has a stronger association with
PTSD in studies with a prospective rather than a retrospective design, suggesting that the
relationship between the two was not just a result of long-term recall being clouded by later
PTSD.
However, another review by van der Velden and Wittmann (2008), which included only
prospective studies and controlled for persisting symptoms of dissociation, found that
peritraumatic dissociation was a relatively weak PTSD predictor, whereas dissociation that
persisted after the trauma was a much better predictor. Cardeña and Carlson (2011) also noted
that other research confirms that dissociative symptoms that persist after trauma exposure are a
relatively strong PTSD predictor, whereas peritraumatic dissociation is a relatively weak
predictor. One reason that some studies have found a stronger relationship between peritraumatic
dissociation and PTSD than have others is that the relationship appears to be significantly
stronger among women than among men. Research conducted with 122 survivors of serious
motor vehicle crashes found that the PTSD risk associated with peritraumatic dissociation was
7.55 times greater for women than for men (Fullerton et al., 2001).
Some authors (e.g., Lawyer et al., 2006) have suggested that peritraumatic panic attacks are
another possible PTSD predictor. However, Adams and Boscarino (2011) examined data on
1,681 survivors of 9/11 and found that, in a model that controlled for potentially confounding
factors, a panic attack at the time of the incident predicted PTSD in the year after the event but
not 2 years after the event. Insomnia and other sleep disturbances that begin following a
traumatic event have also been associated with increased risk for developing PTSD (Babson &
Feldner, 2010). Some small studies have also found that individuals who develop PTSD
following trauma exposure have elevated heart rates (e.g., 96 beats a minute and higher) soon
after and up to a week after that exposure—significantly higher rates than for those who
1-44 Part 3, Section 1—A Review of the Literature
experience trauma but do not develop PTSD (e.g., Bryant, Creamer, O’Donnell, Silove, &
McFarlane, 2011; Shalev et al., 1998). Research from France suggests that heart rate variability
is a better predictor of PTSD than elevated heart rate alone. In this study, 35 survivors of
automobile accidents had a positive predictive value of 75 percent and a negative predictive
value of 90 percent in relation to the later development of PTSD (Shaikh Al Arab et al., 2012).
Genetic factors appear to contribute to both trauma exposure and PTSD development in a
number of ways. For example, research conducted with twins (which enables researchers to
evaluate the relative contribution of common genetics) has found that a genetic predisposition is
involved in assaultive trauma but not other kinds of trauma, which is likely related to behaviors
that might make an individual more prone to becoming involved in situations where this type of
trauma may occur (Afifi, Asmundson, Taylor, & Jang, 2010). Other research included in this
review indicated that genetics affect, to a moderate degree, whether an individual will develop
PTSD symptoms as a result of trauma exposure; the degree to which genetic factors contribute
may differ depending on the type of symptoms under consideration. Genetic factors may also
differ according to the type of trauma and how many incidents of trauma are experienced (e.g.,
genetic factors may play a lesser role when a person experiences three or more types of trauma).
Other reviews reached similar conclusions regarding the contribution of genetic factors to the
development of PTSD. For example, Cornelius, Nugent, Amstadter, and Koenen (2010)
reviewed a wider range of research (not just twin studies), including information concerning the
specific genes associated with PTSD. They also focused on some of the limitations of existing
research (e.g., use of samples with relatively low PTSD rates, use of widely different
methodologies). Sartor and colleagues (2011) looked specifically at genetic and environmental
factors that play a role in both PTSD and substance use disorders for women, as fewer data are
available on the role of genetics for women than for men. They found good evidence for a
genetic link for both types of disorder among women.
Research conducted with veterans has found a common genetic influence on increased exposure
to combat, increased alcohol use, and greater likelihood of having PTSD symptoms (McLeod et
al., 2001). Research reviewed by Afifi and colleagues (2010) confirmed that genetics may
contribute to the co-occurrence of substance use disorders and PTSD as well as to exposure to
assaultive trauma. Genetic factors may also play a role in maintaining PTSD and in an
individual’s response to PTSD treatment. Bryant and colleagues (2011) found that, after
controlling for pretreatment PTSD severity and number of treatment sessions attended, people
with PTSD who had a given genotype had significantly more severe PTSD 6 months after
receiving an 8-week exposure therapy (ET) intervention than others in the study.
Little information is available about specific risk and protective factors for ASD, although many
of the factors relevant to PTSD would also likely apply (Cardeña & Carlson, 2011). However,
these authors did review literature indicating that the ability to be hypnotized (which has a
genetic component), childhood abuse, disturbed attachment in childhood, and a tendency to view
events as catastrophic have all been associated with increased risk for ASD.
Protective factors
Protective factors for trauma almost entirely reflect the risk factors discussed in the preceding
“Risk Factors” section. For trauma, protective factors are typically contextual, including
Trauma-Informed Care in Behavioral Health Services 1-45
characteristics that make it less likely that a person will be in a situation where trauma might
occur. A review by Ahmed (2007) listed internal characteristics that promote resilience to PTSD:
Self-esteem
Trust
Resourcefulness
Self-efficacy
Internal locus of control
Secure attachments
Sense of humor
Self-sufficiency
Sense of mastery
Optimism
Interpersonal abilities (e.g., social skills, problem-solving skills, impulse control)
Ahmed’s review (2007) also listed the following external resilience factors:
Sense of safety
Religious affiliation
Strong role models
Emotional sustenance (i.e., receiving from others understanding, companionship, a sense of
belonging, positive regard)
A review by Agaibi and Wilson (2005) classified protective factors into five categories:
personality factors (e.g., hardiness, internal locus of control, autonomy), affect regulation, coping
skills (e.g., active problem-solving skills), ego defenses, and ability to mobilize and use
resources (e.g., social support). These authors also presented a model for how these different
factors relate to one another in affecting an individual’s response to traumatic stress and
promoting adaptation and resilience. Guay, Billette, and Marchand (2006) reviewed research and
theory on the protective aspects of social support, one of the protective factors most consistently
found to have a significant role with regard to PTSD. Guay and colleagues (2006) reviewed
research and theory regarding the protective aspects of social support as well as PTSD’s potential
negative effects on social interactions. They observed that the most widely held belief is that
social support positively affects PTSD symptoms because it influences individuals’
interpretations of traumatic events and their ability to process traumatic experiences.
In some studies, social support is the most significant factor, with such populations as survivors
of childhood abuse (Collishaw et al., 2007), women who were victims of sexual assault
(Kimerling & Calhoun, 1994), survivors of natural disasters (Cook & Bickman, 1990), veterans
exposed to combat trauma (Pietrzak et al., 2010), law enforcement officers (Martin, Marchand,
Boyer, & Martin, 2009), women who experienced war trauma in Bosnia and Herzegovina (Klarić
et al., 2008), and survivors of torture (Johnson & Thompson, 2008). However, the most
important type of social support may vary according to the specific situation and the type of
trauma; for example, for men exposed to combat trauma, military unit support and cohesion may
be most important during deployment (Office of the Surgeon Multinational Force-Iraq & Office
of the Surgeon General, U.S. Army Medical Command, 2006), whereas for survivors of
1-46 Part 3, Section 1—A Review of the Literature
childhood abuse, support from caregivers and relationships with peers in childhood and with
intimate partners in adulthood seem to be most significant (Aspelmeier, Elliot, & Smith, 2007;
Collishaw et al., 2007).
A good deal of research on protective factors has been conducted with military personnel and
veterans. Some of the protective factors for this population are the same as for others, such as
social support, positive/active coping skill use, greater self-esteem, greater mastery/self-
sufficiency, more education, higher SES, and male gender (Subcommittee on Posttraumatic
Stress Disorder of the Committee on Gulf War and Health, 2006). In addition, better training and
preparation for combat trauma (or at least, feeling more prepared), stronger unit cohesion, and
responses from the civilian population upon returning from combat all have a protective
function. In a study involving 207 combat veterans deployed to the Middle East, individuals’
sense of preparedness, as assessed prior to deployment, affected the relationship between
perceived threat (greater perceived threat has been associated with increased risk for PTSD) and
combat experiences. That is, those who had a better sense of preparedness perceived less threat
from their combat experiences, which translated into lower levels of PTSD (Renshaw, 2011).
Positive attitudes toward military service are related to significantly lower PTSD rates among
military personnel deployed to Iraq (N=2,583; Skopp et al., 2011). The same risk and resilience
factors have also been found for veterans from other conflicts (Vogt & Tanner, 2007), and for the
National Guard as well as active-duty personnel (Polusny et al., 2011). Protective factors
assessed for other specific groups generally do not deviate much from those already mentioned.
For example, Yuan and colleagues (2011) evaluated 233 police officers during their academy
training and again after serving 2 years, finding that a stronger sense of self-worth, stronger
beliefs in the benevolence of the world (assessed with the World Assumptions Scale), greater
social support, and better social adjustment (assessed with the Social Adjustment Scale–Self
Report) were all significant protective factors against later PTSD development. In another
analysis of 132 Canadian police officers, the only significant protective factors identified were
one dimension of the Short Hardiness Scale relating to an officer’s ability to perceive difficulties
as challenges and social support from coworkers (but not from significant others; Martin et al.,
2009).
In an evaluation of PTSD risk and protective factors for 600 women who were sexual assault
victims, the only significant protective factor for PTSD symptoms identified was the victims’
perceptions that they had greater control over their recovery process (Ullman, Filipas,
Townesend, & Starzynski, 2007). For both risk and protective factors, the victims’ perceptions at
the time of the assault and their postassault characteristics (e.g., negative social reactions, coping
skills) had a stronger relationship to PTSD symptom severity than did preassault characteristics
and the characteristics of the assault itself.
Religious belief/affiliation has been found to have a protective function in groups as diverse as
Buddhist Cambodian refugees (Cheung, 1994) and African American women who have been
victims of intimate partner violence (Bradley, Schwartz, & Kaslow, 2005). However, stronger
religious beliefs may not always have a protective function, and much will depend on context.
For example, in a study of Israeli settlers who were forced to move from their homes in the Gaza
Strip (N=104), a stronger secular identity (i.e., one that was not traditionally religious or
orthodox) assessed prior to relocation was associated with significantly lower levels of PTSD
Trauma-Informed Care in Behavioral Health Services 1-47
symptoms assessed 9 months after relocation (Ben-Zur, 2008). Other protective factors included
greater perceived social support (from family, friends, community, and the government), higher
levels of mastery/optimism, more education, and certain demographic factors (e.g., gender).
Many protective/resilience factors for PTSD (including social support) are essentially the same
as protective factors for behavioral health disorders in general. Much of the research in this area
has been conducted with youth and adolescents, but the protective factors thus identified do not
vary much from those for adults. For example, Van Breda (2001) provided an indepth review of
factors associated with resilience in general (i.e., better behavioral health and better resistance to
stressors), which include hardiness, a sense of coherence, learned resourcefulness, self-efficacy,
and a stronger internal locus of control, all of which may also be considered resilience/protective
factors in relation to PTSD.
Certain coping styles and cognitive appraisals of traumatic events can reduce the occurrence
and/or severity of PTSD. For example, Ginzburg, Solomon, and Bleich (2002) found that the use
of repressive coping styles was linked to significantly lower levels of PTSD symptoms following
trauma exposure. Earlier research conducted with 215 female victims of assault (either sexual or
nonsexual) found that greater use of positive distancing (e.g., optimism, acceptance, cognitive
distancing) was associated with significantly less severe PTSD, whereas reliance on wishful
thinking was associated with worse PTSD (Valentiner, Foa, Riggs, & Gershuny, 1996).
Research conducted with 102 women who reported histories of childhood sexual abuse found
that those women who found their traumatic experience more central to their identity, who
believed the trauma was a turning point in their lives, and/or who believed past trauma
influenced their expectations for the future (all factors assessed using the Centrality of Events
Scale) had significantly more severe PTSD (assessed with the PCL-Civilian Version) compared
with other women in the study (Robinaugh & McNally, 2011). Other research indicates that
women with PTSD who have protective self-cognitions are less likely to lose resources (material,
social, family, and work-related) than women with PTSD who do not have such protective
cognitions. (Walter, Horsey, Palmieri, & Hobfoll, 2010). Personality traits may also play a role
in protecting individuals from PTSD. For instance, a British study involving a community
sample of 364 individuals who were assessed in adolescence and again some 30 years later found
that, among those with histories of childhood abuse, a more stable personality (assessed with the
neuroticism scale of the Eyesnck Personality Questionnaire) was associated with being
significantly more likely not to have an anxiety disorder (including PTSD) or depressive disorder
in adulthood (Collishaw et al., 2007).
Effects of Trauma and Traumatic Stress Reactions on Quality of Life, Health,
and Functioning
Trauma, in and of itself, appears to have negative effects on quality of life and health, although
trauma is not as well researched as the effects of PTSD on these outcomes. NCS-R data indicate
that trauma itself often has a greater role in physical health problems than does PTSD, and it has
often been ignored in the research evaluating the health consequences of PTSD (see Sledjeski,
Speisman, & Dierker, 2008). Although trauma itself is associated with functional impairment
and/or decrease in quality of life, a number of studies comparing individuals with PTSD and
individuals who had trauma exposure without PTSD have found that those with PSTD have
1-48 Part 3, Section 1—A Review of the Literature
significantly lower quality of life and more impairments (Breslau, Lucia, & Davis, 2004; Gellis,
Mavandadi, & Oslin, 2010; Stein, Walker, Hazen, & Forde, 1997).
There is no doubt that traumatic experiences that result in physical injury negatively affect
quality of life, health, and functioning (Polinder et al., 2010; Polinder et al., 2012). Although it is
difficult in many cases to tease out the relative effects of physical and psychological trauma (e.g.,
see discussion of burn victims by Corry, Pruzinsky, & Rumsey, 2009), research indicates that
both quality of life and functioning are significantly more impaired among disaster survivors
who sustain physical injury compared with those who do not (e.g., Sudaryo et al., 2012). In a
study of Indonesian survivors of a large earthquake, physical injury and impairment had a more
significant effect on quality of life (Sudaryo et al., 2012).
In general, numerous studies conducted with a variety of different populations have found that
people with PTSD have worse quality of life than do those who never had the disorder, even if
they were exposed to trauma (Olatunji, Cisler & Tolin, 2007; Schnurr, Lunney, Bovin & Marx,
2009). Partial PTSD has also been associated with significantly worse quality of life, although
not to the extent of PTSD, compared with individuals who have had trauma exposure but not
PTSD or partial PTSD (Gellis et al., 2010). Although quality of life appears to be better for
people who are in remission from PTSD, it remains worse compared with those who never had
PTSD (Westphal et al., 2011).
In a study conducted with 184 people with chronic PTSD (largely White American women), the
strongest predictors of worse quality of life were arousal symptoms, depressive symptoms, and
other anxiety symptoms (Doctor, Zoellner, & Feeny, 2011). In another group of 156 Turkish men
with alcohol dependence, dissociation symptoms and a lifetime diagnosis of PTSD were
predictive of worse quality of life (Evren et al., 2011). PTSD is also associated with significantly
worse health (Sala, Cox, & Sareen, 2008) and adjusted health status (a measure of quality of life
and functional impairment as it relates to physical health; Mancino et al., 2006). Specifically,
people with PTSD have an increased risk for myocardial infarction, coronary heart disease,
psychogenic nonepileptic seizure, rheumatoid arthritis, thyroid disease, diabetes, psoriasis, and
different types of cancer (Sala, Cox, & Sareen, 2008). A review by Qureshi, Pyne, Magruder,
Schulz, and Kunik (2009) found strong evidence for a link between PTSD and arthritis, but it
also found conflicting evidence for links between PTSD and stroke, heart disease, and diabetes.
Using NCS-R data, Sledjeski and colleagues (2008) concluded that most types of physical
ailments commonly associated with PTSD could be attributed to repeated trauma exposure. The
exception was headache, which was significantly associated with PTSD even after controlling
for trauma exposure. Most of the other chronic physical complaints included in the study were
significantly associated with the number of traumas, except for high blood pressure and epilepsy.
On the other hand, Del Gaizo, Elhai, and Weaver (2011), using NCS-R data, found that PTSD
mediated the relationship between a number of different traumatic experiences and
gastrointestinal, musculoskeletal, and/or cardiovascular health problems, suggesting that trauma
affected health indirectly through the effects of PTSD. This finding is in line with some earlier
research (e.g., Taft, Vogt, Mechanic, & Resick, 2007). Interestingly, Del Gaizo and colleagues
found that substance use/abuse did not mediate the relationship between PTSD and physical
health problems, thus discounting another possible explanation for how trauma affects health.
Trauma-Informed Care in Behavioral Health Services 1-49
It is unclear to what extent increased health problems linked with trauma reflect physiological
differences (e.g., related to increased arousal) versus worse self-care (Sala et al., 2008). Some
research has found that people with PTSD are less likely to follow medication regimens, which
can also contribute to worse health outcomes (Shemesh et al., 2004). Services that address
trauma have been found effective in improving physical health and promoting better health-
related behaviors (Weissbecker & Clark, 2007). Individuals with PTSD also frequently have
chronic pain (Asmundson, Abrams, & Collimore, 2008; Asmundson & Katz, 2009). According
to NCS-R data, people with episodic migraines or chronic daily headaches are significantly more
likely than others to have PTSD (according to both lifetime and past-year data; Peterlin et al.,
2011). McWilliams, Cox, and Enns (2003), using NCS data, found that PTSD was associated
with 3.7 times the likelihood of also having a chronic pain complaint. Asmundson and Katz
(2009) reviewed research and theory concerning the relationship of PTSD to chronic pain and
suggested two theories to explain the relationship: a mutual maintenance model in which PTSD
exacerbates pain and vice versa and a model in which individuals have a shared vulnerability
(perhaps genetic) that predisposes them to develop PTSD and chronic pain conditions.
Both trauma and PTSD also affect family relationships and the behavioral health of family
members who did not experience the trauma or do not have the disorder, and these effects can be
lasting. For example, children of mothers who endured physical and/or emotional abuse in
childhood have more pronounced physiological responses indicative of anxiety than children of
mothers who were not abused as children (Jovanovic et al., 2011), and increased maternal PTSD
symptoms are associated with a number of other markers indicating worse behavioral health in
children (Bosquet et al., 2011). So too, adults whose parents had PTSD have a strong and
significantly greater risk of having PTSD themselves, but the association between parental
trauma exposure and PTSD in the absence of parental PTSD is rather weak (Yehuda, Halligan, &
Bierer, 2001). However, according to the same research, greater parental trauma exposure was
associated with significantly higher rates of depressive disorder among offspring. In addition,
children of adults with PTSD were more likely to report childhood trauma, which in turn was
associated with increased risk for PTSD in adulthood (Yehuda, Halligan, & Grossman, 2001).
A number of reviews have found evidence that, in families where one or more parents are
veterans with PTSD, there are higher rates of marital problems, more parenting problems, a
greater likelihood of family violence, worse perceived parenting behavior, more behavioral
health problems among children and partners, and worse academic performance by children,
even when controlling for such potentially confounding factors as substance abuse and the
strength of the relationship prior to PTSD (e.g., Erbes, 2011; Galovski & Lyons, 2004; Karney et
al., 2008; Monson, Taft, & Fredman, 2009). The relationship between PTSD symptoms and poor
family functioning has been found to persist for as many as 14 years for some individuals
(Koenen, Stellman, Sommer, & Stellman, 2008). Avoidance/numbing PTSD symptoms have the
strongest association with family dissatisfaction and problems with intimate relations (Renshaw,
Blais, & Caska, 2011), whereas hyperarousal PTSD symptoms have been associated with
increased aggression and violent behavior for veterans (Elbogen, Fuller et al., 2010).
Other research conducted with veterans indicates that the relationship between PTSD and family
functioning is complex; a partner’s perceptions of the veteran’s PTSD symptom severity, what
the partner attributes the PTSD to, and how great the partner perceives his or her own burden to
be as a result of the PTSD all affect the degree to which the partner’s own behavioral health is
1-50 Part 3, Section 1—A Review of the Literature
influenced (Renshaw, Blais, & Caska, 2011). For example, in research conducted with 49 male
National Guard members returning from deployment, symptoms of PTSD and depression among
their wives were not correlated with veterans’ actual PTSD symptom scores, but instead with the
wives’ own ratings of perceived symptoms among their husbands (Renshaw, Rodrigues, &
Jones, 2008). The wives’ symptom severity was greatest when they perceived high symptom
severity in their husbands, even when their husbands perceived their own symptom levels low.
PTSD also appears to impair the ability to use resources that could help individuals overcome
that disorder and other negative trauma effects, thus perpetuating PTSD symptoms. Johnson,
Palmieri, Jackson, and Hobfoll (2007) evaluated resource loss (using the Conservation of
Resource–Evaluation) for 225 inner-city women who reported being victims of interpersonal
violence during childhood or adulthood. PTSD assessed at an initial interview was significantly
related to resources lost 6 months later, even after controlling for resources lost at the initial
assessment and for depressive symptoms. In particular, the authors found that emotional
numbing symptoms of PTSD accounted for the majority of the women’s resource loss.
In research conducted with veterans, PTSD is associated with a significantly higher likelihood of
being unemployed (Savoca & Rosenheck, 2000; Zivin et al., 2011), as is greater PTSD symptom
severity (Smith, Schnurr, & Rosenheck, 2005). Among veterans, PTSD is associated with
decreased productivity (Savoca & Rosenheck, 2000) and greater occupational impairment
(Schnurr & Lunney, 2011). Kessler (2000) observed that, according to NCS data, individuals
with PTSD had significantly more lost work time compared with those who did not have the
disorder and experienced an amount of work-related impairment comparable to that experienced
by people with major depression. Research conducted with nonveterans seeking treatment for
PTSD and/or alcohol use disorders also found that individuals who had both were significantly
more likely than those who had only one of the two disorders to be unemployed, have low
income, and not have a spouse or intimate partner (Riggs, Rukstalis, Volpicelli, Kalmanson, &
Foa, 2003).
Malta, Levitt, Martin, David, and Cloitre (2009) evaluated work-related functional impairment
among a group of 95 individuals who had PTSD symptoms related to the 9/11 attack. They
found that PTSD symptoms, particularly numbing symptoms, were significantly related to work-
related impairment, as were having low expectancies about one’s ability to manage negative
feelings, greater feelings of social discomfort, greater expectations of being disliked by others,
and certain demographic factors (e.g., income level, relationship status). Thorp and Stein (2005)
reviewed a number of studies indicating that people with PTSD, compared with people with
trauma exposure but no PTSD and people in primary care settings with no current mental
disorders, had significantly greater impairment in several areas, including employment. The
authors also noted that many of the studies reviewed found a level of impairment comparable to
major depression.
Other Disorders That May Be Related to Trauma
Other behavioral health disorders besides PTSD have been linked to both trauma exposure and
traumatic stress reactions—at times, it is difficult to tease out which is the contributing factor, so
both are discussed together in the following sections. The various disorders comprising SMI,
which include psychotic disorders and bipolar disorder, are often grouped together in the
literature and hence are discussed together. There is also evidence linking trauma exposure to
Trauma-Informed Care in Behavioral Health Services 1-51
other types of anxiety disorders, depression, certain personality disorders, eating disorders,
substance use disorders, and psychotic disorders.
In addition, PTSD frequently co-occurs with other behavioral health disorders and has been
associated in a number of studies with significantly higher rates of a number of different
disorders. For example, in the NCS-R, Kessler and colleagues (2005) found the following co-
occurring disorders:
Mood disorders (e.g., major depression, dysthymia)
Other anxiety disorders (e.g., GAD, OCD)
Impulse control disorders including oppositional–defiant disorder and intermittent explosive
disorder, but not conduct disorder
Alcohol use/dependence (with no significant association with drug use/dependence
disorders)
NCS data show that the norm for people with PTSD is to have at least one co-occurring
behavioral health disorder; 88 percent of men and 79 percent of women with PTSD have at least
one other diagnosis, and 59 percent of men with PTSD and 44 percent of women have three or
more diagnoses (Kessler et al., 1995). Kessler (2000) also presented NCS data indicating that a
prior PTSD diagnosis significantly increased the risk of subsequently developing a substance use
disorder, major depression, dysthymia, mania, GAD, panic disorder, social phobia, simple
phobias, and/or agoraphobia.
Substance use disorders
Numerous studies have found that the use of alcohol and/or illicit drugs increases risk for a
number of different types of trauma. For example, in a meta-analysis of studies evaluating the
relationship between alcohol use and injury, Taylor and colleagues (2010) found a dose–
response relationship between the amount of alcohol consumed and the odds of having vehicular
crashes and nonvehicular accidents. Other research conducted with emergency room patients
indicated a significant association between blood alcohol level and an increased likelihood of
sustaining a violence-related injury (Cherpitel, 1997). As expected, people with substance use
disorders are at increased risk for a number of different types of trauma besides accidents,
including violent victimization (Farley, Golding, Young, Mulligan, & Minkoff, 2004).
According to NESARC data, people with a past-year diagnosis of alcohol use disorder, cocaine
use disorder, and/or opioid use disorder all had significantly elevated risk for having been
victims of crime in the prior year, although not necessarily violent crime (Vaughn et al., 2010).
A history of trauma exposure, whether or not the individual has a traumatic stress reaction, is
associated with increased risk for substance use disorders (Farley et al., 2004). In a sample of
959 clients receiving outpatient substance abuse treatment services, Farley and colleagues (2004)
found that 88.6 percent reported at least one traumatic event. Among men, the most commonly
reported traumas were serious accidents (reported by 39.9 percent), being robbed (38.2 percent),
and seeing someone killed or injured (37.7 percent). Among women, the most common traumas
were rape (47.4 percent), other sexual assault (44 percent), and serious accidents (40.4 percent).
Histories of multiple traumas are also common among people in treatment for substance use
disorders, with 82.7 percent of one inpatient sample from Great Britain reporting two or more
trauma events (Reynolds et al., 2005).
1-52 Part 3, Section 1—A Review of the Literature
Certain types of trauma appear to be associated with increased substance use, regardless of
whether that use results in a substance use disorder. Survey data from New York, NY, indicate
that in the 6 months after the 9/11 attack, there was a 30.8 percent increase in the use of
cigarettes, marijuana, and/or alcohol among the general population (Vlahov, Galea, Ahern,
Resnick, and Kilpatrick, 2004). Other studies similarly indicate a rise in alcohol consumption,
binge drinking, illicit drug use, and/or smoking in communities after natural disasters (Adams &
Adams, 1984; Lutz, Kramer, Gonnerman, & Downs, 1995; Office of Applied Studies, 2008).
Data from the Multisite Adult Drug Court Evaluation study of 958 adult offenders who were not
incarcerated and who used illicit drugs indicate that experiencing a physical or sexual assault is
associated with a significant increase in illicit drug use in the year following the assault, even
after controlling for other factors related to drug use (Zweig, Yahner, & Rossman, 2012). These
authors also found that the relationship between assaultive trauma and PTSD was mediated by
depressive symptoms (assessed with a 10-item Likert scale). Similarly, in a large longitudinal
study of violence and women (N=3,006), experiences of physical and/or sexual assault were
associated with a significant increase in the likelihood of using illicit drugs and of alcohol abuse
in the following year (Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997). The use of illicit
drugs, but not the abuse of alcohol alone, was also associated with a significant increase in the
likelihood of being assaulted in the following year.
Although there is evidence that PTSD is associated with a high rate of substance use disorders,
not all studies have found a significant association. Some have found associations only between
certain substance use disorders and PTSD or between substance use disorders and PTSD only for
certain populations. For example, research from the Epidemiologic Catchment Area Study
(ECA) regarding 2,985 participants in North Carolina found a significant association between
drug use disorders and PTSD, but not between alcohol use disorders and PTSD (Davidson,
Hughes, Blazer, & George, 1991). More recently, in the NCS, men with a lifetime PTSD
diagnosis were 2.06 times more likely to also have an alcohol use disorder at some point during
their lives and 2.97 times more likely to have a drug use disorder, compared with men who never
had PTSD (Kessler et al., 1995). For women, PTSD increased the odds of having a substance use
disorder to an even greater degree, with the odds of having an alcohol use disorder being 2.48
times higher compared with women who never had PTSD and the odds of having a drug use
disorder 4.46 times higher.
Interestingly, according to these same data, men with alcohol abuse disorder were actually less
likely (about half as likely) than men without the disorder to have PTSD at some point during
their lives, but men with alcohol dependence disorder were significantly more likely than those
without that disorder to also have PTSD at some point (3.2 times more likely; Kessler et al.,
1997). Women with alcohol abuse disorder were about as likely as other women to have PTSD,
whereas those with alcohol dependence were 3.6 times more likely to have PTSD.
Both trauma exposure and PTSD are related to smoking. Feldner, Babson, and Zvolensky (2007)
reviewed epidemiological data on the relationship of smoking to both trauma exposure and
PTSD. Research has consistently shown that trauma exposure, even without PTSD, is associated
with increased smoking and nicotine dependence. Rates are much higher for individuals who
have experienced rape or other sexual trauma, and for women, but not men, who have
experienced a nonsexual physical assault. For example, in one study, women who had been

Trauma-Informed Care in Behavioral Health Services 1-53
physically assaulted during their lives were 1.82 times more likely to be smoking at the time of
the assessment than were women who had never been assaulted (Acierno, Kilpatrick, Resnick,
Saunders, & Best, 1996). Feldner and colleagues (2007) also found that studies of smoking
among people with PTSD report even higher rates than those found in people with trauma
exposure alone. They concluded that, according to data drawn from multiple studies,
approximately 45 percent of people with PTSD smoke—a rate more than twice as high as that in
the general population.
However, other research indicates that certain types of trauma may increase an individual’s risk
for substance abuse, even in the absence of PTSD. Different types of trauma may differently
affect alcohol consumption and alcohol use disorder risk for individuals who do not develop
PTSD. Using data from Wave 2 of NESARC, Fetzner and colleagues (2011) evaluated the
relative risk of different types of trauma on the development of alcohol use disorders, with or
without co-occurring PTSD. Using a model that adjusted for demographic factors and other co-
occurring behavioral health disorders, they found that, for individuals who did not meet criteria
for PTSD, experiences of childhood trauma (particularly sexual abuse), military combat, and
assaultive violence were all associated with significantly higher rates of alcohol use disorders, as
were having a serious/life-threatening accident, witnessing serious injury/death, having someone
close to you die unexpectedly, and learning of trauma experienced by someone close to you.
Being an unarmed civilian in a war zone and being a refugee were associated with significantly
lower odds of having an alcohol use disorder for individuals without PTSD. For individuals with
PTSD, experiences of childhood trauma (particularly sexual abuse), military combat, and
assaultive violence were all associated with a significantly greater likelihood of having an
alcohol use disorder.
Numerous smaller studies show that prevalence estimates for PTSD among people seeking
treatment for substance use disorders are significantly higher than prevalence estimates obtained
from general population studies. Prevalence estimates differ widely among these studies,
however, depending on the study population and research methodology. Exhibit L-5 summarizes
these figures.
Exhibit L-5
Prevalence of PTSD Among Individuals Who Received Substance Abuse Treatment
Reference
Population
N
Measure(s) Used To
Diagnose PTSD
Lifetime
Preva-
lence
Current
Preva-
lence
Back et al.
(2000)
Cocaine-dependent
individuals in an
outpatient
treatment program
91
Structured Clinical
Interview for DSM-III-R
(SCID-III-R);
National Women’s
Study PTSD Module
(NWS-PTSD);
Diagnostic Interview
Schedule
42.9%
25%
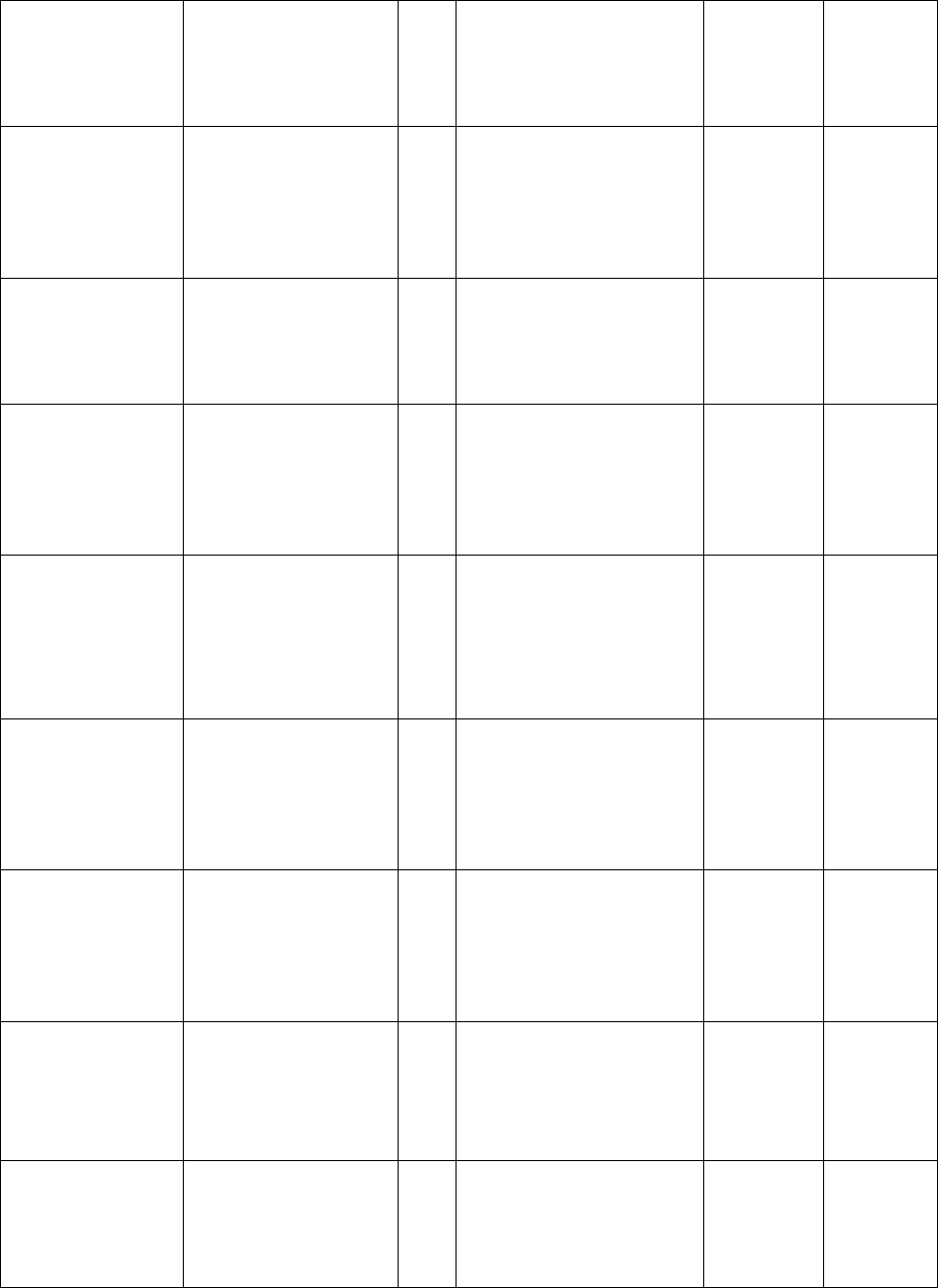
1-54 Part 3, Section 1—A Review of the Literature
Brown, Read, &
Kahler (2003)
Individuals in an
inpatient substance
abuse treatment
program
133
Clinician-Administered
PTSD Scale (CAPS)
41%
Chen and
colleagues,
2011
Clients attending
an inpatient
substance abuse
treatment program
465
Structured Clinical
Interview for DSM-IV
(SCID-IV)
14%
(12.2%
of men;
18.3% of
women)
Dansky,
Saladin, Brady,
Kilpatrick, &
Resnick (1995)
National sample of
women who
received substance
abuse treatment
143
NWS-PTSD Module
50%
29%
Dore, Mills,
Murray,
Teesson, &
Farrugia, 2011
Clients attending
an Australian
inpatient detox
program
253
10-item Trauma
Screening
Questionnaire
(screening for probable
PTSD)
44.9%
(40.9%
of men;
53% of
women)
Driessen and
colleagues
(2008)
Clients seeking
treatment for
substance use
disorders
(Germany)
459
International
Diagnostic Checklists
for DSM-IV;
Posttraumatic
Diagnostic Scale
25.3%
Evren,
Dalbudak,
Cetin, Durkaya,
& Evren (2010)
Men in inpatient
treatment for
alcohol
dependence
(Turkey)
156
CAPS
32.1%
Huang and
colleagues
(2012)
Individuals with
alcohol
dependence
attending inpatient
treatment
196
SCID-IV
21.9%
(15.7% of
men,
35.5% of
women)
Najavits and
colleagues
(1998)
Individuals with
cocaine
dependence in an
outpatient
treatment program
122
Trauma History
Questionnaire (THQ);
PCL
20.5%
Peirce, Kindbom,
Waesche,
Yuscavage, &
Brooner (2008)
Individuals in an
outpatient
substance abuse
treatment program
1440
SCID-IV
3.5%

Trauma-Informed Care in Behavioral Health Services 1-55
Peller, Najavits,
Nelson, LaBrie,
& Shaffer, 2010
DUI offenders (not
necessarily with
substance use
disorders)
attending a 2-week
inpatient program
729
Composite
International
Diagnostic Interview
13%
12%
Reynolds and
colleagues
(2005)
Clients in treatment
for substance use
disorders (United
Kingdom)
52
THQ (Green, 1993);
Posttraumatic Stress
Symptom Scale (Foa,
1993)
51.9%
38.5%
Thompson &
Kingree (1998)
Pregnant women in
a residential
substance abuse
treatment program
96
Civilian Mississippi
Scale for Combat-
Related PTSD (Keane,
Caddell, & Taylor,
1988; diagnosis based
on DSM-IV criteria)
62%
Triffleman,
Marmar,
Dellucchi, &
Ronfeldt (1995)
Male veterans in an
inpatient substance
abuse treatment
program
46
SCID for DSM-III-R,
Version NP-V, PTSD
Module (Spitzer,
Williams, & Gibbon,
1987); Mississippi
Scale for Combat-
Related PTSD (Keane,
Caddell, & Taylor,
1988)
58%
38%
Villagonzalo
and colleagues
(2011)
Clients in a
methadone
maintenance
program
80
PCL—Civilian Version
52.7%
Although less common, prospective studies of PTSD and substance use disorders support the
idea that PTSD, but not necessarily trauma exposure, increases the likelihood that someone
might develop a substance use disorder. For example, a 10-year study of 1,200 members of a
Michigan HMO who were ages 21 to 30 at the initial assessment found that a PTSD diagnosis at
an earlier assessment was associated with a significantly greater risk for subsequently developing
an alcohol use disorder, drug use disorder, and/or nicotine dependence (Breslau, Davis, &
Schulz, 2003). Trauma exposure alone, without PTSD, was not associated with increased risk for
developing these disorders—with one exception, which was that women, but not men, who were
exposed to trauma but did not meet criteria for a PTSD diagnosis subsequently had a
significantly greater risk than did other women for developing alcohol use disorders but not drug
use disorders.
Individuals with PTSD who have a co-occurring substance use disorder, particularly a co-
occurring alcohol use disorder (the most often studied type of disorder) have more severe PTSD
symptoms, a greater chance that PTSD symptoms will return after remission, a greater chance of
1-56 Part 3, Section 1—A Review of the Literature
relapse to substance abuse, more severe symptoms of substance abuse, and more co-occurring
health problems (McCarthy & Petrakis, 2010). For example, a German study of 459 clients in
substance abuse treatment programs found that those with co-occurring PTSD had significantly
more severe substance abuse problems (as measured by ASI scores) than did those with partial
PTSD, trauma exposure without PTSD, or no trauma exposure (Driessen et al., 2008).
Differences in ASI scores were largely accounted for by ASI subscores indicating more severe
psychiatric, family, employment, and drug- related problems among individuals with PTSD.
Individuals with PTSD were also significantly more likely to report frequent substance cravings
and reported a significantly shorter longest period of abstinence from drug use. A study of 1,098
out-of-treatment African Americans who used illicit drugs also found that PTSD was associated
with significantly earlier age of onset for many substance use disorders (Johnson, Striley, &
Cottler, 2006).
PTSD may also affect individuals’ choices regarding substances of abuse. For example, PTSD-
related hyperarousal symptoms have been significantly associated with heroin use among
individuals in substance abuse treatment (Tull, Gratz, Aklin, & Lejuez, 2010) and (along with
reexperiencing symptoms) with marijuana use among individuals in a methadone maintenance
program (Villagonzalo et al., 2011). However, an Australian study of individuals attending an
inpatient detoxification program found no significant differences in the primary substance of
concern between those who did and did not have current PTSD (Dore et al., 2011).
Exposure to certain types of trauma may also affect treatment seeking. Among a group of 40
women with substance use disorders who were incarcerated, severity of childhood sexual abuse
was negatively correlated with the number of prior episodes of substance abuse treatment (Peltan
& Cellucci, 2011). Simpson (2002) had a similar finding with a group of 72 women in public
substance abuse treatment programs, although, unlike Peltan and Cellucci (2011), she also found
that greater use of mental health services correlated with severity of childhood sexual abuse.
Among individuals in treatment for PTSD, co-occurring substance use disorders are associated
with clients being significantly more likely to drop out of treatment (Difede et al., 2007) and
having worse treatment outcomes in a number of areas (Ouimette, Brown, & Najavits, 1998). A
study of 428 clients who were being treated for cocaine dependence found that those who had
co-occurring PTSD, compared with those without current PTSD, entered treatment with
significantly greater impairments in a number of areas, so that even when they improved at a
similar rate, their outcome measures were still worse at the end of treatment (Najavits et al.,
2007). Individuals with PTSD were also less likely to show significant improvements in a
number of areas, including alcohol use, legal problems, family/social problems, and psychiatric
problems (as measured by ASI subscales).
Reasons for co-occurrence of trauma-related disorders and substance use disorders
Chilcoat and Breslau (1998) suggested three major causal pathways to explain the relationship
between PTSD and substance use disorders: people with PTSD use substances of abuse in an
attempt to counteract or cope with PTSD symptoms (a “self-medicate” process); people who
abuse substances have high trauma rates because of the effects of their substance abuse (i.e., they
are at high risk for trauma and hence PTSD); and substance abuse, directly or indirectly,
increases risk for developing PTSD in the wake of trauma exposure (i.e., these individuals have a
high degree of susceptibility to PTSD).
Trauma-Informed Care in Behavioral Health Services 1-57
The self-medication hypothesis (Khantzian, 1997) holds that individuals with PTSD use
substances as a way to manage or avoid distressing PTSD symptoms (e.g., intrusive memories
and physical arousal). Substances such as alcohol, cocaine, barbiturates, opioids, amphetamines,
or other drugs are frequently abused in attempts to relieve or numb emotional pain or forget the
traumatic event. Whether or not substance abuse develops because the individual is using
substances to self-medicate, PTSD does appear to increase risk for developing substance use
disorders. For example, in the NCS, having PTSD increased the risk of subsequently meeting
criteria for alcohol abuse disorder by 2 times for men and 2.1 times for women, of alcohol
dependence disorder by 3 times for men and 3.2 times for women, of drug abuse disorder by 2.2
times for men and 3.7 times for women, and of drug dependence by 3.7 times for men and 4.2
times for women (Kessler, 2000).
The high-risk hypothesis, proposed by Cottler, Compton, Mager, Spitznagel, & Janca (1992),
states that drug and alcohol use places people who use substances in high-risk situations increase
their chances for being exposed to events that lead to PTSD. In a review of research on the co-
occurrence of substance use disorders and PTSD, Johnson (2008) observed that a greater
likelihood of engaging in violence (as either victim or perpetrator) among people with substance
use disorders is likely involved in the high PTSD rates among that population. Among other
research, she observed that some studies have found that the type and intensity of substances
abused affect trauma exposure and hence PTSD.
The susceptibility hypothesis holds that people who use substances are more susceptible to
developing PTSD after exposure to trauma than people who do not use substances. This
increased vulnerability may be a result of the failure to develop effective stress management
strategies. Changes in brain chemistry or damage to neurophysiological systems because of
extensive substance use could also contribute to increased susceptibility (Chilcoat and Breslau,
1998).
Kilpatrick and colleagues (1997) suggested a fourth possible explanation regarding the
relationship between PTSD and substance use. They proposed a bidirectional relationship in
which use is associated with a higher risk of victimization, and victimization tends to escalate
substance use. Clients who have co-occurring PTSD and substance use disorders tend to perceive
the two as linked, and many observe that when one disorder improves or worsens, so does the
other (Brown, Read, & Kahler, 1998).
It is possible that there is no direct causal pathway between PTSD and substance use disorders.
Both disorders may be caused by a third factor, or both disorders may share common genetic
causes (Meyer, 1986). Twin studies have indicated that a genetic component common to both is
likely, although environmental factors also play a role (Xian et al., 2000).
Mood disorders
Laugharne, Lillee, & Janca (2010) found good evidence that a significant number of people will
develop major depression in the wake of trauma exposure. In addition, trauma exposure may
contribute to the development or return of depressive symptoms. The research they reviewed also
indicated that preexisting symptoms of depression may increase risk for developing PTSD and
have also been linked to having more severe PTSD. However, other researchers (e.g., Breslau,
Davis, Peterson, & Schultz, 2000) have found that trauma exposure, in the absence of PTSD,
1-58 Part 3, Section 1—A Review of the Literature
does not increase risk for depression; thus, they suggest that PTSD is responsible for elevated
rates of depression among those who have been exposed to trauma.
The effects of trauma on depression may also depend on the type of trauma experienced. Using
data from an Australian twin study, McCutcheon and colleagues (2010) found that, among
individuals who had experienced trauma, those who were the victims of assaultive violence had
the greatest risk for major depression. In the context of trauma, it is important to note that
symptoms of PTSD and depression often overlap (i.e., sleep problems, difficulty concentrating,
avoidance/withdrawal, lack of interest/pleasure, and feelings of isolation may all be symptoms of
either disorder; Brady, Killeen, Brewerton, & Lucerini, 2000). These reviewers also noted that
there are physiological changes common to the two disorders involving the hypothalamic–
pituitary–adrenal axis and the production of corticotrophin-releasing factor.
Larger studies, such as the NCS (Kessler et al., 1995) and the NCS-R (Kessler, Berglund et al.,
2005), have found that PTSD is associated with significantly higher rates of all depressive
disorders. In the NCS, lifetime rates of all affective disorders were significantly higher for
individuals who had PTSD at some point during their lives compared with those who did not,
with larger increases in the odds ratios found for affective disorders in men than in women
(Kessler et al., 1995). For example, PTSD was associated with 4.1 times greater odds of having
major depression for women and 6.9 times greater odds for men. In the NCS-R, individuals who
met criteria for PTSD in the prior year were significantly more likely than all others to also have
major depression, dysthymia, or bipolar disorder (Kessler, Berglund et al., 2005).
In Wave 2 of NESARC, people who had been diagnosed with PTSD at some point during their
lives were also 2.6 times as likely to have had a mood disorder, 1.9 times as likely to have had
major depression, 1.3 times as likely to have had dysthymic disorder, 2.1 times as likely to have
had bipolar I disorder, and 1.4 times as likely to have had bipolar II disorder. Other studies have
also found high rates of co-occurring PTSD among people with depression and vice versa. For
example, data from the Sequenced Treatment Alternatives to Relieve Depression study for 1,376
adults being treated for major depression indicated that 18.8 percent had current co-occurring
PTSD (Rush et al., 2005).
Using both prospective and retrospective data from a large study of young adults (N=1,007),
Breslau and colleagues (2000) found that having had PTSD at some time prior to the initial
assessment was associated with 2.8 times greater risk for developing major depression, whereas
having a prior diagnosis of major depression was associated with 3.7 times greater risk for
developing PTSD and 2.1 times greater risk for being exposed to trauma. However, prior trauma
exposure was not associated with a significant increase in risk for major depression. They also
found that trauma exposure occurring during the study further increased risk for developing
depression among those who had prior PTSD, but not among those who did not have PTSD.
A number of explanations have been proposed to explain the relationships among trauma, PTSD,
and depression. Breslau and colleagues (2000) reviewed literature proposing five different
possibilities: preexisting depression increases risk for PTSD; PTSD increases risk for depression;
depression increases risk for trauma (which then increases PTSD risk); there is a shared
vulnerability to both PTSD and depression (e.g., a shared genetic factor that increases risk for
both); or traumatic experiences increase risk for depression and potentially cause PTSD. Breslau
Trauma-Informed Care in Behavioral Health Services 1-59
and colleagues concluded, based on their own research, that trauma alone does not seem to
contribute to the development of major depression, but PTSD does. Other researchers have
argued that symptoms of both PTSD and depression represent the same, underlying construct
(e.g., Elhai et al., 2011).
A study of 267 women with low incomes who were receiving treatment for depression found that
those with co-occurring PTSD had more severe depression, more anxiety, and greater functional
impairment (Green et al., 2006). Another study that evaluated depression and trauma histories for
792 adults also found that prior trauma, especially childhood abuse, was associated with
significantly greater severity of depression (measured with the Beck Depression Inventory), even
after controlling for demographic factors and family mental disorder history (Wingo et al., 2010).
Earlier studies (e.g., Blanchard, Buckley, Hickling, & Taylor, 1998) also found that among
individuals with PTSD, those who have co-occurring depression have greater role impairment,
more subjective distress, and lower rates of remission from PTSD.
A study of 178 veterans in treatment for co-occurring depression and substance use disorders
found that clients with PTSD had more severe depressive symptoms (assessed with the Hamilton
Depression Rating Scale), but they experienced a decrease in depressive symptoms following
treatment similar to that seen in clients without PTSD (Norman, Tate, Wilkins, Cummins, &
Brown, 2010). More information on the relationship of traumatic stress reactions to bipolar
disorder can be found in the “Serious Mental Illness” section. The planned TIP, Managing
Anxiety Symptoms in Behavioral Health Services (SAMHSA, planned d), discusses the
relationship of mood and anxiety disorders (including PTSD) in more detail.
Anxiety disorders
A review by Laugharne and colleagues (2010) found some evidence that trauma exposure can
contribute to the development of anxiety disorders, particularly GAD. They also found that
preexisting anxiety symptoms and/or anxiety sensitivity may increase an individual’s risk for
developing PTSD. Brady and colleagues (2000) reviewed research that indicates that PTSD
frequently co-occurs with anxiety disorders, particularly panic disorder and SAD.
A number of studies confirm that PTSD frequently co-occurs with panic disorder. This co-
occurrence may be even more common among individuals with certain cultural backgrounds,
such as people from Southeast Asia (Hinton et al., 2000; Hinton et al., 2001). Cougle, Feldner,
Keough, Hawkins, and Fitch (2010) reviewed earlier studies that indicate that between 7.3 and
18.6 percent of men with PTSD and 12.6 and 17.5 percent of women with PTSD have co-
occurring panic disorder. They noted that other research indicates that people with PTSD are
about twice as likely as others to have had a panic attack (whether or not they have had panic
disorder). Individuals who have been the victims of assaultive violence have greater risk for
panic disorder than do those who have only experienced other kinds of trauma (McCutcheon et
al., 2010).
A study of 884 veterans found high rates of co-occurrence between PTSD and panic disorder,
with more individuals (n=40) having both PTSD and panic disorder than panic disorder alone
(n=33; Gros, Frueh, & Magruder, 2011). This study also found that individuals with PTSD who
had co-occurring panic disorder had more severe PTSD, according to PCL scores, than did those
who had PTSD alone. According to NCS-R data, 35 percent (n=72) of individuals with a past-
1-60 Part 3, Section 1—A Review of the Literature
year diagnosis of PTSD reported having had one or more panic attacks (Cougle et al., 2010).
Individuals with PTSD who reported panic attacks also had greater PTSD-related disability,
more traumatic experiences during their lives, and more time unemployed or absent from work,
and they were more likely to have co-occurring depression and/or substance use disorders.
Some research indicates that individuals who have panic attacks have a greater risk than others
for developing PTSD following trauma exposure (Adams & Boscarino, 2011). Marshall-Berenz,
Vujanovic, and Zvolensky (2011) also found, in a sample of 91 individuals who had experienced
trauma, that a history of panic attacks in the absence of panic disorder was significantly related
to PTSD-related reexperiencing and hyperarousal symptoms. Hinton, Hofmann, Pitman, Pollack,
and Barlow (2008) proposed that panic attacks may be triggered by sensations associated with
traumatic experiences, and in turn, panic attacks may worsen PTSD by increasing arousal and
reactivating traumatic memories. This phenomenon may be affected by cultural beliefs. Hinton,
Nickerson, and Bryant (2011) observed that, among Cambodian refugees, worry often
precipitated panic attacks and increased trauma recall (including flashbacks) and hyperarousal,
which in turn were associated with more severe PTSD.
SAD also frequently co-occurs with PTSD. Collimore, Carleton, Hofmann, and Asmundson
(2010) reviewed research on this co-occurrence. Studies included in their review found that rates
of past-year SAD among individuals with PTSD ranged from 4.3 percent to 72 percent in both
clinical and nonclinical studies with different samples (e.g., veterans, disaster survivors). The
authors considered a number of different factors that may contribute to this co-occurrence,
including common genetic causes, heightened anxiety sensitivity, fears of negative evaluation,
intolerance of uncertainty, increased guilt and/or shame, and co-occurring depression. For
individuals with high levels of social anxiety, episodes of social embarrassment may be
perceived as more traumatic than other events that are typically considered traumatic (Carleton,
Peluso, Collimore, & Asmundson, 2011). Other researchers have observed that there is an
element of experiential avoidance that may be involved in the maintenance of both SAD and
PTSD, which may also explain why the disorders frequently co-occur (e.g., Kashdan, Morina, &
Priebe, 2009).
Personality disorders
Personality disorders frequently co-occur with other behavioral health disorders, and PTSD is
not uncommon among individuals with many of these disorders. Because of its size and
methodology, NESARC provides the most accurate epidemiological data on personality
disorders in the United States. According to NESARC Wave 2 data regarding individuals who
had been exposed to trauma, those who developed PTSD were significantly more likely to have
borderline, narcissistic, and/or schizotypal personality disorders than were those who did not
develop PTSD (Pietrzak et al., 2011a). For women, but not men, PTSD was also associated with
significantly higher odds of having OCD. According to the initial NESARC data, 19.5 percent of
respondents with a past-year diagnosis of narcissistic personality disorder had co-occurring
PTSD, and 25.7 percent of those with a lifetime diagnosis of narcissistic personality disorder had
co-occurring PTSD (Stinson et al., 2008).
Rates of co-occurring PTSD are also high among people with borderline personality disorder
(BPD). In NESARC, 31.2 percent of people with BPD in the past year also had PTSD in that
year, whereas 39.2 percent of those with a lifetime diagnosis of BPD also had PTSD at some
Trauma-Informed Care in Behavioral Health Services 1-61
point (Grant et al., 2008). However, because of the overlap in symptoms between the two
disorders and the high rates of early trauma among those with BPD, there is also an ongoing
debate as to whether BPD may in fact be a traumatic stress reaction (Lewis & Grenyer, 2009).
In NESARC, individuals with schizotypal personality disorder had increased risk for co-
occurring PTSD; 38.1 percent of women and 21.6 percent of men with schizotypal personality
disorder also had co-occurring PTSD (Pulay et al., 2009). Studies have also found high rates of
co-occurring PTSD among individuals with ASPD. In reviewing prior research, Goldstein,
Compton, and Grant (2010) observed that studies have found that between 8 and 21 percent of
people with ASPD have PTSD. They also noted that, in NESARC, individuals with PTSD who
had a co-occurring diagnosis of ASPD were significantly more likely to have a number of other
co-occurring disorders, including substance use disorders, bipolar I disorder, and a number of
other personality disorders.
In a large study of personality disorders, the majority (n=102) of individuals with PTSD at the
start of the 7-year study (n=142) achieved remission during the study; 34 percent of those who
did achieve remission had at least one relapse to PTSD (Ansell et al., 2010). Schizotypal
personality disorder was the only disorder of the four included in the study that was associated
with significantly lower remission (compared with individuals with no personality disorder,
avoidant personality disorder, BPD, or OCD). Research has found that individuals who
experience significant trauma (e.g., sexual abuse) as children are at increased risk for developing
personality disorders (Pratchett et al., 2010). There are gender differences in this pattern—
women are more likely to develop BPD and men are more likely to develop ASPD—but
individuals with both of those personality disorders are significantly more likely than those
without either disorder to have experienced childhood abuse.
Eating disorders
Brewerton (2007) reviewed a number of studies that found high rates of trauma and PTSD
among both men and women with eating disorders. Most eating disorder research does not
include men. Brewerton (2007) found that although child sexual abuse is a particularly strong
risk factor for later developing an eating disorder, other forms of trauma appear to increase the
likelihood of developing eating disorders as well. He cited studies indicating that trauma is more
common among women who have eating disorders with bulimic symptoms than among those
who have eating disorders without such symptoms, and he noted that women with bulimic
disorders are more likely than women without eating disorders or those with nonbulimic
disorders to have had multiple episodes of trauma. Although trauma histories are not associated
with any significant differences in severity of eating disorder symptoms, women with eating
disorders who have trauma histories are more likely than other women with eating disorders to
have major depression, substance use disorders, BPD, and anxiety disorders (including PTSD).
Swinbourne and Touyz (2007) reviewed research that provides epidemiological data on the co-
occurrence of anxiety and eating disorders. They found PTSD rates ranging from 11 to 52
percent in samples of people (typically women) with eating disorders but also noted that studies
that included individuals with both anorexia nervosa and bulimia nervosa found PTSD to be
significantly more common among those with the latter disorder. Among women with histories
of childhood sexual abuse (N=50), eating disorders were associated with significantly lower self-
1-62 Part 3, Section 1—A Review of the Literature
esteem and significantly more symptoms of depression at the conclusion of treatment and at a 6-
month follow-up assessment (Harper, Richter, & Gorey, 2009).
Serious mental illness
SMI typically includes schizophrenia, schizoaffective disorder, and bipolar disorder. Individuals
with these disorders have increased risk for a number of different types of trauma and for PTSD.
According to NESARC data, people with psychotic disorders had a 78 percent greater chance of
having been the victim of violence in the year prior to assessment, but the difference was not
significant, given the relatively small numbers of people with such disorders included in the
study (Vaughn et al., 2009). However, mood disorders, which include bipolar disorder, were
found to be associated with a significantly greater likelihood of being a victim of violent crime
(people with bipolar disorder had an increased risk of 32 percent in the adjusted model).
People with SMI also appear to have increased risk for trauma from accidents. In a study
involving 1,709 admissions to a public hospital trauma unit, individuals with mental disorders
(not limited to SMI, but involving psychosis/schizophrenia in 29 percent of cases) were more
than twice as likely to have an unintentional injury (Wan et al., 2006). Other research indicates
that people with psychosis (Kilcommons, Morrison, Knight, & Lobban, 2008; Read, van Os,
Morrison, & Ross, 2005) and those with bipolar disorder (Garno, Goldberg, Ramirez, & Ritzler,
2005; Goldberg & Garno, 2005) have high rates of childhood physical and/or sexual abuse. A
large British study (N=8,580) found significant associations between a number of traumatic
childhood experiences and increased likelihood of psychosis, with an especially strong
association between childhood sexual abuse and psychosis (Bebbington et al., 2004).
Goldberg and Garno (2005) evaluated trauma histories for 100 consecutive admissions to a
bipolar disorders research clinic; 24 percent of participants had current PTSD. However, current
PTSD was significantly more common (affecting 35 percent) for individuals with childhood
traumatic experiences compared with those who did not report such experiences (13 percent of
whom had PTSD). A greater number of childhood traumatic experiences correlated with a
greater likelihood of PTSD in adulthood.
Whether trauma, particularly childhood trauma, contributes to the development of SMI is still a
subject for debate; some evidence supports the fact that it does, and some does not. An
Australian study of 1,612 individuals (1,327 female) who had been sexually abused in childhood
(according to police records) and who had histories of receiving behavioral health services found
no significant increase in psychotic disorders compared with a general population control group,
but risk for psychotic disorders was elevated in both men and women who had histories of
childhood sexual abuse (e.g., women who were sexually abused as children had 1.5 times greater
risk for psychotic disorders as adults; Spataro, Mullen, Burgess, Wells, & Moss, 2004). Critics of
the study, though, have pointed to methodological problems, including the fact that the study was
limited to those whose abuse was recognized while they were children and who received services
at the time; it excluded individuals whose abuse went unrecognized and who thus had more
chronic and severe trauma histories (Read & Hammersley, 2005).
A German study, which assessed 2,524 adolescents and young adults (ages 14 to 24) and then
reassessed them an average of 42 months later, found that trauma reported at the initial
assessment was significantly associated, in a dose–responsive manner, with the onset of
Trauma-Informed Care in Behavioral Health Services 1-63
psychotic symptoms at the follow-up assessment (Spauwen, Krabbendam, Lieb, Wittchen, & van
Os, 2006). All of the types of trauma evaluated were associated with significant increases in risk
for psychotic symptoms, but the largest increase in relative risk for psychosis was associated
with sexual trauma. Another German study conducted with 4,045 adults ages 18 to 64 also found
that childhood abuse reported during an initial assessment was associated with 11.5 times greater
risk for reporting psychotic symptoms at a follow-up 2 years later (Janssen et al., 2004).
PTSD also appears to cause, for some individuals, some psychotic symptoms (see Braakman et
al., 2009), and studies that examine the relationship between trauma and psychotic symptoms
have found a significant association. Read and colleagues (2005) found evidence for a “strong
relationship” between childhood abuse and both hallucinations and delusional ideations. Read,
Agar, Argyle, and Aderhold (2003) found that sexual assault in adulthood was significantly
associated with hallucinations, delusions, and thought disorder, whereas childhood physical
and/or sexual abuse was significantly associated with hallucinations but not delusions or thought
disorder.
Kilcommons and colleagues (2008) evaluated psychotic experiences among 40 survivors of
sexual assault and 40 individuals who did not have sexual assault histories and interviewed a
subset of 26 from the first group. They found that study participants who had been sexually
assaulted were significantly more likely than those in the control group to have experienced
psychotic symptoms (both delusional ideations and hallucinations). Sixty-six percent of
survivors of sexual abuse met criteria for PTSD, but an even larger percentage reported
psychotic symptoms (with 75 percent reporting the most common symptoms in the study). A
study with a smaller sample (n=32, 53 percent with current PTSD) of individuals with psychotic
disorders (Kilcommons & Morrison, 2005) also found that the severity of traumatic experiences
was significantly associated with severity of PTSD and severity of psychotic symptoms.
Some evidence suggests that the experience of psychosis itself, and attendant issues such as
forced hospitalization, may be traumatic and contribute to PTSD symptoms (Beattie, Shannon,
Kavanagh, & Mulholland, 2009). Sherrer (2011), in an article discussing reasons for high PTSD
rates among people with SMI, reviewed studies that found that between 24 and 43 percent of
people with SMI have co-occurring PTSD. Some literature also indicates that PTSD rates are
higher for individuals with bipolar disorder than for those with schizophrenia spectrum disorders
(O’Hare, Sherrer, & Shen, 2006).
Achim and colleagues (2011) conducted a meta-analytic review of studies giving prevalence data
on co-occurring anxiety disorders among individuals diagnosed with schizophrenia. According
to pooled prevalence data from 52 studies (N=4,032), 12.4 percent had current PTSD. However,
the authors noted a wide variation in rates among the studies they included.
In the NCS-R, 30.9 percent of respondents who had a lifetime diagnosis of bipolar I disorder and
34.3 percent of those with bipolar II also had PTSD at some point during their lives (Merikangas
et al., 2007). Some studies have found lower rates of co-occurring PTSD, however. One study of
500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder found
that 17.2 percent met criteria for a PTSD diagnosis at some point during their lives, and 5.1
percent had current PTSD at the time of assessment, with somewhat higher rates for participants
with bipolar I disorder and somewhat lower rates for those with bipolar II (Simon et al., 2004).
1-64 Part 3, Section 1—A Review of the Literature
Provencher, Hawke, and Thienot (2011) reviewed research on the co-occurrence of bipolar and
anxiety disorders (including PTSD). Some research has found that people with bipolar disorder
who have co-occurring PTSD, compared with others with bipolar disorder, have longer affective
episodes, are more likely to have a recurrence of affective episodes, are more likely to have rapid
cycling, take longer to achieve remission, have greater risk for co-occurring substance use
disorders, have worse health-related quality of life, and are more likely to attempt suicide (Garno
et al., 2005; Goldberg & Garno, 2005).
Other research indicates that individuals with schizophrenia or schizoaffective disorder who have
PTSD also have more severe anxiety and dysphoria symptoms (according to the Positive and
Negative Syndrome Scale [PANSS] and the Endler Multidimensional Anxiety Scale) compared
with those who do not have co-occurring PTSD (Newman, Turnbull, Berman, Rodrigues, &
Serper, 2010). This study also found that a greater number of past traumatic experiences was
associated with more severe psychosis, and a higher number of past experiences of victimization
was associated with more severe cognitive/autistic symptoms (on the PANSS).
Several researchers have argued that PTSD with secondary psychotic features should be
considered as a separate diagnostic category. Braakman, Kortmann, and van den Brink (2009)
defined this diagnostic category as a syndrome in which an individual experiences PTSD
symptoms followed in time by psychotic symptoms and found that certain facets of the syndrome
distinguish it from PTSD and schizophrenia (e.g., elevated plasma dopamine β-hydroxylase and
cerebrospinal concentrations of corticotrophin-releasing factor).
Possible explanations for high PTSD rates among people with SMI are that SMI predisposes
people to trauma, that SMI directly or indirectly causes or contributes to developing PTSD (e.g.,
because psychotic episodes are themselves traumatic), and/or that traumatic experiences (e.g.,
childhood trauma) contribute to the development of SMI as well as PTSD. However, the most
commonly held theory is that SMI affects how individuals interpret traumatic experiences and
thus increases the likelihood of having PTSD as well as PTSD severity (Sherrer, 2011).
Still, rates of crime victimization are high for people with SMI. Teplin and colleagues (2005)
used data from a survey of 936 patients with SMI who attended mental health programs in the
Chicago area from 1997 to 1999 and data from the National Crime Victimization Survey for
residents of large cities during the same period and determined that, compared with others
residing in large cities, people with SMI were over 10 times more likely to have been victims of
violent crime in the prior year.
Sherrer (2011) theorized that high rates of co-occurring PTSD among people with SMI are
attributable to problems in cognitive appraisal related to potentially traumatic events that may
make people less objective in evaluating the nature of those events. She suggested that cognitive
restructuring may be particularly useful for this population as a way to modify problematic
cognitions related to trauma.
Trauma-Informed Care in Behavioral Health Services 1-65
Screening and Assessing Trauma and Trauma-Specific
Disorders
Briere (2002) and others recommended that any behavioral health assessment inquire about
trauma histories and assess traumatic stress reactions. Briere observed that assessments should
elicit information about the client’s psychological functioning prior to the trauma; the exact
nature of the traumatic event(s), including type, duration, frequency, and severity; social and
family support available after the trauma; co-occurring behavioral health problems; and
posttraumatic response, including PTSD symptoms.
Assessing Trauma Histories
Assessment of trauma histories is necessary not only as a first step in assessing traumatic stress
reactions, but also for other forms of assessment and treatment planning. Such assessments need
to take into account factors such as the client’s current level of safety (e.g., whether the client is
at risk for further trauma), current psychological stability (e.g., whether the client is currently
experiencing a level of acute psychological distress that might preclude indepth inquiries about
traumatic experiences), and the client’s readiness for further assessment and treatment (Briere &
Scott, 2006). Briere and Scott (2006) gave some guidelines for assessing trauma exposure, such
as establishing trust and a level of comfort before inquiring about traumatic experiences and
being prepared for intense responses from clients. They also provided a detailed list of symptom
responses to trauma that go beyond typical symptoms of traumatic stress reactions, including
cognitive disturbances (e.g., low self-esteem, helplessness, shame), dysfunctional behaviors
aimed at reducing trauma-related stress (e.g., self-mutilation, compulsive stealing), sexual
disturbances, somatic complaints, symptoms of other behavioral health disorders, and culturally
specific trauma responses. Hanson and Self-Brown (2010) provided some guidelines for
assessing trauma resulting from criminal victimization.
Assessing traumatic experiences to see if a client meets Criterion A for a PTSD diagnosis is a
first step in diagnosing PTSD (Weathers, Keane, & Foa, 2009). O’Donnell, Creamer, and Cooper
(2010) discussed some of the debate around Criterion A for PTSD and potential problems with
using that criterion to guide trauma assessment. They observed that Criterion A may, for
example, cause clinicians to ignore traumatic events that do not involve a clear memory of the
incident. A number of assessment instruments are available to aid in assessing trauma histories
or histories related to a particular type of trauma. These have almost always been developed for
research purposes but may be useful in real-life settings as well. For example, researchers
conducting the Women, Co-Occurring Disorders and Violence study selected the Life Stressor
Checklist-Revised to assess exposure to lifetime and current traumatic experiences for women
with co-occurring disorders and found it effective, reliable, and well tolerated in that context
(McHugo et al., 2005). Bailey, DeOliveira, Wolfe, Evans, and Hartwick (2012) used the
Childhood Trauma Questionnaire to evaluate childhood traumatic experiences for mothers of
preschool children and judged it a valid measure that helped them relate childhood traumatic
experiences to parenting concerns and behaviors.
Corcoran, Green, Goodman, and Krinsley (2000) observed that trauma assessment instruments
are not comprehensive and also reviewed potential complications in accurately assessing a
client’s prior traumatic experiences. They focused on two trauma assessment instruments, the
1-66 Part 3, Section 1—A Review of the Literature
Stressful Life Events Screening Questionnaire (SLESQ) and the Evaluation of Lifetime Stressors
instrument, with attention to how well these instruments capture experiences that meet Criterion
A of a PTSD diagnosis. They noted that the SLESQ is a brief measure that does not collect as
much information about objective and subjective aspects of trauma, and thus the two instruments
may be useful in different contexts. Both instruments have good test–retest reliability and
construct validity, and the SLESQ has good convergent validity as well.
The Traumatic Life Events Questionnaire (TLEQ) is a widely used self-report measure that
evaluates 22 types of traumatic events and certain characteristics of those events (e.g., whether
the event resulted in injury, how often it occurred; Kubany, Leisen, Kaplan, & Kelly, 2000). The
instrument has good reliability and validity (Orsillo, 2001). Compared with a single-item trauma
assessment question from the SCID, the TLEQ elicited 900 percent more traumatic events in a
group receiving treatment for opioid dependence (Peirce, Burke, Stoller, Neufeld, & Brooner,
2009).
Cusack, Frueh, and Brady (2004) described a 13-item self-report version of the Trauma
Assessment of Adults instrument (shortened to make it useful in clinical settings), which, unlike
the aforementioned instruments, was developed for use in clinical settings. In their evaluation of
the instrument with clients from a community mental health center, they found that a higher
number of traumatic events reported on the instrument correlated with worse physical and
behavioral health assessments using other measures. The authors concluded that the instrument is
useful in behavioral health treatment settings and can help improve recognition of PTSD as well
as guide other aspects of treatment. Some concern exists that trauma screening instruments may
prime some respondents to report PTSD symptoms, but Reddy, Polusny, and Murdoch (2009)
found this not to be the case in an evaluation of National Guard members. Fallot and Harris
(2001) also suggested that behavioral health treatment programs check a client’s medical, social,
and criminal histories for evidence of past trauma.
Screening and Assessing ASD
ASD may occur any time from the trauma exposure to 4 weeks after the exposure. The earliest
time an assessment can be made is 2 days following trauma exposure, because symptoms must
last at least 2 days for an ASD diagnosis (APA, 2000). Bryant and Litz (2006) noted that
assessments that occur too soon after trauma exposure are less likely to predict PTSD and that
ASD assessed 4 weeks after trauma exposure is more than twice as accurate as a PTSD marker.
Thus, they recommended that ASD assessment occur later in the window for ASD diagnosis to
make the best use of resources. In Bryant and Litz’s review (2006), they recommended three
instruments for assessing ASD that are also useful for predicting PTSD: Stanford Acute Stress
Reaction Questionnaire (Cardeña, Koopman, Classen, Waelde, & Spiegel, 2000), Acute Stress
Disorder Interview (Brooks et al., 2008), and Acute Stress Disorder Scale (Bryant, Moulds, &
Guthrie, 2000).
Screening and Assessing PTSD
Clients who report trauma histories should generally be further assessed for traumatic stress
symptoms and PTSD (Australian Centre for Posttraumatic Mental Health [ACPMH], 2007).
Screening instruments are available that can help clinicians decide which clients are more likely
to have PTSD and thus require further assessment. For example, Boscarino and colleagues

Trauma-Informed Care in Behavioral Health Services 1-67
(2011) reported on a brief screening tool designed for use in clinical practice, the New York
PTSD Risk Score, which inquires about PTSD symptoms including sleep problems, trauma
exposure, suicidal thoughts, depression symptoms, and demographic factors that may mean an
individual is at greater risk for PTSD. The instrument has been found effective for predicting
PTSD up to 1 year after the initial assessment (Boscarino et al., 2012b) and has specific versions
intended to assess men and women separately (Boscarino et al., 2012a). The National Center for
PTSD (NCPTSD) Web site (http://www.ptsd.va.gov) provides descriptions and basic
information on other commonly used PTSD screening instruments, including a table comparing
them, reproduced below as Exhibit L-6.
Exhibit L-6
Comparison of Screens for PTSD
Screens for PTSD
#
Items
Time to
Administer
(min.)
Allows
Multiple
Trauma
Corresponds
to DSM
Criteria
Beck Anxiety Inventory - Primary Care
7
3
Yes
N/A
Primary Care PTSD Screen
4
2
Yes
N/A
Short Form of the PCL
6
2
Yes
N/A
Short Screening Scale for PTSD
7
3
Yes
N/A
SPAN
4
2
Yes
N/A
Short Post-Traumatic Stress Disorder
Rating Interview
8
3
Yes
N/A
Trauma Screening Questionnaire
10
4
Yes
N/A
PCL
17
5-10
Yes
Yes
Source: NCPTSD Web site (http://www.ptsd.va.gov). Reproduced from material in the public domain.
The ACPMH (2007), as part of its review on the assessment and treatment of PTSD,
recommended that individuals presenting in healthcare settings be asked about whether they have
experienced trauma; when indicated, they should be given a comprehensive PTSD assessment.
Such PTSD assessments should investigate not only PTSD symptoms, but also symptoms of
other mental disorders, substance use/abuse behavior, marital and family functioning, vocational
functioning, quality of life, psychological functioning, and physical health. Assessments should
also establish strengths and sources of resilience. Symptoms should be assessed within the
context of the time elapsed since trauma exposure, recognizing that symptoms experienced in the
few weeks following trauma are likely to remit and also that, for some individuals, symptoms
may not appear until a considerable amount of time after the trauma. Regular reassessment
should also occur and needs to be culturally competent and to take into consideration the effects
an individual’s trauma exposure may have on those close to him or her.

1-68 Part 3, Section 1—A Review of the Literature
Steel, Dunlavey, Stillman, and Pape (2011) reviewed assessment of PTSD and depression for
individuals who have experienced significant trauma. They addressed differential diagnosis with
respect to TBI, the importance of cultural and sociodemographic factors, and potentially
confounding effects of medications. They summarized reliability and validity data for a number
of PTSD assessment instruments, including the PTSD interview, the CAPS, the Structured
Interview for PTSD, the Posttraumatic Diagnostic Scale, the Impact of Events Scale-Revised, the
Primary Care PTSD Screen, the PCL, the Harvard Trauma Questionnaire, the PENN Inventory,
and the PTSD modules of the Composite International Diagnostic Interview and the Diagnostic
Interview Schedule.
Orsillo (2001) also provided information on reliability and validity for these instruments as well
as a number of others. Briere (2002) discussed specific screening and assessment instruments for
both trauma and traumatic stress reactions and addressed how certain general measures of
behavioral health may be used for assessing these. The NCPTSD Web site
(http://www.ptsd.va.gov) also provides descriptions and basic information on clinician-delivered
interview instruments and self-report measures for assessing PTSD. See Exhibits L-7 and L-8,
respectively.
Exhibit L-7
Clinician-Delivered Interview Instruments for Assessing PTSD
Adult PTSD Interviews
#
Items
Time to
Administer
(min.)
Allows
Multiple
Trauma
Corresponds
to DSM
Criteria
CAPS
30
40-60
Up to 3
Yes
PTSD Symptom Scale-Interview Version
17
20-30
No
Yes
SCID-IV PTSD Module
21
20-30
No
Yes
Structured Interview for PTSD
27
20-30
No
Yes
Exhibit L-8
Self-Report Measures Instruments for Assessing PTSD
Adult PTSD Self-Report Measures
# of
items
Time to
Administer
(min.)
Allows
Multiple
Trauma
Corresponds
to DSM
Criteria
Davidson Trauma Scale
17
10-15
No
Yes
Distressing Event Questionnaire
35
10-15
Yes
Yes
Impact of Event Scale-Revised
22
5-10
No
Yes
Los Angeles Symptom Checklist
43
10-15
Yes
No

Trauma-Informed Care in Behavioral Health Services 1-69
Mississippi Scale for Combat-Related PTSD
17
10-15
Yes
No
Modified PTSD Symptom Scale
17
10-15
Yes
Yes
Penn Inventory for Posttraumatic Stress
Disorder
26
15-20
Yes
No
Posttraumatic Diagnostic Scale
49
10-15
No
Yes
PCL - Civilian, Military, Specific Trauma
17
5-10
Yes
Yes
Screen for Posttraumatic Stress Symptoms
17
10-15
Yes
Yes
Trauma Symptom Checklist-40
40
10-15
Yes
No
Trauma Symptom Inventory
100
15-20
Yes
No
A review by Johnson (2008) concerning the relationship of PTSD and substance use disorders
discussed some of the issues involved in assessment and differential diagnosis for clients with
both disorders. Najavits (2004) provided practical guidance on assessing trauma and traumatic
stress reactions in individuals with substance use disorders.
Screening and Assessing Complex PTSD
The assessment of complex PTSD is likely to follow from a more general assessment of trauma
and traumatic stress reactions, but it is a more complex process (Briere & Spinazzola, 2009).
Brown (2009) discussed assessment issues related to attachment styles for adults who have
complex PTSD. Briere and Spinazzola (2009) discussed appropriate instruments for assessing
trauma-related responses that may result from complex trauma (e.g., cognitive disturbance,
dissociation, dysfunctional behaviors).
Cultural, Ethnic, and Gender Factors in Assessment
All behavioral health screening and assessment should be culturally competent and sensitive to
gender, functional impairment, age, and religion/spiritual beliefs. Screening and assessment for
trauma and traumatic stress reactions are no exception, particularly given that research suggests
that culturally defined ways of interpreting traumatic experiences affect an individual’s reaction
to trauma, including the type and degree of behavioral health problems that may result from the
trauma exposure (Wilson, 2007). The planned TIP, Improving Cultural Competence (SAMHSA,
planned c), contains more detailed information on conducting culturally competent assessments
in behavioral health settings.
In assessing the impact of trauma on clients with diverse cultural backgrounds, one must
understand how their culture interprets the traumatic event, the historical and intergenerational
context of the trauma, the types of responses to trauma that the culture considers appropriate, and
what sources of strength/resilience people from that culture rely on in the wake of trauma
(Danieli, 2007; Hoshmand, 2007). Another important issue is how a client’s culture may shape
his or her attitudes toward behavioral health services and behavioral health disorder diagnoses.
For example, people from developing countries who have mood and/or anxiety disorders are
1-70 Part 3, Section 1—A Review of the Literature
about twice as likely as those from developed countries to perceive “stigma” associated with
those disorders, which can affect their willingness to report symptoms (Alonso et al., 2008).
Clients’ understanding and presentation of dissociative symptoms may also vary according to
their cultural backgrounds. For example, a number of researchers and clinicians have observed
that Asians and Asian Americans are more likely than members of many other cultural groups to
present anxiety symptoms, including PTSD symptoms, as somatic complaints (Hinton, Hofmann,
Pollack & Otto, 2009). Others have observed that Asian Americans may be more reticent about
discussing psychological complaints, because their cultures teach that stoic acceptance is the
appropriate response to adversity (Lee & Mock, 2005a,b). Research from the Netherlands has
found that people from non-Western cultures have more physical health-related anxieties
following trauma exposure than do those from Western cultures exposed to the same traumatic
event (Verschuur et al., 2010).
Pole and colleagues (2008) observed that African American clients may be hesitant to discuss
certain traumatic experiences with White American clinicians because they are concerned about
being judged. Instead, they too may present themselves in a reserved or stoic manner that can be
mistaken for the PTSD symptoms of avoidance or numbing. The authors noted that some Latinos
may also somaticize PTSD symptoms or present complaints using terminology that may not fit
easily into PTSD symptom categories (e.g., an attack of nerves).
Members of some cultural groups may also present dissociative symptoms in a manner that may
not readily be assessed as dissociation (e.g., as possession by a spirit; Lewi-Fernández et al.,
2007). Hinton, Pich, Marques, Nickerson, and Pollack (2010) found that severity of khyâl
attacks, a panic-like symptom experienced by Cambodian people and attributed to disruption in
personal energy, was strongly correlated with severity of PTSD symptoms. Certain traumas,
given their importance to members of a culture, may also be more likely to cause traumatic stress
reactions in members of a particular cultural group.
Some, but not all, assessment instruments have been evaluated with different cultural groups.
Pole and colleagues’ (2008) review noted that the Mississippi Combat-Related PTSD Scale, the
Keane PTSD Scale, the CAPS, and the PCL have been found to be effective with African
American populations. It is worth noting that an assessment instrument may have been translated
into another language, but this does not mean it is valid with every cultural group that speaks that
language. For instance, Bourque and Shen (2005) found that the Spanish translation of the
Civilian Mississippi Scale had significantly poorer correlations for Latinos than it did for White
Americans compared with other PTSD measures. Fortuna, Porche, and Alegría (2009)
recommended that clinicians use the Cultural Formulation from the DSM-5 (a model that takes
into consideration cultural identity, the client’s cultural environment, the role of culture in the
clinical relationship, and cultural factors related to behavioral health) when assessing PTSD.
They explained its application but also observed that, in their own research involving community
healthcare settings, the model is not widely used.
Special Issues in Assessment
Clinicians may have concerns that clients will not want to answer questions about certain types
of trauma, such as childhood abuse. Research indicates that a considerable percentage of people
who experience childhood sexual abuse do not report it when asked open-ended questions about
Trauma-Informed Care in Behavioral Health Services 1-71
childhood experiences. In earlier studies reviewed by Goodman and colleagues (2003), 37
percent of women (Williams, 1994) and 38 percent of women and men (Widom & Morris, 1997)
with child sexual abuse histories did not report it. Goodman and colleagues (2003) also reviewed
research indicating that men are less likely than women to disclose childhood sexual abuse and
that individuals are less likely to disclose instances of childhood sexual abuse when the
perpetrator is a family member.
Goodman and colleagues’ (2003) own research involved 175 adults who had participated as
children in a study regarding their sexual abuse and were reinterviewed by phone 13 years later,
ostensibly for a study of their legal experiences and attitudes. They found that only 15.5 percent
(n=26) reported the abuse. They observed that their study, in contrast to the earlier studies they
reviewed, had comprehensive records of the participants’ childhood sexual abuse, which enabled
them to more accurately assess whether participants were disclosing information about the
reported events. Factors associated with significantly lower likelihood of disclosing about
childhood sexual abuse included abuse occurring at an early age (age 5 or earlier), less severe
abuse, and less maternal support following the abuse. The authors did not find significant
differences in disclosure between men and women. On the other hand, Edwards and colleagues
(2003) found in the ACE study, as well as in some other research they reviewed, that most
individuals who sustained childhood abuse are willing to discuss it and also believe that
clinicians can help them cope with the effects of such abuse. The authors observed that
differences in findings may reflect differences in how inquiries about childhood sexual abuse are
made and how nonreporting of such abuse was evaluated, but also noted that the wrong
assessment methods will fail to elicit reports about such trauma.
Clinicians may also have difficulties eliciting information about other types of interpersonal
trauma, such as torture. Westermeyer, Hollifield, Spring, Johnson, and Jaranson (2011) assessed
experiences of torture for 1,134 refugees from Eastern Africa, using a single direct question as to
whether the individual had been tortured and a checklist of the 75 most common experiences of
torture. They found a fair amount of disagreement between the two assessment methods; 14
percent of the sample reported 1 or more item of torture on the checklist but answered the single
question negatively, and 9 percent of the sample answered that they had been tortured but
indicated no experience that would be considered torture.
The authors suggested that those who reported an experience that qualifies as torture but did not
indicate they had been tortured may have done so because they may have been so inundated with
trauma in their environment that they did not perceive their experience as torture, they may have
been afraid of being discriminated against because of their experiences, and/or they may have
perceived their experiences to be punishment for political actions and not as victimization by
torture. Those who indicated being tortured in answer to the general question but did not indicate
any specific experiences differed from others in the study in that they were significantly more
likely to be women; to be separated, divorced, or widowed; and to be significantly older (factors
that may have played a role in shaping their response). The authors noted that this latter group
was, like others in the study, highly traumatized and may have perceived their trauma as a form
of torture, even if their specific experiences would not generally be categorized as torture. The
results of this study suggest that multiple methods of screening/assessment may be needed to
elicit information about certain types of trauma, such as torture.
1-72 Part 3, Section 1—A Review of the Literature
Although childhood sexual abuse often goes unreported, another potential concern in assessment
is whether recovered or discontinuous memories of childhood abuse (particularly childhood
sexual abuse) are valid or accurate portrayals of an individual’s past trauma. Courtois (2000)
discussed the reasons for the controversy surrounding recovered memories and the arguments
given, both pro and con, concerning the validity of such memories. She also reviewed the
conclusions of four expert panels that weighed in on the controversy. An APA panel cautioned
that clinicians should not automatically disbelieve any reports of abuse, nor should they pressure
clients to believe that abuse may have occurred. The APA similarly noted that all clinicians
should take a neutral attitude toward reports of child abuse, and observed that despite it being
possible to construct pseudomemories that may be mistaken for real events, there are no hard and
fast rules as to when reports are inaccurate. She concluded that research has established that
memories can be recovered, but also that false memories are possible.
Geraerts and colleagues (2007) reviewed, in greater detail, evidence that it is possible for
individuals to regain previously forgotten memories of childhood abuse, but they observed that
the cases where this has been established have not involved aggressive memory-recovery
techniques (e.g., hypnosis). They also provided evidence from their own study of a self-selected
sample of individuals with either continuous (n=71) or discontinuous (n=57) memories of
childhood sexual abuse. They substantiated, using other sources, significantly more cases of
discontinuous memory when the memory was recalled outside of therapy and, in fact, they could
not substantiate any of the cases involving discontinuous memories that were recalled within the
context of therapy. Similar percentages of continuous memories and discontinuous memories
recalled outside of therapy were corroborated. Although this does not discount discontinuous
memories first recalled within the context of therapy, it does suggest that it is more likely that
some of them are not authentic.
In another study, Geraerts and colleagues (2009) evaluated the propensity to recall falsely and
the tendency to forget prior instances of remembering among a Dutch sample of individuals who
had memories of childhood sexual abuse recovered in therapy (n=30) or recovered spontaneously
(n=30) or who had continuous memories of childhood sexual abuse (n=30) or no such memories
(n=30). They found that individuals who recovered memories while in treatment appeared to be
more susceptible to false memories; those who recovered memories outside treatment appeared
more prone to forgetting past acts of remembering. Again, the tests used were not conclusive but
do suggest underlying differences between those who may have false recall of childhood sexual
abuse and those who may have forgotten and then recalled acts of childhood sexual abuse.
Certain aspects of traumatic stress reactions may also hinder effective assessment. Briere (2002)
noted that avoidant PTSD symptoms, by their very nature, decrease clients’ responses to
assessment questions and inhibit discussion of trauma. Such symptoms may even manifest as
dissociative amnesia, which may make traumatic memories completely unavailable to clients.
Prevention and Early Interventions for Traumatic Stress
Reactions
This section covers a number of reviews and meta-analyses that evaluate different interventions
for traumatic stress reactions (e.g., ACPMH, 2007; Bisson et al., 2007; Bisson & Andrew, 2009;
Bradley, Greene, Russ, Dutra, & Western, 2005; Cloitre, 2009; Ehlers et al., 2010; Ponniah &
Trauma-Informed Care in Behavioral Health Services 1-73
Hollon, 2009; Seidler & Wagner, 2006). For more information on specific interventions and the
seminal works that highlight them, refer to Part 1 of this TIP, “A Practical Guide for the
Provision of Behavioral Health Services.” The following sections discuss the more commonly
used or recommended interventions for preventing and treating traumatic stress reactions and
provide information about selected research regarding the effectiveness of these interventions.
Prevention and Early Intervention
A number of interventions meant to reduce the effects of trauma and prevent the development of
PTSD have been evaluated in the literature (Resnick, Acierno, Kilpatrick, & Holmes, 2005;
Zatzick et al., 2004). Such prevention activities may be presented as a form of psychological first
aid delivered to everyone who has experienced a given type of trauma (Everly, Phillips, Kane, &
Feldman, 2006). Alternatively, indicated prevention may be provided for individuals who are
considered at high risk for developing PTSD (e.g., people who have ASD) following trauma
exposure.
Zohar, Sonnino, Juven-Wetzler, & Cohen (2009) explored whether PTSD can be prevented.
They reviewed research indicating that individuals who have amnesia related to traumatic
experiences are significantly less likely to develop PTSD. Animal research confirms this and also
shows that stress related to trauma can be reduced/eliminated by chemically inducing amnesia.
They noted that research with people who have had a myocardial infarction (n=116) found that
those who use a repressive coping style had significantly fewer symptoms of ASD and PTSD
(the latter, up to 7 months after the event), suggesting that particular coping skills might aid in
reducing traumatic stress reactions among those exposed to trauma (see Ginzburg et al., 2002).
Zohar and colleagues (2009) also reviewed research indicating that interventions that enhance a
traumatic memory, such as some forms of psychological debriefing, are unlikely to be effective
and may be harmful. Instead, the authors concluded that pharmacological interventions are likely
to be the most effective means of preventing PTSD, although more research is needed to evaluate
such interventions. Another review, conducted by Roberts, Kitchiner, Kenardy, and Bisson
(2009a), looked at 25 randomized controlled trials for multisession prevention interventions and
concluded that trauma-focused cognitive–behavioral therapy (CBT) provided within 3 months of
trauma exposure was effective at reducing PTSD symptoms, especially for those whose
symptom levels met criteria for a PTSD diagnosis.
A review by Agorastos, Marmar, and Otte (2011) did not find sufficient evidence of any benefit
from preventive interventions delivered within hours of trauma exposure, but they found some
evidence that brief CBT delivered days or weeks after trauma reduced PTSD risk. These authors
concluded that brief CBT interventions should be considered the best option for prevention.
Prevention interventions that use CBT are difficult to distinguish from early treatment, but
several other studies have also found them effective for reducing PTSD symptoms. For example,
Israeli researchers compared four different early treatment options (prolonged ET, cognitive
therapy, treatment with a selective serotonin reuptake inhibitor [SSRI], or placebo) with a
waitlist control group (Shalev et al., 2012). The researchers provided follow-up data for 182
participants. At the 5-month follow-up assessment, the PTSD prevalence rates were similar for
the prolonged ET and cognitive therapy groups (21.4 percent and 18.2 percent of whom,
respectively, had PTSD) and were significantly lower for participants who received those
1-74 Part 3, Section 1—A Review of the Literature
interventions compared with all others. Treatment compliance and completion rates were also
similar across intervention groups.
A number of other reviews evaluating interventions to prevent traumatic stress reactions have
been conducted. One that used stringent selection criteria was conducted for the Cochrane
Collaboration (DeSilva et al., 2009). This review evaluated prevention of physical and mental
problems as well as impairments to social functioning that might result from trauma exposure. It
did not, however, find convincing evidence for the effectiveness of interventions aimed at
preventing behavioral health problems and, in fact, found three studies that provided good
evidence that such interventions had a harmful effect on behavioral health.
Although less often recognized as prevention, material and social services provided to trauma
victims appear to reduce PTSD risk. For example, among survivors of a tsunami in India, both
satisfaction with services received and receiving three or more sessions of counseling were
associated with significantly lower PTSD rates (Pyari et al., 2012). Also, Ullman & Filipas
(2001) found that having more services available was associated with a significant decrease in
PTSD risk for women who had been raped or sexually abused. Kantor and Beckett (2011)
reviewed more research that indicates that connecting trauma survivors with family, social
support networks, and needed resources appears to be the most effective strategy for preventing
traumatic stress reactions.
A number of models/interventions for providing social services to trauma victims have been
developed, but most have not had high-quality evaluations. Walsh (2007) reviewed information
on multisystemic, resilience-oriented interventions that have been used to help communities
respond to large-scale traumatic events, drawing on examples from around the world. Agani,
Landau, and Agani (2010) discussed the Linking Human Systems Community Resilience Model,
which attempts to mobilize social resources to improve an entire community’s resilience in
response to traumatic events. They also gave an example of the program’s use in Kosovo.
Principles of Effective PTSD Prevention
It is unclear whether a specific effective intervention is available for preventing PTSD, but some
basic principles have been evaluated that many authors believe are helpful in the wake of trauma
exposure. Hobfoll and colleagues (2007) delineated and reviewed research supporting the use of
five basic principles to use when counseling someone who has recently been exposed to trauma:
1. Promote a sense of safety. Research indicates that reestablishing a feeling of safety following
trauma exposure can decrease PTSD risk, whereas individuals who exaggerate future risk
following trauma have a higher rate of PTSD.
2. Promote calmness. An initial reaction of anxiety and heightened emotional response is
normal in the wake of trauma, yet studies indicate that when this type of response is
prolonged, it is associated with a variety of behavioral health problems. Two interventions
that work to calm individuals exposed to trauma or to teach skills for self-calming prior to
trauma exposure have been evaluated and found effective at reducing PTSD: stress
inoculation training (Hembree & Foa, 2000) and ET (Bryant, Harvey, Guthrie, & Moulds,
2003). Hobfoll and colleagues (2007) also recommend teaching problem-solving skills to
improve clients’ abilities to appraise the nature of their problems realistically and provide
psychoeducation about typical reactions to trauma to help them put feelings into context.
Trauma-Informed Care in Behavioral Health Services 1-75
Both techniques have strong theoretical support but lack research evaluating their
effectiveness. Fostering positive emotions may also be helpful in this context, as such
emotions have been found to have a protective relationship to behavioral health problems.
3. Promote a sense of personal and collective efficacy. A belief in one’s own ability to recover
from trauma (self-efficacy) and the ability of one’s community or group to do so (collective
efficacy) has been shown to have a positive effect on one’s behavioral health. Skills can also
be taught, for example, with CBT to improve self-efficacy. In the case of collective efficacy,
providing social and economic resources is also important (as those individuals who lose
more economically and socially have a harder time recovering from trauma).
4. Promote connectedness. A number of studies have found that greater social support reduces
the likelihood of developing PTSD following trauma exposure and improves recovery from
it, and on the other hand, poor social support or a negative community response increases the
odds that an individual will develop PTSD and hinders recovery. However, the quality of
social support is important, not just the quantity. Studies have also demonstrated that
negative social support, such as minimizing problems, invalidating feelings, or creating
unrealistic expectations, is strongly associated with long-term distress following trauma (e.g.,
Andrews et al., 2003).
5. Instilling hope. A greater sense of hope after trauma is associated with better outcomes in a
number of areas. Research indicates that CBT can be used to address such factors as an
exaggerated sense of personal responsibility or a tendency to classify experiences as
catastrophic (e.g., turning every setback into a catastrophe), which can impede hope.
In a review that specifically addressed pharmacological interventions to prevent PTSD, Zohar
and colleagues (2011) offered a different set of basic guidelines for preventing PTSD that should
be followed when treating someone who has been recently exposed to trauma. These are: don’t
pathologize (instead, explain that the individual’s response is normal given the abnormality of
the situation), don’t psychologize (e.g., increase emotional reactions to the trauma or enhance
traumatic memory through debriefing), and don’t pharmacologize (e.g., administer a
benzodiazepine or sleeping pill in the first few hours). This last item has a caveat that
medications are being researched (e.g., inderal, hydrocortisone) that may reduce PTSD if
administered soon after trauma exposure.
Although most prevention activities for people who have been traumatized are aimed at
preventing PTSD, it is possible to work to prevent other behavioral health problems in the wake
of trauma. For example, Resnick, Acierno, Amstadter, Self-Brown, and Kilpatrick (2007)
evaluated an intervention aimed at preventing substance abuse in the wake of sexual assault.
According to data for 268 female adolescents and adults who received either a two-part
psychoeducational intervention delivered via video or standard care alone and who were
available for at least one of three follow-up assessments, viewing the video intervention was
associated with significantly lower frequency of marijuana use at each of the follow-up times
(less than 3 months, 3 to 6 months, or 6 months or longer post assault). However, women who
did not have a prior rape history displayed higher PTSD and anxiety symptoms at 6 weeks. The
results underscore the need to further explore other aspects of the findings.
1-76 Part 3, Section 1—A Review of the Literature
Psychological First Aid
Some authors have adapted the basic principles suggested by Hobfoll and colleagues (2007; see
“Principles of Effective PTSD Prevention”) as part of a program of psychological first aid (e.g.,
Kantor & Beckett, 2011; Ng & Kantor, 2010). Kantor and Beckett (2011) described the key
features of psychological first aid as “contact and engagement, safety and comfort, stabilization,
information gathering, practical assistance, connection with social supports, information on
coping, and linkage with collaborative services” (p. 203). They also observed that psychological
first aid is flexible and responsive to “the specific human needs and emotional style of an
individual and his or her expressed needs at the moment of intervention” (p. 204).
Young (2006) observed that psychological first aid is indicated when an individual has an acute
stress reaction in response to trauma (e.g., dissociative symptoms, extreme anxiety, a high level
of cognitive impairment) or is at high risk for a traumatic stress reaction. The NCTSN and the
NCPTSD (2006) created a manual, now in its second edition, that provides further guidelines for
providing psychological first aid (available at http://www.nctsn.org/content/psychological-first-
aid). These guidelines have been widely accepted and adopted by organizations such as the
American Red Cross (Kantor & Beckett, 2011).
Military Prevention Programs
Prevention interventions have been developed specifically for members of the military who have
been exposed to trauma (e.g., the Battlemind and the Master Resiliency Training Programs; see
Reivich, Seligman, & McBride, 2011). Some of these programs are more immediate preventive
measures delivered prior to deployment and/or after trauma exposure, and others are intended for
the transition period when military personnel are returning from deployment. In a large study
intended to evaluate these programs, Adler, Bliese, McGurk, Hoge, and Castro (2009) compared
4-month outcomes for 1,060 individuals who had returned from combat deployments in Iraq and
had been randomly assigned to receive stress education delivered in large groups, a Battlemind
debriefing session delivered in small groups, Battlemind training in small groups, or Battlemind
training in large groups. At follow-up, participants in the Battlemind debriefing group with high
levels of combat exposure had significantly fewer PTSD symptoms (according to PCL scores),
fewer depression symptoms (according to scores on the Patient Health Questionnaire-Depression
scale), and fewer sleep problems than did participants with high combat exposure who received
stress education, but there were no significant differences for individuals with less combat
exposure (and presumably less exposure to combat trauma). Individuals who participated in the
large-group Battlemind training also had significantly fewer depression symptoms and fewer
sleep problems than participants in the stress education group.
The VA and the U.S. Department of Defense (VA/DoD; 2010) publication, Clinical Practice
Guideline for Management of Post-Traumatic Stress, reviewed research on these programs and
recommended four to five sessions of brief CBT as having the most benefit, although social
support and psychoeducation/normalization also had some benefit. However, the guidelines did
not address substance abuse or other comorbid conditions, and thus, their implementation
requires careful evaluation depending on the complexity of the clientele.
Trauma-Informed Care in Behavioral Health Services 1-77
Psychoeducation and Related Interventions for Prevention
Many interventions aimed at preventing traumatic stress reactions use psychoeducation to help
people exposed to trauma understand psychological symptoms that may result from trauma, alter
their perception of the traumatic event in a positive way, and be aware of behavioral health
treatments available to alleviate posttraumatic psychological distress (Wessely et al., 2008).
There is evidence that psychoeducation can alleviate anxiety for some anxiety disorders (see
discussion in the planned TIP, Managing Anxiety Symptoms in Behavioral Health Services
[SAMHSA, planned d]). However, evidence concerning the use of psychoeducation for
preventing PTSD is more complicated.
Wessely and colleagues (2008) reviewed research on psychoeducation interventions that have
been evaluated for their ability to reduce posttraumatic psychological distress, some of which
(e.g., stress inoculation approaches) have evidence supporting their use and others of which (e.g.,
single-session psychological debriefing) have been found ineffective or potentially harmful. The
authors concluded that there is not yet sufficient evidence for psychoeducation in this context
and that the quality of interventions for this purpose varies considerably. They noted that some
evidence suggests that psychoeducation that “proactively encourages an expectation of resilience
and, if necessary, help-seeking” may be beneficial (p. 296). The authors also warned that simply
disseminating information about psychological symptoms and mental disorders that may result
from trauma exposure is likely not to be useful and may be harmful. Other reviews (e.g., van
Emmerik, Kamphuis, Hulsbosch, & Emmelkamp, 2002) and studies (e.g., Marchand et al., 2006)
have found that a single session of incident stress debriefing is no better than no intervention for
people exposed to various types of trauma. Educational debriefing and emotional ventilation
debriefing were also found ineffective and actually associated with higher PTSD rates for
individuals who had a high level of hyperarousal at the time of the intervention (Sijbrandij, Olff,
Reitsma, Carlier, & Gersons, 2006).
Medications To Prevent PTSD
Another possible way to prevent PTSD following trauma exposure is to administer a medication
before or immediately following exposure. Fletcher, Creamer, and Forbes (2010) reviewed 15
studies that evaluated the use of medication for this purpose and concluded that, despite limited
evidence, there are indications that hydrocortisone (which reduces the production of cortisol) and
propranolol (which blocks norepinephrine reuptake) administered after trauma exposure may
reduce PTSD rates. They noted that more extensive research is needed before medications such
as these are used for trauma prevention (see also, Zohar et al., 2011).
Animal research appears to indicate that early administration of an SSRI following traumatic
experiences may also significantly reduce PTSD-like behaviors, but more research is needed to
confirm a positive effect for people (Zohar, Sonnino et al., 2009). Notably, some medications
that are used following trauma may actually make PTSD symptoms worse or increase the
likelihood of developing PTSD. Zohar and colleagues (2011) reviewed two small human studies
and one animal study that indicate that benzodiazepines administered following trauma exposure
increase the likelihood of developing PTSD later on. Similarly, research from Germany indicates
that ketamine administered to accident victims aggravates ASD symptoms and is associated with
increased levels of PTSD symptoms 3 to 24 months after trauma exposure (Schönenberg,
Reichwald, Domes, Badke, & Hautzinger, 2005, 2008).
1-78 Part 3, Section 1—A Review of the Literature
Longer-Term Prevention Measures
Interventions 1 to 4 weeks after trauma exposure require different methods and are typically
aimed at achieving different outcomes than are measures provided in the immediate aftermath of
trauma (Bryant & Litz, 2006). Interventions delivered 1 to 4 weeks after trauma exposure (such
as interventions for people with ASD, discussed in the following section) more closely resemble
treatment interventions and may even be labeled as assessment and early intervention rather than
as prevention. Bryant and Litz (2006) reviewed some of the prevention tasks that might be used
at this stage, including assessment of ASD and PTSD symptoms, trauma-focused CBT, ET, and
eye movement desensitization and reprocessing (EMDR). They also observed that prevention
activities at this stage will likely be targeted to individuals with ASD or those believed to be at
high risk for PTSD.
Prevention for People With ASD
ASD following trauma exposure is associated with increased risk for developing PTSD later, so
individuals with ASD are an appropriate target audience for indicated PTSD prevention. Ponniah
and Hollon (2009) reviewed randomized clinical trials for both PTSD and ASD. Even though the
research on ASD was limited to two studies, they concluded that, for preventing PTSD among
people with ASD, trauma-focused CBT by itself or with an additional hypnosis component is
more effective than supportive counseling and that imaginal and in vivo ET are more effective
than either no treatment or cognitive restructuring.
Kornør and colleagues (2008) reviewed research on the delivery of trauma-focused CBT to
people with ASD to prevent PTSD. All the studies included in their review compared trauma-
focused CBT with supportive counseling. The authors concluded that trauma-focused CBT is
superior to supportive therapy in terms of some PTSD outcomes (i.e., significantly lower PTSD
rates at some, but not all, follow-up points; significantly lower levels of intrusion and avoidance
symptoms up to 6 months later). However, the review included a limited number of studies (five
trials, four of which were conducted by the same researchers), and further research is needed.
A review (Roberts, Kitchiner, Kenardy, & Bisson, 2010b) of interventions that treat ASD
symptoms with the goal of preventing PTSD examined 15 studies that compared trauma-focused
CBT, supportive counseling, cognitive restructuring (without exposure), behavioral activation, or
stepped collaborative care with waitlist or treatment-as-usual controls; trauma-focused CBT was
also compared with other active treatments (supportive counseling, structured writing therapy, or
cognitive restructuring without exposure). Roberts and colleagues concluded that trauma-focused
CBT is effective at reducing PTSD symptoms among those who meet criteria for ASD; weaker
evidence suggests that it is effective with individuals who have symptoms of ASD without
meeting all criteria for the diagnosis. Trauma-focused CBT compares favorably with waitlist and
treatment-as-usual controls as well as supportive counseling, and some evidence indicates
superior effectiveness 6 months after treatment compared with cognitive restructuring without
exposure. They also found limited evidence that cognitive restructuring had a greater effect than
waitlist controls. They found no evidence to support the use of other interventions.
It can be difficult to distinguish between interventions aimed at treating ASD and those intended
to prevent the development of PTSD among people with ASD, as they largely focus on the same
outcomes. For example, Bryant and colleagues (2008) evaluated imaginal/in vivo ET (n=30),
Trauma-Informed Care in Behavioral Health Services 1-79
cognitive restructuring (n=30), or assessment and a waitlist (n=30) as treatment for ASD
following either a vehicle crash or a nonsexual assault. Using an intent-to-treat analysis, they
found that individuals who received ET were significantly less likely to have PTSD 6 months
after treatment, had significantly fewer ASD/PTSD symptoms following treatment and at the 6-
month posttreatment assessment, and had significantly better outcomes in terms of general
distress, non-PTSD anxiety symptoms, and depressive symptoms. Individuals receiving
cognitive restructuring also had significantly better outcomes than those in the waitlist control
group, but effect sizes were about half as large as those found with the ET intervention.
Trauma-Specific Treatments
Many different interventions and modalities are available for the treatment of trauma-related
behavioral health problems. Although the focus of this TIP is on adults who have experienced
trauma during their lifetimes, interventions have been designed and evaluated to address traumas
across development—that is, ET and EMDR are designed more for adult populations, whereas
some CBTs have been tailored to reach a broader age range. Treatments need to be
developmentally appropriate and specific. This section focuses on meta-analyses and reviews
rather than seminal works to cover the prolific field of trauma research. For more detailed
information on particular trauma-specific treatments, refer to Part 1 of this TIP, “A Practical
Guide for the Provision of Behavioral Health Services.”
Most reviews and meta-analyses have found that the most effective trauma-related behavioral
health treatments are trauma-focused CBTs, which are broadly defined to include ET and
EMDR. These two approaches are usually found to be about equally effective. Some reviews
(e.g., Bisson et al., 2007) have found that stress management and group CBT are effective, albeit
somewhat less so than CBT and EMDR. Cloitre’s (2009) review provided mean effect sizes for
different treatments across multiple studies and found that trauma-focused CBT with cognitive
restructuring had the largest mean effect size (8.83), followed by CBT with ET (8.04), ET alone
(7.94), EMDR (5.89), and problem-centered therapy (5.67).
Mendes, Mello, Ventura, Passarela, and Mari (2008) reached somewhat different conclusions in
their review of 23 clinical trials comparing CBT with other PTSD treatments. They found that
CBT is associated with better remission rates than EMDR and with efficacy and compliance
outcomes comparable to cognitive therapy and ET, suggesting that CBT is somewhat preferable
to EMDR.
Clinical practice guidelines such as those from the ACMPH (2007), the United Kingdom’s
National Institute for Clinical Excellence (NICE; 2005), and DoD and VA (2010) also generally
endorse trauma-focused CBT and, in some cases, EMDR as the best initial approaches for
treating PTSD. However, the National Institute of Medicine (IOM, 2008), in its review and
recommendations on PTSD treatment, found insufficient evidence supporting the use of EMDR,
cognitive restructuring, coping skills therapy, and group therapy for PTSD, and endorsed only
the use of ET, which they noted was a component of most CBT interventions. Benish, Imel, and
Wampold (2008)—using a statistical approach that was conservative in design and analysis—
concluded in their review that all interventions aimed at treating PTSD were basically equally
effective. This review included trauma desensitization, EMDR, CBT, various forms of ET, stress
inoculation, hypnotherapy, trauma-focused group therapy, psychodynamic therapy, and present-
1-80 Part 3, Section 1—A Review of the Literature
centered therapy. The authors also observed that about 25 percent of participants in the studies
reviewed left treatment early, and thus concluded, “keeping patients in treatment would appear to
be more important in achieving desired outcomes than would prescribing a particular type of
psychotherapy” (p. 755).
Ehlers and colleagues (2010) raised two major objections in response to Benish and colleagues’
(2008) review. The review excluded some widely used treatments (notably, supportive therapy)
because they did not meet their criteria of being a bona fide treatment but included others (e.g.,
present-centered therapy) that used many of the same components but were not as widely
studied, and the review did not account for the need for treatments to show greater efficacy than
natural recovery to establish their effectiveness. Ehlers and colleagues (2010) concluded that
Benish and colleagues’ (2008) review findings are not sufficient to establish that all PTSD
treatments (not just trauma-focused CBT and EMDR) are equally effective.
Large-scale reviews such as these present certain problems. As noted by IOM (2008),
interventions vary from one another in a number of different ways, such as “in their emphasis on
re-exposure to trauma-related memories and stimuli, cognitive restructuring of the trauma
experience, expression and management of emotion, training in stress management (including
relaxation training), and general social and vocational support,” and few studies attempt to
separate these components to evaluate their efficacy/effectiveness independently (p. 93). Thus, it
is difficult to ascertain which parts of a given intervention produce positive change.
IOM (2008) also identified problems with PTSD research, such as study attrition, inadequate
methods for addressing missing data, publication and investigator bias (e.g., pharmacological
studies funded by drug companies), difficulties generalizing results found with one specific
population or applying those results to another specific population, inadequate follow-up, and a
dearth of high-quality randomized controlled studies. The report pointed out that even though a
rigorous evidence base for a particular treatment or intervention may be lacking, this does not
mean the particular treatment lacks clinical efficacy.
Cognitive–Behavioral Therapy
A number of specific PTSD interventions can be classified as CBT, and CBT for trauma and
traumatic stress reactions typically includes multiple techniques/components. It is also usually
trauma-focused (i.e., focused on helping clients address traumatic experiences). For example, in
their review of CBT for trauma, Cahill, Rothbaum, Resick, and Follette (2009) evaluated seven
different techniques/therapies, which they labeled as CBT: ET, stress inoculation training,
cognitive processing therapy (CPT), cognitive therapy, relaxation training, dialectical behavior
therapy (DBT), and acceptance and commitment therapy (ACT). CBT is a well-studied
approach—Cahill and colleagues’ (2009) review included 64 randomized, controlled trials and
many more nonrandomized trials. CBT is also generally recommended in the treatment of PTSD.
Although much of the research has focused on CBT’s use in treating PTSD, a Cochrane review
of treatments for ASD also found CBT to be more efficacious than waitlist controls or supportive
counseling (Roberts et al., 2010).
Reviews of CBT for the treatment of trauma and/or PTSD include those by Cahill and colleagues
(2009), Kar (2011), and Mendes and colleagues (2008). All concluded that evidence supports the
effectiveness of CBT in the treatment of PTSD. Beck, Emery, and Greenberg’s (2005) book on a
Trauma-Informed Care in Behavioral Health Services 1-81
cognitive approach to treating anxiety disorders also has some discussion of how cognitive
therapy may be applied to the treatment of PTSD.
Other reviews of CBT for anxiety disorders also found it to be an effective approach for treating
PTSD and, in some cases, ASD (Hofmann & Smits, 2008; Norton & Price, 2007; Otte, 2011;
Stewart & Chambless, 2009). For example, Stewart and Chambless (2009) found that CBT
performed significantly better in treating PTSD than nontreatment controls and had relatively
large effect sizes in terms of reducing PTSD symptoms (with a combined standardized mean
difference in effect size of 2.59, according to their meta-analysis). CBT has been successfully
used for treating trauma and PTSD in a number of different populations, including child sexual
abuse survivors with or without complex PTSD (McDonagh et al., 2005; Resick, Nishith, &
Griffin, 2003); women who have experienced domestic violence (Johnson, Zlotnick, & Perez,
2011; Kubany et al., 2004); women who are victims of sexual assault (Foa, Zoellner, & Feeny,
2006; Resick, Nishith, Weaver, Astin, & Feuer, 2002); people who survived motor vehicle
crashes (Beck, Coffey, Foy, Keane, & Blanchard, 2009; Maercker, Zöllner, Menning, Rabe, &
Karl, 2006); victims of terrorism/civil conflict (Duffy, Gillespie, & Clark, 2007; Hamblen,
Gibson, Mueser, & Norris, 2006; Levitt, Malta, Martin, Davis, & Cloitre, 2007); refugees/asylum
seekers (Hinton et al., 2009; Paunovic & Öst, 2001); survivors of natural disasters (Başoglu,
Salcioglu, & Livanou, 2007; Hamblen et al., 2009); veterans/military personnel with combat
trauma (Kent, Davis, Stark, & Stewart, 2011; Khoo, Dent, & Oei, 2011; Schnurr, Friedman et al.,
2003); and disaster aid workers (Difede et al., 2007). Ruzek and colleagues (2008) specifically
reviewed the use of CBT to treat trauma and traumatic stress responses in individuals who
survived disasters or terrorist attacks, and Jaycox, Zoellner, and Foa (2002) reviewed its use with
rape survivors.
CBT has also been effectively used to treat PTSD in clients with various co-occurring disorders,
including panic disorder (Falsetti, Resnick, & Davis, 2008; Hinton, Chhean, Pich et al., 2005),
major depression (Nixon & Nearmy, 2011), SMI (i.e., major depression, bipolar disorder,
schizoaffective disorder, and/or schizophrenia; Mueser et al., 2008), substance use disorders (see
the “Integrated Approaches for Trauma and Substance Abuse” section), BPD (Dorrepaal et al.,
2010), both depression and substance use disorders (Norman et al., 2010), and chronic pain
conditions (Otis, Keane, Kerns, Monson, & Scioli, 2009). CBT has also been found to be an
effective treatment for sleep problems associated with PTSD (Carney & Edinger, 2010; DeViva,
Zayfert, Pigeon, & Mellman, 2005; Nishith et al., 2003; Ulmer, Edinger, & Calhoun, 2011).
Trauma-focused CBT interventions have been culturally adapted for various client populations,
including Latinas (Hinton, Hofmann et al., 2011), African refugees from two different nations
(Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004), Cambodians (Hinton, Hofmann et al.,
2009), and Vietnamese (Hinton et al., 2004). Hinton, Kredlow, Bui, Pollack, & Hofmann (2012)
discussed some of the ways in which CBT can be made more culturally relevant for refugees
(and others) from non-Western cultures. For example, using emotional regulation techniques and
imagery drawn from their cultural traditions, focusing on teaching psychological flexibility (an
important skill for individuals trying to adapt to living in a multicultural environment), changing
the focus of some CBT techniques (e.g., focusing on uncontrollable worry, a common expression
of traumatic stress reactions in individuals from non-Western cultures), using culturally relevant
rituals to mark transitions, and using CBT to address culturally specific syndromes (e.g., ataque
de nervios among Latinos). CBT for trauma/traumatic stress reactions can be effectively
1-82 Part 3, Section 1—A Review of the Literature
delivered in groups as well as one on one (e.g., Beck et al., 2009; Kent et al., 2011). It has also
been adapted for delivery by computer or over the Internet (McLean, Steenkamp, Levy, & Litz,
2010).
Trauma-focused CBT can encompass a number of different techniques. Cahill and colleagues’
(2009) review listed various interventions/techniques that involve CBT principles and have been
used for treating trauma/traumatic stress reactions These include ET (discussed separately in this
section); stress inoculation training, a method of managing anxiety/stress; CPT, which teaches
clients to address problematic cognitions such as self-blaming; cognitive therapy, another
approach for modifying problematic/dysfunctional thinking; relaxation training, a behavioral
approach for relaxing the body and mind to reduce stress/anxiety; DBT, a form of CBT
developed to treat BPD; and ACT, an approach that fosters acceptance and awareness of internal
states/feelings. Cahill and colleagues’ (2009) review summarized research supporting the use of
each of these CBT interventions/techniques, noting that the strongest and most extensive
research is for various exposure therapies; there are also multiple studies supporting the use of
CPT, cognitive therapy, and stress inoculation training in this context.
Although the research on ACT for people with PTSD and trauma-related problems is limited,
Walser and Westrup (2007) drew on theory and clinical experience to discuss why the approach
may be effective with this population. They also provided a “how-to” guide for using ACT in
this context. Researchers have found mixed results in comparing the effectiveness of different
components of trauma-focused CBT; typically, this research has involved comparing ET and
cognitive restructuring. Most studies have found that neither ET nor cognitive restructuring alone
is more effective than the other, and although some studies have found that the combination of
the two is more effective than either alone, others have not found that to be the case (Resick et
al., 2008).
Resick and colleagues (2008) took a somewhat different approach to evaluating the components
of CPT, a CBT intervention that involves the use, separately and together, of cognitive therapy to
address thinking patterns and narrative writing to enable clients to be exposed to traumatic
memories in a relatively safe manner. Assessment 6 months after treatment showed no
significant differences in symptoms of depression or PTSD between participants who received
either component alone and those who received both components. However, when the
participants who received cognitive therapy alone were compared with those who received the
narrative therapy component alone, those in the former group had significantly lower levels of
both PTSD and depression symptoms.
Not all CBT interventions used to treat PTSD are trauma-focused. For example, Monson,
Rodriguez, and Warner (2005) compared CBT for PTSD that was trauma-focused (relying
largely on ET to help clients reprocess traumatic experiences) with another CBT intervention
that was skills-focused (helping clients learn and practice skills to manage PTSD symptoms).
They did not find significant differences between the two in terms of outcomes for PTSD
symptoms or alcohol abuse, but they did find that the perceived quality of clients’ intimate
relationships prior to beginning treatment had a stronger negative relationship to violence
perpetration (assessed using four questions from the NVRRS study) if the client received trauma-
focused rather than skills-focused CBT, suggesting that clients with stronger intimate
relationships may gain some added benefit from trauma-focused CBT.
Trauma-Informed Care in Behavioral Health Services 1-83
Building strength and resilience can be the focus of a CBT intervention. In a pilot study, Kent
and colleagues (2011) used a resilience-oriented CBT intervention with 39 veterans who had
PTSD. The authors found large improvements in terms of affective symptoms and positive
emotional health, a moderate improvement in memory, and a small-to-moderate improvement in
executive functioning.
CBT has also been combined with other approaches/interventions to improve treatment of PTSD
and other consequences of trauma. Positive outcomes have been found using CBT combined
with behavioral activation, a more purely behaviorist approach to treatment (Nixon & Nearmy,
2011), as well as with CBT combined with pharmacotherapy (see studies reviewed by Stein,
Ipser, & McAnda, 2009). Although many CBT interventions are manualized, Levitt and
colleagues (2007), in a study that evaluated flexibility in the application of a manualized CBT
treatment for 59 survivors of the 9/11 attack, found that effects sizes for the treatment using a
more flexible approach were comparable to those observed in other studies that had more strict
adherence to the manual.
Eye Movement Desensitization and Reprocessing
EMDR is a technique that helps desensitize clients to traumatic memories, replace distressing
cognitions with positive ones, and learn to attend to bodily sensations, thoughts, and feelings in a
manner similar to mindfulness meditation approaches (Foa, Keane, Friedman, & Cohen, 2009;
Spates, Koch, Cusack, Pagoto, & Waller, 2009). A number of literature reviews/meta-analyses
have found EMDR to be an effective treatment for PTSD, with the caveat that the eye
movements themselves do not appear to be necessary in order for the intervention to be effective
(Ehlers et al., 2010). Although IOM (2008) guidelines do not recommend EMDR, guidelines
from Australia (ACPMH, 2007) and Great Britain (NICE, 2005) have included it as an effective
approach. SAMHSA’s National Registry of Effective Evidence-Based Programs and Practices
(NREPP; http://nrepp.samhsa.gov) also recognizes EMDR as effective in reducing PTSD,
anxiety, and depression symptoms.
Spates and colleagues (2009) reviewed research specifically on EMDR as a treatment for PTSD.
Among the studies they reviewed are ones that found EMDR more effective than relaxation
training, habituation training, fluoxetine, placebo pill, and standard care. They reported on two
studies that found better outcomes for EMDR than for prolonged ET and other studies that found
that ET produced better outcomes than EMDR. They concluded that the two treatments are about
equally effective. One study they reviewed also indicated that EMDR produced significantly
better outcomes for clients with adult-onset rather than childhood-onset trauma.
Ehlers and colleagues’ (2010) review concluded that, although EMDR is effective for PTSD, the
eye movement component of the treatment is not necessary. Davidson and Parker (2001) reached
a similar conclusion in an earlier meta-analysis of EMDR, finding that no additional effect could
be found when EMDR was practiced with the eye movements compared with when it was
practiced without them. Spates and colleagues (2009) also reviewed studies that evaluated the
benefit of the eye movement component of EMDR. They observed that early research did not
find any additional benefit, but that one small study found that bilateral eye movements (the type
used in EMDR) produced somewhat quicker results than other types of eye movements. Other
studies of this aspect of EMDR either have not used clinical samples or have other significant
methodological problems.
1-84 Part 3, Section 1—A Review of the Literature
Exposure Therapy
ET may be considered as a component of trauma-focused CBT (e.g., Cahill et al., 2009) or
evaluated as an intervention in and of itself (e.g., IOM, 2008). It has been recommended for the
treatment of PTSD in a number of guidelines (e.g., ACPMH, 2007; DoD/VA, 2010; IOM, 2008)
and reviews (e.g., Bisson & Andrew, 2007; Bradley, Greene et al., 2005; Cloitre, 2009; Ehlers et
al., 2010). Prolonged exposure (PE; Foa & Rothbaum, 1998; Foa, Hembree, & Rothbaum, 2007;
see also NREPP) is the specific model of ET for PTSD that has been the most widely researched
and is recommended in a number of PTSD treatment guidelines and reviews (e.g., IOM, 2008).
In their review of PE, McLean and Foa (2011) described recommended practice, presented the
theoretical underpinnings of the intervention, and briefly reviewed the research supporting its
use. Reviewing 25 randomized, controlled trials, the authors concluded that studies have
consistently found that PE is effective in reducing PTSD. A few studies also indicated that PE is
effective for both acute and chronic PTSD, produces results that persist for 1 year or more,
produces relatively quick results, and has relatively large effect sizes. PE is more effective than
waitlist controls, relaxation training, supportive counseling, and treatment as usual; it is as
effective as other recommended PTSD treatments.
Another meta-analysis of PE, which included 13 studies and a total sample of 657, reached
similar conclusions (Powers, Helpern, Ferenschak, Gillihan, & Foa, 2010), finding it more
effective than nontreatment control conditions and as effective as other active treatments (e.g.,
EMDR, CBT). According to Powers et al.’s analysis of combined data, the average client
receiving PE had better posttreatment outcomes than 86 percent of participants in control groups.
PE had high to medium effect sizes for primary and secondary outcomes at follow-up
assessments. Rachamim, Nacasch, Shafran, Tzur, and Gilboa-Schechtman (2009) also reviewed
research on the use of PE for PTSD, with particular attention to research conducted in Israel.
Another meta-analytic review by Ougrin (2011) compared data on the effectiveness of cognitive
therapy and ET and found no significant differences in effectiveness between the two.
A few studies of PE have been published since these reviews. One by Resick, Williams, Suvak,
Monson, and Gradus (2012) followed up earlier research and provided long-term (i.e., 5 to 10
years after initial treatment) follow-up data for 126 women (out of an initial 171) who had been
rape victims and had PTSD that was treated with either PE or CPT. Participants in both treatment
groups had significant reductions in PTSD symptoms (according to both the PTSD Symptom
Scale and the CAPS) that persisted over the long-term follow-up period, with no significant
differences between the two treatment arms. At the long-term follow-up assessment, 93.4 percent
of those who received CPT and 91.9 percent of those who received PE had 10-point reductions
in CAPS scores from pretreatment levels, and 88.5 percent of those who received CPT and 88.7
percent of those who received PE had 20-point reductions. Also, at the long-term follow-up
assessment, only 22.2 percent of those who received CPT and 17.5 percent of those who received
PE met criteria for a current PTSD diagnosis (down from 100 percent at the start of treatment).
ET (typically PE) has been found to be effective with different populations, including female
veterans (Schnurr et al., 2007), male combat veterans (Yoder et al., 2012), female victims of rape
(Resick et al., 2012), women who were victims of childhood sexual assault (McDonagh et al.,
2005), survivors of terrorist attacks (Schneier et al., 2012), and refugees exposed to political
Trauma-Informed Care in Behavioral Health Services 1-85
violence/torture (Paunovic & Öst, 2001). ET has been found to be effective when delivered in
groups (Ready et al., 2008) as well as individually.
Some research suggests that traditional ET models may not be suitable for members of all
cultural groups and that individuals from non-Western cultures may find ET harder to tolerate or
may have some degree of worsening of symptoms before they respond to treatment (Hinton,
Rivera, Hofmann, Barlow, & Otto, 2012). However, there is a lack of research evaluating this,
and no significant data are available.
Hinton, Rivera, and colleagues (2012) recommended that, when using ET with refugees from
non-Western cultures, clinicians should take a phased approach (e.g., teach emotional regulation
skills such as meditation or muscle relaxation before using exposure techniques), use a trauma
protocol (described in the article) that includes emotional regulation techniques and discussion to
make ET more acceptable, and use interoceptive exposure techniques with positive
reassociations (as this population has a high level of somatic complaints associated with their
trauma, and those somatic sensations often perpetuate PTSD). They also recommended ways
these techniques can be made more culturally relevant (e.g., understanding and using imagery
and techniques drawn from clients’ cultural traditions when teaching emotional regulation).
Their advice is also applicable to nonrefugee populations from diverse cultural backgrounds.
ET has also been adapted, as multiple channel exposure therapy, to treat co-occurring PTSD and
panic disorder (Falsetti et al., 2008), and it has been combined with DBT to treat co-occurring
PTSD and BPD (Harned, Korslund, Foa, & Linehan, 2012). Najavits, Schmitz, Gotthardt, and
Weiss (2005) also reported on a small study (N=5) combining ET and Seeking Safety for men
with co-occurring PTSD and substance use disorders. Looking at whether ET may be made more
effective and palatable if used in combination with other treatments, Foa, Rothbaum, and Furr
(2003) reviewed five studies combining ET and other CBT interventions and found little
significant improvement associated with the additional therapies (only one of the studies found
some improvement in outcomes). A later study by Foa and colleagues (2005) also found no
significant differences when cognitive restructuring was added to ET, but there was some
evidence that individuals with severe trauma-related thoughts did better in ET alone than in the
combined treatment.
More recent research suggests benefits to adding cognitive restructuring to ET. A study that
randomly assigned 118 individuals with PTSD to receive imaginal exposure, in vivo exposure,
both combined, or both with additional cognitive restructuring found that fewer participants in
the combined group had PTSD at the 6-month follow-up; findings also showed significantly
larger effect sizes for PTSD and depression outcomes in the combined treatment group compared
with all others (Bryant, Moulds et al., 2008). A randomized trial of ET with and without
additional cognitive restructuring found that men who received ET alone (n=32) had
significantly higher levels of PTSD symptoms at a 6-month posttreatment follow-up assessment
than did men who received ET plus cognitive therapy (n=20) or women in either group (n=56;
Felmingham & Bryant, 2012). The authors concluded that these gendered differences in
treatment responses suggest that the combined treatment is a better option for men with PTSD.
Beidel, Frueh, Uhde, Wong, and Mentrikoski (2011) compared ET alone with ET in combination
with social–emotional rehabilitation for combat veterans (N=35). They found no significant
1-86 Part 3, Section 1—A Review of the Literature
differences in PTSD outcomes, but they did find that people who received the additional
treatment participated in social activities more frequently and spent a greater amount of time
engaged in such activities. ET has also been effectively combined with pharmacotherapy.
Schneier and colleagues (2012) found that PE combined with pharmacotherapy (Paroxetine) was
associated with better outcomes than PE alone in a group of survivors of the 9/11 attack (N=37).
One recent modification of ET is the use of virtual reality (VR) software to deliver exposure
experiences in a more controlled and perhaps more realistic manner (Alcañiz, Lozano, & Rey,
2004; Botella et al., 2004). Recent literature reviews by Gerardi, Cukor, Difede, Rizzo, and
Rothbaum (2010) and Meyerbröker and Emmelkamp (2010) have found that VR shows promise
as a way to enhance ET for people with PTSD. However, the studies included in these reviews
are small, often do not use control groups or random assignment, and mostly involve veterans
with combat-related PTSD. A study from Spain compared a VR intervention (n=19) with
standard CBT (N=20) for individuals with a stress-related disorder (PTSD, pathological grief, or
adjustment disorders) and found no significant differences in outcomes related to those disorders
and significantly better outcomes in terms of depression, social interference, and relaxation for
those who received the VR intervention (Baños et al., 2011).
Another promising innovation in the delivery of ET is narrative ET, which was originally
developed for use in countries with less economic development but has since been used in more
developed nations (Robjant & Fazel, 2010). This approach was designed to be delivered by
individuals who are not mental health professionals and to require a relatively short treatment
time; it was also intended to document atrocities as well as treat PTSD. It is a manualized
approach and involves emotional exposure to memories of trauma that takes place in the context
of creating a narrative about the traumatic event. Robjant and Fazel (2010) reviewed findings
from six trials involving the treatment of both children and adults that were conducted in
countries with low to medium economic development and four conducted in countries with high
economic development (although typically with refugee populations). These studies found that
participation in the intervention was associated with reductions in PTSD symptoms and, in some
cases, with reductions in other mental disorder symptoms and improvements in overall
psychological well-being. Studies found greater improvements in outcomes among those
receiving the intervention compared with no treatment, treatment as usual, psychoeducation,
interpersonal therapy, or supportive counseling.
Some authors have raised concerns that ET may worsen symptoms for some clients and that
dropout rates are high because the treatment is unpalatable to some. Cahill, Foa, Hembree,
Marshall, and Nacash (2006) reviewed research regarding dropout and worsening of symptoms
in the context of a larger review on the dissemination of ET for PTSD. They observed that
studies have found dropout rates for ET to be comparable to those of other active treatments but
significantly higher than nontreatment controls; the amount of worsening of symptoms was no
different from that found in other active treatments but significantly lower than found in
nontreatment controls.
Psychodynamic Approaches
Most research reviews and meta-analyses have found psychodynamic therapies to be relatively
ineffectual in the treatment of PTSD. However, in a review of research on psychodynamic
treatments for PTSD, Schottenbauer, Glass, Arnkoff, & Gray (2008) argued that this is because
Trauma-Informed Care in Behavioral Health Services 1-87
such reviews consider only limited outcomes and claimed that psychodynamic approaches are
helpful in ways that are typically not evaluated in the research, such as by improving self-esteem,
relationships, problem-solving, and social functioning. They also noted that research indicates
that such improvements often continue after treatment concludes. In addition, their review
discussed how research and clinical observation indicate best uses for psychodynamic therapy
with clients who have PTSD, particularly those with complex PTSD.
Kudler, Krupnick, Blank, Herman, & Horowitz (2009) reviewed research on psychodynamic
therapy in the treatment of PTSD and derived similar conclusions. They observed that
psychodynamic approaches place a priority on individualizing treatment but that such
approaches are not indicated for every client. They also provided guidelines for which clients are
best suited to this treatment modality.
Pharmacotherapy
A number of treatment guidelines also recommend pharmacotherapy as a possible treatment for
PTSD, although typically not as the first line of treatment (e.g., ACPMH, 2007; Benedek,
Friedman, Zatzick, & Ursano, 2009; DoD/VA, 2010; NICE, 2005). A variety of medications
have been evaluated as PTSD treatments, but the most often recommended or suggested
medications are, in order of preference, SSRIs, serotonin norepinephrine reuptake inhibitors
(SNRIs), tricyclic antidepressants, monoamine oxidase inhibitors (MAOs), and atypical
antipsychotics (see reviews by Friedman & Davidson, 2007; Ravindran & Stein, 2009; Stein,
Ipser, & Seedat, 2006). Paroxetine and sertraline (both SSRIs) have been approved by the Food
and Drug Administration for the treatment of PTSD, the latter for long-term as well as short-term
treatment (Ipser & Stein, 2011).
Various reviews and guidelines recommend SSRIs as the first medication to try when treating
PTSD (see review by Stein et al., 2009). Ravindran and Stein (2009) agreed with other reviews
in noting that SSRIs have the most research supporting their use in this context, and, of the
SSRIs, fluoxetine is the most researched and has generally been found to be effective in
alleviating PTSD symptoms, reducing the likelihood of relapse to PTSD once remission is
achieved, and alleviating other mental disorder symptoms that might complicate treatment.
Acute-phase trials of sertraline have had somewhat mixed results; at least one trial involving
veterans with relatively severe PTSD found that symptom improvements associated with
sertraline were not significantly better than those associated with placebo use. Stein et al.
observed that current guidelines recommend that SSRIs be used for 6 to 12 months for acute
PTSD and 12 to 24 months for chronic PTSD; in some cases, an even longer period of treatment
may be required. Studies of longer-term use of sertraline have shown better results and have
consistently found significantly better improvements than placebo use.
A Cochrane review by Stein and colleagues (2006) found that, in the 35 randomized controlled
trials they evaluated, a significantly larger percentage of clients with PTSD responded to
medications than to placebo; most of these studies indicate that SSRIs are effective for treating
PTSD. Ravindran and Stein (2009) noted that paroxetine also has a number of studies supporting
its use, albeit fewer than the other SSRIs; a few other SSRIs (i.e., citalopram, escitalopram,
fluvoxamine) have also been found effective in more limited research. Research comparing
different SSRIs/SNRIs has not generally found significant differences in PTSD outcomes
(Benedek et al., 2009).
1-88 Part 3, Section 1—A Review of the Literature
A review by Ipser and Stein (2011) added to the knowledge base but also drew the same basic
conclusions that SSRIs, the SNRI venlafaxine, and the atypical antipsychotic risperidone all are
effective at reducing PTSD severity/symptoms. These authors also observed that sample
characteristics do not appear to have a significant relationship to treatment response for these
medications. Ravindran and Stein (2009) noted that the SNRI venlafaxine has been evaluated in
a couple of research trials that found its use to be associated with significantly better outcomes
than use of a placebo, although one trial did not find significant differences between venlafaxine
and the SSRI sertraline. Other research has found no significant ethnic/racial or gender
differences associated with response to venlafaxine, whereas differences in type of trauma were
associated with significant differences in some outcomes (i.e., symptom-related disability,
resilience) but not others (e.g., PTSD symptoms; Rothbaum et al., 2009).
Berger and colleagues (2009) specifically reviewed the use of medications other than SSRIs,
which may be needed because many clients with PTSD do not respond to SSRIs. The authors
found the strongest evidence for the use of atypical antipsychotics, especially risperidone, which
has been found to be superior to placebo in reducing PTSD symptoms in three trials. Olazapine
has also been found effective in this regard in some, but not all, studies. The authors observed,
however, that these medications do not appear to have an effect on avoidance behavior or
emotional numbness. In a meta-analytic review of atypical antipsychotics for PTSD, Pae and
colleagues (2008) noted that, although these medications have been shown in a number of
studies to reduce PTSD symptoms to a greater degree than placebos, most of the difference is a
result of reduced intrusion symptoms. Ravindran and Stein (2009) noted that, as expected, these
medications are particularly helpful for clients who have PTSD with psychotic symptoms, but
the authors also cautioned about negative side effects, such as excessive weight gain.
Other medications evaluated for PTSD show less promise but may be indicated in cases where
individuals do not respond to SSRIs. Ravindran and Stein (2009) noted that the tricyclic
antidepressants amitriptyline and desipramine perform better than placebos in reducing some
PTSD symptoms. Also, some, but not all, studies have found MAOs more effective than placebo
in addressing PTSD symptoms. Both Berger and colleagues (2009) and Ravindran and Stein
(2009) pointed to research indicating that the antiadrenergic agent prazosin is an effective
medication for improving sleep quality and reducing nightmares among people with PTSD.
More research on these medications is needed.
Not all reviews/guidelines recommend pharmacotherapy for PTSD, however. Notably, IOM
(2008) found that for all the medications included in the review (including SSRIs and atypical
antipsychotics), there was inadequate evidence to determine their efficacy in treating PTSD. One
IOM panel member contributed a dissenting opinion in Appendix H of the report, stating that he
believed this conclusion was incorrect and disagreed with the panel decision to group research
conducted with civilian and veteran populations. He noted that if studies showing a lack of
efficacy with veterans who had chronic PTSD were removed from the pool, remaining evidence
would indicate that SSRIs and atypical antipsychotics could be effective treatments for PTSD.
Ravindran and Stein (2009) also observed, in response to the IOM report, that SSRI efficacy
varies considerably among individuals, and hence, the modest effect sizes do not mean that these
medications should be discounted. A review by Choi, Rothbaum, Gerardi, and Ressler (2010) of
the use of pharmacological agents to improve the results of other therapies concluded that most
Trauma-Informed Care in Behavioral Health Services 1-89
studies have not found any additional improvement in outcomes associated with the addition of
SSRIs. However, their review did not consider evidence for the use of SSRIs with individuals
who have not been responsive to other therapies. They also suggested that there are new
medications being evaluated (notably D-cycloserine) that may improve clients’ responses to
PTSD therapy.
A Cochrane review by Hetrick, Purcell, Garner, and Parslow (2010) on combined
pharmacotherapy and psychological therapies for PTSD looked at four that met more stringent
inclusion criteria and concluded that there was insufficient data to determine whether
combination therapy produced better results than pharmacotherapy or a psychological therapy
alone. Little research evaluates the effects of culture on outcomes in pharmacotherapy for PTSD,
but one study by Hinton, Kredlow, and colleagues (2012) found that CBT combined with
paroxetine was effective in reducing not only PTSD symptoms, but also culturally salient
somatic complaints and culturally specific disorders in a group of 56 Cambodian refugees with
PTSD.
Group Therapy
Several of the therapies previously mentioned, and some discussed in the “Other Interventions”
section, may be delivered in a group format. However, many of these interventions have not been
evaluated as group treatments for clients who have PTSD and/or trauma histories. Group
interventions may be particularly useful for clients with PTSD, because PTSD often causes
isolation and disengagement from others (Ford, Fallot, & Harris, 2009).
Therapeutic groups may consist of people who share a common type of trauma, such as combat
trauma (Schnurr et al., 2003) or torture/political violence (Kira et al., 2012). Homogeneity in
clients’ backgrounds may be advisable for reasons connected to trauma. For example, in an
article on group therapy for refugees and torture survivors, Kira and colleagues (2012)
recommended single-gender groups (to facilitate expression of taboo topics) and groups of a
single ethnicity (to build self-esteem/group pride and avoid intergroup conflicts). Survivors of
childhood sexual abuse (Classen, Koopman, Nevill-Manning, & Spiegel, 2001) or other sexual
trauma (Lynch, 2011) are other populations for whom trauma-specific and/or gender-specific
groups may be preferred.
Shea, McDevitt-Murphy, Ready, and Schnurr (2009) reviewed research on group therapy for
PTSD. They noted that cognitive–behavioral group therapy, which has been evaluated with
combat veterans and adult survivors of sexual abuse, is more effective than nontreatment
controls and about as effective as present-centered group therapy at reducing PTSD symptoms.
Another review of PTSD treatments by Bisson and Andrew (2009) similarly concluded that
trauma-focused CBT groups are more effective than waitlist controls and not significantly
different from group CBT not focused on trauma.
The major study evaluated by both these reviews found that both trauma-focused CBT and
present-centered group interventions were associated with significant improvements in a number
of PTSD symptom measures and significant reductions in the use of VA services during the year
after the interventions (Schnurr, Friedman et al., 2003). Although dropout rates were somewhat
higher for clients who received the trauma-focused CBT group intervention, for those clients
who completed 24 or more sessions (out of 35), participation in the trauma-focused CBT group
1-90 Part 3, Section 1—A Review of the Literature
was associated with more improvement in avoidance/numbing and hyperarousal PTSD
symptoms than was participation in the other group. Shea and colleagues (2009) also noted that
survivors of childhood sexual abuse who participated in interpersonal/process groups had better
outcomes than nontreatment controls and outcomes that were not significantly different from
those of survivors who participated in trauma-focused groups. However, this type of group
intervention has been found to be ineffective in groups where one or more participants have
BPD. Insight-oriented/supportive groups may be more effective than no-treatment controls.
Another study conducted with survivors of childhood sexual abuse (N=166) found significantly
greater reductions in PTSD symptoms among those who participated in either trauma-focused
group or present-centered group therapy (both based on CBT principles) than among those
assigned to a waitlist control group, but it found no significant differences in PTSD outcomes
between the two treatment groups (Classen et al., 2011). The only significant difference in
outcomes between the two treatment groups was that participants in the trauma-focused group
had a significantly greater reduction in anger. Additionally, Shea and colleagues (2009) observed
that, although trauma-focused groups appeared to be as effective as other types of group therapy
for treating PTSD, there was little evidence suggesting that they were any more effective.
Likewise, there was no evidence that group therapy for PTSD was any more or less effective
than one-on-one interventions (although they were only able to locate one study that made such a
comparison).
Family and Couples Therapy
Although it is not recommended for everyone with PTSD, a number of reviews and guidelines
indicate that family or couples therapy is a useful second-line approach to treating otherwise
resistant PTSD and is a useful primary approach for clients who have significant family issues
that need to be addressed as part of their treatment (e.g., Cukor, Spitalnick, Difede, Rizzo, &
Rothbaum, 2009; DoD/VA, 2010; Sherman, Zanotti, & Jones, 2005). There is good reason to
believe that family and couples interventions may be helpful for people with PTSD, and a family
member’s PTSD will likely negatively affect family interactions and the entire family’s
behavioral health (Erbes, 2011; Guay et al., 2006). In their review of couples and family therapy
for clients with PTSD, Riggs, Monson, Glynn, and Canterino (2009) observed that such
interventions typically either focus on healing the disruptions to the family and/or relationship
that results when one member has PTSD or involving the family/partner in treating one family
member/partner’s PTSD, although some more recent interventions (e.g., Monson, Stevens, &
Schnurr, 2005) attempt both. In some cases, for example in the wake of natural disasters, more
than one family member may be exhibiting the effects of posttraumatic stress, and a somewhat
different focus may be required.
Riggs and colleagues (2009) reviewed limited research regarding behavioral family therapy,
behavioral marital therapy, cognitive–behavioral couples treatment, lifestyle management
courses, emotionally focused couple therapy, spousal education and support programs, family
systems-based therapy, and critical interaction therapy. They found relatively strong evidence
supporting the use of behavioral family and behavioral marital therapies, somewhat weaker
evidence supporting the use of cognitive–behavioral couples treatment and lifestyle management
courses, and weak to no support for the other types of family interventions included in the
review. Structured approach therapy (SAT) is yet another couples-based therapy for PTSD that
Trauma-Informed Care in Behavioral Health Services 1-91
has been evaluated with veterans and their spouses for reducing PTSD avoidance symptoms
(Sautter, Armelie, Glynn, & Wielt, 2011). Preliminary research indicates that participants (six
Vietnam veterans and their partners) experienced significant reductions in avoidance symptoms
(according to self-reports, clinician ratings, and partner ratings), emotional numbing, and overall
PTSD severity according to both the CAPS and the PCL following participation in SAT (Sautter,
Glynn, Thompson, Franklin, & Han, 2009).
Fredman, Monson, and Adair (2011) recommended cognitive–behavioral conjoint therapy for
PTSD specifically with veterans and their families and provided a case study in its use. Weine
and colleagues (2008) recommended multiple-family groups for refugees with PTSD and their
families to increase participation in behavioral health services. Some clients may express a
preference for family/couples therapy, especially if it is offered as an option for treatment. For
instance, a survey of 97 National Guard members with spouses and children (47 with PTSD)
expressed a preference for family therapy (Khaylis, Polusny, Erbes, Gewirtz, & Rath, 2011).
Other Interventions
Promising new approaches for treating PTSD are also being tried or evaluated but require further
research before they can be recommended. Cukor and colleagues (2009) reviewed research on
many of these, including couples/family therapy, behavioral activation, trauma management
therapy, interoceptive exposure, mindfulness, imagery rescripting, imagery rehearsal therapy,
DBT, ACT, thought-field therapy, trauma incident reduction, visual kinesthetic disassociation,
and virtual reality ET. Their major conclusions in regard to these new approaches were:
There is strong evidence supporting the use of new technology, including virtual reality, in
the treatment of PTSD.
D-cycloserine for use in enhancing ET is the most promising new medication being
evaluated, and its use is likely to reduce the time needed for ET.
There is good theoretical support and some evidence suggesting that family and couples
therapy will be useful for some clients, but conclusive evidence is still lacking.
ACT and DBT may be useful for increasing distress tolerance, and the latter has been found
effective for women with histories of childhood abuse but not with other populations
(whereas the former lacks research demonstrating its effectiveness for people with PTSD).
Behavioral or cognitive–behavioral approaches (e.g., behavioral activation, mindfulness
meditation therapy) have good evidence demonstrating their usefulness in ameliorating some
PTSD symptoms.
Trauma management therapy, used together with ET, shows promise as a treatment for
negative PTSD symptoms.
Imagery-based treatments (i.e., imagery rescripting and imagery rehearsal therapy) appear to
be useful in some contexts, the former as a treatment for PTSD-related nightmares and the
latter as a potential enhancement to imaginal ET.
For all of these interventions, further research is needed. The authors observed that some of the
other approaches they considered (e.g., complementary approaches such as yoga and
acupuncture) may also prove to be useful adjuncts to treatment. Hollifield (2011) also discussed
the use of acupuncture to treat PTSD, noting that no research studies are available concerning its
effectiveness, but some research and theory suggest that acupuncture may be effective given its
1-92 Part 3, Section 1—A Review of the Literature
action in other areas. People who are susceptible to hypnosis have an elevated risk for
developing PTSD following trauma exposure, and for this and other reasons related to the nature
of PTSD symptoms, several authors have recommended hypnosis as an adjunctive treatment for
PTSD (Cardeña, Maldonado, van der Hart, & Spiegel, 2009). This review also discussed
methods for using hypnosis to help clients with PTSD. Creative therapies, such as art and music
therapy, have been used with this population. Clinical reports indicate that they can be effective,
but there is little research supporting their use with adults who have PTSD (more is available
regarding children and adolescents; see review by Johnson, Lahad, & Gray, 2009).
Dropout and Treatment Response
Rates of dropout and nonresponse to treatment are high for most of the interventions discussed
thus far, even those most often recommended for this population. Schottenbauer, Glass, Arnkoff,
Tendick, and Gray (2008) reviewed data on dropout and nonresponse rates for the most
commonly used PTSD treatments. They found dropout rates ranging from 0 to 50 percent for ET/
PE, 5 to 32 percent for CBT, and 0 to 36 percent for EMDR. Nonresponse rates were 20 to 67
percent for ET/PE, 16 to 71 percent for CBT, and 7.3 to 92 percent for EMDR. Although the
authors observed that these rates are high, they also cautioned against making comparisons of
dropout/nonresponse between different types of interventions because of substantial differences
in methodology. A meta-analysis that included 25 studies evaluating ET, CBT, or EMDR found
that dropout rates for the three types of interventions did not differ significantly; control
conditions had significantly lower dropout rates than either ET or CBT, but not EMDR
(Hembree et al., 2003).
Schottenbauer, Glass, Arnkoff, Tendick, and Gray (2008) also reviewed research associated with
dropout and nonresponse to treatment. They found that dropout rates for a number of
recommended treatments (ET, cognitive therapy, stress inoculation therapy, and EMDR) were
higher than those found in control conditions, such as waitlists and relaxation training. Surveys
of clients who had dropped out of treatment suggested that logistical issues (e.g., lack of
transportation, inability to find child care) were often a problem, as were problems with social
adjustment (the latter according to a study of ET conducted with clients who had PTSD and co-
occurring alcohol dependence). Another study included in the review found that the credibility of
the treatment for the client was a significant factor in dropout.
Zayfert and DeViva (2010) cited studies that found that the risk of treatment dropout is greater
for clients with more severe PTSD symptoms (especially more severe avoidance symptoms),
with greater anxiety, with more severe symptoms of depression, and with greater use of alcohol.
Male clients are also more likely to drop out of treatment than female clients. These authors also
observed that worsening of symptoms during treatment, which many clinicians believe is a cause
of treatment dropout, has not been associated with increased dropout rates.
Zayfert and DeViva (2010) analyzed factors associated with treatment response, observing that
studies have found that childhood trauma and/or complex trauma is associated with worse
response, as is use of prescription sedatives, male gender, higher suicidality ratings, being single
(rather than married or living with a partner), having more severe PTSD symptoms, having
GAD, having greater anger, and having more physical pain. On the other hand, Schottenbauer,
Glass, Arnkoff, Tendick, and Gray (2008) observed, based on their review, that demographic
factors appear to have very little relationship to treatment response. Also, trauma severity
Trauma-Informed Care in Behavioral Health Services 1-93
(particularly severity of childhood abuse) may have a negative effect on outcomes, but not every
study has found this to be the case. They also found mixed evidence on the effects of co-
occurring depression, co-occurring personality disorders, anger related to trauma, and
guilt/shame on PTSD treatment outcomes. They discussed some of the methods suggested in the
literature to improve treatment response, including being flexible about the number of sessions
and offering or using more than one treatment technique/intervention.
Integrated Approaches for Trauma and Substance Abuse
Traumatic stress and PTSD frequently co-occur with substance use disorders. As a result, many
clients seeking treatment for PTSD will require substance abuse treatment services and vice
versa. Ouimette, Moos, and Brown (2003) reviewed early research on the treatment of co-
occurring PTSD and substance use disorders and concluded, as did later reviews, that concurrent
PTSD and substance abuse treatment is preferred.
Dass-Brailsford and Myrick (2010) reviewed research and clinical opinions on the importance of
integrated treatment for clients with co-occurring PTSD and substance use disorders, discussing
factors such as the potential benefits of integrated approaches, potential implementation barriers,
and specific models of integrated substance abuse and trauma/PTSD treatment. Limited research
suggests that some of the integrated treatment models they discussed are effective at reducing
substance abuse, PTSD symptoms, and other mental disorder symptoms. They also observed
that, because of the lack of research recommending one specific model over another, providers
should consider other factors, such as training requirements, philosophical/theoretical
orientations, and appropriate settings in selecting a specific intervention.
The specific interventions included in Dass-Brailsford and Myrick’s (2010) review were:
Addictions and Trauma Recovery Integration, a 12-week program that uses
psychoeducation, expressive therapy, mindfulness, and guided relaxation that can be
provided in a group or individual format and is delivered by either peers or professionals
(Miller & Guidry, 2001).
TRANSCEND, a 12-week CBT intervention intended for veterans in partial hospitalization
settings (Donovan, Padin-Rivera, & Kowaliw, 2001).
Assisted Recovery Trauma and Substances, a 20-week, individual CBT intervention that
addresses both PTSD and substance use disorders; it has been evaluated with clients in
methadone maintenance and cocaine treatment programs (Triffleman, 2002).
Helping Women Recover, a 17-week, gender-responsive intervention that uses CBT,
expressive arts, and relational theory (Covington, 2008).
Substance-Dependence Posttraumatic Stress Disorder Therapy (SDPT), a 20-week
intervention intended for outpatients that uses ET, psychoeducation, and coping skills
training (Triffleman, 2000).
Concurrent Treatment of PTSD and Cocaine Dependence, which the developers believe
can be used with any substance use disorders, and which uses coping skills training,
cognitive restructuring, relapse prevention, and ET (Coffey, Schumacher, Brimo, & Brady,
2005).
1-94 Part 3, Section 1—A Review of the Literature
Seeking Safety, a 25-session, present-focused therapy for co-occurring disorders, which is
one of the more extensively evaluated of the integrated interventions included in the review
(Najavits, 2002).
Trauma Affect Regulation: Guide for Education and Therapy (TARGET), a nine-
session, gender-specific intervention adapted from a trauma treatment intervention for clients
with other mental disorders, which uses psychoeducation and present-centered therapy to
help clients learn effective emotional regulation techniques (Ford & Russo, 2006; Frisman,
Ford, Lin, Mallon, & Chang, 2008).
Trauma Recovery and Empowerment Model (TREM), a 24- to 29-session group
intervention originally developed for women who were survivors of physical/sexual abuse
that since has been adapted for men (M-TREM); it has been implemented in a wide variety of
treatment settings (Fallot & Harris, 2002).
The Triad Women’s Project, a 16-week group intervention for women that uses integrated
case management services, a curriculum-based treatment group, and a peer support group
(Clark & Fearday, 2003)
Torchalla, Nosen, Rostam, and Allen (2012) conducted a meta-analysis of 17 trials of integrated
treatments for PTSD/trauma and substance use disorders. Their review included six of the
interventions listed previously (i.e., Seeking Safety, TARGET, TREM, TRANSCEND, SDPT,
and CTPCD) and an additional three, which were:
Integrated CBT for PTSD in Addictions Treatment, an 8- to 12-session intervention that
uses psychoeducation, skills training, and cognitive processing and restructuring (McGovern
et al., 2009; McGovern, Lambert–Harris, Alterman, Xie, & Meier, 2011).
Dual Assessment and Recovery Track, a treatment for co-occurring substance use and
other mental disorders (including PTSD) that involves 9 hours of treatment per week for a
12-week period and is designed to be implemented in a therapeutic community-oriented
outpatient program (Sacks, McKendrick, Sacks, Banks, & Harle, 2008).
Integrated Tobacco Cessation Treatment, a six-session intervention involving behavioral
counseling, stress management, and pharmacotherapy for smoking cessation (McFall et al.,
2006).
Torchalla and colleagues (2012) found that integrated treatments can reduce both PTSD
symptoms and substance abuse, and across the reviewed studies, the data suggest that such
treatments are associated with relatively large reductions in symptoms. However, most of the
studies that compare integrated and nonintegrated treatments (the latter typically being substance
abuse treatment interventions) did not report significant differences between the two in terms of
either substance abuse or PTSD outcomes, nor did the authors’ meta-analysis find significant
differences between these various integrated treatments (taken as an aggregate) and active
controls. The authors explored reasons for their failure to find significant differences in outcomes
between integrated and nonintegrated treatments, including low participation in many of the
studies. They also pointed out that, even though some research suggests that integrated
treatments do not have as great an effect on clients with low levels of PTSD symptoms, the
majority of the studies did not limit participation to clients with diagnosable PTSD; integrated
treatments may be effective in reducing PTSD symptoms because they either reduce substance
Trauma-Informed Care in Behavioral Health Services 1-95
abuse or affect general mental health. Comparison treatments in many of these studies
accomplish the same ends.
One study included in Torchalla and colleagues’ (2012) review appears to contradict the idea that
addressing substance abuse alone is usually sufficient to reduce PTSD symptoms’ severity. Hien,
Campbell, Ruglass, Hu, and Killeen (2010) analyzed data from a National Institute on Drug
Abuse clinical trial (N=353). They found that participants who responded to treatment with
improvements in PTSD symptoms (as measured with the CAPS) but not with reductions in the
amount of substances used were significantly more likely to later be classified as “globally
responsive” (indicating improvements in both PTSD and substance use) compared with those
who showed improvements in substance abuse use outcomes but not PTSD. This suggests that if
a sequential approach to treatment is used, it is probably more beneficial to address PTSD first.
In a recent study not included in the reviews previously discussed, the Integrated CBT for PTSD
in Addictions Treatment intervention was found to be more effective than individual substance
abuse treatment counseling for reducing PTSD reexperiencing symptoms and increasing
remission from PTSD, whereas both options were comparable in terms of reducing substance
abuse (McGovern et al., 2011). In addition, participants in the study who received the integrated
CBT intervention were more likely to initiate and engage in treatment than those who received
individual substance abuse treatment counseling.
Other Integrated Approaches
Although most of the integrated treatment interventions that address traumatic stress and PTSD
are intended for people with substance use disorders, a few interventions have been developed
for clients with PTSD and other mental disorders. A large percentage of people with BPD have
significant trauma histories, and many have co-occurring PTSD. Harned and colleagues (2012)
conducted a preliminary evaluation of a year-long integrated treatment that uses DBT for BPD
and exposure therapy for PTSD. Of the 13 participants who completed at least one treatment
session, 60 percent no longer met criteria for PTSD at the end of treatment (for treatment
completers, 71.4 percent no longer had PTSD). Participants also showed significant
improvements in terms of suicidal ideation, anxiety, shame, guilt, depression, and social
adjustment, and they demonstrated no increase in self-injurious thoughts and behaviors.
A pilot study by Nixon and Nearmy (2011) of an integrated intervention for clients with PTSD
and major depression that uses behavioral activation for depression and ET and cognitive
restructuring for PTSD found the intervention to be promising. Twenty clients with those co-
occurring disorders were included in the trial (14 of whom completed the intervention); 3 months
after the intervention, participants had significant reductions in both PTSD and depression
symptoms, with 60 percent no longer meeting criteria for a PTSD diagnosis and 70 percent no
longer meeting criteria for major depression.
Integrated interventions have also been developed to treat co-occurring PTSD and panic
disorder/attacks. Falsetti and colleagues (2008) evaluated one such integrated treatment, Multiple
Channel Exposure Therapy, with 62 women who had PTSD and a history of panic attacks (89
percent of whom met criteria for a panic disorder diagnosis). They found that participants in the
intervention had significantly greater improvements in terms of PTSD, panic attacks, and
1-96 Part 3, Section 1—A Review of the Literature
symptoms of depression than did participants assigned to a waitlist control group. Improvements
in PTSD and panic symptoms had not diminished significantly at a 6-month follow-up. Another
culturally relevant model of integrated CBT for PTSD and panic disorder was found to be
effective in small trials with Cambodian (Hinton et al., 2005) and Vietnamese (Hinton et al.,
2004) refugees.
Treating Complex Trauma/PTSD
Although many existing guidelines for the treatment of PTSD may provide some guidance in
treating the effects of complex trauma, there are no widely disseminated practice guidelines
focused specifically on its treatment (Courtois, Ford, & Cloitre, 2009). However, Cloitre and
colleagues (2011) have provided guidance from an expert clinician survey of 50 clinical experts
(25 of whom specialize in treatment for complex trauma). The survey respondents largely agreed
that treatment for complex trauma should have a phased approach in which multiple
interventions are available; if the client does not respond to the first option, others should be
used. They also generally agreed that interventions should be tailored to the client’s specific
needs, taking the client’s specific symptoms into account. There was almost universal agreement
that treatment should be provided in an individual format, but that as a second-line approach,
additional sessions of group treatment could be added. They generally agreed that treatment
should be provided at least on a weekly basis in the initial phase.
Regarding specific treatment elements or interventions recommended by the expert panel, the
only first-line approaches in terms of effectiveness, safety, and acceptability were ones that were
emotion-focused or addressed emotion regulation (Cloitre et al., 2011). Other approaches that
were considered first-line in terms of effectiveness and with reasonably high ratings in safety and
acceptability were anxiety/stress management, cognitive restructuring, and psychoeducation
about the effects of trauma. Meditation and mindfulness approaches were frequently cited as
appropriate second-line treatments useful for addressing emotional, attention-related, and
behavioral problems. The survey respondents also recommended first- and second-line
interventions for specific sets of symptoms. For example, psychoeducation, anxiety/stress
management, and emotion regulation were recommended as the first approaches to use for
hyperarousal, whereas narration of trauma memory and cognitive restructuring were
recommended as second-line approaches for those symptoms.
In an earlier review, Courtois and colleagues (2009) provided specific recommendations for
conducting therapy with clients who have complex PTSD. These recommendations included
suggestions for assessment, defining treatment goals, specific tasks for treatment to meet those
goals, and principles and tasks to guide clinicians through three phases of treatment (i.e.,
promoting safety and stabilization, processing traumatic memories, reintegration). Many of the
approaches recommended for treating PTSD in other populations are also effective for clients
with complex PTSD, including CBT (Jackson et al., 2009) and pharmacotherapy (Opler,
Grennan & Ford, 2009). Both family/couples interventions (Ford & Saltzman, 2009; Johnson &
Courtois, 2009; Schwartz, Schwartz, & Galperin, 2009) and group interventions (Dorrepaal et
al., 2010; Ford et al., 2009) may also be beneficial, and they may even be more important in
cases of complex trauma, because complex trauma histories typically have a negative effect on
an individual’s ability to form positive relationships with partners and friends (Schwartz et al.,
2009). Other clinicians have recommended the use of experiential and emotion-focused therapies
Trauma-Informed Care in Behavioral Health Services 1-97
(Fosha, Paivio, Gleiser, & Ford, 2009) and sensorimotor techniques, such as mindfulness and
sensorimotor memory processing (Fisher & Ogden, 2009), with this population. Jackson and
colleagues (2010) discussed basic steps involved in treating PTSD as well as commonly
encountered problems, such as resistance to experiencing feelings, to change, and to improving
interpersonal functioning.
Some of the studies discussed elsewhere in this TIP do include individuals who have experienced
complex trauma. In particular, survivors of severe childhood abuse often have complex PTSD.
The “Survivors of Childhood Abuse” section includes studies relevant in this context. Other
populations with histories of repeated interpersonal violence, such as torture survivors (Johnson
& Thompson, 2008) and prisoners of war (Solomon, Dekel, & Mikulincer, 2008), also often
have complex trauma. However, few controlled trials are available that specifically focus on
clients with complex PTSD, and more research in this area is needed (Dorrepaal et al., 2010).
Some interventions have been developed specifically for clients with complex PTSD. Contextual
behavior trauma therapy (CBTT) is another intervention designed specifically for clients with
histories of complex trauma and the experiential avoidance and developmental deficits that result
from such traumatic experiences (Follette, Iverson, & Ford, 2009). CBTT uses techniques drawn
from ACT, behavioral activation, DBT, and functional analytic psychotherapy. Contextual
therapy was developed to treat adults who have sustained prolonged childhood abuse (Gold,
2009). Contextual therapy looks at the context of a client’s trauma; it has an initial phase to help
clients work on building a sense of safety/security prior to addressing trauma and a final phase to
help clients integrate gains made in terms of interpersonal interactions, practical skills, and
insight into experiences and behaviors.
A group intervention designed for people with complex trauma that was evaluated in the
Netherlands is Stabilizing Group Treatment (Dorrepaal et al., 2010). This 20-week intervention
used psychoeducation and CBT skills training. In a pilot study, participants (n=36) had
significant reductions in PTSD and BPD symptoms from baseline to the end of the intervention.
At a 6-month follow-up assessment, 78 percent no longer met criteria for complex PTSD. In a
review concerning the use of psychodynamic approaches to treat trauma/PTSD, Schottenbauer,
Glass, Arnkoff, & Gray (2008) suggested that psychodynamic approaches may be particularly
relevant for clients with complex trauma/PTSD, because they may be well-suited for addressing
problems with social/interpersonal relationships, general life functioning, and underlying
personality problems that may have developed as the result of repeated trauma (particularly
occurring in childhood).
Treatment for Specific Populations
Any treatment for traumatic stress reactions should be tailored to the specific needs of each
client, but general information pertaining to population characteristics may help guide that
treatment.
People From Diverse Cultural Groups
As with any behavioral health treatment, it is extremely important that providers be culturally
competent when treating clients with traumatic stress reactions and/or trauma histories. Cultural
background influences how individuals respond to trauma and how they present traumatic stress
1-98 Part 3, Section 1—A Review of the Literature
reactions and other behavioral health problems related to traumatic experiences. The section
entitled “Cultural, Ethnic, and Gender Factors in Assessment” provides more information on
culture as a factor in assessing traumatic stress reactions.
Osterman and de Jong (2007) provided a good overview of some of the treatment issues involved
in providing culturally responsive behavioral health services relating to trauma, including the
adaptation of assessment instruments, theoretical ideas about how to respond to traumatic
experiences and traumatic stress reactions with clients from culturally diverse backgrounds, and
the somewhat limited research evaluating PTSD treatment with diverse cultural groups. The
treatment sections refer to such literature when it is available (e.g., the CBT section includes
references to studies evaluating trauma-focused CBT with members of diverse cultural groups).
The section “Refugees” also discusses treatment options and adaptations that are useful with
non-Western cultural groups.
Few studies are available that compare PTSD treatment outcomes for members of diverse
cultural groups, and those that do often fail to account for potentially confounding factors, such
as SES (Lester, Resick, Young-Xu, & Artz, 2010). These authors compared outcomes and
treatment retention rates for African American women (n=94) and White American women
(n=214) who had been victims of interpersonal violence and had PTSD. They found that African
American women were significantly more likely to drop out of treatment than were White
American women, even after controlling for education and income. However, the authors
observed that there were no significant differences in treatment outcomes between African
Americans and White Americans, and this may indicate that a higher dropout rate reflected
greater symptom improvement among African Americans who left treatment.
A volume edited by Marsella, Johnson, Watson, and Gryczynski (2008) discussed in greater
detail how to address traumatic experiences with members of diverse cultural groups found in the
United States. For individuals belonging to cultural groups that have sustained trauma for
multiple generations, treatment should address issues of historical trauma and the relationship of
the client’s traumatic experiences with those of his parents and other generations (Danieli, 2007;
Sotero, 2006). A few specific interventions have been developed for addressing historical trauma
in Native Americans that might also guide similar interventions with other groups (e.g., Yellow
Horse & Brave Heart, 2005). Culture can serve as a factor in building resilience and healing the
effects of trauma; even so, individuals in certain trauma-related predicaments (e.g., internment
during war) may have a strong desire to remove themselves from the persecuted culture, leading
to accelerated deacculturation (Danieli, 2007). In such cases, it may be even more important to
integrate elements of the individual’s cultural background into treatment (Danieli, 2007).
Refugees
Although it is not just a cultural issue, the treatment of refugees from outside the United States
also typically involves cross-cultural exchanges and requires cultural competence. Nickerson,
Bryan, Silove, and Steel (2011) reviewed research on PTSD treatment that specifically involved
refugee populations. They found two approaches that have been studied with this population:
trauma-focused therapies (typically trauma-focused CBT) and multimodal treatments that
attempt to address extensive behavioral and other health problems experienced by this
population. The studies they reviewed indicate that trauma-focused therapies are associated with
significant long-term reductions in PTSD symptoms, but the research involving multimodal
Trauma-Informed Care in Behavioral Health Services 1-99
approaches has generally not found significant long-term reductions (although shorter-term
reductions have been observed). Although research is lacking, published clinical opinion
generally agrees that ET is inappropriate for refugees. Hinton, Rivera, and colleagues (2012)
discussed adapting CBT interventions for refugee populations with non-Western cultural
backgrounds. Many of the suggestions they provided can also be used with other treatment
interventions for this population.
Veterans
The VA and DoD (2010) have published guidelines on treating PTSD for veterans and active-
duty personnel entitled Clinical Practice Guideline for Management of Post-Traumatic Stress
(described in the “Military Prevention Programs” section). Other guidance on appropriate
treatments may be found in reviews on treating trauma/traumatic stress reactions in this
population (e.g., Goodson et al., 2011; Hoge, 2011; Sharpless & Barber, 2011). However, these
guidelines do not address co-occurring complexities, such as substance abuse, psychosis,
individuals in danger of harming self or others, personality disorders, current homelessness or
domestic violence, and other issues. Thus, for these populations, the clinician should use careful
judgment in applying the guidelines.
Goodson and colleagues (2011) recommended treatments for veterans that are largely the same
as those recommended for the general population. Their review found that treatments for PTSD
in veterans, taken as a whole, have a medium effect size (i.e., d=0.43 across all the studies and
d=0.48 for the controlled studies), with larger effect sizes for CPT and trauma-focused CBT. The
review also observed that 66 percent of veterans included in the research reviewed had better
outcomes than did those who were in control groups. More detailed information on PTSD
treatment for veterans can be found in the planned TIP, Reintegration-Related Behavioral Health
Issues in Veterans and Military Families (SAMHSA, planned f).
Survivors of Sexual Assault
Survivors of sexual assault have elevated risk for a number of behavioral health disorders and
problems in addition to PTSD (e.g., eating disorders, depression, sleep disorders, other anxiety
disorders, suicide attempts), and many will have complex trauma (Chen et al., 2010), so
behavioral health services for this population will often need to address multiple issues.
Vickerman and Margolin (2009) reviewed research on behavioral health treatment for survivors
of rape, including treatment for PTSD, depression, and/or other anxiety disorders. They
concluded that CPT and PE have the most data supporting their effectiveness; EMDR has also
been found effective, albeit in fewer studies. In research comparing interventions, CBT
interventions have been found to be more effective than supportive counseling. Across all
interventions, however, there is a high rate of dropout from treatment, with more than a third of
clients leaving before completing treatment. Foa and Rothbaum (1998) also discussed behavioral
health treatment for survivors of rape, with particular attention to CBT techniques. Women with
sexual trauma may prefer working with female clinicians and/or all-female treatment groups
(Lee, Westrup, Ruzek, Keller, & Weitlauf, 2007; Nelson-Zlupko, Dore, Kauffman, &
Kaltenbach, 1996), but perhaps more important than the gender of clinicians or group members
is that services be responsive to gender issues and centered on the needs of women who have
experienced such trauma.
1-100 Part 3, Section 1—A Review of the Literature
Survivors of Childhood Abuse
As with other populations of people with PTSD, CBT has been found to be effective at reducing
PTSD symptoms for adults with PTSD related to childhood abuse, which in most studies
involved sexual abuse (e.g., Classen et al., 2011; McDonagh et al., 2005; Resick et al., 2003).
Cloitre and colleagues (2010) noted that not all trauma-focused CBT interventions are designed
to address the interpersonal, social adjustment, and/or emotional regulation problems that are
common among people with histories of repeated childhood abuse, and thus caution must be
used in selecting appropriate interventions. They also indicated that their own CBT intervention,
Skills Training in Affective and Interpersonal Regulation (STAIR), was developed for this
population.
Particular CBT interventions may be useful for addressing specific behavioral health
symptoms/concerns. For example, a small (n=9) pilot study found that two sessions of cognitive
restructuring and imagery modification were effective at alleviating feelings of contamination
experienced by survivors of childhood sexual abuse (Steil, Jung, & Stangier, 2011). Only a few
studies have evaluated optimum duration and intensity of treatment for adults with histories of
childhood sexual abuse, but given that members of this population frequently drop out of
treatment and often require long-term treatment (Gilbert et al., 2009; Schumm et al., 2006), this
issue may be even more important in their treatment. One study, which has some methodological
problems, found that a 6-month group treatment for childhood sexual abuse was associated with
somewhat better outcomes than a 12-month group treatment, leading the authors to conclude that
a shorter, more intensive course of treatment may be preferred for this population (Kreidler &
Einsporn, 2012).
Treatment sequencing is another important issue with this population, as multiple interventions
are often required to address complex trauma. Researchers randomly assigned 104 women with
PTSD related to childhood sexual abuse to receive the STAIR intervention followed by narrative
ET, supportive counseling followed by narrative ET, or STAIR followed by supportive
counseling (Cloitre et al., 2010). The authors found that participants in the first group were
significantly more likely to achieve sustained remission from PTSD than were participants in the
other two groups (whereas those in group 3 were more likely to do so than those in group 2). In
terms of percentages, 27 percent of group 1 achieved sustained full remission, 13 percent of
group 3 did, and none of the members in group 2 did. In a later analysis of study data, Cloitre,
Petkova, Wang, and Lu (2012) found that the level of dissociative symptoms a client had at
baseline did not significantly change these outcomes, except that participants with high levels of
dissociative symptoms who were in group 1 continued to show improvements in PTSD
symptoms during follow-up, but those assigned to the other two groups did not.
People With Lower SES
People with lower SES are likely to have multiple needs that should be addressed if treatment for
PTSD is to succeed (Kelly et al., 2010). Kelly and colleagues (2010) discussed case examples of
medical and psychosocial needs relating to PTSD, methods of outreach and engagement, and
suggestions for providing appropriate services for this population. Dropout rates are high for
PTSD treatment, but a study of CBT treatment (N=31) found significantly higher dropout rates
for individuals with low income and lower levels of education (Difede et al., 2007).
Trauma-Informed Care in Behavioral Health Services 1-101
People With SMI
Only a few studies have addressed PTSD treatments specifically for people with SMI; these
studies, along with some authors’ clinical opinions, suggest that CBT is likely the best option for
this population. Most of the research on using trauma-focused CBT to treat PTSD in people with
SMI found it to be an effective approach. In one study, 108 clients with SMI (85 percent of
whom had a major mood disorder, 15 percent of whom had schizophrenia or schizoaffective
disorder, and 25 percent of whom had co-occurring BPD) were randomly assigned to receive
trauma-focused CBT or standard treatment (Mueser et al., 2008). The authors found, using an
intent-to-treat analysis to account for missing data, that CBT was associated at a 6-month follow-
up with significantly better outcomes for PTSD symptoms, other mental disorder symptoms, and
perceived health. CBT appeared to have the greatest effect on participants with more severe
PTSD. The authors also found that homework completion was associated with greater reductions
in PTSD symptoms, arguing for the importance of this CBT component. Sherrer (2011) argued
that cognitive restructuring (another CBT intervention) is likely the most appropriate PTSD
treatment for people with SMI, as this population has difficulties objectively evaluating
traumatic experiences. Rakofsky and Dunlop (2010) also reviewed research on the treatment of
PTSD and other anxiety disorders for clients with bipolar disorder. They covered little research
specific to PTSD but presented some general considerations for treating anxiety and anxiety
disorders in this population.
People Who Are Homeless
Hopper and colleagues (2010) reviewed literature regarding people who are homeless and gave
recommendations for providing them with trauma-informed services. They concluded that
providing trauma-informed services to this population can produce better behavioral health
outcomes, improve housing stability, and decrease use of crisis-based services such as
emergency room services. The authors also noted that these services are cost-effective for and
well-received by this population.
People With Physical and Cognitive Disabilities
Few studies have looked at the treatment of trauma-related behavioral health problems in people
with disabilities. Focht-New, Clements, Barol, Faulkner, and Service (2008), however, provided
guidelines on treating and assessing trauma and traumatic stress reactions in this population and
reviewed some relevant research. Mevissen and de Jongh (2010) also reviewed research on
assessment and treatment of PTSD in people with intellectual disabilities, discussing several
adaptations to treatment, such as training caregivers and making changes to assessments.
Studies have been conducted concerning the treatment of PTSD in veterans with trauma-related
disabilities (particularly TBI). Veterans from recent conflicts have high rates of both TBI and
PTSD, and it is often difficult to distinguish resulting impairments, especially in cases of mild
TBI (Hill, Mobo, & Cullen, 2009). In their review of the literature on TBI and PTSD, Vasterling,
Verfaellie, and Sullivan (2009) observed that there is good evidence that PTSD is even more
common in cases of mild TBI than in more severe TBI, and mild TBI is even more common than
PTSD among veterans of recent conflicts.
The VA and DoD have developed TBI screening tools that may aid in distinguishing TBI and
PTSD (Hill et al., 2009; Terrio, Nelson, Betthauser, Harwood, & Brenner, 2011). The
1-102 Part 3, Section 1—A Review of the Literature
combination of PTSD, mild TBI, and chronic pain complaints is common enough among
veterans of OEF/OIF that it has been labeled “post-deployment multi-symptom disorder”
(Walker, Clark, & Sanders, 2010). These authors suggested the use of an integrated treatment
model to help improve coping and decrease functional disability, but more research is needed to
evaluate the intervention.
Trauma-Informed Intervention Considerations
Special considerations in the treatment of clients with traumatic stress reactions and/or trauma
histories are not covered in the previous treatment sections but deserve special attention.
Self-Harm and Suicidality
Traumatic experiences may contribute to suicidal behaviors regardless of whether those events
result in a traumatic stress reaction, and, in fact, some research suggests that PTSD does not
increase suicidality after controlling for trauma exposure. In the largest study to date to evaluate
suicidality and trauma exposure, 102,245 respondents in 21 countries were interviewed as part of
the World Mental Health Survey (Stein et al., 2010). A wide range of traumatic experiences were
associated with increased odds of suicidal ideation and/or suicide attempts, but the greatest
increase was associated with being the victim of sexual violence followed by interpersonal
violence. Being exposed to war was associated with a significant increase in the odds of having a
planned suicide attempt, whereas being the victim of sexual violence was associated with a
significant increase in the odds of making an attempt without a plan (no other traumas were
associated with significant increases in the rates of these two outcomes).
Trauma exposure also appears to have a cumulative effect on suicidality, with repeated
experiences of trauma being associated with increased rates of suicidal ideation and attempts, but
this effect appears to level off at a certain point (at seven traumatic events for ideation and six for
attempts). When the authors evaluated trauma-related suicidality with respect to PTSD
(according to DSM-IV diagnostic criteria), they did not find any further increase in suicidality
associated with PTSD, suggesting that it was the traumatic experience and not the subsequent
mental disorder that largely influenced suicidality. The association of trauma and suicidality was
found to be valid for individuals from diverse cultural backgrounds and from both developing
and developed nations.
Other research has found PTSD to be associated with increased suicidality, although not to the
same degree as many other behavioral health disorders. For example, a study of veterans found
that PTSD increased risk to a lesser degree than did substance use disorders, bipolar disorder,
depression, schizophrenia, or other anxiety disorders, but this study did not control for trauma
exposure (Ilgen et al., 2010). Other research evaluating veterans with depression found that co-
occurring PTSD did not increase suicide rates, although certain other co-occurring mental
disorders did (Pfeiffer, Ganoczy, Ilgen, Zivin, & Valenstein, 2009).
Other reviews on the subject have also concluded that PTSD does affect suicidality, independent
of the effects of trauma exposure. Panagioti, Gooding, and Tarrier (2009) reviewed a wide range
of research on PTSD and suicidality, including studies relating specifically to the effects of
different types of trauma, the role of other co-occurring behavioral health disorders, and the
relationship of the two in specific populations (i.e., people with HIV, refugees, and police
Trauma-Informed Care in Behavioral Health Services 1-103
officers). They concluded that PTSD does have an independent effect on increasing suicidality,
and this is often further increased by the presence of co-occurring depression, which may
mediate the relationship between PTSD and suicidality. This relationship exists regardless of the
type of trauma involved. Research also indicates that the PTSD symptom of reexperiencing has
the strongest relationship with suicidality.
Krysinska and Lester (2010) conducted a meta-analytic review of 50 studies that evaluated the
relationship between PTSD and suicidality (defined as suicide attempts and/or suicidal ideation).
They concluded that PTSD did have a significant relationship to suicidality, but that, when
controlling for other behavioral health disorders, that relationship was substantially weaker.
However, they did not find a significant relationship between PTSD and completed suicide. The
evidence is somewhat stronger that PTSD is associated with increased self-harming behavior
(self-harm is any type of intentionally self-inflicted harm, regardless of the severity of injury or
whether suicide is intended). In research conducted with 2,854 soldiers returning from OIF,
individuals with PTSD diagnoses were significantly more likely to report thoughts about self-
harm than were those without PTSD, but they were not significantly more likely to report
suicidal ideation (Maguen et al., 2011).
Other research indicates that complex PTSD is associated with greater self-harming behavior
than simple PTSD (Dyer et al., 2009). Also, a study of deliberate self-harming behavior in
substance abuse treatment clients found a significant association between symptoms of
emotional dysregulation and self-harm behavior, suggesting that such symptoms may play a key
role in promoting such behaviors among individuals with PTSD (Gratz & Tull, 2010). Complex
PTSD is also associated with more self-harming behavior than noncomplex PTSD (Dyer et al.,
2009). It is worth noting that the relative impact of PTSD on suicidality may vary by culture, as
Joe, Baser, Breeden, Neighbors, and Jackson (2006) found that anxiety disorders appeared to
have a significantly greater effect on suicide risk for African Americans than for members of
other major racial/ethnic groups. More information on treating clients with suicidal thoughts and
behaviors can be found in TIP 50, Addressing Suicidal Thoughts and Behaviors in Substance
Abuse Treatment (CSAT, 2009a).
Sleep Disturbances
Although difficulties falling or staying asleep may be a symptom of PTSD and may respond to
standard PTSD treatment, they often require specific interventions to be effectively treated
(Nappi, Drummond, & Hall, 2012). Carney and Edinger (2010) reviewed research indicating that
the majority of people with PTSD will have some sleep disturbances and that sleep complaints
following a traumatic event are associated with an increased risk for developing PTSD. Among
returning OEF/OIF veterans with PTSD, sleep disturbances are the most commonly reported
symptom and often predate the advent of other PTSD symptoms (McLay, Klam, & Volkert,
2010). Other recent research also confirms that disordered/disrupted sleep is a core feature of
PTSD (Nappi et al., 2012). Sleep disturbances among people with PTSD are also associated with
increased risk for suicidal ideation, neurocognitive deficits, impaired social functioning, and a
variety of physical health complaints (Nappi et al., 2012).
In another review, Babson and Feldner (2010) observed that traumatic events, whether or not the
individual develops PTSD, can cause or exacerbate difficulties falling asleep, falling back to
sleep after waking, and staying asleep through the night. Certain aspects of traumatic events also
1-104 Part 3, Section 1—A Review of the Literature
appear to affect sleep patterns, such that traumatic events of longer duration have a greater effect,
and people experience more severe sleep disturbance when the event has occurred more recently.
However, such problems, at least for those individuals who develop PTSD, also may persist for
many years (as many as 45 years in one study). The authors also referenced literature indicating
that sleep problems can interfere with recovery from PTSD.
Carney and Edinger (2010) and Nappi and colleagues (2012) also reviewed research on the
treatment of sleep disturbances in people with PTSD. Nappi and colleagues (2012) concluded
that some, but not all, research regarding the effects of standard PTSD treatments (e.g., trauma-
focused CBT, EMDR) indicates that they can be effective at eliminating nightmares but not
PTSD-related insomnia, which often continues after such treatment. Therefore, they
recommended either psychological or pharmacological treatments specifically aimed at insomnia
and reviewed available options.
Spirituality and Religious Beliefs
Religious beliefs have been found in a number of contexts to have a protective function relative
to PTSD (e.g., Bradley, Schwartz, & Kaslow, 2005; Cheung, 1994), but not in every context
(Ben-Zur, 2008). It is also not clear whether changes in religiosity positively affect traumatic
stress reactions among those who have been traumatized, as both posttrauma weakening and
strengthening of religious beliefs have been associated with significant increases in PTSD
symptoms compared with those individuals whose beliefs did not change (Falsetti, Resick, &
Davis, 2003; Hussain, Weisaeth, & Heir, 2011). Other research, however, indicates that certain
types of trauma (e.g., combat trauma) may cause a spiritual crisis; for some clients, addressing
that crisis may improve their behavioral health (Baroody, 2011). Research conducted with
veterans also indicates that loss of religious faith is a major factor in motivating individuals to
seek treatment for PTSD (Fontana & Rosenheck, 2004).
Religious belief/spirituality may also affect other factors, such as finding meaning in life or self-
esteem. For example, according to NCS data, among survivors of childhood abuse, greater
religiosity is associated with significantly higher self-esteem (Reiland & Lauterbach, 2008).
Owens, Steger, Whitesell, and Herrera (2009) conducted an Internet survey of 174 veterans and
found that higher levels of PTSD symptom severity were significantly related to finding less
meaning in life according to self-report. However, when depression was factored into the
equation, a somewhat different picture emerged, so that for veterans with low to moderate levels
of depression (measured with the Depression Anxiety Stress Scales-21), perceiving greater
meaning in one’s life was associated with significantly less severe PTSD; the same was not true
for veterans with severe depression. The authors concluded that improving an individual’s
perception of meaning in his or her life may reduce PTSD symptom severity, except when the
individual also has severe depression.
Although interventions targeting spirituality or religious beliefs are difficult to evaluate, small
studies conducted with veterans have found that spiritual practices, such as mantra repetition
(Bormann, Lui, Thorp, and & Lang, 2011) and transcendental meditation (Rosenthal, Grosswald,
Ross, & Rosenthal, 2011), typically presented in a nondenominational manner, are effective at
reducing PTSD symptom severity. Lang and colleagues (2012) reviewed research and theoretical
support for the use of meditation as an aid in PTSD treatment. Harris and colleagues (2011)
evaluated an eight-session group treatment designed to help veterans who experienced combat
Trauma-Informed Care in Behavioral Health Services 1-105
trauma find religious/spiritual meaning in their experiences and found that participants who
received the intervention had significantly less PTSD symptom severity than did those who were
in a waitlist control group.
Building a Trauma-Informed Workforce
There is general agreement that behavioral health programs where staff members need to address
issues related to trauma and/or need to work with clients who have traumatic stress disorders
should prepare their workforce to serve such clients and to be able to deal with the stress and
problems they may experience as a result of that work. Failure to address these problems and
related problems involving institutional practices may further traumatize clients and harm the
staff members who work with them (Bloom & Farragher, 2011).
Staff Development and Training
Weine and colleagues (2002) summarized findings from an international expert consensus panel
on training behavioral health staff members to treat clients with trauma histories. Core
components of trauma-informed training, according to this panel, involve teaching:
Competence in listening.
Ability to recognize psychosocial and mental problems to promote appropriate assessment.
Familiarity with established interventions in the client population.
The importance of understanding the local context, including help-seeking expectations,
duration of treatment, attitudes toward intervention, cost-effectiveness of intervention, and
family attitudes and involvement.
Use of problem-solving strategies that can be used on individual, family, and community
levels.
Appropriate treatment approaches for medically unexplained somatic pain.
Ability to collaborate with existing local resources and change agents (e.g., clergy, traditional
healers, informal leaders).
Counselor self-care skills.
Secondary Traumatization and Burnout
Both burnout and secondary traumatization (also known as vicarious trauma) can affect
clinicians working with clients who have trauma issues. In a review concerning secondary
traumatization and ways to prevent it, Trippany, Kress, and Wilcoxon (2004) distinguished
vicarious trauma from burnout (the former is a reaction to specific information presented by
clients and involves problems with trust, control, intrusive imagery, safety, and intimacy) and
from general countertransference reactions (observing that even though vicarious trauma may
involve countertransference, it is not inherent in or equated with countertransference). These
authors also discuss the needs commonly experienced by clinicians with vicarious trauma (needs
related to safety, trust, esteem, intimacy, and control) and some of the ways those needs may be
met by programs. A similar review was conducted by Collins and Long (2003).
Secondary trauma can lead to difficulty responding appropriately to clients’ feelings and/or cause
clinical mistakes in judgment resulting from a failure to understand what the client is trying to
express (Figley, 2002). Figley (2002) presented a model for conceptualizing secondary
1-106 Part 3, Section 1—A Review of the Literature
trauma/compassion fatigue. Mathieu and colleagues (2007) provided self-care tips for behavioral
health providers to help them reduce/overcome compassion fatigue. Elwood, Mott, Lohr, and
Galovski (2011) also reviewed this issue, but focused more on the empirical literature that
provides data on the prevalence of the problem. Research has found that the extent and severity
of secondary traumatization varies widely across studies, which the authors accounted for both
by differences in research methodology and difference in the client population involved (e.g., it
does appear that clinicians working with clients who were sexually assaulted have a greater risk
for secondary traumatization than do those who work with clients who experienced a variety of
other types of trauma).
Elwood and colleagues (2011) also observed that a few studies have found a significant
association between the percentage of clients with trauma issues whom a clinician serves and
secondary trauma symptoms for that clinician, but that a greater number of studies have found no
significant association. Some, but not all, studies have also found a significant association
between weekly hours spent working with trauma clients and clinician burnout. Also, a few
studies have found that having spent more time working with trauma clients is associated with
greater secondary traumatization symptom severity, but again, other studies have found no such
association. Additionally, some studies have found significantly higher risk for secondary
traumatization among clinicians who have personal trauma histories, whereas other studies have
not. The authors also observed that if prior trauma histories do play a significant role in what is
labeled secondary traumatization, this may mean that what is really being evaluated is
retraumatization brought on by discussions of similar traumatic experiences.
Whether factors such as counselors’ own trauma histories or hours spent with trauma clients
affect secondary traumatization may also depend on the nature of the trauma involved. For
example, a study of 114 women who specialized in treating sexual trauma did find a significant
association between their own traumatic experiences and secondary traumatization (Trippany,
Wilcoxon, & Satcher, 2003). Similarly, a study by Schauben and Frazier (1995) found that
having more clients who were victims of sexual violence was associated with increased PTSD
symptoms among a group of female counselors.
Elwood and colleagues (2011) observed that, in one study, the clinicians described secondary
traumatization symptoms that occurred after exposure to clients’ trauma stories, yet none of
those clinicians mentioned symptoms occurring 6 weeks or more after the exposure, suggesting
that long-term effects of secondary traumatization may be limited. Also, findings about the
effects of secondary traumatization on employment or performance were not clear. One group of
researchers found a significant association between secondary trauma symptoms and less
expressed intent to remain in the behavioral health field, but clinicians interviewed in other
research deny that secondary trauma symptoms affect their work performance. They concluded
that research findings concerning secondary traumatization of providers “are neither clear nor
consistent and warrant additional research” (p. 34).
Beck (2011) reviewed literature on secondary traumatization as it applies specifically to nurses,
but some of the information provided, such as how to assess secondary traumatization, is
applicable to other providers. Elwood and colleagues (2011) reviewed the instruments that have
been used in research to assess secondary traumatization. Counselor burnout is not specific to
providers working with trauma survivors, but it may affect them just as it does other counselors.
Trauma-Informed Care in Behavioral Health Services 1-107
In a review of research regarding burnout among behavioral health counselors (with a focus on
substance abuse treatment providers), Lacoursiere (2001) discussed instruments for assessing
counselor burnout and noted some factors associated with an increased likelihood of burnout:
Increased job stress/workplace pressure
A lack of clarity about rules and policies
A lack of organizational commitment to counselor goals
Worse counselor coping skills
Greater client/patient distress
Worse management/supervision
Lower professional status
A lack of intellectual stimulation
Unsatisfactory relationships with clients, client families, and other staff members
Preventing Burnout/Secondary Traumatization
Although burnout and secondary traumatization may increase counselor turnover, it is possible to
implement program policies that ameliorate the problem—for example, by providing effective
clinical supervision, because perceived quality of supervision has been associated with lower
self-ratings of emotional exhaustion and desire to leave a counseling position (Knudsen,
Ducharme, & Roman, 2006). Trippany and colleagues (2004) also concluded that good peer
supervision can help reduce the effects of secondary traumatization. Support from coworkers is
also important for reducing burnout/emotional exhaustion; generally, a cohesive and supportive
workplace will help reduce burnout (Ducharme, Knudsen, & Roman, 2008; Lent, 2010).
Research with a group of behavioral health service providers who identified themselves as
trauma specialists (N=532) determined that the use of evidence-based practices in the workplace
was associated with significantly less burnout and compassion fatigue and significantly greater
satisfaction with doing an effective job (Craig & Sprang, 2010). In addition, proper education
regarding the provision of trauma services and how treating trauma clients may affect the
clinician also appears to reduce symptoms of secondary traumatization, according to research
reviewed by Trippany, Kress, and Wilcoxon (2004). Counselors who have a stronger sense of
personal efficacy, more job autonomy, more recognition of their ideas, a stronger sense that their
programs are open to change, and a greater sense that work and rewards were fairly distributed
across the organization (i.e., greater distributive justice) also have lower burnout rates
(Ducharme, Knudsen, & Roman, 2008; Garner, Knight, & Simpson, 2007; Knudsen et al., 2006;
Shoptaw, Stein, & Rawson, 2000).
Adequate resources, including access to computers and sufficient staffing, have been associated
with lower rates of burnout/emotional exhaustion in a group of 151 substance abuse counselors
working with clients in the criminal justice system (Garner et al., 2007). Awa, Plaumann, and
Walter (2010) reviewed 25 program practices intended to reduce/prevent burnout that have been
used in a variety of workplace settings. They grouped these as person-directed (i.e., focused on
helping employees cope with workplace stress and burnout), organization-directed (i.e., focused
on changing workplace organization/practices that may affect all staff), or combined (having
features of both person-directed and organization-directed practices). They concluded that
person-directed interventions have a greater effect in the short term (a period of 6 months or less
1-108 Part 3, Section 1—A Review of the Literature
after the practice is instituted) and that combined interventions have the longest-lasting effects
(with positive effects lasting a year or more). In all cases, the positive effects of the interventions
appear to diminish over time. In addition, practices that reduce stress may also help reduce
burnout. Teaching counselors time management skills (Hawkins & Klas, 1997), cognitive
therapy techniques to address dysfunctional thought patterns (Gardner, Rose, Mason, Tyler, &
Cushway, 2005), and how to meditate (Oman, Hedberg, & Thoresen, 2006) may all reduce
stress.
References
Achim, A. M., Maziade, M., Raymond, E., Olivier, D., Merette, C., & Roy, M. A. (2011). How prevalent
are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant
association. Schizophrenia Bulletin, 37, 811–821.
Acierno, R., Brady, K., Gray, M., Kilpatrick, D. G., Resnick, H., & Best, C. L. (2002). Psychopathology
following interpersonal violence: A comparison of risk factors in older and younger adults. Journal of
Clinical Geropsychology, 8, 13–23.
Acierno, R., Kilpatrick, D. G., Resnick, H. S., Saunders, B. E., & Best, C. L. (1996). Violent assault,
posttraumatic stress disorder, and depression: Risk factors for cigarette use among adult women.
Behavior Modification, 20, 363–384.
Acierno, R., Ruggiero, K. J., Kilpatrick, D. G., Resnick, H. S., & Galea, S. (2006). Risk and protective
factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. The
American Journal of Geriatric Psychiatry, 14, 1051–1059.
Adams, P. R. & Adams, G. R. (1984). Mount Saint Helens’s ashfall: Evidence for a disaster stress
reaction. American Psychologist, 39, 252–260.
Adams, R. E. & Boscarino, J. A. (2011). A structural equation model of perievent panic and posttraumatic
stress disorder after a community disaster. Journal of Traumatic Stress, 24, 61–69.
Adler, A. B., Bliese, P. D., McGurk, D., Hoge, C. W., & Castro, C. A. (2009). Battlemind debriefing and
battlemind training as early interventions with soldiers returning from Iraq: Randomization by
platoon. Journal of Consulting and Clinical Psychology, 77, 928–940.
Afifi, T. O., Asmundson, G. J. G., Taylor, S., & Jang, K. L. (2010). The role of genes and environment on
trauma exposure and posttraumatic stress disorder symptoms: A review of twin studies. Clinical
Psychology Review, 30, 101–112.
Agaibi, C. E. & Wilson, J. P. (2005). Trauma, PTSD, and resilience: A review of the literature. Trauma,
Violence, & Abuse, 6, 195–216.
Agani, F., Landau, J., & Agani, N. (2010). Community–building before, during, and after times of trauma:
the application of the LINC model of community resilience in Kosovo. American Journal of
Orthopsychiatry, 80, 143–149.
Agorastos, A., Marmar, C. R., & Otte, C. (2011). Immediate and early behavioral interventions for the
prevention of acute and posttraumatic stress disorder. Current Opinion in Psychiatry, 24, 526–532.
Ahmed, A. S. (2007). Post-traumatic stress disorder, resilience and vulnerability. Advances in Psychiatric
Treatment, 13, 369–375.
Alarcon, L. H., Germain, A., Clontz, A. S., Roach, E., Nicholas, D. H., Zenati, M. S. et al. (2012).
Predictors of acute posttraumatic stress disorder symptoms following civilian trauma: Highest
incidence and severity of symptoms after assault. Journal of Trauma and Acute Care Surgery, 72,
629–635.
Trauma-Informed Care in Behavioral Health Services 1-109
Alcañiz, M., Lozano, J. A., & Rey, B. (2004). Technological background about VR. In G. Riva, C. Botella,
P. Legeron, & G. Optale (Eds.), Cybertherapy: Internet and virtual reality as assessment and
rehabilitation tools for clinical psychology and neuroscience. (pp. 199–216). Amsterdam: Ios Press.
Alegría, M., Canino, G., Shrout, P. E., Woo, M., Duan, N., Vila, D. et al. (2008). Prevalence of mental
illness in immigrant and non–immigrant U.S. Latino groups. American Journal of Psychiatry, 165,
359–369.
Alim, T. N., Graves, E., Mellman, T. A., Aigbogun, N., Gray, E., Lawson, W. et al. (2006). Trauma
exposure, posttraumatic stress disorder and depression in an African-American primary care
population. Journal of the National Medical Association, 98, 1630–1636.
Alonso, J., Buron, A., Bruffaerts, R., He, Y., Posada-Villa, J., Lepine, J. P. et al. (2008). Association of
perceived stigma and mood and anxiety disorders: Results from the World Mental Health Surveys.
Acta Psychiatrica Scandinavica, 118, 305–314.
American Psychiatric Association (1980). Diagnostic and statistical manual of mental disorders. (3rd ed.)
Washington, DC: American Psychiatric Association.
American Psychiatric Association (1987). Diagnostic and statistical manual of mental disorders. (3rd rev.
ed.) Washington, DC: American Psychiatric Association.
American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders. (4th ed.)
Washington, DC: American Psychiatric Association.
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders. (4th Text
Revision ed.) Washington, DC: American Psychiatric Association.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. (5th ed.)
Arlington, VA: American Psychiatric Association.
Amstadter, A. B., Acierno, R., Richardson, L. K., Kilpatrick, D. G., Gros, D. F., Gaboury, M. T. et al.
(2009). Posttyphoon prevalence of posttraumatic stress disorder, major depressive disorder, panic
disorder, and generalized anxiety disorder in a Vietnamese sample. Journal of Traumatic Stress, 22,
180–188.
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S.R., & Giles,
W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood: A
convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and
Clinical Neuroscience, 256, 174–186.
Andrews, B., Brewin, C. R., & Rose, S. (2003). Gender, social support, and PTSD in victims of violent
crime. Journal of Traumatic Stress, 16, 421–427.
Ansell, E. B., Pinto, A., Edelen, M. O., Markowitz, J. C., Sanislow, C. A., Yen, S. et al. (2011). The
association of personality disorders with the prospective 7-year course of anxiety disorders.
Psychological Medicine, 41, 1019–1028.
Antony, M. M., Orsillo, S. M., & Roemer, L. (2001). Practitioner’s guide to empirically based measures
of anxiety. New York: Kluwer Academic/Plenum Publishers.
Asmundson, G. J. & Katz, J. (2009). Understanding the co-occurrence of anxiety disorders and chronic
pain: State-of-the-art. Depression and Anxiety, 26, 888–901.
Asmundson, G. J. G., Abrams, M. P., & Collimore, K. C. (2008). Pain and anxiety disorders. In Anxiety in
health behaviors and physical illness (pp. 207–235). New York: Springer Science + Business Media.
Asnaani, A., Richey, J. A., Dimaite, R., Hinton, D. E., & Hofmann, S. G. (2010). A cross–ethnic
comparison of lifetime prevalence rates of anxiety disorders. Journal of Nervous and Mental Disease,
198, 551–555.
1-110 Part 3, Section 1—A Review of the Literature
Aspelmeier, J. E., Elliott, A. N., & Smith, C. H. (2007). Childhood sexual abuse, attachment, and trauma
symptoms in college women: The moderating role of attachment. Child Abuse & Neglect, 31, 549–
566.
Australian Centre for Posttraumatic Mental Health (2007). Australian guidelines for the treatment of adults
with acute stress disorder and posttraumatic stress disorder. Retrieved July 4, 2013, from:
http://www.acpmh.unimelb.edu.au/resources/resources-guidelines.html
Awa, W. L., Plaumann, M., & Walter, U. (2010). Burnout prevention: A review of intervention programs.
Patient Education and Counseling, 78, 184–190.
Babson, K. A. & Feldner, M. T. (2010). Temporal relations between sleep problems and both traumatic
event exposure and PTSD: A critical review of the empirical literature. Journal of Anxiety Disorders,
24, 1–15.
Back, S., Dansky, B. S., Coffey, S. F., Saladin, M. E., Sonne, S., & Brady, K. T. (2000). Cocaine
dependence with and without Posttraumatic Stress Disorder: A comparison of substance use, trauma
history and psychiatric comorbidity. American Journal on Addictions, 9, 51–62.
Bailey, H. N., DeOliveira, C. A., Wolfe, V. V., Evans, E. M., & Hartwick, C. (2012). The impact of
childhood maltreatment history on parenting: A comparison of maltreatment types and assessment
methods. Child Abuse & Neglect, 36, 236–246.
Balsam, K. F., Lehavot, K., Beadnell, B., & Circo, E. (2010). Childhood abuse and mental health
indicators among ethnically diverse lesbian, gay, and bisexual adults. Journal of Consulting and
Clinical Psychology, 78, 459–468.
Balsam, K. F., Rothblum, E. D., & Beauchaine, T. P. (2005). Victimization over the life span: A
comparison of lesbian, gay, bisexual, and heterosexual siblings. Journal of Consulting and Clinical
Psychology, 73, 477–487.
Baños, R. M., Guillen, V., Quero, S., Garcia-Palacios, A., Alcañiz, M., & Botella, C. (2011). A virtual
reality system for the treatment of stress–related disorders: A preliminary analysis of efficacy
compared to a standard cognitive behavioral program. International Journal of Human Computer
Studies, 69, 602–613.
Banyard, V. L., Williams, L. M., & Siegel, J. A. (2004). Childhood sexual abuse: A gender perspective on
context and consequences. Child Maltreatment, 9, 223–238.
Baroody, A. N. (2011). Spirituality and trauma during a time of war: A systemic approach to pastoral care
and counseling. In Families under fire: Systemic therapy with military families (pp. 165–190). New
York: Routledge/Taylor & Francis Group.
Başoğlu, M., Livanou, M., Crnobaric, C., Franciskovic, T., Suljic, E., Duric, D. et al. (2005). Psychiatric
and cognitive effects of war in former Yugoslavia: Association of lack of redress for trauma and
posttraumatic stress reactions. JAMA, 294, 580–590.
Başoğlu, M., Salcioglu, E., & Livanou, M. (2007). A randomized controlled study of single-session
behavioural treatment of earthquake-related post-traumatic stress disorder using an earthquake
simulator. Psychological Medicine, 37, 203–213.
Beals, J., Manson, S. M., Shore, J. H., Friedman, M. J., Ashcraft, M., Fairbank, J. A. et al. (2002). The
prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: Disparities and
context. Journal of Traumatic Stress, 15, 89–97.
Beals, J., Manson, S. M., Whitesell, N. R., Spicer, P., Novins, D. K., & Mitchell, C. M. (2005). Prevalence
of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations.
Archives of General Psychiatry, 62, 99–108.
Beals, J., Novins, D. K., Whitesell, N. R., Spicer, P., Mitchell, C. M., & Manson, S. M. (2005). Prevalence
of mental disorders and utilization of mental health services in two American Indian reservation
Trauma-Informed Care in Behavioral Health Services 1-111
populations: Mental health disparities in a national context. American Journal of Psychiatry, 162,
1723–1732.
Beattie, N., Shannon, C., Kavanagh, M., & Mulholland, C. (2009). Predictors of PTSD symptoms in
response to psychosis and psychiatric admission. Journal of Nervous and Mental Disease, 197, 56–
60.
Bebbington, P. E., Bhugra, D., Brugha, T., Singleton, N., Farrell, M., Jenkins, R. et al. (2004). Psychosis,
victimisation and childhood disadvantage: Evidence from the second British National Survey of
Psychiatric Morbidity. British Journal of Psychiatry, 185, 220–226.
Beck, A. J., Harrison, P. M., Berzofsky, M., Caspar, R., & Krebs, C. (2010). Sexual victimization in
prisons and jails reported by inmates, 2008–09. Washington, DC: U.S. Department of Justice, Office
of Justice Programs, Bureau of Justice Statistics.
Beck, A. T., Emery, G., & Greenberg, R. L. (2005). Anxiety disorders and phobias: A cognitive
perspective. New York: Basic Books.
Beck, C. T. (2011). Secondary traumatic stress in nurses: A systematic review. Archives of Psychiatric
Nursing, 25, 1–10.
Beck, J. G., Coffey, S. F., Foy, D. W., Keane, T. M., & Blanchard, E. B. (2009). Group cognitive behavior
therapy for chronic posttraumatic stress disorder: An initial randomized pilot study. Behav.Ther., 40,
82–92.
Beidel, D. C., Frueh, B. C., Uhde, T. W., Wong, N., & Mentrikoski, J. M. (2011). Multicomponent
behavioral treatment for chronic combat-related posttraumatic stress disorder: a randomized
controlled trial. Journal of Anxiety Disorders, 25, 224–231.
Bell, N. S., Amoroso, P. J., Yore, M. M., Smith, G. S., & Jones, B. H. (2000). Self-reported risk-taking
behaviors and hospitalization for motor vehicle injury among active duty army personnel. American
Journal of Preventive Medicine, 18, 85–95.
Benedek, D. M., Friedman, M. J., Zatzick, D., & Ursano, R. J. (2009). Guideline watch (March 2009):
Practice guideline for the treatment of patients with acute stress disorder and
posttraumatic stress disorder. FOCUS: The Journal of Lifelong Learning in Psychiatry, VII, 204–213.
Benish, S. G., Imel, Z. E., & Wampold, B. E. (2008). The relative efficacy of bona fide psychotherapies
for treating post-traumatic stress disorder: A meta-analysis of direct comparisons. Clinical
Psychology Review, 28, 746–758.
Ben-Zur, H. (2008). Personal resources of mastery–optimism, and communal support beliefs, as predictors
of posttraumatic stress in uprooted Israelis. Anxiety Stress Coping, 21, 295–307.
Berger, W., Mendlowicz, M. V., Marques-Portella, C., Kinrys, G., Fontenelle, L. F., Marmar, C. R. et al.
(2009). Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: A systematic
review. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 33, 169–180.
Bisson, J. & Andrew, M. (2007). Psychological treatment of post-traumatic stress disorder (PTSD).
Cochrane Database of Systematic Reviews, CD003388.
Bisson, J. I., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007). Psychological
treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. British
Journal of Psychiatry, 190, 97–104.
Blanchard, E. B., Buckley, T. C., Hickling, E. J., & Taylor, A. E. (1998). Posttraumatic stress disorder and
comorbid major depression: Is the correlation an illusion? Journal of Anxiety Disorders, 12, 21–37.
Bloom, S. L. & Farragher, B. (2011). Destroying sanctuary: The crisis in human service delivery systems.
New York: Oxford University Press.
Bober, T. & Regehr, C. (2006). Strategies for reducing secondary or vicarious trauma: Do they work?
Brief Treatment and Crisis Intervention, 6, 1–9.
1-112 Part 3, Section 1—A Review of the Literature
Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2007). What predicts psychological resilience
after disaster? The role of demographics, resources, and life stress. Journal of Consulting & Clinical
Psychology, 75, 671–682.
Booth, B. M., Mengeling, M., Torner, J., & Sadler, A. G. (2011). Rape, sex partnership, and substance use
consequences in women veterans. Journal of Traumatic Stress, 24, 287–294.
Bormann, J. E., Liu, L., Thorp, S. R., & Lang, A. J. (2012). Spiritual wellbeing mediates PTSD change in
veterans with military-related PTSD. International Journal of Behavioral Medicine, 19(4), 496–502.
Boscarino, J. A., Kirchner, H. L., Hoffman, S. N., Sartorius, J., Adams, R. E., & Figley, C. R. (2011). A
brief screening tool for assessing psychological trauma in clinical practice: development and
validation of the New York PTSD Risk Score. General Hospital Psychiatry, 33, 489–500.
Boscarino, J. A., Kirchner, H. L., Hoffman, S. N., Sartorius, J., Adams, R. E., & Figley, C. R. (2012a).
Predicting future PTSD using a modified New York Risk Score: Implications for patient screening
and management. Minerva Psichiatrica, 53, 47–59.
Boscarino, J. A., Kirchner, H. L., Hoffman, S. N., Sartorius, J., Adams, R. E., & Figley, C. R. (2012b).
The New York PTSD risk score for assessment of psychological trauma: Male and female versions.
Psychiatry Research, 200(2-3), 827–834.
Bosquet, E. M., Kitts, R. L., Blood, E., Bizarro, A., Hofmeister, M., & Wright, R. J. (2011). Maternal
posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behav.
Dev., 34, 487–503.
Botella, C., Quero, S., Baños, R. M., Perpina, C., Garcia Palacios, A., & Riva, G. (2004). Virtual reality
and psychotherapy. In G. Riva, C. Botella, P. Legeron, & G. Optale (Eds.), Cybertherapy: Internet
and virtual reality as assessment and rehabilitation tools for clinical psychology and neuroscience.
(pp. 37–54). Amsterdam: Ios Press.
Böttche, M., Kuwert, P., & Knaevelsrud, C. (2012). Posttraumatic stress disorder in older adults: An
overview of characteristics and treatment approaches. International Journal of Geriatric Psychiatry,
27, 230–239.
Bourque, L. B. & Shen, H. (2005). Psychometric characteristics of Spanish and English versions of the
Civilian Mississippi scale. Journal of Traumatic Stress, 18, 719–728.
Braakman, M. H., Kortmann, F. A., & van den Brink, W. (2009). Validity of ‘post-traumatic stress
disorder with secondary psychotic features’: A review of the evidence. Acta Psychiatrica
Scandinavica, 119, 15–24.
Bradley, R., Greene, J., Russ, E., Dutra, L., & Westen, D. (2005). A multidimensional meta-analysis of
psychotherapy for PTSD. American Journal of Psychiatry, 162, 214–227.
Bradley, R., Schwartz, A. C., & Kaslow, N. J. (2005). Posttraumatic stress disorder symptoms among low-
income, African American women with a history of intimate partner violence and suicidal behaviors:
Self-esteem, social support, and religious coping. Journal of Traumatic Stress, 18, 685–696.
Brady, K. T., Killeen, T. K., Brewerton, T., & Lucerini, S. (2000). Comorbidity of psychiatric disorders
and posttraumatic stress disorder. Journal of Clinical Psychiatry, 61, 22–32.
Brave Heart, M. Y. H. (1999). Gender differences in the historical trauma response among the Lakota.
Journal of Health & Social Policy, 10, 1–20.
Brave Heart, M. Y. H. (2003). The historical trauma response among natives and its relationship with
substance abuse: A Lakota illustration. Journal of Psychoactive Drugs, 35, 7–13.Brave Heart, M. Y.
H. (2004). The historical trauma response among natives and its relationship to substance abuse: A
Lakota illustration. In E. Nebelkopf & M. Phillips (Eds.), Healing and mental health for Native
Americans: Speaking in red (pp. 7–18). Walnut Creek, CA: AltaMira Press.
Trauma-Informed Care in Behavioral Health Services 1-113
Breh, D. C. & Seidler, G. H. (2007). Is peritraumatic dissociation a risk factor for PTSD? Journal of
Trauma & Dissociation, 8, 53–69.
Brenner, L. A. (2011). Neuropsychological and neuroimaging findings in traumatic brain injury and post-
traumatic stress disorder. Dialogues in Clinical Neuroscience, 13, 311–323.
Breslau, N. (2002). Gender differences in trauma and posttraumatic stress disorder. Journal of Gender
Specific Medicine, 5, 34–40.
Breslau, N., Davis, G. C., & Schultz, L. R. (2003). Posttraumatic stress disorder and the incidence of
nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of
General Psychiatry, 60, 289 –294.
Breslau, N., Lucia, V. C., & Alvarado, G. F. (2006). Intelligence and other predisposing factors in
exposure to trauma and posttraumatic stress disorder: A follow-up study at age 17 years. Archives of
General Psychiatry, 63, 1238–1245.
Breslau, N., Lucia, V. C., & Davis, G. C. (2004). Partial PTSD versus full PTSD: An empirical
examination of associated impairment. Psychological Medicine, 34, 1205–1214.
Breslau, N., Davis, C., Peterson, E. L., & Schultz, L. (2000). A second look at comorbidity in victims of
trauma: The posttraumatic stress disorder–major depression connection. Biological Psychiatry, 48,
902–909.
Brewerton, T. D. (2007). Eating disorders, trauma, and comorbidity: Focus on PTSD. Journal of Eating
Disorders, 15, 285–304.
Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic
stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–
766.
Briere, J. (2001). Detailed assessment of posttraumatic stress: Professional manual. Odessa, FL:
Psychological Assessment Resources.
Briere, J. & Scott, C. (2006). Principles of trauma therapy: A guide to symptoms, evaluation, and
treatment. Thousand Oaks, CA: Sage Publications.
Briere, J., & Scott, C. (2012). Principles of trauma therapy: A guide to symptoms, evaluation, and
treatment (2nd ed.). Thousand Oaks, CA: Sage.
Briere, J. & Spinazzola, J. (2009). Assessment of the sequelae of complex trauma: Evidence-based
measures. In C. A. Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based
guide (pp. 104–123). New York: Guilford Press.
Brooks, R., Silove, D., Bryant, R., O’Donnell, M., Creamer, M., & McFarlane, A. (2008). A confirmatory
factor analysis of the acute stress disorder interview. Journal of Traumatic Stress, 21, 352–355.
Brown, D. (2009). Assessment of attachment and abuse history, and adult attachment style. In C. A.
Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 124–144).
New York: Guilford Press.
Brown, P. J., Read, J. P., & Kahler, C. W. (2003). Comorbid posttraumatic stress disorder and substance
use disorders: Treatment outcomes and the role of coping. In P. Ouimette & P. J. Brown (Eds.),
Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders (pp. 171–
188). Washington, DC: American Psychological Association.
Brown, P. J., Stout, R. L., & Gannon-Rowley, J. (1998). Substance use disorder–PTSD comorbidity:
Patients’ perceptions of symptom interplay and treatment issues. Journal of Substance Abuse
Treatment, 15, 445–448.
Bryant, R. A. (2011). Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic
review. Journal of Clinical Psychiatry, 72, 233–239.Bryant, R. A., Creamer, M., O’Donnell, M.,
Silove, D., & McFarlane, A. C. (2011). Heart rate after trauma and the specificity of fear circuitry
1-114 Part 3, Section 1—A Review of the Literature
disorders. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 41,
2573–2580.
Bryant, R. A., Harvey, A. G., Guthrie, R. M., & Moulds, M. L. (2003). Acute psychophysiological arousal
and posttraumatic stress disorder: a two-year prospective study. Journal of Traumatic Stress, 16, 439–
443.
Bryant, R. A. & Litz, B. T. (2006). Intermediate Interventions. In E. C. Ritchie, P. J. Watson, & M. J.
Friedman (Eds.), Interventions following mass violence and disasters: Strategies for mental health
practice (pp. 155–173). New York: Guilford Press.
Bryant, R. A., Mastrodomenico, J., Felmingham, K. L., Hopwood, S., Kenny, L., Kandris, E. et al. (2008).
Treatment of acute stress disorder: A randomized controlled trial. Archives of General Psychiatry, 65,
659–667.
Bryant, R. A., Moulds, M. L., & Guthrie, R. M. (2000). Acute Stress Disorder Scale: A self-report measure
of acute stress disorder. Psychological Assessment, 12, 61–68.
Bryant, R. A., Moulds, M. L., Guthrie, R. M., Dang, S. T., Mastrodomenico, J., Nixon, R. D. et al. (2008).
A randomized controlled trial of exposure therapy and cognitive restructuring for posttraumatic stress
disorder. Journal of Consulting and Clinical Psychology, 76, 695–703.
Byers, A. L., Yaffe, K., Covinsky, K. E., Friedman, M. B., & Bruce, M. L. (2010). High occurrence of
mood and anxiety disorders among older adults: The National Comorbidity Survey Replication.
Archives of General Psychiatry, 67, 489–496.
Cahill, S. P., Foa, E. B., Hembree, E. A., Marshall, R. D., & Nacash, N. (2006). Dissemination of exposure
therapy in the treatment of posttraumatic stress disorder. Journal of Traumatic Stress, 19, 597–610.
Cahill, S. P., Rothbaum, B. O., Resick, P. A., & Follette, V. M. (2009). Cognitive–behavioral therapy for
adults. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for
PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.) (pp.
139–222). New York: Guilford Press.
Cardeña, E. & Carlson, E. (2011). Acute stress disorder revisited. Annual Review of Clinical Psychology,
7, 245–267.
Cardeña, E., Koopman, C., Classen, C., Waelde, L. C., & Spiegel, D. (2000). Psychometric properties of
the Stanford Acute Stress Reaction Questionnaire (SASRQ): a valid and reliable measure of acute
stress. Journal of Traumatic Stress, 13, 719–734.
Cardeña, E., Maldonado, J. R., van der Hart, O., & Spiegel, D. (2009). Hypnosis. In E.B.Foa, T. M. Keane,
M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines from the
International Society for Traumatic Stress Studies (2nd ed.) (pp. 427–457). New York: Guilford
Press.
Carleton, R. N., Peluso, D. L., Collimore, K. C., & Asmundson, G. J. (2011). Social anxiety and
posttraumatic stress symptoms: The impact of distressing social events. Journal of Anxiety Disorders,
25, 49–57.
Carlson, E. B., Lauderdale, S., Hawkins, J., & Sheikh, J. I. (2008). Posttraumatic stress and aggression
among veterans in long-term care. Journal of Geriatric Psychiatry and Neurology, 21, 61–71.
Carney, C. E. & Edinger, J. D. (2010). Insomnia and anxiety. New York: Springer Science + Business
Media.
Carswell, K., Blackburn, P., & Barker, C. (2011). The relationship between trauma, post-migration
problems and the psychological well-being of refugees and asylum seekers. International Journal of
Social Psychiatry, 57, 107–119.
Casteel, C., Martin, S. L., Smith, J. B., Gurka, K. K., & Kupper, L. L. (2008). National study of physical
and sexual assault among women with disabilities. Injury Prevention, 14, 87–90.
Trauma-Informed Care in Behavioral Health Services 1-115
Catalano, S. (2012). Intimate partner violence in the U.S. Washington, DC: U.S. Department of Justice,
Office of Justice Programs, Bureau of Justice Statistics.
Center for Substance Abuse Treatment (2000). Substance abuse treatment for persons with child abuse
and neglect issues HHS Publication No. (SMA) 00–3357. Rockville, MD: Substance Abuse and
Mental Health Services Administration.
Center for Substance Abuse Treatment. (2009a). Addressing suicidal thoughts and behaviors in substance
abuse treatment. Treatment Improvement Protocol (TIP) Series 50. HHS Publication No. (SMA) 09–
4381. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2009b). Substance abuse treatment: Addressing the specific needs
of women. HHS Publication No. (SMA) 09–4426. Rockville, MD: Substance Abuse and Mental
Health Services Administration.
Chen, K. W., Banducci, A. N., Guller, L., Macatee, R. J., Lavelle, A., Daughters, S. B. et al. (2011). An
examination of psychiatric comorbidities as a function of gender and substance type within an
inpatient substance use treatment program. Drug and Alcohol Dependence, 118, 92–99.
Chen, L. P., Murad, M. H., Paras, M. L., Colbenson, K. M., Sattler, A. L., Goranson, E. N. et al. (2010).
Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis.
Mayo Clinic Proceedings, 85, 618–629.
Cherpitel, C. J. (1997). Alcohol and violence-related injuries in the emergency room. Recent Developments
in Alcoholism, 13, 105–118.
Cheung, P. (1994). Posttraumatic stress disorder among Cambodian refugees in New Zealand.
International Journal of Social Psychiatry, 40, 17–26.
Chilcoat, H. D. & Breslau, N. (1998). Investigations of causal pathways between PTSD and drug use
disorders. Addictive Behaviors, 23, 827–840.
Chiu, K. B., deRoon–Cassini, T. A., & Brasel, K. J. (2011). Factors identifying risk for psychological
distress in the civilian trauma population. Academic Emergency Medicine, 18, 1156–1160.
Choi, D. C., Rothbaum, B. O., Gerardi, M., & Ressler, K. J. (2010). Pharmacological enhancement of
behavioral therapy: Focus on posttraumatic stress disorder. Current Topics in Behavioral
Neurosciences, 2, 279–299.
Clark, C. & Fearday, F. E. (2003). Triad women’s project: Group facilitator’s manual. Tampa, FL: Louis
de la Parte Florida Mental Health Institute, University of South Florida.
Classen, C. C., Palesh, O. G., & Aggarwal, R. (2005). Sexual revictimization: A review of the empirical
literature. Trauma, Violence, & Abuse, 6, 103–129.
Classen, C. C., Palesh, O. G., Cavanaugh, C., Koopman, C., Kaupp, J. W., Kraemer, H. C. et al. (2011). A
comparison of trauma-focused and present-focused group therapy for survivors of childhood sexual
abuse: A randomized controlled trial. Psychological Trauma: Theory, Research, Practice, and Policy,
3, 84–93.
Classen, C., Koopman, C., Nevill-Manning, K., & Spiegel, D. (2001). A preliminary report comparing
trauma-focused and present-focused group therapy against a wait-listed condition among childhood
sexual abuse survivors with PTSD. Journal of Aggression, Maltreatment & Trauma, 4, 265–288.
Cloitre, M. (2009). Effective psychotherapies for posttraumatic stress disorder: A review and critique. CNS
Spectrums, 14, 32–43.
Cloitre, M., Courtois, C. A., Charuvastra, A., Carapezza, R., Stolbach, B. C., & Green, B. L. (2011).
Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. Journal
of Traumatic Stress, 24(6), 615–627.
1-116 Part 3, Section 1—A Review of the Literature
Cloitre, M., Petkova, E., Wang, J., & Lu, L. F. (2012). An examination of the influence of a sequential
treatment on the course and impact of dissociation among women with PTSD related to childhood
abuse. Depression and Anxiety, 29(8), 709–717.
Cloitre, M., Stovall-McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L. et al. (2010).
Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of
Psychiatry, 167, 915–924.
Coffey, S. F., Schumacher, J. A., Brimo, M. L., & Brady, K. T. (2005). Exposure therapy for substance
abusers with PTSD: translating research to practice. Behavior Modification, 29, 10–38.
Coker, A. L., Weston, R., Creson, D. L., Justice, B., & Blakeney, P. (2005). PTSD symptoms among men
and women survivors of intimate partner violence: The role of risk and protective factors. Violence
and Victims, 20, 625–643.
Collimore, K. C., Carleton, R. N., Hofmann, S. G., & Asmundson, G. J. G. (2010). Posttraumatic stress
and social anxiety: The interaction of traumatic events and interpersonal fears. Depression and
Anxiety, 27, 1017–1026.
Collins, S. & Long, A. (2003). Too tired to care? The psychological effects of working with trauma.
Journal of Psychiatric and Mental Health Nursing, 10, 17–27.
Collishaw, S., Pickles, A., Messer, J., Rutter, M., Shearer, C., & Maughan, B. (2007). Resilience to adult
psychopathology following childhood maltreatment: Evidence from a community sample. Child
Abuse & Neglect, 31, 211–229.
Cook, A., Blaustein, M., Spinazzola, J., & van der Kolk, B. (2003). Complex trauma in children and
adolescents. White Paper from the National Child Traumatic Stress Network, Complex Trauma Task
Force. Durham, NC and Los Angeles: National Child Traumatic Stress Network.
Cook, J. M. & Niederehe, G. (2007). Trauma in older adults. In M. J. Friedman, T. M. Keane, & P. A.
Resick (Eds.), Handbook of PTSD: Science and practice (pp. 252–276). New York: Guilford Press.
Cook, J. D. & Bickman, L. (1990). Social support and psychological symptomatology following a natural
disaster. Journal of Traumatic Stress, 3, 541–556.
Corcoran, C. B., Green, B. L., Goodman, L. A., & Krinsley, K. E. (2000). Conceptual and methodological
issues in trauma history assessment. In A. Y. Shalev, R. Yehuda, & A. C. McFarlane (Eds.),
International handbook of human response to trauma (pp. 223–232). Dordrecht, Netherlands: Kluwer
Academic Publishers.
Cornelius, M. C., Nugent, N. R., Amstadter, A. B., & Koenen, K. C. (2010). Genetics of post-traumatic
stress disorder: Review and recommendations for genome-wide association studies. Current
Psychiatry Reports, 12, 313–326.
Corry, N., Pruzinsky, T., & Rumsey, N. (2009). Quality of life and psychosocial adjustment to burn injury:
Social functioning, body image, and health policy perspectives. International Review of Psychiatry,
21, 539–548.
Cottler, L. B., Compton, W. M., Mager, D., Spitznagel, E. L., & Janca, A. (1992). Posttraumatic stress
disorder among substance users from the general population. American Journal of Psychiatry, 149,
664–670.
Cougle, J. R., Feldner, M. T., Keough, M. E., Hawkins, K. A., & Fitch, K. E. (2010). Comorbid panic
attacks among individuals with posttraumatic stress disorder: associations with traumatic event
exposure history, symptoms, and impairment. Journal of Anxiety Disorders, 24, 183–188.
Cougle, J. R., Timpano, K. R., Sachs–Ericsson, N., Keough, M. E., & Riccardi, C. J. (2010). Examining
the unique relationships between anxiety disorders and childhood physical and sexual abuse in the
National Comorbidity Survey–Replication. Psychiatry Research, 177, 150–155.
Trauma-Informed Care in Behavioral Health Services 1-117
Courtois, C. A. (2000). Implications of the memory controversy for clinical practice: An overview of
treatment recommendations and guidelines. Journal of Child Sexual Abuse, 9, 183–210.
Courtois, C. A., Ford, J. D., & Cloitre, M. (2009). Best practices in psychotherapy for adults. In C. A.
Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 82–103).
New York: Guilford Press.
Covington, S. S. (2008). Helping women recover: A program for treating addiction. (Revised (Loose Leaf)
ed.) San Francisco: Jossey-Bass.
Craig, C. D. & Sprang, G. (2010). Compassion satisfaction, compassion fatigue, and burnout in a national
sample of trauma treatment therapists. Anxiety, Stress & Coping: An International Journal, 23, 319–
339.
Cubbin, C. & Smith, G. S. (2002). Socioeconomic inequalities in injury: critical issues in design and
analysis. Annual Review of Public Health, 23, 349–375.
Cukor, J., Spitalnick, J., Difede, J., Rizzo, A., & Rothbaum, B. O. (2009). Emerging treatments for PTSD.
Clinical Psychology Review, 29, 715–726.
Cusack, K. J., Frueh, B. C., & Brady, K. T. (2004). Trauma history screening in a community mental
health center. Psychiatric Services, 55, 157–162.
Danieli, Y. (2007). Assessing trauma across cultures from a multigenerational perspective. In J. P. Wilson
& C. S. Tang (Eds.), Cross-cultural assessment of psychological trauma and PTSD (pp. 65–89). New
York: Springer Science + Business Media.
Dannlowski, U., Stuhrmann, A., Beutelmann, V., Zwanzger, P., Lenzen, T., Grotegerd, D. et al. (2012).
Limbic scars: Long-term consequences of childhood maltreatment revealed by functional and
structural magnetic resonance imaging. Biological Psychiatry, 71, 286–293.
Dansky, B. S., Saladin, M. E., Brady, K. T., Kilpatrick, D. G., & Resnick, H. S. (1995). Prevalence of
victimization and posttraumatic stress disorder among women with substance use disorders:
Comparison of telephone and in-person assessment samples. International Journal of the Addictions,
30, 1079–1099.
Dass-Brailsford, P. & Myrick, A. C. (2010). Psychological trauma and substance abuse: The need for an
integrated approach. Trauma, Violence, & Abuse, 11, 202–213.
D’Augelli, A. R., Grossman, A. H., & Starks, M. T. (2006). Childhood gender atypicality, victimization,
and PTSD among lesbian, gay, and bisexual youth. Journal of Interpersonal Violence, 21, 1462–
1482.
Davidson, J. R., Hughes, D., Blazer, D. G., & George, L. K. (1991). Post-traumatic stress disorder in the
community: An epidemiological study. Psychological Medicine: A Journal of Research in Psychiatry
and the Allied Sciences, 21, 713–721.
Davidson, P. R. & Parker, K. C. (2001). Eye movement desensitization and reprocessing (EMDR): A
meta-analysis. Journal of Consulting and Clinical Psychology, 69, 305–316.
Del Gaizo, A. L., Elhai, J. D., & Weaver, T. L. (2011). Posttraumatic stress disorder, poor physical health
and substance use behaviors in a national trauma-exposed sample. Psychiatry Research, 188, 390–
395.
DeSilva M., Maclachlan, M., Devane, D., Desmond, D., Gallagher, P., Schnyder, U. et al. (2009).
Psychosocial interventions for the prevention of disability following traumatic physical injury.
Cochrane Database of Systematic Reviews, CD006422.
DeViva, J. C., Zayfert, C., Pigeon, W. R., & Mellman, T. A. (2005). Treatment of residual insomnia after
CBT for PTSD: Case studies. Journal of Traumatic Stress, 18, 155–159.
1-118 Part 3, Section 1—A Review of the Literature
Dietz, P. M., Spitz, A. M., Anda, R. F., Williamson, D. F., McMahon, P. M., Santelli, J. S. et al. (1999).
Unintended pregnancy among adult women exposed to abuse or household dysfunction during their
childhood. JAMA, 282, 1359–1364.
Difede, J., Malta, L. S., Best, S., Henn–Haase, C., Metzler, T., Bryant, R. et al. (2007). A randomized
controlled clinical treatment trial for World Trade Center attack-related PTSD in disaster workers.
Journal of Nervous and Mental Disease, 195, 861–865.
DiGrande, L., Neria, Y., Brackbill, R. M., Pulliam, P., & Galea, S. (2011). Long-term posttraumatic stress
symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World
Trade Center. American Journal of Epidemiology, 173, 271–281.
Doctor, J. N., Zoellner, L. A., & Feeny, N. C. (2011). Predictors of health-related quality-of-life utilities
among persons with posttraumatic stress disorder. Psychiatric Services, 62, 272–277.
Dohrenwend, B. P., Turner, J. B., Turse, N. A., Adams, B. G., Koenen, K. C., & Marshall, R. (2006). The
psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science, 313,
979–982.
Dohrenwend, B. P., Turner, J. B., Turse, N. A., Adams, B. G., Koenen, K. C., & Marshall, R. (2007).
Continuing controversy over the psychological risks of Vietnam for U.S. veterans. Journal of
Traumatic Stress, 20, 449–465.
Donovan, B., Padin-Rivera, E., & Kowaliw, S. (2001). Transcend: Initial outcomes from a posttraumatic
stress disorder/substance abuse treatment program. Journal of Traumatic Stress, 14, 757–772.
Dore, G., Mills, K., Murray, R., Teesson, M., & Farrugia, P. (2011). Post-traumatic stress disorder,
depression and suicidality in inpatients with substance use disorders. Drug And Alcohol Review.
Dorrepaal, E., Thomaes, K., Smit, J. H., van Balkom, A. J., Van, D. R., Veltman, D. J. et al. (2010).
Stabilizing group treatment for Complex Posttraumatic Stress Disorder related to childhood abuse
based on psycho-education and cognitive behavioral therapy: A pilot study. Child Abuse and Neglect,
34, 284–288.
Driessen, M., Schulte, S., Luedecke, C., Schaefer, I., Sutmann, F., Ohlmeier, M. et al. (2008). Trauma and
PTSD in patients with alcohol, drug, or dual dependence: A multi-center study. Alcoholism: Clinical
& Experimental Research, 32, 481–488.
Drogendijk, A. N., van der Velden, P. G., & Kleber, R. J. (2012). Acculturation and post-disaster mental
health problems among affected and non–affected immigrants: A comparative study. Journal of
Affective Disorders, 138, 485–489.
Drozdek, B. & Wilson, J. P. (2007). Wrestling with the ghosts from the past in exile: Assessing trauma in
asylum seekers. In J. P. Wilson & C. S. Tang (Eds.), Cross-cultural assessment of psychological
trauma and PTSD (pp. 113–131). New York: Springer Science + Business Media.
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001).
Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span:
Findings from the adverse childhood experiences study. JAMA: The Journal of the American Medical
Association, 286, 3089–3096.
Dube, S. R., Anda, R. F., Whitfield, C. L., Brown, D. W., Felitti, V. J., Dong, M. et al. (2005). Long-term
consequences of childhood sexual abuse by gender of victim. American Journal of Preventive
Medicine, 28, 430–438.
Ducharme, L. J., Knudsen, H. K., & Roman, P. M. (2008). Emotional exhaustion and turnover intention in
human service occupations: The protective role of coworker support. Sociological Spectrum, 28, 81–
104.
Trauma-Informed Care in Behavioral Health Services 1-119
Duffy, M., Gillespie, K., & Clark, D. M. (2007). Post-traumatic stress disorder in the context of terrorism
and other civil conflict in Northern Ireland: Randomised controlled trial. BMJ: British Medical
Journal, 334, 1147.
Dulin, P. L. & Passmore, T. (2010). Avoidance of potentially traumatic stimuli mediates the relationship
between accumulated lifetime trauma and late-life depression and anxiety. Journal of Traumatic
Stress, 23, 296–299.
Dunlavy, A. C. (2010). The impact of acculturation, trauma, and post-migration stressors on the mental
health of African immigrants and refugees in Sweden. Pittsburgh, PA: University of Pittsburgh.
Dunn, E. C., Gilman, S. E., Willett, J. B., Slopen, N. B., & Molnar, B. E. (2012). The impact of exposure
to interpersonal violence on gender differences in adolescent-onset major depression: Results from
the National Comorbidity Survey Replication (NCS–R). Depression and Anxiety.
Duran, B., Duran, E., & Brave Heart, M. Y. H. (1998). Native Americans and trauma of history. In R.
Thornton (Ed.), Studying Native America: Problems and prospects (pp. 60–76). Madison, WI:
University of Wisconsin Press.
Duran, E., Duran, B., Brave Heart, M. Y. H., & Yellow Horse-Davis, S. (1998). Healing the American
Indian soul wound. In Y. Danieli (Ed.), International handbook of multigenerational legacies of
trauma (pp. 341–354). New York: Plenum Press.
Dyer, K. F. W., Dorahy, M. J., Hamilton, G., Corry, M., Shannon, M., MacSherry, A. et al. (2009). Anger,
aggression, and self-harm in PTSD and complex PTSD. Journal of Clinical Psychology, 65, 1099–
1114.
Edwards, V. J., Anda, R. F., Felitti, V. J., & Dube, S. R. (2004). Adverse childhood experiences and
health-related quality of life as an adult. In Health consequences of abuse in the family: A clinical
guide for evidence-based practice (pp. 81–94). Washington, DC: American Psychological
Association.
Ehlers, A., Bisson, J., Clark, D. M., Creamer, M., Pilling, S., Richards, D. et al. (2010). Do all
psychological treatments really work the same in posttraumatic stress disorder? Clinical Psychology
Review, 30, 269–276.
Elbogen, E. B., Fuller, S., Johnson, S. C., Brooks, S., Kinneer, P., Calhoun, P. S. et al. (2010). Improving
risk assessment of violence among military veterans: An evidence-based approach for clinical
decision–making. Clinical Psychology Review, 30, 595–607.
Elbogen, E. B., Wagner, H. R., Fuller, S. R., Calhoun, P. S., Kinneer, P. M., & Beckham, J. C. (2010).
Correlates of anger and hostility in Iraq and Afghanistan war veterans. American Journal of
Psychiatry, 167, 1051–1058.
El-Gabalawy, R. (2012). Association between traumatic experiences and physical health conditions in a
nationally representative sample. Silver Spring, MD: Anxiety and Depression Association of
America.
Elhai, J. D., de Francisco, C. L., Miguel, F. K., Palmieri, P. A., Primi, R., & Christopher, F. B. (2011).
Testing whether posttraumatic stress disorder and major depressive disorder are similar or unique
constructs. Journal of Anxiety Disorders, 25, 404–410.
Elliott, D. E., Bjelajac, P., Fallot, R. D., Markoff, L. S., & Reed, B. G. (2005). Trauma-informed or
trauma-denied: Principles and implementation of trauma-informed services for women. Journal of
Community Psychology, 33, 461–477.
Elwood, L. S., Mott, J., Lohr, J. M., & Galovski, T. E. (2011). Secondary trauma symptoms in clinicians:
A critical review of the construct, specificity, and implications for trauma–focused treatment. Clinical
Psychology Review, 31, 25–36.
1-120 Part 3, Section 1—A Review of the Literature
Engdahl, B., Dikel, T. N., Eberly, R., & Blank, A., Jr. (1997). Posttraumatic stress disorder in a
community group of former prisoners of war: A normative response to severe trauma. American
Journal of Psychiatry, 154, 1576–1581.
Erbes, C. R. (2011). Couple functioning and PTSD in returning OIF soldiers: Preliminary findings from
the Readiness and Resilience in National Guard Soldiers Project. In Risk and resilience in U.S.
military families (pp. 47–67). New York: Springer Science + Business Media.
Evans, D. L., Foa, E. B., Gur, R. E., Herbert, H., O’Brien, C. P., Seligman, M. E. P. et al. (2005). Treating
and preventing adolescent mental health disorders: What we know and what we don’t know: A
research agenda for improving the mental health of our youth. New York: Oxford University Press.
Evans-Campbell, T. (2008). Historical trauma in American Indian/Native Alaska communities: A
multilevel framework for exploring impacts on individuals, families, and communities. Journal of
Interpersonal Violence, 23, 316–338.
Everly, G. S., Jr., Phillips, S. B., Kane, D., & Feldman, D. (2006). Introduction to and overview of group
psychological first aid. Brief Treatment and Crisis Intervention, 6, 130–136.
Evren, C., Dalbudak, E., Cetin, R., Durkaya, M., & Evren, B. (2010). Relationship of alexithymia and
temperament and character dimensions with lifetime post-traumatic stress disorder in male alcohol-
dependent inpatients. Psychiatry and Clinical Neurosciences, 64, 111–119.
Evren, C., Sar, V., Dalbudak, E., Cetin, R., Durkaya, M., Evren, B. et al. (2011). Lifetime PTSD and
quality of life among alcohol-dependent men: Impact of childhood emotional abuse and dissociation.
Psychiatry Research, 186, 85–90.
Fallot, R. D. & Harris, M. (2001). A trauma-informed approach to screening and assessment. In M. Harris
& R. D. Fallot (Eds.), Using trauma theory to design service systems (pp. 23–31). San Francisco:
Jossey-Bass.
Fallot, R. D. & Harris, M. (2002). The Trauma Recovery and Empowerment Model (TREM): Conceptual
and practical issues in a group intervention for women. Community Mental Health Journal, 38, 475–
485.
Falsetti, S. A., Resick, P. A., & Davis, J. L. (2003). Changes in religious beliefs following trauma. Journal
of Traumatic Stress, 16, 391–398.
Falsetti, S. A., Resnick, H. S., & Davis, J. L. (2008). Multiple channel exposure therapy for women with
PTSD and comorbid panic attacks. Cognitive Behaviour Therapy, 37, 117–130.
Farley, M., Golding, J. M., Young, G., Mulligan, M., & Minkoff, J. R. (2004). Trauma history and relapse
probability among patients seeking substance abuse treatment. Journal of Substance Abuse
Treatment, 27, 161–167.
Feldner, M. T., Babson, K. A., & Zvolensky, M. J. (2007). Smoking, traumatic event exposure, and post-
traumatic stress: A critical review of the empirical literature. Clinical Psychology Review, 27, 14–45.
Felitti, V. J. (2002). The relation between adverse childhood experiences and adult health: Turning gold
into lead. The Permanente Journal, 6, 44–47.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V. et al. (1998).
Relationship of childhood abuse and household dysfunction to many of the leading causes of death in
adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine,
14, 245–258.
Felmingham, K. L. & Bryant, R. A. (2012). Gender differences in the maintenance of response to
cognitive behavior therapy for posttraumatic stress disorder. Journal of Consulting and Clinical
Psychology, 80, 196–200.
Trauma-Informed Care in Behavioral Health Services 1-121
Fetzner, M. G., McMillan, K. A., Sareen, J., & Asmundson, G. J. (2011). What is the association between
traumatic life events and alcohol abuse/dependence in people with and without PTSD? Findings from
a nationally representative sample. Depression and Anxiety, 28, 632–638.
Figley, C. R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical
Psychology, 58, 1433–1441.
Finkelhor, D., Ormrod, R., Turner, H., & Hamby, S. L. (2005). The victimization of children and youth: a
comprehensive, national survey. Child Maltreatment, 10, 5–25.
Fisher, J. & Ogden, P. (2009). Sensorimotor psychotherapy. In C. A. Courtois (Ed.), Treating complex
traumatic stress disorders: An evidence-based guide (pp. 312–328). New York: Guilford Press.
Fisher, M. H., Hodapp, R. M., & Dykens, E. M. (2008). Child abuse among children with disabilities:
What we know and what we need to know. In M. G. Laraine (Ed.), International Review of Research
in Mental Retardation (Volume 35 ed., pp. 251–289). Academic Press.
Fletcher, S., Creamer, M., & Forbes, D. (2010). Preventing post traumatic stress disorder: Are drugs the
answer? Australian and New Zealand Journal of Psychiatry, 44, 1064–1071.
Foa, E. B. & International Society For Traumatic Stress Studies (2009). Effective treatments for PTSD:
Practice guidelines from the International Society for Traumatic Stress Studies. (2nd ed ed.) New
York: Guilford Press.
Foa, E. B. & Rothbaum, B. O. (1998). Treating the trauma of rape: Cognitive–behavioral therapy for
PTSD. New York: Guilford Press.
Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional
processing of traumatic experiences: Therapist guide. Oxford University Press: New York.
Foa, E. B., Hembree, E. A., Cahill, S. P., Rauch, S. A., Riggs, D. S., Feeny, N. C. et al. (2005).
Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive
restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical
Psychology, 73, 953–964.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (2009). Introduction. In E. B. Foa, T. M. Keane,
M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines from the
International Society for Traumatic Stress Studies (2nd ed.) (pp. 1–20). New York: Guilford Press.
Foa, E. B., Rothbaum, B. O., & Furr, J. M. (2003). Augmenting exposure therapy with other CBT
procedures. Psychiatric Annals, 33, 47–53.
Foa, E. B., Zoellner, L. A., & Feeny, N. C. (2006). An evaluation of three brief programs for facilitating
recovery after assault. Journal of Traumatic Stress, 19, 29–43.
Focht-New, G., Barol, B., Clements, P. T., & Milliken, T. F. (2008). Persons with developmental disability
exposed to interpersonal violence and crime: Approaches for intervention. Perspectives in Psychiatric
Care, 44, 89–98.
Follette, V. M., Iverson, K. M., & Ford, J. D. (2009). Contextual behavior trauma therapy. In C. A.
Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 264–285).
New York: Guilford Press.
Fontana, A. & Rosenheck, R. (2004). Trauma, change in strength of religious faith, and mental health
service use among veterans treated for PTSD. Journal of Nervous and Mental Disease, 192, 579–584.
Fontana, A. & Rosenheck, R. (2006). Treatment of female veterans with posttraumatic stress disorder: The
role of comfort in a predominantly male environment. Psychiatric Quarterly, 77, 55–67.
Ford, J. D. (2009). Neurobiological and developmental research: Clinical implications. In Treating
complex traumatic stress disorders: An evidence-based guide (pp. 31–58). New York: Guilford Press.
1-122 Part 3, Section 1—A Review of the Literature
Ford, J. D. & Russo, E. (2006). Trauma-focused, present-centered, emotional self-regulation approach to
integrated treatment for posttraumatic stress and addiction: Trauma Adapative Recovery Group
Education and Therapy (TARGET). American Journal of Psychotherapy, 60, 335–355.
Ford, J. D. & Saltzman, W. (2009). Family systems therapy. In C. A. Courtois & J. D. Ford (Eds.),
Treating complex traumatic stress disorders: An evidence-based guide (pp. 391–414). New York:
Guilford Press.
Ford, J. D., Fallot, R. D., & Harris, M. (2009). Group therapy. In C. A. Courtois & J. D. Ford (Eds.),
Treating complex traumatic stress disorders: An evidence-based guide (pp. 415–440). New York:
Guilford Press.
Fortuna, L. R., Porche, M. V., & Alegría, M. (2008). Political violence, psychosocial trauma, and the
context of mental health services use among immigrant Latinos in the United States. Ethnicity and
Health, 13, 435–463.
Fortuna, L. R., Porche, M. V., & Alegría, M. (2009). A qualitative study of clinicians’ use of the cultural
formulation model in assessing posttraumatic stress disorder. Transcult.Psychiatry, 46, 429–450.
Fosha, D., Paivio, S. C., Gleiser, K., & Ford, J. D. (2009). Experiential and emotion–focused therapy. In C.
A. Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 286–
311). New York: Guilford Press.
Fredman, S. J., Monson, C. M., & Adair, K. C. (2011). Implementing cognitive–behavioral conjoint
therapy for PTSD with the newest generation of veterans and their partners. Cognitive and Behavioral
Practice, 18, 120–130.
Frencher, S. K., Jr., Benedicto, C. M., Kendig, T. D., Herman, D., Barlow, B., & Pressley, J. C. (2010). A
comparative analysis of serious injury and illness among homeless and housed low income residents
of New York City. Journal of Trauma, 69, S191–S199.
Friedman, M. J. & Davidson, J. R. T. (2007). Pharmacotherapy for PTSD. In M. J. Friedman, T. M. Keane,
& P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 376–405). New York: Guilford
Press.
Friedman, M. J., Marmar, C. R., Baker, D. G., Sikes, C. R., & Farfel, G. M. (2007). Randomized, double-
blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of
Veterans Affairs setting. Journal of Clinical Psychiatry, 68, 711–720.
Frisman, L., Ford, J., Lin, H. J., Mallon, S., & Chang, R. (2008). Outcomes of trauma treatment using the
TARGET model. Journal of Groups in Addiction and Recovery, 3, 285–303.
Fullerton, C. S., Ursano, R. J., Epstein, R. S., Crowley, B., Vance, K., Kao, T. C. et al. (2001). Gender
differences in posttraumatic stress disorder after motor vehicle accidents. American Journal of
Psychiatry, 158, 1486–1491.
Galea, S., Ahern, J., Tracy, M., Hubbard, A., Cerda, M., Goldmann, E. et al. (2008). Longitudinal
determinants of posttraumatic stress in a population-based cohort study. Epidemiology, 19, 47–54.
Galea, S., Vlahov, D., Tracy, M., Hoover, D. R., Resnick, H. S., & Kilpatrick, D. G. (2004). Hispanic
ethnicity and post-traumatic stress disorder after a disaster: evidence from a general population survey
after September 11, 2001. Annals of Epidemiology, 14, 520–531.
Galovski, T. & Lyons, J. A. (2004). Psychological sequelae of combat violence: A review of the impact of
PTSD on the veteran’s family and possible interventions. Aggression and Violent Behavior, 9, 477–
501.
Gapen, M., Cross, D., Ortigo, K., Graham, A., Johnson, E., Evces, M. et al. (2011). Perceived
neighborhood disorder, community cohesion, and PTSD symptoms among low-income African
Americans in an urban health setting. American Journal of Orthopsychiatry, 81, 31–37.
Trauma-Informed Care in Behavioral Health Services 1-123
Gardner, B., Rose, J., Mason, O., Tyler, P., & Cushway, D. (2005). Cognitive therapy and behavioural
coping in the management of work–related stress: An intervention study. Work & Stress, 19, 137–
152.
Garfinkel, S. N. & Liverzon, I. (2009). Neurobiology of PTSD: A review of neuroimaging. Psychiatric
Annals, 39, 370–381.
Garner, B. R., Knight, K., & Simpson, D. D. (2007). Burnout among corrections-based drug treatment
staff: Impact of individual and organizational factors. International Journal of Offender Therapy and
Comparative Criminology, 51, 510–522.
Garno, J. L., Goldberg, J. F., Ramirez, P. M., & Ritzler, B. A. (2005). Impact of childhood abuse on the
clinical course of bipolar disorder. British Journal of Psychiatry, 186, 121–125.
Gellis, L. A., Mavandadi, S., & Oslin, D. W. (2010). Functional quality of life in full versus partial
posttraumatic stress disorder among veterans returning from Iraq and Afghanistan. Primary Care
Companion Journal of Clinical Psychiatry, 12.
Geraerts, E., Lindsay, D. S., Merckelbach, H., Jelicic, M., Raymaekers, L., Arnold, M. M. et al. (2009).
Cognitive mechanisms underlying recovered-memory experiences of childhood sexual abuse.
Psychological Science, 20, 92–98.
Geraerts, E., Schooler, J. W., Merckelbach, H., Jelicic, M., Hauer, B. J., & Ambadar, Z. (2007). The reality
of recovered memories: Corroborating continuous and discontinuous memories of childhood sexual
abuse. Psychological Science, 18, 564–568.
Gerardi, M., Cukor, J., Difede, J., Rizzo, A., & Rothbaum, B. O. (2010). Virtual reality exposure therapy
for post-traumatic stress disorder and other anxiety disorders. Current Psychiatry Reports, 12, 298–
305.
Gewirtz, A. H., Polusny, M. A., DeGarmo, D. S., Khaylis, A., & Erbes, C. R. (2010). Posttraumatic stress
symptoms among National Guard Soldiers deployed to Iraq: Associations with parenting behaviors
and couple adjustment. Journal of Consulting and Clinical Psychology, 78, 599–610.
Gilbert, R., Widom, C. S., Browne, K., Fergusson, D., Webb, E., & Janson, S. (2009). Burden and
consequences of child maltreatment in high-income countries. Lancet, 373, 68–81.
Gillespie, C. F., Bradley, B., Mercer, K., Smith, A. K., Conneely, K., Gapen, M. et al. (2009). Trauma
exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry,
31, 505–514.
Ginzburg, K., Solomon, Z., & Bleich, A. (2002). Repressive coping style, acute stress disorder, and
posttraumatic stress disorder after myocardial infarction. Psychosomatic Medicine, 64, 748–757.
Gold, S. D., Marx, B. P., Soler-Baillo, J. M., & Sloan, D. M. (2005). Is life stress more traumatic than
traumatic stress? Journal of Anxiety Disorders., 19, 687–698.
Gold, S. N. (2009). Contextual therapy. In C. A. Courtois & J. D. Ford (Eds.), Treating complex traumatic
stress disorders: An evidence-based guide (pp. 227–242). New York: Guilford Press.
Goldberg, J. F. & Garno, J. L. (2005). Development of posttraumatic stress disorder in adult bipolar
patients with histories of severe childhood abuse. Journal of Psychiatric Research, 39, 595–601.
Goldmann, E., Aiello, A., Uddin, M., Delva, J., Koenen, K., Gant, L. M. et al. (2011). Pervasive exposure
to violence and posttraumatic stress disorder in a predominantly African American Urban
Community: The Detroit neighborhood health study. Journal of Traumatic Stress, 24(6), 747–751.
Goldstein, R. B., Compton, W. M., & Grant, B. F. (2010). Antisocial behavioral syndromes and additional
psychiatric comorbidity in posttraumatic stress disorder among U.S. adults: Results from wave 2 of
the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of the American
Psychiatric Nurses Association, 16, 145–165.
1-124 Part 3, Section 1—A Review of the Literature
Gonzalez, P. & Gonzalez, G. M. (2008). Acculturation, optimism, and relatively fewer depression
symptoms among Mexican immigrants and Mexican Americans. Psychological Reports, 103, 566–
576.
Goodman, G. S., Ghetti, S., Quas, J. A., Edelstein, R. S., Alexander, K. W., Redlich, A. D. et al. (2003). A
prospective study of memory for child sexual abuse: New findings relevant to the repressed-memory
controversy. Psychological Science, 14, 113–118.
Goodson, J., Helstrom, A., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Powers, M. B. (2011). The
treatment of posttraumatic stress disorder in U.S. combat veterans: A meta-analytic review.
Psychological Reports, 109, 573–599.
Govindshenoy, M. & Spencer, N. (2007). Abuse of the disabled child: A systematic review of population-
based studies. Child: Care, Health and Development, 33, 552–558.
Grammer, G. G. & Moran, S. C. (2011). Geriatrics. In D. M. Benedek (Ed.), Clinical manual for
management of PTSD (pp. 371–381). Arlington, VA: American Psychiatric Publishing, Inc.
Grant, B. F., Chou, S. P., Goldstein, R. B., Huang, B., Stinson, F. S., Saha, T. D. et al. (2008). Prevalence,
correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the
Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical
Psychiatry., 69, 533–545.
Grant, B. F., Stinson, F. S., Hasin, D. S., Dawson, D. A., Chou, S. P., & Anderson, K. (2004). Immigration
and lifetime prevalence of DSM-IV Psychiatric disorders among Mexican Americans and non-
Hispanic whites in the United States: Results from the National Epidemiologic Survey on Alcohol
and Related Conditions. Archives of General Psychiatry, 61, 1226–1233.
Gratz, K. L. & Tull, M. T. (2010). The relationship between emotion dysregulation and deliberate self-
harm among inpatients with substance use disorders. Cognitive Therapy and Research, 34, 544–553.
Green, B. L., Krupnick, J. L., Chung, J., Siddique, J., Krause, E. D., Revicki, D. et al. (2006). Impact of
PTSD comorbidity on one-year outcomes in a depression trial. Journal of Clinical Psychology, 62,
815–835.
Green, J. G., McLaughlin, K. A., Berglund, P. A., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M. et al.
(2010). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey
Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67,
113–123.
Greenberg, G. A. & Rosenheck, R. A. (2010). Mental health correlates of past homelessness in the
National Comorbidity Study Replication. Journal of Health Care for the Poor and Underserved, 21,
1234–1249.
Grieger, T. A., Cozza, S. J., Ursano, R. J., Hoge, C., Martinez, P. E., Engel, C. C. et al. (2006).
Posttraumatic stress disorder and depression in battle-injured soldiers. American Journal of
Psychiatry, 163, 1777–1783.
Gros, D. F., Frueh, B. C., & Magruder, K. M. (2011). Prevalence and features of panic disorder and
comparison to posttraumatic stress disorder in VA primary care. General Hospital Psychiatry, 33,
482–488.
Guay, S., Billette, V., & Marchand, A. (2006). Exploring the links between posttraumatic stress disorder
and social support: Processes and potential research avenues. Journal of Traumatic Stress, 19, 327–
338.
Hamblen, J. L., Gibson, L. E., Mueser, K. T., & Norris, F. H. (2006). Cognitive behavioral therapy for
prolonged postdisaster distress. Journal of Clinical Psychology, 62, 1043–1052.
Trauma-Informed Care in Behavioral Health Services 1-125
Hamblen, J. L., Norris, F. H., Pietruszkiewicz, S., Gibson, L. E., Naturale, A., & Louis, C. (2009).
Cognitive behavioral therapy for postdisaster distress: A community based treatment program for
survivors of Hurricane Katrina. Administration and Policy in Mental Health, 36, 206–214.
Hankin, C. S., Skinner, K. M., Sullivan, L. M., Miller, D. R., Frayne, S., & Tripp, T. J. (1999). Prevalence
of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing
sexual assault while in the military. Journal of Traumatic Stress, 12, 601–612.
Hanson, R. F. & Self-Brown, S. (2010). Screening and assessment of crime victimization and its effects.
Journal of Traumatic Stress, 23, 207–214.
Harned, M. S., Korslund, K. E., Foa, E. B., & Linehan, M. M. (2012). Treating PTSD in suicidal and self-
injuring women with borderline personality disorder: Development and preliminary evaluation of a
Dialectical Behavior Therapy Prolonged Exposure Protocol. Behaviour Research and Therapy, 50,
381–386.
Harper, K., Richter, N. L., & Gorey, K. M. (2009). Group work with female survivors of childhood sexual
abuse: Evidence of poorer outcomes among those with eating disorders. Eating Behaviors, 10, 45–48.
Harris, J. I., Erbes, C. R., Engdahl, B. E., Thuras, P., Murray-Swank, N., Grace, D. et al. (2011). The
effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma.
Journal of Clinical Psychology, 67, 425–438.
Harris, M. & Fallot, R. D. (2001). Trauma-informed inpatient services. In M. Harris & R. D. Fallot (Eds.),
Using trauma theory to design service systems (pp. 33–46). San Francisco: Jossey-Bass.
Harvard School of Medicine (2007). NCS–R lifetime prevalence estimates: Table 1. Lifetime prevalence of
DSM-IV/WMH-CIDI disorders by sex and cohort 1 (n=9282). National Comorbidity Survey (NCS)
and National Comorbidity Survey Replication (NCS–R). Cambridge, MA: Harvard University Press.
Harvard School of Medicine (2007). NCS–R Twelve-month prevalence estimates: Table 2. 12–month
prevalence of DSM-IV/WMH-CIDI disorders by sex and cohort 1 (n=9282). National Comorbidity
Survey (NCS) and National Comorbidity Survey Replication (NCS–R). Cambridge, MA: Harvard
University Press.
Haskell, S. G., Mattocks, K., Goulet, J. L., Krebs, E. E., Skanderson, M., Leslie, D. et al. (2011). The
burden of illness in the first year home: Do male and female VA users differ in health conditions and
healthcare utilization. Women’s Health Issues, 21, 92–97.
Hawkins, F. & Klas, L. (1997). Time management as a stressor for helping professionals: Implications for
employment. Journal of Employment Counseling, 34, 2–6.
Hembree, E. A. & Foa, E. B. (2000). Posttraumatic stress disorder: Psychological factors and psychosocial
interventions. Journal of Clinical Psychiatry, 61, 33–39.
Hembree, E. A., Foa, E. B., Dorfan, N. M., Street, G. P., Kowalski, J., & Tu, X. (2003). Do patients drop
out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress, 16, 555–562.
Herek, G. M. (2009). Hate crimes and stigma-related experiences among sexual minority adults in the
United States: prevalence estimates from a national probability sample. Journal of Interpersonal
Violence, 24, 54–74.
Herman, D. B., Susser, E. S., Struening, E. L., & Link, B. L. (1997). Adverse childhood experiences: Are
they risk factors for adult homelessness? American Journal of Public Health, 87, 249–255.
Herman, J. L. (1992). Trauma and recovery. New York: Basic Books.
Herman, J. L. (1997). Trauma and recovery. (Rev. ed.) New York: Basic Books.
Hetrick, S. E., Purcell, R., Garner, B., & Parslow, R. (2010). Combined pharmacotherapy and
psychological therapies for post traumatic stress disorder (PTSD). Cochrane Database of Systematic
Reviews, CD007316.
1-126 Part 3, Section 1—A Review of the Literature
Hien, D. A., Campbell, A. N. C., Ruglass, L. M., Hu, M. C., & Killeen, T. (2010). The role of alcohol
misuse in PTSD outcomes for women in community treatment: A secondary analysis of NIDA’s
Women and Trauma Study. Drug and Alcohol Dependence, 111, 114–119.
Hill, J. J., III, Mobo, B. H., Jr., & Cullen, M. R. (2009). Separating deployment-related traumatic brain
injury and posttraumatic stress disorder in veterans: Preliminary findings from the Veterans Affairs
traumatic brain injury screening program. American Journal of Physical Medicine and Rehabilitation,
88, 605–614.
Hillis, S. D., Anda, R. F., Felitti, V. J., Nordenberg, D., & Marchbanks, P. A. (2000). Adverse childhood
experiences and sexually transmitted diseases in men and women: A retrospective study. Pediatrics,
106, E11.
Himmelfarb, N., Yaeger, D., & Mintz, J. (2006). Posttraumatic stress disorder in female veterans with
military and civilian sexual trauma. Journal of Traumatic Stress, 19, 837–846.
Hinton, D., Ba, P., Peou, S., & Um, K. (2000). Panic disorder among Cambodian refugees attending a
psychiatric clinic. Prevalence and subtypes. General Hospital Psychiatry, 22, 437–444.
Hinton, D., Chau, H., Nguyen, L., Nguyen, M., Pham, T., Quinn, S. et al. (2001). Panic disorder among
Vietnamese refugees attending a psychiatric clinic: prevalence and subtypes. General Hospital
Psychiatry, 23, 337–344
Hinton, D. E., Chhean, D., Pich, V., Safren, S. A., Hofmann, S. G., & Pollack, M. H. (2005). A
randomized controlled trial of cognitive–behavior therapy for Cambodian refugees with treatment–
resistant PTSD and panic attacks: A cross-over design. Journal of Traumatic Stress, 18, 617–629.
Hinton, D. E., Hinton, A. L., Pich, V., Loeum, J. R., & Pollack, M. H. (2009). Nightmares among
Cambodian refugees: The breaching of concentric ontological security. Culture, Medicine and
Psychiatry, 33, 219–265.
Hinton, D. E., Hofmann, S. G., Pollack, M. H., & Otto, M. W. (2009). Mechanisms of efficacy of CBT for
Cambodian refugees with PTSD: Improvement in emotion regulation and orthostatic blood pressure
response. CNS Neuroscience & Therapeutics, 15, 255–263.
Hinton, D. E., Hofmann, S. G., Rivera, E., Otto, M. W., & Pollack, M. H. (2011). Culturally adapted CBT
(CA–CBT) for Latino women with treatment–resistant PTSD: A pilot study comparing CA–CBT to
applied muscle relaxation. Behaviour Research and Therapy, 49, 275–280.
Hinton, D. E., Kredlow, M. A., Bui, E., Pollack, M. H., & Hofmann, S. G. (2012). Treatment change of
somatic symptoms and cultural syndromes among Cambodian refugees with PTSD. Depression and
Anxiety, 29, 148–155.
Hinton, D. E., Nickerson, A., & Bryant, R. A. (2011). Worry, worry attacks, and PTSD among Cambodian
refugees:A path analysis investigation. Social Science and Medicine, 72, 1817–1825.
Hinton, D. E., Park, L., Hsia, C., Hofmann, S., & Pollack, M. H. (2009). Anxiety disorder presentations in
Asian populations: A review. CNS Neuroscience & Therapeutics, 15, 295–303.
Hinton, D. E., Pham, T., Tran, M., Safren, S. A., Otto, M. W., & Pollack, M. H. (2004). CBT for
Vietnamese refugees with treatment-resistant PTSD and panic attacks: A pilot study. Journal of
Traumatic Stress, 17, 429–433.
Hinton, D. E., Pich, V., Marques, L., Nickerson, A., & Pollack, M. H. (2010). Khyal attacks: A key idiom
of distress among traumatized Cambodia refugees. Culture, Medicine and Psychiatry, 34, 244–278.
Hinton, D. E., Rivera, E. I., Hofmann, S. G., Barlow, D. H., & Otto, M. W. (2012). Adapting CBT for
traumatized refugees and ethnic minority patients: Examples from culturally adapted CBT (CA–
CBT). Transcultural Psychiatry, 49, 340–365.Hiskey, S., Luckie, M., Davies, S., & Brewin, C. R.
(2008). The emergence of posttraumatic distress in later life: a review. Journal of Geriatric
Psychiatry and Neurology, 21, 232–241.
Trauma-Informed Care in Behavioral Health Services 1-127
Hobfoll, S. E., Canetti-Nisim, D., Johnson, R. J., Palmieri, P. A., Varley, J. D., & Galea, S. (2008). The
association of exposure, risk, and resiliency factors with PTSD among Jews and Arabs exposed to
repeated acts of terrorism in Israel. Journal of Traumatic Stress, 21, 9–21.
Hobfoll, S. E., Watson, P., Bell, C. C., Bryant, R. A., Brymer, M. J., Friedman, M. J. et al. (2007). Five
essential elements of immediate and mid–term mass trauma intervention: empirical evidence.
Psychiatry, 70, 283–315.
Hofmann, S. G. & Smits, J. A. (2008). Cognitive–behavioral therapy for adult anxiety disorders: a meta-
analysis of randomized placebo-controlled trials. Journal of Clinical Psychiatry, 69, 621–632.
Hoge, C. W. (2011). Public health strategies and treatment of service members and veterans with combat-
related mental health problems. In A. B. Adler, P. D. Bliese, & C. A. Castro (Eds.), Deployment
psychology: Evidence-based strategies to promote mental health in the military (pp. 17–34).
Washington, DC, US: American Psychological Association.
Hoge, C. W., Terhakopian, A., Castro, C. A., Messer, S. C., & Engel, C. C. (2007). Association of
posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq
War veterans. The American Journal of Psychiatry, 164, 150–153.
Holbrook, T. L., Hoyt, D. B., Stein, M. B., & Sieber, W. J. (2001). Perceived threat to life predicts
posttraumatic stress disorder after major trauma: Risk factors and functional outcome. Journal of
Trauma, 51, 287–292.
Holbrook, T. L., Hoyt, D. B., Stein, M. B., & Sieber, W. J. (2002). Gender differences in long-term
posttraumatic stress disorder outcomes after major trauma: Women are at higher risk of adverse
outcomes than men. Journal of Trauma, 53, 882–888.
Hollifield, M. (2011). Acupuncture for posttraumatic stress disorder: Conceptual, clinical, and biological
data support further research. CNS Neuroscience & Therapeutics, 17, 769–779.
Hopper, E. K., Bassuk, E. L., & Olivet, J. (2010). Shelter from the storm: Trauma-informed care in
homelessness services settings. The Open Health Services and Policy Journal, 3, 80–100.
Horowitz, M. J. (1989). Posttraumatic Stress Disorder. In American Psychiatric Association Task Force on
Treatments of Psychiatric Disorders (Ed.), Treatments of psychiatric disorders: A task force report of
the American Psychiatric Association. (pp. 2065–2082). Washington, DC: American Psychiatric
Association.
Hoshmand, L. T. (2007). Cultural–ecological perspectives on the understanding and assessment of trauma.
In Cross-cultural assessment of psychological trauma and PTSD (pp. 31–50). New York: Springer
Science + Business Media.
Huang, M. C., Schwandt, M. L., Ramchandani, V. A., George, D. T., & Heilig, M. (2012). Impact of
multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic
inpatients. Alcoholism, Clinical and Experimental Research, 36(6), 1099–1107.
Hughes, K. C. & Shin, L. M. (2011). Functional neuroimaging studies of post-traumatic stress disorder.
Expert Review of Neurotherapeutics, 11, 275–285.
Hussain, A., Weisaeth, L., & Heir, T. (2011). Changes in religious beliefs and the relation of religiosity to
posttraumatic stress and life satisfaction after a natural disaster. Social Psychiatry and Psychiatric
Epidemiology, 46, 1027–1032.
Ilgen, M. A., Bohnert, A. S., Ignacio, R. V., McCarthy, J. F., Valenstein, M. M., Kim, H. M. et al. (2010).
Psychiatric diagnoses and risk of suicide in veterans. Archives of General Psychiatry, 67, 1152–1158.
Institute of Medicine (2008). Treatment of posttraumatic stress disorder: An assessment of the evidence.
Washington, DC: Institute of Medicine.
Ipser, J. C. & Stein, D. J. (2012). Evidence-based pharmacotherapy of post-traumatic stress disorder
(PTSD). The International Journal of Neuropharmacology, 15, 825–840.
1-128 Part 3, Section 1—A Review of the Literature
Jackson, C., Nissenson, K., & Cloitre, M. (2010). Treatment for complex PTSD. In D. Sookman (Ed.),
Treatment resistant anxiety disorders: Resolving impasses to symptom remission (pp. 75–104). New
York: Routledge/Taylor & Francis Group.
Jainchill, N., Hawke, J., & Yagelka, J. (2000). Gender, psychopathology, and patterns of homelessness
among clients in shelter-based TCs. American Journal of Drug and Alcohol Abuse, 26, 553–567.
Janssen, I., Krabbendam, L., Bak, M., Hanssen, M., Vollebergh, W., de, G. R. et al. (2004). Childhood
abuse as a risk factor for psychotic experiences. Acta Psychiatrica Scandinavica, 109, 38–45.
Jaycox, L. H., Zoellner, L., & Foa, E. B. (2002). Cognitive–behavior therapy for PTSD in rape survivors.
Journal of Clinical Psychology, 58, 891–906.
Joe, S., Baser, R. E., Breeden, G. K., Neighbors, H. W., & Jackson, J. S. (2006). Prevalence of and risk
factors for lifetime suicide attempts among blacks in the United States. JAMA, 296, 2112–2123.
Johnson, D. M., Palmieri, P. A., Jackson, A. P., & Hobfoll, S. E. (2007). Emotional numbing weakens
abused inner-city women’s resiliency resources. Journal of Traumatic Stress, 20, 197–206.
Johnson, D. M., Zlotnick, C., & Perez, S. (2011). Cognitive behavioral treatment of PTSD in residents of
battered women’s shelters: Results of a randomized clinical trial. Journal of Consulting and Clinical
Psychology, 79, 542–551.
Johnson, D. R., Lahad, M., & Gray, A. (2009). Creative therapies for adults. In E. B. Foa, T. M. Keane, M.
J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines from the
International Society for Traumatic Stress Studies (2nd ed.) (pp. 479–490). New York: Guilford
Press.
Johnson, H. & Thompson, A. (2008). The development and maintenance of post-traumatic stress disorder
(PTSD) in civilian adult survivors of war trauma and torture: A review. Clinical Psychology Review,
28, 36–47.
Johnson, H., Thompson, A., & Downs, M. (2009). Non–Western interpreters’ experiences of trauma: The
protective role of culture following exposure to oppression. Ethnicity and Health, 14, 407–418.
Johnson, S. D. (2008). Substance use, post-traumatic stress disorder and violence. Current Opinion in
Psychiatry, 21, 242–246.
Johnson, S. D., Striley, C., & Cottler, L. B. (2006). The association of substance use disorders with trauma
exposure and PTSD among African American drug users. Addictive Behaviors, 31, 2063–2073.
Johnson, S. M. & Courtois, C. A. (2009). Couple therapy. In C. A. Courtois & J. D. Ford (Eds.), Treating
complex traumatic stress disorders: An evidence-based guide (pp. 371–390). New York: Guilford
Press.
Jones, B. H. & Knapik, J. J. (1999). Physical training and exercise–related injuries. Surveillance, research
and injury prevention in military populations. Sports Medicine, 27, 111–125.
Jordan, B. K., Schlenger, W. E., Hough, R., Kulka, R. A., Weiss, D., Fairbank, J. A. et al. (1991). Lifetime
and current prevalence of specific psychiatric disorders among Vietnam veterans and controls.
Archives of General Psychiatry, 48, 207–215.
Jovanovic, T., Smith, A., Kamkwalala, A., Poole, J., Samples, T., Norrholm, S. D. et al. (2011).
Physiological markers of anxiety are increased in children of abused mothers. Journal of Child
Psychology and Psychiatry, 52, 844–852.
Kang, H., Dalager, N., Mahan, C., & Ishii, E. (2005). The role of sexual assault on the risk of PTSD
among Gulf War veterans. Annals of Epidemiology, 15, 191–195.
Kang, H. K., Natelson, B. H., Mahan, C. M., Lee, K. Y., & Murphy, F. M. (2003). Post-traumatic stress
disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based
survey of 30,000 veterans. American Journal of Epidemiology, 157, 141–148.Kantor, E. M. &
Beckett, D. R. (2011). Psychological first aid. In F. J. Stoddard, Jr., A. Pandya, & C. L. Katz (Eds.),
Trauma-Informed Care in Behavioral Health Services 1-129
Disaster psychiatry: Readiness, evaluation, and treatment (pp. 203–212). Arlington, VA: American
Psychiatric Publishing, Inc.
Kar, N. (2011). Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: A review.
Neuropsychiatric Disease and Treatment, 7, 167–181.
Karney, B. R., Ramchand, R., Osilla, K. C., Caldarone, L. B., & Burns, R. M. (2008). Invisible wounds:
Predicting the immediate and long term consequences of mental health problems in veterans of
Operation Enduring Freedom and Operation Iraqi Freedom. Santa Monica, CA: RAND Corporation.
Kashdan, T. B., Morina, N., & Priebe, S. (2009). Post-traumatic stress disorder, social anxiety disorder,
and depression in survivors of the Kosovo War: Experiential avoidance as a contributor to distress
and quality of life. Journal of Anxiety Disorders, 23, 185–196.
Keane, T. M., Caddell, J. M., & Taylor, K. L. (1988). Mississippi Scale for Combat-Related Posttraumatic
Stress Disorder: Three studies in reliability and validity. Journal of Consulting & Clinical
Psychology, 56, 85–90.
Kelly, V. G., Merrill, G. S., Shumway, M., Alvidrez, J., & Boccellari, A. (2010). Outreach, engagement,
and practical assistance: Essential aspects of PTSD care for urban victims of violent crime. Trauma,
Violence, and Abuse: A Review Journal, 11, 144–156.
Kent, M., Davis, M. C., Stark, S. L., & Stewart, L. A. (2011). A resilience-oriented treatment for
posttraumatic stress disorder: Results of a preliminary randomized clinical trial. Journal of Traumatic
Stress, 24, 591–595.
Kersting, A., Reutemann, M., Gast, U., Ohrmann, P., Suslow, T., Michael, N. et al. (2003). Dissociative
disorders and traumatic childhood experiences in transsexuals. Journal of Nervous and Mental
Disease, 191, 182–189.Kessler, R. C. (2000). Posttraumatic stress disorder: The burden to the
individual and to society. Journal of Clinical Psychiatry, 61 Supplement 5, 4–12.
Kessler, R. C. & Merikangas, K. R. (2004). The National Comorbidity Survey Replication (NCS–R):
Background and aims. International Journal of Methods in Psychiatric Research, 13, 60–68.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime
prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey
Replication. Archives of General Psychiatry, 62, 593–602.
Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of
12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General
Psychiatry, 62, 617–627.
Kessler, R. C., Crum, R. M., Warner, L. A., Nelson, C. B., Schulenberg, J., & Anthony, J. C. (1997).
Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders
in the National Comorbidity Survey. Archives of General Psychiatry, 54, 313–321.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder
in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., Nelson, C. B., & Breslau, N. N. (1999).
Epidemiological risk factors for trauma and PTSD. In R. Yehuda (Ed.), Risk factors for PTSD. (pp.
23–59). Washington, DC: American Psychiatric Press.
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and
recent applications. Harvard Review of Psychiatry, 4, 231–244.
Khaylis, A., Polusny, M. A., Erbes, C. R., Gewirtz, A., & Rath, M. (2011). Posttraumatic stress, family
adjustment, and treatment preferences among National Guard Soldiers deployed to OEF/OIF. Military
Medicine, 176, 126–131.
1-130 Part 3, Section 1—A Review of the Literature
Khoo, A., Dent, M. T., & Oei, T. P. S. (2011). Group cognitive behaviour therapy for military service–
related post-traumatic stress disorder: Effectiveness, sustainability and repeatability. Australian and
New Zealand Journal of Psychiatry, 45, 663–672.
Kilcommons, A. M. & Morrison, A. P. (2005). Relationships between trauma and psychosis: An
exploration of cognitive and dissociative factors. Acta Psychiatrica Scandinavica, 112, 351–359.
Kilcommons, A. M., Morrison, A. P., Knight, A., & Lobban, F. (2008). Psychotic experiences in people
who have been sexually assaulted. Social Psychiatry and Psychiatric Epidemiology, 43, 602–611.
Kilpatrick, D. G., Acierno, R., Resnick, H. S., Saunders, B. E., & Best, C. L. (1997). A 2-year longitudinal
analysis of the relationships between violent assault and substance use in women. Journal of
Consulting and Clinical Psychology, 65, 834–847.
Kim, M. M., Ford, J. D., Howard, D. L., & Bradford, D. W. (2010). Assessing trauma, substance abuse,
and mental health in a sample of homeless men. Health & Social Work, 35, 39–48.
Kimerling, R. & Calhoun, K. S. (1994). Somatic symptoms, social support, and treatment seeking among
sexual assault victims. Journal of Consulting and Clinical Psychology, 62, 333–340.
Kimerling, R., Ouimette, P., & Weitlauf, J. C. (2007). Gender issues in PTSD. In M. J. Friedman, T. M.
Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 207–228). Guilford
Press: New York.
Kimerling, R., Street, A. E., Pavao, J., Smith, M. W., Cronkite, R. C., Holmes, T. H. et al. (2010).
Military-related sexual trauma among Veterans Health Administration patients returning from
Afghanistan and Iraq. American Journal of Public Health, 100, 1409–1412.
King, D. W., King, L. A., Foy, D. W., & Gudanowski, D. M. (1996). Prewar factors in combat-related
posttraumatic stress disorder: structural equation modeling with a national sample of female and male
Vietnam veterans. Journal of Consulting and Clinical Psychology, 64, 520–531.
Kira, I. A., Ahmed, A., Wasim, F., Mahmoud, V., Colrain, J., & Rai, D. (2012). Group therapy for
refugees and torture survivors: Treatment model innovations. International Journal of Group
Psychotherapy, 62, 69–88.
Kira, I. A., Lewandowski, L. A., Templin, T. N., Ramaswamy, V., Ozkan, B., & Mohanesh, J. (2009). The
effects of post-retribution inter-group forgiveness: The case of Iraqi refugees. Peace and Conflict, 15,
385–413.
Klariç, M., Francciskovic, T., Klariç, B., Kresiç, M., Grkoviç, J., Lisica, I. D. et al. (2008). Social support
and PTSD symptoms in war-traumatized women in Bosnia and Herzegovina. Psychiatria Danubina,
20, 466–473.
Knoll, J. & Resnick, P. J. (2006). The detection of malingered post-traumatic stress disorder. Psychiatric
Clinics of North America, 29, 629–647.
Knudsen, H. K., Ducharme, L. J., & Roman, P. M. (2006). Counselor emotional exhaustion and turnover
intention in therapeutic communities. Journal of Substance Abuse Treatment, 31, 173–180.
Koenen, K. C. (2006). Developmental epidemiology of PTSD: self-regulation as a central mechanism.
Annals of the New York Academy of Sciences, 1071, 255–266.
Koenen, K. C., Moffitt, T. E., Caspi, A., Gregory, A., Harrington, H., & Poulton, R. (2008). The
developmental mental–disorder histories of adults with posttraumatic stress disorder: A prospective
longitudinal birth cohort study. Journal of Abnormal Psychology, 117, 460–466.
Koenen, K. C., Stellman, S. D., Sommer, J. F., Jr., & Stellman, J. M. (2008). Persisting posttraumatic
stress disorder symptoms and their relationship to functioning in Vietnam veterans: A 14-year follow-
up. Journal of Traumatic Stress, 21, 49–57.
Trauma-Informed Care in Behavioral Health Services 1-131
Kornør, H., Winje, D., Ekeberg, Ÿ., Weisaeth, L., Kirkehei, I., Johansen, K. et al. (2008). Early trauma-
focused cognitive–behavioural therapy to prevent chronic post-traumatic stress disorder and related
symptoms: A systematic review and meta-analysis. BMC Psychiatry, 8.
Kreidler, M. & Einsporn, R. (2012). A comparative study of therapy duration for survivors of childhood
sexual abuse. Journal of Psychosocial Nursing and Mental Health Services, 50, 26–32.
Krysinska, K. & Lester, D. (2010). Post-traumatic stress disorder and suicide risk: A systematic review.
Archives of Suicide Research, 14, 1–23.
Kubany, E. S., Hill, E. E., Owens, J. A., Iannce–Spencer, C., McCaig, M. A., Tremayne, K. J. et al. (2004).
Cognitive trauma therapy for battered women with PTSD (CTT–BW). Journal of Consulting and
Clinical Psychology, 72, 3–18.
Kubany, E. S., Leisen, M. B., Kaplan, A. S., & Kelly, M. P. (2000). Validation of a brief measure of
posttraumatic stress disorder: The distressing event questionnaire (DEQ). Psychological Assessment,
12, 197–209.
Kudler, H. S., Krupnick, J. L., Blank, A. S., Jr., Herman, J. L., & Horowitz, M. J. (2009). Psychodynamic
therapy for adults. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective
treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies
(2nd ed.) (pp. 346–369). New York: Guilford Press.
Kuhn, J. H. & Nakashima, J. (2011). Community Homelessness Assessment, Local Education and
Networking Group (CHALENG) for veterans: The fifteenth annual progress report on public law
105–114 services for homeless veterans assessment and coordination March 11, 2009. Washington,
DC: U.S. Department of Veterans Affairs.Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R.
L., Jordan, B. K., Marmar, C. R. et al. (1990a). The National Vietnam Veterans Readjustment Study:
Tables of findings and technical appendices Research Triangle Park, NC: Research Triangle Institute.
Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R. L., Jordan, B. K., Marmar, C. R. et al. (1990b).
Trauma and the Vietnam war generation: Report of findings from the National Vietnam Veterans
Readjustment Study. New York: Brunner/Mazel.
Kushner, M. G., Krueger, R., Frye, B., & Peterson, J. (2008). Epidemiological perspectives on co-
occurring anxiety disorder and substance use disorder. In S. H. Stewart & P. J. Conrod (Eds.), Anxiety
and substance use disorders: The vicious cycle of comorbidity (pp. 3–17). New York: Springer
Science + Business Media.
Lacoursiere, R. B. (2001). “Burnout” and substance user treatment: The phenomenon and the
administrator–clinician’s experience. Substance Use & Misuse, 36, 1839–1874.
Laflamme, L., Burrows, S., & Hasselberg, M. (2009). Socioeconomic differences in injury risks: A review
of findings and a discussion of potential countermeasures. Geneva: World Health Organization.
Lalor, K. & McElvaney, R. (2010). Child sexual abuse, links to later sexual exploitation/high-risk sexual
behavior, and prevention/treatment programs. Trauma, Violence, & Abuse, 11, 159–177.
Lang, A. J., Strauss, J. L., Bomyea, J., Bormann, J. E., Hickman, S. D., Good, R. C. et al. (2012). The
theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification,
36(6), 759–786.
Laugharne, J., Lillee, A., & Janca, A. (2010). Role of psychological trauma in the cause and treatment of
anxiety and depressive disorders. Current Opinion in Psychiatry, 23, 25–29.
Lawyer, S. R., Resnick, H. S., Galea, S., Ahern, J., Kilpatrick, D. G., & Vlahov, D. (2006). Predictors of
peritraumatic reactions and PTSD following the September 11th terrorist attacks. Psychiatry, 69,
130–141.
Layne, C. M., Warren, J. S., Watson, P. J., & Shalev, A. Y. (2007). Risk, vulnerability, resistance, and
resilience: Toward an integrative conceptualization of posttraumatic adaptation. In M. J. Friedman, T.
1-132 Part 3, Section 1—A Review of the Literature
M. Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 497–520). New
York: Guilford Press.
Lee, B. A. & Schreck, C. J. (2005). Danger on the streets: Marginality and victimization among homeless
people. American Behavioral Scientist, 48, 1055–1081.
Lee, C. S., Chang, J. C., Liu, C. Y., Chang, C. J., Chen, T. H. H., Chen, C. H. et al. (2009). Acculturation,
psychiatric comorbidity and posttraumatic stress disorder in a Taiwanese aboriginal population.
Social Psychiatry and Psychiatric Epidemiology, 44, 55–62.
Lee, E. & Mock, M. R. (2005a). Asian families: An overview. In M. McGoldrick, J. Giordano, & N.
Garcia-Preto (Eds.), Ethnicity and family therapy (3rd ed.) (pp. 269–289). Guilford Press: New York.
Lee, E. & Mock, M. R. (2005b). Chinese families. In M. McGoldrick, J. Giordano, & N. Garcia-Preto
(Eds.), Ethnicity and family therapy (3rd ed.) (pp. 302–318). Guilford Press: New York.
Lee, T. T., Westrup, D. A., Ruzek, J. I., Keller, J., & Weitlauf, J. C. (2007). Impact of clinician gender on
examination anxiety among female veterans with sexual trauma: A pilot study. Journal of Women’s
Health, 16, 1291–1299.
Lensvelt-Mulders, G., van der Hart, O., van Ochten, J. M., van Son, M. J. M., Steele, K., & Breeman, L.
(2008). Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis.
Clinical Psychology Review, 28, 1138–1151.
Lent, J. (2010). Stressors and stress management of counselors: Findings from interviews of professional
counselors. Retrieved July 4, 2013, from:
http://counselingoutfitters.com/vistas/vistas10/Article_73.pdf
Lester, K., Resick, P. A., Young–Xu, Y., & Artz, C. (2010). Impact of race on early treatment termination
and outcomes in posttraumatic stress disorder treatment. Journal of Consulting and Clinical
Psychology, 78, 480–489.
Levitt, J. T., Malta, L. S., Martin, A., Davis, L., & Cloitre, M. (2007). The flexible application of a
manualized treatment for PTSD symptoms and functional impairment related to the 9/11 World Trade
Center attack. Behaviour Research and Therapy, 45, 1419–1433.
Lewis, K. L. & Grenyer, B. F. (2009). Borderline personality or complex posttraumatic stress disorder? An
update on the controversy. Harvard Review of Psychiatry, 17, 322–328.
Lewis-Fernández, R., Martínez-Taboas, A., Sar, V., Patel, S., & Boatin, A. (2007). The cross-cultural
assessment of dissociation. In J. P. Wilson & C. S. Tang (Eds.), Cross-cultural assessment of
psychological trauma and PTSD (pp. 279–317). New York: Springer Science + Business Media.
Libby, A. M., Orton, H. D., Beals, J., Buchwald, D., & Manson, S. M. (2008). Childhood abuse and later
parenting outcomes in two American Indian tribes. Child Abuse & Neglect, 32, 195–211.
Lilly, M. M. & Graham-Bermann, S. A. (2009). Ethnicity and risk for symptoms of posttraumatic stress
following intimate partner violence. Journal of Interpersonal Violence, 24, 3–19.
Lu, W., Mueser, K. T., Rosenberg, S. D., & Jankowski, M. K. (2008). Correlates of adverse childhood
experiences among adults with severe mood disorders. Psychiatric Services, 59, 1018–1026.
Luce, H., Schrager, S., & Gilchrist, V. (2010). Sexual assault of women. American Family Physician, 81,
489–495.
Lutz, G. M., Kramer, R. E., Gonnerman, M. E., Lantz, G. L., & Downs, W. R. (1995). Substance abuse
and the Iowa flood disaster of 1993: Final report. Cedar Falls, IA: University of Northern Iowa.
Lynch, M. and Cicchetti, D. (1998). An ecological–transactional analysis of children and contexts: The
longitudinal interplay among child maltreatment, community violence, and children’s
symptomatology. Development and Psychopathology, 10, 235–257.
Trauma-Informed Care in Behavioral Health Services 1-133
Lynch, S. M. (2011). Restoring relationships: Group interventions for survivors of sexual traumas. In
Surviving sexual violence: A guide to recovery and empowerment (pp. 179–198). Lanham, MD:
Rowman & Littlefield.
Macklin, M. L., Metzger, L. J., Litz, B. T., McNally, R. J., Lasko, N. B., Orr, S. P. et al. (1998). Lower
precombat intelligence is a risk factor for posttraumatic stress disorder. Journal of Consulting and
Clinical Psychology, 66, 323–326.
Maercker, A., Zöllner, T., Menning, H., Rabe, S., & Karl, A. (2006). Dresden PTSD treatment study:
Randomized controlled trial of motor vehicle accident survivors. BMC. Psychiatry, 6, 29.
Maes, M., Delmeire, L., Mylle, J., & Atamura, C. (2001). Risk and preventive factors of post-traumatic
stress disorder (PTSD): Alcohol consumption and intoxication prior to a traumatic event diminishes
the relative risk to develop PTSD in response to that trauma. Journal of Affective Disorders, 63, 113–
121.
Maguen, S., Luxton, D. D., Skopp, N. A., & Madden, E. (2011). Gender differences in traumatic
experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. Journal
of Psychiatric Research, 46(3), 311–316.
Maguen, S., Ren, L., Bosch, J. O., Marmar, C. R., & Seal, K. H. (2010). Gender differences in mental
health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care.
American Journal of Public Health, 100, 2450–2456.
Maguen, S., Suvak, M., & Litz, B. T. (2006). Predictors and prevalence of posttraumatic stress disorder
among military veterans. In A. B. Adler, C. A. Castro, & T. W. Britt (Eds.), Military life: The
psychology of serving in peace and combat (Vol. 2): Operational stress (pp. 141–169). Westport, CT:
Praeger Security International.
Malta, L. S., Levitt, J. T., Martin, A., Davis, L., & Cloitre, M. (2009). Correlates of functional impairment
in treatment-seeking survivors of mass terrorism. Behavior Therapy, 40, 39–49.
Mancino, M. J., Pyne, J. M., Tripathi, S., Constans, J., Roca, V., & Freeman, T. (2006). Quality-adjusted
health status in veterans with posttraumatic stress disorder. Journal of Nervous and Mental Disease,
194, 877–879.
Manson, S. M., Beals, J., Klein, S. A., & Croy, C. D. (2005). Social epidemiology of trauma among 2
American Indian reservation populations. American Journal of Public Health, 95, 851–859.
Marchand, A., Guay, S., Boyer, R., Lucci, S., Martin, A., & St-Hilaire, M. H. (2006). A Randomized
controlled trial of an adapted form of individual critical incident stress debriefing for victims of an
armed robbery. Brief Treatment and Crisis Intervention, 6, 122–129.
Marques, L., Robinaugh, D. J., LeBlanc, N. J., & Hinton, D. (2011). Cross-cultural variations in the
prevalence and presentation of anxiety disorders. Expert Review of Neurotherapeutics, 11, 313–322.
Marsella, A. J. (2010). Ethnocultural aspects of PTSD: An overview of concepts, issues, and treatments.
Traumatology, 16, 17–26.
Marsella, A. J. & Christopher, M. A. (2004). Ethnocultural considerations in disasters: An overview of
research, issues, and directions. Psychiatric Clinics of North America, 27, 521–539.Marsella, A. J.,
Johnson, J. L., Watson, P., & Gryczynski, J. (2008). Essential concepts and foundations. In A. J.
Marsella, J. L. Johnson, P. Watson, & J. Gryczynski (Eds.), Ethnocultural perspectives on disaster
and trauma: Foundations, issues, and applications (pp. 3–13). New York: Springer Science +
Business Media.
Marshall, G. N., Schell, T. L., & Miles, J. N. (2009). Ethnic differences in posttraumatic distress:
Hispanics’ symptoms differ in kind and degree. Journal of Consulting & Clinical Psychology, 77,
1169–1178.
1-134 Part 3, Section 1—A Review of the Literature
Marshall, G. N., Schell, T. L., Elliott, M. N., Berthold, S. M., & Chun, C. A. (2005). Mental health of
Cambodian refugees 2 decades after resettlement in the United States. JAMA, 294, 571–579.
Marshall-Berenz, E. C., Vujanovic, A. A., & Zvolensky, M. J. (2011). Main and interactive effects of a
nonclinical panic attack history and distress tolerance in relation to PTSD symptom severity. Journal
of Anxiety Disorders, 25, 185–191.
Martin, M., Marchand, A., Boyer, R., & Martin, N. (2009). Predictors of the development of posttraumatic
stress disorder among police officers. Journal of Trauma & Dissociation, 10, 451–468.
Martin, S. L., Ray, N., Sotres-Alvarez, D., Kupper, L. L., Moracco, K. E., Dickens, P. A. et al. (2006).
Physical and sexual assault of women with disabilities. Violence Against Women, 12, 823–837.
Maschi, T., Dennis, K. S., Gibson, S., MacMillan, T., Sternberg, S., & Hom, M. (2011). Trauma and stress
among older adults in the criminal justice system: A review of the literature with implications for
social work. Journal of Gerontological Social Work, 54, 390–424.
Mathieu, A., Mazza, S., Petit, D., Decary, A., Massicotte-Marquez, J., Malo, J. et al. (2007). Does age
worsen EEG slowing and attention deficits in obstructive sleep apnea syndrome? Clinical
Neurophysiology, 118, 1538–1544.
McCarthy, E. & Petrakis, I. (2010). Epidemiology and management of alcohol dependence in individuals
with post-traumatic stress disorder. CNS Drugs, 24, 997–1007.
McCutcheon, V. V., Heath, A. C., Nelson, E. C., Bucholz, K. K., Madden, P. A., & Martin, N. G. (2010).
Clustering of trauma and associations with single and co-occurring depression and panic attack over
twenty years. Twin Research and Human Genetics, 13, 57–65.
McDonagh, A., Friedman, M., McHugo, G., Ford, J., Sengupta, A., Mueser, K. et al. (2005). Randomized
trial of cognitive–behavioral therapy for chronic posttraumatic stress disorder in adult female
survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology, 73, 515–524.
McFall, M., Atkins, D. C., Yoshimoto, D., Thompson, C. E., Kanter, E., Malte, C. A. et al. (2006).
Integrating tobacco cessation treatment into mental health care for patients with posttraumatic stress
disorder. American Journal on Addictions, 15, 336–344.
McGovern, M. P., Lambert-Harris, C., Acquilano, S., Xie, H., Alterman, A. I., & Weiss, R. D. (2009). A
cognitive behavioral therapy for co-occurring substance use and posttraumatic stress disorders.
Addictive Behaviors, 34, 892–897.
McGovern, M. P., Lambert–Harris, C., Alterman, A. I., Xie, H., & Meier, A. (2011). A randomized
controlled trial comparing integrated cognitive behavioral therapy versus individual addiction
counseling for co-occurring substance use and posttraumatic stress disorders. Journal of Dual
Diagnosis, 7, 207–227.
McHugo, G. J., Caspi, Y., Kammerer, N., Mazelis, R., Jackson, E. W., Russell, L. et al. (2005). The
assessment of trauma history in women with co-occurring substance abuse and mental disorders and a
history of interpersonal violence. The Journal of Behavioral Health Services & Research, 32, 113–
127.
McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C.
(2010a). Childhood adversities and adult psychiatric disorders in the national comorbidity survey
replication II: Associations with persistence of DSM-IV disorders. Archives of General Psychiatry,
67, 124–132.
McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C.
(2010b). Childhood adversities and adult psychopathology in the National Comorbidity Survey
Replication (NCS–R) III: Associations with functional impairment related to DSM-IV disorders.
Psychological Medicine, 40, 847–859.
Trauma-Informed Care in Behavioral Health Services 1-135
McLay, R. N., Klam, W. P., & Volkert, S. L. (2010). Insomnia is the most commonly reported symptom
and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from
military deployments. Military Medicine, 175, 759–762.
McLean, C. P. & Anderson, E. R. (2009). Brave men and timid women? A review of the gender
differences in fear and anxiety. Clinical Psychology Review, 29, 496–505.
McLean, C. P. & Foa, E. B. (2011). Prolonged exposure therapy for post-traumatic stress disorder: A
review of evidence and dissemination. Expert Review of Neurotherapeutics, 11, 1151–1163.
McLean, C. P., Asnaani, A., Litz, B. T., & Hofmann, S. G. (2011). Gender differences in anxiety
disorders: prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric
Research, 45, 1027–1035.
McLean, C. P., Steenkamp, M. M., Levy, H. C., & Litz, B. T. (2010). Posttraumatic stress disorder. In M.
A. Cucciare & K. R. Weingardt (Eds.), Using technology to support evidence-based behavioral
health practices: A clinician’s guide (pp. 45–68). New York: Routledge/Taylor & Francis Group.
McLeod, D. S., Koenen, K. C., Meyer, J. M., Lyons, M. J., Eisen, S., True, W. et al. (2001). Genetic and
environmental influences on the relationship among combat exposure, posttraumatic stress disorder
symptoms, and alcohol use. Journal of Traumatic Stress, 14, 259–275.
McNamara, C., Schumacher, J. E., Milby, J. B., Wallace, D., & Usdan, S. (2001). Prevalence of
nonpsychotic mental disorders does not affect treatment outcome in a homeless cocaine-dependent
sample. American Journal of Drug and Alcohol Abuse, 27, 91–106.
McWilliams, L. A., Cox, B. J., & Enns, M. W. (2003). Mood and anxiety disorders associated with chronic
pain: An examination in a nationally representative sample. Pain, 106, 127–133.
Mendes, D. D., Mello, M. F., Ventura, P., Passarela, C. M., & Mari, J. J. (2008). A systematic review on
the effectiveness of cognitive behavioral therapy for posttraumatic stress disorder. International
Journal of Psychiatry in Medicine, 38, 241–259.
Merikangas, K. R., Akiskal, H. S., Angst, J., Greenberg, P. E., Hirschfeld, R. M., Petukhova, M. et al.
(2007). Lifetime and 12–month prevalence of bipolar spectrum disorder in the National Comorbidity
Survey replication. Archives of General Psychiatry, 64, 543–552.
Mevissen, L. & de Jongh, A. (2010). PTSD and its treatment in people with intellectual disabilities: A
review of the literature. Clinical Psychology Review, 30, 308–316.
Meyer, R. E. (1986). Psychobiology and the treatment of drug dependence: The biobehavioral interface.
American Journal of Drug and Alcohol Abuse, 12, 223–233.
Meyerbröker, K. & Emmelkamp, P. M. (2010). Virtual reality exposure therapy in anxiety disorders: a
systematic review of process-and-outcome studies. Depression and Anxiety, 27, 933–944.
Miller, D. & Guidry, L. (2001). Addictions and trauma recovery: Healing the body, mind and spirit. New
York: W. W. Norton & Co.
Moak, Z. B. & Agrawal, A. (2010). The association between perceived interpersonal social support and
physical and mental health: results from the National Epidemiological Survey on Alcohol and Related
Conditions. Journal of Public Health: Oxford Journals, 32, 191–201.
Moffitt, T. E., Caspi, A., Taylor, A., Kokaua, J., Milne, B. J., Polanczyk, G. et al. (2010). How common
are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective
versus retrospective ascertainment. Psychological Medicine: A Journal of Research in Psychiatry and
the Allied Sciences, 40, 899–909.
Mollica, R. F., McInnes, K., Poole, C., & Tor, S. (1998). Dose–effect relationships of trauma to symptoms
of depression and post-traumatic stress disorder among Cambodian survivors of mass violence.
British Journal of Psychiatry, 173, 482–488.
1-136 Part 3, Section 1—A Review of the Literature
Monson, C. M., Rodriguez, B. F., & Warner, R. (2005). Cognitive–behavioral therapy for PTSD in the real
world: Do interpersonal relationships make a real difference? Journal of Clinical Psychology, 61,
751–761.
Monson, C. M., Stevens, S. P., & Schnurr, P. P. (2005). Cognitive–behavioral couple’s treatment for
posttraumatic stress disorder. In T. A. Corales (Ed.), Focus on posttraumatic stress disorder research
(pp. 245–274). Hauppauge, NY: Nova Science Publishers.
Monson, C. M., Taft, C. T., & Fredman, S. J. (2009). Military-related PTSD and intimate relationships:
From description to theory-driven research and intervention development. Clinical Psychology
Review, 29, 707–714.
Mouton, C. P., Rodabough, R. J., Rovi, S. L., Hunt, J. L., Talamantes, M. A., Brzyski, R. G. et al. (2004).
Prevalence and 3-year incidence of abuse among postmenopausal women. American Journal of
Public Health, 94, 605–612.
Mueser, K. T., Rosenberg, S. D., Xie, H., Jankowski, M. K., Bolton, E. E., Lu, W. et al. (2008). A
randomized controlled trial of cognitive–behavioral treatment for posttraumatic stress disorder in
severe mental illness. Journal of Consulting & Clinical Psychology, 76, 259–271.
Mylle, J. & Maes, M. (2004). Partial posttraumatic stress disorder revisited. Journal of Affective Disorders,
78, 37–48.
Najavits, L. M. (2002). Seeking safety: A treatment manual for PTSD and substance abuse. New York:
Guilford Press.
Najavits, L. M. (2004). Assessment of trauma, PTSD, and substance use disorder: A practical guide. In J.
P. Wilson & T. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 466–491). New York:
Guilford.
Najavits, L. M., Gastfriend, D. R., Barber, J. P., Reif, S., Muenz, L. R., Blaine, J. et al. (1998). Cocaine
dependence with and without PTSD among subjects in the National Institute on Drug Abuse
Collaborative Cocaine Treatment Study. American Journal of Psychiatry, 155, 214–219.
Najavits, L. M., Harned, M. S., Gallop, R. J., Butler, S. F., Barber, J. P., Thase, M. E. et al. (2007). Six-
month treatment outcomes of cocaine-dependent patients with and without PTSD in a multisite
national trial. Journal of Studies on Alcohol and Drugs, 68, 353–361.
Najavits, L. M., Schmitz, M., Gotthardt, S., & Weiss, R. D. (2005). Seeking safety plus exposure therapy:
An outcome study on dual diagnosis men. Journal of Psychoactive Drugs, 37, 425–435.
Nappi, C. M., Drummond, S. P., & Hall, J. M. (2012). Treating nightmares and insomnia in posttraumatic
stress disorder: A review of current evidence. Neuropharmacology, 62, 576–585.
Narrow, W. E., Rae, D. S., Robins, L. N., & Regier, D. A. (2002). Revised prevalence based estimates of
mental disorders in the United States: Using a clinical significance criterion to reconcile 2 surveys’
estimates. Archives of General Psychiatry, 59, 115–123.
National Child Traumatic Stress Network & National Center for PTSD (2006). Psychological first aid:
Field operations guide. White River Junction, VT: National Center for PTSD.
National Institute for Health and Clinical Excellence (2005). Post-traumatic stress disorder (PTSD).
London: National Institute for Health and Clinical Excellence.
Nelson-Zlupko, L., Dore, M. M., Kauffman, E., & Kaltenbach, K. (1996). Women in recovery: Their
perceptions of treatment effectiveness. Journal of Substance Abuse Treatment, 13, 51–59.
Neuner, F., Schauer, M., Klaschik, C., Karunakara, U., & Elbert, T. (2004). A comparison of narrative
exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress
disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology, 72, 579–
587.
Trauma-Informed Care in Behavioral Health Services 1-137
Newman, J. M., Turnbull, A., Berman, B. A., Rodrigues, S., & Serper, M. R. (2010). Impact of traumatic
and violent victimization experiences in individuals with schizophrenia and schizoaffective disorder.
Journal of Nervous and Mental Disease, 198, 708–714.
Nickerson, A., Bryant, R. A., Silove, D., & Steel, Z. (2011). A critical review of psychological treatments
of posttraumatic stress disorder in refugees. Clinical Psychology Review, 31, 399–417.
Nishith, P., Duntley, S. P., Domitrovich, P. P., Uhles, M. L., Cook, B. J., & Stein, P. K. (2003). Effect of
cognitive behavioral therapy on heart rate variability during REM sleep in female rape victims with
PTSD. Journal of Traumatic Stress, 16, 247–250.
Nixon, R. D. V. & Nearmy, D. M. (2011). Treatment of comorbid posttraumatic stress disorder and major
depressive disorder: A pilot study. Journal of Traumatic Stress, 24, 451–455.
Noll, J. G., Horowitz, L. A., Bonanno, G. A., Trickett, P. K., & Putnam, F. W. (2003). Revictimization and
self-harm in women who experienced childhood sexual abuse: Results from a prospective study.
Journal of Interpersonal Violence, 18, 1452–1471.
Norman, S. B., Tate, S. R., Wilkins, K. C., Cummins, K., & Brown, S. A. (2010). Posttraumatic stress
disorder’s role in integrated substance dependence and depression treatment outcomes. Journal of
Substance Abuse Treatment, 38, 346–355.
Norris, F. H. & Slone, L. B. (2007). The epidemiology of trauma and PTSD. In M. J. Friedman, T. M.
Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 78–98). Guilford Press:
New York.
Norris, F. H., Friedman, M. J., & Watson, P. J. (2002). 60,000 disaster victims speak: Part II. Summary
and implications of the disaster mental health research. Psychiatry, 65, 240–260.
Norris, F. H., Friedman, M. J., Watson, P. J., Byrne, C. M., Diaz, E., & Kaniasty, K. (2002). 60,000
disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry,
65, 207–239.
Norris, F. H., Kaniasty, K. Z., Conrad, M. L., Inman, G. L., & Murphy, A. D. (2002). Placing age
differences in cultural context: A comparison of the effects of age on PTSD after disasters in the
United States, Mexico, and Poland. Journal of Clinical Geropsychology, 8, 153–173.
Norris, F. H., Perilla, J. L., Ibanez, G. E., & Murphy, A. D. (2001). Sex differences in symptoms of
posttraumatic stress: Does culture play a role? Journal of Traumatic Stress, 14, 7–28.
Norton, P. J. & Price, E. C. (2007). A meta-analytic review of adult cognitive–behavioral treatment
outcome across the anxiety disorders. Journal of Nervous and Mental Disease, 195, 521–531.
O’Donnell, M. L., Creamer, M., & Cooper, J. (2010). Criterion A: Controversies and clinical implications.
In G. M. Rosen (Ed.), Clinician’s guide to posttraumatic stress disorder (pp. 51–75). Hoboken, NJ,
US: John Wiley & Sons Inc.
Office of the Surgeon Multi-National Corps–Iraq & Office of The Surgeon General United States Army
Medical Command (2006). Mental Health Advisory Team (MHAT) IV Operation Iraqi Freedom 05–
07. Final report 17 November 2006. Washington, DC: U. S. Army Medical Department.
O’Hare, T., Sherrer, M. V., & Shen, C. (2006). Subjective distress from stressful events and high-risk
behaviors as predictors of PTSD symptom severity in clients with severe mental illness. Journal of
Traumatic Stress, 19, 375–386.
Olatunji, B. O., Cisler, J. M., & Tolin, D. F. (2007). Quality of life in the anxiety disorders: A meta-
analytic review. Clinical Psychology Review, 27, 572–581.
Olff, M., Langeland, W., Draijer, N., & Gersons, B. P. R. (2007). Gender differences in posttraumatic
stress disorder. Psychological Bulletin, 133, 183–204.
1-138 Part 3, Section 1—A Review of the Literature
Oman, D., Hedberg, J., & Thoresen, C. E. (2006). Passage meditation reduces perceived stress in health
professionals: A randomized, controlled trial. Journal of Consulting and Clinical Psychology, 74,
714–719.
Opler, L. A., Grennan, M. S., & Ford, J. D. (2009). Pharmacotherapy. In C. A. Courtois & J. D. Ford
(Eds.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 329–349). New
York: Guilford Press.
Orsillo, S. M. (2001). Measures for social phobia. In M. M. Antony, S. M. Orsillo, & L. Roemer (Eds.),
Practitioner’s guide to empirically based measures of anxiety (pp. 165–187). Dordrecht, Netherlands:
Kluwer Academic Publishers.
Ortega, A. N. & Rosenheck, R. (2001). Mental and physical health and acculturation among Hispanic
Vietnam Veterans. Military Medicine, 166, 894–897.
Osterman, J. E. & de Jong, J. T. V. M. (2007). Cultural issues and trauma. In M. J. Friedman, T. M. Keane,
& P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 425–446). Guilford Press: New
York.
Otis, J. D., Keane, T. M., Kerns, R. D., Monson, C., & Scioli, E. (2009). The development of an integrated
treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Med., 10,
1300–1311.
Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: Current state of the evidence.
Dialogues in Clinical Neuroscience, 13, 413–421.
Ougrin, D. (2011). Efficacy of exposure versus cognitive therapy in anxiety disorders: Systematic review
and meta-analysis. BMC. Psychiatry, 11, 200.
Ouimette, P. C., Brown, P. J., & Najavits, L. M. (1998). Course and treatment of patients with both
substance use and posttraumatic stress disorders. Addictive Behaviors, 23, 785–795.
Ouimette, P., Moos, R. H., & Brown, P. J. (2003). Substance use disorder–posttraumatic stress disorder
comorbidity: A survey of treatments and proposed practice guidelines. In P. Ouimette & P. J. Brown
(Eds.), Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders
(pp. 91–110). Washington, DC: American Psychological Association.
Owens, G. P., Steger, M. F., Whitesell, A. A., & Herrera, C. J. (2009). Posttraumatic stress disorder, guilt,
depression, and meaning in life among military veterans. Journal of Traumatic Stress, 22, 654–657.
Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder
and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73.
Pae, C. U., Lim, H. K., Peindl, K., Ajwani, N., Serretti, A., Patkar, A. A. et al. (2008). The atypical
antipsychotics olanzapine and risperidone in the treatment of posttraumatic stress disorder: a meta-
analysis of randomized, double-blind, placebo-controlled clinical trials. International Clinical
Psychopharmacology, 23, 1–8.
Palinkas, L., Downs, M., Patterson, J., & Russell, J. (1993). Social, cultural, and psychological impacts of
the Exxon Valdez oil spill. Human Organization, 52, 1–13.
Panagioti, M., Gooding, P., & Tarrier, N. (2009). Post-traumatic stress disorder and suicidal behavior: A
narrative review. Clinical Psychology Review, 29, 471–482.
Paunovic, N. & Öst, L. G. (2001). Cognitive–behavior therapy vs exposure therapy in the treatment of
PTSD in refugees. Behaviour Research and Therapy, 39, 1183–1197.
Peirce, J. M., Burke, C. K., Stoller, K. B., Neufeld, K. J., & Brooner, R. K. (2009). Assessing traumatic
event exposure: Comparing the Traumatic Life Events Questionnaire to the Structured Clinical
Interview for DSM-IV. Psychological Assessment, 21, 210–218.
Trauma-Informed Care in Behavioral Health Services 1-139
Peirce, J. M., Kindbom, K. A., Waesche, M. C., Yuscavage, A. S. E., & Brooner, R. K. (2008).
Posttraumatic stress disorder, gender, and problem profiles in substance dependent patients.
Substance Use & Misuse, 43, 596–611.
Peller, A. J., Najavits, L. M., Nelson, S. E., LaBrie, R. A., & Shaffer, H. J. (2010). PTSD among a
treatment sample of repeat DUI offenders. Journal of Traumatic Stress, 23, 468–473.
Peltan, J. R. & Cellucci, T. (2011). Childhood sexual abuse and substance abuse treatment utilization
among substance-dependent incarcerated women. Journal of Substance Abuse Treatment, 41, 215–
224.
Perilla, J. L., Norris, F. H., & Lavizzo, E. A. (2002). Ethnicity, culture, and disaster response: Identifying
and explaining ethnic differences in PTSD six months after Hurricane Andrew. Journal of Social and
Clinical Psychology, 21, 20–45.
Peterlin, B. L., Rosso, A. L., Sheftell, F. D., Libon, D. J., Mossey, J. M., & Merikangas, K. R. (2011).
Post-traumatic stress disorder, drug abuse and migraine: New findings from the National Comorbidity
Survey Replication (NCS–R). Cephalalgia, 31, 235–244.
Petersilia, J. R. (2001). Crime victims with developmental disabilities: A review essay. Criminal Justice
and Behavior, 28, 655–694.
Pfeiffer, P. N., Ganoczy, D., Ilgen, M., Zivin, K., & Valenstein, M. (2009). Comorbid anxiety as a suicide
risk factor among depressed veterans. Depression and Anxiety, 26, 752–757.
Pico-Alfonso, M. A. (2005). Psychological intimate partner violence: The major predictor of posttraumatic
stress disorder in abused women. Neuroscience and Biobehavioral Reviews, 29, 181–193.
Pietrzak, R. H., Goldstein, M. B., Malley, J. C., Rivers, A. J., Johnson, D. C., & Southwick, S. M. (2010).
Risk and protective factors associated with suicidal ideation in veterans of Operations Enduring
Freedom and Iraqi Freedom. Journal of Affective Disorders, 123, 102–107.
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011a). Personality disorders
associated with full and partial posttraumatic stress disorder in the U.S. population: Results from
Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of
Psychiatric Research, 45, 678–686.
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011b). Prevalence and Axis I
comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2
of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety
Disorders, 25, 456–465.
Plummer, S. B. & Findley, P. A. (2012). Women with disabilities’ experience with physical and sexual
abuse. Trauma, Violence, & Abuse, 13, 15–29.
Pole, N., Best, S. R., Metzler, T., & Marmar, C. R. (2005). Why are Hispanics at greater risk for PTSD?
Cultural Diversity and Ethnic Minority Psychology, 11, 144–161.
Pole, N., Best, S. R., Weiss, D. S., Metzler, T., Liberman, A. M., Fagan, J. et al. (2001). Effects of gender
and ethnicity on duty-related posttraumatic stress symptoms among urban police officers. Journal of
Nervous & Mental Disease, 189, 442–448.
Pole, N., Gone, J. P., & Kulkarni, M. (2008). Posttraumatic stress disorder among ethnoracial minorities in
the United States. Clinical Psychology: Science and Practice, 15, 35–61.
Polinder, S., Haagsma, J. A., Belt, E., Lyons, R. A., Erasmus, V., Lund, J. et al. (2010). A systematic
review of studies measuring health-related quality of life of general injury populations. BMC Public
Health, 10, 783.
Polinder, S., Haagsma, J. A., Lyons, R. A., Gabbe, B. J., Ameratunga, S., Cryer, C. et al. (2012).
Measuring the population burden of fatal and nonfatal injury. Epidemiologic Reviews, 34, 17–31.
1-140 Part 3, Section 1—A Review of the Literature
Polusny, M. A., Erbes, C. R., Murdoch, M., Arbisi, P. A., Thuras, P., & Rath, M. B. (2011). Prospective
risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq.
Psychological Medicine, 41, 687–698.
Ponniah, K. & Hollon, S. D. (2009). Empirically supported psychological treatments for adult acute stress
disorder and posttraumatic stress disorder: A review. Depression and Anxiety, 26, 1086–1109.
Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Foa, E. B. (2010). A meta-analytic
review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30, 635–
641.
Pratchett, L. C., Pelcovitz, M. R., & Yehuda, R. (2010). Trauma and violence: Are women the weaker sex?
Psychiatric Clinics of North America, 33, 465–474.
Prigerson, H. G., Maciejewski, P. K., & Rosenheck, R. A. (2002). Population attributable fractions of
psychiatric disorders and behavioral outcomes associated with combat exposure among US men.
American Journal of Public Health, 92, 59–63.
Provencher, M. D., Hawke, L. D., & Thienot, E. (2011). Psychotherapies for comorbid anxiety in bipolar
spectrum disorders. Journal of Affective Disorders, 133, 371–380.
Pulay, A. J., Stinson, F. S., Dawson, D. A., Goldstein, R. B., Chou, S. P., Huang, B. et al. (2009).
Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder:
Results From the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions.
Primary Care Companion to the Journal of Clinical Psychiatry, 11, 53–67.
Pyari, T. T., Kutty, R. V., & Sarma, P. S. (2012). Risk factors of post-traumatic stress disorder in tsunami
survivors of Kanyakumari District, Tamil Nadu, India. Indian Journal of Psychiatry, 54, 48–53.
Qureshi, S. U., Pyne, J. M., Magruder, K. M., Schulz, P. E., & Kunik, M. E. (2009). The link between
post-traumatic stress disorder and physical comorbidities: A systematic review. Psychiatric
Quarterly, 80, 87–97.
Rachamim, L., Nacasch, N., Shafran, N., Tzur, D., & Gilboa-Schechtman, E. (2009). Exposure-based
therapy for post-traumatic stress disorder in children and adults. Israel Journal of Psychiatry and
Related Sciences, 46, 274–281.
Rakofsky, J. J. & Dunlop, B. W. (2011). Treating nonspecific anxiety and anxiety disorders in patients
with bipolar disorder: A review. Journal of Clinical Psychiatry, 72, 81–90.
Rand, M. R. & Robinson, J. F. (2012). Criminal victimization in the United States, 2008—Statistical
tables. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice
Statistics.
Ravindran, L. N. & Stein, M. B. (2009). Pharmacotherapy of PTSD: Premises, principles, and priorities.
Brain Research, 1293, 24–39.
Razza, N. J., Tomasulo, D. J., & Sobsey, D. (2011). Group psychotherapy for trauma-related disorders in
people with intellectual disabilities. Advances in Mental Health and Intellectual Disabilities, 5, 40–
45.
Read, J. & Hammersley, P. (2005). Child sexual abuse and schizophrenia. British Journal of Psychiatry,
186, 76.
Read, J., Agar, K., Argyle, N., & Aderhold, V. (2003). Sexual and physical abuse during childhood and
adulthood as predictors of hallucinations, delusions and thought disorder. Psychology and
Psychotherapy: Theory, Research and Practice, 76, 1–22.
Read, J., van Os, J., Morrison, A. P., & Ross, C. A. (2005). Childhood trauma, psychosis and
schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica
Scandinavica, 112, 330–350.
Trauma-Informed Care in Behavioral Health Services 1-141
Ready, D. J., Thomas, K. R., Worley, V., Backscheider, A. G., Harvey, L. A., Baltzell, D. et al. (2008). A
field test of group based exposure therapy with 102 veterans with war–related posttraumatic stress
disorder. Journal of Traumatic Stress, 21, 150–157.
Reddy, M. K., Polusny, M. A., & Murdoch, M. (2009). On counterbalancing of symptom-reporting in
trauma surveys. Psychological Reports, 105, 1154–1158.
Reiland, S. & Lauterbach, D. (2008). Effects of trauma and religiosity on self-esteem. Psychological
Reports, 102, 779–790.
Reivich, K. J., Seligman, M. E., & McBride, S. (2011). Master resilience training in the U.S. Army.
American Psychology, 66, 25–34.
Renshaw, K. D. (2011). An integrated model of risk and protective factors for post-deployment PTSD
symptoms in OEF/OIF era combat veterans. Journal of Affective Disorders, 128, 321–326.
Renshaw, K. D., Blais, R. K., & Caska, C. M. (2011). Distress in spouses of combat veterans with PTSD:
The importance of interpersonally based cognitions and behaviors. In S. M. Wadsworth & D. Riggs
(Eds.), Risk and resilience in U.S. military families (pp. 69–84). New York: Springer Science +
Business Media.
Renshaw, K. D., Rodrigues, C. S., & Jones, D. H. (2008). Psychological symptoms and marital satisfaction
in spouses of Operation Iraqi Freedom veterans: Relationships with spouses' perceptions of veterans'
experiences and symptoms. Journal of Family Psychology, 22, 586–594.
Resick, P. A., Galovski, T. E., O’Brien, U. M., Scher, C. D., Clum, G. A., & Young–Xu, Y. (2008). A
randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic
stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical
Psychology, 76, 243–258.
Resick, P. A., Nishith, P., & Griffin, M. G. (2003). How well does cognitive–behavioral therapy treat
symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial.
CNS Spectrums, 8, 340–355.
Resick, P. A., Nishith, P., Weaver, T. L., Astin, M. C., & Feuer, C. A. (2002). A comparison of cognitive–
processing therapy with prolonged exposure and a waiting condition for the treatment of chronic
posttraumatic stress disorder in female rape victims. Journal of Consulting & Clinical Psychology,
70, 867–879.
Resick, P. A., Williams, L. F., Suvak, M. K., Monson, C. M., & Gradus, J. L. (2012). Long-term outcomes
of cognitive–behavioral treatments for posttraumatic stress disorder among female rape survivors.
Journal of Consulting and Clinical Psychology, 80, 201–210.
Resnick, H. S., Acierno, R., Amstadter, A. B., Self-Brown, S., & Kilpatrick, D. G. (2007). An acute post–
sexual assault intervention to prevent drug abuse: Updated findings. Addictive Behaviors, 32, 2032–
2045.
Resnick, H. S., Acierno, R., Kilpatrick, D. G., Holmes, M. (2005). Description of an early intervention to
prevent substance abuse and psychopathology in recent rape victims. Behavior Modification, 29, 156–
188.
Reynolds, M., Mezey, G., Chapman, M., Wheeler, M., Drummond, C., & Baldacchino, A. (2005). co-
morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol
Dependence, 77, 251–258.
Richardson, J. D., Elhai, J. D., & Pedlar, D. J. (2006). Association of PTSD and depression with medical
and specialist care utilization in modern peacekeeping veterans in Canada with health-related
disabilities. Journal of Clinical Psychiatry, 67, 1240–1245.
Riggs, D. S., Monson, C. M., Glynn, S. M., & Canterino, J. (2009). Couple and family therapy for adults.
In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD:
1-142 Part 3, Section 1—A Review of the Literature
Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.) (pp. 458–
478). New York: Guilford Press.
Riggs, D. S., Rukstalis, M., Volpicelli, J. R., Kalmanson, D., & Foa, E. B. (2003). Demographic and social
adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol
dependence: Potential pitfalls to PTSD treatment. Addictive Behaviors, 28, 1717–1730.
Roberts, A. L., Austin, S. B., Corliss, H. L., Vandermorris, A. K., & Koenen, K. C. (2010). Pervasive
trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress
disorder. American Journal of Public Health, 100, 2433–2441.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic differences in
exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking
for post-traumatic stress disorder in the United States. Psychological Medicine: A Journal of
Research in Psychiatry and the Allied Sciences, 41, 71–83.
Roberts, A. L., McLaughlin, K. A., Conron, K. J., & Koenen, K. C. (2011). Adulthood stressors, history of
childhood adversity, and risk of perpetration of intimate partner violence. American Journal of
Preventive Medicine, 40, 128–138.
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. (2009a). Multiple session early psychological
interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic
Reviews, CD006869.
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. I. (2009b). Systematic review and meta-analysis
of multiple-session early interventions following traumatic events. American Journal of Psychiatry,
166, 293–301.
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. I. (2010). Early psychological interventions to
treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews, CD007944.
Robinaugh, D. J. & McNally, R. J. (2011). Trauma centrality and PTSD symptom severity in adult
survivors of childhood sexual abuse. Journal of Traumatic Stress, 24, 483–486.
Robjant, K. & Fazel, M. (2010). The emerging evidence for Narrative Exposure Therapy: A review.
Clinical Psychology Review, 30, 1030–1039.
Roht-Arriaza, N. (1995). Punishment, redress, and pardon: Theoretical and psychological approaches. In
N. Roht-Arriaza (Ed.), Impunity and human rights international law and practice. (pp. 13–23).
Oxford, England: Oxford University Press.
Rosenberg, S. D., Lu, W., Mueser, K. T., Jankowski, M. K., & Cournos, F. (2007). Correlates of adverse
childhood events among adults with schizophrenia spectrum disorders. Psychiatric Services, 58, 245–
253.
Rosenthal, J. Z., Grosswald, S., Ross, R., & Rosenthal, N. (2011). Effects of transcendental meditation in
veterans of Operation Enduring Freedom and Operation Iraqi Freedom with posttraumatic stress
disorder: A pilot study. Military Medicine, 176, 626–630.
Rossen, L. M., Pollack, K. M., Canham-Chervak, M., Canada, S., & Baker, S. P. (2011). Motor vehicle
crashes among active duty U.S. Army personnel, 1999 to 2006. Military Medicine, 176, 1019–1026.
Rothbaum, B. O., Davidson, J. R., Stein, D. J., Pedersen, R., Musgnung, J., Tian, X. W. et al. (2008). A
pooled analysis of gender and trauma-type effects on responsiveness to treatment of PTSD with
venlafaxine extended release or placebo. Journal of Clinical Psychiatry, 69, 1529–1539.
Ruef, A. M., Litz, B. T., & Schlenger, W. E. (2000). Hispanic ethnicity and risk for combat-related
posttraumatic stress disorder. Cultural Diversity and Ethnic Minority Psychology, 6, 235–251.
Rush, A. J., Zimmerman, M., Wisniewski, S. R., Fava, M., Hollon, S. D., Warden, D. et al. (2005).
Comorbid psychiatric disorders in depressed outpatients: Demographic and clinical features. Journal
of Affective Disorders, 87, 43–55.
Trauma-Informed Care in Behavioral Health Services 1-143
Ruzek, J., Walser, R. D., Naugle, A. E., Litz, B., Mennin, D. S., Polusny, M. A. et al. (2008). Cognitive–
behavioral psychology: Implications for disaster and terrorism response. Prehospital and Disaster
Medicine, 23, 397–410.
Sacks, J. Y., McKendrick, K., & Banks, S. (2008). The impact of early trauma and abuse on residential
substance abuse treatment outcomes for women. Journal of Substance Abuse Treatment, 34, 90–100.
Sacks, S., McKendrick, K., Sacks, J. Y., Banks, S., & Harle, M. (2008). Enhanced outpatient treatment for
co-occurring disorders: Main outcomes. Journal of Substance Abuse Treatment, 34, 48–60.
Sadler, A. G., Booth, B. M., Cook, B. L., & Doebbeling, B. N. (2003). Factors associated with women’s
risk of rape in the military environment. American Journal of Industrial Medicine, 43, 262–273.
Sala, T., Cox, B. J., & Sareen, J. (2008). Anxiety disorders and physical illness comorbidity: An overview.
In Anxiety in health behaviors and physical illness (pp. 131–154). New York: Springer Science +
Business Media.
Sartor, C. E., McCutcheon, V. V., Pommer, N. E., Nelson, E. C., Grant, J. D., Duncan, A. E. et al. (2011).
Common genetic and environmental contributions to post-traumatic stress disorder and alcohol
dependence in young women. Psychological Medicine, 41, 1497–1505.
Sautter, F. J., Armelie, A. P., Glynn, S. M., & Wielt, D. B. (2011). The development of a couple-based
treatment for PTSD in returning veterans. Professional Psychology: Research and Practice, 42, 63–
69.
Sautter, F. J., Glynn, S. M., Thompson, K. E., Franklin, L., & Han, X. (2009). A couple–based approach to
the reduction of PTSD avoidance symptoms: Preliminary findings. Journal of Marital and Family
Therapy, 35, 343–349.
Savoca, E. & Rosenheck, R. (2000). The civilian labor market experiences of Vietnam-era veterans: The
influence of psychiatric disorders. Journal of Mental Health Policy and Economics, 3, 199–207.
Sayer, N. A., Carlson, K. F., & Schnurr, P. P. (2011). Assessment of functioning and disability. In D. M.
Benedek & G. H. Wynn (Eds.), Clinical manual for management of PTSD (pp. 255–287). Arlington,
VA: American Psychiatric Publishing, Inc.
Sayer, N. A., Noorbaloochi, S., Frazier, P., Carlson, K., Gravely, A., & Murdoch, M. (2010). Reintegration
problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical
care. Psychiatric Services, 61, 589–597.
Schauben, L. J. & Frazier, P. A. (1995). Vicarious trauma: The effects on female counselors of working
with sexual violence survivors. Psychology of Women Quarterly, 19, 49–64.
Schneier, F. R., Neria, Y., Pavlicova, M., Hembree, E., Suh, E. J., Amsel, L. et al. (2012). Combined
prolonged exposure therapy and paroxetine for PTSD related to the World Trade Center attack: a
randomized controlled trial. American Journal of Psychiatry, 169, 80–88.
Schnurr, P. P. & Lunney, C. A. (2011). Work-related quality of life and posttraumatic stress disorder
symptoms among female veterans. Women’s Health Issues, 21, S169–S175.
Schnurr, P. P., Friedman, M. J., Engel, C. C., Foa, E. B., Shea, M. T., Chow, B. K. et al. (2007). Cognitive
behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. JAMA:
The Journal of the American Medical Association, 297, 820–830.
Schnurr, P. P., Friedman, M. J., Foy, D. W., Shea, M. T., Hsieh, F. Y., Lavori, P. W. et al. (2003).
Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a
Department of Veterans Affairs Cooperative Study. Archives of General Psychiatry, 60, 481–489.
Schnurr, P. P., Lunney, C. A., Bovin, M. J., & Marx, B. P. (2009). Posttraumatic stress disorder and
quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical
Psychology Review, 29, 727–735.
1-144 Part 3, Section 1—A Review of the Literature
Schnurr, P. P., Lunney, C. A., Sengupta, A., & Waelde, L. C. (2003). A descriptive analysis of PTSD
chronicity in Vietnam veterans. Journal of Traumatic Stress, 16, 545–553.
Schönenberg, M., Reichwald, U., Domes, G., Badke, A., & Hautzinger, M. (2005). Effects of
peritraumatic ketamine medication on early and sustained posttraumatic stress symptoms in
moderately injured accident victims. Psychopharmacology (Berlin), 182, 420–425.
Schönenberg, M., Reichwald, U., Domes, G., Badke, A., & Hautzinger, M. (2008). Ketamine aggravates
symptoms of acute stress disorder in a naturalistic sample of accident victims. Journal of
Psychopharmacology, 22, 493–497.
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., & Gray, S. H. (2008). Contributions of psychodynamic
approaches to treatment of PTSD and trauma: A review of the empirical treatment and
psychopathology literature. Psychiatry, 71, 13–34.
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., Tendick, V., & Gray, S. H. (2008). Nonresponse and
dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry, 71,
134–168.
Schubert, C. C. & Punamäki, R. L. (2011). Mental health among torture survivors: Cultural background,
refugee status and gender. Nordic Journal of Psychiatry, 65, 175–182.
Schumm, J. A., Briggs-Phillips, M., & Hobfoll, S. E. (2006). Cumulative interpersonal traumas and social
support as risk and resiliency factors in predicting PTSD and depression among inner-city women.
Journal of Traumatic Stress, 19, 825–836.
Schwartz, R. C., Schwartz, M. F., & Galperin, L. (2009). Internal family systems therapy. Internal family
(Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 353–370). New
York: Guilford Press.
Schweitzer, R. D., Brough, M., Vromans, L., & Asic-Kobe, M. (2011). Mental health of newly arrived
Burmese refugees in Australia: Contributions of pre-migration and post-migration experience.
Australian and New Zealand Journal of Psychiatry, 45, 299–307.
Schweitzer, R., Melville, F., Steel, Z., & Lacherez, P. (2006). Trauma, post–migration living difficulties,
and social support as predictors of psychological adjustment in resettled Sudanese refugees.
Australian and New Zealand Journal of Psychiatry, 40, 179–187.
Scott, J. C. (1990). Domination and the arts of resistance: Hidden transcripts. New Haven: Yale
University Press.
Seal, K. H., Metzler, T. J., Gima, K. S., Bertenthal, D., Maguen, S., & Marmar, C. R. (2009). Trends and
risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of
Veterans Affairs health care, 2002–2008. American Journal of Public Health, 99, 1651–1658.
Seidler, G. H. & Wagner, F. E. (2006). Comparing the efficacy of EMDR and trauma-focused cognitive–
behavioral therapy in the treatment of PTSD: a meta-analytic study. Psychological Medicine, 36,
1515–1522.
Shaikh Al Arab, A., Guedon-Moreau, L., Ducrocq, F., Molenda, S., Duhem, S., Salleron, J. et al. (2012).
Temporal analysis of heart rate variability as a predictor of post traumatic stress disorder in road
traffic accidents survivors. Journal of Psychiatric Research.
Shalev, A. Y., Ankri, Y., Israeli–Shalev, Y., Peleg, T., Adessky, R., & Freedman, S. (2012). Prevention of
posttraumatic stress disorder by early treatment: Results from the Jerusalem Trauma Outreach And
Prevention study. Archives of General Psychiatry, 69, 166–176.
Shalev, A. Y., Sahar, T., Freedman, S., Peri, T., Glick, N., Brandes, D. et al. (1998). A prospective study
of heart rate response following trauma and the subsequent development of posttraumatic stress
disorder. Archives of General Psychiatry, 55, 553–559.
Trauma-Informed Care in Behavioral Health Services 1-145
Sharpless, B. A. & Barber, J. P. (2011). A clinician’s guide to PTSD treatments for returning veterans.
Professional Psychology: Research and Practice, 42, 8–15.
Shea, M. T., McDevitt-Murphy, M., Ready, D. J., & Schnurr, P. P. (2009). Group therapy. In E. B. Foa, T.
M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines
from the International Society for Traumatic Stress Studies (2nd ed.) (pp. 306–326). New York:
Guilford Press.
Shemesh, E., Yehuda, R., Milo, O., Dinur, I., Rudnick, A., Vered, Z. et al. (2004). Posttraumatic stress,
nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosomatic Medicine,
66, 521–526.
Sherin, J. E. & Nemeroff, C. B. (2011). Post-traumatic stress disorder: the neurobiological impact of
psychological trauma. Dialogues in Clinical Neuroscience, 13, 263–278.
Sherman, M. D., Zanotti, D. K., & Jones, D. E. (2005). Key elements in couples therapy with veterans with
combat-related posttraumatic stress disorder. Professional Psychology–Research and Practice, 36,
626–633.
Sherrer, M. V. (2011). The role of cognitive appraisal in adaptation to traumatic stress in adults with
serious mental illness: A critical review. Trauma, Violence, & Abuse, 12, 151–167.
Shoptaw, S., Stein, J. A., & Rawson, R. A. (2000). Burnout in substance abuse counselors: Impact of
environment, attitudes, and clients with HIV. Journal of Substance Abuse Treatment, 19, 117–126.
Sijbrandij, M., Olff, M., Reitsma, J. B., Carlier, I. V., & Gersons, B. P. (2006). Emotional or educational
debriefing after psychological trauma. Randomised controlled trial. British Journal of Psychiatry,
189, 150–155.
Silver, R. C., Holman, E. A., McIntosh, D. N., Poulin, M., & Gil-Rivas, V. (2002). Nationwide logitudinal
study of psychological responses to September 11. Journal of the American Medical Association,
288, 1235–1244.
Simon, N. M., Otto, M. W., Wisniewski, S. R., Fossey, M., Sagduyu, K., Frank, E. et al. (2004). Anxiety
disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the
Systematic Treatment Enhancement Program for Bipolar Disorder (STEP–BD). American Journal of
Psychiatry, 161, 2222–2229.
Simpson, T. L. (2002). Women’s treatment utilization and its relationship to childhood sexual abuse
history and lifetime PTSD. Substance Abuse, 23, 17–30.
Skinner, K. M., Kressin, N., Frayne, S., Tripp, T. J., Hankin, C. S., Miller, D. R. et al. (2000). The
prevalence of military sexual assault among female Veterans’ Administration outpatients. Journal of
Interpersonal Violence, 15, 291–310.
Skopp, N. A., Reger, M. A., Reger, G. M., Mishkind, M. C., Raskind, M., & Gahm, G. A. (2011). The role
of intimate relationships, appraisals of military service, and gender on the development of
posttraumatic stress symptoms following Iraq deployment. Journal of Traumatic Stress, 24, 277–286.
Sledjeski, E. M., Speisman, B., & Dierker, L. C. (2008). Does number of lifetime traumas explain the
relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity
Survey–Replication (NCS–R). Journal of Behavioral Medicine, 31, 341–349.
Smid, G. E., Mooren, T. T., van der Mast, R. C., Gersons, B. P., & Kleber, R. J. (2009). Delayed
posttraumatic stress disorder: Systematic review, meta-analysis, and meta-regression analysis of
prospective studies. Journal of Clinical Psychiatry, 70, 1572–1582.
Smid, G. E., van der Velden, P. G., Gersons, B. P. R., & Kleber, R. J. (2012). Late-onset posttraumatic
stress disorder following a disaster: A longitudinal study. Psychological Trauma: Theory, Research,
Practice, and Policy, 4, 312–322.
1-146 Part 3, Section 1—A Review of the Literature
Smid, G. E., van der Velden, P. G., Lensvelt–Mulders, G. J., Knipscheer, J. W., Gersons, B. P., & Kleber,
R. J. (2011). Stress sensitization following a disaster: A prospective study. Psychological Medicine,
1–12.
Smith, M. W., Schnurr, P. P., & Rosenheck, R. A. (2005). Employment outcomes and PTSD symptom
severity. Mental Health Services Research, 7, 89–101.
Solomon, Z., Dekel, R., & Mikulincer, M. (2008). Complex trauma of war captivity: A prospective study
of attachment and post-traumatic stress disorder. Psychological Medicine: A Journal of Research in
Psychiatry and the Allied Sciences, 38, 1427–1434.
Söndergaard, H. P. & Theorell, T. (2004). Language acquisition in relation to cumulative posttraumatic
stress disorder symptom load over time in a sample of re-settled refugees. Psychotherapy and
Psychosomatics, 73, 320–323.
Sotero, M. (2006). A conceptual model of historical trauma: Implications for public health practice and
research. Journal of Health Disparities Research and Practice, 1, 93–108.
Spataro, J., Mullen, P. E., Burgess, P. M., Wells, D. L., & Moss, S. A. (2004). Impact of child sexual abuse
on mental health: Prospective study in men and women. British Journal of Psychiatry, 184, 416–421.
Spates, C. R., Koch, E., Cusack, K., Pagoto, S., & Waller, S. (2009). Eye movement desensitization and
reprocessing. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments
for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.)
(pp. 279–305). New York: Guilford Press.
Spauwen, J., Krabbendam, L., Lieb, R., Wittchen, H. U., & van Os, J.,(2006). Impact of psychological
trauma on the development of psychotic symptoms: Relationship with psychosis proneness. British
Journal of Psychiatry, 188, 527–533.
Spitzer, R. L., Williams, J. B., & Gibbon, M. (1987). Structured clinical interview for DSM-III-R—Patient
version (SCID-P). New York: New York State Psychiatric Institute, Biometrics Research.
Steel, J. L., Dunlavy, A. C., Stillman, J., & Pape, H. C. (2011). Measuring depression and PTSD after
trauma: Common scales and checklists. Injury, 42, 288–300.
Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van, O. M. (2009). Association of torture and
other potentially traumatic events with mental health outcomes among populations exposed to mass
conflict and displacement: A systematic review and meta-analysis. JAMA, 302, 537–549.
Steil, R., Jung, K., & Stangier, U. (2011). Efficacy of a two-session program of cognitive restructuring and
imagery modification to reduce the feeling of being contaminated in adult survivors of childhood
sexual abuse: a pilot study. Journal of Behavior Therapy and Experimental Psychiatry, 42, 325–329.
Stein, D. J., Chiu, W. T., Hwang, I., Kessler, R. C., Sampson, N., Alonso, J. et al. (2010). Cross-national
analysis of the associations between traumatic events and suicidal behavior: Findings from the WHO
World Mental Health Surveys. PLoS ONE, 5.
Stein, D. J., Ipser, J. C., & Seedat, S. (2006). Pharmacotherapy for post traumatic stress disorder (PTSD).
Cochrane Database of Systematic Reviews, CD002795.
Stein, D. J., Ipser, J., & McAnda, N. (2009). Pharmacotherapy of posttraumatic stress disorder: A review
of meta-analyses and treatment guidelines. CNS Spectr., 14, 25–31.
Stein, M. B., Walker, J. R., Hazen, A. L., & Forde, D. R. (1997). Full and partial posttraumatic stress
disorder: Findings from a community survey. American Journal of Psychiatry, 154, 1114–1119.
Stewart, R. E. & Chambless, D. L. (2009). Cognitive–behavioral therapy for adult anxiety disorders in
clinical practice: a meta-analysis of effectiveness studies. Journal of Consulting and Clinical
Psychology, 77, 595–606.
Stinson, F. S., Dawson, D. A., Goldstein, R. B., Chou, S. P., Huang, B., Smith, S. M. et al. (2008).
Prevalence, correlates, disability, and comorbidity of DSM-IV narcissistic personality disorder:
Trauma-Informed Care in Behavioral Health Services 1-147
results from the wave 2 national epidemiologic survey on alcohol and related conditions. Journal of
Clinical Psychiatry, 69, 1033–1045.
Subcommittee on Posttraumatic Stress Disorder of the Committee on Gulf War and Health: Physiologic,
Psychologic, and Psychosocial Effects of Deployment-Related Stress (2006). Posttraumatic stress
disorder: Diagnosis and assessment. Washington, DC: The National Academies Press.
Substance Abuse and Mental Health Services Administration. (2013b). Behavioral health services for
people who are homeless. Treatment Improvement Protocol (TIP) Series 55. (HHS Publication No.
SMA 13-4734). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned c). Improving cultural competence.
Treatment Improvement Protocol (TIP) Series. Rockville, MD: Substance Abuse and Mental Health
Services Administration.
Substance Abuse and Mental Health Services Administration. (planned d). Managing anxiety symptoms in
behavioral health services. Treatment Improvement Protocol (TIP) Series. Rockville, MD: Substance
Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned f). Reintegration-related
behavioral health issues in veterans and military families. Treatment Improvement Protocol (TIP)
Series. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration & Office of Applied Studies (2008). Impact
of hurricanes Katrina and Rita on substance use and mental health. The NSDUH Report. Rockville,
MD: Substance Abuse and Mental Health Services Administration and Office of Applied Studies.
Substance Abuse and Mental Health Services Administration, Trauma and Justice Strategic Initiative
(2012). SAMHSA's working definition of trauma and guidance for trauma-informed approach.
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Sudaryo, M. K., Besral, Endarti, A. T., Rivany, R., Phalkey, R., Marx, M. et al. (2012). Injury, disability
and quality of life after the 2009 earthquake in Padang, Indonesia: A prospective cohort study of adult
survivors. Global Health Action, 5.
Sullivan, P. M. & Knutson, J. F. (2000). Maltreatment and disabilities: A population-based
epidemiological study. Child Abuse & Neglect, 24, 1257–1273.
Suris, A., Lind, L., Kashner, T. M., & Borman, P. D. (2007). Mental health, quality of life, and health
functioning in women veterans: Differential outcomes associated with military and civilian sexual
assault. Journal of Interpersonal Violence, 22, 179–197.
Swinbourne, J. M. & Touyz, S. W. (2007). The co-morbidity of eating disorders and anxiety disorders: A
review. European Eating Disorders Review, 15, 253–274.
Taft, C. T., Vogt, D. S., Mechanic, M. B., & Resick, P. A. (2007). Posttraumatic stress disorder and
physical health symptoms among women seeking help for relationship aggression. Journal of Family
Psychology, 21, 354–362.
Tam, T. W., Zlotnick, C., & Robertson, M. J. (2003). Longitudinal perspective: Adverse childhood events,
substance use, and labor force participation among homeless adults. American Journal of Drug and
Alcohol Abuse, 29, 829–846.
Tanielian, T. L., Jaycox, L. H., Schell, T. L., Marshall, G. N., Burnam, M. A., Eibner, C. et al. (2008).
Invisible wounds of war: Summary and recommendations for addressing psychological and cognitive
injuries. Santa Monica: RAND.
Taylor, B., Irving, H. M., Kanteres, F., Room, R., Borges, G., Cherpitel, C. et al. (2010). The more you
drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption
and injury or collision risk increase together. Drug and Alcohol Dependence, 110, 108–116.
1-148 Part 3, Section 1—A Review of the Literature
Teplin, L. A., McClelland, G. M., Abram, K. M., & Weiner, D. A. (2005). Crime victimization in adults
with severe mental illness: Comparison with the national crime victimization survey. Archives of
General Psychiatry, 62, 911–921.
Terrio, H. P., Nelson, L. A., Betthauser, L. M., Harwood, J. E., & Brenner, L. A. (2011). Postdeployment
traumatic brain injury screening questions: Sensitivity, specificity, and predictive values in returning
soldiers. Rehabilitation Psychology, 56, 26–31.
The APSAC handbook on child maltreatment (2nd ed.) (2002). Thousand Oaks, CA: Sage Publications,
Inc.
Thompson, M. P. & Kingree, J. B. (1998). The frequency and impact of violent trauma among pregnant
substance abusers. Addictive Behaviors, 23, 257–262.
Thorp, S. R. & Stein, M. B. (2005). Posttraumatic stress disorder and functioning. PTSD Research
Quarterly, 16, 1–7.
Tjaden, P. & Thoennes, N. (2000). Extent, nature, and consequences of intimate partner violence.
Findings from the National Violence Against Women Survey. Washington, DC: U.S. Department of
Justice, Office of Justice Programs.
Torchalla, I., Nosen, L., Rostam, H., & Allen, P. (2012). Integrated treatment programs for individuals
with concurrent substance use disorders and trauma experiences: A systematic review and meta-
analysis. Journal of Substance Abuse Treatment, 42, 65–77.
Treating Compassion Fatigue (2002). New York: Brunner-Routledge.
Triffleman, E. (2000). Gender differences in a controlled pilot study of psychosocial treatment in
substance dependent patients with post-traumatic stress disorder: Design considerations and
outcomes. Alcoholism Treatment Quarterly, 18, 113–126.
Triffleman, E. (2002). Implementing substance dependence posttraumatic stress disorder therapy in a
community-based methadone clinic. In J. L. Sorensen, R. A. Rawson, J. Guydish, & J. E. Zweben
(Eds.), Research to practice, practice to research: Promoting scientific clinical interchange in drug
abuse treatment. (pp. 227–248). Washington, DC: American Psychological Association.
Triffleman, E. G., Marmar, C. R., Delucchi, K. L., & Ronfeldt, H. (1995). Childhood trauma and
posttraumatic stress disorder in substance abuse inpatients. Journal of Nervous & Mental Disease,
183, 172–176.
Trippany, R. L., Kress, V. E. W., & Wilcoxon, S. A. (2004). Preventing vicarious trauma: What counselors
should know when working with trauma survivors. Journal of Counseling & Development, 82, 31–
37.
Trippany, R. L., Wilcoxon, S. A., & Satcher, J. F. (2003). Factors influencing vicarious traumatization for
therapists of survivors of sexual victimization. Journal of Trauma Practice, 2, 47–60.
Truman, J. L. (2011). Criminal victimization, 2010. Washington, DC: U.S. Department of Justice, Bureau
of Justice Statistics.
Tull, M. T., Gratz, K. L., Aklin, W. M., & Lejuez, C. W. (2010). A preliminary examination of the
relationships between posttraumatic stress symptoms and crack/cocaine, heroin, and alcohol
dependence. Journal of Anxiety Disorders, 24, 55–62.
Turnbull, G. J. (1998). A review of post-traumatic stress disorder; part I: Historical development and
classification. Injury, 29, 87–91.
Ullman, S. E. & Filipas, H. H. (2001). Predictors of PTSD symptom severity and social reactions in sexual
assault victims. Journal of Traumatic Stress, 14, 369–389.
Ullman, S. E., Filipas, H. H., Townsend, S. M., & Starzynski, L. L. (2007). Psychosocial correlates of
PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress, 20, 821–831.
Trauma-Informed Care in Behavioral Health Services 1-149
Ulmer, C. S., Edinger, J. D., & Calhoun, P. S. (2011). A multi-component cognitive–behavioral
intervention for sleep disturbance in veterans with PTSD: A pilot study. Journal of Clinical Sleep
Medicine, 7, 57–68.
U.S. Department of Veterans Affairs & Department of Defense (2010). VA/DoD clinical practice guideline
for management of post-traumatic stress. Washington, DC: U. S. Department of Veterans Affairs.
Valentiner, D. P., Foa, E. B., Riggs, D. S., & Gershuny, B. S. (1996). Coping strategies and posttraumatic
stress disorder in female victims of sexual and nonsexual assault. Journal of Abnormal Psychology,
105, 455–458.
Van Breda, A. D. (2001). Resilience theory: A literature review. Gezina, South Africa: South African
Military Health Service, Military Psychological Institute, Social Work Research & Development.
van der Kolk, B. A., McFarlane, A. C., & Van der Hart, O. (1996). A general approach to treatment of
posttraumatic stress disorder. In B. A. van der Kolk, A. C. McFarlane, & L. Weisaeth (Eds.),
Traumatic stress: The effects of overwhelming experience on mind, body, and society (pp. 417–440).
New York: Guilford Press.
van der Kolk, B. A., McFarlane, A. C., & Weisaeth, L. (1996). Traumatic stress: The effects of
overwhelming experience on mind, body, and society. New York: Guilford Press.
van der Velden, P. G. & Wittmann, L. (2008). The independent predictive value of peritraumatic
dissociation for PTSD symptomatology after type I trauma: A systematic review of prospective
studies. Clinical Psychology Review, 28, 1009–1020.
Van Emmerik, A. A. P., Kamphuis, J. H., Hulsbosch, A. M., & Emmelkamp, P. M. G. (2002). Single
session debriefing after psychological trauma: a meta-analysis. Lancet, 360, 766–771.
Vasterling, J. J., Verfaellie, M., & Sullivan, K. D. (2009). Mild traumatic brain injury and posttraumatic
stress disorder in returning veterans: Perspectives from cognitive neuroscience. Clinical Psychology
Review, 29, 674–684.
Vaughn, M. G., Fu, Q., DeLisi, M., Beaver, K. M., Perron, B. E., & Howard, M. O. (2010). Criminal
victimization and comorbid substance use and psychiatric disorders in the United States: Results from
the NESARC. Annals of Epidemiology, 20, 281–288.
Verschuur, M. J., Maric, M., & Spinhoven, P. (2010). Differences in changes in health-related anxiety
between Western and non-Western participants in a trauma-focused study. Journal of Traumatic
Stress, 23, 300–303.
Vest, J. R., Catlin, T. K., Chen, J. J., & Brownson, R. C. (2002). Multistate analysis of factors associated
with intimate partner violence. American Journal of Preventive Medicine, 22, 156–164.
Vickerman, K. A. & Margolin, G. (2009). Rape treatment outcome research: Empirical findings and state
of the literature. Clinical Psychology Review, 29, 431–448.
Villagonzalo, K. A., Dodd, S., Ng, F., Mihaly, S., Langbein, A., & Berk, M. (2011). The relationship
between substance use and posttraumatic stress disorder in a methadone maintenance treatment
program. Comprehensive Psychiatry, 52, 562–566.
Vlahov, D., Galea, S., Ahern, J., Resnick, H., & Kilpatrick, D. (2004). Sustained increased consumption of
cigarettes, alcohol, and marijuana among Manhattan residents after September 11, 2001. American
Journal of Public Health, 94, 253–254.
Vogt, D. S. & Tanner, L. R. (2007). Risk and resilience factors for posttraumatic stress symptomatology in
Gulf War I veterans. Journal of Traumatic Stress, 20, 27–38.
Vogt, D. S., King, D. W., & King, L. A. (2007). Risk pathways for PTSD: Making sense of the literature.
In M. J. Friedman, T. M. Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice
(pp. 99–115). New York: Guilford Press.
1-150 Part 3, Section 1—A Review of the Literature
Vogt, D. S., Pless, A. P., King, L. A., & King, D. W. (2005). Deployment stressors, gender, and mental
health outcomes among Gulf War I veterans. Journal of Traumatic Stress, 18, 272–284.
Walker, R. L., Clark, M. E., & Sanders, S. H. (2010). The postdeployment multi-symptom disorder: An
emerging syndrome in need of a new treatment paradigm. Psychological Services, 7, 136–147.
Walser, R. D. & Westrup, D. (2007). Acceptance & commitment therapy for the treatment of post-
traumatic stress disorder & trauma-related problems: A practitioner’s guide to using mindfulness &
acceptance strategies. Oakland, CA: New Harbinger Publications.
Walsh, F. (2007). Traumatic Loss and Major Disasters: Strengthening Family and Community Resilience.
Family Process, 46, 207–227.
Walter, K. H., Horsey, K. J., Palmieri, P. A., & Hobfoll, S. E. (2010). The role of protective self-cognitions
in the relationship between childhood trauma and later resource loss. Journal of Traumatic Stress, 23,
264–273.
Wan, J. J., Morabito, D. J., Khaw, L., Knudson, M. M., & Dicker, R. A. (2006). Mental illness as an
independent risk factor for unintentional injury and injury recidivism. Journal of Trauma, 61, 1299–
1304.
Weathers, F. W., Keane, T. M., & Foa, E. B. (2009). Assessment and diagnosis of adults. In E. B. Foa, T.
M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines
from the International Society for Traumatic Stress Studies (2nd ed.) (pp. 23–61). New York:
Guilford Press.
Weine, S., Danieli, Y., Silove, D., Ommeren, M. V., Fairbank, J. A., & Saul, J. (2002). Guidelines for
international training in mental health and psychosocial interventions for trauma exposed populations
in clinical and community settings. Psychiatry, 65, 156–164.
Weine, S., Kulauzovic, Y., Klebic, A., Besic, S., Mujagic, A., Muzurovic, J. et al. (2008). Evaluating a
multiple-family group access intervention for refugees with PTSD. Journal of Marital and Family
Therapy, 34, 149–164.
Weissbecker, I. & Clark, C. (2007). The impact of violence and abuse on womens physical health: Can
trauma-informed treatment make a difference? Journal of Community Psychology, 35, 909–923.
Wenzel, S. L., Tucker, J. S., Elliott, M. N., Hambarsoomians, K., Perlman, J., Becker, K. et al. (2004).
Prevalence and co-occurrence of violence, substance use and disorder, and HIV risk behavior: a
comparison of sheltered and low-income housed women in Los Angeles County. Preventive
Medicine, 39, 617–624.
Wessely, S., Bryant, R. A., Greenberg, N., Earnshaw, M., Sharpley, J., & Hughes, J. H. (2008). Does
psychoeducation help prevent posttraumatic psychological distress? Psychiatry: Interpersonal and
Biological Processes, 71, 287–302.
Westermeyer, J., Hollifield, M., Spring, M., Johnson, D., & Jaranson, J. (2011). Comparison of two
methods of inquiry for torture with East African refugees: Single query versus checklist. Torture., 21,
155–172.
Westphal, M., Olfson, M., Gameroff, M. J., Wickramaratne, P., Pilowsky, D. J., Neugebauer, R. et al.
(2011). Functional impairment in adults with past posttraumatic stress disorder: findings from
primary care. Depression and Anxiety, 28, 686–695.
Whitbeck, L. B., Chen, X., Hoyt, D. R., & Adams, G. W. (2004). Discrimination, historical loss and
enculturation: Culturally specific risk and resiliency factors for alcohol abuse among American
Indians. Journal of Studies on Alcohol, 65, 409–418.
Whitfield, C. L., Anda, R. F., Dube, S. R., & Felitti, V. J. (2003). Violent childhood experiences and the
risk of intimate partner violence in adults: Assessment in a large health maintenance organization.
Journal of Interpersonal Violence, 18, 166–185.
Trauma-Informed Care in Behavioral Health Services 1-151
Widom, C. S. & Morris, S. (1997). Accuracy of adult recollections of childhood victimization, Part 2:
Childhood sexual abuse. Psychological Assessment, 9, 34–46.
Wilcox, J., Briones, D., & Suess, L. (1991). Auditory hallucinations, posttraumatic stress disorder, and
ethnicity. Comprehensive Psychiatry, 32, 320–323.
Wilkinson, D. M., Blacker, S. D., Richmond, V. L., Horner, F. E., Rayson, M. P., Spiess, A. et al. (2011).
Injuries and injury risk factors among British army infantry soldiers during predeployment training.
Injury Prevention, 17, 381–387.
Williams, L. M. (1994). Recall of childhood trauma: A prospective study of women’s memories of child
sexual abuse. Journal of Consulting and Clinical Psychology, 62, 1167–1176.
Wilson, J. P. (2007). The lens of culture: Theoretical and conceptual perspectives in the assessment of
psychological trauma and PTSD. In J. P. Wilson & C. S. Tang (Eds.), Cross–cultural assessment of
psychological trauma and PTSD (pp. 3–30). New York: Springer Science + Business Media.
Wingo, A. P., Wrenn, G., Pelletier, T., Gutman, A. R., Bradley, B., & Ressler, K. J. (2010). Moderating
effects of resilience on depression in individuals with a history of childhood abuse or trauma
exposure. Journal of Affective Disorders, 126, 411–414.
Woodward, A. T., Taylor, R. J., Bullard, K. M., Aranda, M. P., Lincoln, K. D., & Chatters, L. M. (2011).
Prevalence of lifetime DSM-IV affective disorders among older African Americans, Black
Caribbeans, Latinos, Asians and Non-Hispanic White people. International Journal of Geriatric
Psychiatry.
World Health Organization (1979). International statistical classification of diseases and related health
problems. (9th revision ed.) Geneva, Switzerland: World Health Organization.
Wrenn, G. L., Wingo, A. P., Moore, R., Pelletier, T., Gutman, A. R., Bradley, B. et al. (2011). The effect
of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients.
Journal of the National Medical Association, 103, 560–566.
Xian, H., Chantarujikapong, S. I., Scherrer, J. F., Eisen, S. A., Lyons, M. J., Goldberg, J. et al. (2000).
Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence
in twin pairs. Drug and Alcohol Dependence, 61, 95–102.
Xie, Y. & Greenman, E. (2005). Research report: Segmented assimilation theory: A reformulation and
empirical test. Ann Arbor, MI: University of Michigan.
Yehuda, R., Halligan, S. L., & Bierer, L. M. (2001). Relationship of parental trauma exposure and PTSD
to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research, 35, 261–
270.
Yehuda, R., Halligan, S. L., & Grossman, R. (2001). Childhood trauma and risk for PTSD: Relationship to
intergenerational effects of trauma, parental PTSD, and cortisol excretion. Development and
Psychopathology, 13, 733–753.
Yellow Horse, S. & Brave Heart, M. Y. H. (2005). Chapter 3: Native American children. Colorado
Springs, CO: White Bison, Inc.
Yoder, M., Tuerk, P. W., Price, M., Grubaugh, A. L., Strachan, M., Myrick, H. et al. (2012). Prolonged
exposure therapy for combat-related posttraumatic stress disorder: Comparing outcomes for veterans
of different wars. Psychol. Serv., 9, 16–25.
Young, B. H. (2006). The immediate response to disaster: Guidelines for adult psychological first aid. In
E. C. Ritchie, P. J. Watson, & M. J. Friedman (Eds.), Interventions following mass violence and
disasters: Strategies for mental health practice (pp. 134–154). New York: Guilford Press.
Yuan, C., Wang, Z., Inslicht, S. S., McCaslin, S. E., Metzler, T. J., Henn-Haase, C. et al. (2011). Protective
factors for posttraumatic stress disorder symptoms in a prospective study of police officers.
Psychiatry Research, 188, 45–50.
1-152 Part 3, Section 1—A Review of the Literature
Zatzick, D., Roy-Byrne, P., Russo, J., Rivara, F., Droesch, R., Wagner, A., Dunn, C , Jurkovich, G.,
Uehara, E., & Katon, W. (2004). A randomized effectiveness trial of stepped collaborative care for
acutely injured trauma survivors. Archives of General Psychiatry, 61, 498–506.
Zayfert, C. & DeViva, J. C. (2010). Avoiding treatment failures in PTSD. In Avoiding treatment failures in
the anxiety disorders (pp. 147–168). New York: Springer Science + Business Media.
Zivin, K., Bohnert, A. S. B., Mezuk, B., Ilgen, M. A., Welsh, D., Ratliff, S. et al. (2011). Employment
status of patients in the VA health system: Implications for mental health services. Psychiatric
Services, 62, 35–38.
Zohar, J., Fostick, L., Cohen, A., Bleich, A., Dolfin, D., Weissman, Z. et al. (2009). Risk factors for the
development of posttraumatic stress disorder following combat trauma: A semiprospective study.
Journal of Clinical Psychiatry, 70, 1629–1635.
Zohar, J., Juven-Wetzler, A., Sonnino, R., Cwikel-Hamzany, S., Balaban, E., & Cohen, H. (2011). New
insights into secondary prevention in post-traumatic stress disorder. Dialogues in Clinical
Neuroscience, 13, 301–309.
Zohar, J., Sonnino, R., Juven-Wetzler, A., & Cohen, H. (2009). Can posttraumatic stress disorder be
prevented? CNS Spectrums, 14, 44–51.
Zweig, J. M., Yahner, J., & Rossman, S. B. (2012). Does recent physical and sexual victimization affect
further substance use for adult drug-involved offenders? Journal of Interpersonal Violence.
Trauma-Informed Care in Behavioral Health Services 1-153
Appendix—Methodology
Some of the sources cited in the Treatment Improvement Protocol (TIP) Trauma-Informed Care
in Behavioral Health Services were suggested early on in the TIP’s development by consensus
panel members, reviewers, and consultants working together with staff members of the
Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) Knowledge
Application Program (KAP) staff. More recently, broad searches were conducted to find research
from the past 10 years involving trauma and behavioral health (including both mental health and
substance abuse) as well as posttraumatic stress disorder (PTSD) and acute stress disorder.
At various times during the development of the TIP, searches on specific topics were conducted
per the requests of SAMHSA staff and/or reviewers of the TIP. Early searches focused on
trauma/PTSD and September 11, 2001, trauma/PTSD and Hurricane Katrina, trauma/PTSD and
motivational interviewing, and historical trauma. Later in the TIP’s development, additional
searches were conducted using the American Psychological Association’s PsychNet databases,
the National Library of Medicine’s PubMed database, and, occasionally, Elsevier’s Scopus
database as needed on topics such as:
Trauma-informed care.
Trauma teams.
Stockholm syndrome/traumatic bonding.
Vicarious trauma.
Compassion fatigue and trauma.
Environmental safety and trauma/PTSD.
Sleep disorders and trauma.
Ecological models and trauma.
Psychological trauma/PTSD and quality of life.
Psychological trauma/PTSD and culture.
Trauma and health disparities.
Trauma and rural health.
Psychological trauma and torture.
Recovered memories.
Adverse childhood experiences/child abuse.
Assessment and psychological trauma/PTSD.
Trauma and mood disorders.
Trauma and anxiety disorders (excluding PTSD).
Trauma and personality disorders.
Trauma and eating disorders.
Trauma and substance use disorders.
Trauma and schizophrenia.
Self-harm/suicidality and trauma.
Trauma and psychological first aid.
1-154 Part 3, Section 1—A Review of the Literature
Acute stress disorder/PTSD and prevention.
Family therapy and trauma.
Group therapy and trauma.
Cognitive–behavioral therapy and PTSD.
Eye movement desensitization and PTSD.
Exposure therapy and PTSD.
Pharmacotherapy/medication and PTSD.
Searches were generally conducted by the author of the literature review; abstracts were typically
reviewed online by the TIP’s Expert Content Director, who then requested copies of promising
citations. Relevant articles were reviewed by the writer in consultation with the KAP Senior
Researcher and Applied Psychologist.
When available, review articles were acquired first and used to summarize older literature.
Review articles as well as other articles that were retrieved suggested further promising or
seminal literature, which was also obtained. In addition, Internet searches were conducted for
relevant literature available from government and nongovernmental sources.

Trauma-Informed Care in Behavioral Health Services 2-1
Section 2—Links to Select Abstracts
Afifi, T. O., Asmundson, G. J. G., Taylor, S., & Jang, K. L. (2010). The role of genes and
environment on trauma exposure and posttraumatic stress disorder symptoms: A review of
twin studies. Clinical Psychology Review, 30, 101–112. Click here to view abstract.
Agaibi, C. E. & Wilson, J. P. (2005). Trauma, PTSD, and resilience: A review of the literature.
Trauma, Violence, & Abuse, 6, 195–216. Click here to view abstract.
Agorastos, A., Marmar, C. R., & Otte, C. (2011). Immediate and early behavioral interventions
for the prevention of acute and posttraumatic stress disorder. Current Opinion in Psychiatry,
24, 526–532. Click here to view abstract.
Benish, S. G., Imel, Z. E., & Wampold, B. E. (2008). The relative efficacy of bona fide
psychotherapies for treating post–traumatic stress disorder: A meta-analysis of direct
comparisons. Clinical Psychology Review, 28, 746–758. Click here to view abstract.
Ben-Zur, H. (2008). Personal resources of mastery–optimism, and communal support beliefs, as
predictors of posttraumatic stress in uprooted Israelis. Anxiety Stress Coping, 21, 295–307.
Click here to view abstract.
Bisson, J. I., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007).
Psychological treatments for chronic post–traumatic stress disorder: Systematic review and
meta-analysis. British Journal of Psychiatry, 190, 97–104. Click here to view abstract.
Breslau, N., Davis, C., Peterson, E. L., & Schultz, L. (2000). A second look at comorbidity in
victims of trauma: The posttraumatic stress disorder–major depression connection. Biological
Psychiatry, 48, 902–909. Click here to view abstract.
Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for
posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical
Psychology, 68, 748–766. Click here to view abstract.
Bryant, R. A., Moulds, M. L., Guthrie, R. M., Dang, S. T., Mastrodomenico, J., Nixon, R. D. et
al. (2008). A randomized controlled trial of exposure therapy and cognitive restructuring for
posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 76, 695–703.
Click here to view abstract.
Cahill, S. P., Foa, E. B., Hembree, E. A., Marshall, R. D., & Nacash, N. (2006). Dissemination of
exposure therapy in the treatment of posttraumatic stress disorder. Journal of Traumatic
Stress, 19, 597– 610. Click here to view abstract.
Chen, L. P., Murad, M. H., Paras, M. L., Colbenson, K. M., Sattler, A. L., Goranson, E. N. et al.
(2010). Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and
meta-analysis. Mayo Clinic Proceedings, 85, 618–629. Click here to view abstract.
Cloitre, M. (2009). Effective psychotherapies for posttraumatic stress disorder: A review and
critique. CNS Spectrums, 14, 32–43. Click here to view abstract.

2-2 Part 3, Section 2—Links to Select Abstracts
Cloitre, M., Courtois, C. A., Charuvastra, A., Carapezza, R., Stolbach, B. C., & Green, B. L.
(2011). Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best
practices. Journal of Traumatic Stress, 24, 615–627.Click here to view abstract.
Cloitre, M., Stovall-McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L. et al.
(2010). Treatment for PTSD related to childhood abuse: A randomized controlled trial.
American Journal of Psychiatry, 167, 915–924. Click here to view abstract.
Coker, A. L., Weston, R., Creson, D. L., Justice, B., & Blakeney, P. (2005). PTSD symptoms
among men and women survivors of intimate partner violence: The role of risk and
protective factors. Violence and Victims, 20, 625–643. Click here to view abstract.
Collimore, K. C., Carleton, R. N., Hofmann, S. G., & Asmundson, G. J. G. (2010). Posttraumatic
stress and social anxiety: The interaction of traumatic events and interpersonal fears.
Depression and Anxiety, 27, 1017–1026. Click here to view abstract.
Cougle, J. R., Feldner, M. T., Keough, M. E., Hawkins, K. A., & Fitch, K. E. (2010). Comorbid
panic attacks among individuals with posttraumatic stress disorder: Associations with
traumatic event exposure history, symptoms, and impairment. Journal of Anxiety Disorders,
24, 183–188. Click here to view abstract.
Cukor, J., Spitalnick, J., Difede, J., Rizzo, A., & Rothbaum, B. O. (2009). Emerging treatments
for PTSD. Clinical Psychology Review, 29, 715–726. Click here to view abstract.
Dass-Brailsford, P. & Myrick, A. C. (2010). Psychological trauma and substance abuse: The need
for an integrated approach. Trauma, Violence, & Abuse, 11, 202–213. Click here to view
abstract.
Difede, J., Malta, L. S., Best, S., Henn-Haase, C., Metzler, T., Bryant, R. et al. (2007). A
randomized controlled clinical treatment trial for World Trade Center attack–related PTSD in
disaster workers. Journal of Nervous and Mental Disease, 195, 861–865. Click here to view
abstract.
DiGrande, L., Neria, Y., Brackbill, R. M., Pulliam, P., & Galea, S. (2011). Long–term
posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001,
terrorist attacks on the World Trade Center. American Journal of Epidemiology, 173, 271–
281. Click here to view abstract.
Domino, M. E., Morrissey, J. P., Chung, S., Huntington, N., Larson, M. J., & Russell, L. A.
(2005). Service use and costs for women with co-occurring mental and substance use
disorders and a history of violence. Psychiatric Services, 56, 1223–1232. Click here to view
abstract.
Drogendijk, A. N., van der Velden, P. G., & Kleber, R. J. (2012). Acculturation and post-disaster
mental health problems among affected and non–affected immigrants: A comparative study.
Journal of Affective Disorders, 138, 485–489. Click here to view abstract.
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001).
Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the
life span: Findings from the adverse childhood experiences study. JAMA: The Journal of the
American Medical Association, 286, 3089–3096. Click here to view abstract.

Trauma-Informed Care in Behavioral Health Services 2-3
Dube, S. R., Anda, R. F., Whitfield, C. L., Brown, D. W., Felitti, V. J., Dong, M. et al. (2005).
Long-term consequences of childhood sexual abuse by gender of victim. American Journal
of Preventive Medicine, 28, 430–438. Click here to view abstract.
Ehlers, A., Bisson, J., Clark, D. M., Creamer, M., Pilling, S., Richards, D. et al. (2010). Do all
psychological treatments really work the same in posttraumatic stress disorder? Clinical
Psychology Review, 30, 269–276. Click here to view abstract.
Elwood, L. S., Mott, J., Lohr, J. M., & Galovski, T. E. (2011). Secondary trauma symptoms in
clinicians: A critical review of the construct, specificity, and implications for trauma–focused
treatment. Clinical Psychology Review, 31, 25–36. Click here to view abstract.
Falsetti, S. A., Resnick, H. S., & Davis, J. L. (2008). Multiple channel exposure therapy for
women with PTSD and comorbid panic attacks. Cognitive Behaviour Therapy, 37, 117–130.
Click here to view abstract.
Farley, M., Golding, J. M., Young, G., Mulligan, M., & Minkoff, J. R. (2004). Trauma history
and relapse probability among patients seeking substance abuse treatment. Journal of
Substance Abuse Treatment, 27, 161–167. Click here to view abstract.
Felmingham, K. L. & Bryant, R. A. (2012). Gender differences in the maintenance of response to
cognitive behavior therapy for posttraumatic stress disorder. Journal of Consulting and
Clinical Psychology, 80, 196–200. Click here to view abstract.
Fetzner, M. G., McMillan, K. A., Sareen, J., & Asmundson, G. J. (2011). What is the association
between traumatic life events and alcohol abuse/dependence in people with and without
PTSD? Findings from a nationally representative sample. Depression and Anxiety, 28, 632–
638. Click here to view abstract.
Foa, E. B., Zoellner, L. A., & Feeny, N. C. (2006). An evaluation of three brief programs for
facilitating recovery after assault. Journal of Traumatic Stress, 19, 29–43. Click here to view
abstract.
Geraerts, E., Schooler, J. W., Merckelbach, H., Jelicic, M., Hauer, B. J., & Ambadar, Z. (2007).
The reality of recovered memories: Corroborating continuous and discontinuous memories of
childhood sexual abuse. Psychological Science, 18, 564–568. Click here to view abstract.
Gillespie, C. F., Bradley, B., Mercer, K., Smith, A. K., Conneely, K., Gapen, M. et al. (2009).
Trauma exposure and stress–related disorders in inner city primary care patients. General
Hospital Psychiatry, 31, 505–514. Click here to view abstract.
Goldmann, E., Aiello, A., Uddin, M., Delva, J., Koenen, K., Gant, L. M. et al. (2011). Pervasive
exposure to violence and posttraumatic stress disorder in a predominantly African American
Urban Community: The Detroit neighborhood health study. Journal of Traumatic Stress, 24,
747–751. Click here to view abstract.
Goodman, G. S., Ghetti, S., Quas, J. A., Edelstein, R. S., Alexander, K. W., Redlich, A. D. et al.
(2003). A prospective study of memory for child sexual abuse: New findings relevant to the
repressed-memory controversy. Psychological Science, 14, 113–118. Click here to view
abstract.

2-4 Part 3, Section 2—Links to Select Abstracts
Goodson, J., Helstrom, A., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Powers, M. B.
(2011). The treatment of posttraumatic stress disorder in U.S. combat veterans: A meta-
analytic review. Psychological Reports, 109, 573–599. Click here to view abstract.
Guay, S., Billette, V., & Marchand, A. (2006). Exploring the links between posttraumatic stress
disorder and social support: Processes and potential research avenues. Journal of Traumatic
Stress, 19, 327–338. Click here to view abstract.
Harned, M. S., Korslund, K. E., Foa, E. B., & Linehan, M. M. (2012). Treating PTSD in suicidal
and self-injuring women with borderline personality disorder: Development and preliminary
evaluation of a Dialectical Behavior Therapy Prolonged Exposure Protocol. Behaviour
Research and Therapy, 50, 381–386. Click here to view abstract.
Hinton, D. E., Kredlow, M. A., Bui, E., Pollack, M. H., & Hofmann, S. G. (2012). Treatment
change of somatic symptoms and cultural syndromes among Cambodian refugees with
PTSD. Depression and Anxiety, 29, 148–155. Click here to view abstract.
Hobfoll, S. E., Watson, P., Bell, C. C., Bryant, R. A., Brymer, M. J., Friedman, M. J. et al. (2007).
Five essential elements of immediate and mid-term mass trauma intervention: Empirical
evidence. Psychiatry, 70, 283–315. Click here to view abstract.
Holbrook, T. L., Hoyt, D. B., Stein, M. B., & Sieber, W. J. (2001). Perceived threat to life
predicts posttraumatic stress disorder after major trauma: risk factors and functional outcome.
Journal of Trauma, 51, 287–292. Click here to view abstract.
Hopper, E. K., Bassuk, E. L., & Olivet, J. (2010). Shelter from the storm: Trauma-informed care
in homelessness services settings. The Open Health Services and Policy Journal, 3, 80–100.
Click here to view abstract.
Ipser, J. C. & Stein, D. J. (2012). Evidence–based pharmacotherapy of post–traumatic stress
disorder (PTSD). International Journal of Neuropsychopharmacology, 15, 825–840. Click
here to view abstract.
Johnson, H. & Thompson, A. (2008). The development and maintenance of post-traumatic stress
disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clinical
Psychology Review, 28, 36–47. Click here to view abstract.
Kar, N. (2011). Cognitive behavioral therapy for the treatment of post–traumatic stress disorder:
A review. Neuropsychiatric Disease and Treatment, 7, 167–181. Click here to view abstract.
Kessler, R. C. (2000). Posttraumatic stress disorder: the burden to the individual and to society.
Journal of Clinical Psychiatry, 61 Supplementement 5, 4–12. Click here to view abstract.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005).
Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National
Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602. Click here to
view abstract.
Kreidler, M. & Einsporn, R. (2012). A comparative study of therapy duration for survivors of
childhood sexual abuse. Journal of Psychosocial Nursing and Mental Health Services, 50,
26–32. Click here to view abstract.
Krysinska, K. & Lester, D. (2010). Post-traumatic stress disorder and suicide risk: A systematic
review. Archives of Suicide Research, 14, 1–23. Click here to view abstract.

Trauma-Informed Care in Behavioral Health Services 2-5
Laugharne, J., Lillee, A., & Janca, A. (2010). Role of psychological trauma in the cause and
treatment of anxiety and depressive disorders. Current Opinion in Psychiatry, 23, 25–29.
Click here to view abstract.
Lester, K., Resick, P. A., Young–Xu, Y., & Artz, C. (2010). Impact of race on early treatment
termination and outcomes in posttraumatic stress disorder treatment. Journal of Consulting
and Clinical Psychology, 78, 480–489. Click here to view abstract.
Levitt, J. T., Malta, L. S., Martin, A., Davis, L., & Cloitre, M. (2007). The flexible application of
a manualized treatment for PTSD symptoms and functional impairment related to the 9/11
World Trade Center attack. Behaviour Research and Therapy, 45, 1419–1433. Click here to
view abstract.
Marques, L., Robinaugh, D. J., LeBlanc, N. J., & Hinton, D. (2011). Cross-cultural variations in
the prevalence and presentation of anxiety disorders. Expert Review of Neurotherapeutics,
11, 313–322 Click here to view abstract.
McDonagh, A., Friedman, M., McHugo, G., Ford, J., Sengupta, A., Mueser, K. et al. (2005).
Randomized trial of cognitive–behavioral therapy for chronic posttraumatic stress disorder in
adult female survivors of childhood sexual abuse. Journal of Consulting and Clinical
Psychology, 73, 515–524. Click here to view abstract.
McLean, C. P. & Foa, E. B. (2011). Prolonged exposure therapy for post-traumatic stress
disorder: A review of evidence and dissemination. Expert Review of Neurotherapeutics, 11,
1151–1163. Click here to view abstract.
Monson, C. M., Rodriguez, B. F., & Warner, R. (2005). Cognitive–behavioral therapy for PTSD
in the real world: Do interpersonal relationships make a real difference? Journal of Clinical
Psychology, 61, 751–761. Click here to view abstract.
Morrissey, J. P., Jackson, E. W., Ellis, A. R., Amaro, H., Brown, V. B., & Najavits, L. M. (2005).
Twelve-month outcomes of trauma-informed interventions for women with co-occurring
disorders. Psychiatric Services, 56, 1213–1222. Click here to view abstract.
Mueser, K. T., Rosenberg, S. D., Xie, H., Jankowski, M. K., Bolton, E. E., Lu, W. et al. (2008). A
randomized controlled trial of cognitive–behavioral treatment for posttraumatic stress
disorder in severe mental illness. Journal of Consulting & Clinical Psychology, 76, 259–271.
Click here to view abstract.
Najavits, L. M., Harned, M. S., Gallop, R. J., Butler, S. F., Barber, J. P., Thase, M. E. et al.
(2007). Six-month treatment outcomes of cocaine–dependent patients with and without
PTSD in a multisite national trial. Journal of Studies on Alcohol and Drugs, 68, 353–361.
Click here to view abstract.
Nappi, C. M., Drummond, S. P., & Hall, J. M. (2012). Treating nightmares and insomnia in
posttraumatic stress disorder: A review of current evidence. Neuropharmacology, 62, 576–
585. Click here to view abstract.
Nickerson, A., Bryant, R. A., Silove, D., & Steel, Z. (2011). A critical review of psychological
treatments of posttraumatic stress disorder in refugees. Clinical Psychology Review, 31, 399–
417. Click here to view abstract.

2-6 Part 3, Section 2—Links to Select Abstracts
Norris, F. H., Friedman, M. J., & Watson, P. J. (2002). 60,000 disaster victims speak: Part II.
Summary and implications of the disaster mental health research. Psychiatry, 65, 240–260.
Click here to view abstract.
Norris, F. H., Friedman, M. J., Watson, P. J., Byrne, C. M., Diaz, E., & Kaniasty, K. (2002).
60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–
2001. Psychiatry, 65, 207–239. Click here to view abstract.
Olff, M., Langeland, W., Draijer, N., & Gersons, B. P. R. (2007). Gender differences in
posttraumatic stress disorder. Psychological Bulletin, 133, 183–204. Click here to view
abstract.
Ouimette, P. C., Brown, P. J., & Najavits, L. M. (1998). Course and treatment of patients with
both substance use and posttraumatic stress disorders. Addictive Behaviors, 23, 785–795
Click here to view abstract.
Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress
disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73 Click
here to view abstract.
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011). Prevalence and Axis I
comorbidity of full and partial posttraumatic stress disorder in the United States: Results
from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions.
Journal of Anxiety Disorders, 25, 456–465. Click here to view abstract.
Ponniah, K. & Hollon, S. D. (2009). Empirically supported psychological treatments for adult
acute stress disorder and posttraumatic stress disorder: A review. Depression and Anxiety,
26, 1086–1109. Click here to view abstract.
Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Foa, E. B. (2010). A meta-
analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology
Review, 30, 635–641. Click here to view abstract.
Resick, P. A., Galovski, T. E., O’Brien, U. M., Scher, C. D., Clum, G. A., & Young-Xu, Y.
(2008). A randomized clinical trial to dismantle components of cognitive processing therapy
for posttraumatic stress disorder in female victims of interpersonal violence. J.Consult
Clin.Psychol., 76, 243–258. Click here to view abstract.
Resick, P. A., Williams, L. F., Suvak, M. K., Monson, C. M., & Gradus, J. L. (2012). Long-term
outcomes of cognitive–behavioral treatments for posttraumatic stress disorder among female
rape survivors. Journal of Consulting and Clinical Psychology, 80, 201–210 Click here to
view abstract.
Roberts, A. L., Austin, S. B., Corliss, H. L., Vandermorris, A. K., & Koenen, K. C. (2010).
Pervasive trauma exposure among US sexual orientation minority adults and risk of
posttraumatic stress disorder. American Journal of Public Health, 100, 2433–2441. Click
here to view abstract.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic
differences in exposure to traumatic events, development of post–traumatic stress disorder,
and treatment–seeking for post–traumatic stress disorder in the United States. Psychological
Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 41, 71–83. Click
here to view abstract.

Trauma-Informed Care in Behavioral Health Services 2-7
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. (2009). Multiple session early
psychological interventions for the prevention of post-traumatic stress disorder. Cochrane
Database of Systematic Reviews, CD006869. Click here to view abstract.
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. I. (2010). Early psychological
interventions to treat acute traumatic stress symptoms. Cochrane Database of Systematic
Reviews, CD007944. Click here to view abstract.
Robinaugh, D. J. & McNally, R. J. (2011). Trauma centrality and PTSD symptom severity in
adult survivors of childhood sexual abuse. Journal of Traumatic Stress, 24, 483–486. Click
here to view abstract.
Robjant, K. & Fazel, M. (2010). The emerging evidence for Narrative Exposure Therapy: A
review. Clinical Psychology Review, 30, 1030–1039. Click here to view abstract.
Schnurr, P. P., Friedman, M. J., Foy, D. W., Shea, M. T., Hsieh, F. Y., Lavori, P. W. et al. (2003).
Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results
from a Department of Veterans Affairs Cooperative Study. Archives of General Psychiatry,
60, 481–489. Click here to view abstract.
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., & Gray, S. H. (2008). Contributions of
psychodynamic approaches to treatment of PTSD and trauma: A review of the empirical
treatment and psychopathology literature. Psychiatry, 71, 13–34. Click here to view abstract.
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., Tendick, V., & Gray, S. H. (2008).
Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological
considerations. Psychiatry, 71, 134–168 Click here to view abstract.
Seidler, G. H. & Wagner, F. E. (2006). Comparing the efficacy of EMDR and trauma–focused
cognitive–behavioral therapy in the treatment of PTSD: A meta-analytic study.
Psychological Medicine, 36, 1515–1522 Click here to view abstract.
Shalev, A. Y., Ankri, Y., Israeli-Shalev, Y., Peleg, T., Adessky, R., & Freedman, S. (2012).
Prevention of posttraumatic stress disorder by early treatment: Results from the Jerusalem
Trauma Outreach And Prevention study. Archives of General Psychiatry, 69, 166–176. Click
here to view abstract.
Sherin, J. E. & Nemeroff, C. B. (2011). Post-traumatic stress disorder: The neurobiological
impact of psychological trauma. Dialogues in Clinical Neuroscience, 13, 263–278. Click
here to view abstract.
Sherrer, M. V. (2011). The role of cognitive appraisal in adaptation to traumatic stress in adults
with serious mental illness: A critical review. Trauma, Violence, & Abuse, 12, 151–167.
Click here to view abstract.
Steel, J. L., Dunlavy, A. C., Stillman, J., & Pape, H. C. (2011). Measuring depression and PTSD
after trauma: common scales and checklists. Injury, 42, 288–300 Click here to view abstract.
Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van, O. M. (2009). Association of
torture and other potentially traumatic events with mental health outcomes among
populations exposed to mass conflict and displacement: A systematic review and meta-
analysis. JAMA, 302, 537–549. Click here to view abstract.

2-8 Part 3, Section 2—Links to Select Abstracts
Stein, D. J., Chiu, W. T., Hwang, I., Kessler, R. C., Sampson, N., Alonso, J. et al. (2010). Cross-
national analysis of the associations between traumatic events and suicidal behavior:
Findings from the WHO World Mental Health Surveys. PLoS ONE, 5. Click here to view
abstract.
Torchalla, I., Nosen, L., Rostam, H., & Allen, P. (2012). Integrated treatment programs for
individuals with concurrent substance use disorders and trauma experiences: A systematic
review and meta-analysis. Journal of Substance Abuse Treatment, 42, 65–77. Click here to
view abstract.
Vasterling, J. J., Verfaellie, M., & Sullivan, K. D. (2009). Mild traumatic brain injury and
posttraumatic stress disorder in returning veterans: Perspectives from cognitive neuroscience.
Clinical Psychology Review, 29, 674–684. Click here to view abstract.
Verschuur, M. J., Maric, M., & Spinhoven, P. (2010). Differences in changes in health-related
anxiety between Western and non-Western participants in a trauma-focused study. Journal of
Traumatic Stress, 23, 300–303. Click here to view abstract.
Vickerman, K. A. & Margolin, G. (2009). Rape treatment outcome research: Empirical findings
and state of the literature. Clinical Psychology Review, 29, 431–448. Click here to view
abstract.
Vlahov, D., Galea, S., Ahern, J., Resnick, H., & Kilpatrick, D. (2004). Sustained increased
consumption of cigarettes, alcohol, and marijuana among Manhattan residents after
September 11, 2001. American Journal of Public Health, 94, 253–254. Click here to view
abstract.
Walter, K. H., Horsey, K. J., Palmieri, P. A., & Hobfoll, S. E. (2010). The role of protective self-
cognitions in the relationship between childhood trauma and later resource loss. Journal of
Traumatic Stress, 23, 264–273. Click here to view abstract.
Weine, S., Danieli, Y., Silove, D., Ommeren, M. V., Fairbank, J. A., & Saul, J. (2002). Guidelines
for international training in mental health and psychosocial interventions for trauma exposed
populations in clinical and community settings. Psychiatry, 65, 156–164. Click here to view
abstract.
Westermeyer, J., Hollifield, M., Spring, M., Johnson, D., & Jaranson, J. (2011). Comparison of
two methods of inquiry for torture with East African refugees: Single query versus checklist.
Torture., 21, 155–172. Click here to view abstract.
Wrenn, G. L., Wingo, A. P., Moore, R., Pelletier, T., Gutman, A. R., Bradley, B. et al. (2011).
The effect of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary
care patients. Journal of the National Medical Association, 103, 560–566. Click here to view
abstract.
Zohar, J., Juven-Wetzler, A., Sonnino, R., Cwikel-Hamzany, S., Balaban, E., & Cohen, H. (2011).
New insights into secondary prevention in post-traumatic stress disorder. Dialogues in
Clinical Neuroscience, 13, 301–309. Click here to view abstract.
Trauma-Informed Care in Behavioral Health Services 3-1
Section 3—General Bibliography
Abrahams, I. A., Ali, O., Davidson, L., Evans, A. C., King, J. K., Poplawski, P. et al. (2010). Philadelphia
behavioral health services transformation: Practice guidelines for recovery and resilience oriented
treatment. Philadelphia: Department of Behavioral Health & Intellectual Disability Services.
Academy of Traumatology (2007). Standards of traumatology practice revised (Rep. No. 3.1).
Tallahassee, FL: Green Cross Foundation.
Achim, A. M., Maziade, M., Raymond, E., Olivier, D., Merette, C., & Roy, M. A. (2011). How prevalent
are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant
association. Schizophrenia Bulletin, 37, 811–821.
Acierno, R., Brady, K., Gray, M., Kilpatrick, D. G., Resnick, H., & Best, C. L. (2002). Psychopathology
following interpersonal violence: A comparison of risk factors in older and younger adults. Journal of
Clinical Geropsychology, 8, 13–23.
Acierno, R., Gray, M., Best, C., Resnick, H., Kilpatrick, D., Saunders, B. et al. (2001). Rape and physical
violence: Comparison of assault characteristics in older and younger adults in the National Women’s
Study. Journal of Traumatic Stress, 14, 685–695.
Acierno, R., Kilpatrick, D. G., Resnick, H. S., Saunders, B. E., & Best, C. L. (1996). Violent assault,
posttraumatic stress disorder, and depression: Risk factors for cigarette use among adult women.
Behavior Modification, 20, 363–384.
Acierno, R., Ruggiero, K. J., Kilpatrick, D. G., Resnick, H. S., & Galea, S. (2006). Risk and protective
factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. The
American Journal of Geriatric Psychiatry, 14, 1051–1059.
Adams, P. F., Martinez, M. E., & Vickerie, J. L. (2010). Summary health statistics for the U. S.
population: National Health Interview. (Rep. No. 10: 248). Hyattsville, MD: Centers for Disease
Control and Prevention, National Center for Health Statistics.
Adams, P. R. & Adams, G. R. (1984). Mount Saint Helens’s ashfall: Evidence for a disaster stress
reaction. American Psychologist, 39, 252–260.
Adams, R. E. & Boscarino, J. A. (2005). Differences in mental health outcomes among Whites, African
Americans, and Hispanics following a community disaster. Psychiatry, 68, 250–265.
Adams, R. E. & Boscarino, J. A. (2011). A structural equation model of perievent panic and posttraumatic
stress disorder after a community disaster. Journal of Traumatic Stress, 24, 61–69.
Adams, R. E., Figley, C. R., & Boscarino, J. A. (2008). The Compassion Fatigue Scale: Its use with social
workers following urban disaster. Research on Social Work Practice, 18, 238–250.
Adler, A. B., Bliese, P. D., McGurk, D., Hoge, C. W., & Castro, C. A. (2009). Battlemind debriefing and
battlemind training as early interventions with soldiers returning from iraq: Randomization by
platoon. Journal of Consulting and Clinical Psychology, 77, 928–940.
3-2 Part 3, Section 3—General Bibliography
Adler, A. B., Litz, B. T., Castro, C. A., Suvak, M., Thomas, J. L., Burrell, L. et al. (2008). A group
randomized trial of critical incident stress debriefing provided to U.S. peacekeepers. Journal of
Traumatic Stress, 21, 253–263.
Administration on Children Youth and Families (2002). Sexual Abuse among Homeless Adolescents:
Prevalence, Correlates, and Sequelae. Washington, DC: Administration for Children and Families.
Advanced Trauma Solutions Inc. (2012). Freedom Steps. Farmington, CT: Advanced Trauma Solutions,
Inc.
Adverse childhood experiences reported by adults—Five states, 2009 (2010). MMWR
Morb.Mortal.Wkly.Report, 59, 1609–1613.
Afifi, T. O., Asmundson, G. J. G., Taylor, S., & Jang, K. L. (2010). The role of genes and environment on
trauma exposure and posttraumatic stress disorder symptoms: A review of twin studies. Clinical
Psychology Review, 30, 101–112.
AfterDeployment.org (2010). Trauma triggers and memories—Overview. Joint Base Lewis–McChord,
WA: National Center for Telehealth & Technology.
AfterDeployment.org (2010). Understanding resilience. Joint Base Lewis–McChord, WA: National Center
for Telehealth & Technology.
Agaibi, C. E. & Wilson, J. P. (2005). Trauma, PTSD, and resilience: A review of the literature. Trauma,
Violence, & Abuse, 6, 195–216.
Agani, F., Landau, J., & Agani, N. (2010). Community-building before, during, and after times of trauma:
The application of the LINC model of community resilience in Kosovo. American Journal of
Orthopsychiatry, 80, 143–149.
Agorastos, A., Marmar, C. R., & Otte, C. (2011). Immediate and early behavioral interventions for the
prevention of acute and posttraumatic stress disorder. Current Opinion in Psychiatry, 24, 526–532.
Ahmed, A. S. (2007). Post-traumatic stress disorder, resilience and vulnerability. Advances in Psychiatric
Treatment, 13, 369–375.
Ahmed, A. T. & McCaw, B. R. (2010). Mental health services utilization among women experiencing
intimate partner violence. American Journal of Managed Care, 16, 731–738.
Aisenberg, E. & Ell, K. (2005). Contextualizing community violence and its effects: An ecological model
of parent–child interdependent coping. Journal of Interpersonal Violence, 20, 855–871.
Alarcon, L. H., Germain, A., Clontz, A. S., Roach, E., Nicholas, D. H., Zenati, M. S. et al. (2012).
Predictors of acute posttraumatic stress disorder symptoms following civilian trauma: highest
incidence and severity of symptoms after assault. Journal of Trauma and Acute Care Surgery, 72,
629–635.
Alcañiz, M., Lozano, J. A., & Rey, B. (2004). Technological background about VR. In G. Riva, C. Botella,
P. Legeron, & G. Optale (Eds.), Internet and virtual reality as assessment and rehabilitation tools for
clinical psychology and neuroscience. (pp. 199–216). Amsterdam: Ios Press.
Alegría, M., Canino, G., Shrout, P. E., Woo, M., Duan, N., Vila, D. et al. (2008). Prevalence of mental
illness in immigrant and non-immigrant U.S. Latino groups. American Journal of Psychiatry, 165,
359–369.
Trauma-Informed Care in Behavioral Health Services 3-3
Alim, T. N., Feder, A., Graves, R. E., Wang, Y., Weaver, J., Westphal, M. et al. (2008). Trauma,
resilience, and recovery in a high-risk African–American population. American Journal of
Psychiatry, 165, 1566–1575.
Alim, T. N., Graves, E., Mellman, T. A., Aigbogun, N., Gray, E., Lawson, W. et al. (2006). Trauma
exposure, posttraumatic stress disorder and depression in an African-American primary care
population. Journal of the National Medical Association, 98, 1630–1636.
Allen, B., Brymer, M. J., Steinberg, A. M., Vernberg, E. M., Jacobs, A., Speier, A. H. et al. (2010).
Perceptions of psychological first aid among providers responding to Hurricanes Gustav and Ike.
Journal of Traumatic Stress, 23, 509–513.
Allen, J. G. (2001). Traumatic relationships and serious mental disorders. New York: John Wiley & Sons
Ltd.
Alonso, J., Buron, A., Bruffaerts, R., He, Y., Posada–Villa, J., Lepine, J. P. et al. (2008). Association of
perceived stigma and mood and anxiety disorders: Results from the World Mental Health Surveys.
Acta Psychiatrica Scandinavica, 118, 305–314.
Al-Saffar, S. & Borga, P. (2006). Focusing on trauma and PTSD in general psychiatric services––Could
outcome be improved? In G. D. Kume (Ed.), Posttraumatic stress: New research (pp. 147–166).
Hauppauge, NY: Nova Science Publishers.
Amaro, H., Dai, J., Arevalo, S., Acevedo, A., Matsumoto, A., Nieves, R. et al. (2007). Effects of integrated
trauma treatment on outcomes in a racially/ethnically diverse sample of women in urban community-
based substance abuse treatment. Journal of Urban Health, 84, 508–522.
American Psychiatric Association (1980). Diagnostic and statistical manual of mental disorders. (3rd ed.)
Washington, DC: American Psychiatric Association.
American Psychiatric Association (1987). Diagnostic and statistical manual of mental disorders. (3rd rev.
ed.) Washington, DC: American Psychiatric Association.
American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders. (4th ed.)
Washington, DC: American Psychiatric Association.
American Psychiatric Association (2000a). Diagnostic and statistical manual of mental disorders. (4th
Text Revision ed.) Washington, DC: American Psychiatric Association.
American Psychiatric Association (2000b). Position statement on therapies focused on memories of
childhood physical and sexual abuse Arlington, VA: American Psychiatric Association.
American Psychiatric Association (2010). Practice guideline for the treatment of patients with acute stress
disorder and posttraumatic stress disorder. Arlington, VA: American Psychiatric Association.
American Psychiatric Association (2012). G 03 posttraumatic stress disorder. Arlington, VA: American
Psychiatric Association.
American Psychiatric Association (2012). Proposed draft revisions to DSM disorders and criteria.
Arlington, VA: American Psychiatric Association.
American Psychiatric Association (2013a). Diagnostic and statistical manual of mental disorders. (5th ed.)
Arlington, VA: American Psychiatric Association.
3-4 Part 3, Section 3—General Bibliography
American Psychiatric Association (2013b). Highlights of changes from DSM-IV-TR to DSM-V. Arlington,
VA: American Psychiatric Association.
American Psychological Association & The Ad Hoc Committee on Legal and Ethical Issues in the
Treatment of Interpersonal Violence (2003). Potential Problems for Psychologists Working with the
Area of Interpersonal Violence. Washington, DC: American Psychological Association.
Amstadter, A. B., Acierno, R., Richardson, L. K., Kilpatrick, D. G., Gros, D. F., Gaboury, M. T. et al.
(2009). Posttyphoon prevalence of posttraumatic stress disorder, major depressive disorder, panic
disorder, and generalized anxiety disorder in a Vietnamese sample. Journal of Traumatic Stress, 22,
180–188.
Amstadter, A. B., Zinzow, H. M., McCauley, J. L., Strachan, M., Ruggiero, K. J., Resnick, H. S. et al.
(2010). Prevalence and correlates of service utilization and help seeking in a national college sample
of female rape victims. Journal of Anxiety Disorders, 24, 900–902.
Anda, R. F., Felitti, V. J., Brown, D., Chapman, D., Dong, M., Dube, S. R. et al. (2006). Insights into
intimate partner violence from the Adverse Childhood Experiences (ACE) Study. In The physician’s
guide to intimate partner violence and abuse (pp. 77–88). Volcano, CA: Volcano Press.
Anders, S. L., Shallcross, S. L., & Frazier, P. A. (2012). Beyond Criterion A1: The effects of relational and
non-relational traumatic events. Journal of Trauma & Dissociation, 13, 134–151.
Andreasen, N. C. (2010). Posttraumatic stress disorder: A history and a critique. Annals of the New York
Academy of Sciences, 1208, 67–71.
Andrews, B., Brewin, C. R., & Rose, S. (2003). Gender, social support, and PTSD in victims of violent
crime. Journal of Traumatic Stress, 16, 421–427.
Ansell, E. B., Pinto, A., Edelen, M. O., Markowitz, J. C., Sanislow, C. A., Yen, S. et al. (2011). The
association of personality disorders with the prospective 7-year course of anxiety disorders.
Psychological Medicine, 41, 1019–1028.
Antony, M. M., Orsillo, S. M., & Roemer, L. (2001). Practitioner’s guide to empirically based measures
of anxiety. New York: Kluwer Academic/Plenum Publishers.
Apter, A. J., Garcia, L. A., Boyd, R. C., Wang, X., Bogen, D. K., & Ten Have, T. (2010). Exposure to
community violence is associated with asthma hospitalizations and emergency department visits.
Journal of Allergy and Clinical Immunology, 126, 552–557.
Archambeau, O. G., Frueh, B. C., Deliramich, A. N., Elhai, J. D., Grubaugh, A. L., Herman, S. et al.
(2010). Interpersonal violence and mental health outcomes among Asian American and Native
Hawaiian/other Pacific Islander college students. Psychological Trauma: Theory, Research, Practice,
and Policy, 2, 273–283.
Arkowitz, H., Miller, W. R., Westra, H. A., & Rollnick, S. (2008). Motivational interviewing in the
treatment of psychological problems: Conclusions and future directions. In Motivational interviewing
in the treatment of psychological problems (pp. 324–342). New York: Guilford Press.
Arredondo, P., Bordes, V., & Paniagua, F. A. (2008). Mexicans, Mexican Americans, Caribbean, and other
Latin Americans. In A. J. Marsella, J. L. Johnson, P. Watson, & J. Gryczynski (Eds.), Ethnocultural
perspectives on disaster and trauma: Foundations, issues, and applications (pp. 299–320). New
York: Springer Publishing Science + Business Media.
Trauma-Informed Care in Behavioral Health Services 3-5
Asmundson, G. J. & Katz, J. (2009). Understanding the co-occurrence of anxiety disorders and chronic
pain: State-of-the-art. Depression and Anxiety, 26, 888–901.
Asmundson, G. J. G., Abrams, M. P., & Collimore, K. C. (2008). Pain and anxiety disorders. In Anxiety in
health behaviors and physical illness (pp. 207–235). New York: Springer Publishing Science +
Business Media.
Asnaani, A., Richey, J. A., Dimaite, R., Hinton, D. E., & Hofmann, S. G. (2010). A cross-ethnic
comparison of lifetime prevalence rates of anxiety disorders. Journal of Nervous and Mental Disease,
198, 551–555.
Aspelmeier, J. E., Elliott, A. N., & Smith, C. H. (2007). Childhood sexual abuse, attachment, and trauma
symptoms in college women: The moderating role of attachment. Child Abuse & Neglect, 31, 549–
566.
Astin, M. C., Lawrence, K. J., & Foy, D. W. (1993). Posttraumatic stress disorder among battered women:
Risk and resiliency factors. Violence and Victims, 8, 17–28.
Auerbach, S. (2003). Sleep disorders related to alcohol and other drug use. In A. W. Graham, T. K.
Schultz, M. F. Mayo–Smith, R. K. Ries, & B. B. Wilford (Eds.), Principles of Addiction Medicine
(3rd ed., pp. 1179–1193). Chevy Chase, MD: American Society of Addiction Medicine.
Australian Centre for Posttraumatic Mental Health (2007). Australian guidelines for the treatment of
adults with acute stress disorder and posttraumatic stress disorder. Melbourne, Victoria: Australian
Centre for Posttraumatic Mental Health.
Awa, W. L., Plaumann, M., & Walter, U. (2010). Burnout prevention: A review of intervention programs.
Patient Education and Counseling, 78, 184–190.
Ayers, J. W., Hofstetter, C. R., Usita, P., Irvin, V. L., Kang, S., & Hovell, M. F. (2009). Sorting out the
competing effects of acculturation, immigrant stress, and social support on depression: A report on
Korean women in CAornia. Journal of Nervous and Mental Disease, 197, 742–747.
Azeem, M. W., Aujla, A., Rammerth, M., Binsfeld, G., & Jones, R. B. (2011). Effectiveness of six core
strategies based on trauma informed care in reducing seclusions and restraints at a child and
adolescent psychiatric hospital. Journal of Child and Adolescent Psychiatric Nursing, 24, 11–15.
Babson, K. A. & Feldner, M. T. (2010). Temporal relations between sleep problems and both traumatic
event exposure and PTSD: A critical review of the empirical literature. Journal of Anxiety Disorders,
24, 1–15.
Back, S., Dansky, B. S., Coffey, S. F., Saladin, M. E., Sonne, S., & Brady, K. T. (2000). Cocaine
dependence with and without posttraumatic stress disorder: A comparison of substance use, trauma
history and psychiatric comorbidity. American Journal on Addictions, 9, 51–62.
Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review.
Clinical Psychology: Science and Practice, 10, 125–143.
Baglioni, C., Battagliese, G., Feige, B., Spiegelhalder, K., Nissen, C., Voderholzer, U. et al. (2011).
Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological
studies. Journal of Affective Disorders, 135, 10–19.
3-6 Part 3, Section 3—General Bibliography
Bailey, H. N., DeOliveira, C. A., Wolfe, V. V., Evans, E. M., & Hartwick, C. (2012). The impact of
childhood maltreatment history on parenting: A comparison of maltreatment types and assessment
methods. Child Abuse & Neglect, 36, 236–246.
Bailey, K., Webster, R., Baker, A. L., & Kavanagh, D. J. (2011). Exposure to dysfunctional parenting and
trauma events and posttraumatic stress profiles among a treatment sample with coexisting depression
and alcohol use problems. Drug Alcohol Revjew.
Baker, D. G., Nash, W. P., Litz, B. T., Geyer, M. A., Risbrough, V. B., Nievergelt, C. M. et al. (2012).
Predictors of risk and resilience for posttraumatic stress disorder among ground combat marines:
Methods of the Marine Resiliency Study. Preventing Chronic Disease, 9, E97.
Baker, K. G. & Gippenreiter, J. B. (1998). Stalin’s purge and its impact on Russian families: A pilot study.
In Y. Danieli (Ed.), International handbook of multigenerational legacies of trauma (pp. 403–434).
New York: Plenum Press.
Balsam, K. F., Lehavot, K., Beadnell, B., & Circo, E. (2010). Childhood abuse and mental health
indicators among ethnically diverse lesbian, gay, and bisexual adults. Journal of Consulting and
Clinical Psychology, 78, 459–468.
Balsam, K. F., Rothblum, E. D., & Beauchaine, T. P. (2005). Victimization over the life span: A
comparison of lesbian, gay, bisexual, and heterosexual siblings. Journal of Consulting and Clinical
Psychology, 73, 477–487.
Baños, R. M., Guillen, V., Quero, S., Garcia-Palacios, A., Alcañiz, M., & Botella, C. (2011). A virtual
reality system for the treatment of stress-related disorders: A preliminary analysis of efficacy
compared to a standard cognitive behavioral program. International Journal of Human Computer
Studies, 69, 602–613.
Banyard, V. L., Williams, L. M., & Siegel, J. A. (2004). Childhood Sexual Abuse: A Gender Perspective
on Context and Consequences. Child Maltreatment, 9, 223–238.
Baranowsky, A. B., Young, M., Johnson-Douglas, S., Williams-Keeler, L., & McCarrey, M. (1998). PTSD
transmission: A review of secondary traumatization in Holocaust survivor families. Canadian
Psychology/Psychologie canadienne, 39, 247–256.
Barner, J. R. & Carney, M. M. (2011). Interventions for intimate partner violence: A historical review.
Journal of Family Violence, 26, 235–244.
Barnes, M. & Figley, C. R. (2005). Family therapy: Working with traumatized families. In J. L. Lebow
(Ed.), Handbook of clinical family therapy (pp. 309–326). Hoboken, NJ: John Wiley and Sons, Inc.
Baroody, A. N. (2011). Spirituality and trauma during a time of war: A systemic approach to pastoral care
and counseling. In Families under fire: Systemic therapy with military families (pp. 165–190). New
York: Routledge/Taylor & Francis Group.
Bartone, P. T., Roland, R. R., Picano, J. J., & Williams, T. (2008). Psychological hardiness predicts
success in US Army special forces candidates. International Journal of Selection and Assessment, 16,
78–81.
Başoğlu, M., Livanou, M., Crnobaric, C., Franciskovic, T., Suljic, E., Duric, D. et al. (2005). Psychiatric
and cognitive effects of war in former Yugoslavia: Association of lack of redress for trauma and
posttraumatic stress reactions. JAMA, 294, 580–590.
Trauma-Informed Care in Behavioral Health Services 3-7
Başoğlu, M., Salcioglu, E., & Livanou, M. (2007). A randomized controlled study of single-session
behavioural treatment of earthquake-related post-traumatic stress disorder using an earthquake
simulator. Psychological Medicine, 37, 203–213.
Batten, S. V. & Hayes, S. C. (2005). Acceptance and commitment therapy in the treatment of comorbid
substance abuse and post-traumatic stress disorder: A case study. Clinical Case Studies, 4, 246–262.
Beals, J., Manson, S. M., Shore, J. H., Friedman, M. J., Ashcraft, M., Fairbank, J. A. et al. (2002). The
prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: Disparities and
context. Journal of Traumatic Stress, 15, 89–97.
Beals, J., Manson, S. M., Whitesell, N. R., Spicer, P., Novins, D. K., & Mitchell, C. M. (2005). Prevalence
of DSM-IV disorders and attendant help–seeking in 2 American Indian reservation populations.
Archives of General Psychiatry, 62, 99–108.
Beals, J., Novins, D. K., Whitesell, N. R., Spicer, P., Mitchell, C. M., & Manson, S. M. (2005). Prevalence
of mental disorders and utilization of mental health services in two American Indian reservation
populations: Mental health disparities in a national context. American Journal of Psychiatry, 162,
1723–1732.
Beard, C., Weisberg, R. B., & Keller, M. B. (2010). Health-related quality of life across the anxiety
disorders: findings from a sample of primary care patients. Journal of Anxiety Disorders, 24, 559–
564.
Beattie, N., Shannon, C., Kavanagh, M., & Mulholland, C. (2009). Predictors of PTSD symptoms in
response to psychosis and psychiatric admission. Journal of Nervous and Mental Disease, 197, 56–
60.
Bebbington, P. E., Bhugra, D., Brugha, T., Singleton, N., Farrell, M., Jenkins, R. et al. (2004). Psychosis,
victimisation and childhood disadvantage: evidence from the second British National Survey of
Psychiatric Morbidity. British Journal of Psychiatry, 185, 220–226.
Beck, A. T. (1993). Beck anxiety inventory. San Antonio, TX: The Psychological Corporation.
Beck, A. T., Emery, G., & Greenberg, R. L. (2005). Anxiety disorders and phobias: A cognitive
perspective. New York: Basic Books.
Beck, A. J., Harrison, P. M., Berzofsky, M., Caspar, R., & Krebs, C. (2010). Sexual victimization in
prisons and jails reported by inmates, 2008–09. Washington, DC: Bureau of Justice Statistics, U.S.
Department of Justice.
Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive Therapy of Depression. New York,
N.Y.: Guilford Press.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory – II Manual. San Antonio,
TX: The Psychological Corporation.
Beck, A. T., Wright, F. D., Newman, C. F., & Liese, B. F. (1993). Cognitive Therapy of Substance Abuse.
New York: Guilford Press.
Beck, C. T. (2011). Secondary traumatic stress in nurses: A systematic review. Archives of Psychiatric
Nursing, 25, 1–10.
3-8 Part 3, Section 3—General Bibliography
Beck, J. G., Coffey, S. F., Foy, D. W., Keane, T. M., & Blanchard, E. B. (2009). Group cognitive behavior
therapy for chronic posttraumatic stress disorder: An initial randomized pilot study. Behav.Ther. 40,
82–92.
Becker, M. A., Noether, C. D., Larson, M. J., Gatz, M., Brown, V., Heckman, J. P. et al. (2005).
Characteristics of women engaged in treatment for trauma and co-occurring disorders: Findings from
a national multisite study. Journal of Community Psychology, 33, 429–443.
Beidel, D. C., Frueh, B. C., Uhde, T. W., Wong, N., & Mentrikoski, J. M. (2011). Multicomponent
behavioral treatment for chronic combat-related posttraumatic stress disorder: A randomized
controlled trial. Journal of Anxiety Disorders, 25, 224–231.
Beiser, M. & Wickrama, K. A. S. (2004). Trauma, time and mental health: A study of temporal
reintegration and depressive disorder among Southeast Asian refugees. Psychological Medicine: A
Journal of Research in Psychiatry and the Allied Sciences, 34, 899–910.
Bell, C. C. (2011). Trauma, culture, and resiliency. In S. M. Southwick, B. T. Litz, D. Charney, & M. J.
Friedman (Eds.), Resilience and mental health: Challenges across the lifespan (pp. 176–187). New
York: Cambridge University Press.
Bell, H., Kulkarni, S., & Dalton, L. (2003). Organizational prevention of vicarious trauma. Families in
Society, 84, 463–470.
Bell, N. S., Amoroso, P. J., Yore, M. M., Smith, G. S., & Jones, B. H. (2000). Self-reported risk-taking
behaviors and hospitalization for motor vehicle injury among active duty army personnel. American
Journal of Preventive Medicine, 18, 85–95.
Benedek, D. M. & Ursano, R. J. (2009). Posttraumatic stress disorder: From phenomenology to clinical
practice. FOCUS: The Journal of Lifelong Learning in Psychiatry, 7, 160–175.
Benedek, D. M., Friedman, M. J., Zatzick, D., & Ursano, R. J. (2009). Guideline watch (March 2009):
Practice guideline for the treatment of patients with acute stress disorder and
posttraumatic stress disorder. FOCUS: The Journal of Lifelong Learning in Psychiatry, VII, 204–213.
Benish, S. G., Imel, Z. E., & Wampold, B. E. (2008). The relative efficacy of bona fide psychotherapies
for treating post-traumatic stress disorder: A meta-analysis of direct comparisons. Clinical
Psychology Review, 28, 746–758.
Bent-Goodley, T. B. (2005). Culture and domestic violence: Transforming knowledge development.
Journal of Interpersonal Violence, 20, 195–203.
Bent-Goodley, T. B. (2007). Health disparities and violence against women: Why and how cultural and
societal influences matter. Trauma, Violence, & Abuse, 8, 90–104.
Ben-Zur, H. (2008). Personal resources of mastery–optimism, and communal support beliefs, as predictors
of posttraumatic stress in uprooted Israelis. Anxiety Stress Coping, 21, 295–307.
Berceli, D. & Napoli, M. (2006). A proposal for a mindfulness-based trauma prevention program for social
work professionals. Complementary Health Practice Review, 11, 153–165.
Berg, G. (2011). The relationship between spiritual distress, PTSD and depression in Vietnam combat
veterans. Journal of Pastoral Care and Counseling., 65, 6–11.
Trauma-Informed Care in Behavioral Health Services 3-9
Berger, W., Mendlowicz, M. V., Marques-Portella, C., Kinrys, G., Fontenelle, L. F., Marmar, C. R. et al.
(2009). Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: A systematic
review. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 33, 169–180.
Berkowitz, S. J., Stover, C. S., & Marans, S. R. (2011). The Child and Family Traumatic Stress
Intervention: Secondary prevention for youth at risk of developing PTSD. Journal of Child
Psychology and Psychiatry, 52, 676–685.
Bernard, J. M. & Goodyear, R. K. (2009). Fundamentals of clinical supervision. (4th ed.) Upper Saddle
River, NJ: Merrill/Pearson.
Bernstein, D. P. (2000). Childhood trauma and drug addiction: Assessment, diagnosis, and treatment.
Alcoholism Treatment Quarterly, 18, 19–30.
Bernstein, E. M. & Putnam, F. W. (1986). Development, reliability, and validity of a dissociation scale.
Journal of Nervous and Mental Disease, 174, 727–735.
Bhugra, D. (2003). Migration and depression. Acta Psychiatrica Scandinavica, 108, 67–72.
Bills, L. J. (2003). Using trauma theory and S.A.G.E. in outpatient psychiatric practice. Psychiatric
Quarterly, 74, 191–203.
Birman, D. & Tran, N. (2008). Psychological distress and adjustment of Vietnamese refugees in the United
States: Association with pre– and postmigration factors. American Journal of Orthopsychiatry, 78,
109–120.
Bisson, J. & Andrew, M. (2007). Psychological treatment of post-traumatic stress disorder (PTSD).
Cochrane Database of Systematic Reviews, CD003388.
Bisson, J. I., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007). Psychological
treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. British
Journal of Psychiatry, 190, 97–104.
Blackburn, C. (1995, November). Family and relapse. Counselor, Alexandria, VA: National Association of
Alcoholism and Drug Abuse Counselors.
Blake, D., Weathers, F., Nagy, L., Koloupek, D., Klauminzer, G., Charney, D. et al. (1990). Clinician
administered PTSD scale (CAPS) Boston: National Center for Post-Traumatic Stress Disorder.
Blanchard, E. B. & Hickling, E. J. (2004). Determining who develops PTSD from MVAs. In After the
crash: Psychological assessment and treatment of survivors of motor vehicle accidents (2nd ed.) (pp.
99–124). Washington, DC: American Psychological Association.
Blanchard, E. B., Buckley, T. C., Hickling, E. J., & Taylor, A. E. (1998). Posttraumatic stress disorder and
comorbid major depression: Is the correlation an illusion? Journal of Anxiety Disorders, 12, 21–37.
Blanco, C. (2011). Epidemiology of PTSD. In D. J. Stein, M. J. Friedman, & C. Blanco (Eds.), Post-
traumatic stress disorder (pp. 49–74). Chichester, UK: John Wiley & Sons.
Bleich, A., Gelkopf, M., & Solomon, Z. (2003). Exposure to terrorism, stress-related mental health
symptoms, and coping behaviors among a nationally representative sample in Israel. Journal of the
American Medical Association, 290, 612–620.
Bleich, A., Gelkopf, M., Melamed, Y., & Solomon, Z. (2006). Mental health and resiliency following 44
months of terrorism: A survey of an Israeli national representative sample. BMC Medicine, 4, 21.
3-10 Part 3, Section 3—General Bibliography
Bliss, M. J., Cook, S. L., & Kaslow, N. J. (2007). An ecological approach to understanding incarcerated
women’s responses to abuse. Women & Therapy, 29, 97–115.
Block, S. H. & Block, C. B. (2010). Improve everyday life by melting away your tension. In Mind–body
workbook for PTSD (pp. 21–43). Oakland, CA: New Harbinger Publications, Inc.
Block, S. H. & Block, C. B. (2010). Mind–body workbook for PTSD: A 10-week program for healing after
trauma. Oakland, CA: New Harbinger Publications, Inc.
Block, S. H. & Block, C. B. (2010). Self-discovery and self-healing of PTSD. In Mind–body workbook for
PTSD (pp. 6–20). Oakland, CA: New Harbinger Publications, Inc.
Blomstedt, Y., Johansson, S. E., & Sundquist, J. (2007). Mental health of immigrants from the former
Soviet Bloc: A future problem for primary health care in the enlarged European Union? A cross-
sectional study. BMC Public Health, 7, 27.
Bloom, S. L. & Farragher, B. (2011). Destroying sanctuary: The crisis in human service delivery systems.
New York: Oxford University Press.
Bloom, S. L. (1997). Creating sanctuary: Toward the evolution of sane societies. New York: Routledge.
Bloom, S. L. (2010). Organizational stress and trauma-informed services. In A public health perspective of
women’s mental health (pp. 295–311). New York: Springer Publishing Science + Business Media.
Bloom, S. L., Bennington-Davis, M., Farragher, B., McCorkle, D., Nice-Martini, K., & Wellbank, K.
(2003). Multiple opportunities for creating sanctuary. Psychiatric Quarterly, 74, 173–190.
Bloom, S. L., Foderaro, J. F., & Ryan, R. (2006). S.E.L.F.: A trauma-informed psychoeducational group
curriculum. Retrieved on July 4, 2013, from: http://www.sanctuaryweb.com/self-manual.php
Bober, T. & Regehr, C. (2006). Strategies for reducing secondary or vicarious trauma: Do they work?
Brief Treatment and Crisis Intervention, 6, 1–9.
Bonanno, G. A. & Mancini, A. D. (2011). Toward a lifespan approach to resilience and potential trauma.
In S. M. Southwick, B. T. Litz, D. Charney, & M. J. Friedman (Eds.), Resilience and mental health:
Challenges across the lifespan (pp. 120–134). New York: Cambridge University Press.
Bonanno, G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity
to thrive after extremely aversive events? American Psychologist, 29, 20–28.
Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2007). What predicts psychological resilience
after disaster? The role of demographics, resources, and life stress. Journal of Consulting & Clinical
Psychology, 75, 671–682.
Bonow, J. T. & Follette, W. C. (2012). A functional analytic conceptualization of retraumatization:
Implications for clinical assessment. In M. P. Duckworth (Ed.), Retraumatization: Assessment,
treatment, and prevention (pp. 129–162). New York: Routledge/Taylor & Francis Group.
Booth, B. M., Mengeling, M., Torner, J., & Sadler, A. G. (2011). Rape, sex partnership, and substance use
consequences in women veterans. Journal of Traumatic Stress, 24, 287–294.
Bormann, J. E., Liu, L., Thorp, S. R., & Lang, A. J. (2011). Spiritual wellbeing mediates PTSD change in
veterans with military-related PTSD. Int.J.Behav.Med.
Boscarino, J. A. & Adams, R. E. (2009). Peritraumatic panic attacks and health outcomes two years after
psychological trauma: Implications for intervention and research. Psychiatry Research, 167, 139–150.
Trauma-Informed Care in Behavioral Health Services 3-11
Boscarino, J. A., Figley, C. R., & Adams, R. E. (2004). Compassion fatigue following the September 11
terrorist attacks: A study of secondary trauma among New York City social workers. International
Journal of Emergency Mental Health, 6, 57–66.
Boscarino, J. A., Kirchner, H. L., Hoffman, S. N., Sartorius, J., Adams, R. E., & Figley, C. R. (2011a). A
brief screening tool for assessing psychological trauma in clinical practice: Development and
validation of the New York PTSD Risk Score. General Hospital Psychiatry, 33, 489–500.
Boscarino, J. A., Kirchner, H. L., Hoffman, S. N., Sartorius, J., Adams, R. E., & Figley, C. R. (2011b). A
brief screening tool for assessing psychological trauma in clinical practice: Development and
validation of the New York PTSD Risk Score. General Hospital Psychiatry, 33, 489–500.
Boscarino, J. A., Kirchner, H. L., Hoffman, S. N., Sartorius, J., Adams, R. E., & Figley, C. R. (2012a).
Predicting future PTSD using a modified New York Risk Score: Implications for patient screening
and management. Minerva Psichiatrica, 53, 47–59.
Boscarino, J. A., Kirchner, H. L., Hoffman, S. N., Sartorius, J., Adams, R. E., & Figley, C. R. (2012b).
The New York PTSD Risk Score for assessment of psychological trauma: Male and female versions.
Psychiatry Research.
Bosquet, E. M., Kitts, R. L., Blood, E., Bizarro, A., Hofmeister, M., & Wright, R. J. (2011). Maternal
posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant
Behavior & Development, 34, 487–503.
Botella, C., Quero, S., Baños, R. M., Perpina, C., Garcia Palacios, A., & Riva, G. (2004). Virtual reality
and psychotherapy. In G. Riva, C. Botella, P. Legeron, & G. Optale (Eds.), Internet and virtual
reality as assessment and rehabilitation tools for clinical psychology and neuroscience. (pp. 37–54).
Amsterdam: Ios Press.
Böttche, M., Kuwert, P., & Knaevelsrud, C. (2012). Posttraumatic stress disorder in older adults: An
overview of characteristics and treatment approaches. International Journal of Geriatric Psychiatry,
27, 230–239.
Bourque, L. B. & Shen, H. (2005). Psychometric characteristics of Spanish and English versions of the
Civilian Mississippi scale. Journal of Traumatic Stress, 18, 719–728.
Bovin, M. J. & Marx, B. P. (2011). The importance of the peritraumatic experience in defining traumatic
stress. Psychological Bulletin, 137, 47–67.
Bowman, C. G. & Mertz, E. (1996). A dangerous direction: Legal intervention in sexual abuse survivor
therapy. Harvard Law Review, 109, 551–639.
Bowman, M. L. & Yehuda, R. (2004). Risk factors and the adversity–stress model. In G.M.Rosen (Ed.),
Posttraumatic stress disorder: Issues and controversies (pp. 15–38). New York: John Wiley & Sons,
Inc.
Braakman, M. H., Kortmann, F. A., & van den Brink, W. (2009). Validity of ‘post-traumatic stress
disorder with secondary psychotic features’: A review of the evidence. Acta Psychiatrica
Scandinavica, 119, 15–24.
Bradley, R., Greene, J., Russ, E., Dutra, L., & Westen, D. (2005). A multidimensional meta-analysis of
psychotherapy for PTSD. American Journal of Psychiatry, 162, 214–227.
3-12 Part 3, Section 3—General Bibliography
Bradley, R., Schwartz, A. C., & Kaslow, N. J. (2005). Posttraumatic stress disorder symptoms among low-
income, African American women with a history of intimate partner violence and suicidal behaviors:
Self-esteem, social support, and religious coping. Journal of Traumatic Stress, 18, 685–696.
Brady, K. T., Killeen, T. K., Brewerton, T., & Lucerini, S. (2000). Comorbidity of psychiatric disorders
and posttraumatic stress disorder. Journal of Clinical Psychiatry, 61, 22–32.
Brady, K. T., Killeen, T., Saladin, M. E., Dansky, B., & Becker, S. (1994). Comorbid substance abuse and
posttraumatic stress disorder: Characteristics of women in treatment. American Journal on
Addictions, 3, 160–164.
Brave Heart, M. Y. H. (1999). Gender differences in the historical trauma response among the Lakota.
Journal of Health & Social Policy, 10, 1–20.
Brave Heart, M. Y. H. (2003). The historical trauma response among natives and its relationship with
substance abuse: A Lakota illustration. Journal of Psychoactive Drugs, 35, 7–13.Brave Heart, M. Y.
H. (2004). The historical trauma response among natives and its relationship to substance abuse: A
Lakota illustration. In E. Nebelkopf & M. Phillips (Eds.), Healing and mental health for Native
Americans: Speaking in red (pp. 7–18). Walnut Creek, CA: AltaMira Press.
Breh, D. C. & Seidler, G. H. (2007). Is peritraumatic dissociation a risk factor for PTSD? Journal of
Trauma & Dissociation, 8, 53–69.
Brenner, L. A. (2011). Neuropsychological and neuroimaging findings in traumatic brain injury and post-
traumatic stress disorder. Dialogues in Clinical Neuroscience, 13, 311–323.
Breno, A. L. & Galupo, M. P. (2007). Sexual abuse histories of young women in the U.S. child welfare
system: A focus on trauma-related beliefs and resilience. Journal of Child Sexual Abuse, 16, 97–113.
Breslau, N. (2002). Gender differences in trauma and posttraumatic stress disorder. Journal of Gender
Specific Medicine, 5, 34–40.
Breslau, N., Davis, G. C., Andreski, P., & Peterson, E. (1991). Traumatic events and posttraumatic stress
disorder in an urban population of young adults. Archives of General Psychiatry, 48, 216–222.
Breslau, N., Davis, C., Peterson, E. L., & Schultz, L. (2000). A second look at comorbidity in victims of
trauma: The posttraumatic stress disorder–major depression connection. Biological Psychiatry, 48,
902–909.
Breslau, N., Davis, G. C., & Schultz, L. R. (2003). Posttraumatic stress disorder and the incidence of
nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of
General Psychiatry, 60, 289 –294.
Breslau, N., Lucia, V. C., & Alvarado, G. F. (2006). Intelligence and other predisposing factors in
exposure to trauma and posttraumatic stress disorder: A follow-up study at age 17 years. Archives of
General Psychiatry, 63, 1238–1245.
Breslau, N., Lucia, V. C., & Davis, G. C. (2004). Partial PTSD versus full PTSD: An empirical
examination of associated impairment. Psychological Medicine, 34, 1205–1214.
Brewerton, T. D. (2007). Eating disorders, trauma, and comorbidity: Focus on PTSD. Journal of Eating
Disorders, 15, 285–304.
Trauma-Informed Care in Behavioral Health Services 3-13
Brewin, C. R. (2007). Remembering and forgetting. In M. J. Friedman, T. M. Keane, & P. A. Resick
(Eds.), Handbook of PTSD: Science and practice (pp. 116–134). New York: Guilford Press.
Brewin, C. R. (2011). The nature and significance of memory disturbance in posttraumatic stress disorder.
Annual Review of Clinical Psychology, 7, 203–227.
Brewin, C. R. (2011). Walking the line in defining PTSD: Comprehensiveness versus core features. In D.
J. Stein, M. J. Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 35–37). Chichester,
UK: John Wiley and Sons, Inc.
Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic
stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–
766.
Bride, B. E. (2007). Prevalence of secondary traumatic stress among social workers. Social Work, 52, 63–
70.
Bride, B. E., Robinson, M. M., Yegidis, B., & Figley, C. R. (2004). Development and validation of the
Secondary Traumatic Stress Scale. Research on Social Work Practice, 14, 27–35.
Bridges, A. J., de Arellano, M. A., Rheingold, A. A., Danielson, C. K., & Silcott, L. (2010). Trauma
exposure, mental health, and service utilization rates among immigrant and United States-born
Hispanic youth: Results from the Hispanic family study. Psychological Trauma: Theory, Research,
Practice, and Policy, 2, 40–48.
Briere, J. (1995). Trauma symptom inventory professional manual. Odessa, FL: Psychological Assessment
Resources.
Briere, J. (1996a). Therapy for adults molested as children: Beyond survival. (2nd ed.) New York:
Springer Publishing Publishing.
Briere, J. (1996b). Trauma symptom checklist for children professional manual. Odessa, FL: Psychological
Assessment Resources.
Briere, J. (1997). Psychological assessment of adult posttraumatic states. (1st ed.) Washington, DC:
American Psychological Association.
Briere, J. (2001). Detailed assessment of posttraumatic stress: Professional manual. Odessa, FL:
Psychological Assessment Resources.
Briere, J. & Scott, C. (2006). Central issues in trauma treatment. In Principles of trauma therapy: A guide
to symptoms, evaluation, and treatment (pp. 67–85). Thousand Oaks, CA: Sage Publications.
Briere, J. & Scott, C. (2006). Principles of trauma therapy: A guide to symptoms, evaluation, and
treatment. Thousand Oaks, CA: Sage Publications.
Briere, J. & Spinazzola, J. (2009). Assessment of the sequelae of complex trauma: Evidence-based
measures. In C.A.Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based
guide (pp. 104–123). New York: Guilford Press.Brohawn, K. H., Offringa, R., Pfaff, D. L., Hughes,
K. C., & Shin, L. M. (2010). The neural correlates of emotional memory in posttraumatic stress
disorder. Biological Psychiatry, 68, 1023–1030.
Bronfenbrenner, U. & Ceci, S. J. (1994). Nature–nurture reconceptualized in developmental perspective: A
bioecological model. Psychological Review, 101, 568–586.
3-14 Part 3, Section 3—General Bibliography
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design.
Cambridge, Mass: Harvard University Press.
Brooks, R., Silove, D., Bryant, R., O’Donnell, M., Creamer, M., & McFarlane, A. (2008). A confirmatory
factor analysis of the acute stress disorder interview. Journal of Traumatic Stress, 21, 352–355.
Brown, D. (2009). Assessment of attachment and abuse history, and adult attachment style. In C. A.
Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 124–144).
New York: Guilford Press.
Brown, L. M., Shiang, J., & Bongar, B. (2003). Crisis intervention. In Handbook of psychology: Clinical
psychology, Vol. 8 (pp. 431–451). Hoboken: John Wiley and Sons, Inc.
Brown, L. S. (2008a). Entering the healing process. In Cultural competence in trauma therapy: Beyond the
flashback (pp. 61–93). Washington, DC: American Psychological Association.
Brown, L. S. (2008b). Feminist therapy. In J. L. Lebow (Ed.), Twenty-first century psychotherapies:
Contemporary approaches to theory and practice (pp. 277–306). Hoboken, NJ: John Wiley and Sons,
Inc.
Brown, L. S. (2009). Cultural competence. In C. A. Courtois & J. D. Ford (Eds.), Treating complex
traumatic stress disorders: An evidence-based guide (pp. 166–182). New York: Guilford Press.
Brown, P. J., Read, J. P., & Kahler, C. W. (2003). Comorbid posttraumatic stress disorder and substance
use disorders: Treatment outcomes and the role of coping. In P. Ouimette & P. J. Brown (Eds.),
Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders (pp.
171–188). Washington, DC: American Psychological Association.
Brown, P. J., Stout, R. L., & Gannon-Rowley, J. (1998). Substance use disorder–PTSD comorbidity:
Patients’ perceptions of symptom interplay and treatment issues. Journal of Substance Abuse
Treatment, 15, 445–448.
Brown, T. A., Campbell, L. A., Lehman, C. L., Grisham, J. R., & Mancill, R. B. (2001). Current and
lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of
Abnormal Psychology, 110, 585–599.
Bryant, R. (2011). Post-traumatic stress disorder vs. traumatic brain injury. Dialogues in Clinical
Neuroscience, 13, 251–262.
Bryant, R. A. & Harvey, A. G. (2000). Acute stress disorder: A handbook of theory, assessment, and
treatment. (1st ed.) Washington, DC: American Psychological Association.
Bryant, R. A. & Harvey, A. G. (2003). Gender differences in the relationship between acute stress disorder
and posttraumatic stress disorder following motor vehicle accidents. Australian and New Zealand
Journal of Psychiatry, 37, 226–229.
Bryant, R. A. & Litz, B. T. (2006). Intermediate Interventions. In E. C. Ritchie, P. J. Watson, & M. J.
Friedman (Eds.), Interventions following mass violence and disasters: Strategies for mental health
practice (pp. 155–173). New York: Guilford Press.
Bryant, R. A. (2011). Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic
review. Journal of Clinical Psychiatry, 72, 233–239.
Trauma-Informed Care in Behavioral Health Services 3-15
Bryant, R. A. (2011). Psychological interventions for trauma exposure and PTSD. In D.J.Stein, M. J.
Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 171–202). Chichester, UK: John
Wiley & Sons.
Bryant, R. A., Creamer, M., O’Donnell, M., Silove, D., & McFarlane, A. C. (2011). Heart rate after trauma
and the specificity of fear circuitry disorders. Psychological Medicine: A Journal of Research in
Psychiatry and the Allied Sciences, 41, 2573–2580.
Bryant, R. A., Felmingham, K. L., Falconer, E. M., Pe, B. L., Dobson-Stone, C., Pierce, K. D. et al.
(2010). Preliminary evidence of the short allele of the serotonin transporter gene predicting poor
response to cognitive behavior therapy in posttraumatic stress disorder. Biological Psychiatry, 67,
1217–1219.
Bryant, R. A., Harvey, A. G., Guthrie, R. M., & Moulds, M. L. (2003). Acute psychophysiological arousal
and posttraumatic stress disorder: A two-year prospective study. Journal of Traumatic Stress, 16,
439–443.
Bryant, R. A., Mastrodomenico, J., Felmingham, K. L., Hopwood, S., Kenny, L., Kandris, E. et al. (2008).
Treatment of acute stress disorder: A randomized controlled trial. Archives of General Psychiatry, 65,
659–667.
Bryant, R. A., Moulds, M. L., & Guthrie, R. M. (2000). Acute Stress Disorder Scale: A self-report measure
of acute stress disorder. Psychological Assessment, 12, 61–68.
Bryant, R. A., Moulds, M. L., Guthrie, R. M., Dang, S. T., Mastrodomenico, J., Nixon, R. D. et al. (2008).
A randomized controlled trial of exposure therapy and cognitive restructuring for posttraumatic stress
disorder. Journal of Consulting and Clinical Psychology, 76, 695–703.
Bryant, R. A., Moulds, M. L., Guthrie, R. M., Dang, S. T., Mastrodomenico, J., Nixon, R. D. et al. (2008).
A randomized controlled trial of exposure therapy and cognitive restructuring for posttraumatic stress
disorder. Journal of Consulting and Clinical Psychology, 76, 695–703.
Bryant, R. A., Moulds, M. L., Mastrodomenico, J., Hopwood, S., Felmingham, K., & Nixon, R. D. V.
(2007). Who drops out of treatment for post-traumatic stress disorder? Clinical Psychologist, 11, 13–
15.
Bryant-Davis, T. & Ocampo, C. (2005). Racist incident based trauma. The Counseling Psychologist, 33,
479–500.
Brymer, M., Jacobs, A., Layne, C., Pynoos, R., Ruzek, J., Steinberg, A. et al. (2006). Appendix E:
Handouts: Connecting with others: Seeking Social Support (Rep. No. 2nd). White River Junction,
VT: National Center for PTSD.
Bugg, A., Turpin, G., Mason, S., & Scholes, C. (2009). A randomised controlled trial of the effectiveness
of writing as a self-help intervention for traumatic injury patients at risk of developing post-traumatic
stress disorder. Behaviour Research and Therapy, 47, 6–12.
Burke, P. A., Carruth, B., & Prichard, D. (2006). Counselor self-care in work with traumatized addicted
people. In B. Carruth (Ed.), Psychological trauma and addiction treatment (pp. 283–302). New York:
Haworth Press.
Burnam, M. A., Meredith, L. S., Tanielian, T., & Jaycox, L. H. (2009). Mental health care For Iraq and
Afghanistan war veterans. Health Affairs, 28, 771–782.
3-16 Part 3, Section 3—General Bibliography
Byers, A. L., Yaffe, K., Covinsky, K. E., Friedman, M. B., & Bruce, M. L. (2010). High occurrence of
mood and anxiety disorders among older adults: The National Comorbidity Survey Replication.
Archives of General Psychiatry, 67, 489–496.
Byers, M. G., Allison, K. M., Wendel, C. S., & Lee, J. K. (2010). Prazosin versus quetiapine for nighttime
posttraumatic stress disorder symptoms in veterans: An assessment of long-term comparative
effectiveness and safety. Journal of Clinical Psychopharmacology, 30, 225–229.
Cahill, S. P., Foa, E. B., Hembree, E. A., Marshall, R. D., & Nacash, N. (2006). Dissemination of exposure
therapy in the treatment of posttraumatic stress disorder. Journal of Traumatic Stress, 19, 597–610.
Cahill, S. P., Rothbaum, B. O., Resick, P. A., & Follette, V. M. (2009). Cognitive–behavioral therapy for
adults. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for
PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.) (pp.
139–222). New York: Guilford Press.
Caldwell, B. A. & Redeker, N. (2005). Sleep and trauma: An overview. Issues in Mental Health Nursing,
26, 721–738.
Callcott, P., Dudley, R., Standart, S., Freeston, M., & Turkington, D. (2011). Treating trauma in people
with first-episode psychosis using cognitive behavioural therapy. In CBT for psychosis: A symptom-
based approach (pp. 175–192). New York: Routledge/Taylor & Francis Group.
Campbell, R., Dworkin, E., & Cabral, G. (2009). An ecological model of the impact of sexual assault on
women’s mental health. Trauma Violence Abuse, 10, 225–246.
Campbell-Sills, L. & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor–Davidson
Resilience Scale (CD–RISC): Validation of a 10-item measure of resilience. Journal of Traumatic
Stress, 20, 1019–1028.
Cardeña, E. & Croyle, K. (2005). Acute reactions to trauma and psychotherapy: A multidisciplinary and
international perspective. Binghamton, NY: Haworth Medical Press.
Cardeña, E. & Carlson, E. (2011). Acute stress disorder revisited. Annual Review of Clinical Psychology,
7, 245–267.
Cardeña, E., Koopman, C., Classen, C., Waelde, L. C., & Spiegel, D. (2000). Psychometric properties of
the Stanford Acute Stress Reaction Questionnaire (SASRQ): A valid and reliable measure of acute
stress. Journal of Traumatic Stress, 13, 719–734.
Cardeña, E., Maldonado, J. R., Hart, O. V. D., & Spiegel, D. (2009). Hypnosis. In E. B. Foa, T. M. Keane,
M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines from the
International Society for Traumatic Stress Studies (2nd ed.) (pp. 427–457). New York: Guilford
Press.
Carleton, R. N. & Asmundson, G. J. G. (2007). Review of cognitive–behavioral therapies for trauma (2nd
edition). Canadian Psychology/Psychologie canadienne, 48, 201–203.
Carleton, R. N. & Carleton, N. (2007). Review of Clinician’s guide to PTSD: A cognitive–behavioral
approach. Cognitive Behaviour Therapy, 36, 123–124.
Carleton, R. N., Peluso, D. L., Collimore, K. C., & Asmundson, G. J. (2011). Social anxiety and
posttraumatic stress symptoms: the impact of distressing social events. Journal of Anxiety Disorders,
25, 49–57.
Trauma-Informed Care in Behavioral Health Services 3-17
Carlson, B. E. (2005). The most important things learned about violence and trauma in the past 20 years.
Journal of Interpersonal Violence, 20, 119–126.
Carlson, E. B. & Putnam, F. W. (1993). An update on the Dissociative Experiences Scale. Dissociation, 6,
16–27.
Carlson, E. B. & Rosser-Hogan, R. (1994). Cross-cultural response to trauma: A study of traumatic
experiences and posttraumatic symptoms in Cambodian refugees. Journal of Traumatic Stress, 7, 43–
58.
Carlson, E. B., Lauderdale, S., Hawkins, J., & Sheikh, J. I. (2008). Posttraumatic stress and aggression
among veterans in long-term care. Journal of Geriatric Psychiatry and Neurology;Journal of
Geriatric Psychiatry and Neurology, 21, 61–71.
Carney, C. E. & Edinger, J. D. (2010). Insomnia and anxiety. New York: Springer Publishing Science +
Business Media.
Carroll, J. F. X. & McGinley, J. J. (2001). A screening form for identifying mental health problems in
alcohol/other drug dependent persons. Alcoholism Treatment Quarterly, 19, 33–47.
Carswell, K., Blackburn, P., & Barker, C. (2011). The relationship between trauma, post-migration
problems and the psychological well-being of refugees and asylum seekers. International Journal of
Social Psychiatry, 57, 107–119.
Casteel, C., Martin, S. L., Smith, J. B., Gurka, K. K., & Kupper, L. L. (2008). National study of physical
and sexual assault among women with disabilities. Injury Prevention, 14, 87–90.
Castro, C. A., Engel, C. C., Jr., & Adler, A. B. (2004). The challenge of providing mental health
prevention and early intervention in the U.S. military. In Early intervention for trauma and traumatic
loss (pp. 301–318). New York: Guilford Press.
Catalano, S. (2012). Intimate partner violence in the U.S. Washington, DC: Bureau of Justice Statistics.
Catalano, S. M. (2004). Criminal Victimization, 2003. Washington, DC: Bureau of Justice Statistics.
Center for Mental Health Services (1996). Responding to the needs of people with serious and persistent
mental illness in times of major disaster (Rep. No. SMA 96-3077). Rockville, MD: Substance Abuse
and Mental Health Services Administration.
Center for Mental Health Services (2002). Dealing with the effects of trauma: A self-help guide. Rockville,
MD: Substance Abuse and Mental Health Services Administration.
Center for Mental Health Services (2003). Center for Mental Health Services Division of Prevention,
Traumatic Stress and Special Programs, Emergency Mental Health and Traumatic Stress Services
Branch: Fact sheet. Rockville, MD: Center for Mental Health Services.
Center for Mental Health Services, Substance Abuse and Mental Health Services Administration (2005).
Roadmap to seclusion and restraint free mental health services. Rockville, MD: Substance Abuse and
Mental Health Services Administration.
Center for Substance Abuse Treatment. (1993a). Improving treatment for drug-exposed infants. Treatment
Improvement Protocol (TIP) Series 5. HHS Publication No. (SMA) 95-3057. Rockville, MD:
Substance Abuse and Mental Health Services Administration.
3-18 Part 3, Section 3—General Bibliography
Center for Substance Abuse Treatment. (1993b). Pregnant, substance-using women. Treatment
Improvement Protocol (TIP) Series 2. (HHS Publication No. (SMA) 93-1998). Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (1993c). Screening for infectious diseases among substance
abusers. Treatment Improvement Protocol (TIP) Series 6. (HHS Publication No. (SMA) 95-3060).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment (1994). Simple screening instruments for outreach for alcohol and
other drug abuse and infectious diseases (Rep. No. HHS Publication No. (SMA) 94-2094). Rockville,
MD: Center for Substance Abuse Treatment.
Center for Substance Abuse Treatment. (1995a). Alcohol and other drug screening of hospitalized trauma
patients. Treatment Improvement Protocol (TIP) Series 16. (HHS Publication No. (SMA) 95-3041).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (1995b). Combining alcohol and other drug treatment with
diversion for juveniles in the justice system. Treatment Improvement Protocol (TIP) Series 21. (HHS
Publication No. (SMA) 95-3051). Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Center for Substance Abuse Treatment. (1995c). Developing state outcomes monitoring systems for
alcohol and other drug abuse treatment. Treatment Improvement Protocol (TIP) Series 14. (HHS
Publication No. (SMA) 95-3031). Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Center for Substance Abuse Treatment. (1995d). The role and current status of patient placement criteria
in the treatment of substance use disorders. Treatment Improvement Protocol (TIP) Series 13. (HHS
Publication No. (SMA) 95-3021). Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Center for Substance Abuse Treatment. (1995e). The tuberculosis epidemic: Legal and ethical issues for
alcohol and other drug abuse treatment providers. Treatment Improvement Protocol (TIP) Series 18.
(HHS Publication No. (SMA) 95-3047). Rockville, MD: Substance Abuse and Mental Health
Services Administration.
Center for Substance Abuse Treatment. (1996). Treatment drug courts: Integrating substance abuse
treatment with legal case processing. Treatment Improvement Protocol (TIP) Series 23. (HHS
Publication No. (SMA) 96-3113). Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Center for Substance Abuse Treatment (1997a). A guide to substance abuse services for primary care
clinicians (Rep. No. HHS Publication No. (SMA) 97-3139). Rockville, MD: Substance Abuse and
Mental Health Administration.
Center for Substance Abuse Treatment (1997b). Substance abuse treatment and domestic violence (Rep.
No. HHS Publication No. (SMA) 97-3163). Rockville, MD: Substance Abuse and Mental Health
Services Administration.
Center for Substance Abuse Treatment. (1998a). Comprehensive case management for substance abuse
treatment. Treatment Improvement Protocol (TIP) Series 27. (HHS Publication No. (SMA) 98-3222).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Trauma-Informed Care in Behavioral Health Services 3-19
Center for Substance Abuse Treatment. (1998b). Continuity of offender treatment for substance use
disorders from institution to community. Treatment Improvement Protocol (TIP) Series 30. (HHS
Publication No. (SMA) 98-3245). Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Center for Substance Abuse Treatment. (1998c). Naltrexone and alcoholism treatment. Treatment
Improvement Protocol (TIP) Series 28. (HHS Publication No. (SMA) 98-3206). Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (1998d). Substance abuse among older adults. Treatment
Improvement Protocol (TIP) Series 26. (HHS Publication No. (SMA) 98-3179). Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (1998e). Substance use disorder treatment for people with physical
and cognitive disabilities. Treatment Improvement Protocol (TIP) Series 29. (HHS Publication No.
(SMA) 98-3249). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (1999a). Brief interventions and brief therapies for substance
abuse. Treatment Improvement Protocol (TIP) Series 34. (HHS Publication No. (SMA) 99-3353).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment (1999b). Cultural issues in substance abuse treatment (Rep. No.
HHS Publication No. (SMA) 99-3278). Rockville, MD: Center for Substance Abuse Treatment.
Center for Substance Abuse Treatment (1999e). Enhancing motivation for change in substance abuse
treatment (Rep. No. HHS Publication No. (SMA) 99–3354). Rockville, MD: Center for Substance
Abuse Treatment.
Center for Substance Abuse Treatment (1999c). Screening and assessing adolescents for substance use
disorders (Rep. No. HHS Publication No. (SMA) 99-3282). Rockville, MD: Substance Abuse and
Mental Health Services Administration.
Center for Substance Abuse Treatment. (1999d). Treatment of adolescents with substance use disorders.
Treatment Improvement Protocol (TIP) Series 32. (HHS Publication No. (SMA) 99-3283). Rockville,
MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (1999e). Treatment for stimulant use disorders. Treatment
Improvement Protocol (TIP) Series 33. (HHS Publication No. (SMA) 99-3296). Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2000a). Integrating substance abuse treatment and vocational
services. Treatment Improvement Protocol (TIP) Series 38. (HHS Publication No. (SMA) 00-3470).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment (2000b). Substance abuse treatment for persons with child abuse
and neglect issues (Rep. No. HHS Publication No. (SMA) 00-3357). Rockville, MD: Substance
Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2000c). Substance abuse treatment for persons with HIV/AIDS.
Treatment Improvement Protocol (TIP) Series 37. (HHS Publication No. (SMA) 00-3459). Rockville,
MD: Substance Abuse and Mental Health Services Administration.
3-20 Part 3, Section 3—General Bibliography
Center for Substance Abuse Treatment (2001). A provider’s introduction to substance abuse treatment for
lesbian, gay, bisexual, and transgender individuals (Rep. No. HHS Publication No. (SMA) 01-3498).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2004b). Substance abuse treatment and family therapy. Treatment
Improvement Protocol (TIP) Series 39. (HHS Publication No. (SMA) 04-3957). Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2005a). Medication-assisted treatment for opioid addiction.
Treatment Improvement Protocol (TIP) Series 43. (HHS Publication No. SMA 05-4048). Rockville,
MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2005b). Substance abuse treatment for adults in the criminal
justice system. Treatment Improvement Protocol (TIP) Series 44. (HHS Publication No. (SMA) 05-
4056). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment (2005c). Substance abuse treatment for persons with co-occurring
disorders (Rep. No. Treatment Improvement Protocol (TIP) Series 42 HHS Publication No. SMA 05-
3992). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2005d). Substance abuse treatment: Group therapy. Treatment
Improvement Protocol (TIP) Series 41. (HHS Publication No. SMA 05-4056). Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2006a). Detoxification and substance abuse treatment. Treatment
Improvement Protocol (TIP) Series 45. (HHS Publication No. SMA 06-4131). Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2006b). Substance abuse: Administrative issues in intensive
outpatient treatment. Treatment Improvement Protocol (TIP) Series 46. (HHS Publication No. SMA
06-4151). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. (2006c). Substance abuse: Clinical issues in intensive outpatient
treatment. Treatment Improvement Protocol (TIP) Series 47. (HHS Publication No. SMA 06-4182).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment (2008). Managing depressive symptoms in substance abuse clients
during early recovery (Rep. No. Treatment Improvement Protocol (TIP) Series 48. HHS Publication
No. (SMA) 08-4353.). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment (2009a). Addressing suicidal thoughts and behaviors in substance
abuse treatment (Rep. No. Treatment Improvement Protocol (TIP) Series 50. HHS Publication No.
(SMA) 09-4381). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment (2009b). Clinical supervision and professional development of the
substance abuse counselor Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Center for Substance Abuse Treatment. (2009c). Incorporating alcohol pharmacotherapies into medical
practice. Treatment Improvement Protocol (TIP) Series 49. (HHS Publication No. SMA 09-4380).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Trauma-Informed Care in Behavioral Health Services 3-21
Center for Substance Abuse Treatment (2009d). Substance abuse treatment: Addressing the specific needs
of women (Rep. No. HHS Publication No. (SMA) 09-4426). Rockville, MD: Substance Abuse and
Mental Health Services Administration.
Center for Substance Abuse Treatment (2009d). What are peer recovery support services? (Rep. No. HHS
Publication No. (SMA) 09-4454). Rockville, MD: Substance Abuse and Mental Health Services
Administration, U.S. Department of Health and Human Services.
Centers for Disease Control & Prevention (2011). Adverse childhood experiences (ACE) study. Atlanta,
GA: Centers for Disease Control and Prevention.
Centers for Disease Control & Prevention (2012). Publications by health outcome. Atlanta, GA: Centers
for Disease Control and Prevention.
Centre for Addiction and Mental Health (2011). Are you trauma-informed? Toronto, Ontario: Centre for
Addiction and Mental Health.
Centre for Clinical Interventions (2008). Calming technique. Northbridge, Western Australia: Centre for
Clinical Interventions.
Chaikin, N. D. & Prout, M. F. (2004). Treating complex trauma in women within community mental
health. American Journal of Orthopsychiatry, 74, 160–173.
Chambless, D. L. & Hollon, S. D. (1998). Defining empirically supported therapies. Journal of Consulting
and Clinical Psychology, 66, 7–18.
Charney, D. S. & Manji, H. K. (2004). Life stress, genes, and depression: Multiple pathways lead to
increased risk and new opportunities for intervention. Science Signaling, 2004, re5.
Chaudieu, I., Norton, J., Ritchie, K., Birmes, P., Vaiva, G., & Ancelin, M. L. (2011). Late-life health
consequences of exposure to trauma in a general elderly population: The mediating role of
reexperiencing posttraumatic symptoms. Journal of Clinical Psychiatry, 72, 929–935.
Chen, K. W., Banducci, A. N., Guller, L., Macatee, R. J., Lavelle, A., Daughters, S. B. et al. (2011). An
examination of psychiatric comorbidities as a function of gender and substance type within an
inpatient substance use treatment program. Drug and Alcohol Dependence, 118, 92–99.
Chen, L. P., Murad, M. H., Paras, M. L., Colbenson, K. M., Sattler, A. L., Goranson, E. N. et al. (2010).
Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis.
Mayo Clinic Proceedings, 85, 618–629.
Cherpitel, C. J. (1997). Alcohol and violence-related injuries in the emergency room. Recent Developments
in Alcoholism, 13, 105–118.
Chessen, C. E., Comtois, K. A., & Landes, S. J. (2011). Untreated posttraumatic stress among persons with
severe mental illness despite marked trauma and symptomatology. Psychiatric Services, 62, 1201–
1206.
Cheung, P. (1994). Posttraumatic stress disorder among Cambodian refugees in New Zealand.
International Journal of Social Psychiatry, 40, 17–26.
Chilcoat, H. D. & Breslau, N. (1998). Investigations of causal pathways between PTSD and drug use
disorders. Addictive Behaviors, 23, 827–840.
3-22 Part 3, Section 3—General Bibliography
Chilcoat, H. D. & Breslau, N. (1998). Posttraumatic stress disorder and drug disorders: Testing causal
pathways. Archives of General Psychiatry, 55, 913–917.
Chiu, K. B., deRoon-Cassini, T. A., & Brasel, K. J. (2011). Factors identifying risk for psychological
distress in the civilian trauma population. Academic Emergency Medicine, 18, 1156–1160.
Choi, D. C., Rothbaum, B. O., Gerardi, M., & Ressler, K. J. (2010). Pharmacological enhancement of
behavioral therapy: focus on posttraumatic stress disorder. Current Topics in Behavioral
Neurosciences, 2, 279–299.
Christensen, R. C., Hodgkins, C. C., Garces, L. K., Estlund, K. L., Miller, M. D., & Touchton, R. (2005).
Homeless, mentally ill and addicted: The need for abuse and trauma services. Journal of Health Care
for the Poor and Underserved, 16, 615–621.
Cicchetti, D. & Valentino, K. (2006). An ecological–transactional perspective on child maltreatment:
Failure of the average expectable environment and its influence on child development. In
Developmental psychopathology, Vol 3: Risk, disorder, and adaptation (2nd ed.) (pp. 129–201).
Hoboken, NJ: John Wiley and Sons, Inc.
Cimmarusti, R. A. & Gamero, S. L. (2009). Compassionate accountability in residential care: A trauma
informed model. Residential Treatment for Children & Youth, 26, 181–193.
Claes, L., Vandereycken, W., & Vertommen, H. (2005). Self-care versus self-harm: Piercing, tattooing,
and self-injuring in eating disorders. European Eating Disorders Review, 13, 11–18.
Clark, C. & Fearday, F. E. (2003). Triad women’s project: Group facilitator’s manual. Tampa, FL: Louis
de la Parte Florida Mental Health Institute, University of South Florida.
Clark, C. R., McFarlane, A. C., Morris, P., Weber, D. L., Sonkkilla, C., Shaw, M. et al. (2003). Cerebral
function in posttraumatic stress disorder during verbal working memory updating: A positron
emission tomography study. Biological Psychiatry, 53, 474–481.
Clark, C., Young, M. S., Jackson, E., Graeber, C., Mazelis, R., Kammerer, N. et al. (2008). Consumer
perceptions of integrated trauma-informed services among women with co-occurring disorders. The
Journal of Behavioral Health Services & Research, 35, 71–90.
Classen, C. C., Palesh, O. G., & Aggarwal, R. (2005). Sexual revictimization: A review of the empirical
literature. Trauma, Violence, & Abuse, 6, 103–129.
Classen, C. C., Palesh, O. G., Cavanaugh, C., Koopman, C., Kaupp, J. W., Kraemer, H. C. et al. (2011). A
comparison of trauma-focused and present-focused group therapy for survivors of childhood sexual
abuse: A randomized controlled trial. Psychological Trauma: Theory, Research, Practice, and Policy,
3, 84–93.
Classen, C., Koopman, C., Nevill-Manning, K., & Spiegel, D. (2001). A preliminary report comparing
trauma-focused and present-focused group therapy against a wait-listed condition among childhood
sexual abuse survivors with PTSD. Journal of Aggression, Maltreatment & Trauma, 4, 265–288.
Cloitre, M. (2009). Effective psychotherapies for posttraumatic stress disorder: A review and critique. CNS
Spectrums, 14, 32–43.
Cloitre, M., Courtois, C. A., Charuvastra, A., Carapezza, R., Stolbach, B. C., & Green, B. L. (2011).
Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. Journal
of Traumatic Stress, 24, 615–627.
Trauma-Informed Care in Behavioral Health Services 3-23
Cloitre, M., Koenen, K. C., Cohen, L. R., & Han, H. (2002). Skills training in affective and interpersonal
regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse.
Journal of Consulting and Clinical Psychology, 70, 1067–1074.
Cloitre, M., Petkova, E., Wang, J., & Lu, L. F. (2012). An examination of the influence of a sequential
treatment on the course and impact of dissociation among women with PTSD related to childhood
abuse. Depression and Anxiety.
Cloitre, M., Stovall–McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L. et al. (2010).
Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of
Psychiatry, 167, 915–924.
Cocozza, J. J., Jackson, E. W., Hennigan, K., Morrissey, J. P., Reed, B. G., Fallot, R. et al. (2005).
Outcomes for women with co-occurring disorders and trauma: Program-level effects. Journal of
Substance Abuse Treatment, 28, 109–119.
Coffey, S. F., Dansky, B. S., & Brady, K. T. (2003). Exposure-based, trauma focused therapy for comorbid
posttraumatic stress disorder–substance use disorder. In P. Ouimette & P. J. Brown (Eds.), Trauma
and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders (pp. 127–146).
Washington, DC: American Psychological Association.
Coffey, S. F., Schumacher, J. A., Brady, K. T., & Dansky, B. S. (2003). Reductions in trauma
symptomalogy during acute and protracted alcohol and cocaine abstinence. Symposium Conducted
at the Annual Meeting of the International Society for Traumatic Stress Studies, Chicago, IL.
Coffey, S. F., Schumacher, J. A., Brimo, M. L., & Brady, K. T. (2005). Exposure therapy for substance
abusers with PTSD: translating research to practice. Behavior Modification, 29, 10–38.
Cohen, H., Kaplan, Z., Matar, M. A., Loewenthal, U., Zohar, J., & Richter-Levin, G. (2007). Long–lasting
behavioral effects of juvenile trauma in an animal model of PTSD associated with a failure of the
autonomic nervous system to recover. European Neuropsychopharmacology, 17, 464–477.
Cohen, J. A., Mannarino, A. P., & Murray, L. K. (2011). Trauma-focused CBT for youth who experience
ongoing traumas. Child Abuse & Neglect, 35, 637–646.
Cohen, L. R. & Hien, D. A. (2006). Treatment outcomes for women with substance abuse and PTSD who
have experienced complex trauma. Psychiatric Services, 57, 100–106.
Cohen, P. F. (2004). The care and feeding of the therapist in times of trauma. Psychoanalysis &
Psychotherapy, 21, 81–99.
Coker, A. L., Weston, R., Creson, D. L., Justice, B., & Blakeney, P. (2005). PTSD symptoms among men
and women survivors of intimate partner violence: The role of risk and protective factors. Violence
and Victims, 20, 625–643.
Collimore, K. C., Carleton, R. N., Hofmann, S. G., & Asmundson, G. J. G. (2010). Posttraumatic stress
and social anxiety: The interaction of traumatic events and interpersonal fears. Depression and
Anxiety, 27, 1017–1026.
Collins, S. & Long, A. (2003). Too tired to care? The psychological effects of working with trauma.
Journal of Psychiatric and Mental Health Nursing, 10, 17–27.
3-24 Part 3, Section 3—General Bibliography
Collishaw, S., Pickles, A., Messer, J., Rutter, M., Shearer, C., & Maughan, B. (2007). Resilience to adult
psychopathology following childhood maltreatment: Evidence from a community sample. Child
Abuse & Neglect, 31, 211–229.
Committee on Treatment of Posttraumatic Stress Disorder & Institute of Medicine (2008). Treatment of
posttraumatic stress disorder: An assessment of the evidence. The National Academies Press.
Community Connections (2002). Trauma and abuse in the lives of homeless women and men. Washington,
DC: Community Connections, U.S. Department of Housing and Urban Development.
Conners-Burrow, N. A., Johnson, B., & Whiteside-Mansell, L. (2009). Maternal substance abuse and
children’s exposure to violence. Journal of Pediatric Nursing, 24, 360–368.
Connor, K. M. & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor-Davidson
Resilience Scale (CD-RISC). Depression and Anxiety, 18, 76–82.
Connors, G. J., Donovan, D. M., & DiClemente, C. C. (2001). Substance abuse treatment and the stages of
change, selecting and planning interventions. New York: Guilford Press.
Cook, A., Blaustein, M., Spinazzola, J., & van der Kolk, B. (2003). Complex trauma in children and
adolescents. Los Angeles: National Child Traumatic Stress Network.
Cook, A., Spinazzola, J., Ford, J., Lanktree, C., Blaustein, M., Cloitre, M. et al. (2005). Complex trauma in
children and adolescents. Psychiatric Annals, 35, 390–398.
Cook, F., Ciorciari, J., Varker, T., & Devilly, G. J. (2009). Changes in long term neural connectivity
following psychological trauma. Clinical Neurophysiology, 120, 309–314.
Cook, J. D. & Bickman, L. (1990). Social support and psychological symptomatology following a natural
disaster. Journal of Traumatic Stress, 3, 541–556.
Cook, J. M. & Niederehe, G. (2007). Trauma in older adults. In M. J. Friedman, T. M. Keane, & P. A.
Resick (Eds.), Handbook of PTSD: Science and practice (pp. 252–276). New York: Guilford Press.
Copeland, L. A., Zeber, J. E., Bingham, M. O., Pugh, M. J., Noël, P. H., Schmacker, E. R. et al. (2011).
Transition from military to VHA care: Psychiatric health services for Iraq/Afghanistan combat-
wounded. Journal of Affective Disorders, 130, 226–230.
Corcoran, C. B., Green, B. L., Goodman, L. A., & Krinsley, K. E. (2000). Conceptual and methodological
issues in trauma history assessment. In A. Y. Shalev, R. Yehuda, & A. C. McFarlane (Eds.),
International handbook of human response to trauma (pp. 223–232). Dordrecht, Netherlands: Kluwer
Academic Publishers.
Cornelius, M. C., Nugent, N. R., Amstadter, A. B., & Koenen, K. C. (2010). Genetics of post-traumatic
stress disorder: Review and recommendations for genome-wide association studies. Current
Psychiatry Reports, 12, 313–326.
Corry, N., Pruzinsky, T., & Rumsey, N. (2009). Quality of life and psychosocial adjustment to burn injury:
Social functioning, body image, and health policy perspectives. International Review of Psychiatry,
21, 539–548.
Cottler, L. B., Compton, W. M., Mager, D., Spitznagel, E. L., & Janca, A. (1992). Posttraumatic stress
disorder among substance users from the general population. American Journal of Psychiatry, 149,
664–670.
Trauma-Informed Care in Behavioral Health Services 3-25
Cottler, L. B., Nishith, P., & Compton, W. M. (2001). Gender differences in risk factors for trauma
exposure and post-traumatic stress disorder among inner-city drug abusers in and out of treatment.
Comprehensive Psychiatry, 42, 111–117.
Cougle, J. R., Feldner, M. T., Keough, M. E., Hawkins, K. A., & Fitch, K. E. (2010). Comorbid panic
attacks among individuals with posttraumatic stress disorder: Associations with traumatic event
exposure history, symptoms, and impairment. Journal of Anxiety Disorders, 24, 183–188.
Cougle, J. R., Timpano, K. R., Sachs-Ericsson, N., Keough, M. E., & Riccardi, C. J. (2010). Examining
the unique relationships between anxiety disorders and childhood physical and sexual abuse in the
National Comorbidity Survey–Replication. Psychiatry Research, 177, 150–155.
Coulter, S. (2011). Systemic family therapy for families who have experienced trauma: A randomised
controlled trial. British Journal of Social Work, 41, 502–519.
Courtois, C. A. (2000). Implications of the memory controversy for clinical practice: An overview of
treatment recommendations and guidelines. Journal of Child Sexual Abuse, 9, 183–210.
Courtois, C. A., Ford, J. D., & Cloitre, M. (2009). Best practices in psychotherapy for adults. In C. A.
Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 82–103).
New York: Guilford Press.
Covington, S. S. (2003). Beyond trauma: A healing journey for women: Facilitator’s guide. Center City,
Minnesota: Hazelden.
Covington, S. S. (2008). Helping women recover: A program for treating addiction. (Revised (Loose Leaf)
ed.) San Francisco: Jossey-Bass.
Covington, S. S. (2008). Women and addiction: A trauma-informed approach. Journal of Psychoactive
Drugs, Supplementement 5, 377–385.
Covington, S. S., Burke, C., Keaton, S., & Norcott, C. (2008). Evaluation of a trauma-informed and
gender-responsive intervention for women in drug treatment. Journal of Psychoactive Drugs,
Supplement 5, 387–398.
Craig, C. D. & Sprang, G. (2010). Compassion satisfaction, compassion fatigue, and burnout in a national
sample of trauma treatment therapists. Anxiety, Stress & Coping: An International Journal, 23, 319–
339.
Cross, T. L., Bazron, B. J., Dennis, K. W., & Isaacs, M. R. (1989). Towards a culturally competent system
of care: A monograph on effective services for minority children who are severely emotionally
disturbed (Vol. 1). Washington, DC: Georgetown University Child Development Center.
Cubbin, C. & Smith, G. S. (2002). Socioeconomic inequalities in injury: Critical issues in design and
analysis. Annual Review of Public Health, 23, 349–375.
Cubbin, C., LeClere, F. B., & Smith, G. S. (2000). Socioeconomic status and the occurrence of fatal and
nonfatal injury in the United States. American Journal of Public Health, 90, 70–77.
Cukor, J., Spitalnick, J., Difede, J., Rizzo, A., & Rothbaum, B. O. (2009). Emerging treatments for PTSD.
Clinical Psychology Review, 29, 715–726.
3-26 Part 3, Section 3—General Bibliography
Curie, C. G., Brounstein, P. J., & Davis, N. J. (2004). Resilience-building prevention programs that work:
A federal perspective. In C. Clauss-Ehlers & M. Weist (Eds.), Community planning to foster
resilience in children. (pp. 343–359). New York: Kluwer Academic/Plenum Publishers.
Cusack, K. J., Frueh, B. C., & Brady, K. T. (2004). Trauma history screening in a community mental
health center. Psychiatric Services, 55, 157–162.
Cusack, K. J., Grubaugh, A. L., Yim, E., Knapp, R. G., Robins, C. S., & Frueh, B. C. (2007). Are there
racial differences in the experience of harmful or traumatic events within psychiatric settings?
Psychiatric Quarterly, 78, 101–115.
Daie-Gabai, A., Aderka, I. M., Allon–Schindel, I., Foa, E. B., & Gilboa-Schechtman, E. (2011).
Posttraumatic Cognitions Inventory (PTCI): Psychometric properties and gender differences in an
Israeli sample. Journal of Anxiety Disorders, 25, 266–271.
Daly, R. J. (1983). Samuel Pepys and post-traumatic stress disorder. British Journal of Psychiatry, 143,
64–68.
Dana, R. H. (2007). Refugee assessment practices and cultural competency training. In Cross-cultural
assessment of psychological trauma and PTSD (pp. 91–112). New York: Springer Publishing Science
+ Business Media.
Danieli, Y. & Nader, K. (2006). Respecting cultural, religious, and ethnic differences in the prevention and
treatment of psychological sequelae. In Psychological effects of catastrophic disasters: Group
approaches to treatment (pp. 203–234). New York: Haworth Press.
Danieli, Y. (2007). Assessing trauma across cultures from a multigenerational perspective. In J. P. Wilson
& C. S. Tang (Eds.), Cross-cultural assessment of psychological trauma and PTSD (pp. 65–89). New
York: Springer Publishing Science + Business Media.
Danieli, Y., Brom, D., & Sills, J. (2005). Sharing knowledge and shared care. Journal of Aggression,
Maltreatment & Trauma, 10, 775–790.
Daniels, A., Grant, E., Filson, B., Powell, I., Fricks, L., & Goodale, L. (2010). Pillars of peer support:
transforming mental health systems of care through peer support services (Rep. No. January).
Chicago: Depression and Bipolar Support Alliance.
Daniels, A. S., Tunner, T. P., Ashenden, P., Bergeson, S., Fricks, L., & Powell, I. (2012). Pillars of peer
support – III: Whole health peer support services (Rep. No. January). Chicago: Depression and
Bipolar Support Alliance.
Danielson, C. K., Amstadter, A. B., Dangelmaier, R. E., Resnick, H. S., Saunders, B. E., & Kilpatrick, D.
G. (2009). Trauma-related risk factors for substance abuse among male versus female young adults.
Addict.Behav, 34, 395–399.
Dannlowski, U., Stuhrmann, A., Beutelmann, V., Zwanzger, P., Lenzen, T., Grotegerd, D. et al. (2012).
Limbic scars: Long-term consequences of childhood maltreatment revealed by functional and
structural magnetic resonance imaging. Biological Psychiatry, 71, 286–293.
Dansky, B. S., Saladin, M. E., Brady, K. T., Kilpatrick, D. G., & Resnick, H. S. (1995). Prevalence of
victimization and posttraumatic stress disorder among women with substance use disorders:
Comparison of telephone and in-person assessment samples. International Journal of the Addictions,
30, 1079–1099.
Trauma-Informed Care in Behavioral Health Services 3-27
Dass–Brailsford, P. & Myrick, A. C. (2010). Psychological trauma and substance abuse: The need for an
integrated approach. Trauma, Violence, & Abuse, 11, 202–213.
D’Augelli, A. R., Grossman, A. H., & Starks, M. T. (2006). Childhood gender atypicality, victimization,
and PTSD among lesbian, gay, and bisexual youth. Journal of Interpersonal Violence, 21, 1462–
1482.
Davidson, G., Shannon, C., Mulholland, C., & Campbell, J. (2009). A longitudinal study of the effects of
childhood trauma on symptoms and functioning of people with severe mental health problems.
Journal of Trauma Dissociation, 10, 57–68.
Davidson, J. R. & Connor, K. M. (2008). The impairment of Presidents Pierce and Coolidge after
traumatic bereavement. Comprehensive Psychiatry, 49, 413–419.
Davidson, J. R. T., Payne, V. M., Connor, K. M., Foa, E. B., Rothbaum, B. O., Hertzberg, M. A. et al.
(2005). Trauma, resilience and saliostasis: Effects of treatment in post-traumatic stress disorder.
International Clinical Psychopharmacology, 20, 43–48.
Davidson, J. R., Book, S. W., Colket, J. T., Tupler, L. A., Roth, S., David, D. et al. (1997). Assessment of
a new self-rating scale for post-traumatic stress disorder. Psychological Medicine, 27, 153–160.
Davidson, J. R., Hughes, D., Blazer, D. G., & George, L. K. (1991). Post-traumatic stress disorder in the
community: An epidemiological study. Psychological Medicine: A Journal of Research in Psychiatry
and the Allied Sciences, 21, 713–721.
Davidson, J. R., Stein, D. J., Rothbaum, B. O., Pedersen, R., Szumski, A., & Baldwin, D. S. (2011).
Resilience as a predictor of treatment response in patients with posttraumatic stress disorder treated
with venlafaxine extended release or placebo. Journal of Psychopharmacology, 26(6), 778–783.
Davidson, P. R. & Parker, K. C. (2001). Eye movement desensitization and reprocessing (EMDR): A
meta-analysis. Journal of Consulting and Clinical Psychology, 69, 305–316.
Davies, D. R., Burlingame, G. M., & Layne, C. M. (2006). Integrating small-group process principles into
trauma-focused group psychotherapy: What should a group trauma therapist know? In L. A. Schein,
H. I. Spitz, G. M. Burlingame, & P. R. Muskin (Eds.), Psychological effects of catastrophic disasters:
Group approaches to treatment (pp. 385–423). New York: Haworth Press.
Davis, J. L., Combs-Lane, A. M., & Smith, D. W. (2004). Victimization and health risk behaviors:
Implications for prevention programs. In Health consequences of abuse in the family: A clinical guide
for evidence-based practice (pp. 179–195). Washington, DC: American Psychological Association.
Davis, L. L., Leon, A. C., Toscano, R., Drebing, C. E., Ward, L. C., Parker, P. E. et al. (2012). A
randomized controlled trial of supported employment among veterans with posttraumatic stress
disorder. Psychiatric Services, 63, 464–470.
Davis, M. C., Luecken, L., & Lemery-Chalfant, K. (2009). Resilience in common life: Introduction to the
special issue. Journal of Personality, 77, 1637–1644.
Davis, R. C. & Taylor, B. G. (1999). Does batterer treatment reduce violence? A synthesis of the literature.
Women and Criminal Justice, 10, 69–93.
Davis, R. G., Ressler, K. J., Schwartz, A. C., Stephens, K. J., & Bradley, R. G. (2008). Treatment barriers
for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. Journal of
Traumatic Stress, 21, 218–222.
3-28 Part 3, Section 3—General Bibliography
De Bellis, M. D. (2002). Developmental traumatology: A contributory mechanism for alcohol and
substance use disorders. Psychoneuroendocrinology, 27, 155–170.
de Fabrique, N., Van Hasselt, V. B., Vecchi, G. M., & Romano, S. J. (2007). Common variables associated
with the development of Stockholm Syndrome: Some case examples. Victims & Offenders, 2, 91–98.
de Girolamo, G. (1993). International perspectives on the treatment and prevention of posttraumatic stress
disorder. In J. P. Wilson & Raphael Beverley (Eds.), International handbook of traumatic stress
syndrome (pp. 935–946). New York: Plenum Press.
de Snyder, V., Friel, S., Fotso, J., Khadr, Z., Meresman, S., Monge, P. et al. (2011). Social conditions and
urban health inequities: Realities, challenges and opportunities to transform the urban landscape
through research and action. Journal of Urban Health, 88, 1183–1193.
Deahl, M. P., Klein, S., & Alexander, D. A. (2011). The costs of conflict: Meeting the mental health needs
of serving personnel and service veterans. International Review of Psychiatry, 23, 201–209.
DeBate, R. D. & Pyle, G. F. (2004). The Behavioral Ecological Model: A framework for early WIC
participation. American Journal of Health Studies, 19, 138–147.
Dedert, E. A., Wilson, S. M., Calhoun, P. S., Moore, S. D., Hamlett–Berry, K. W., & Beckham, J. C.
(2010). Public health clinical demonstration project for smoking cessation in veterans with
posttraumatic stress disorder. Addictive Behaviors, 35, 19–22.
Deighton, R. M., Gurris, N., & Traue, H. (2007). Factors affecting burnout and compassion fatigue in
psychotherapists treating torture survivors: Is the therapist’s attitude to working through trauma
relevant? Journal of Traumatic Stress, 20, 63–75.
Dekel, R. & Goldblatt, H. (2008). Is there intergenerational transmission of trauma? The case of combat
veterans’ children. American Journal of Orthopsychiatry, 78, 281–289.
Dekel, R. & Solomon, Z. (2007). Secondary traumatization among wives of war veterans with PTSD. In C.
R. Figley & W. P. Nash (Eds.), Combat stress injury: Theory, research, and management (pp. 137–
157). New York: Routledge/Taylor & Francis Group.
Del Gaizo, A. L., Elhai, J. D., & Weaver, T. L. (2011). Posttraumatic stress disorder, poor physical health
and substance use behaviors in a national trauma-exposed sample. Psychiatry Research, 188, 390–
395.
Delahanty, D. L. (2008). The psychobiology of trauma and resilience across the lifespan. Lanham, MD:
Jason Aronson.
Dell’Osso, L., Carmassi, C., Rucci, P., Capparelli, A., Paggini, R., Ramacciotti, C. E. et al. (2009).
Lifetime subthreshold mania is related to suicidality in posttraumatic stress disorder. CNS Spectrums,
14, 262–266.
dePanfilis, D. (2006). Child neglect: A guide for prevention, assessment, and intervention. Washington,
DC: U.S. Department of Health and Human Services, Administration for Children and Families,
Administration on Children, Youth and Families Children’s Bureau, Office on Child Abuse and
Neglect.
Department of Veterans Affairs & Department of Defense (2010). VA/DoD clinical practice guideline for
management of post-traumatic stress. Washington, DC: U.S. Department of Defense.
Trauma-Informed Care in Behavioral Health Services 3-29
DeSilva M., Maclachlan, M., Devane, D., Desmond, D., Gallagher, P., Schnyder, U. et al. (2009).
Psychosocial interventions for the prevention of disability following traumatic physical injury.
Cochrane Database of Systematic Reviews, CD006422.
Devilly, G. J. & Annab, R. (2008). A randomised controlled trial of group debriefing. Journal of Behavior
Therapy and Experimental Psychiatry, 39, 42–56.
Devilly, G. J. & Varker, T. (2008). The effect of stressor severity on outcome following group debriefing.
Behaviour Research and Therapy, 46, 130–136.
Devilly, G. J., Gist, R., & Cotton, P. (2006). Ready! Fire! Aim! The status of psychological debriefing and
therapeutic interventions: In the work place and after disasters. Review of General Psychology, 10,
318–345.
DeViva, J. C., Zayfert, C., Pigeon, W. R., & Mellman, T. A. (2005). Treatment of residual insomnia after
CBT for PTSD: Case studies. Journal of Traumatic Stress, 18, 155–159.
DeWolfe, D. J. (2000). Training manual: For mental health and human service workers in major disasters
(Rep. No. ADM 90–538). Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Dietz, P. M., Spitz, A. M., Anda, R. F., Williamson, D. F., McMahon, P. M., Santelli, J. S. et al. (1999).
Unintended pregnancy among adult women exposed to abuse or household dysfunction during their
childhood. JAMA, 282, 1359–1364.
Difede, J., Malta, L. S., Best, S., Henn–Haase, C., Metzler, T., Bryant, R. et al. (2007). A randomized
controlled clinical treatment trial for World Trade Center attack-related PTSD in disaster workers.
Journal of Nervous and Mental Disease, 195, 861–865.
DiGrande, L., Neria, Y., Brackbill, R. M., Pulliam, P., & Galea, S. (2011). Long-term posttraumatic stress
symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World
Trade Center. American Journal of Epidemiology, 173, 271–281.
DiGrande, L., Perrin, M. A., Thorpe, L. E., Thalji, L., Murphy, J., Wu, D. et al. (2008). Posttraumatic
stress symptoms, PTSD, and risk factors among lower Manhattan residents 2–3 years after the
September 11, 2001 terrorist attacks. Journal of Traumatic Stress, 21, 264–273.
Dillon, J. R. (2001). Internalized homophobia, attributions of blame, and psychological distress among
lesbian, gay, and bisexual trauma victims. Dissertation Abstracts International: Section B: the
Sciences & Engineering, 62, 2054.
Dipietro, F. (2006). Vicarious trauma and compassion fatigue in battered women’s advocates: A
secondary prevention program. Ann Arbor, MI: ProQuest Information & Learning.
Dirkzwager, A. J. E., Grievink, L., van der Velden, P. G., & Yzermans, C. J. (2006). Risk factors for
psychological and physical health problems after a man–made disaster: Prospective study. British
Journal of Psychiatry, 189, 144–149.
Doctor, J. N., Zoellner, L. A., & Feeny, N. C. (2011). Predictors of health-related quality-of-life utilities
among persons with posttraumatic stress disorder. Psychiatric Services, 62, 272–277.
Dohrenwend, B. P., Turner, J. B., Turse, N. A., Adams, B. G., Koenen, K. C., & Marshall, R. (2006). The
psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science, 313,
979–982.
3-30 Part 3, Section 3—General Bibliography
Dohrenwend, B. P., Turner, J. B., Turse, N. A., Adams, B. G., Koenen, K. C., & Marshall, R. (2007).
Continuing controversy over the psychological risks of Vietnam for U.S. veterans. Journal of
Traumatic Stress, 20, 449–465.
Doll, L. S. & Haas, E. N. (2007). Handbook of injury and violence prevention. New York: Springer
Publishing.
Dom, G., De, W. B., Hulstijn, W., & Sabbe, B. (2007). Traumatic experiences and posttraumatic stress
disorders: Differences between treatment-seeking early- and late-onset alcoholic patients. Compr
Psychiatry, 48, 178–185.
Domino, M. E., Morrissey, J. P., Chung, S., & Nadlicki, T. (2006). Changes in service use during a
trauma-informed intervention for women. Women and Health, 44, 105–122.
Domino, M. E., Morrissey, J. P., Chung, S., Huntington, N., Larson, M. J., & Russell, L. A. (2005).
Service use and costs for women with co-occurring mental and substance use disorders and a history
of violence. Psychiatric Services, 56, 1223–1232.
Donovan, B., Padin-Rivera, E., & Kowaliw, S. (2001). Transcend: Initial outcomes from a posttraumatic
stress disorder/substance abuse treatment program. Journal of Traumatic Stress, 14, 757–772.
Dorahy, M. J. & van der Hart, O. (2007). Relationship between trauma and dissociation: A historical
analysis. In Traumatic dissociation: Neurobiology and treatment (pp. 3–30). Arlington, VA:
American Psychiatric Publishing, Inc.
Dore, G., Mills, K., Murray, R., Teesson, M., & Farrugia, P. (2011). Post-traumatic stress disorder,
depression and suicidality in inpatients with substance use disorders. Drug and Alcohol Review,
31(3), 294–302.
Dorrepaal, E., Thomaes, K., Smit, J. H., van Balkom, A. J., Van, D. R., Veltman, D. J. et al. (2010).
Stabilizing group treatment for Complex Posttraumatic Stress Disorder related to childhood abuse
based on psycho-education and cognitive behavioral therapy: A pilot study. Child Abuse and Neglect,
34, 284–288.
Douglas, A. N., Jimenez, S., Lin, H. J., & Frisman, L. K. (2008). Ethnic differences in the effects of
spiritual well-being on long-term psychological and behavioral outcomes within a sample of
homeless women. Cultural Diversity & Ethnic Minority Psychology, 14, 344–352.
Driessen, M., Schulte, S., Luedecke, C., Schaefer, I., Sutmann, F., Ohlmeier, M. et al. (2008). Trauma and
PTSD in patients with alcohol, drug, or dual dependence: A multi-center study. Alcoholism: Clinical
& Experimental Research, 32, 481–488.
Drogendijk, A. N., Dirkzwager, A. J., Grievink, L., van der Velden, P. G., Marcelissen, F. G., & Kleber, R.
J. (2007). The correspondence between persistent self-reported post-traumatic problems and general
practitioners’ reports after a major disaster. Psychological Medicine, 37, 193–202.
Drogendijk, A. N., van der Velden, P. G., & Kleber, R. J. (2012). Acculturation and post-disaster mental
health problems among affected and non-affected immigrants: A comparative study. Journal of
Affective Disorders, 138, 485–489.
Drozdek, B. & Wilson, J. P. (2007). Wrestling with the ghosts from the past in exile: Assessing trauma in
asylum seekers. In J. P. Wilson & C. S. Tang (Eds.), Cross-cultural assessment of psychological
trauma and PTSD (pp. 113–131). New York: Springer Publishing, Science + Business Media.
Trauma-Informed Care in Behavioral Health Services 3-31
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001).
Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span:
Findings from the adverse childhood experiences study. JAMA: The Journal of the American Medical
Association, 286, 3089–3096.
Dube, S. R., Anda, R. F., Felitti, V. J., Edwards, V. J., & Croft, J. B. (2002). Adverse childhood
experiences and personal alcohol abuse as an adult. Addictive Behaviors, 27, 713–725.
Dube, S. R., Anda, R. F., Whitfield, C. L., Brown, D. W., Felitti, V. J., Dong, M. et al. (2005). Long-term
consequences of childhood sexual abuse by gender of victim. American Journal of Preventive
Medicine, 28, 430–438.
Ducharme, L. J., Knudsen, H. K., & Roman, P. M. (2008). Emotional exhaustion and turnover intention in
human service occupations: The protective role of coworker support. Sociological Spectrum, 28, 81–
104.
Duckworth, M. P. & Follette, V. M. (2011). Retraumatization: Assessment, treatment, and prevention.
New York: Brunner-Routledge.
Duffy, M., Gillespie, K., & Clark, D. M. (2007). Post-traumatic stress disorder in the context of terrorism
and other civil conflict in Northern Ireland: Randomised controlled trial. BMJ: British Medical
Journal, 334, 1147.
Dulin, P. L. & Passmore, T. (2010). Avoidance of potentially traumatic stimuli mediates the relationship
between accumulated lifetime trauma and late-life depression and anxiety. Journal of Traumatic
Stress, 23, 296–299.
Dunlavy, A. C. (2010). The impact of acculturation, trauma, and post-migration stressors on the mental
health of African immigrants and refugees in Sweden. Pittsburgh, PA: University of Pittsburgh.
Dunn, E. C., Gilman, S. E., Willett, J. B., Slopen, N. B., & Molnar, B. E. (2012). The impact of exposure
to interpersonal violence on gender differences in adolescent-onset major depression: Results from
the National Comorbidity Survey Replication (NCS–R). Depression and Anxiety.
Dunn, N. J., Rehm, L. P., Schillaci, J., Souchek, J., Mehta, P., Ashton, C. M. et al. (2007). A randomized
trial of self-management and psychoeducational group therapies for comorbid chronic posttraumatic
stress disorder and depressive disorder. Journal of Traumatic Stress, 20, 221–237.
Duran, B., Duran, E., & Brave Heart, M. Y. H. (1998). Native Americans and trauma of history. In R.
Thornton (Ed.), Studying Native America: Problems and prospects (pp. 60–76). Madison, WI:
University of Wisconsin Press.
Duran, E., Duran, B., Brave Heart, M. Y. H., & Yellow Horse-Davis, S. (1998). Healing the American
Indian soul wound. In Y. Danieli (Ed.), International handbook of multigenerational legacies of
trauma (pp. 341–354). New York: Plenum Press.
Dutton, M. A. & Greene, R. (2010). Resilience and crime victimization. Journal of Traumatic Stress, 23,
215–222.
Dyer, K. F. W., Dorahy, M. J., Hamilton, G., Corry, M., Shannon, M., MacSherry, A. et al. (2009). Anger,
aggression, and self-harm in PTSD and complex PTSD. Journal of Clinical Psychology, 65, 1099–
1114.
3-32 Part 3, Section 3—General Bibliography
Edwards, V. J., Anda, R. F., Felitti, V. J., & Dube, S. R. (2004). Adverse childhood experiences and
health-related quality of life as an adult. In Health consequences of abuse in the family: A clinical
guide for evidence-based practice (pp. 81–94). Washington, DC: American Psychological
Association.
Ehlers, A. & Clark, D. (2003). Early psychological interventions for adult survivors of trauma: A review.
Biological Psychiatry, 53, 817–826.
Ehlers, A., Bisson, J., Clark, D. M., Creamer, M., Pilling, S., Richards, D. et al. (2010). Do all
psychological treatments really work the same in posttraumatic stress disorder? Clinical Psychology
Review, 30, 269–276.
Ehntholt, K. A. & Yule, W. (2006). Practitioner review: Assessment and treatment of refugee children and
adolescents who have experienced war-related trauma. Journal of Child Psychology and Psychiatry,
47, 1197–1210.
Eilenberg, J., Fullilove, M. T., Goldman, R. G., & Mellman, L. (1996). Quality and use of trauma histories
obtained from psychiatric outpatients through mandated inquiry. Psychiatric Services, 47, 165–169.
Eisenman, D. P., Meredith, L. S., Rhodes, H., Green, B. L., Kaltman, S., Cassells, A. et al. (2008). PTSD
in Latino patients: Illness beliefs, treatment preferences, and implications for care. Journal of General
Internal Medicine, 23, 1386–1392.
Elbogen, E. B., Fuller, S., Johnson, S. C., Brooks, S., Kinneer, P., Calhoun, P. S. et al. (2010). Improving
risk assessment of violence among military veterans: An evidence-based approach for clinical
decision–making. Clinical Psychology Review, 30, 595–607.
Elbogen, E. B., Wagner, H. R., Fuller, S. R., Calhoun, P. S., Kinneer, P. M., & Beckham, J. C. (2010).
Correlates of anger and hostility in Iraq and Afghanistan war veterans. American Journal of
Psychiatry, 167, 1051–1058.
El-Gabalawy, R. (2012). Association between traumatic experiences and physical health conditions in a
nationally representative sample. Silver Spring, MD: Anxiety and Depression Association of
America.
Elhai, J. D. & Palmieri, P. A. (2011). The factor structure of posttraumatic stress disorder: A literature
update, critique of methodology, and agenda for future research. Journal of Anxiety Disorders, 25,
849–854.
Elhai, J. D., de Francisco, C. L., Miguel, F. K., Palmieri, P. A., Primi, R., & Christopher, F. B. (2011).
Testing whether posttraumatic stress disorder and major depressive disorder are similar or unique
constructs. Journal of Anxiety Disorders, 25, 404–410.
Elhai, J. D., Kashdan, T. B., Snyder, J. J., North, T. C., Heaney, C. J., & Frueh, B. C. (2007). Symptom
severity and lifetime and prospective health service use among military veterans evaluated for PTSD.
Depression and Anxiety, 24, 178–184.
Elhai, J. D., North, T. C., & Frueh, B. C. (2005). Health service use predictors among trauma survivors: A
critical review. Psychological Services, 2, 3–19.
Elhai, J. D., Patrick, S. L., Anderson, S., Simons, J. S., & Frueh, B. C. (2006). Gender- and trauma-related
predictors of use of mental health treatment services among primary care patients. Psychiatric
Services, 57, 1505–1509.
Trauma-Informed Care in Behavioral Health Services 3-33
Elklit, A. & Petersen, T. (2008). Exposure to traumatic events among adolescents in four nations. Torture.,
18, 2–11.
Elliott, D. E., Bjelajac, P., Fallot, R. D., Markoff, L. S., & Reed, B. G. (2005). Trauma-informed or
trauma-denied: Principles and implementation of trauma-informed services for women. Journal of
Community Psychology, 33, 461–477.
Elliott, S., Latini, D. M., Walker, L. M., Wassersug, R., & Robinson, J. W. (2010). Androgen deprivation
therapy for prostate cancer: Recommendations to improve patient and partner quality of life. Journal
of Sexual Medicine, 7, 2996–3010.
Elwood, L. S., Mott, J., Lohr, J. M., & Galovski, T. E. (2011). Secondary trauma symptoms in clinicians:
A critical review of the construct, specificity, and implications for trauma-focused treatment. Clinical
Psychology Review, 31, 25–36.
EMDR Network (2012). A brief description of EMDR therapy. Hamden, CT: EMDR Network.
Emshoff, J., Blakely, C., Gray, D., Jakes, S., Brounstein, P., Coulter, J. et al. (2003). An ESID case study
at the federal level. American Journal of Community Psychology, 32, 345–357.
Engdahl, B., Dikel, T. N., Eberly, R., & Blank, A., Jr. (1997). Posttraumatic stress disorder in a
community group of former prisoners of war: A normative response to severe trauma. American
Journal of Psychiatry, 154, 1576–1581.
Erbes, C. R. (2011). Couple functioning and PTSD in returning OIF soldiers: Preliminary findings from
the Readiness and Resilience in National Guard Soldiers Project. In Risk and resilience in U.S.
military families (pp. 47–67). New York: Springer Publishing Science + Business Media.
Ethnocultural perspectives on disaster and trauma: Foundations, issues, and applications (2008). New
York: Springer Publishing Science + Business Media.
Evans, D. L., Foa, E. B., Gur, R. E., Herbert, H., O’Brien, C. P., Seligman, M. E. P. et al. (2005). Treating
and preventing adolescent mental health disorders: What we know and what we don’t know: A
research agenda for improving the mental health of our youth. New York: Oxford University Press.
Evans-Campbell, T. (2008). Historical trauma in American Indian/Native Alaska communities: A
multilevel framework for exploring impacts on individuals, families, and communities. Journal of
Interpersonal Violence, 23, 316–338.
Everall, R. D. & Paulson, B. L. (2004). Burnout and secondary traumatic stress: Impact on ethical
behaviour. Canadian Journal of Counselling, 38, 25–35.
Everly, G. S., Jr., Phillips, S. B., Kane, D., & Feldman, D. (2006). Introduction to and overview of group
psychological first Aid. Brief Treatment and Crisis Intervention, 6, 130–136.
Everly, G. S., Jr., Welzant, V., & Jacobson, J. M. (2008). Resistance and resilience: The final frontier in
traumatic stress management. International Journal of Emergency Mental Health, 10, 1522–4821.
Evren, C., Dalbudak, E., Cetin, R., Durkaya, M., & Evren, B. (2010). Relationship of alexithymia and
temperament and character dimensions with lifetime post-traumatic stress disorder in male alcohol-
dependent inpatients. Psychiatry and Clinical Neurosciences, 64, 111–119.
3-34 Part 3, Section 3—General Bibliography
Evren, C., Sar, V., Dalbudak, E., Cetin, R., Durkaya, M., Evren, B. et al. (2011). Lifetime PTSD and
quality of life among alcohol-dependent men: Impact of childhood emotional abuse and dissociation.
Psychiatry Research, 186, 85–90.
Fahy, A. (2007). The unbearable fatigue of compassion: Notes from a substance abuse counselor who
dreams of working at Starbucks. Clinical Social Work Journal, 35, 199–205.
Falck, R. S., Wang, J., Siegal, H. A., & Carlson, R. G. (2004). The prevalence of psychiatric disorder
among a community sample of crack cocaine users: An exploratory study with practical implications.
Journal of Nervous and Mental Disease, 192, 503–507.
Falender, C. A. & Shafranske, E. P. (2004). Clinical supervision: A competency-based approach. (1st ed.)
Washington, DC: American Psychological Association.
Fallot, R. D. & Harris, M. (2001). A trauma-informed approach to screening and assessment. In M. Harris
& R. D. Fallot (Eds.), Using trauma theory to design service systems (pp. 23–31). San Francisco:
Jossey-Bass.
Fallot, R. D. & Harris, M. (2009). Creating Cultures of Trauma-Informed Care (CCTIC): A self-
assessment and planning protocol. Washington, DC: Community Connections.
Fallot, R. D. & Harris, M. (2002). The Trauma Recovery and Empowerment Model (TREM): Conceptual
and practical issues in a group intervention for women. Community Mental Health Journal, 38, 475–
485.
Falsetti, S. A., Resick, P. A., & Davis, J. L. (2003). Changes in religious beliefs following trauma. Journal
of Traumatic Stress, 16, 391–398.
Falsetti, S. A., Resnick, H. S., & Davis, J. L. (2008). Multiple channel exposure therapy for women with
PTSD and comorbid panic attacks. Cognitive Behaviour Therapy, 37, 117–130.
Falsetti, S. A., Resnick, H. S., Resnick, P. A., & Kilpatrick, D. (1993). The Modified PTSD Symptom
Scale: A brief self-report measure of posttraumatic stress disorder. Behavior Therapist, 16, 161–162.
Farley, M., Golding, J. M., Young, G., Mulligan, M., & Minkoff, J. R. (2004). Trauma history and relapse
probability among patients seeking substance abuse treatment. Journal of Substance Abuse
Treatment, 27, 161–167.
Feder, A., Charney, D., & Collins, K. (2011). Neurobiology of resilience. In S. M. Southwick, B. T. Litz,
D. Charney, & M. J. Friedman (Eds.), Resilience and mental health: challenges across the lifespan
(pp. 1–29). New York: Cambridge University Press.
Feeny, N. C. & Foa, E. B. (2005). Posttraumatic Stress Disorder. In Improving outcomes and preventing
relapse in cognitive–behavioral therapy (pp. 174–203). New York: Guilford Press.
Feldner, M. T., Babson, K. A., & Zvolensky, M. J. (2007). Smoking, traumatic event exposure, and post-
traumatic stress: A critical review of the empirical literature. Clinical Psychology Review, 27, 14–45.
Feldner, M. T., Monson, C. M., & Friedman, M. J. (2007). A critical analysis of approaches to targeted
PTSD prevention: Current status and theoretically derived future directions. Behavior Modification,
31, 80–116.
Felitti, V. J. (2002). The relation between adverse childhood experiences and adult health: Turning gold
into lead. The Permanente Journal, 6, 44–47.
Trauma-Informed Care in Behavioral Health Services 3-35
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V. et al. (1998).
Relationship of childhood abuse and household dysfunction to many of the leading causes of death in
adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine,
14, 245–258.
Felmingham, K. L. & Bryant, R. A. (2012). Gender differences in the maintenance of response to
cognitive behavior therapy for posttraumatic stress disorder. Journal of Consulting and Clinical
Psychology, 80, 196–200.
Fergusson, D. M., Horwood, L. J., & Woodward, L. J. (2000). The stability of child abuse reports: A
longitudinal study of the reporting behaviour of young adults. Psychological Medicine, 30, 529–544.
Ferrier-Auerbach, A. G., Erbes, C. R., Polusny, M. A., Rath, M., & Sponheim, S. R. (2010). Predictors of
emotional distress reported by soldiers in the combat zone. Journal of Psychiatric Research, 44, 470–
476.
Fetzner, M. G., McMillan, K. A., Sareen, J., & Asmundson, G. J. (2011). What is the association between
traumatic life events and alcohol abuse/dependence in people with and without PTSD? Findings from
a nationally representative sample. Depression and Anxiety, 28, 632–638.
Field, C. A. & Caetano, R. (2004). Ethnic differences in intimate partner violence in the U.S. general
population: The role of alcohol use and socioeconomic status. Trauma Violence Abuse, 5, 303–
317.Figley, C. R. (1995). Compassion fatigue: Toward a new understanding of the costs of caring. In
B. H. Stamm (Ed.), Secondary traumatic stress: Self-care issues for clinicians, researchers, and
educators (pp. 3–28). Lutherville, MD: Sidran Press.
Figley, C. R. (2002a). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical
Psychology, 58, 1433–1441.
Figley, C. R. (2002b). Origins of traumatology and prospects for the future, part I. Journal of Trauma
Practice, 1, 17–32.
Figley, C. R. & Nash, W. P. (2007). Combat stress injury: Theory, research, and management. New York:
Routledge.
Finkelhor, D., Ormrod, R., Turner, H., & Hamby, S. L. (2005). The victimization of children and youth: A
comprehensive, national survey. Child Maltreatment, 10, 5–25.
Finkelhor, D., Turner, H., Ormrod, R., & Hamby, S. L. (2009). Violence, abuse, and crime exposure in a
national sample of children and youth. Pediatrics, 124, 1411–1423.
Finkelstein, N. & Markoff, L. S. (2004). The Women Embracing Life and Living (WELL) Project: Using
the relational model to develop integrated systems of care for women with alcohol/drug use and
mental health disorders with histories of violence. Alcoholism Treatment Quarterly, 22, 63–80.
Finkelstein, N., Rechberger, E., Russell, L. A., VanDeMark, N. R., Noether, C. D., O’Keefe, M. et al.
(2005). Building resilience in children of mothers who have co-occurring disorders and histories of
violence: Intervention model and implementation issues. The Journal of Behavioral Health Services
& Research, 32, 141–154.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (2011a). Structured clinical interview for
DSM-IV-TR Axis I disorders, research version, non-patient edition. (SCID–I/NP) revised. November.
New York: Biometrics Research, New York State Psychiatric Institute.
3-36 Part 3, Section 3—General Bibliography
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (2011b). Structured clinical interview for
DSM-IV-TR Axis I disorders, research version, patient edition. (SCID–I/P) revised. November. New
York: Biometrics Research, New York State Psychiatric Institute.
Fisher, J. & Ogden, P. (2009). Sensorimotor psychotherapy. In C. A. Courtois (Ed.), Treating complex
traumatic stress disorders: An evidence-based guide (pp. 312–328). New York: Guilford Press.
Fisher, M. H., Hodapp, R. M., & Dykens, E. M. (2008). Child abuse among children with disabilities:
What We know and what we need to know. In M. G. Laraine (Ed.), International review of research
in mental retardation (Volume 35 ed., pp. 251–289). Academic Press.
Flannery, R. B., Jr. (2001). The employee victim of violence: Recognizing the impact of untreated
psychological trauma. American Journal of Alzheimer’s Disease, 16, 230–233.
Fletcher, S., Creamer, M., & Forbes, D. (2010). Preventing post traumatic stress disorder: Are drugs the
answer? Australian and New Zealand Journal of Psychiatry, 44, 1064–1071.
Foa, E. B. & International Society For Traumatic Stress Studies (2009). Effective treatments for PTSD:
Practice guidelines from the International Society for Traumatic Stress Studies. (2nd ed.) New York:
Guilford Press.
Foa, E. B. & Rothbaum, B. O. (1998). Treating the trauma of rape: Cognitive–behavioral therapy for
PTSD. New York: Guilford Press.
Foa, E. B., Dancu, C. V., Hembree, E. A., Jaycox, L. H., Meadows, E. A., & Street, G. P. (1999). A
comparison of exposure therapy, stress inoculation training, and their combination for reducing
posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical
Psychology, 67, 194–200.
Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional
processing of traumatic experiences: Therapist guide. Oxford University Press: New York.
Foa, E. B., Hembree, E. A., Cahill, S. P., Rauch, S. A., Riggs, D. S., Feeny, N. C. et al. (2005).
Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive
restructuring: outcome at academic and community clinics. Journal of Consulting and Clinical
Psychology, 73, 953–964.
Foa, E. B., Keane, T. M., & Friedman, M. J. (2000). Effective treatments of PTSD: Practice guidelines
from the International Society for Traumatic Stress Studies. New York: Guilford Press.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (2009). Introduction. In E. B. Foa, T. M. Keane,
M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines from the
International Society for Traumatic Stress Studies (2nd ed.) (pp. 1–20). New York: Guilford Press.
Foa, E. B., Rothbaum, B. O., & Furr, J. M. (2003). Augmenting exposure therapy with other CBT
procedures. Psychiatric Annals, 33, 47–53.
Foa, E. B., Rothbaum, B. O., Riggs, D. S., & Murdock, T. B. (1991). Treatment of posttraumatic stress
disorder in rape victims: A comparison between cognitive–behavioral procedures and counseling.
Journal of Consulting & Clinical Psychology, 59, 715–723.
Foa, E. B., Stein, D. J., & McFarlane, A. C. (2006). Symptomatology and psychopathology of mental
health problems after disaster. Journal of Clinical Psychiatry, 67 Supplement 2, 15–25.
Trauma-Informed Care in Behavioral Health Services 3-37
Foa, E. B., Zoellner, L. A., & Feeny, N. C. (2006). An evaluation of three brief programs for facilitating
recovery after Assault. Journal of Traumatic Stress, 19, 29–43.
Focht-New, G., Barol, B., Clements, P. T., & Milliken, T. F. (2008). Persons with developmental disability
exposed to interpersonal violence and crime: Approaches for intervention. Perspectives in Psychiatric
Care, 44, 89–98.
Follette, V. M., Iverson, K. M., & Ford, J. D. (2009). Contextual behavior trauma therapy. In C. A.
Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 264–285).
New York: Guilford Press.
Fontana, A. & Rosenheck, R. (2004). Trauma, change in strength of religious faith, and mental health
service use among veterans treated for PTSD. Journal of Nervous and Mental Disease, 192, 579–584.
Fontana, A. & Rosenheck, R. (2006). Treatment of female veterans with posttraumatic stress disorder: The
role of comfort in a predominantly male environment. Psychiatric Quarterly, 77, 55–67.
Forbes, D., Creamer, M. C., Phelps, A. J., Couineau, A. L., Cooper, J. A., Bryant, R. A. et al. (2007).
Treating adults with acute stress disorder and post-traumatic stress disorder in general practice: A
clinical update. Medical Journal of Australia, 187, 120–123.
Forbes, D., Lockwood, E., Elhai, J. D., Creamer, M., O’Donnell, M., Bryant, R. et al. (2011). An
examination of the structure of posttraumatic stress disorder in relation to the anxiety and depressive
disorders. Journal of Affective Disorders, 132, 165–172.
Ford, J. D. (2005). Treatment implications of altered affect regulation and information processing
following child maltreatment. Psychiatric Annals, 35, 410–419.
Ford, J. D. (2009). Neurobiological and developmental research: Clinical implications. In Treating
complex traumatic stress disorders: An evidence-based guide (pp. 31–58). New York: Guilford Press.
Ford, J. D. & Courtois, C. A. (2009). Defining and understanding complex trauma and complex traumatic
stress disorders. In C. A. Courtois & J. D. Ford (Eds.), Treating complex traumatic stress disorders:
An evidence-based guide (pp. 13–30). New York: Guilford Press.
Ford, J. D. & Fournier, D. (2007). Psychological trauma and post-traumatic stress disorder among women
in community mental health aftercare following psychiatric intensive care. Journal of Psychiatric
Intensive Care, 3, 27–34.
Ford, J. D. & Russo, E. (2006). Trauma-focused, present-centered, emotional self-regulation approach to
integrated treatment for posttraumatic stress and addiction: Trauma Adapative Recovery Group
Education and Therapy (TARGET). American Journal of Psychotherapy, 60, 335–355.
Ford, J. D. & Saltzman, W. (2009). Family systems therapy. In C. A. Courtois & J. D. Ford (Eds.),
Treating complex traumatic stress disorders: An evidence-based guide (pp. 391–414). New York:
Guilford Press.
Ford, J. D., Fallot, R. D., & Harris, M. (2009). Group therapy. In C. A. Courtois & J. D. Ford (Eds.),
Treating complex traumatic stress disorders: An evidence-based guide (pp. 415–440). New York:
Guilford Press.
Ford, J. D., Hawke, J., Alessi, S., Ledgerwood, D., & Petry, N. (2007). Psychological trauma and PTSD
symptoms as predictors of substance dependence treatment outcomes. Behavior Research and
Therapy, 45, 2417–2431.
3-38 Part 3, Section 3—General Bibliography
Forde, D. R. (2005). Reflections on 20 years of research on violence and trauma. Journal of Interpersonal
Violence, 20, 26–30.
Fortuna, L. R., Porche, M. V., & Alegría, M. (2008). Political violence, psychosocial trauma, and the
context of mental health services use among immigrant Latinos in the United States. Ethnicity and
Health, 13, 435–463.
Fortuna, L. R., Porche, M. V., & Alegría, M. (2009). A qualitative study of clinicians’ use of the cultural
formulation model in assessing posttraumatic stress disorder. Transcult.Psychiatry, 46, 429–450.
Fosha, D., Paivio, S. C., Gleiser, K., & Ford, J. D. (2009). Experiential and emotion-focused therapy. In C.
A. Courtois (Ed.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 286–
311). New York: Guilford Press.
Foy, D. W., Ruzek, J. I., Glynn, S. M., Riney, S. J., & Gusman, F. D. (2002). Trauma focus group therapy
for combat-related PTSD: An update. Journal of Clinical Psychology, 58, 907–918.
Foy, D. W., Schnurr, P. P., Weiss, D. S., Wattenberg, M. S., Glynn, S. M., Marmar, C. R. et al. (2001).
Group psychotherapy for PTSD. In J. P. Wilson, M. J. Friedman, & J. D. Lindy (Eds.), Treating
psychological trauma and PTSD (pp. 183–202). New York: Guilford Press.
Frank, B., Dewart, T., Schmeidler, J., & Demirjian, A. (2006). The Impact of 9/11 on New York City’s
substance abuse treatment programs: A study of program administrators. Journal of Addictive
Diseases, 25, 5–14.
Frankl, V. E. (1992). Man’s Search For Meaning: An Introduction To Logotherapy. (4th ed.) Boston:
Beacon Press.
Frappell-Cooke, W., Gulina, M., Green, K., Hacker, H. J., & Greenberg, N. (2010). Does trauma risk
management reduce psychological distress in deployed troops? Occupational Medicine, 60, 645–650.
Frazier, P., Tennen, H., Gavian, M., Park, C., Tomich, P., & Tashiro, T. (2009). Does self-reported
posttraumatic growth reflect genuine positive change? Psychological Science, 20, 912–919.
Fredman, S. J., Monson, C. M., & Adair, K. C. (2011). Implementing cognitive–behavioral conjoint
therapy for PTSD with the newest generation of veterans and their partners. Cognitive and Behavioral
Practice, 18, 120–130.
Frencher, S. K., Jr., Benedicto, C. M., Kendig, T. D., Herman, D., Barlow, B., & Pressley, J. C. (2010). A
comparative analysis of serious injury and illness among homeless and housed low income residents
of New York City. Journal of Trauma, 69, S191–S199.
Friborg, O., Hjemdal, O., Rosenvinge, J. H., & Martinussen, M. (2003). A new rating scale for adult
resilience: What are the central protective resources behind healthy adjustment? International Journal
of Methods in Psychiatric Research, 12, 65–76.
Friedman, M. J. & Davidson, J. R. T. (2007). Pharmacotherapy for PTSD. In M. J. Friedman, T. M. Keane,
& P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 376–405). New York: Guilford
Press.
Friedman, M. J. (2006). Posttraumatic stress disorder among military returnees from Afghanistan and Iraq.
American Journal of Psychiatry, 163, 586–593.
Trauma-Informed Care in Behavioral Health Services 3-39
Friedman, M. J. (2009). PTSD and other posttraumatic syndromes. In D. McKay, J. S. Abramowitz, S.
Taylor, & G. J. G. Asmundson (Eds.), Current perspectives on the anxiety disorders: Implications for
DSM-V and beyond (pp. 377–409). New York: Springer Publishing Co.
Friedman, M. J. (2011). PTSD and related disorders. In D. J. Stein, M. J. Friedman, & C. Blanco (Eds.),
Post-traumatic stress disorder (pp. 1–34). Chichester, UK: John Wiley and Sons, Inc.
Friedman, M. J., Cohen, J. A., Foa, E. B., & Keane, T. M. (2009). Integration and summary. In Effective
treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies
(2nd ed.) (pp. 617–642). New York: Guilford Press.
Friedman, M. J., Keane, T. M., & Resick, P. A. (2007). Handbook of PTSD: Science and practice. New
York: Guilford Press.
Friedman, M. J., Marmar, C. R., Baker, D. G., Sikes, C. R., & Farfel, G. M. (2007). Randomized, double-
blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of
Veterans Affairs setting. Journal of Clinical Psychiatry, 68, 711–720.
Frisman, L., Ford, J., Lin, H. J., Mallon, S., & Chang, R. (2008). Outcomes of trauma treatment using the
TARGET model. Journal of Groups in Addiction and Recovery, 3, 285–303.
Fritch, A. M. & Lynch, S. M. (2008). Group treatment for adult survivors of interpersonal trauma. Journal
of Psychological Trauma, 7, 145–169.
Frueh, B. C., Cousins, V. C., Hiers, T. G., Cavenaugh, S. D., Cusack, K. J., & Santos, A. B. (2002). The
need for trauma assessment and related clinical services in a state-funded mental health system.
Community Mental Health Journal, 38, 351–356.
Frueh, B. C., Dalton, M. E., Johnson, M. R., Hiers, T. G., Gold, P. B., Magruder, K. M. et al. (2000).
Trauma within the psychiatric setting: Conceptual framework, research directions, and policy
implications. Administration and Policy in Mental Health, 28, 147–154.
Frueh, B. C., Grubaugh, A. L., Cusack, K. J., & Elhai, J. D. (2009). Disseminating evidence-based
practices for adults with PTSD and severe mental illness in public-sector mental health agencies.
Behavior Modification, 33, 66–81.
Frueh, B. C., Knapp, R. G., Cusack, K. J., Grubaugh, A. L., Sauvageot, J. A., Cousins, V. C. et al. (2005).
Patients’ reports of traumatic or harmful experiences within the psychiatric setting. Psychiatric
Services, 56, 1123–1133.
Fullerton, C. S., Ursano, R. J., & Wang, L. (2004). Acute stress disorder, posttraumatic stress disorder, and
depression in disaster or rescue workers. American Journal of Psychiatry, 161, 1370–1376.
Furnham, A., Petrides, K. V., Sisterson, G., & Baluch, B. (2003). Repressive coping style and positive
self-presentation. British Journal of Health Psychology, 8, 223–249.
Gaillot, S. J. (2011). Disparities in trauma and mental health service use. Ann Arbor, MI: ProQuest
Information & Learning.
Galea, S., Ahern, J., Resnick, Kilpatrick, D., Bucuvalas, M., Gold, J. et al. (2002). Psychological sequelae
of the September 11 terrorist attacks in New York City. New England Journal of Medicine, 346, 982–
987.
3-40 Part 3, Section 3—General Bibliography
Galea, S., Ahern, J., Tracy, M., Hubbard, A., Cerda, M., Goldmann, E. et al. (2008). Longitudinal
determinants of posttraumatic stress in a population-based cohort study. Epidemiology, 19, 47–54.
Galovski, T. & Lyons, J. A. (2004). Psychological sequelae of combat violence: A review of the impact of
PTSD on the veteran’s family and possible interventions. Aggression and Violent Behavior, 9, 477–
501.
Gapen, M., Cross, D., Ortigo, K., Graham, A., Johnson, E., Evces, M. et al. (2011). Perceived
neighborhood disorder, community cohesion, and PTSD symptoms among low-income African
Americans in an urban health setting. American Journal of Orthopsychiatry, 81, 31–37.
Gardner, B., Rose, J., Mason, O., Tyler, P., & Cushway, D. (2005). Cognitive therapy and behavioural
coping in the management of work-related stress: An intervention study. Work & Stress, 19, 137–152.
Garfinkel, S. N. & Liverzon, I. (2009). Neurobiology of PTSD: A review of neuroimaging. Psychiatric
Annals, 39, 370–381.
Garner, B. R., Knight, K., & Simpson, D. D. (2007). Burnout among corrections-based drug treatment
staff: impact of individual and organizational factors. International Journal of Offender Therapy and
Comparative Criminology, 51, 510–522.
Garno, J. L., Goldberg, J. F., Ramirez, P. M., & Ritzler, B. A. (2005). Impact of childhood abuse on the
clinical course of bipolar disorder. British Journal of Psychiatry, 186, 121–125.
Gelkopf, M., Solomon, Z., Berger, R., & Bleich, A. (2008). The mental health impact of terrorism in
Israel: A repeat cross-sectional study of Arabs and Jews. Acta Psychiatrica Scandinavica, 117, 369–
380.
Geller, J. A., Madsen, L. H., & Ohrenstein, L. (2004). Secondary trauma: A team approach. Clinical Social
Work Journal, 32, 415–430.
Geller, J. L., Nicholson, J., & Traverso, A. (1997). The victimization of women with mental illness by
treaters: A historical perspective. In Sexual abuse in the lives of women diagnosed with serious
mental illness (pp. 139–160). Amsterdam: Harwood Academic Publishers.
Geller, R., Krasner, M., & Korones, D. (2010). Clinician self-care: The applications of mindfulness-based
approaches in preventing professional burnout and compassion fatigue. The Journal of Pain &
Symptom Management, 39, 336.
Gellis, L. A., Mavandadi, S., & Oslin, D. W. (2010). Functional quality of life in full versus partial
posttraumatic stress disorder among veterans returning from Iraq and Afghanistan. Primary Care
Companion Journal of Clinical Psychiatry, 12.
Gentilello, L. M., Ebel, B. E., Wickizer, T. M., Salkever, D. S., & Rivara, F. P. (2005). Alcohol
interventions for trauma patients treated in emergency departments and hospitals: A cost benefit
analysis. Annals of Surgery, 241, 541–550.
Gentilello, L. M., Villaveces, A., Ries, R. R., Nason, K. S., Daranciang, E., Donovan, D. M. et al. (1999).
Detection of acute alcohol intoxication and chronic alcohol dependence by trauma center staff.
Journal of Trauma, 47, 1131–1135.
Gentry, J. E., Baranowsky, A. B., & Dunning, K. (2002). The Accelerated Recovery Program (ARP) for
compassion fatigue. In Treating compassion fatigue (pp. 123–137). New York: Brunner-Routledge.
Trauma-Informed Care in Behavioral Health Services 3-41
Geraerts, E., Lindsay, D. S., Merckelbach, H., Jelicic, M., Raymaekers, L., Arnold, M. M. et al. (2009).
Cognitive mechanisms underlying recovered-memory experiences of childhood sexual abuse.
Psychological Science, 20, 92–98.
Geraerts, E., Schooler, J. W., Merckelbach, H., Jelicic, M., Hauer, B. J., & Ambadar, Z. (2007). The reality
of recovered memories: Corroborating continuous and discontinuous memories of childhood sexual
abuse. Psychological Science, 18, 564–568.
Gerardi, M., Cukor, J., Difede, J., Rizzo, A., & Rothbaum, B. O. (2010). Virtual reality exposure therapy
for post-traumatic stress disorder and other anxiety disorders. Current Psychiatry Reports, 12, 298–
305.
Gerra, G., Somaini, L., Zaimovic, A., Gerra, M. L., Maremmani, I., Amore, M. et al. (2010).
Developmental traumatic experiences, PTSD and substance abuse vulnerability: The neurobiological
link. In L. Sher & A. Vilens (Eds.), Neurobiology of post-traumatic stress disorder (pp. 175–200).
Nova Science Publishers, Inc.
Gewirtz, A. H., Polusny, M. A., DeGarmo, D. S., Khaylis, A., & Erbes, C. R. (2010). Posttraumatic stress
symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors
and couple adjustment. Journal of Consulting and Clinical Psychology, 78, 599–610.
Gewirtz, A., Forgatch, M., & Wieling, E. (2008). Parenting practices as potential mechanisms for child
adjustment following mass trauma. Journal of Marital and Family Therapy, 34, 177–192.
Ghafoori, B. & Hierholzer, R. W. (2010). Personality patterns among Black, White, and Hispanic combat
veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 2, 12–18.
Ghafoori, B., Hierholzer, R., Howsepian, B., & Boardman, A. (2008). The role of adult attachment,
parental bonding, and spiritual love in the adjustment to military trauma. Journal of Trauma &
Dissociation, 9, 85–106.
Gilbert, R., Widom, C. S., Browne, K., Fergusson, D., Webb, E., & Janson, S. (2009). Burden and
consequences of child maltreatment in high-income countries. Lancet, 373, 68–81.
Gill, D. A. & Picou, J. S. (1997). The day the water died: Cultural impacts of the Exxon Valdez oil spill. In
The Exxon Valdez disaster: Readings on a modern social problem (pp. 167–187).
Gill, J., Vythilingam, M., & Page, G. G. (2008). Low cortisol, high DHEA, and high levels of stimulated
TNF-alpha and IL–6 in women with PTSD. Journal of Traumatic Stress, 21, 530–539.
Gillespie, C. F., Bradley, B., Mercer, K., Smith, A. K., Conneely, K., Gapen, M. et al. (2011). Trauma
exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry,
31, 505–514.
Gillespie, C. F., Phifer, J., Bradley, B., & Ressler, K. J. (2009). Risk and resilience: Genetic and
environmental influences on development of the stress response. Depression and Anxiety, 26, 984–
992.
Ginzburg, K., Solomon, Z., & Bleich, A. (2002). Repressive coping style, acute stress disorder, and
posttraumatic stress disorder after myocardial infarction. Psychosomatic Medicine, 64, 748–757.
Glantz, M. D., Anthony, J. C., Berglund, P. A., Degenhardt, L., Dierker, L., Kalaydjian, A. et al. (2009).
Mental disorders as risk factors for later substance dependence: estimates of optimal prevention and
treatment benefits. Psychological Medicine, 39, 1365–1377.
3-42 Part 3, Section 3—General Bibliography
Goggins, K. (2011). Focus: Expanding the circle of care: What does trauma-informed care mean for
family-centered care? Cross Currents: The Journal of Addictions and Mental Health Vol.12 No.3.
Gold, S. D., Marx, B. P., Soler-Baillo, J. M., & Sloan, D. M. (2005). Is life stress more traumatic than
traumatic stress? Journal of Anxiety Disorders., 19, 687–698.
Gold, S. N. & Elhai, J. D. (2007). Trauma and serious mental illness. Binghamton, NY: Haworth
Maltreatment & Trauma Press.
Gold, S. N. (2008). Benefits of a contextual approach to understanding and treating complex trauma.
Journal of Trauma Dissociation, 9, 269–292.
Gold, S. N. (2009). Contextual therapy. In C. A. Courtois & J. D. Ford (Eds.), Treating complex traumatic
stress disorders: An evidence-based guide (pp. 227–242). New York: Guilford Press.
Goldberg, J. F. & Garno, J. L. (2005). Development of posttraumatic stress disorder in adult bipolar
patients with histories of severe childhood abuse. Journal of Psychiatric Research, 39, 595–601.
Goldmann, E., Aiello, A., Uddin, M., Delva, J., Koenen, K., Gant, L. M. et al. (2011). Pervasive exposure
to violence and posttraumatic stress disorder in a predominantly African American urban community:
The Detroit neighborhood health study. Journal of Traumatic Stress, 24, 747–751.
Goldstein, R. B., Compton, W. M., & Grant, B. F. (2010). Antisocial behavioral syndromes and additional
psychiatric comorbidity in posttraumatic stress disorder among U.S. adults: Results from Wave 2 of
the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of the American
Psychiatric Nurses Association, 16, 145–165.
Gone, J. P. (2009). A community-based treatment for Native American historical trauma: Prospects for
evidence-based practice. Journal of Consulting and Clinical Psychology, 77, 751–762.
Gonzalez, P. & Gonzalez, G. M. (2008). Acculturation, optimism, and relatively fewer depression
symptoms among Mexican immigrants and Mexican Americans. Psychological Reports, 103, 566–
576.
Goodell, J. (2003). Who’s a hero now? Retrieved July 4, 2013, from:
http://www.nytimes.com/2003/07/27/magazine/who-s-a-hero-now.html?pagewanted=all&src=pm
Goodkind, J. R., Lanoue, M. D., & Milford, J. (2010). Adaptation and implementation of cognitive
behavioral intervention for trauma in schools with American Indian youth. J Clin.Child Adolesc
Psychol., 39, 858–872.
Goodman, G. S., Ghetti, S., Quas, J. A., Edelstein, R. S., Alexander, K. W., Redlich, A. D. et al. (2003). A
prospective study of memory for child sexual abuse: New findings relevant to the repressed-memory
controversy. Psychological Science, 14, 113–118.
Goodson, J., Helstrom, A., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Powers, M. B. (2011). The
treatment of posttraumatic stress disorder in U.S. combat veterans: A meta-analytic review.
Psychological Reports, 109, 573–599.
Goto, T. & Wilson, J. P. (2003). A review of the history of traumatic stress studies in Japan: From
traumatic neurosis to PTSD. Trauma Violence Abuse, 4, 195–209.
Govindshenoy, M. & Spencer, N. (2007). Abuse of the disabled child: A systematic review of population-
based studies. Child: Care, Health and Development, 33, 552–558.
Trauma-Informed Care in Behavioral Health Services 3-43
Grammer, G. G. & Moran, S. C. (2011). Geriatrics. In D. M. Benedek (Ed.), Clinical manual for
management of PTSD (pp. 371–381). Arlington, VA: American Psychiatric Publishing, Inc.
Grant, B. F., Chou, S. P., Goldstein, R. B., Huang, B., Stinson, F. S., Saha, T. D. et al. (2008). Prevalence,
correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the
Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical
Psychiatry., 69, 533–545.
Grant, B. F., Stinson, F. S., Dawson, D. A., Chou, S. P., Dufour, M. C., Compton, W. et al. (2004).
Prevalence and co-occurrence of substance use disorders and independent mood and anxiety
disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions.
Archives of General Psychiatry, 61, 807–816.
Grant, B. F., Stinson, F. S., Hasin, D. S., Dawson, D. A., Chou, S. P., & Anderson, K. (2004). Immigration
and lifetime prevalence of DSM-IV Psychiatric disorders among Mexican Americans and non-
Hispanic Whites in the United States: Results from the National Epidemiologic Survey on Alcohol
and Related Conditions. Archives of General Psychiatry, 61, 1226–1233.
Gratz, K. L. & Tull, M. T. (2010). The relationship between emotion dysregulation and deliberate self-
harm among inpatients with substance use disorders. Cognitive Therapy and Research, 34, 544–553.
Gray, M. J., Elhai, J. D., & Frueh, B. C. (2004). Enhancing patient satisfaction and increasing treatment
compliance: patient education as a fundamental component of PTSD treatment. Psychiatric
Quarterly, 75, 321–332.
Gray, M. J., Elhai, J. D., & Schmidt, L. O. (2007). Trauma professionals’ attitudes toward and utilization
of evidence-based practices. Behavior Modification, 31, 732–748.
Green, B. L. (1996). Trauma History Questionnaire. In B. H. Stamm (Ed.), Measurement of stress, trauma,
and adaptation (pp. 366–369). Lutherville, MD: Sidran Press.
Green, B. L., Chung, J. Y., Daroowalla, A., Kaltman, S., & Debenedictis, C. (2006). Evaluating the
cultural validity of the stressful life events screening questionnaire. Violence Against Women, 12,
1191–1213.
Green, B. L., Krupnick, J. L., Chung, J., Siddique, J., Krause, E. D., Revicki, D. et al. (2006). Impact of
PTSD comorbidity on one-year outcomes in a depression trial. Journal of Clinical Psychology, 62,
815–835.
Green, D., Rasmussen, A., & Rosenfeld, B. (2010). Defining torture: A review of 40 years of health
science research. Journal of Traumatic Stress, 23, 528–531.
Green, J. G., McLaughlin, K. A., Berglund, P. A., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M. et al.
(2010). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey
Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67,
113–123.
Green, K. T., Calhoun, P. S., Dennis, M. F., & Beckham, J. C. (2010). Exploration of the resilience
construct in posttraumatic stress disorder severity and functional correlates in military combat
veterans who have served since September 11, 2001. Journal of Clinical Psychiatry, 71, 823–830.
3-44 Part 3, Section 3—General Bibliography
Greenberg, G. A. & Rosenheck, R. A. (2010). Correlates of past homelessness in the National
Epidemiological Survey on Alcohol and Related Conditions. Administration and Policy in Mental
Health, 37, 357–366.
Greenberg, G. A. & Rosenheck, R. A. (2010). Mental health correlates of past homelessness in the
National Comorbidity Study Replication. Journal of Health Care for the Poor and Underserved, 21,
1234–1249.
Greene, L. R., Meisler, A. W., Pilkey, D., Alexander, G., Cardella, L. A., Sirois, B. C. et al. (2004).
Psychological work with groups in the Veterans Administration. In J. L. DeLucia–Waack, D. A.
Gerrity, C. R. Kalodner, & M. T. Riva (Eds.), Handbook of group counseling and psychotherapy (pp.
322–337). Thousand Oaks, CA: Sage Publications Ltd.
Grieger, T. A., Cozza, S. J., Ursano, R. J., Hoge, C., Martinez, P. E., Engel, C. C. et al. (2006).
Posttraumatic stress disorder and depression in battle-injured soldiers. American Journal of
Psychiatry, 163, 1777–1783.
Grievink, L., van der Velden, P. G., Stellato, R. K., Dusseldorp, A., Gersons, B. P., Kleber, R. J. et al.
(2007). A longitudinal comparative study of the physical and mental health problems of affected
residents of the firework disaster in Enschede, The Netherlands. Public Health, 121, 367–374.
Gros, D. F., Frueh, B. C., & Magruder, K. M. (2011). Prevalence and features of panic disorder and
comparison to posttraumatic stress disorder in VA primary care. General Hospital Psychiatry, 33,
482–488.
Grossman, D. (1995). On killing: The psychological cost of learning to kill in war and society. (1st ed.)
Boston: Little Brown.
Grubaugh, A. L., Elhai, J. D., Cusack, K. J., Wells, C., & Frueh, B. C. (2007). Screening for PTSD in
public-sector mental health settings: The diagnostic utility of the PTSD Checklist. Depression and
Anxiety, 24, 124–129.
Grubaugh, A. L., Magruder, K. M., Waldrop, A. E., Elhai, J. D., Knapp, R. G., & Frueh, B. C. (2005).
Subthreshold PTSD in primary care: Prevalence, psychiatric disorders, healthcare use, and functional
status. Journal of Nervous & Mental Disease, 193, 658–664.
Guarino, K., Soares, P., Konnath, K., Clervil, R., & Bassuk, E. (2009). Trauma-informed organizational
toolkit. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health
Services Administration and The Daniels Fund, the National Child Traumatic Stress Network and the
W.K. Kellogg Foundation.
Guay, S., Billette, V., & Marchand, A. (2006). Exploring the links between posttraumatic stress disorder
and social support: Processes and potential research avenues. Journal of Traumatic Stress, 19, 327–
338.
Gureje, O. (2008). Comorbidity of pain and anxiety disorders. Current Psychiatry Reports, 10, 318–322.
Gutheil, T. G. & Brodsky, A. (2008). Preventing boundary violations in clinical practice. New York:
Guilford Press.
Gutner, C. A., Pineles, S. L., Griffin, M. G., Bauer, M. R., Weierich, M. R., & Resick, P. A. (2010).
Physiological predictors of posttraumatic stress disorder. Journal of Traumatic Stress, 23, 775–784.
Trauma-Informed Care in Behavioral Health Services 3-45
Gwadz, M. V., Nish, D., Leonard, N. R., & Strauss, S. M. (2007). Gender differences in traumatic events
and rates of post-traumatic stress disorder among homeless youth. Journal of Adolescence, 30, 117–
129.
Haagsma, J. A., Polinder, S., Olff, M., Toet, H., Bonsel, G. J., & van Beeck, E. F. (2012). Posttraumatic
stress symptoms and health-related quality of life: A two year follow-up study of injury treated at the
Emergency Department. BMC.Psychiatry, 12, 1.
Haagsma, J. A., Polinder, S., Toet, H., Panneman, M., Havelaar, A. H., Bonsel, G. J. et al. (2011). Beyond
the neglect of psychological consequences: post-traumatic stress disorder increases the non-fatal
burden of injury by more than 50%. Injury Prevention, 17, 21–26.
Haasen, C., Demiralay, C., & Reimer, J. (2008). Acculturation and mental distress among Russian and
Iranian migrants in Germany. European Psychiatry, 23 Supplementement 1, 10–13.
Habukawa, M., Maeda, M., & Uchimura, N. (2010). Sleep disturbances in posttraumatic stress disorder. In
L. Sher & A. Vilens (Eds.), Neurobiology of post-traumatic stress disorder (pp. 119–135). Nova
Science Publishers, Inc.
Hagenaars, M. A., van, M. A., & Hoogduin, K. A. (2009). Reliving and disorganization in posttraumatic
stress disorder and panic disorder memories. Journal of Nervous and Mental Disease, 197, 627–630.
Halcon, L. L., Robertson, C. L., Savik, K., Johnson, D. R., Spring, M. A., Butcher, J. N. et al. (2004).
Trauma and coping in Somali and Oromo refugee youth. Journal of Adolescent Health, 35, 17–25.
Hall, C. W. & Webster, R. E. (2002). Traumatic symptomatology characteristics of adult children of
alcoholics. Journal of Drug Education, 32, 195–211.
Halliday, G. (1987). Direct psychological therapies for nightmares: A review. Clinical Psychology Review,
7, 501–523.
Hamblen, J. (2001). PTSD in Children and Adolescents. White River Junction, VT: National Center for
Post-Traumatic Stress Disorder.
Hamblen, J. L., Gibson, L. E., Mueser, K. T., & Norris, F. H. (2006). Cognitive behavioral therapy for
prolonged postdisaster distress. Journal of Clinical Psychology, 62, 1043–1052.
Hamblen, J. L., Norris, F. H., Pietruszkiewicz, S., Gibson, L. E., Naturale, A., & Louis, C. (2009).
Cognitive behavioral therapy for postdisaster distress: A community based treatment program for
survivors of Hurricane Katrina. Administration and Policy in Mental Health, 36, 206–214.
Hammersley, P., Dias, A., Todd, G., Bowen-Jones, K., Reilly, B., & Bentall, R. P. (2003). Childhood
trauma and hallucinations in bipolar affective disorder: preliminary investigation. British Journal of
Psychiatry, 182, 543–547.
Hankin, C. S., Skinner, K. M., Sullivan, L. M., Miller, D. R., Frayne, S., & Tripp, T. J. (1999). Prevalence
of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing
sexual assault while in the military. Journal of Traumatic Stress, 12, 601–612.
Hanson, R. F. & Self-Brown, S. (2010). Screening and assessment of crime victimization and its effects.
Journal of Traumatic Stress, 23, 207–214.
Harder, L. H., Chen, S., Baker, D. G., Chow, B., McFall, M., Saxon, A. et al. (2011). The influence of
posttraumatic stress disorder numbing and hyperarousal symptom clusters in the prediction of
3-46 Part 3, Section 3—General Bibliography
physical health status in veterans with chronic tobacco dependence and posttraumatic stress disorder.
Journal of Nervous & Mental Disease, 199, 940–945.
Hardt, J. & Rutter, M. (2004). Validity of adult retrospective reports of adverse childhood experiences:
review of the evidence. Journal of Child Psychology and Psychiatry, 45, 260–273.
Harned, M. S., Korslund, K. E., Foa, E. B., & Linehan, M. M. (2012). Treating PTSD in suicidal and self-
injuring women with borderline personality disorder: Development and preliminary evaluation of a
Dialectical Behavior Therapy Prolonged Exposure Protocol. Behaviour Research and Therapy, 50,
381–386.
Harned, M. S., Najavits, L. M., & Weiss, R. D. (2006). Self-harm and suicidal behavior in women with
comorbid PTSD and substance dependence. American Journal of Addiction, 15, 392–395.
Harney, P. A. (2007). Resilience processes in context: Contributions and implications of Bronfenbrenner’s
person–process–context model. Journal of Aggression, Maltreatment & Trauma, 14, 73–87.
Harpaz-Rotem, I. & Rosenheck, R. A. (2011). Serving those who served: Retention of newly returning
veterans from Iraq and Afghanistan in mental health treatment. Psychiatric Services, 62, 22–27.
Harper, K., Richter, N. L., & Gorey, K. M. (2009). Group work with female survivors of childhood sexual
abuse: Evidence of poorer outcomes among those with eating disorders. Eating Behaviors, 10, 45–48.
Harris, J. I., Erbes, C. R., Engdahl, B. E., Thuras, P., Murray-Swank, N., Grace, D. et al. (2011). The
effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma.
Journal of Clinical Psychology, 67, 425–438.
Harris, M. & Fallot, R. D. (2001). Designing trauma-informed addictions services. In M. Harris & R. D.
Fallot (Eds.), Using trauma theory to design service systems (pp. 57–73). San Francisco: Jossey-Bass.
Harris, M. & Fallot, R. D. (2001). Envisioning a trauma-informed service system: A vital paradigm shift.
In M. Harris & R. D. Fallot (Eds.), Using trauma theory to design service systems (pp. 3–22). San
Francisco: Jossey-Bass.
Harris, M. & Fallot, R. D. (2001). Trauma-informed inpatient services. In M. Harris & R. D. Fallot (Eds.),
Using trauma theory to design service systems (pp. 33–46). San Francisco: Jossey-Bass.
Harris, M. & Fallot, R. D. (2001). Using trauma theory to design service systems: New directions for
mental health services, No.89. San Francisco: Jossey-Bass.
Harris, M. & The Community Connections Trauma Work Group (1998). Trauma recovery and
empowerment: A clinician’s guide for working with women in groups. New York: Simon & Schuster.
Harris, M., Fallot, R. D., & Berley, R. W. (2005). Qualitative interviews on substance abuse relapse and
prevention among female trauma survivors. Psychiatric Services, 56, 1292–1296.
Harris, T. B., Carlisle, L. L., Sargent, J., & Primm, A. B. (2010). Trauma and diverse child populations.
Child and Adolescent Psychiatric Clinics of North America, 19, 869–887.
Harrison, R. L. & Westwood, M. J. (2009). Preventing vicarious traumatization of mental health therapists:
Identifying protective practices. Psychotherapy: Theory, Research, Practice, Training, 46, 203–219.
Harvard School of Medicine (2007a). NCS–R Lifetime Prevalence estimates: Table 1. Lifetime prevalence
of DSM-IV/WMH–CIDI disorders by sex and cohort 1 (n=9282). Cambridge, MA: Harvard
University.
Trauma-Informed Care in Behavioral Health Services 3-47
Harvard School of Medicine (2007b). NCS–R Twelve-month Prevalence estimates: Table 2. 12-month
prevalence of DSM-IV/WMH–CIDI disorders by sex and cohort 1 (n=9282). Cambridge, MA:
Harvard University.
Harvey, M. R. & Tummala-Narra, P. (2007). Sources and expression of resilience in trauma survivors:
Ecological theory, multicultural perspectives. Journal of Aggression, Maltreatment & Trauma, 14, 1–
7.
Harvey, M. R. (1996). An ecological view of psychological trauma and trauma recovery. Journal of
Traumatic Stress, 9, 3–23.
Harvey, M. R. (2007). Towards an ecological understanding of resilience in trauma survivors: Implications
for theory, research, and practice. Journal of Aggression, Maltreatment and Trauma, 14, 9–32.
Harville, E. W., Xiong, X., Smith, B. W., Pridjian, G., Elkind-Hirsch, K., & Buekens, P. (2011).
Combined effects of Hurricane Katrina and Hurricane Gustav on the mental health of mothers of
small children. Journal of Psychiatric and Mental Health Nursing, 18, 288–296.
Haskell, S. G., Mattocks, K., Goulet, J. L., Krebs, E. E., Skanderson, M., Leslie, D. et al. (2011). The
burden of illness in the first year home: Do male and female VA users differ in health conditions and
healthcare utilization. Womens Health Issues, 21, 92–97.
Haugen, P. T., Evces, M., & Weiss, D. S. Treating posttraumatic stress disorder in first responders: A
systematic review. Clinical Psychology Review, (in press).
Hawkins, E. J., Malte, C. A., Imel, Z. E., Saxon, A. J., & Kivlahan, D. R. (2012). Prevalence and trends of
benzodiazepine use among Veterans Affairs patients with posttraumatic stress disorder, 2003–2010.
Drug and Alcohol Dependence.
Hawkins, F. & Klas, L. (1997). Time management as a stressor for helping professionals: Implications for
employment. Journal of Employment Counseling, 34, 2–6.
Hayes, S. C. (2004). Acceptance and commitment therapy and the new behavior therapies: Mindfulness,
acceptance, and relationship. In S. C. Hayes, V. M. Follette, & M. M. Linehan (Eds.), Mindfulness
and acceptance: Expanding the cognitive–behavioral tradition (pp. 1–29). New York: Guilford Press.
Hebert, M. & Bergeron, M. (2007). Efficacy of a group intervention for adult women survivors of sexual
abuse. Journal of Child Sexual Abuse, 16, 37–61.
Hegadoren, K. M., Lasiuk, G. C., & Coupland, N. J. (2006). Posttraumatic stress disorder Part III: Health
effects of interpersonal violence among women. Perspectives in Psychiatric Care, 42, 163–173.
Heim, C., Mletzko, T., Purselle, D., Musselman, D. L., & Nemeroff, C. B. (2008). The
dexamethasone/corticotropin–releasing factor test in men with major depression: Role of childhood
trauma. Biological Psychiatry, 63, 398–405.
Heim, C., Newport, D. J., Mletzko, T., Miller, A. H., & Nemeroff, C. B. (2008). The link between
childhood trauma and depression: Insights from HPA axis studies in humans.
Psychoneuroendocrinology, 33, 693–710.
Helms, J. E., Nicolas, G., & Green, C. E. (2010). Racism and ethnoviolence as trauma: Enhancing
professional training. Traumatology, 16, 53–62.
3-48 Part 3, Section 3—General Bibliography
Helzer, J., Robins, L., & McEvoy, L. (1987). Post-traumatic stress disorder in the general population:
Findings of the Epidemiologic Catchment Area survey. New England Journal of Medicine, 317,
1630–1634.
Hembree, E. A. & Foa, E. B. (2000). Posttraumatic stress disorder: Psychological factors and psychosocial
interventions. Journal of Clinical Psychiatry, 61, 33–39.
Hembree, E. A., Foa, E. B., Dorfan, N. M., Street, G. P., Kowalski, J., & Tu, X. (2003). Do patients drop
out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress, 16, 555–562.
Herbert, J. D. & Forman, E. M. (2010). Cross-cultural perspectives on posttraumatic stress. In G. M.
Rosen & B. C. Frueh (Eds.), Clinician’s guide to posttraumatic stress disorder (pp. 235–261).
Hoboken, NJ: John Wiley and Sons, Inc.
Herbert, M. & Bergeron, M. (2007). Efficacy of a group intervention for adult women survivors of sexual
abuse. Journal of Child Sexual Abuse, 16, 37–61.
Herek, G. M. (2009). Hate crimes and stigma-related experiences among sexual minority adults in the
United States: Prevalence estimates from a national probability sample. Journal of Interpersonal
Violence, 24, 54–74.
Herman, D. B., Susser, E. S., Struening, E. L., & Link, B. L. (1997). Adverse childhood experiences: Are
they risk factors for adult homelessness? American Journal of Public Health, 87, 249–255.
Herman, J. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal
of Traumatic Stress, 5, 377–391.
Herman, J. L. (1992). Trauma and recovery . New York: Basic Books.
Herman, J. L. (1997). Trauma and recovery. (Rev. ed.) New York: Basic Books.
Hermes, E. D., Rosenheck, R. A., Desai, R., & Fontana, A. F. (2012). Recent trends in the treatment of
posttraumatic stress disorder and other mental disorders in the VHA. Psychiatric Services.
Hernandez, P., Gangsei, D., & Engstrom, D. (2007). Vicarious resilience: A new concept in work with
those who survive trauma. Family Process, 46, 229–241.
Herrenkohl, T. I., Sousa, C., Tajima, E. A., Herrenkohl, R. C., & Moylan, C. A. (2008). Intersection of
child abuse and children’s exposure to domestic violence. Trauma, Violence, & Abuse, 9, 84–99.
Hetrick, S. E., Purcell, R., Garner, B., & Parslow, R. (2010). Combined pharmacotherapy and
psychological therapies for post traumatic stress disorder (PTSD). Cochrane Database of Systematic
Reviews, CD007316.
Hetzel-Riggin, M. D. (2010). Peritraumatic dissociation and PTSD effects on physiological response
patterns in sexual assault victims. Psychological Trauma: Theory, Research, Practice, and Policy, 2,
192–200.
Hewitt, L. N., Bhavsar, P., & Phelan, H. A. (2011). The secrets women keep: Intimate partner violence
screening in the female trauma patient. Journal of Trauma, 70, 320–323.
Hien, D. A., Campbell, A. N. C., Ruglass, L. M., Hu, M. C., & Killeen, T. (2010). The role of alcohol
misuse in PTSD outcomes for women in community treatment: A secondary analysis of NIDA’s
Women and Trauma Study. Drug and Alcohol Dependence, 111, 114–119.
Trauma-Informed Care in Behavioral Health Services 3-49
Hien, D. A., Wells, E. A., Jiang, H., Suarez-Morales, L., Campbell, A. N., Cohen, L. R. et al. (2009).
Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and
substance use disorders. Journal of Consulting and Clinical Psychology, 77, 607–619.
Hien, D., Litt, L. C., Cohen, L. R., Miele, G. M., & Campbell, A. (2009). Moving research to practice:
Three community-based examples of concurrent trauma and substance abuse treatment. In D.Hien, L.
C. Litt, L. R. Cohen, G. M. Miele, & A. Campbell (Eds.), Trauma services for women in substance
abuse treatment: An integrated approach (pp. 199–222). Washington, DC: American Psychological
Association.
Hien, D., Litt, L. C., Cohen, L. R., Miele, G. M., & Campbell, A. (2009). Ethnocultural considerations in
the treatment of trauma and addictions. In Trauma services for women in substance abuse treatment:
An integrated approach (pp. 183–198). Washington, DC: American Psychological Association.
Hill, J. J., III, Mobo, B. H., Jr., & Cullen, M. R. (2009). Separating deployment-related traumatic brain
injury and posttraumatic stress disorder in veterans: Preliminary findings from the Veterans Affairs
traumatic brain injury screening program. American Journal of Physical Medicine and Rehabilitation,
88, 605–614.
Hill, J. M., Vernig, P. M., Lee, J. K., Brown, C., & Orsillo, S. M. (2011). The development of a brief
acceptance and mindfulness-based program aimed at reducing sexual revictimization among college
women with a history of childhood sexual abuse. Journal of Clinical Psychology, 67, 969–980.
Hillis, S. D., Anda, R. F., Felitti, V. J., & Marchbanks, P. A. (2001). Adverse childhood experiences and
sexual risk behaviors in women: A retrospective cohort study. Family Planning Perspectives, 33,
206–211.
Hillis, S. D., Anda, R. F., Felitti, V. J., Nordenberg, D., & Marchbanks, P. A. (2000). Adverse childhood
experiences and sexually transmitted diseases in men and women: A retrospective study. Pediatrics,
106, E11.
Himmelfarb, N., Yaeger, D., & Mintz, J. (2006). Posttraumatic stress disorder in female veterans with
military and civilian sexual trauma. Journal of Traumatic Stress, 19, 837–846.
Hinton, D. E., Ba, P., Peou, S., & Um, K. (2000). Panic disorder among Cambodian refugees attending a
psychiatric clinic. Prevalence and subtypes. General Hospital Psychiatry, 22, 437–444.
Hinton, D. E., Chau, H., Nguyen, L., Nguyen, M., Pham, T., Quinn, S. et al. (2001). Panic disorder among
Vietnamese refugees attending a psychiatric clinic: Prevalence and subtypes. General Hospital
Psychiatry, 23, 337–344.
Hinton, D. E., Chhean, D., Pich, V., Safren, S. A., Hofmann, S. G., & Pollack, M. H. (2005). A
randomized controlled trial of cognitive–behavior therapy for Cambodian refugees with treatment-
resistant PTSD and panic attacks: A cross-over design. Journal of Traumatic Stress, 18, 617–629.
Hinton, D. E., Hinton, A. L., Pich, V., Loeum, J. R., & Pollack, M. H. (2009). Nightmares among
Cambodian refugees: The breaching of concentric ontological security. Culture, Medicine and
Psychiatry, 33, 219–265.
Hinton, D. E., Hofmann, S. G., Orr, S. P., Pitman, R. K., Pollack, M. H., & Pole, N. (2010). A
psychobiocultural model of orthostatic panic among Cambodian refugees: Flashbacks, catastrophic
cognitions, and reduced orthostatic blood-pressure response. Psychological Trauma: Theory,
Research, Practice, and Policy, 2, 63–70.
3-50 Part 3, Section 3—General Bibliography
Hinton, D. E., Hofmann, S. G., Pitman, R. K., Pollack, M. H., & Barlow, D. H. (2008). The panic attack–
posttraumatic stress disorder model: Applicability to orthostatic panic among Cambodian refugees.
Cognitive Behaviour Therapy, 37, 101–116.
Hinton, D. E., Hofmann, S. G., Pollack, M. H., & Otto, M. W. (2009). Mechanisms of efficacy of CBT for
Cambodian refugees with PTSD: Improvement in emotion regulation and orthostatic blood pressure
response. CNS Neuroscience & Therapeutics, 15, 255–263.
Hinton, D. E., Hofmann, S. G., Rivera, E., Otto, M. W., & Pollack, M. H. (2011). Culturally adapted CBT
(CA–CBT) for Latino women with treatment-resistant PTSD: A pilot study comparing CA–CBT to
applied muscle relaxation. Behaviour Research and Therapy, 49, 275–280.
Hinton, D. E., Kredlow, M. A., Bui, E., Pollack, M. H., & Hofmann, S. G. (2012). Treatment change of
somatic symptoms and cultural syndromes among Cambodian refugees with PTSD. Depression and
Anxiety, 29, 148–155.
Hinton, D. E., Nickerson, A., & Bryant, R. A. (2011). Worry, worry attacks, and PTSD among Cambodian
refugees: A path analysis investigation. Social Science and Medicine, 72, 1817–1825.
Hinton, D. E., Park, L., Hsia, C., Hofmann, S., & Pollack, M. H. (2009). Anxiety disorder presentations in
Asian populations: A review. CNS Neuroscience & Therapeutics, 15, 295–303.
Hinton, D. E., Pham, T., Tran, M., Safren, S. A., Otto, M. W., & Pollack, M. H. (2004). CBT for
Vietnamese refugees with treatment–resistant PTSD and panic attacks: A pilot study. Journal of
Traumatic Stress, 17, 429–433.
Hinton, D. E., Pich, V., Marques, L., Nickerson, A., & Pollack, M. H. (2010). Khyal attacks: A key idiom
of distress among traumatized Cambodia refugees. Culture, Medicine and Psychiatry, 34, 244–278.
Hinton, D. E., Rivera, E. I., Hofmann, S. G., Barlow, D. H., & Otto, M. W. (2012). Adapting CBT for
traumatized refugees and ethnic minority patients: Examples from culturally adapted CBT (CA–
CBT). Transcultural Psychiatry, 49, 340–365.
Hiskey, S., Luckie, M., Davies, S., & Brewin, C. R. (2008). The emergence of posttraumatic distress in
later life: A review. Journal of Geriatric Psychiatry and Neurology, 21, 232–241.
Hobfoll, S. E., Canetti-Nisim, D., Johnson, R. J., Palmieri, P. A., Varley, J. D., & Galea, S. (2008). The
association of exposure, risk, and resiliency factors with PTSD among Jews and Arabs exposed to
repeated acts of terrorism in Israel. Journal of Traumatic Stress, 21, 9–21.
Hobfoll, S. E., Watson, P., Bell, C. C., Bryant, R. A., Brymer, M. J., Friedman, M. J. et al. (2007). Five
essential elements of immediate and mid–term mass trauma intervention: Empirical evidence.
Psychiatry, 70, 283–315.
Hodas, G. R. (2006). Responding to childhood trauma: The promise and practice of trauma informed care.
Hofmann, S. G. & Smits, J. A. (2008). Cognitive–behavioral therapy for adult anxiety disorders: A meta-
analysis of randomized placebo-controlled trials. Journal of Clinical Psychiatry, 69, 621–632.
Hoge, C. W. (2011). Public health strategies and treatment of service members and veterans with combat-
related mental health problems. In A. B. Adler, P. D. Bliese, & C. A. Castro (Eds.), Deployment
psychology: Evidence-based strategies to promote mental health in the military (pp. 17–34).
Washington, DC: American Psychological Association.
Trauma-Informed Care in Behavioral Health Services 3-51
Hoge, C. W., Terhakopian, A., Castro, C. A., Messer, S. C., & Engel, C. C. (2007). Association of
posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq
War veterans. The American Journal of Psychiatry, 164, 150–153.
Hoge, M. A., Morris, J. A., Daniels, A. S., Stuart, G. W., Huey, L. Y., & Adams, N. (2007). An action plan
for behavioral health workforce development a framework for discussion. Rockville, MD: Substance
Abuse and Mental Health Services Administration.
Holbrook, T. L., Hoyt, D. B., Stein, M. B., & Sieber, W. J. (2001). Perceived threat to life predicts
posttraumatic stress disorder after major trauma: Risk factors and functional outcome. Journal of
Trauma, 51, 287–292.
Holbrook, T. L., Hoyt, D. B., Stein, M. B., & Sieber, W. J. (2002). Gender differences in long-term
posttraumatic stress disorder outcomes after major trauma: Women are at higher risk of adverse
outcomes than men. Journal of Trauma, 53, 882–888.
Hollifield, M. (2011). Acupuncture for posttraumatic stress disorder: conceptual, clinical, and biological
data support further research. CNS Neuroscience & Therapeutics, 17, 769–779.
Honig, A. L. (2010). War then and now: From surviving to thriving. International Journal of Emergency
Mental Health, 12, 207–212.
Hopper, E. K., Bassuk, E. L., & Olivet, J. (2010). Shelter from the storm: Trauma-informed care in
homelessness services settings. The Open Health Services and Policy Journal, 3, 80–100.
Horowitz, M. J. (1989). Posttraumatic stress disorder. In American Psychiatric Association Task Force on
Treatments of Psychiatric Disorders (Ed.), Treatments of psychiatric disorders: A task force report of
the American Psychiatric Association. (pp. 2065–2082). Washington, DC: American Psychiatric
Association.
Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of Event Scale: A measure of subjective stress.
Psychosomatic Medicine, 41, 209–218.
Hoshmand, L. T. (2007). Cultural–ecological perspectives on the understanding and assessment of trauma.
In Cross-cultural assessment of psychological trauma and PTSD (pp. 31–50). New York: Springer
Publishing Science + Business Media.
Hourani, L., Bender, R., Weimer, B., Peeler, R., Bradshaw, M., Lane, M. B. et al. (2012). Longitudinal
study of resilience and mental health in marines leaving military service. Journal of Affective
Disorders.
Houston, J. E., Shevlin, M., Adamson, G., & Murphy, J. (2011). A person-centred approach to modelling
population experiences of trauma and mental illness. Social Psychiatry and Psychiatric
Epidemiology, 46, 149–157.
Hovell, M. F., Wahlgren, D. R., & Adams, M. A. (2009). The logical and empirical basis for the
behavioral ecological model. In R. J. DiClemente, R. Crosby, & M. Kegler (Eds.), Emerging theories
and models in health promotion practice and research. (pp. 415–449). San Francisco: Jossey-Bass
Publishers.
Hovell, M. F., Wahlgren, D. R., & Gehrman, C. (2002). The behavioral ecological model: Integrating
public health and behavioral science. In R. J. DiClemente, R. Crosby, & M. Kegler (Eds.), Emerging
3-52 Part 3, Section 3—General Bibliography
theories and models in health promotion practice and research. (1st ed.), San Francisco: Jossey-Bass
Publishers.
Hoyt, T. & Yeater, E. A. (2010). Comparison of posttraumatic stress disorder symptom structure models in
Hispanic and White college students. Psychological Trauma: Theory, Research, Practice, and Policy,
2, 19–30.
Huang, M. C., Schwandt, M. L., Ramchandani, V. A., George, D. T., & Heilig, M. (2012). Impact of
multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic
inpatients. Alcoholism, Clinical and Experimental Research, 36(6), 598–606.
Huckshorn, K. (2009). Transforming cultures of care toward recovery oriented services: Guidelines
toward creating a trauma informed system of care. Austin, TX: Texas Network of Youth Services.
Hughes, H. M., Humphrey, N. N., & Weaver, T. L. (2005). Advances in Violence and Trauma. Journal of
Interpersonal Violence, 20, 31–38.
Hughes, K. C. & Shin, L. M. (2011). Functional neuroimaging studies of post-traumatic stress disorder.
Expert Review of Neurotherapeutics, 11, 275–285.
Hughes, T., McCabe, S. E., Wilsnack, S. C., West, B. T., & Boyd, C. J. (2010). Victimization and
substance use disorders in a national sample of heterosexual and sexual minority women and men.
Addiction, 105, 2130–2140.
Hui, C. H. & Triandis, H. C. (1986). Individualism–collectivism: A study of cross-cultural researchers.
Journal of Cross-Cultural Psychology, 17, 225–248.
Hulette, A. C., Kaehler, L. A., & Freyd, J. J. (2011). Intergenerational associations between trauma and
dissociation. Journal of Family Violence, 26, 217–225.
Humphreys, C. (2007). A health inequalities perspective on violence against women. Health and Social
Care in the Community, 15, 120–127.
Huriwai, T. (2002). Re-enculturation: Culturally congruent interventions for Maori with alcohol- and drug-
use–associated problems in New Zealand. Substance Use and Misuse, 37, 1259–1268.
Hussain, A., Weisaeth, L., & Heir, T. (2011). Changes in religious beliefs and the relation of religiosity to
posttraumatic stress and life satisfaction after a natural disaster. Social Psychiatry and Psychiatric
Epidemiology, 46, 1027–1032.
Hussain, A., Weisaeth, L., & Heir, T. (2011). Psychiatric disorders and functional impairment among
disaster victims after exposure to a natural disaster: A population based study. Journal of Affective
Disorders, 128, 135–141.
Hutton, D. (2000). Patterns of psychosocial coping and adaptation among riverbank erosion-induced
displacees in Bangladesh: Implications for development programming. Prehospital Disaster
Medicine, 15, S99.
Ilgen, M. A., Bohnert, A. S., Ignacio, R. V., McCarthy, J. F., Valenstein, M. M., Kim, H. M. et al. (2010).
Psychiatric diagnoses and risk of suicide in veterans. Archives of General Psychiatry, 67, 1152–1158.
Ilgen, M. A., Haas, E., Czyz, E., Webster, L., Sorrell, J. T., & Chermack, S. (2011). Treating chronic pain
in veterans presenting to an addictions treatment program. Cognitive and Behavioral Practice, 18,
149–160.
Trauma-Informed Care in Behavioral Health Services 3-53
Iliffe, G. & Steed, L. G. (2000). Exploring the counselor’s experience of working with perpetrators and
survivors of domestic violence. Journal of Interpersonal Violence, 15, 393–412.
Institute of Medicine (2008). Treatment of posttraumatic stress disorder: An assessment of the evidence.
Washington, DC: The National Academies Press.
Institute of Medicine (2012). Treatment of posttraumatic stress disorder in military and veteran
populations: Initial assessment. Washington, DC: The National Academies Press.
Institute of Medicine, Committee on Prevention of Mental Disorders and Substance Abuse Among
Children, O’Connell, M. E., Boat, T. F., Warner, K. E., National Research Council (U.S.) et al.
(2009). Preventing mental, emotional, and behavioral disorders among young people progress and
possibilities. Washington, DC: National Academies Press.
Institute of Medicine & National Research Council (2007). PTSD compensation and military service.
Washington, DC: The National Academies Press.
Inter-Agency Standing Committee (2008). Mental health and psychosocial support in emergency settings
Geneva, Switzerland: World Health Organization.
Introduction to the special issue on trauma and ethnoracial diversity (2010). Psychological Trauma:
Theory, Research, Practice, and Policy, 2, 1–3.
Ipser, J. C. & Stein, D. J. (2012). Evidence-based pharmacotherapy of post-traumatic stress disorder
(PTSD). The International Journal of Neuropharmacology, 15, 825–840.
Isserlin, L., Zerach, G., & Solomon, Z. (2008). Acute stress responses: A review and synthesis of ASD,
ASR, and CSR. American Journal of Orthopsychiatry, 78, 423–429.
Jackson, C., Nissenson, K., & Cloitre, M. (2009). Cognitive–behavioral therapy. In C. A. Courtois (Ed.),
Treating complex traumatic stress disorders: An evidence-based guide (pp. 243–263). New York:
Guilford Press.
Jackson, C., Nissenson, K., & Cloitre, M. (2010). Treatment for complex PTSD. In D. Sookman (Ed.),
Treatment resistant anxiety disorders: Resolving impasses to symptom remission (pp. 75–104). New
York: Routledge/Taylor & Francis Group.
Jacobs, G. A. & Meyer, D. L. (2006). Psychological first aid: Clarifying the concept. In L. Barbanel & R.
J. Sternberg (Eds.), Psychological interventions in times of crisis (pp. 57–71). New York: Springer
Publishing.
Jainchill, N., Hawke, J., & Yagelka, J. (2000). Gender, psychopathology, and patterns of homelessness
among clients in shelter-based TCs. American Journal of Drug and Alcohol Abuse, 26, 553–567.
James, D. J. & Glaze, L. E. (2006). Mental health problems of prison and jail inmates. Washington, DC:
Bureau of Justice Statistics.
Jameson, C. (2010). The “short step” from love to hypnosis: A reconsideration of the Stockholm
syndrome. Journal for Cultural Research, 14, 337–355.
Jankoski, J. A. (2010). Is vicarious trauma the culprit? A study of child welfare professionals. Child
Welfare, 89, 105–120.
Janoff-Bulman, R. (1992). Shattered assumptions: Towards a new psychology of trauma. New York: Free
Press.
3-54 Part 3, Section 3—General Bibliography
Janssen, I., Krabbendam, L., Bak, M., Hanssen, M., Vollebergh, W., de, G. R. et al. (2004). Childhood
abuse as a risk factor for psychotic experiences. Acta Psychiatrica Scandinavica, 109, 38–45.
Jason, L. A., Mileviciute, I., Aase, D. M., Stevens, E., DiGangi, J., Contreras, R. et al. (2011). How type of
treatment and presence of PTSD affect employment, self-regulation, and abstinence. North American
Journal of Psychology, 13, 175–186.
Jayasinghe, N., Spielman, L., Cancellare, D., Difede, J., Klausner, E. J., & Giosan, C. (2005). Predictors of
treatment utilization in World Trade Center attack disaster workers: Role of race/ethnicity and
symptom severity. International Journal of Emergency Mental Health, 7, 91–99.
Jaycox, L. H., Marshall, G. N., & Schell, T. (2004). Use of mental health services by men injured through
community violence. Psychiatric Services, 55, 415–420.
Jaycox, L. H., Zoellner, L., & Foa, E. B. (2002). Cognitive–behavior therapy for PTSD in rape survivors.
Journal of Clinical Psychology, 58, 891–906.
Jenkins, S. R. & Baird, S. (2002). Secondary traumatic stress and vicarious trauma: A validational study.
Journal of Traumatic Stress, 15, 423–432.
Jennings, A. (2004). Models for developing trauma-informed behavioral health systems and trauma-
specific services. Rockville, MD: Center for Mental Health Services.
Jennings, A. (2007). Blueprint for action: Building trauma-informed mental health service systems: state
accomplishments, activities and resources. Alexandria, VA: National Association of State Mental
Health Program Directors (NASMHPD) and the National Technical Assistance Center for State
Mental Health Planning (NTAC).
Jennings, A. (2007). Criteria for building a trauma-informed mental health service system. Adapted from
“Developing trauma-informed behavioral health systems”(2003), Andrea Blanch PhD.
Jennings, A. (2009). Models for developing trauma-informed behavioral health systems and trauma-
specific services: 2008 update. Alexandria, VA: National Center for Trauma-Informed Care.
Jobson, L. & O’Kearney, R. (2008). Cultural differences in personal identity in post-traumatic stress
disorder. British Journal of Clinical Psychology, 47, 95–109.
Jobson, L. & O’Kearney, R. T. (2009). Impact of cultural differences in self on cognitive appraisals in
posttraumatic stress disorder. Behavioural and Cognitive Psychotherapy, 37, 249–266.
Joe, S., Baser, R. E., Breeden, G. K., Neighbors, H. W., & Jackson, J. S. (2006). Prevalence of and risk
factors for lifetime suicide attempts among blacks in the United States. JAMA, 296, 2112–2123.
Johnson, D. M. & Zlotnick, C. (2006). A cognitive–behavioral treatment for battered women with PTSD in
shelters: findings from a pilot study. Journal of Traumatic Stress, 19, 559–564.
Johnson, D. M. & Zlotnick, C. (2007). Utilization of mental health treatment and other services by battered
women in shelters. Psychiatric Services, 58, 1595–1597.
Johnson, D. M., Palmieri, P. A., Jackson, A. P., & Hobfoll, S. E. (2007). Emotional numbing weakens
abused inner-city women’s resiliency resources. Journal of Traumatic Stress, 20, 197–206.
Johnson, D. M., Zlotnick, C., & Perez, S. (2011). Cognitive behavioral treatment of PTSD in residents of
battered women’s shelters: results of a randomized clinical trial. Journal of Consulting and Clinical
Psychology, 79, 542–551.
Trauma-Informed Care in Behavioral Health Services 3-55
Johnson, D. R., Lahad, M., & Gray, A. (2009). Creative therapies for adults. In E. B. Foa, T. M. Keane, M.
J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines from the
International Society for Traumatic Stress Studies (2nd ed.) (pp. 479–490). New York: Guilford
Press.
Johnson, H. & Thompson, A. (2008). The development and maintenance of post-traumatic stress disorder
(PTSD) in civilian adult survivors of war trauma and torture: A review. Clinical Psychology Review,
28, 36–47.
Johnson, H., Thompson, A., & Downs, M. (2009). Non-Western interpreters’ experiences of trauma: The
protective role of culture following exposure to oppression. Ethnicity and Health, 14, 407–418.
Johnson, J. L., Baldwin, J., Haring, R. C., Wiechelt, S. A., Roth, S., Gryczynski, J. et al. (2008). Essential
information for disaster management and trauma specialists working with American Indians. In A. J.
Marsella, J. L. Johnson, P. Watson, & J. Gryczynski (Eds.), Ethnocultural perspectives on disaster
and trauma: Foundations, issues, and applications (pp. 73–113). New York: Springer Publishing
Science + Business Media.
Johnson, S. D. (2008). Substance use, post-traumatic stress disorder and violence. Current Opinion in
Psychiatry, 21, 242–246.
Johnson, S. D., Striley, C., & Cottler, L. B. (2006). The association of substance use disorders with trauma
exposure and PTSD among African American drug users. Addictive Behaviors, 31, 2063–2073.
Johnson, S. M. & Courtois, C. A. (2009). Couple therapy. In C. A. Courtois & J. D. Ford (Eds.), Treating
complex traumatic stress disorders: An evidence-based guide (pp. 371–390). New York: Guilford
Press.
Johnson, S. M., Hunsley, J., Greenberg, L., & Schindler, D. (1999). Emotionally focused couples therapy:
Status and challenges. Clinical Psychology: Science and Practice, 6, 67–79.
Jones, B. H. & Knapik, J. J. (1999). Physical training and exercise-related injuries. Surveillance, research
and injury prevention in military populations. Sports Medicine, 27, 111–125.
Jones, N., Roberts, P., & Greenberg, N. (2003). Peer-group risk assessment: A post-traumatic management
strategy for hierarchical organizations. Occupational Medicine, 53, 469–475.
Jordan, B. K., Schlenger, W. E., Hough, R., Kulka, R. A., Weiss, D., Fairbank, J. A. et al. (1991). Lifetime
and current prevalence of specific psychiatric disorders among Vietnam veterans and controls.
Archives of General Psychiatry, 48, 207–215.
Jovanovic, T., Smith, A., Kamkwalala, A., Poole, J., Samples, T., Norrholm, S. D. et al. (2011).
Physiological markers of anxiety are increased in children of abused mothers. Journal of Child
Psychology and Psychiatry, 52, 844–852.
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. (1st ed.)
New York: Hyperion.
Kabat-Zinn, J., University of Massachusetts Medical Center/Worcester, & Stress, R. C. (1990). Full
catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New
York: Delacorte Press.
Kalra, H., Kamath, P., Trivedi, J. K., & Janca, A. (2008). Caregiver burden in anxiety disorders. Current
Opinion in Psychiatry, 21, 70–73.
3-56 Part 3, Section 3—General Bibliography
Kaltman, S., Green, B. L., Mete, M., Shara, N., & Miranda, J. (2010). Trauma, depression, and comorbid
PTSD/depression in a community sample of Latina immigrants. Psychological Trauma: Theory,
Research, Practice, and Policy, 2, 31–39.
Kang, H. K., Natelson, B. H., Mahan, C. M., Lee, K. Y., & Murphy, F. M. (2003). Post-traumatic stress
disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based
survey of 30,000 veterans. American Journal of Epidemiology, 157, 141–148.
Kang, H., Dalager, N., Mahan, C., & Ishii, E. (2005). The role of sexual assault on the risk of PTSD
among Gulf War veterans. Annals of Epidemiology, 15, 191–195.
Kang, Y. S., Choi, S. Y., & Ryu, E. (2009). The effectiveness of a stress coping program based on
mindfulness meditation on the stress, anxiety, and depression experienced by nursing students in
Korea. Nurse Education Today, 29, 538–543.
Kanter, J. (2007). Compassion fatigue and secondary traumatization: A second look. Clinical Social Work
Journal, 35, 289–293.
Kantor, E. M. & Beckett, D. R. (2011). Psychological first aid. In F. J. Stoddard, Jr., A. Pandya, & C. L.
Katz (Eds.), Disaster psychiatry: Readiness, evaluation, and treatment (pp. 203–212). Arlington, VA:
American Psychiatric Publishing, Inc.
Kar, N. (2011). Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: A review.
Neuropsychiatric Disease and Treatment, 7, 167–181.
Karatzias, T., Power, K., Brown, K., McGoldrick, T., Begum, M., Young, J. et al. (2011). A controlled
comparison of the effectiveness and efficiency of two psychological therapies for posttraumatic stress
disorder: Eye movement desensitization and reprocessing vs. emotional freedom techniques. Journal
of Nervous and Mental Disease, 199, 372–378.
Karl, A., Schaefer, M., Malta, L. S., Dorfel, D., Rohleder, N., & Werner, A. (2006). A meta-analysis of
structural brain abnormalities in PTSD. Neuroscience and Biobehavioral Reviews, 30, 1004–1031.
Karney, B. R., Ramchand, R., Osilla, K. C., Caldarone, L. B., & Burns, R. M. (2008). Invisible wounds:
Predicting the immediate and long term consequences of mental health problems in veterans of
Operation Enduring Freedom and Operation Iraqi Freedom. Santa Monica, CA: The RAND Center
for Military Health Policy Research.
Karon, B. P. & Widener, A. J. (1997). Repressed memories and World War II: Lest we forget!
Professional Psychology: Research and Practice, 28, 338–340.
Kartha, A., Brower, V., Saitz, R., Samet, J. H., Keane, T. M., & Liebschutz, J. (2008). The impact of
trauma exposure and post-traumatic stress disorder on healthcare utilization among primary care
patients. Medical Care, 46, 388–393.
Kashdan, T. B., Morina, N., & Priebe, S. (2009). Post-traumatic stress disorder, social anxiety disorder,
and depression in survivors of the Kosovo War: Experiential avoidance as a contributor to distress
and quality of life. Journal of Anxiety Disorders, 23, 185–196.
Kastrup, M. (2011). PTSD epidemiology with particular reference to gender. In D. J. Stein, M. J.
Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 82–87). Chichester, UK: John
Wiley and Sons, Inc.
Trauma-Informed Care in Behavioral Health Services 3-57
Kataoka, S. H., Stein, B. D., Jaycox, L. H., Wong, M., Escudero, P., Tu, W. et al. (2003). A school-based
mental health program for traumatized Latino immigrant children. Journal of the American Academy
of Child & Adolescent Psychiatry, 42, 311–318.
Kauffman, J. (2002). Loss of the assumptive world: A theory of traumatic loss. New York: Brunner-
Routledge.
Kawachi, I. & Subramanian, S. V. (2006). Measuring and modeling the social and geographic context of
trauma: a multilevel modeling approach. Journal of Traumatic Stress, 19, 195–203.
Keane, T. M., Caddell, J. M., & Taylor, K. L. (1988). Mississippi Scale for Combat-Related Posttraumatic
Stress Disorder: Three studies in reliability and validity. Journal of Consulting & Clinical
Psychology, 56, 85–90.
Keane, T. M., Brief, D. J., Pratt, E. M., & Miller, M. W. (2007). Assessment of PTSD and its
comorbidities in adults. In M. J. Friedman, T. M. Keane, & P. A. Resick (Eds.), Handbook of PTSD:
Science and practice (pp. 279–305). New York: Guilford Press.
Keane, T. M., Fairbank, J. A., Caddell, J. M., Zimering, R. T., Taylor, K. L., & Mora, C. A. (1989).
Clinical evaluation of a measure to assess combat exposure. Psychological Assessment, 1, 53–55.
Keane, T. M. & Piwowarczyk, L. A. (2006). Trauma, terror, and fear: Mental health professionals respond
to the impact of 9/11––An overview. In L. A. Schein, H. I. Spitz, G. M. Burlingame, & P. R. Muskin
(Eds.), Psychological effects of catastrophic disasters: Group approaches to treatment (pp. 3–16).
New York: Haworth Press.
Kearney, D. J., McDermott, K., Malte, C., Martinez, M., & Simpson, T. L. (2012). Association of
participation in a mindfulness program with measures of PTSD, depression and quality of life in a
veteran sample. Journal of Clinical Psychology, 68, 101–116.
Keim, J., Olguin, D. L., Marley, S. C., & Thieman, A. (2008). Trauma and burnout: Counselors in training.
In Compelling counseling interventions: Celebrating VISTAS’ fifth anniversary (pp. 293–303).
Alexandria, VA, US: American Counseling Association; Ann Arbor, MI: Counseling Outfitters.
Keinan, G., Shrira, A., & Shmotkin, D. (2011). The association between cumulative adversity and mental
health: Considering dose and primary focus of adversity. Quality of Life Research.
Keller, L. O., Strohschein, S., Schaffer, M. A., & Lia-Hoagberg, B. (2004). Population-based public health
interventions: Innovations in practice, teaching, and management, part II. Public Health Nursing, 21,
469–487.
Kelly, C. M., Jorm, A. F., & Kitchener, B. A. (2010). Development of mental health first aid guidelines on
how a member of the public can support a person affected by a traumatic event: A Delphi study. BMC
Psychiatry, 10, 49.
Kelly, D. C., Howe–Barksdale, S., & Gitelson, D. (2011). Treating young veterans: Promoting resilience
through practice and advocacy. New York: Springer Publishing.
Kelly, U. A., Skelton, K., Patel, M., & Bradley, B. (2011). More than military sexual trauma: Interpersonal
violence, PTSD, and mental health in women veterans. Research in Nursing and Health, 34, 457–
467.
3-58 Part 3, Section 3—General Bibliography
Kelly, V. G., Merrill, G. S., Shumway, M., Alvidrez, J., & Boccellari, A. (2010). Outreach, engagement,
and practical assistance: Essential aspects of PTSD care for urban victims of violent crime. Trauma,
Violence, and Abuse: A Review Journal, 11, 144–156.
Kent, M., Davis, M. C., Stark, S. L., & Stewart, L. A. (2011). A resilience-oriented treatment for
posttraumatic stress disorder: Results of a preliminary randomized clinical trial. Journal of Traumatic
Stress, 24, 591–595.
Kerig, P. K., Sink, H. E., Cuellar, R. E., Vanderzee, K. L., & Elfstrom, J. L. (2010). Implementing trauma-
focused CBT with fidelity and flexibility: A family case study. Journal of Clinical Child &
Adolescent Psychology, 39, 713–722.
Kersting, A., Reutemann, M., Gast, U., Ohrmann, P., Suslow, T., Michael, N. et al. (2003). Dissociative
disorders and traumatic childhood experiences in transsexuals. Journal of Nervous and Mental
Disease, 191, 182–189.
Kessler, R. C. & Merikangas, K. R. (2004). The National Comorbidity Survey Replication (NCS–R):
Background and aims. International Journal of Methods in Psychiatric Research, 13, 60–68.
Kessler, R. C. (2000). Posttraumatic stress disorder: The burden to the individual and to society. Journal of
Clinical Psychiatry, 61 Supplement 5, 4–12.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime
prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey
Replication. Archives of General Psychiatry, 62, 593–602.
Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of
12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General
Psychiatry, 62, 617–627.
Kessler, R. C., Cox, B. J., Green, J. G., Ormel, J., McLaughlin, K. A., Merikangas, K. R. et al. (2011). The
effects of latent variables in the development of comorbidity among common mental disorders.
Depression and Anxiety, 28, 29–39.
Kessler, R. C., Crum, R. M., Warner, L. A., Nelson, C. B., Schulenberg, J., & Anthony, J. C. (1997).
Lifetime co-occurrence of DSM-III–R alcohol abuse and dependence with other psychiatric disorders
in the National Comorbidity Survey. Archives of General Psychiatry, 54, 313–321.
Kessler, R. C., McGonagle, K. A., Zhao, S., Nelson, C. B., Hughes, M., Eshleman, S. et al. (1994).
Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Archives
of General Psychiatry, 51, 8–19.
Kessler, R. C., McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M. et al.
(2010). Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys.
The British Journal of Psychiatry, 197, 378–385.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder
in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., Nelson, C. B., & Breslau, N. N. (1999).
Epidemiological risk factors for trauma and PTSD. In R. Yehuda (Ed.), Risk Factors for PTSD. (pp.
23–59). Washington, DC: American Psychiatric Press.
Trauma-Informed Care in Behavioral Health Services 3-59
Khan, F., Amatya, B., & Hoffman, K. (2012). Systematic review of multidisciplinary rehabilitation in
patients with multiple trauma. British Journal of Surgery, 99, Supplementement 1, 88–96.
Khantzian, E. J. (1985). The self-medication hypothesis of addictive disorders: Focus on heroin and
cocaine dependence. American Journal of Psychiatry, 142, 1259–1264.
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and
recent applications. Harvard Review of Psychiatry, 4, 231–244.
Khaylis, A., Polusny, M. A., Erbes, C. R., Gewirtz, A., & Rath, M. (2011). Posttraumatic stress, family
adjustment, and treatment preferences among National Guard Soldiers deployed to OEF/OIF. Military
Medicine, 176, 126–131.
Khoo, A., Dent, M. T., & Oei, T. P. S. (2011). Group cognitive behaviour therapy for military service-
related post-traumatic stress disorder: Effectiveness, sustainability and repeatability. Australian and
New Zealand Journal of Psychiatry, 45, 663–672.
Kichic, R., Vera, M., & Reyes-Rabanillo, M. L. (2011). Challenges in the dissemination and
implementation of exposure-based CBT for the treatment of Hispanics with PTSD. In D. J. Stein, M.
J. Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 205–207). Chichester, UK: John
Wiley and Sons, Inc.
Kilcommons, A. M. & Morrison, A. P. (2005). Relationships between trauma and psychosis: An
exploration of cognitive and dissociative factors. Acta Psychiatrica Scandinavica, 112, 351–359.
Kilcommons, A. M., Morrison, A. P., Knight, A., & Lobban, F. (2008). Psychotic experiences in people
who have been sexually assaulted. Social Psychiatry and Psychiatric Epidemiology, 43, 602–611.
Kilpatrick, D. G., Acierno, R., Resnick, H. S., Saunders, B. E., & Best, C. L. (1997). A 2-year longitudinal
analysis of the relationships between violent assault and substance use in women. Journal of
Consulting and Clinical Psychology, 65, 834–847.
Kilpatrick, D. G., Veronen, L. J., & Resick, P. A. (1982). Psychological sequelae to rape: Assessment and
treatment strategies. In D. M. Doleys, R. L. Meredith, & A. R. Ciminero (Eds.), Behavioral medicine:
Assessment and treatment strategies (pp. 473–497). New York: Plenum.
Kim, E. (2009). Multidimensional acculturation attitudes and depressive symptoms in Korean Americans.
Issues in Mental Health Nursing, 30, 98–103.
Kim, M. M., Ford, J. D., Howard, D. L., & Bradford, D. W. (2010). Assessing trauma, substance abuse,
and mental health in a sample of homeless men. Health & Social Work, 35, 39–48.
Kimbrough, E., Magyari, T., Langenberg, P., Chesney, M., & Berman, B. (2010). Mindfulness
intervention for child abuse survivors. Journal of Clinical Psychology, 66, 17–33.
Kimerling, R. & Baumrind, N. (2005). Access to specialty mental health services among women in
California. Psychiatric Services, 56, 729–734.
Kimerling, R. & Calhoun, K. S. (1994). Somatic symptoms, social support, and treatment seeking among
sexual assault victims. Journal of Consulting and Clinical Psychology, 62, 333–340.
Kimerling, R., Ouimette, P., & Weitlauf, J. C. (2007). Gender issues in PTSD. In M. J. Friedman, T. M.
Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 207–228). New York:
Guilford Press.
3-60 Part 3, Section 3—General Bibliography
Kimerling, R., Street, A. E., Pavao, J., Smith, M. W., Cronkite, R. C., Holmes, T. H. et al. (2010).
Military-related sexual trauma among Veterans Health Administration patients returning from
Afghanistan and Iraq. American Journal of Public Health, 100, 1409–1412.
King, D. W., King, L. A., Foy, D. W., & Gudanowski, D. M. (1996). Prewar factors in combat-related
posttraumatic stress disorder: Structural equation modeling with a national sample of female and male
Vietnam veterans. Journal of Consulting and Clinical Psychology, 64, 520–531.
Kira, I. A. (2010). Etiology and treatment of post-cumulative traumatic stress disorders in different
cultures. Traumatology, 16, 128–141.
Kira, I. A., Ahmed, A., Wasim, F., Mahmoud, V., Colrain, J., & Rai, D. (2012). Group therapy for
refugees and torture survivors: Treatment model innovations. International Journal of Group
Psychotherapy, 62, 69–88.
Kira, I. A., Lewandowski, L. A., Templin, T. N., Ramaswamy, V., Ozkan, B., & Mohanesh, J. (2009). The
effects of post-retribution inter-group forgiveness: The case of Iraqi refugees. Peace and Conflict, 15,
385–413.
Kirmayer, L. J. (1996). Confusion of the senses: Implications of ethnocultural variations in somatoform
and dissociative disorders for PTSD. In A. J. Marsella & M. J. Friedman (Eds.), Ethnocultural
aspects of posttraumatic stress disorder: Issues, research, and clinical applications (pp. 131–163).
Washington, DC: American Psychological Association.
Kirmayer, L. J., Rousseau, C., & Measham, T. (2011). Sociocultural considerations. In D. M. Benedek &
G. H. Wynn (Eds.), Clinical manual for management of PTSD (pp. 415–444). Arlington, VA:
American Psychiatric Publishing, Inc.
Kiser, L. J. (2007). Protecting children from the dangers of urban poverty. Clinical Psychology Review, 27,
211–225.
Kiser, L. J., Donohue, A., Hodgkinson, S., Medoff, D., & Black, M. M. (2010). Strengthening family
coping resources: The feasibility of a multifamily group intervention for families exposed to trauma.
Journal of Traumatic Stress, 23, 802–806.
Kitayama, N., Vaccarino, V., Kutner, M., Weiss, P., & Bremner, J. D. (2005). Magnetic resonance
imaging (MRI) measurement of hippocampal volume in posttraumatic stress disorder: A meta-
analysis. Journal of Affective Disorders, 88, 79–86.
Klariç, M., Francciskovic, T., Klariç, B., Kresiç, M., Grkoviç, J., Lisica, I. D. et al. (2008). Social support
and PTSD symptoms in war-traumatized women in Bosnia and Herzegovina. Psychiatria Danubina,
20, 466–473.
Klaus, P. A. (2007). Crime and the nation’s households, 2005. Washington, DC: U.S. Department of
Justice.
Klinic Community Health Centre (2008). Trauma-informed: The trauma toolkit: A resource for service
organizations and providers to deliver services that are trauma-informed. Winnipeg, Manitoba:
Klinic Community Health Centre.
Knoll, J. & Resnick, P. J. (2006). The detection of malingered post-traumatic stress disorder. Psychiatric
Clinics of North America, 29, 629–647.
Trauma-Informed Care in Behavioral Health Services 3-61
Knudsen, H. K., Ducharme, L. J., & Roman, P. M. (2006). Counselor emotional exhaustion and turnover
intention in therapeutic communities. Journal of Substance Abuse Treatment, 31, 173–180.
Koenen, K. C. (2006). Developmental epidemiology of PTSD: self-regulation as a central mechanism.
Annals of the New York Academy of Sciences, 1071, 255–266.
Koenen, K. C., Moffitt, T. E., Caspi, A., Gregory, A., Harrington, H., & Poulton, R. (2008). The
developmental mental-disorder histories of adults with posttraumatic stress disorder: A prospective
longitudinal birth cohort study. Journal of Abnormal Psychology, 117, 460–466.
Koenen, K. C., Moffitt, T. E., Poulton, R., Martin, J., & Caspi, A. (2007). Early childhood factors
associated with the development of post-traumatic stress disorder: Results from a longitudinal birth
cohort. Psychol. Med, 37, 181–192.
Koenen, K. C., Nugent, N. R., & Amstadter, A. B. (2008). Gene–environment interaction in posttraumatic
stress disorder: Review, strategy and new directions for future research. European Archives of
Psychiatry and Clinical Neuroscience, 258, 82–96.
Koenen, K. C., Stellman, J. M., Stellman, S. D., & Sommer, J. F., Jr. (2003). Risk factors for course of
posttraumatic stress disorder among Vietnam veterans: A 14-year follow-up of American
Legionnaires. Journal of Consulting & Clinical Psychology, 71, 980–986.
Koenen, K. C., Stellman, S. D., Sommer, J. F., Jr., & Stellman, J. M. (2008). Persisting posttraumatic
stress disorder symptoms and their relationship to functioning in Vietnam veterans: A 14-year
follow–up. Journal of Traumatic Stress, 21, 49–57.
Kohrt, B. A. & Hruschka, D. J. (2010). Nepali concepts of psychological trauma: The role of idioms of
distress, ethnopsychology and ethnophysiology in alleviating suffering and preventing stigma.
Culture, Medicine and Psychiatry, 34, 322–352.
Kolassa, I. T., Eckart, C., Ruf, M., Neuner, F., de Quervain, D. J. F., & Elbert, T. (2007). Lack of cortisol
response in patients with posttraumatic stress disorder (PTSD) undergoing a diagnostic interview.
BMC Psychiatry, 7.
Kornør, H., Winje, D., Ekeberg, Ÿ., Weisaeth, L., Kirkehei, I., Johansen, K. et al. (2008). Early trauma-
focused cognitive–behavioural therapy to prevent chronic post-traumatic stress disorder and related
symptoms: A systematic review and meta-analysis. BMC Psychiatry, 8.
Koss, M. P. (2005). Empirically enhanced reflections on 20 years of rape research. Journal of
Interpersonal Violence, 20, 100–107.
Kozaric-Kovacic, D., Ljubin, T., & Grappe, M. (2000). Comorbidity of posttraumatic stress disorder and
alcohol dependence in displaced persons. Croatian Medical Journal, 41, 173–178.
Kramer, T. L. & Green, B. L. (1997). Post-traumatic stress disorder: A historical context and evolution. In
D.F.Halpern (Ed.), States of mind: American and post-Soviet perspectives on contemporary issues in
psychology (pp. 215–237). New York: Oxford University Press.
Krause, E. D., Kaltman, S., Goodman, L. A., & Dutton, M. A. (2008). Avoidant coping and PTSD
symptoms related to domestic violence exposure: A longitudinal study. Journal of Traumatic Stress,
21, 83–90.
Kreidler, M. & Einsporn, R. (2012). A comparative study of therapy duration for survivors of childhood
sexual abuse. Journal of Psychosocial Nursing and Mental Health Services, 50, 26–32.
3-62 Part 3, Section 3—General Bibliography
Kremen, W. S., Koenen, K. C., Boake, C., Purcell, S., Eisen, S. A., Franz, C. E. et al. (2007). Pretrauma
cognitive ability and risk for posttraumatic stress disorder: A twin study. Archives of General
Psychiatry, 64, 361–368.
Kress, V. E. & Hoffman, R. M. (2008). Non-suicidal self-injury and motivational interviewing: Enhancing
readiness for change. Journal of Mental Health Counseling, 30, 311–329.
Krieger, N. (2011). Epidemiology and the people’s health: Theory and context. New York: Oxford
University Press.
Kroes, M. C., Rugg, M. D., Whalley, M. G., & Brewin, C. R. (2011). Structural brain abnormalities
common to posttraumatic stress disorder and depression. Journal of Psychiatry and Neuroscience, 36,
256–265.
Krupnick, J. L., Green, B. L., Stockton, P., Miranda, J., Krause, E., & Mete, M. (2008). Group
interpersonal psychotherapy for low-income women with posttraumatic stress disorder. Psychother
Res, 18, 497–507.
Krysinska, K. & Lester, D. (2010). Post-traumatic stress disorder and suicide risk: A systematic review.
Archives of Suicide Research, 14, 1–23.
Krysinska, K., Lester, D., & Martin, G. (2009). Suicidal behavior after a traumatic event. Journal of
Trauma Nursing, 16, 103–110.
Kubany, E. S., Haynes, S. N., Leisen, M. B., Owens, J. A., Kaplan, A. S., Watson, S. B. et al. (2000).
Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The
Traumatic Life Events Questionnaire. Psychological Assessment, 12, 210–224.
Kubany, E. S., Hill, E. E., Owens, J. A., Iannce–Spencer, C., McCaig, M. A., Tremayne, K. J. et al. (2004).
Cognitive trauma therapy for battered women with PTSD (CTT–BW). Journal of Consulting and
Clinical Psychology, 72, 3–18.
Kubany, E. S., Leisen, M. B., Kaplan, A. S., & Kelly, M. P. (2000). Validation of a brief measure of
posttraumatic stress disorder: The distressing event questionnaire (DEQ). Psychological Assessment,
12, 197–209.
Kubzansky, L. D., Koenen, K. C., Spiro III, A., Vokonas, P. S., & Sparrow, D. (2007). Perspective study
of posttraumatic stress disorder symptoms and coronary heart disease in the normative aging study.
Archives of General Psychiatry, 64, 109–116.
Kudler, H. S., Krupnick, J. L., Blank, A. S., Jr., Herman, J. L., & Horowitz, M. J. (2009). Psychodynamic
therapy for adults. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective
treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies
(2nd ed.) (pp. 346–369). New York: Guilford Press.
Kuhn, J. H. & Nakashima, J. (2011). Community Homelessness Assessment, Local Education and
Networking Group (CHALENG) for veterans: The fifteenth annual progress report on public law
105–114 services for homeless veterans assessment and coordination, March 11, 2009. Washington,
DC: Department of Veterans Affairs.
Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R. L., Jordan, B. K., & Marmar, C. R. (1990a).
The National Vietnam Veterans Readjustment Study: Tables of findings and technical appendices.
Research Triangle Park, NC: Research Triangle Institute.
Trauma-Informed Care in Behavioral Health Services 3-63
Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R. L., Jordan, B. K., Marmar, C. R. et al. (1990b).
Trauma and the Vietnam war generation: Report of findings from the National Vietnam Veterans
Readjustment Study. New York: Brunner/Mazel.
Kun, P., Han, S., Chen, X., & Yao, L. (2009). Prevalence and risk factors for posttraumatic stress disorder:
A cross-sectional study among survivors of the Wenchuan 2008 earthquake in China. Depression and
Anxiety, 26, 1134–1140.
Kushner, M. G., Krueger, R., Frye, B., & Peterson, J. (2008). Epidemiological perspectives on co-
occurring anxiety disorder and substance use disorder. In S. H. Stewart & P. J. Conrod (Eds.), Anxiety
and substance use disorders: The vicious cycle of comorbidity (pp. 3–17). New York: Springer
Publishing Science + Business Media.
Kutter, C. J., Wolf, E. J., & McKeever, V. M. (2004). Predictors of veterans’ participation in cognitive–
behavioral group treatment for PTSD. Journal of Traumatic Stress, 17, 157–162.
Kuzma, J. M. & Black, D. W. (2004). Integrating pharmacotherapy and psychotherapy in the management
of anxiety disorders. Current Psychiatry Reports, 6, 268–273.
Laban, C. J., Gernaat, H. B. P. E., Komproe, I. H., van der Tweel, I., & de Jong, J. T. V. M. (2005).
Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the
Netherlands. Journal of Nervous and Mental Disease, 193, 825–832.
Laban, C. J., Komproe, I. H., Gernaat, H. B. P. E., & De Jong, T. V. M. (2008). The impact of a long
asylum procedure on quality of life, disability and physical health in Iraqi asylum seekers in the
Netherlands. Social Psychiatry and Psychiatric Epidemiology, 43, 507–515.
Labrie, V. & Roder, J. C. (2010). The role of NMDA receptors in the pathophysiology and treatment of
anxiety syndromes. In L. Sher & A. Vilens (Eds.), Neurobiology of post-traumatic stress disorder
(pp. 291–308). Nova Science Publishers, Inc.
Lacoursiere, R. B. (2001). “Burnout” and substance user treatment: The phenomenon and the
administrator–clinician’s experience. Substance Use & Misuse, 36, 1839–1874.
Laflamme, L., Burrows, S., & Hasselberg, M. (2009). Socioeconomic differences in injury risks: A review
of findings and a discussion of potential countermeasures. Denmark: World Health Organization.
Lalor, K. & McElvaney, R. (2010). Child sexual abuse, links to later sexual exploitation/high-risk sexual
behavior, and prevention/treatment programs. Trauma, Violence, & Abuse, 11, 159–177.
Landau, J. (2010). Communities that care for families: The LINC Model for enhancing individual, family,
and community resilience. American Journal of Orthopsychiatry, 80, 516–524.
Landau, J., Mittal, M., & Wieling, E. (2008). Linking human systems: Strengthening individuals, families,
and communities in the wake of mass trauma. Journal of Marital and Family Therapy, 34, 193–209.
Landre, L., Destrieux, C., Baudry, M., Barantin, L., Cottier, J. P., Martineau, J. et al. (2010). Preserved
subcortical volumes and cortical thickness in women with sexual abuse-related PTSD. Psychiatry
Research, 183, 181–186.
Lang, A. J., Strauss, J. L., Bomyea, J., Bormann, J. E., Hickman, S. D., Good, R. C. et al. (2012). The
theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification,
36(6), 759–786 .
3-64 Part 3, Section 3—General Bibliography
Lang, J. M., Ford, J. D., & Fitzgerald, M. M. (2010). An algorithm for determining use of trauma-focused
cognitive–behavioral therapy. Psychotherapy (Chicago.), 47, 554–569.
Lasiuk, G. C. & Hegadoren, K. M. (2006a). Posttraumatic stress disorder part I: Historical development of
the concept. Perspectives in Psychiatric Care, 42, 13–20.
Lasiuk, G. C. & Hegadoren, K. M. (2006b). Posttraumatic stress disorder part II: Development of the
construct within the North American psychiatric taxonomy. Perspectives in Psychiatric Care, 42, 72–
81.
Lau, E. X. & Rapee, R. M. (2011). Prevention of anxiety disorders. Current Psychiatry Reports, 13, 258–
266.
Laugharne, J., Lillee, A., & Janca, A. (2010). Role of psychological trauma in the cause and treatment of
anxiety and depressive disorders. Current Opinion in Psychiatry, 23, 25–29.
Lavretsky, H., Siddarth, P., & Irwin, M. R. (2010). Improving depression and enhancing resilience in
family dementia caregivers: A pilot randomized placebo-controlled trial of escitalopram. The
American Journal of Geriatric Psychiatry, 18, 154–162.
Lawyer, S. R., Resnick, H. S., Galea, S., Ahern, J., Kilpatrick, D. G., & Vlahov, D. (2006). Predictors of
peritraumatic reactions and PTSD following the September 11th terrorist attacks. Psychiatry, 69,
130–141.
Layne, C. M., Warren, J. S., Saltzman, W. R., Fulton, J. B., Steinberg, A. M., & Pynoos, R. S. (2006).
Contextual influences on posttraumatic adjustment: Retraumatization and the roles of revictimization,
posttraumatic adversities, and distressing reminders. In L. A. Schein, H. I. Spitz, G. M. Burlingame,
& P. R. Muskin (Eds.), Psychological effects of catastrophic disasters: Group approaches to
treatment (pp. 235–286). New York: Haworth Press.
Layne, C. M., Warren, J. S., Watson, P. J., & Shalev, A. Y. (2007). Risk, vulnerability, resistance, and
resilience: Toward an integrative conceptualization of posttraumatic adaptation. In M. J. Friedman, T.
M. Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 497–520). New
York, NY: Guilford Press.
Lee, B. A. & Schreck, C. J. (2005). Danger on the streets: Marginality and victimization among homeless
people. American Behavioral Scientist, 48, 1055–1081.
Lee, C. S., Chang, J. C., Liu, C. Y., Chang, C. J., Chen, T. H. H., Chen, C. H. et al. (2009). Acculturation,
psychiatric comorbidity and posttraumatic stress disorder in a Taiwanese aboriginal population.
Social Psychiatry and Psychiatric Epidemiology, 44, 55–62.
Lee, E. & Mock, M. R. (2005a). Asian families: An overview. In M. McGoldrick, J. Giordano, & N.
Garcia-Preto (Eds.), Ethnicity and family therapy (3rd ed.) (pp. 269–289). New York: Guilford Press.
Lee, E. & Mock, M. R. (2005b). Chinese families. In M. McGoldrick, J. Giordano, & N. Garcia-Preto
(Eds.), Ethnicity and family therapy (3rd ed.) (pp. 302–318). New York: Guilford Press.
Lee, T. T., Westrup, D. A., Ruzek, J. I., Keller, J., & Weitlauf, J. C. (2007). Impact of clinician gender on
examination anxiety among female veterans with sexual trauma: A pilot study. Journal of Women’s
Health, 16, 1291–1299.
Trauma-Informed Care in Behavioral Health Services 3-65
Lehmann, P. & Elliston, E. J. (2001). Traumatic responding in children exposed to domestic violence: A
cross-cultural study. Journal of Ethnic & Cultural Diversity in Social Work: Innovation in Theory,
Research & Practice, 10, 81–102.
Lensvelt-Mulders, G., van der Hart, O., van Ochten, J. M., van Son, M. J. M., Steele, K., & Breeman, L.
(2008). Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis.
Clinical Psychology Review, 28, 1138–1151.
Lent, J. (2010). Stressors and stress management of counselors: Findings from interviews of professional
counselors. Retrieved July 4, 2013, from:
http://counselingoutfitters.com/vistas/vistas10/Article_73.pdf
Leserman, J., Whetten, K., Lowe, K., Stangl, D., Swartz, M. S., & Thielman, N. M. (2005). How trauma,
recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected
patients in the south. Psychosomatic Medicine, 67, 500–507.
Lesser, L. (2003). Review of trauma: A genealogy. Journal of the American Academy of Psychoanalysis,
31, 735–738.
Lester, K. M., Milby, J. B., Schumacher, J. E., Vuchinich, R., Person, S., & Clay, O. J. (2007). Impact of
behavioral contingency management intervention on coping behaviors and PTSD symptom reduction
in cocaine-addicted homeless. Journal of Traumatic Stress, 20, 565–575.
Lester, K., Resick, P. A., Young-Xu, Y., & Artz, C. (2010). Impact of race on early treatment termination
and outcomes in posttraumatic stress disorder treatment. Journal of Consulting and Clinical
Psychology, 78, 480–489.
Leverich, G. S. & Post, R. M. (2006). Course of bipolar illness after history of childhood trauma. Lancet,
367, 1040–1042.
Levitt, J. T., Malta, L. S., Martin, A., Davis, L., & Cloitre, M. (2007). The flexible application of a
manualized treatment for PTSD symptoms and functional impairment related to the 9/11 World Trade
Center attack. Behaviour Research and Therapy, 45, 1419–1433.
Lewis, K. L. & Grenyer, B. F. (2009). Borderline personality or complex posttraumatic stress disorder? An
update on the controversy. Harvard Review of Psychiatry, 17, 322–328.
Lewis-Fernandez, R., Martinez-Taboas, A., Sar, V., Patel, S., & Boatin, A. (2007). The cross-cultural
assessment of dissociation. In J. P. Wilson & C. S. Tang (Eds.), Cross-cultural assessment of
psychological trauma and PTSD (pp. 279–317). New York: Springer Publishing Science + Business
Media.
Libby, A. M., Orton, H. D., Beals, J., Buchwald, D., & Manson, S. M. (2008). Childhood abuse and later
parenting outcomes in two American Indian tribes. Child Abuse & Neglect, 32, 195–211.
Lilly, M. M. & Graham-Bermann, S. A. (2009). Ethnicity and risk for symptoms of posttraumatic stress
following intimate partner violence. Journal of Interpersonal Violence, 24, 3–19.
Linehan, M. M. (1993). Dialectical behavior therapy for treatment of borderline personality disorder:
Implications for the treatment of substance abuse. In L. S. Onken, J. D. Blaine, & J. J. Boren (Eds.),
Behavioral Treatments for Drug Abuse and Dependence (pp. 201–216). Rockville, MD: National
Institute on Drug Abuse.
3-66 Part 3, Section 3—General Bibliography
Linley, P. A., Joseph, S., & Loumidis, K. (2005). Trauma work, sense of coherence, and positive and
negative changes in therapists. Psychotherapy and Psychosomatics, 74, 185–188.
Litz, B. T. & Gray, M. J. (2002). Early Intervention for mass violence: What is the evidence? What should
be done? Cognitive and Behavioral Practice, 9, 266–272.
Litz, B. T. (2008). Early intervention for trauma: Where are we and where do we need to go? A
commentary. Journal of Traumatic Stress, 21, 503–506.
Litz, B. T., Miller, M., Ruef, A., & McTeague, L. (2002). Exposure to trauma in adults. In M. Antony &
D. Barlow (Eds.), Handbook of assessment and treatment planning for psychological disorders. New
York: Guilford Press.
Liu, D., Diorio, J., Day, J. C., Francis, D. D., & Meaney, M. J. (2000). Maternal care, hippocampal
synaptogenesis and cognitive development in rats. Nature Neuroscience, 3, 799–806.
Lockwood, A., Steinke, D. T., & Botts, S. R. (2009). Medication adherence and its effect on relapse among
patients discharged from a Veterans Affairs posttraumatic stress disorder treatment program. Ann
Pharmacother., 43, 1227–1232.
Lommen, M. J. & Restifo, K. (2009). Trauma and posttraumatic stress disorder (PTSD) in patients with
schizophrenia or schizoaffective disorder. Community Mental Health Journal, 45, 485–496.
Long, M. E., Grubaugh, A. L., Elhai, J. D., Cusack, K. J., Knapp, R., & Frueh, B. C. (2010). Therapist
fidelity with an exposure-based treatment of PTSD in adults with schizophrenia of schizoaffective
disorder. Journal of Clinical Psychology, 66, 383–393.
Lovell, K. (2011). What else do we need to know about evidence-based psychological interventions for
PTSD. In D. J. Stein, M. J. Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 208–
210). Chichester, UK: John Wiley and Sons, Inc.
Lu, W., Mueser, K. T., Rosenberg, S. D., & Jankowski, M. K. (2008). Correlates of adverse childhood
experiences among adults with severe mood disorders. Psychiatric Services, 59, 1018–1026.
Luce, H., Schrager, S., & Gilchrist, V. (2010). Sexual assault of women. American Family Physician, 81,
489–495.
Lueger–Schuster, B. (2010). Supporting interventions after exposure to torture. Torture., 20, 32–44.
Lunasco, T. K., Goodwin, E. A., Ozanian, A. J., & Loflin, E. M. (2010). One Shot–One Kill: A culturally
sensitive program for the warrior culture. Mil.Med, 175, 509–513.
Lutz, G. M., Kramer, R. E., Gonnerman, M. E., Lantz, G. L., & Downs, W. R. (1995). Substance abuse
and the Iowa flood disaster of 1993: Final report. Cedar Falls, IA: University of Northern Iowa.
Lynch, M. & Cicchetti, D. (1998). An ecological–transactional analysis of children and contexts: The
longitudinal interplay among child maltreatment, community violence, and children’s
symptomatology. Development and Psychopathology, 10, 235–257.
Lynch, S. M. (2011). Restoring relationships: Group interventions for survivors of sexual traumas. In
Surviving sexual violence: A guide to recovery and empowerment (pp. 179–198). Lanham, MD:
Rowman & Littlefield.
Trauma-Informed Care in Behavioral Health Services 3-67
MacDermott, D. (2010). Psychological hardiness and meaning making as protection against sequelae in
veterans of the wars in Iraq and Afghanistan. International Journal of Emergency Mental Health, 12,
199–206.
Macklin, M. L., Metzger, L. J., Litz, B. T., McNally, R. J., Lasko, N. B., Orr, S. P. et al. (1998). Lower
precombat intelligence is a risk factor for posttraumatic stress disorder. Journal of Consulting and
Clinical Psychology, 66, 323–326.
Mackowiak, P. A. & Batten, S. V. (2008). Post-traumatic stress reactions before the advent of post-
traumatic stress disorder: Potential effects on the lives and legacies of Alexander the Great, Captain
James Cook, Emily Dickinson, and Florence Nightingale. Military Medicine, 173, 1158–1163.
MacMillan, H. L., Wathen, C. N., Jamieson, E., Boyle, M. H., Shannon, H. S., Ford-Gilboe, M. et al.
(2009). Screening for intimate partner violence in health care settings: A randomized trial. JAMA,
302, 493–501.
Macy, R. D., Behar, L., Paulson, R., Delman, J., Schmid, L., & Smith, S. F. (2004). Community-based,
acute posttraumatic stress management: A description and evaluation of a psychosocial–intervention
continuum. Harvard Review of Psychiatry, 12, 217–228.
Macy, R. J., Giattina, M., Sangster, T. H., Crosby, C., & Montijo, N. J. (2009). Domestic violence and
sexual assault services: Inside the black box. Aggression and Violent Behavior, 14, 359–373.
Madrid, P. A., Grant, R., Reilly, M. J., & Redlener, N. B. (2006). Challenges in meeting immediate
emotional needs: Short-term impact of a major disaster on children’s mental health: Building
resiliency in the aftermath of Hurricane Katrina. Pediatrics, 117, S448–S453.
Madsen, L. H., Blitz, L. V., McCorkle, D., & Panzer, P. G. (2003). Sanctuary in a domestic violence
shelter: A team approach to healing. Psychiatric Quarterly, 74, 155–171.
Maercker, A., Zöllner, T., Menning, H., Rabe, S., & Karl, A. (2006). Dresden PTSD treatment study:
Randomized controlled trial of motor vehicle accident survivors. BMC. Psychiatry, 6, 29.
Maes, M., delmeire, L., Mylle, J., & Atamura, C. (2001). Risk and preventive factors of post-traumatic
stress disorder (PTSD): Alcohol consumption and intoxication prior to a traumatic event diminishes
the relative risk to develop PTSD in response to that trauma. Journal of Affective Disorders, 63, 113–
121.
Maguen, S., Lucenko, B. A., Reger, M. A., Gahm, G. A., Litz, B. T., Seal, K. H. et al. (2010). The impact
of reported direct and indirect killing on mental health symptoms in Iraq War veterans. Journal of
Traumatic Stress, 23, 86–90.
Maguen, S., Luxton, D. D., Skopp, N. A., & Madden, E. (2011). Gender differences in traumatic
experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. Journal
of Psychiatric Research, 46(3), 311–316.
Maguen, S., Luxton, D. D., Skopp, N. A., Gahm, G. A., Reger, M. A., Metzler, T. J. et al. (2011). Killing
in combat, mental health symptoms, and suicidal ideation in Iraq war veterans. Journal of Anxiety
Disorders, 25(4), 563–567.
Maguen, S., Ren, L., Bosch, J. O., Marmar, C. R., & Seal, K. H. (2010). Gender differences in mental
health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care.
American Journal of Public Health, 100, 2450–2456.
3-68 Part 3, Section 3—General Bibliography
Maguen, S., Suvak, M., & Litz, B. T. (2006). Predictors and prevalence of posttraumatic stress disorder
among military veterans. In A. B. Adler, C. A. Castro, & T. W. Britt (Eds.), Military life: The
psychology of serving in peace and combat (Vol. 2): Operational stress (pp. 141–169). Westport, CT:
Praeger Security International.
Maguire, C., McCusker, C. G., Meenagh, C., Mulholland, C., & Shannon, C. (2008). Effects of trauma on
bipolar disorder: The mediational role of interpersonal difficulties and alcohol dependence. Bipolar.
Disorder, 10, 293–302.
Mahalik, J. R. (2001). Cognitive therapy for men. In G. R. Brooks & G. E. Good (Eds.), The new
handbook of psychotherapy and counseling with men: A comprehensive guide to settings, problems,
and treatment approaches (pp. 544–564). San Francisco, CA: Jossey-Bass.
Maker, A. H., Kemmelmeier, M., & Peterson, C. (2001). Child sexual abuse, peer sexual abuse, and sexual
assault in adulthood: A multi-risk model of revictimization. Journal of Traumatic Stress, 14, 351–
368.
Makin-Byrd, K., Gifford, E., McCutcheon, S., & Glynn, S. (2011). Family and couples treatment for
newly returning veterans. Professional Psychology: Research and Practice, 42, 47–55.
Malik, M. L., Connor, K. M., Sutherland, S. M., Smith, R. D., Davison, R. M., & Davidson, J. R. (1999).
Quality of life and posttraumatic stress disorder: A pilot study assessing changes in SF–36 scores
before and after treatment in a placebo-controlled trial of fluoxetine. Journal of Traumatic Stress, 12,
387–393.
Malta, L. S., Levitt, J. T., Martin, A., Davis, L., & Cloitre, M. (2009). Correlates of functional impairment
in treatment–seeking survivors of mass terrorism. Behavior Therapy, 40, 39–49.
Mancino, M. J., Pyne, J. M., Tripathi, S., Constans, J., Roca, V., & Freeman, T. (2006). Quality-adjusted
health status in veterans with posttraumatic stress disorder. Journal of Nervous and Mental Disease,
194, 877–879.
Maniglio, R. (2009). Severe mental illness and criminal victimization: A systematic review. Acta
Psychiatrica Scandinavica, 119, 180–191.
Manson, S. M., Beals, J., Klein, S. A., & Croy, C. D. (2005). Social epidemiology of trauma among 2
American Indian reservation populations. American Journal of Public Health, 95, 851–859.
Marchand, A., Guay, S., Boyer, R., Lucci, S., Martin, A., & St-Hilaire, M. H. (2006). A randomized
controlled trial of an adapted form of individual critical incident stress debriefing for victims of an
armed robbery. Brief Treatment and Crisis Intervention, 6, 122–129.
Marcus, S. & Dubi, M. (2006). The relationship between resilience and compassion fatigue in counselors.
In G. R. Walz, J. C. Bleuer, & R. K. Yep (Eds.), Vistas: Compelling perspectives on counseling 2006
(pp. 223–225). Alexandria, VA: American Counseling Association.
Markowitz, J. C. (2010). IPT and PTSD. Depression and Anxiety, 27, 879–881.
Marques, L., Robinaugh, D. J., LeBlanc, N. J., & Hinton, D. (2011). Cross-cultural variations in the
prevalence and presentation of anxiety disorders. Expert Review of Neurotherapeutics, 11, 313–322.
Marsella, A. J. & Christopher, M. A. (2004). Ethnocultural considerations in disasters: An overview of
research, issues, and directions. Psychiatric Clinics of North America, 27, 521–539.
Trauma-Informed Care in Behavioral Health Services 3-69
Marsella, A. J. (2010). Ethnocultural aspects of PTSD: An overview of concepts, issues, and treatments.
Traumatology, 16, 17–26.
Marsella, A. J., Johnson, J. L., Watson, P., & Gryczynski, J. (2008). Essential concepts and foundations. In
A. J. Marsella, J. L. Johnson, P. Watson, & J. Gryczynski (Eds.), Ethnocultural perspectives on
disaster and trauma: Foundations, issues, and applications (pp. 3–13). New York: Springer
Publishing Science + Business Media.
Marshall, G. N., Schell, T. L., & Miles, J. N. V. (2009). Ethnic differences in posttraumatic distress:
Hispanics symptoms differ in kind and degree. Journal of Consulting and Clinical Psychology, 77,
1169–1178.
Marshall, G. N., Schell, T. L., Elliott, M. N., Berthold, S. M., & Chun, C. A. (2005). Mental health of
Cambodian refugees 2 decades after resettlement in the United States. JAMA, 294, 571–579.
Marshall-Berenz, E. C., Vujanovic, A. A., & Zvolensky, M. J. (2011). Main and interactive effects of a
nonclinical panic attack history and distress tolerance in relation to PTSD symptom severity. Journal
of Anxiety Disorders, 25, 185–191.
Martin, M., Marchand, A., Boyer, R., & Martin, N. (2009). Predictors of the development of posttraumatic
stress disorder among police officers. Journal of Trauma & Dissociation, 10, 451–468.
Martin, S. L., Ray, N., Sotres-Alvarez, D., Kupper, L. L., Moracco, K. E., Dickens, P. A. et al. (2006).
Physical and sexual assault of women with disabilities. Violence Against Women, 12, 823–837.
Martino, S., Canning-Ball, M., Carroll, K. M., & Rounsaville, B. J. (2011). A criterion-based stepwise
approach for training counselors in motivational interviewing. Journal of Substance Abuse Treatment,
40, 357–365.
Martorell, A. & Tsakanikos, E. (2008). Traumatic experiences and life events in people with intellectual
disability. Current Opinion in Psychiatry, 21, 445–448.
Martorell, A., Tsakanikos, E., Pereda, A., Gutierrez-Recacha, P., Bouras, N., & Ayuso-Mateos, J. L.
(2009). Mental health in adults with mild and moderate intellectual disabilities: The role of recent life
events and traumatic experiences across the life span. Journal of Nervous and Mental Disease, 197,
182–186.
Martsolf, D. S., Draucker, C. B., Cook, C. B., Ross, R., Stidham, A. W., & Mweemba, P. (2010). A meta-
summary of qualitative findings about professional services for survivors of sexual violence.
Qual.Rep., 15, 489–506.
Maschi, T. & Brown, D. (2010). Professional self-care and prevention of secondary trauma. In Helping
bereaved children: A handbook for practitioners (3rd ed.) (pp. 345–373). New York: Guilford Press.
Maschi, T., Dennis, K. S., Gibson, S., MacMillan, T., Sternberg, S., & Hom, M. (2011). Trauma and stress
among older adults in the criminal justice system: A review of the literature with implications for
social work. Journal of Gerontological Social Work, 54, 390–424.
Masho, S. W. & Ahmed, G. (2007). Age at sexual assault and posttraumatic stress disorder among women:
Prevalence, correlates, and implications for prevention. Journal of Women’s Health, 16, 262–271.
Mathieu, A., Mazza, S., Petit, D., Decary, A., Massicotte-Marquez, J., Malo, J. et al. (2007). Does age
worsen EEG slowing and attention deficits in obstructive sleep apnea syndrome? Clinical
Neurophysiology, 118, 1538–1544.
3-70 Part 3, Section 3—General Bibliography
Maxfield, L. (2009). Looking back, moving forward. Journal of EMDR Practice and Research, 3, 210.
McCabe, O. L., Lating, J. M., Everly, G. S., Jr., Mosley, A. M., Teague, P. J., Links, J. M. et al. (2007).
Psychological first aid training for the faith community: A model curriculum. International Journal of
Emergency Mental Health, 9, 181–192.
McCabe, O. L., Mosley, A. M., Gwon, H. S., Everly, G. S., Jr., Lating, J. M., Links, J. M. et al. (2007).
The tower of ivory meets the house of worship: Psychological first aid training for the faith
community. International Journal of Emergency Mental Health, 9, 171–180.
McCaig, L. F. & Burt, C. W. (2005). National Hospital Ambulatory Medical Care Survey: 2003
emergency department summary (Rep. No. No. 358). Hyattsville, MD: National Center for Health
Statistics.
McCarthy, E. & Petrakis, I. (2010). Epidemiology and management of alcohol dependence in individuals
with post-traumatic stress disorder. CNS Drugs, 24, 997–1007.
McCutcheon, V. V., Heath, A. C., Nelson, E. C., Bucholz, K. K., Madden, P. A., & Martin, N. G. (2010).
Clustering of trauma and associations with single and co-occurring depression and panic attack over
twenty years. Twin Research and Human Genetics, 13, 57–65.
McDonagh, A., Friedman, M., McHugo, G., Ford, J., Sengupta, A., Mueser, K. et al. (2005). Randomized
trial of cognitive–behavioral therapy for chronic posttraumatic stress disorder in adult female
survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology, 73, 515–524.
McFall, M., Atkins, D. C., Yoshimoto, D., Thompson, C. E., Kanter, E., Malte, C. A. et al. (2006).
Integrating tobacco cessation treatment into mental health care for patients with posttraumatic stress
disorder. Am.J.Addict, 15, 336–344.
McFarlane, A. C. (2010). Phenomenology of posttraumatic stress disorder. In D.J.Stein, E. Hollander, &
B. O. Rothbaum (Eds.), Textbook of anxiety disorders (2nd ed.) (pp. 547–565). Arlington, VA:
American Psychiatric Publishing, Inc.
McFarlane, A. C. (2011). Redefining PTSD in DSM-V: Conundrums and potentially unintended risks. In
D. J. Stein, M. J. Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 42–47).
Chichester, UK: John Wiley and Sons, Inc.
McGarrigle, T. & Walsh, C. A. (2011). Mindfulness, self-care, and wellness in social work: Effects of
contemplative training. Journal of Religion & Spirituality in Social Work: Social Thought, 30, 212–
233.
McGovern, M. P., Lambert-Harris, C., Acquilano, S., Xie, H., Alterman, A. I., & Weiss, R. D. (2009). A
cognitive behavioral therapy for co-occurring substance use and posttraumatic stress disorders.
Addictive Behaviors, 34, 892–897.
McGovern, M. P., Lambert-Harris, C., Alterman, A. I., Xie, H., & Meier, A. (2011). A randomized
controlled trial comparing integrated cognitive behavioral therapy versus individual addiction
counseling for co-occurring substance use and posttraumatic stress disorders. Journal of Dual
Diagnosis, 7, 207–227.
McHugh, P. R. & Treisman, G. (2007). PTSD: A problematic diagnostic category. Journal of Anxiety
Disorders, 21, 211–222.
Trauma-Informed Care in Behavioral Health Services 3-71
McHugo, G. J., Caspi, Y., Kammerer, N., Mazelis, R., Jackson, E. W., Russell, L. et al. (2005). The
assessment of trauma history in women with co-occurring substance abuse and mental disorders and a
history of interpersonal violence. The Journal of Behavioral Health Services & Research, 32, 113–
127.
McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C.
(2010a). Childhood adversities and adult psychopathology in the National Comorbidity Survey
Replication (NCS–R) III: Associations with functional impairment related to DSM-IV disorders.
Psychological Medicine, 40, 847–859.
McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C.
(2010b). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey
Replication II: Associations with persistence of DSM-IV disorders. Archives of General Psychiatry,
67, 124–132.
McLay, R. N., Klam, W. P., & Volkert, S. L. (2010). Insomnia is the most commonly reported symptom
and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from
military deployments. Military Medicine, 175, 759–762.
McLean, C. P. & Anderson, E. R. (2009). Brave men and timid women? A review of the gender
differences in fear and anxiety. Clinical Psychology Review, 29, 496–505.
McLean, C. P. & Foa, E. B. (2011). Prolonged exposure therapy for post-traumatic stress disorder: A
review of evidence and dissemination. Expert Review of Neurotherapeutics, 11, 1151–1163.
McLean, C. P., Asnaani, A., Litz, B. T., & Hofmann, S. G. (2011). Gender differences in anxiety
disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric
Research, 45, 1027–1035.
McLean, C. P., Steenkamp, M. M., Levy, H. C., & Litz, B. T. (2010). Posttraumatic stress disorder. In M.
A. Cucciare & K. R. Weingardt (Eds.), Using technology to support evidence-based behavioral
health practices: A clinician’s guide (pp. 45–68). New York: Routledge/Taylor & Francis Group.
McLeod, D. S., Koenen, K. C., Meyer, J. M., Lyons, M. J., Eisen, S., True, W. et al. (2001). Genetic and
environmental influences on the relationship among combat exposure, posttraumatic stress disorder
symptoms, and alcohol use. Journal of Traumatic Stress, 14, 259–275.
McLeod, J. (1997). Narrative and psychotherapy. London: Sage Publications.
McNally, R. J. (2003). Remembering trauma. Cambridge, MA: Belknap Press of Harvard University
Press.
McNally, R. J. (2005). Debunking myths about trauma and memory. The Canadian Journal of Psychiatry/
La Revue Canadienne de Psychiatrie, 50, 817–822.
McNally, R. J., Bryant, R. A., & Ehlers, A. (2003). Does early psychological intervention promote
recovery from posttraumatic stress? Psychological Science in the Public Interest, 4, 45–79.
McNamara, C., Schumacher, J. E., Milby, J. B., Wallace, D., & Usdan, S. (2001). Prevalence of
nonpsychotic mental disorders does not affect treatment outcome in a homeless cocaine-dependent
sample. American Journal of Drug and Alcohol Abuse, 27, 91–106.
McWilliams, L. A., Cox, B. J., & Enns, M. W. (2003). Mood and anxiety disorders associated with chronic
pain: An examination in a nationally representative sample. Pain, 106, 127–133.
3-72 Part 3, Section 3—General Bibliography
Mead, S. & MacNeil, C. (2006). Peer support: What makes it unique? International Journal of
Psychosocial Rehabilitation, 10, 29–38.
Mead, S. (2008). Intentional peer support: An alternative approach. Plainfield, NH: Shery Mead
Consulting.
Meaney, M. J., Brake, W., & Gratton, A. (2002). Environmental regulation of the development of
mesolimbic dopamine systems: A neurobiological mechanism for vulnerability to drug abuse?
Psychoneuroendocrinology, 27, 127–138.
Meichenbaum, D. (1994). A clinical handbook/practical therapist manual for assessing and treating adults
with post-traumatic stress disorder (PTSD). Waterloo, Ontario: Institute Press.
Meichenbaum, D. (1996). Stress inoculation training for coping with stressors. The Clinical Psychologist,
49, 4–7.
Meichenbaum, D. (2007). Stress inoculation training: A preventative and treatment approach. In Principles
and practice of stress management (3rd ed.) (pp. 497–516). New York: Guilford Press.
Meichenbaum, D. H. & Deffenbacher, J. L. (1988). Stress inoculation training. Counseling Psychologist,
16, 69–90.
Meis, L. A., Barry, R. A., Kehle, S. M., Erbes, C. R., & Polusny, M. A. (2010). Relationship adjustment,
PTSD symptoms, and treatment utilization among coupled National Guard soldiers deployed to Iraq.
Journal of Family Psychology, 24, 560–567.
Mello, M. F. (2011). Critical view of the pharmacological treatment of trauma. In D. J. Stein, M. J.
Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 163). Chichester, UK: John Wiley
and Sons, Inc.
Melnick, S. M. & Bassuk, E. L. (2000). Identifying and responding to violence among poor and homeless
women. Nashville, TN: National Health Care for the Homeless Council.
Meltzer-Brody, S., Churchill, E., & Davidson, J. R. T. (1999). Derivation of the SPAN, a brief diagnostic
screening test for post-traumatic stress disorder. Psychiatry Research, 88, 63–70.
Mendenhall, T. J. & Berge, J. M. (2010). Family therapists in trauma-response teams: Bringing systems
thinking into interdisciplinary fieldwork. Journal of Family Therapy, 32, 43–57.
Mendenhall, T. J. (2006). Trauma-response teams: Inherent challenges and practical strategies in
interdisciplinary fieldwork. Families, Systems, & Health, 24, 357–362.
Mendes, D. D., Mello, M. F., Ventura, P., Passarela, C. M., & Mari, J. J. (2008). A systematic review on
the effectiveness of cognitive behavioral therapy for posttraumatic stress disorder. International
Journal of Psychiatry in Medicine, 38, 241–259.
Mental Health America, Centers for Technical Assistance (2012). Trauma Recovery and Empowerment
Model (TREM). Alexandria, VA: Mental Health America, Centers for Technical Assistance.
Merikangas, K. R., Akiskal, H. S., Angst, J., Greenberg, P. E., Hirschfeld, R. M., Petukhova, M. et al.
(2007). Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity
Survey replication. Archives of General Psychiatry, 64, 543–552.
Mevissen, L. & de Jongh, A. (2010). PTSD and its treatment in people with intellectual disabilities: A
review of the literature. Clinical Psychology Review, 30, 308–316.
Trauma-Informed Care in Behavioral Health Services 3-73
Meyer, R. E. (1986). Psychobiology and the treatment of drug dependence: The biobehavioral interface.
American Journal of Drug and Alcohol Abuse, 12, 223–233.
Meyerbröker, K. & Emmelkamp, P. M. (2010). Virtual reality exposure therapy in anxiety disorders: A
systematic review of process-and-outcome studies. Depression and Anxiety, 27, 933–944.
Miller, D. & Guidry, L. (2001). Addictions and trauma recovery: Healing the body, mind, and spirit. New
York: W.W. Norton.
Miller, G. H. (2009). The trauma of insidious racism. Journal of the Academy of Psychiatry and the Law,
37, 41–44.
Miller, K. E., Weine, S. M., Ramic, A., Brkic, N., Bjedic, Z. D., Smajkic, A. et al. (2002). The relative
contribution of war experiences and exile-related stressors to levels of psychological distress among
Bosnian refugees. Journal of Traumatic Stress, 15, 377–387.
Miller, N. A. & Najavits, L. M. (2012). Creating trauma-informed correctional care: A balance of goals
and environment. European Journal of Psychotraumatology; Vol 3 (2012) including Supplements.
Miller, W. R. & Rollnick, S. (2002). Motivational interviewing: Preparing people for change. (2nd ed.)
New York: Guilford Press.
Mills, K. L., Teesson, M., Ross, J., & Peters, L. (2006). Trauma, PTSD, and substance use disorders:
findings from the Australian National Survey of Mental Health and Well–Being. American Journal of
Psychiatry, 163, 652–658.
Mitchell, J. T. & Everly, G. S. (2000). Critical incident stress management and critical incident stress
debriefings: Evolutions, effects and outcomes. In B. Raphael & J. Wilson (Eds.), Psychological
debriefing: Theory, practice and evidence. (pp. 71–90). Cambridge: Cambridge University Press.
Mitchell, J. T. & Everly, G. S. Jr. (2001). Critical Incident Stress Debriefing: An operations manual for
CISD, defusing and other group crisis intervention services. (3rd ed.) Ellicott City, MD: Chevron
Publishing Corporation.
Moak, Z. B. & Agrawal, A. (2010). The association between perceived interpersonal social support and
physical and mental health: Results from the National Epidemiological Survey on Alcohol and
Related Conditions. Journal of Public Health: Oxford Journals, 32, 191–201.
Mock, S. E. & Arai, S. M. (2010). Childhood trauma and chronic illness in adulthood: Mental health and
socioeconomic status as explanatory factors and buffers. Frontiers in Psychology, 1, 246.
Moffitt, T. E., Caspi, a., Taylor, A., Kokaua, J., Milne, B. J., Polanczyk, G. et al. (2010). How common are
common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus
retrospective ascertainment. Psychological Medicine: A Journal of Research in Psychiatry and the
Allied Sciences, 40, 899–909.
Mollica, R. F. (2009). Healing invisible wounds: Paths to hope and recovery in a violent world. Nashville,
TN: Vanderbilt University Press.
Mollica, R. F., McInnes, K., Poole, C., & Tor, S. (1998). Dose–effect relationships of trauma to symptoms
of depression and post-traumatic stress disorder among Cambodian survivors of mass violence.
British Journal of Psychiatry, 173, 482–488.
3-74 Part 3, Section 3—General Bibliography
Mollick, L. & Spett, M. (2002). Cloitre: Why exposure fails with most PTSD patients. Cranford, NJ: NJ
Association of Cognitive–Behavioral Therapistsl.
Monson, C. M., Fredman, S. J., & Dekel, R. (2010). Posttraumatic stress disorder in an interpersonal
context. In G. J. Beck (Ed.), Interpersonal processes in the anxiety disorders: Implications for
understanding psychopathology and treatment (pp. 179–208). Washington, DC: American
Psychological Association.
Monson, C. M., Rodriguez, B. F., & Warner, R. (2005). Cognitive–behavioral therapy for PTSD in the real
world: Do interpersonal relationships make a real difference? Journal of Clinical Psychology, 61,
751–761.
Monson, C. M., Schnurr, P. P., Resick, P. A., Friedman, M. J., Young-Xu, Y., & Stevens, S. P. (2006).
Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal
of Consulting and Clinical Psychology, 74, 898–907.
Monson, C. M., Stevens, S. P., & Schnurr, P. P. (2005). Cognitive–behavioral couple’s treatment for
posttraumatic stress disorder. In T. A. Corales (Ed.), Focus on posttraumatic stress disorder research
(pp. 245–274). Hauppauge, NY: Nova Science Publishers.
Monson, C. M., Taft, C. T., & Fredman, S. J. (2009). Military-related PTSD and intimate relationships:
From description to theory-driven research and intervention development. Clinical Psychology
Review, 29, 707–714.
Montoya, I. D., Covarrubias, L. D., Patek, J. A., & Graves, J. A. (2003). Posttraumatic stress disorder
among Hispanic and African-American drug users. The American Journal of Drug and Alcohol
Abuse, 29, 729–741.
Moore, B. A. & Kennedy, C. H. (2011). Wheels down: Adjusting to life after deployment. (1st ed.)
Washington, DC: American Psychological Association.
Morland, L. A., Greene, C. J., Grubbs, K., Kloezeman, K., Mackintosh, M. A., Rosen, C. et al. (2011).
Therapist adherence to manualized cognitive–behavioral therapy for anger management delivered to
veterans with PTSD via videoconferencing. Journal of Clinical Psychology, 67, 629–638.
Morrissey, J. P., Ellis, A. R., Gatz, M., Amaro, H., Reed, B. G., Savage, A. et al. (2005). Outcomes for
women with co-occurring disorders and trauma: Program and person-level effects. Journal of
Substance Abuse Treatment, 28, 121–133.
Morrissey, J. P., Jackson, E. W., Ellis, A. R., Amaro, H., Brown, V. B., & Najavits, L. M. (2005). Twelve-
month outcomes of trauma-informed interventions for women with co-occurring disorders.
Psychiatric Services, 56, 1213–1222.
Morsette, A., Swaney, G., Stolle, D., Schuldberg, D., van den Pol, R., & Young, M. (2009). Cognitive
behavioral intervention for trauma in schools (CBITS): School-based treatment on a rural American
Indian reservation. Journal of Behavior Therapy and Experimental Psychiatry, 40, 169–178.
Moses, D. J., Reed, B. G., Mazelis, R., & D’Ambrosio, B. (2003). Creating trauma services for women
with co-occurring disorders: Experiences from the SAMHSA Women with Alcohol, Drug Abuse and
Mental Health Disorders Who Have Histories of Violence Study. Rockville, MD: Substance Abuse
And Mental Health Services Administration.
Trauma-Informed Care in Behavioral Health Services 3-75
Mota, N. P., Medved, M., Wang, J., Asmundson, G. J., Whitney, D., & Sareen, J. (2012). Stress and
mental disorders in female military personnel: Comparisons between the sexes in a male dominated
profession. J. Psychiatr. Res, 46, 159–167.
Moul, D. E., Hall, M., Pilkonis, P. A., & Buysse, D. J. (2004). Self-report measures of insomnia in adults:
rationales, choices, and needs. Sleep Medicine Reviews, 8, 177–198.
Mouton, C. P., Rodabough, R. J., Rovi, S. L., Hunt, J. L., Talamantes, M. A., Brzyski, R. G. et al. (2004).
Prevalence and 3-year incidence of abuse among postmenopausal women. American Journal of
Public Health, 94, 605–612.
Mueser, K. T., Bolton, E., Carty, P. C., Bradley, M. J., Ahlgren, K. F., Distaso, D. R. et al. (2007). The
Trauma Recovery Group: A cognitive–behavioral program for post-traumatic stress disorder in
persons with severe mental illness. Community Mental Health Journal, 43, 281–304.
Mueser, K. T., Essock, S. M., Haines, M., Wolfe, R., & Xie, H. (2004). Posttraumatic stress disorder,
supported employment, and outcomes in people with severe mental illness. CNS Spectrums, 9, 913–
925.
Mueser, K. T., Rosenberg, S. D., Xie, H., Jankowski, M. K., Bolton, E. E., Lu, W. et al. (2008). A
randomized controlled trial of cognitive–behavioral treatment for posttraumatic stress disorder in
severe mental illness. Journal of Consulting & Clinical Psychology, 76, 259–271.
Mueser, K. T., Salyers, M. P., Rosenberg, S. D., Goodman, L. A., Essock, S. M., Osher, F. C. et al. (2004).
Interpersonal trauma and posttraumatic stress disorder in patients with severe mental illness:
Demographic, clinical, and health correlates. Schizophrenia Bulletin, 30, 45–57.
Myers, D. G. & Wee, D. F. (2002). Strategies for managing disaster mental health worker stress. In C. R.
Figley (Ed.), Treating compassion fatigue (pp. 181–211). New York: Brunner-Routledge.
Mylle, J. & Maes, M. (2004). Partial posttraumatic stress disorder revisited. Journal of Affective Disorders,
78, 37–48.
Nader, K. (2008). Review of when helping hurts: Preventing and treating compassion fatigue.
Traumatology, 14, 148.
Najavits, L. (2012). PTSD. Newton Centre, MA: Treatment Innovations.
Najavits, L. M. (2002a). Seeking safety: A treatment manual for PTSD and substance abuse. New York:
Guilford Press.
Najavits, L. M. (2002b). Seeking Safety: Psychotherapy for PTSD and substance abuse. Belmont, MA:
McLean Hospital.
Najavits, L. M. (2004). Assessment of trauma, PTSD, and substance use disorder: A practical guide. In J.
P. Wilson & T. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 466–491). New York:
Guilford.
Najavits, L. M. (2007a). Psychosocial treatments for posttraumatic stress disorder. In P. E. Nathan & E. M.
Gorman (Eds.), A guide to treatments that Work (3d ed., pp. 513–530). New York: Oxford Press.
Najavits, L. M. (2007b). Seeking safety: An evidence-based model for substance abuse and trauma/PTSD.
In Therapist’s guide to evidence-based relapse prevention (pp. 141–167). San Diego, CA: Elsevier
Academic Press.
3-76 Part 3, Section 3—General Bibliography
Najavits, L. M., Gastfriend, D. R., Barber, J. P., Reif, S., Muenz, L. R., Blaine, J. et al. (1998). Cocaine
dependence with and without PTSD among subjects in the National Institute on Drug Abuse
Collaborative Cocaine Treatment Study. American Journal of Psychiatry, 155, 214–219.
Najavits, L. M., Griffin, M. L., Luborsky, L., Frank, A., Weiss, R. D., Liese, B. S. et al. (1995).
Therapists’ emotional reactions to substance abusers: A new questionnaire and initial findings.
Psychotherapy: Theory, Research, Practice, Training, 32, 669–677.
Najavits, L. M., Harned, M. S., Gallop, R. J., Butler, S. F., Barber, J. P., Thase, M. E. et al. (2007). Six-
month treatment outcomes of cocaine-dependent patients with and without PTSD in a multisite
national trial. Journal of Studies on Alcohol and Drugs, 68, 353–361.
Najavits, L. M., Ryngala, D., Back, S. E., Bolton, E., Mueser, K. T., & Brady, K. T. (2009). Treatment of
PTSD and comorbid disorders. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.),
Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic
Stress Studies (2nd ed.) (pp. 508–535). New York: Guilford Press.
Najavits, L. M., Schmitz, M., Gotthardt, S., & Weiss, R. D. (2005). Seeking safety plus exposure therapy:
An outcome study on dual diagnosis men. Journal of Psychoactive Drugs, 37, 425–435.
Najavits, L. M., Sonn, J., Walsh, M., & Weiss, R. D. (2004). Domestic violence in women with PTSD and
substance abuse. Addictive Behaviors, 29, 707–715.
Najavits, L. M., Weiss, R. D., & Shaw, S. R. (1997). The link between substance abuse and posttraumatic
stress disorder in women: A research review. American Journal on Addictions, 6, 273–283.
Najavits, L. M., Weiss, R. D., Reif, S., Gastfriend, D. R., Siqueland, L., Barber, J. P. et al. (1998). The
Addiction Severity Index as a screen for trauma and posttraumatic stress disorder. Journal of Studies
on Alcohol, 59, 56–62.
Nandi, A., Galea, S., Tracy, M., Ahern, J., Resnick, H., Gershon, R. et al. (2004). Job loss, unemployment,
work stress, job satisfaction, and the persistence of posttraumatic stress disorder one year after the
September 11 attacks. Journal of Occupational and Environmental Medicine, 46, 1057–1064.
Nappi, C. M., Drummond, S. P., & Hall, J. M. (2012). Treating nightmares and insomnia in posttraumatic
stress disorder: A review of current evidence. Neuropharmacology, 62, 576–585.
Narrow, W. E., Rae, D. S., Robins, L. N., & Regier, D. A. (2002). Revised prevalence based estimates of
mental disorders in the United States: using a clinical signficance criterion to reconcile 2 surveys’
estimates. Archives of General Psychiatry, 59, 115–123.
National Association of State Mental Health Program Directors (2004). The damaging consequences of
violence and trauma: Facts, discussion points and recommendations for the behavioral health system.
Alexandria, VA: National Association of State Mental Health Program Directors.
National Association of State Mental Health Program Directors. (2005). Trauma informed care (TIC)
planning guidelines for use in developing an organizational action plan. [Draft.] Alexandria, VA:
National Association of State Mental Health Program Directors.
National Center for Post-Traumatic Stress Disorder (2002). Working with trauma survivors. White River
Junction, VT: National Center for Post-Traumatic Stress Disorder.
National Center for PTSD (2007a). Chart – Adult PTSD interviews. White River Junction, VT: National
Center for PTSD.
Trauma-Informed Care in Behavioral Health Services 3-77
National Center for PTSD (2007b). Chart – Adult PTSD self-report measures. White River Junction, VT:
National Center for PTSD.
National Center for PTSD (2007c). Chart – screens for PTSD. White River Junction, VT: National Center
for PTSD.
National Center for PTSD, U.S. Department of Veterans Affairs (2010). Understanding PTSD. White
River Junction, VT: National Center for PTSD.
National Center for Trauma-Informed Care, Center for Mental Health Services (2011). Psychological
trauma. Beau Bassin, Mauritius: Betascript Publishing.
National Child Traumatic Stress Network & National Center for PTSD (2012). Psychological first aid. Los
Angeles: National Center for Child Traumatic Stress.
National Child Traumatic Stress Network (2012). Neglect. Los Angeles: National Child Traumatic Stress
Network.
National Child Traumatic Stress Network, Child Sexual Abuse Task Force and Research & Practice Core.
(2004). How to implement trauma-focused cognitive behavioral therapy (TF–CBT) (Rep. No. Version
2). Durham, NC and Los Angeles: National Center for Child Traumatic Stress.
National Coalition for the Homeless (2002). Why are people homeless? Washington, DC: National
Coalition for the Homeless.
National Coalition for the Homeless (2004). Who is homeless? Washington, DC: National Coalition for the
Homeless.
National Collaborating Centre for Mental Health (2005). Post-traumatic stress disorder (PTSD): The
management of PTSD in adults and children in primary and secondary care. Leicester, UK: National
Collaborating Centre for Mental Health.
National Institute for Health and Clinical Excellence (2005). Post-traumatic stress disorder (PTSD)
(CG26) London: National Institute for Health and Clinical Excellence.
National Institute of Mental Health (2002). Mental health and mass violence: Evidence-based early
psychological intervention for victims/survivors of mass violence. A workshop to reach consensus on
best practices. Washington, DC: U. S. Government Printing Office.
Nebelkopf, E. & Wright, S. (2011). Holistic system of care: A ten-year perspective. Journal of
Psychoactive Drugs, 43, 302–308.
Nelson, E. C., Heath, A. C., Madden, P. A. F., Cooper, M. L., Dinwiddie, S. H., Bucholz, K. K. et al.
(2002). Association between self-reported childhood sexual abuse and adverse psychosocial
outcomes: results from a twin study. Archives of General Psychiatry, 59, 139–145.
Nelson, S. D. (2011). The posttraumatic growth path: An emerging model for prevention and treatment of
trauma-related behavioral health conditions. Journal of Psychotherapy Integration, 21, 1–42.
Nelson-Zlupko, L., Dore, M. M., Kauffman, E., & Kaltenbach, K. (1996). Women in recovery: Their
perceptions of treatment effectiveness. Journal of Substance Abuse Treatment, 13, 51–59.
Nemeroff, C. B., Bremner, J. D., Foa, E. B., Mayberg, H. S., North, C. S., & Stein, M. B. (2006).
Posttraumatic stress disorder: A state-of-the-science review. Journal of Psychiatric Research, 40, 1–
21.
3-78 Part 3, Section 3—General Bibliography
Neuner, F., Schauer, M., Klaschik, C., Karunakara, U., & Elbert, T. (2004). A comparison of narrative
exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress
disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology, 72, 579–
587.
New Logic Organizational Learning (2011). Creating a culture of care: A toolkit for creating a trauma-
informed environment. Austin, TX: New Logic Organizational Learning.
New South Wales Institute of Psychiatry & Centre for Mental Health (2000). Disaster mental health
response handbook: An educational resource for mental health professionals involved in disaster
management. Parramatta, New South Wales: New South Wales Institute of Psychiatry.
New, A. S., Fan, J., Murrough, J. W., Liu, X., Liebman, R. E., Guise, K. G. et al. (2009). A functional
magnetic resonance imaging study of deliberate emotion regulation in resilience and posttraumatic
stress disorder. Biological Psychiatry, 66, 656–664.
Newell, J. M. & MacNeil, G. A. (2010). Professional burnout, vicarious trauma, secondary traumatic
stress, and compassion fatigue: A review of theoretical terms, risk factors, and preventive methods for
clinicians and researchers. Best Practices in Mental Health: An International Journal, 6, 57–68.
Newman, J. M., Turnbull, A., Berman, B. A., Rodrigues, S., & Serper, M. R. (2010). Impact of traumatic
and violent victimization experiences in individuals with schizophrenia and schizoaffective disorder.
Journal of Nervous and Mental Disease, 198, 708–714.
Ng, A. T. & Kantor, E. M. (2010). Psychological first aid. In F. J. Stoddard, C. L. Katz, & J. P. Merlino
(Eds.), Hidden impact: What you need to know for the next disaster: A practical mental health guide
for clinicians (pp. 115–123). Sudbury, MA: Jones and Bartlett Publishers.
Ng, A. T. (2005). Cultural diversity in the integration of disaster mental health and public health: A case
study in response to bioterrorism. International Journal of Emergency Mental Health, 7, 23–31.
Nguyen, L. (2011). The ethics of trauma: Re-traumatization in society’s approach to the traumatized
subject. Int.J Group Psychother, 61, 26–47.
Nickerson, A., Bryant, R. A., Silove, D., & Steel, Z. (2011). A critical review of psychological treatments
of posttraumatic stress disorder in refugees. Clinical Psychology Review, 31, 399–417.
Nishith, P., Duntley, S. P., Domitrovich, P. P., Uhles, M. L., Cook, B. J., & Stein, P. K. (2003). Effect of
cognitive behavioral therapy on heart rate variability during REM sleep in female rape victims with
PTSD. Journal of Traumatic Stress, 16, 247–250.
Nishith, P., Mechanic, M. B., & Resick, P. A. (2000). Prior interpersonal trauma: The contribution to
current PTSD symptoms in female rape victims. Journal of Abnormal Psychology, 109, 20–5.
Nishith, P., Resick, P. A., & Griffin, M. G. (2002). Pattern of change in prolonged exposure and
cognitive–processing therapy for female rape victims with posttraumatic stress disorder. Journal of
Consulting and Clinical Psychology, 70, 880–886.
Nixon, R. D. V. & Nearmy, D. M. (2011). Treatment of comorbid posttraumatic stress disorder and major
depressive disorder: A pilot study. Journal of Traumatic Stress, 24, 451–455.
Noether, C. D., Finkelstein, N., VanDeMark, N. R., Savage, A., Reed, B. G., & Moses, D. J. (2005).
Design strengths and issues of SAMHSA’s Women, Co-occurring Disorders, and Violence Study.
Psychiatric Services, 56, 1233–1236.
Trauma-Informed Care in Behavioral Health Services 3-79
Noll, J. G., Horowitz, L. A., Bonanno, G. A., Trickett, P. K., & Putnam, F. W. (2003). Revictimization and
self-harm in women who experienced childhood sexual abuse: Results from a prospective study.
Journal of Interpersonal Violence, 18, 1452–1471.
Norman, S. B., Tate, S. R., Wilkins, K. C., Cummins, K., & Brown, S. A. (2010). Posttraumatic stress
disorder’s role in integrated substance dependence and depression treatment outcomes. Journal of
Substance Abuse Treatment, 38, 346–355.
Norris, F. H. & Slone, L. B. (2007). The epidemiology of trauma and PTSD. In M. J. Friedman, T. M.
Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 78–98). New York:
Guilford Press.
Norris, F. H., Friedman, M. J., & Watson, P. J. (2002). 60,000 disaster victims speak: Part II. Summary
and implications of the disaster mental health research. Psychiatry, 65, 240–260.
Norris, F. H., Friedman, M. J., Watson, P. J., Byrne, C. M., Diaz, E., & Kaniasty, K. (2002). 60,000
disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry,
65, 207–239.
Norris, F. H., Kaniasty, K. Z. C. M. L., & Inman, G. L. M. A. D. (2002). Placing age differences in
cultural context: A comparison of the effects of age on PTSD after disasters in the United States,
Mexico, and Poland. Journal of Clinical Geropsychology, 8, 153–173.
Norris, F. H., Murphy, A. D., Baker, C. K., & Perilla, J. L. (2003). Severity, timing, and duration of
reactions to trauma in the population: An example from Mexico. Biological Psychiatry, 53, 769–778.
Norris, F. H., Perilla, J. L., Ibanez, G. E., & Murphy, A. D. (2001). Sex differences in symptoms of
posttraumatic stress: Does culture play a role? Journal of Traumatic Stress, 14, 7–28.
North, C. S., Eyrich, K. M., Pollio, D. E., & Spitznagel, E. L. (2004). Are rates of psychiatric disorders in
the homeless population changing? American Journal of Public Health, 94, 103–108.
Norton, P. J. & Price, E. C. (2007). A meta-analytic review of adult cognitive–behavioral treatment
outcome across the anxiety disorders. Journal of Nervous and Mental Disease, 195, 521–531.
Nugent, N. R., Amstadter, A. B., & Koenen, K. C. (2008). Genetics of post-traumatic stress disorder:
informing clinical conceptualizations and promoting future research. Am. J. Med. Genet. C. Semin.
Med. Genet., 148C, 127–132.
Obasaju, M. A., Palin, F. L., Jacobs, C., Anderson, P., & Kaslow, N. J. (2009). Won’t you be my
neighbor?: Using an ecological approach to examine the impact of community on revictimization.
Journal of Interpersonal Violence, 24, 38–53.
O’Donnell, C. & Cook, J. M. (2006). Cognitive–behavioral therapies for psychological trauma and
comorbid substance use disorders. In B. Carruth (Ed.), Psychological trauma and addiction
treatment. New York: Haworth Press.
O’Donnell, M. L., Creamer, M., & Cooper, J. (2010). Criterion A: Controversies and clinical implications.
In G. M. Rosen (Ed.), Clinician’s guide to posttraumatic stress disorder (pp. 51–75). Hoboken, NJ:
John Wiley and Sons, Inc.
Office of Applied Studies (2002). Results from the 2001 National Household Survey on Drug Abuse:
Vol.1. Summary of national findings (Rep. No. HHS Publication No. (SMA) 02–3758). Rockville,
MD: Substance Abuse and Mental Health Services Administration.
3-80 Part 3, Section 3—General Bibliography
Office of the Surgeon Multi-National Corps–Iraq & Office of The Surgeon General United States Army
Medical Command (2006). Mental Health Advisory Team (MHAT) IV Operation Iraqi Freedom 05–
07. Final Report 17 November 2006. Washington, DC: U. S. Army Medical Department.
O’Hare, T. & Sherrer, M. (2011). Drinking motives as mediators between PTSD symptom severity and
alcohol consumption in persons with severe mental illnesses. Addictive Behaviors, 36, 465–469.
O’Hare, T. & Sherrer, M. V. (2009). Impact of the most frequently reported traumatic events on
community mental health clients. Journal of Human Behavior in the Social Environment, 19, 186–
195.
O’Hare, T., Shen, C., & Sherrer, M. (2010). High-risk behaviors and drinking-to-cope as mediators of
lifetime abuse and PTSD symptoms in clients with severe mental illness. Journal of Traumatic Stress,
23, 255–263.
O’Hare, T., Sherrer, M. V., & Shen, C. (2006). Subjective distress from stressful events and high-risk
behaviors as predictors of PTSD symptom severity in clients with severe mental illness. Journal of
Traumatic Stress;Journal of Traumatic Stress, 19, 375–386.
Ohayon, M. M. & Shapiro, C. M. (2000). Sleep disturbances and psychiatric disorders associated with
posttraumatic stress disorder in the general population. Comprehensive Psychiatry, 41, 469–478.
Ohio Legal Rights Service (2007). Trauma informed treatment in behavioral health settings. Columbus,
OH: Ohio Legal Rights Service.
Okuda, M., Olfson, M., Hasin, D., Grant, B. F., Lin, K. H., & Blanco, C. (2011). Mental health of victims
of intimate partner violence: Results from a national epidemiologic survey. Psychiatric Services, 62,
959–962.
Olatunji, B. O., Cisler, J. M., & Tolin, D. F. (2007). Quality of life in the anxiety disorders: A meta-
analytic review. Clinical Psychology Review, 27, 572–581.
Olatunji, B. O., Cisler, J. M., & Tolin, D. F. (2010). A meta-analysis of the influence of comorbidity on
treatment outcome in the anxiety disorders. Clinical Psychology Review.
Olff, M., Langeland, W., Draijer, N., & Gersons, B. P. R. (2007). Gender differences in posttraumatic
stress disorder. Psychological Bulletin, 133, 183–204.
Oman, D., Hedberg, J., & Thoresen, C. E. (2006). Passage meditation reduces perceived stress in health
professionals: A randomized, controlled trial. Journal of Consulting and Clinical Psychology, 74,
714–719.
Ompad, D. C., Ikeda, R. M., Shah, N., Fuller, C. M., Bailey, S., Morse, E. et al. (2005). Childhood sexual
abuse and age at initiation of injection drug Use. American Journal of Public Health, 95, 703–709.
Opler, L. A., Grennan, M. S., & Ford, J. D. (2009). Pharmacotherapy. In C. A. Courtois & J. D. Ford
(Eds.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 329–349). New
York: Guilford Press.
Orsillo, S. M. (2001). Measures for acute stress disorder and posttraumatic stress disorder. In M. M.
Antony, S. M. Orsillo, & L. Roemer (Eds.), Practitioner’s guide to empirically based measures of
anxiety (pp. 255–307). Dordrecht, Netherlands: Kluwer Academic Publishers.
Trauma-Informed Care in Behavioral Health Services 3-81
Orsillo, S. M. (2001). Measures for social phobia. In M. M. Antony, S. M. Orsillo, & L. Roemer (Eds.),
Practitioner’s guide to empirically based measures of anxiety (pp. 165–187). Dordrecht, Netherlands:
Kluwer Academic Publishers.
Ortega, A. N. & Rosenheck, R. (2001). Mental and physical health and acculturation among Hispanic
Vietnam veterans. Military Medicine, 166, 894–897.
Ortlepp, K. & Friedman, M. (2002). Prevalence and correlates of secondary traumatic stress in workplace
lay trauma counselors. Journal of Traumatic Stress, 15, 213–222.
Osterman, J. E. & de Jong, J. T. V. M. (2007). Cultural issues and trauma. In M. J. Friedman, T. M. Keane,
& P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 425–446). New York: Guilford
Press.
Otis, J. D., Keane, T. M., Kerns, R. D., Monson, C., & Scioli, E. (2009). The development of an integrated
treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Medicine,
10, 1300–1311.
Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: Current state of the evidence.
Dialogues in Clinical Neuroscience, 13, 413–421.
Otto, M. W. & Hinton, D. E. (2006). Modifying exposure-based CBT for Cambodian refugees with
posttraumatic stress disorder. Cognitive and Behavioral Practice, 13, 261–270.
Ougrin, D. (2011). Efficacy of exposure versus cognitive therapy in anxiety disorders: Systematic review
and meta-analysis. BMC. Psychiatry, 11, 200.
Ouimette, P. & Brown, P. J. (2003). Trauma and substance abuse: Causes, consequences, and treatment of
comorbid disorders. Washington, DC: American Psychological Association.
Ouimette, P. C., Ahrens, C., Moos, R. H., & Finney, J. W. (1998). During treatment changes in substance
abuse patients with posttraumatic stress disorder: The influence of specific interventions and program
environments. Journal of Substance Abuse Treatment, 15, 555–564.
Ouimette, P. C., Brown, P. J., & Najavits, L. M. (1998). Course and treatment of patients with both
substance use and posttraumatic stress disorders. Addictive Behaviors, 23, 785–795.
Ouimette, P., Moos, R. H., & Brown, P. J. (2003). Substance use disorder–posttraumatic stress disorder
comorbidity: A survey of treatments and proposed practice guidelines. In P. Ouimette & P. J. Brown
(Eds.), Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders
(pp. 91–110). Washington, DC: American Psychological Association.
Overmier, J. B. & Murison, R. (2005). Trauma and resulting sensitization effects are modulated by
psychological factors. Psychoneuroendocrinology, 30, 965–973.
Owens, G. P., Steger, M. F., Whitesell, A. A., & Herrera, C. J. (2009). Posttraumatic stress disorder, guilt,
depression, and meaning in life among military veterans. Journal of Traumatic Stress, 22, 654–657.
Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder
and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73.
Pae, C. U., Lim, H. K., Peindl, K., Ajwani, N., Serretti, A., Patkar, A. A. et al. (2008). The atypical
antipsychotics olanzapine and risperidone in the treatment of posttraumatic stress disorder: A meta-
3-82 Part 3, Section 3—General Bibliography
analysis of randomized, double-blind, placebo-controlled clinical trials. International Clinical
Psychopharmacology, 23, 1–8.
Palinkas, L., Downs, M., Patterson, J., & Russell, J. (1993). Social, cultural, and psychological impacts of
the Exxon Valdez oil spill. Human Organization, 52, 1–13.
Panagioti, M., Gooding, P., & Tarrier, N. (2009). Post-traumatic stress disorder and suicidal behavior: A
narrative review. Clinical Psychology Review, 29, 471–482.
Pandya, A. (2011). Group and family interventions. In F. J. Stoddard, Jr., A. Pandya, & C. L. Katz (Eds.),
Disaster psychiatry: Readiness, evaluation, and treatment (pp. 213–226). Arlington, VA: American
Psychiatric Publishing, Inc.
Paranjape, A. & Liebschutz, J. (2003). STaT: A three-question screen for intimate partner violence.
Journal of Women’s Health (Larchment), 12, 233–239.
Pastor, L. H. (2004). Culture as examining the causes and consequences of collective trauma. Psychiatric
Annals, 34, 616–622.
Paulson, D. S. & Krippner, S. (2007). Haunted by combat: Understanding PTSD in war veterans including
women, reservists, and those coming back from Iraq. Westport, CT: Praeger Security International.
Paunovic, N. & Öst, L. G. (2001). Cognitive–behavior therapy vs exposure therapy in the treatment of
PTSD in refugees. Behaviour Research and Therapy, 39, 1183–1197.
Pearlman, L. A. & Courtois, C. A. (2005). Clinical applications of the attachment framework: Relational
treatment of complex trauma. Journal of Traumatic Stress, 18, 449–459.
Pearlman, L. A. & Saakvitne, K. W. (1995). Trauma and the therapist: Countertransference and vicarious
traumatization in psychotherapy with incest survivors. New York: W. W. Norton.
Peddle, N. (2007). Assessing trauma impact, recovery, and resiliency in refugees of war. Journal of
Aggression, Maltreatment & Trauma, 14, 185–204.
Peebles, M. J. (1989). Posttraumatic stress disorder: A historical perspective on diagnosis and treatment.
Bulletin of the Menninger Clinic, 53, 274–286.
Peirce, J. M., Burke, C. K., Stoller, K. B., Neufeld, K. J., & Brooner, R. K. (2009). Assessing traumatic
event exposure: Comparing the Traumatic Life Events Questionnaire to the Structured Clinical
Interview for DSM-IV. Psychological Assessment, 21, 210–218.
Peirce, J. M., Kindbom, K. A., Waesche, M. C., Yuscavage, A. S. E., & Brooner, R. K. (2008).
Posttraumatic stress disorder, gender, and problem profiles in substance dependent patients.
Substance Use & Misuse, 43, 596–611.
Peller, A. J., Najavits, L. M., Nelson, S. E., LaBrie, R. A., & Shaffer, H. J. (2010). PTSD among a
treatment sample of repeat DUI offenders. Journal of Traumatic Stress, 23, 468–473.
Peltan, J. R. & Cellucci, T. (2011). Childhood sexual abuse and substance abuse treatment utilization
among substance-dependent incarcerated women. Journal of Substance Abuse Treatment, 41, 215–
224.
Penning, R., Veldstra, J. L., Daamen, A. P., Olivier, B., & Verster, J. C. (2010). Drugs of abuse, driving
and traffic safety. Current Drug Abuse Reviews, 3, 23–32.
Trauma-Informed Care in Behavioral Health Services 3-83
Peres, J. F. P., Newberg, A. B., Mercante, J. P., Simão, M., Albuquerque, V. E., Peres, M. J. P. et al.
(2007). Cerebral blood flow changes during retrieval of traumatic memories before and after
psychotherapy: A SPECT study. Psychological Medicine: A Journal of Research in Psychiatry and
the Allied Sciences, 37, 1481–1491.
Perez Benitez, C. I., Yen, S., Shea, M. T., Edelen, M. O., Markowitz, J. C., McGlashan, T. H. et al. (2010).
Ethnicity in trauma and psychiatric disorders: Findings from the collaborative longitudinal study of
personality disorders. Journal of Clinical. Psychology, 66, 583–598.
Perilla, J. L., Norris, F. H., & Lavizzo, E. A. (2002). Ethnicity, culture, and disaster response: Identifying
and explaining ethnic differences in PTSD six months after Hurricane Andrew. Journal of Social and
Clinical Psychology, 21, 20–45.
Peterlin, B. L., Rosso, A. L., Sheftell, F. D., Libon, D. J., Mossey, J. M., & Merikangas, K. R. (2011).
Post-traumatic stress disorder, drug abuse and migraine: New findings from the National Comorbidity
Survey Replication (NCS–R). Cephalalgia, 31, 235–244.
Petersilia, J. R. (2001). Crime victims with developmental disabilities: A review essay. Criminal Justice
and Behavior, 28, 655–694.
Pfefferbaum, B. J., Reissman, D. B., Pfefferbaum, R. L., Klomp, R. W., & Gurwitch, R. H. (2007).
Building resilience to mass trauma events. In L. S. Doll, S. E. Bonzo, J. A. Mercy, & D. A. Sleet
(Eds.), Handbook of injury and violence prevention (pp. 347–358). New York: Springer Publishing
Science + Business Media.
Pfeiffer, P. N., Ganoczy, D., Ilgen, M., Zivin, K., & Valenstein, M. (2009). Comorbid anxiety as a suicide
risk factor among depressed veterans. Depression and Anxiety, 26, 752–757.
Phillips, C. J., Leardmann, C. A., Gumbs, G. R., & Smith, B. (2010). Risk factors for posttraumatic stress
disorder among deployed US male marines. BMC Psychiatry, 10, 52.
Phoenix, B. J. (2007). Psychoeducation for survivors of trauma. Perspectives in Psychiatric Care, 43, 123–
131.
Picken, A. & Tarrier, N. (2011). Trauma and comorbid posttraumatic stress disorder in individuals with
schizophrenia and substance abuse. Comprehensive Psychiatry, 52, 490–497.
Pickering, R. P., Goldstein, R. B., Hasin, D. S., Blanco, C., Smith, S. M., Huang, B. et al. (2011).
Temporal relationships between overweight and obesity and DSM-IV substance use, mood, and
anxiety disorders: Results from a prospective study, the National Epidemiologic Survey on Alcohol
and Related Conditions. Journal of Clinical Psychiatry, 72, 1494–1502.
Pico-Alfonso, M. A. (2005). Psychological intimate partner violence: the major predictor of posttraumatic
stress disorder in abused women. Neuroscience and Biobehavioral Reviews, 29, 181–193.
Piefke, M., Pestinger, M., Arin, T., Kohl, B., Kastrau, F., Schnitker, R. et al. (2007). The neurofunctional
mechanisms of traumatic and non-traumatic memory in patients with acute PTSD following accident
trauma. Neurocase, 13, 342–357.
Pietrzak, R. H., Goldstein, M. B., Malley, J. C., Rivers, A. J., Johnson, D. C., & Southwick, S. M. (2010).
Risk and protective factors associated with suicidal ideation in veterans of Operations Enduring
Freedom and Iraqi Freedom. Journal of Affective Disorders, 123, 102–107.
3-84 Part 3, Section 3—General Bibliography
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2012). Physical health conditions
associated with posttraumatic stress disorder in U.S. older adults: Results from Wave 2 of the
National Epidemiologic Survey on Alcohol and Related Conditions. Journal of the American
Geriatrics Society, 60, 296–303.
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011a). Personality disorders
associated with full and partial posttraumatic stress disorder in the U.S. population: Results from
Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of
Psychiatric Research, 45, 678–686.
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011b). Prevalence and Axis I
comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2
of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety
Disorders, 25, 456–465.
Pietrzak, R. H., Johnson, D. C., Goldstein, M. B., Malley, J. C., Rivers, A. J., Morgan, C. A. et al. (2009).
Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in
veterans of Operations Enduring Freedom and Iraqi Freedom: The role of resilience, unit support, and
postdeployment social support. Journal of Special Operations Medicine, 9, 74–78.
Plummer, S. B. & Findley, P. A. (2012). Women with disabilities’ experience with physical and sexual
abuse. Trauma, Violence, & Abuse, 13, 15–29.
Pole, N., Best, S. R., Metzler, T., & Marmar, C. R. (2005). Why are Hispanics at greater risk for PTSD?
Cultural Diversity and Ethnic Minority Psychology, 11, 144–161.
Pole, N., Best, S. R., Weiss, D. S., Metzler, T., Liberman, A. M., Fagan, J. et al. (2003). Effects of gender
and ethnicity on duty-related posttraumatic stress symptoms among urban police officers. Journal of
Nervous & Mental Disease, 189, 442–448.
Pole, N., Gone, J. P., & Kulkarni, M. (2008). Posttraumatic stress disorder among ethnoracial minorities in
the United States. Clinical Psychology: Science and Practice, 15, 35–61.
Polinder, S., Haagsma, J. A., Belt, E., Lyons, R. A., Erasmus, V., Lund, J. et al. (2010). A systematic
review of studies measuring health-related quality of life of general injury populations. BMC Public
Health, 10, 783.
Polinder, S., Haagsma, J. A., Lyons, R. A., Gabbe, B. J., Ameratunga, S., Cryer, C. et al. (2012).
Measuring the population burden of fatal and nonfatal injury. Epidemiologic Reviews, 34, 17–31.
Polusny, M. A., Erbes, C. R., Murdoch, M., Arbisi, P. A., Thuras, P., & Rath, M. B. (2011). Prospective
risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq.
Psychological Medicine, 41, 687–698.
Polusny, M. A., Ries, B. J., Schultz, J. R., Calhoun, P., Clemensen, L., & Johnsen, I. R. (2008). PTSD
symptom clusters associated with physical health and health care utilization in rural primary care
patients exposed to natural disaster. Journal of Traumatic Stress, 21, 75–82.
Ponniah, K. & Hollon, S. D. (2009). Empirically supported psychological treatments for adult acute stress
disorder and posttraumatic stress disorder: A review. Depression and Anxiety, 26, 1086–1109.
Pope, K. S. & Brown, L. S. (1996). Recovered memories of abuse: Assessment, therapy, forensics.
Washington, DC: American Psychological Association.
Trauma-Informed Care in Behavioral Health Services 3-85
Possemato, K., Ouimette, P., & Knowlton, P. (2011). A brief self-guided telehealth intervention for post-
traumatic stress disorder in combat veterans: A pilot study. Journal of Telemedicine and Telecare, 17,
245–250.
Poulin, M. J., Silver, R. C., Gil-Rivas, V., Holman, E. A., & McIntosh, D. N. (2009). Finding social
benefits after a collective trauma: perceiving societal changes and well–being following 9/11. Journal
of Traumatic Stress., 22, 81–90.
Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J., & Foa, E. B. (2010). A meta-analytic
review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30, 635–
641.
Pratchett, L. C., Pelcovitz, M. R., & Yehuda, R. (2010). Trauma and violence: Are women the weaker sex?
Psychiatric Clinics of North America, 33, 465–474.
Prescott, L., Soares, P., Konnath, K., & Bassuk, E. (2008). A long journey home: A guide for creating
trauma-informed services for mothers and children experiencing homelessness. Draft. Rockville,
MD: Center for Mental Health Services, Substance Abuse and Mental Health Services
Administration; and the Daniels Fund, National Child Traumatic Stress Network, and the W.K.
Kellogg Foundation.
Prigerson, H. G., Maciejewski, P. K., & Rosenheck, R. A. (2002). Population attributable fractions of
psychiatric disorders and behavioral outcomes associated with combat exposure among US men.
American Journal of Public Health, 92, 59–63.
Prins, A., Cimpean, D., & Schnurr, P. P. (2009). Treatment in primary care settings. In Treatment of
posttraumatic stress disorder in special populations: A cognitive restructuring program (pp. 301–
314). Washington, DC: American Psychological Association.
Prins, A., Ouimette, P., Kimerling, R., Cameron, R. P., Hugelshofer, D. S., Shaw-Hegwer, J. et al. (2004).
The Primary Care PTSD Screen (PC–PTSD): Development and operating characteristics. Primary
Care Psychiatry, 9, 9–14.
Provencher, M. D., Hawke, L. D., & Thienot, E. (2011). Psychotherapies for comorbid anxiety in bipolar
spectrum disorders. Journal of Affective Disorders, 133, 371–380.
PsychologyTools.org (2012). Checklist for Better Sleep UK: Psychology Tools.org.
Ptasznik, A. (2009). No safe haven: Restraints reform targets traumatizing hospital practices. Cross
Currents Vol.12 No.3 .
Pulay, A. J., Stinson, F. S., Dawson, D. A., Goldstein, R. B., Chou, S. P., Huang, B. et al. (2009).
Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder:
Results From the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. The
Primary Care Companion to The Journal of Clinical Psychiatry, 11, 53–67.
Pyari, T. T., Kutty, R. V., & Sarma, P. S. (2012). Risk factors of post-traumatic stress disorder in tsunami
survivors of Kanyakumari District, Tamil Nadu, India. Indian Journal of Psychiatry, 54, 48–53.
Pynoos, R. S., Steinberg, A. M., Schreiber, M. D., & Brymer, M. J. (2006). Children and families: A new
framework for preparedness and response to danger, terrorism, and trauma. In L. A. Schein, H. I.
Spitz, G. M. Burlingame, & P. R. Muskin (Eds.), Psychological effects of catastrophic disasters:
Group approaches to treatment (pp. 83–112). New York: Haworth Press.
3-86 Part 3, Section 3—General Bibliography
Quarantini, L. C., Miranda-Scippa, A., Nery-Fernandes, F., Andrade–Nascimento, M., Galvão–de–
Almeida , A., Guimarães , J. L. et al. (2010). The impact of comorbid posttraumatic stress disorder on
bipolar disorder patients. Journal of Affective Disorders, 123, 71–76.
Quosh, C. & Gergen, K. J. (2008). Constructing trauma and its treatment: Knowledge, power and
resistance. In T. Sugiman, K. J. Gergen, W. Wagner, & Y. Yamada (Eds.), Meaning in action:
Constructions, narratives, and representations (pp. 97–111). New York: Springer Publishing Science
+ Business Media.
Qureshi, S. U., Pyne, J. M., Magruder, K. M., Schulz, P. E., & Kunik, M. E. (2009). The link between
post-traumatic stress disorder and physical comorbidities: A systematic review. Psychiatric
Quarterly, 80, 87–97.
Racanelli, C. (2005). Attachment and compassion fatigue among American and Israeli mental health
clinicians working with traumatized victims of terrorism. International Journal of Emergency Mental
Health, 7, 115–124.
Rachamim, L., Nacasch, N., Shafran, N., Tzur, D., & Gilboa-Schechtman, E. (2009). Exposure-based
therapy for post-traumatic stress disorder in children and adults. Israel Journal of Psychiatry and
Related Sciences, 46, 274–281.
Rakofsky, J. J. & Dunlop, B. W. (2011). Treating nonspecific anxiety and anxiety disorders in patients
with bipolar disorder: A review. Journal of Clinical Psychiatry, 72, 81–90.
Rand, M. R. & obinson, J. F. (2012). Criminal victimization in the United States, 2008 – Statistical tables.
Washington, DC: Bureau of Justice Statistics.
Raphael, B. & Wooding, S. (2006). Group intervention for the prevention and treatment of acute initial
stress reactions in civilians. In Psychological effects of catastrophic disasters: Group approaches to
treatment (pp. 481–503). New York: Haworth Press.
Rasmussen, B. (2012). The effects of trauma treatment on the therapist. In S. Ringel & J. R. Brandell
(Eds.), Trauma: Contemporary directions in theory, practice, and research. (pp. 223–246). Thousand
Oaks, CA: Sage Publications.
Rasmussen, T. & Bloomenfeld, J. (2009). Focus: Healping to heal the scars: What does trauma-informed
look like? Cross Currents Vol.12 No.3.
Rauch, S. A., Grunfeld, T. E., Yadin, E., Cahill, S. P., Hembree, E., & Foa, E. B. (2009). Changes in
reported physical health symptoms and social function with prolonged exposure therapy for chronic
posttraumatic stress disorder. Depression and Anxiety, 26, 732–738.
Ravindran, L. N. & Stein, M. B. (2009). Pharmacotherapy of PTSD: Premises, principles, and priorities.
Brain Research, 1293, 24–39.
Ravindran, L. N. & Stein, M. B. (2010). Pharmacotherapy of post-traumatic stress disorder. Current
Topics in Behavioral Neurosciences, 2, 505–525.
Ravindran, L. N., Stein, M. B., & Ravindran, A. V. (2010). Pharmacotherapy of PTSD: An evidence-based
review. In L. Sher & A. Vilens (Eds.), Neurobiology of post-traumatic stress disorder (pp. 271–290).
New York: Nova Biomedical.
Trauma-Informed Care in Behavioral Health Services 3-87
Ray, L. A., Capone, C., Sheets, E., Young, D., Chelminski, I., & Zimmerman, M. (2009). Posttraumatic
stress disorder with and without alcohol use disorders: Diagnostic and clinical correlates in a
psychiatric sample. Psychiatry Research, 170, 278–281.
Razza, N. J., Tomasulo, D. J., & Sobsey, D. (2011). Group psychotherapy for trauma-related disorders in
people with intellectual disabilities. Advances in Mental Health and Intellectual Disabilities, 5, 40–
45.
Read, J. & Hammersley, P. (2005). Child sexual abuse and schizophrenia. British Journal of Psychiatry,
186, 76.
Read, J. P., Bollinger, A. R., & Sharkansky, E. (2003). Assessment of comorbid substance use disorder
and posttraumatic stress disorder. In P. Ouimette & P. J. Brown (Eds.), Trauma and substance abuse:
Causes, consequences, and treatment of comorbid disorders (pp. 111–125). Washington, DC:
American Psychological Association.
Read, J., Agar, K., Argyle, N., & Aderhold, V. (2003). Sexual and physical abuse during childhood and
adulthood as predictors of hallucinations, delusions and thought disorder. Psychology and
Psychotherapy: Theory, Research and Practice, 76, 1–22.
Read, J., van Os, J.,Morrison, A. P., & Ross, C. A. (2005). Childhood trauma, psychosis and
schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica
Scandinavica, 112, 330–350.
Ready, D. J., Thomas, K. R., Worley, V., Backscheider, A. G., Harvey, L. A., Baltzell, D. et al. (2008). A
field test of group based exposure therapy with 102 veterans with war-related posttraumatic stress
disorder. Journal of Traumatic Stress, 21, 150–157.
Reddy, M. K., Polusny, M. A., & Murdoch, M. (2009). On counterbalancing of symptom–reporting in
trauma surveys. Psychological Reports, 105, 1154–1158.
Rees, B. (2011). Overview of outcome data of potential meditation training for soldier resilience. Military
Medicine, 176, 1232–1242.
Regel, S., Joseph, S., & Dyregrov, A. (2007). Psychological debriefing in cross-cultural contexts: Ten
implications for practice. Int.J Emerg.Ment Health, 9, 37–45.
Reiland, S. & Lauterbach, D. (2008). Effects of trauma and religiosity on self-esteem. Psychological
Reports, 102, 779–790.
Relapse prevention: Maintenance strategies in the treatment of addictive behaviors (2005). (2nd ed.) New
York: Guilford Press.
Renshaw, K. D. (2011). An integrated model of risk and protective factors for post-deployment PTSD
symptoms in OEF/OIF era combat veterans. Journal of Affective Disorders, 128, 321–326.
Renshaw, K. D., Blais, R. K., & Caska, C. M. (2011). Distress in spouses of combat veterans with PTSD:
The importance of interpersonally based cognitions and behaviors. In S. M. Wadsworth & D. Riggs
(Eds.), Risk and resilience in U.S. military families (pp. 69–84). New York: Springer Publishing
Science + Business Media.
Renshaw, K. D., Rodrigues, C. S., & Jones, D. H. (2008). Psychological symptoms and marital satisfaction
in spouses of Operation Iraqi Freedom veterans: Relationships with spouses' perceptions of veterans'
experiences and symptoms. Journal of Family Psychology, 22, 586–594.
3-88 Part 3, Section 3—General Bibliography
Resick, P. A. (2001). Cognitive therapy for posttraumatic stress disorder. Journal of Cognitive
Psychotherapy: An International Quarterly, 15, 321–329.
Resick, P. A. & Schnicke, M. K. (1992). Cognitive processing therapy for sexual assault victims. Journal
of Consulting and Clinical Psychology, 60, 748–756.
Resick, P. A. & Schnicke, M. K. (1993). Cognitive processing therapy for rape victims: A treatment
manual. Newbury Park, CA: Sage Publications.Resick, P. A., Galovski, T. E., O’Brien, U. M., Scher,
C. D., Clum, G. A., & Young-Xu, Y. (2008). A randomized clinical trial to dismantle components of
cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal
violence. Journal of Consulting and Clinical Psychology, 76, 243–258.
Resick, P. A., Nishith, P., & Griffin, M. G. (2003). How well does cognitive–behavioral therapy treat
symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial.
CNS Spectrums, 8, 340–355.
Resick, P. A., Nishith, P., Weaver, T. L., Astin, M. C., & Feuer, C. A. (2002). A comparison of cognitive–
processing therapy with prolonged exposure and a waiting condition for the treatment of chronic
posttraumatic stress disorder in female rape victims. Journal of Consulting & Clinical Psychology,
70, 867–879.
Resick, P. A., Williams, L. F., Suvak, M. K., Monson, C. M., & Gradus, J. L. (2012). Long-term outcomes
of cognitive–behavioral treatments for posttraumatic stress disorder among female rape survivors.
Journal of Consulting and Clinical Psychology, 80, 201–210.
Resnick, H. S., Acierno, R., Amstadter, A. B., Self-Brown, S., & Kilpatrick, D. G. (2007). An acute post-
sexual assault intervention to prevent drug abuse: Updated findings. Addict.Behav, 32, 2032–2045.
Resnick, H. S., Kilpatrick, D. G., Dansky, B. S., Saunders, B. E., & Best, C. L. (1993). Prevalence of
civilian trauma and posttraumatic stress disorder in a representative national sample of women.
Journal of Consulting and Clinical Psychology, 61, 984–991.
Resnick, S. G., Bond, G. R., & Mueser, K. T. (2003). Trauma and posttraumatic stress disorder in people
with schizophrenia. Journal of Abnormal Psychology, 112, 415–423.
Reynolds, M., Mezey, G., Chapman, M., Wheeler, M., Drummond, C., & Baldacchino, A. (2005). Co-
morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol
Dependence, 77, 251–258.
Reyome, N. D. (2010). Childhood emotional maltreatment and later intimate relationships: Themes from
the empirical literature. Journal of Aggression, Maltreatment & Trauma, 19, 224–242.
Rhatigan, D. L., Moore, T. M., & Street, A. E. (2005). Reflections on partner violence. Journal of
Interpersonal Violence, 20, 82–88.
Richardson, J. D., Elhai, J. D., & Pedlar, D. J. (2006). Association of PTSD and depression with medical
and specialist care utilization in modern peacekeeping veterans in Canada with health-related
disabilities. Journal of Clinical Psychiatry, 67, 1240–1245.
Richardson, J. I. (2001). Guidebook on vicarious trauma: Recommended solutions for anti-violence
workers. Ottawa, Ontario: Health Canada.
Riggs, D. S., Monson, C. M., Glynn, S. M., & Canterino, J. (2009). Couple and family therapy for adults.
In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD:
Trauma-Informed Care in Behavioral Health Services 3-89
Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.) (pp. 458–
478). New York: Guilford Press.
Riggs, D. S., Rukstalis, M., Volpicelli, J. R., Kalmanson, D., & Foa, E. B. (2003). Demographic and social
adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol
dependence: potential pitfalls to PTSD treatment. Addictive Behaviors, 28, 1717–1730.
Risk and resilience in U.S. military families (2011). New York: Springer Publishing Science + Business
Media.
Roberts, A. L., Austin, S. B., Corliss, H. L., Vandermorris, A. K., & Koenen, K. C. (2010). Pervasive
trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress
disorder. American Journal of Public Health, 100, 2433–2441.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic differences in
exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking
for post-traumatic stress disorder in the United States. Psychological Medicine: A Journal of
Research in Psychiatry and the Allied Sciences, 41, 71–83.
Roberts, A. L., McLaughlin, K. A., Conron, K. J., & Koenen, K. C. (2011). Adulthood stressors, history of
childhood adversity, and risk of perpetration of intimate partner violence. American Journal of
Preventive Medicine, 40, 128–138.
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. (2009a). Multiple session early psychological
interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic
Reviews, CD006869.
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. I. (2009b). Systematic review and meta-analysis
of multiple-session early interventions following traumatic events. American Journal of Psychiatry,
166, 293–301.
Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. I. (2010). Early psychological interventions to
treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews, CD007944.
Robinaugh, D. J. & McNally, R. J. (2011). Trauma centrality and PTSD symptom severity in adult
survivors of childhood sexual abuse. Journal of Traumatic Stress, 24, 483–486.
Robjant, K. & Fazel, M. (2010). The emerging evidence for narrative exposure therapy: A review. Clinical
Psychology Review, 30, 1030–1039.
Rohde, P., Ichikawa, L., Simon, G. E., Ludman, E. J., Linde Jongh, A., Jeffery, R. W. et al. (2008).
Associations of child sexual and physical abuse with obesity and depression in middle–aged women.
Child Abuse & Neglect, 32, 878–887.
Roht-Arriaza, N. (1995). Punishment, redress, and pardon: Theoretical and psychological approaches. In
N. Roht-Arriaza (Ed.), Impunity and human rights in international law and practice. (pp. 13–23).
Oxford, England: Oxford University Press.
Roman, P. M. & Johnson, J. A. (2002). National Treatment Center Study summary report: Private
treatment centers. Athens, GA: Institute for Behavioral Research, University of Georgia.
Rosen, G. M. & Frueh, B. C. (2010). Clinician’s guide to posttraumatic stress disorder. Hoboken, NJ:
John Wiley and Sons, Inc.
3-90 Part 3, Section 3—General Bibliography
Rosenbaum, S., Nguyen, D., Lenehan, T., Tiedemann, A., van der Ploeg, H. P., & Sherrington, C. (2011).
Exercise augmentation compared to usual care for post traumatic stress disorder: A randomised
controlled trial (the REAP study: Randomised Exercise Augmentation for PTSD). BMC Psychiatry,
11.
Rosenberg, L. (2011). 2011 Letters: Trauma-informed care: A call to arms. Washington, DC: National
Council for Community Behavioral Healthcare.
Rosenberg, S. D. & Mueser, K. T. (2008). Trauma and posttraumatic stress syndromes. In K.T.Mueser &
D. V. Jeste (Eds.), Clinical handbook of schizophrenia (pp. 447–458). New York: Guilford Press.
Rosenberg, S. D., Lu, W., Mueser, K. T., Jankowski, M. K., & Cournos, F. (2007). Correlates of adverse
childhood events among adults with schizophrenia spectrum disorders. Psychiatric Services, 58, 245–
253.
Rosenberg, S. D., Mueser, K. T., Friedman, M. J., Gorman, P. G., Drake, R. E., Vidaver, R. M. et al.
(2001). Developing effective treatments for posttraumatic disorders among people with severe mental
illness. Psychiatric Services, 52, 1453–1461.
Rosenheck, R. & Fontana, A. (1996). Race and outcome of treatment for veterans suffering from PTSD.
Journal of Traumatic Stress, 9, 343–351.
Rosenthal, B. S. & Wilson, W. C. (2003). The association of ecological variables and psychological
distress with exposure to community violence among adolescents. Adolescence, 38, 459–479.
Rosenthal, J. Z., Grosswald, S., Ross, R., & Rosenthal, N. (2011). Effects of transcendental meditation in
veterans of Operation Enduring Freedom and Operation Iraqi Freedom with posttraumatic stress
disorder: A pilot study. Military Medicine, 176, 626–630.
Rossen, L. M., Pollack, K. M., Canham-Chervak, M., Canada, S., & Baker, S. P. (2011). Motor vehicle
crashes among active duty U.S. Army personnel, 1999 to 2006. Military Medicine, 176, 1019–1026.
Rothbaum, B. O. (2011). Another perspective on exposure therapy for PTSD. In D.J.Stein, M. J. Friedman,
& C. Blanco (Eds.), Post-traumatic stress disorder (pp. 211–215). Chichester, UK: John Wiley and
Sons, Inc.
Rothbaum, B. O., Davidson, J. R., Stein, D. J., Pedersen, R., Musgnung, J., Tian, X. W. et al. (2008). A
pooled analysis of gender and trauma-type effects on responsiveness to treatment of PTSD with
venlafaxine extended release or placebo. Journal of Clinical Psychiatry, 69, 1529–1539.
Rothbaum, B. O., Meadows, E. A., Resick, P., & Foy, D. W. (2000). Cognitive–behavioral therapy. In E.
B. Foa & T. M. Keane (Eds.), Effective treatments for PTSD: Practice guidelines from the
International Society for Traumatic Stress Studies (pp. 60–83). New York: Guilford Press.
Rothman, E. F., Exner, D., & Baughman, A. L. (2011). The prevalence of sexual assault against people
who identify as gay, lesbian, or bisexual in the United States: A systematic review. Trauma, Violence,
& Abuse, 12, 55–66.
Roy-Byrne, P. P., Russo, J., Michelson, E., Zatzick, D., Pitman, R. K., & Berliner, L. (2004). Risk factors
and outcome in ambulatory assault victims presenting to the acute emergency department setting:
implications for secondary prevention studies in PTSD. Depression and Anxiety, 19, 77–84.
Royle, L., Keenan, P., & Farrell, D. (2009). Issues of stigma for first responders accessing support for post
traumatic stress. International Journal of Emergency Mental Health, 11, 79–85.
Trauma-Informed Care in Behavioral Health Services 3-91
Rubin, D. C., Berntsen, D., & Bohni, M. K. (2008). A memory-based model of posttraumatic stress
disorder: Evaluating basic assumptions underlying the PTSD diagnosis. Psychological Review, 115,
985–1011.
Ruef, A. M., Litz, B. T., & Schlenger, W. E. (2000). Hispanic ethnicity and risk for combat-related
posttraumatic stress disorder. Cultural Diversity and Ethnic Minority Psychology, 6, 235–251.
Rush, A. J., Zimmerman, M., Wisniewski, S. R., Fava, M., Hollon, S. D., Warden, D. et al. (2005).
Comorbid psychiatric disorders in depressed outpatients: Demographic and clinical features. Journal
of Affective Disorders, 87, 43–55.
Rush, B. & Koegl, C. J. (2008). Prevalence and profile of people with co-occurring mental and substance
use disorders within a comprehensive mental health system. Canadian Journal of Psychiatry, 53,
810–821.
Russell, M. C. (2008). War-related medically unexplained symptoms, prevalence, and treatment: Utilizing
EMDR within the armed services. Journal of EMDR Practice and Research, 2, 212–225.
Ruzek, J. I. (2006). Models of early intervention following mass violence and other trauma. In
Interventions following mass violence and disasters: Strategies for mental health practice (pp. 16–
34). New York: Guilford Press.
Ruzek, J., Walser, R. D., Naugle, A. E., Litz, B., Mennin, D. S., Polusny, M. A. et al. (2008). Cognitive–
behavioral psychology: Implications for disaster and terrorism response. Prehospital and Disaster
Medicine, 23, 397–410.
Saakvitne, K. W., Pearlman, L. A., & Traumatic Stress Institute/Center for Adult & Adolescent
Psychotherapy (1996). Transforming the pain: A workbook on vicarious traumatization. (1st ed.)
New York: W.W. Norton.
Sacks, J. Y., McKendrick, K., & Banks, S. (2008). The impact of early trauma and abuse on residential
substance abuse treatment outcomes for women. Journal of Substance Abuse Treatment, 34, 90–100.
Sacks, S., McKendrick, K., Sacks, J. Y., Banks, S., & Harle, M. (2008). Enhanced outpatient treatment for
co-occurring disorders: Main outcomes. Journal of Substance Abuse Treatment, 34, 48–60.
Sadler, A. G., Booth, B. M., Cook, B. L., & Doebbeling, B. N. (2003). Factors associated with women’s
risk of rape in the military environment. American Journal of Industrial Medicine, 43, 262–273.
Sala, T., Cox, B. J., & Sareen, J. (2008). Anxiety disorders and physical illness comorbidity: An overview.
In Anxiety in health behaviors and physical illness (pp. 131–154). New York: Springer Publishing
Science + Business Media.
Salasin, S. (2011). Sine qua non for public health. National Council Magazine, 18.
Salyers, M. P., Evans, L. J., Bond, G. R., & Meyer, P. S. (2004). Barriers to assessment and treatment of
posttraumatic stress disorder and other trauma-related problems in people with severe mental illness:
Clinician perspectives. Community Mental Health Journal, 40, 17–31.
San Diego Trauma Informed Guide Team. (2012). Are you asking the right questions? A client centered
approach. San Diego, CA: San Diego Trauma Informed Guide Team.
Sandoval, J., Scott, A. N., & Padilla, I. (2009). Crisis counseling: An overview. Psychology in the Schools,
46, 246–256.
3-92 Part 3, Section 3—General Bibliography
Santa Mina, E. E. & Gallop, R. M. (1998). Childhood sexual and physical abuse and adult self-harm and
suicidal behaviour: A literature review. Canadian Journal of Psychiatry, 43, 793–800.
Santos, M. R., Russo, J., Aisenberg, G., Uehara, E., Ghesquiere, A., & Zatzick, D. F. (2008). Ethnic/racial
diversity and posttraumatic distress in the acute care medical setting. Psychiatry, 71, 234–245.
Sarapas, C., Cai, G., Bierer, L. M., Golier, J. A., Galea, S., Ising, M. et al. (2011). Genetic markers for
PTSD risk and resilience among survivors of the World Trade Center attacks. Disease Markers, 30,
101–110.
Sartor, C. E., McCutcheon, V. V., Pommer, N. E., Nelson, E. C., Grant, J. D., Duncan, A. E. et al. (2011).
Common genetic and environmental contributions to post-traumatic stress disorder and alcohol
dependence in young women. Psychological Medicine, 41, 1497–1505.
Sautter, F. J., Armelie, A. P., Glynn, S. M., & Wielt, D. B. (2011). The development of a couple-based
treatment for PTSD in returning veterans. Professional Psychology: Research and Practice, 42, 63–
69.
Sautter, F. J., Glynn, S. M., Thompson, K. E., Franklin, L., & Han, X. (2009). A couple-based approach to
the reduction of PTSD avoidance symptoms: Preliminary findings. Journal of Marital and Family
Therapy, 35, 343–349.
Savage, A., Quiros, L., Dodd, S. J., & Bonavota, D. (2007). Building trauma informed practice:
Appreciating the impact of trauma in the lives of women with substance abuse and mental health
problems. Journal of Social Work Practice in the Addictions, 7, 91–116.
Savoca, E. & Rosenheck, R. (2000). The civilian labor market experiences of Vietnam–era veterans: The
influence of psychiatric disorders. Journal of Mental Health Policy and Economics, 3, 199–207.
Saxon, A. J., Davis, T. M., Sloan, K. L., McKnight, K. M., Jeammet, P., & Kivlahan, D. R. (2001).
Trauma, symptoms of posttraumatic stress disorder, and associated problems among incarcerated
veterans. Psychiatric Services, 52, 959–964.
Sayed, A. M. & Galea, S. (2011). Challenges and future horizons in epedemiological research into PTSD.
In D. J. Stein, M. J. Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 75–81).
Chichester, UK: John Wiley and Sons, Inc.
Sayer, N. A., Carlson, K. F., & Schnurr, P. P. (2011). Assessment of functioning and disability. In D. M.
Benedek & G. H. Wynn (Eds.), Clinical manual for management of PTSD (pp. 255–287). Arlington,
VA, US: American Psychiatric Publishing, Inc.
Sayer, N. A., Noorbaloochi, S., Frazier, P., Carlson, K., Gravely, A., & Murdoch, M. (2010). Reintegration
problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical
care. Psychiatric Services, 61, 589–597.
Schacht, L., Pandiani, J. A., & Banks, S. M. (2007). Access to community mental health services: A study
of adult victims of trauma. Best Practices in Mental Health: An International Journal, 3, 1–8.
Schafer, I. & Fisher, H. L. (2011). Childhood trauma and posttraumatic stress disorder in patients with
psychosis: clinical challenges and emerging treatments. Current Opinion in Psychiatry, 24.
Schafer, I., Morgan, C., Demjaha, A., Morgan, K., Dazzan, P., Fearon, P. et al. (2011). Assessment of
posttraumatic symptoms in patients with first-episode psychosis. Journal of Nervous and Mental
Disease, 199, 896–898.
Trauma-Informed Care in Behavioral Health Services 3-93
Schauben, L. J. & Frazier, P. A. (1995). Vicarious trauma: The effects on female counselors of working
with sexual violence survivors. Psychology of Women Quarterly, 19, 49–64.
Schechter, D. S. & Willheim, E. (2009). The effects of violent experiences on infants and young children.
In Handbook of infant mental health (3rd ed.) (pp. 197–213). New York: Guilford Press.
Schein, L. A., Spitz, H. I., Burlingame, G. M., & Muskin, P. R. (2006). Psychological effects of
catastrophic disasters: Group approaches to treatment. New York: Haworth Press.
Schneier, F. R., Neria, Y., Pavlicova, M., Hembree, E., Suh, E. J., Amsel, L. et al. (2012). Combined
prolonged exposure therapy and paroxetine for PTSD related to the World Trade Center attack: A
randomized controlled trial. American Journal of Psychiatry, 169, 80–88.
Schnurr, P. P. & Lunney, C. A. (2011). Work-related quality of life and posttraumatic stress disorder
symptoms among female veterans. Womens Health Issues, 21, S169–S175.
Schnurr, P. P., Friedman, M. J., Engel, C. C., Foa, E. B., Shea, M. T., Chow, B. K. et al. (2007). Cognitive
behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. JAMA:
The Journal of the American Medical Association, 297, 820–830.
Schnurr, P. P., Friedman, M. J., Foy, D. W., Shea, M. T., Hsieh, F. Y., Lavori, P. W. et al. (2003).
Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a
Department of Veterans Affairs Cooperative Study. Archives of General Psychiatry, 60, 481–489.
Schnurr, P. P., Lunney, C. A., Bovin, M. J., & Marx, B. P. (2009). Posttraumatic stress disorder and
quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical
Psychology Review, 29, 727–735.
Schnurr, P. P., Lunney, C. A., Sengupta, A., & Waelde, L. C. (2003). A descriptive analysis of PTSD
chronicity in Vietnam veterans. Journal of Traumatic Stress, 16, 545–553.
Schönenberg, M., Reichwald, U., Domes, G., Badke, A., & Hautzinger, M. (2005). Effects of
peritraumatic ketamine medication on early and sustained posttraumatic stress symptoms in
moderately injured accident victims. Psychopharmacology (Berl), 182, 420–425.
Schönenberg, M., Reichwald, U., Domes, G., Badke, A., & Hautzinger, M. (2008). Ketamine aggravates
symptoms of acute stress disorder in a naturalistic sample of accident victims. Journal of
Psychopharmacology, 22, 493–497.
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., & Gray, S. H. (2008). Contributions of psychodynamic
approaches to treatment of PTSD and trauma: A review of the empirical treatment and
psychopathology literature. Psychiatry, 71, 13–34.
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., Tendick, V., & Gray, S. H. (2008). Nonresponse and
dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry, 71,
134–168.
Schredl, M. & Reinhard, I. (2011). Gender differences in nightmare frequency: A meta-analysis. Sleep
Medicine Reviews, 15, 115–121.
Schubert, C. C. & Punamäki, R. L. (2011). Mental health among torture survivors: Cultural background,
refugee status and gender. Nordic Journal of Psychiatry, 65, 175–182.
3-94 Part 3, Section 3—General Bibliography
Schulz, P. M., Marovic-Johnson, D., & Huber, L. C. (2006). Cognitive–behavioral treatment of rape- and
war-related posttraumatic stress disorder with a female, Bosnian refugee. Clinical Case Studies, 5,
191–208.
Schumm, J. A., Briggs-Phillips, M., & Hobfoll, S. E. (2006). Cumulative interpersonal traumas and social
support as risk and resiliency factors in predicting PTSD and depression among inner-city women.
Journal of Traumatic Stress, 19, 825–836.
Schwartz, R. C., Schwartz, M. F., & Galperin, L. (2009). Internal family systems therapy. In Treating
complex traumatic stress disorders: An evidence-based guide (pp. 353–370). New York: Guilford
Press.
Schwartz, S., Hoyte, J., James, T., Conoscenti, L., Johnson, R., & Liebschutz, J. (2010). Challenges to
engaging Black male victims of community violence in healthcare research: Lessons learned from
two studies. Psychological trauma: Theory, research, practice, and policy, 2, 54–62.
Schwartzbard, R. (1997). On the scene report of the Missouri floods. Ronkonkoma, NY: American
Academy of Experts in Traumatic Stress.
Schweitzer, R. D., Brough, M., Vromans, L., & Asic-Kobe, M. (2011). Mental health of newly arrived
Burmese refugees in Australia: Contributions of pre-migration and post-migration experience.
Australian and New Zealand Journal of Psychiatry, 45, 299–307.
Schweitzer, R., Melville, F., Steel, Z., & Lacherez, P. (2006). Trauma, post-migration living difficulties,
and social support as predictors of psychological adjustment in resettled Sudanese refugees.
Australian and New Zealand Journal of Psychiatry, 40, 179–187.
Scott, J. C. (1990). Domination and the arts of resistance: Hidden transcripts. New Haven, CT: Yale
University Press.
Scott, W. J. (1990). PTSD in DSM-III: A case in the politics of diagnosis and disease. Social Problems,
37, 294–310.
Seal, K. H., Metzler, T. J., Gima, K. S., Bertenthal, D., Maguen, S., & Marmar, C. R. (2009). Trends and
risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of
Veterans Affairs health care, 2002–2008. American Journal of Public Health, 99, 1651–1658.
Seal, K. H., Shi, Y., Cohen, G., Cohen, B. E., Maguen, S., Krebs, E. E. et al. (2012). Association of mental
health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and
Afghanistan. JAMA, 307, 940–947.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for
depression: A new approach to preventing relapse. New York: Guilford Press.
Seidler, G. H. & Wagner, F. E. (2006). Comparing the efficacy of EMDR and trauma-focused cognitive–
behavioral therapy in the treatment of PTSD: A meta-analytic study. Psychological Medicine, 36,
1515–1522.
Seng, J. S., Kohn–Wood, L. P., McPherson, M. D., & Sperlich, M. (2011). Disparity in posttraumatic
stress disorder diagnosis among African American pregnant women. Archives of Women’s Mental
Health, 14, 295–306.
Trauma-Informed Care in Behavioral Health Services 3-95
Seng, J. S., Low, L. K., Sperlich, M., Ronis, D. L., & Liberzon, I. (2011). Post-traumatic stress disorder,
child abuse history, birthweight and gestational age: A prospective cohort study. International
Journal of Obstetrics and Gynaecology, 118, 1329–1339.
Sequeira, H. & Hollins, S. (2003). Clinical effects of sexual abuse on people with learning disability:
Critical literature review. British Journal of Psychiatry, 182, 13–19.
Sexton, L. (1999). Vicarious traumatisation of counsellors and effects on their workplaces. British Journal
of Guidance & Counselling, 27, 393–403.
Shah, S. A. (2007). Ethnomedical best practices for international psychosocial efforts in disaster and
trauma. In J. P. Wilson & C. S. Tang (Eds.), Cross-cultural assessment of psychological trauma and
PTSD (pp. 51–64). New York: Springer Publishing Science + Business Media.
Shaikh Al Arab, A., Guedon-Moreau, L., Ducrocq, F., Molenda, S., Duhem, S., Salleron, J. et al. (2012).
Temporal analysis of heart rate variability as a predictor of post traumatic stress disorder in road
traffic accidents survivors. Journal of Psychiatric Research.
Shalev, A. Y., Ankri, Y., Israeli-Shalev, Y., Peleg, T., Adessky, R., & Freedman, S. (2012). Prevention of
posttraumatic stress disorder by early treatment: results from the Jerusalem Trauma Outreach And
Prevention study. Archives of General Psychiatry, 69, 166–176.
Shalev, A. Y., Sahar, T., Freedman, S., Peri, T., Glick, N., Brandes, D. et al. (1998). A prospective study
of heart rate response following trauma and the subsequent development of posttraumatic stress
disorder. Archives of General Psychiatry, 55, 553–559.
Shalev, A. Y., Tuval-Mashiach, R., & Hadar, H. (2004). Posttraumatic stress disorder as a result of mass
trauma. Journal of Clinical Psychiatry, 65 Supplement 1, 4–10.
Shapiro, F. (2001). Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols,
and procedures. (2nd ed.) New York: Guilford Press.
Sharpless, B. A. & Barber, J. P. (2011). A clinician’s guide to PTSD treatments for returning veterans.
Professional Psychology: Research and Practice, 42, 8–15.
Sharpley, J. G., Fear, N. T., Greenberg, N., Jones, M., & Wessely, S. (2008). Pre-deployment stress
briefing: Does it have an effect? Occupational Medicine, 58, 30–34.
Shaw, J. A., Espinel, Z., & Shultz, J. M. (2007). The context of trauma. In Children: Stress, trauma and
disasters (pp. 45–59). Tampa, FL: Disaster Life Support Publishing.
Shea, M. T., McDevitt–Murphy, M., Ready, D. J., & Schnurr, P. P. (2009). Group therapy. In E. B. Foa, T.
M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines
from the International Society for Traumatic Stress Studies (2nd ed.) (pp. 306–326). New York:
Guilford Press.
Sheinberg, M. & True, F. (2008). Treating family relational trauma: A recursive process using a decision
dialogue. Family Process, 47, 173–195.
Shemesh, E., Yehuda, R., Milo, O., Dinur, I., Rudnick, A., Vered, Z. et al. (2004). Posttraumatic stress,
nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosomatic Medicine,
66, 521–526.
3-96 Part 3, Section 3—General Bibliography
Shen, Y. C., Arkes, J., & Williams, T. V. (2012). Effects of Iraq/Afghanistan deployments on major
depression and substance use disorder: Analysis of active duty personnel in the US military.
American Journal of Public Health, 102, S80–S87.
Sher, L. & Vilens, A. (2010). Neurobiology of post-traumatic stress disorder. New York: Nova
Biomedical.
Sher, L. (2010). Traumatic Stress, depression and suicide. In L. Sher & A. Vilens (Eds.), Neurobiology of
post-traumatic stress disorder (pp. 259–270). New York: Nova Biomedical.
Sherbourne, C. D., Sullivan, G., Craske, M. G., Roy-Byrne, P., Golinelli, D., Rose, R. D. et al. (2010).
Functioning and disability levels in primary care out-patients with one or more anxiety disorders.
Psychological Medicine, 40, 2059–2068.
Sherin, J. E. & Nemeroff, C. B. (2011). Post-traumatic stress disorder: The neurobiological impact of
psychological trauma. Dialogues in Clinical Neuroscience, 13, 263–278.
Sherman, M. D., Zanotti, D. K., & Jones, D. E. (2005). Key elements in couples therapy with veterans with
combat-related posttraumatic stress disorder. Professional Psychology–Research and Practice, 36,
626–633.
Sherrer, M. V. (2011). The role of cognitive appraisal in adaptation to traumatic stress in adults with
serious mental illness: A critical review. Trauma, Violence, & Abuse, 12, 151–167.
Sholomskas, D. E. & Carroll, K. M. (2006). One small step for manuals: Computer-assisted training in
twelve-step facilitation. Journal of Studies on Alcohol, 67, 939–945.
Shoptaw, S., Stein, J. A., & Rawson, R. A. (2000). Burnout in substance abuse counselors: Impact of
environment, attitudes, and clients with HIV. Journal of Substance Abuse Treatment, 19, 117–126.
Showalter, S. E. (2010). Compassion fatigue: What is it? Why does it matter? Recognizing the symptoms,
acknowledging the impact, developing the tools to prevent compassion fatigue, and strengthen the
professional already suffering from the effects. American Journal of Hospice & Palliative Medicine,
27, 239–242.
Sijbrandij, M., Olff, M., Reitsma, J. B., Carlier, I. V., & Gersons, B. P. (2006). Emotional or educational
debriefing after psychological trauma. Randomised controlled trial. British Journal of Psychiatry,
189, 150–155.
Silver, R. C., Holman, E. A., McIntosh, D. N., Poulin, M., & Gil-Rivas, V. (2002). Nationwide logitudinal
study of psychological responses to September 11. Journal of the American Medical Association,
288, 1235–1244.
Silver, R. C., Holman, E. A., McIntosh, D. N., Poulin, M., Gil-Rivas, V., & Pizarro, J. (2006). Coping with
a national trauma: A nationwide longitudinal study of responses to the terrorist attacks of September
11. In 9/11: Mental health in the wake of terrorist attacks (pp. 45–70). New York: Cambridge
University Press.
Silver, R. C., Poulin, M., Holman, E. A., Mclntosh, D. N., Gil-Rivas, V., & Pizarro, J. (2004). Exploring
the myths of coping with a national trauma: A longitudinal study of responses to the September 11th
terrorist attacks. Journal of Aggression, Maltreatment & Trauma, 9, 129–141.
Simon, N. M., Otto, M. W., Wisniewski, S. R., Fossey, M., Sagduyu, K., Frank, E. et al. (2004). Anxiety
disorder comorbidity in bipolar disorder patients: Data from the first 500 participants in the
Trauma-Informed Care in Behavioral Health Services 3-97
Systematic Treatment Enhancement Program for Bipolar Disorder (STEP–BD). American Journal of
Psychiatry, 161, 2222–2229.
Simpson, T. L. (2002). Women’s treatment utilization and its relationship to childhood sexual abuse
history and lifetime PTSD. Substance Abuse, 23, 17–30.
Skinner, K. M., Kressin, N., Frayne, S., Tripp, T. J., Hankin, C. S., Miller, D. R. et al. (2000). The
prevalence of military sexual assault among female Veterans’ Administration outpatients. Journal of
Interpersonal Violence, 15, 291–310.
Skopp, N. A., Reger, M. A., Reger, G. M., Mishkind, M. C., Raskind, M., & Gahm, G. A. (2011). The role
of intimate relationships, appraisals of military service, and gender on the development of
posttraumatic stress symptoms following Iraq deployment. Journal of Traumatic Stress, 24, 277–286.
Slattery, S. M. & Goodman, L. A. (2009). Secondary traumatic stress among domestic violence advocates:
Workplace risk and protective factors. Violence Against Women, 15, 1358–1379.
Sleat, G. K., Ardolino, A. M., & Willett, K. M. (2011). Outcome measures in major trauma care: A review
of current international trauma registry practice. Emergency Medicine Journal, 28, 1008–1012.
Sledjeski, E. M., Speisman, B., & Dierker, L. C. (2008). Does number of lifetime traumas explain the
relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity
Survey–Replication (NCS–R). Journal of Behavioral Medicine, 31, 341–349.
Smid, G. E., Mooren, T. T., van der Mast, R. C., Gersons, B. P., & Kleber, R. J. (2009). Delayed
posttraumatic stress disorder: Systematic review, meta-analysis, and meta–regression analysis of
prospective studies. Journal of Clinical Psychiatry, 70, 1572–1582.
Smid, G. E., van der Velden, P. G., Gersons, B. P. R., & Kleber, R. J. (2012). Late–onset posttraumatic
stress disorder following a disaster: A longitudinal study. Psychological Trauma: Theory, Research,
Practice, and Policy, 4, 312–322.
Smid, G. E., van der Velden, P. G., Lensvelt-Mulders, G. J., Knipscheer, J. W., Gersons, B. P., & Kleber,
R. J. (2011). Stress sensitization following a disaster: A prospective study. Psychological Medicine,
1–12.
Smith, A. J., Kleijn, W. C., Trijsburg, R. W., & Hutschemaekers, G. J. (2007). How therapists cope with
clients’ traumatic experiences. Torture., 17, 203–215.
Smith, B. W., Ortiz, J. A., Steffen, L. E., Tooley, E. M., Wiggins, K. T., Yeater, E. A. et al. (2011).
Mindfulness is associated with fewer PTSD symptoms, depressive symptoms, physical symptoms,
and alcohol problems in urban firefighters. Journal of Consulting and Clinical Psychology, 79, 613–
617.
Smith, D. W., Christiansen, E. H., Vincent, R. D., & Hann, N. E. (1999). Population effects of the
bombing of Oklahoma City. Journal of the Oklahoma State Medical Association, 92, 193–198.
Smith, M. E. (2005). Bilateral hippocampal volume reduction in adults with post-traumatic stress disorder:
A meta-analysis of structural MRI studies. Hippocampus, 15, 798–807.
Smith, M. W., Schnurr, P. P., & Rosenheck, R. A. (2005). Employment outcomes and PTSD symptom
severity. Mental Health Services Research, 7, 89–101.
3-98 Part 3, Section 3—General Bibliography
Smith, T. C., Wingard, D. L., Ryan, M. A., Kritz-Silverstein, D., Slymen, D. J., & Sallis, J. F. (2008). Prior
assault and posttraumatic stress disorder after combat deployment. Epidemiology, 19, 505–512.
Smith-Osborne, A. (2009). Mental health risk and social ecological variables associated with educational
attainment for gulf war veterans: Implications for veterans returning to civilian life. American Journal
of Community Psychology, 44, 327–337.
Smyth, J. M., Hockemeyer, J. R., & Tulloch, H. (2008). Expressive writing and post-traumatic stress
disorder: Effects on trauma symptoms, mood states, and cortisol reactivity. British Journal of Health
Psychology, 13, 85–93.
Solomon, E. P. & Heide, K. M. (2005). The biology of trauma. Journal of Interpersonal Violence, 20, 51–
60.
Solomon, Z., Dekel, R., & Mikulincer, M. (2008). Complex trauma of war captivity: A prospective study
of attachment and post-traumatic stress disorder. Psychological Medicine: A Journal of Research in
Psychiatry and the Allied Sciences, 38, 1427–1434.
Sommer, C. A. (2008). Vicarious traumatization, trauma-sensitive supervision, and counselor preparation.
Counselor Education and Supervision, 48, 61–71.
Söndergaard, H. P. & Theorell, T. (2004). Language acquisition in relation to cumulative posttraumatic
stress disorder symptom load over time in a sample of re-settled refugees. Psychotherapy and
Psychosomatics, 73, 320–323.
Sotero, M. (2006). A conceptual model of historical trauma: Implications for public health practice and
research. Journal of Health Disparities Research and Practice, 1, 93–108.
Southwick, S. M., Litz, B. T., Charney, D., & Friedman, M. (2011). Resilience and mental health:
Challenges across the lifespan. Cambridge England: Cambridge University Press.
Spasojevic, J., Heffer, R. W., & Snyder, D. K. (2000). Effects of posttraumatic stress and acculturation on
marital functioning in Bosnian refugee couples. Journal of Traumatic Stress, 13, 205–217.
Spataro, J., Mullen, P. E., Burgess, P. M., Wells, D. L., & Moss, S. A. (2004). Impact of child sexual abuse
on mental health: Prospective study in men and women. British Journal of Psychiatry, 184, 416–421.
Spates, C. R., Koch, E., Cusack, K., Pagoto, S., & Waller, S. (2009). Eye movement desensitization and
reprocessing. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments
for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.)
(pp. 279–305). New York: Guilford Press.
Spauwen, J., Krabbendam, L., Lieb, R., Wittchen, H. U., & van Os, J.,(2006). Impact of psychological
trauma on the development of psychotic symptoms: Relationship with psychosis proneness. British
Journal of Psychiatry, 188, 527–533.
Spira, J. L., Pyne, J. M., & Wiederhold, B. K. (2007). Experiential methods in the treatment of combat
PTSD. In C. R. Figley & W. P. Nash (Eds.), Combat stress injury: Theory, research, and
management (pp. 205–218). New York: Routledge/Taylor & Francis Group.
Spitzer, C., Vogel, M., Barnow, S., Freyberger, H. J., & Grabe, H. J. (2007). Psychopathology and
alexithymia in severe mental illness: The impact of trauma and posttraumatic stress symptoms.
European Archives of Psychiatry and Neurological Sciences, 257, 191–196.
Trauma-Informed Care in Behavioral Health Services 3-99
Spitzer, R. L., First, M. B., & Wakefield, J. C. (2007). Saving PTSD from itself in DSM-V. Journal of
Anxiety Disorders, 21, 233–241.
Spitzer, R. L., Rosen, G. M., & Lilienfeld, S. O. (2008). Revisiting the Institute of Medicine report on the
validity of posttraumatic stress disorder. Comprehensive Psychiatry, 49, 319–320.
Spitzer, R. L., Williams, J. B., & Gibbon, M. (1987). Structured clinical interview for DSM-III-R—Patient
version (SCID-P). New York: New York State Psychiatric Institute, Biometrics Research.
Splevins, K. A., Cohen, K., Joseph, S., Murray, C., & Bowley, J. (2010). Vicarious posttraumatic growth
among interpreters. Qualitative Health Research, 20, 1705–1716.
Sprang, G., Clark, J. J., & Whitt-Woosley, A. (2007). Compassion fatigue, compassion satisfaction, and
burnout: Factors impacting a professional’s quality of life. Journal of Loss and Trauma, 12, 259–280.
Stallard, P., Velleman, R., Salter, E., Howse, I., Yule, W., & Taylor, G. (2006). A randomised controlled
trial to determine the effectiveness of an early psychological intervention with children involved in
road traffic accidents. Journal of Child Psychology and Psychiatry, 47, 127–134.
Stamm, B. H. (1997). Work Related Secondary Traumatic Stress. PTSD Research Quarterly, 8, 1–3.
Stamm, B. H. (2009). Professional Quality of Life: Compassion Satisfaction and Fatigue Version 5
(ProQOL) Pocatello, ID: ProQOL.org.
Stamm, B. H. & Figley, C. R. (1996). Compassion satisfaction and fatigue test. Pocatello, ID: Idaho State
University.Stamm, H. & Friedman, M. (2000). Cultural diversity in the appraisal and expression of
trauma. In A. Y. Shalev, R. Yehuda, & A. C. McFarlane (Eds.), International handbook of human
response to trauma (pp. 69–85). New York: Kluwer Academic/Plenum Publishers.
Stamm, B. H. & Hudnall, A. C. (2006). Telecommuting to support workers in disasters. In Psychological
interventions in times of crisis (pp. 99–118). New York: Springer Publishing Publishing Co.
Starr, A. J., Smith, W. R., Frawley, W. H., Borer, D. S., Morgan, S. J., Reinert, C. M. et al. (2004).
Symptoms of posttraumatic stress disorder after orthopaedic trauma. Journal of Bone and Joint
Surgery, 86–A, 1115–1121.
Steel, J. L., Dunlavy, A. C., Stillman, J., & Pape, H. C. (2011). Measuring depression and PTSD after
trauma: Common scales and checklists. Injury, 42, 288–300.
Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van Os, M. (2009). Association of torture
and other potentially traumatic events with mental health outcomes among populations exposed to
mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302, 537–549.
Steil, R., Jung, K., & Stangier, U. (2011). Efficacy of a two-session program of cognitive restructuring and
imagery modification to reduce the feeling of being contaminated in adult survivors of childhood
sexual abuse: A pilot study. Journal of Behavior Therapy and Experimental Psychiatry, 42, 325–329.
Stein, B. D., Elliott, M. N., Jaycox, L. H., Collins, R. L., Berry, S. H., Klein, D. J. et al. (2004). A national
longitudinal study of the psychological consequences of the September 11, 2001 terrorist attacks:
Reactions, impairment, and help–seeking. Psychiatry, 67, 105–117.
Stein, D. J. & Ipser, J. C. (2011). Pharmacotherapy of PTSD. In D. J. Stein, M. J. Friedman, & C. Blanco
(Eds.), Post-traumatic stress disorder (pp. 149–162). Chichester, UK: John Wiley and Sons, Inc.
3-100 Part 3, Section 3—General Bibliography
Stein, D. J., Chiu, W. T., Hwang, I., Kessler, R. C., Sampson, N., Alonso, J. et al. (2010). Cross-national
analysis of the associations between traumatic events and suicidal behavior: Findings from the WHO
World Mental Health Surveys. PLoS ONE, 5.
Stein, D. J., Friedman, M. J., & Blanco, C. (2011). Post-traumatic stress disorder. Chichester, UK: John
Wiley and Sons, Inc.
Stein, D. J., Ipser, J. C., & Seedat, S. (2006). Pharmacotherapy for post traumatic stress disorder (PTSD).
Cochrane Database of Systematic Reviews, CD002795.
Stein, D. J., Ipser, J., & McAnda, N. (2009). Pharmacotherapy of posttraumatic stress disorder: A review
of meta-analyses and treatment guidelines. CNS Spectrums, 14, 25–31.
Stein, M. B. (2011). Dire need for new PTSD pharmacotherapeutics. In D. J. Stein, M. J. Friedman, & C.
Blanco (Eds.), Post-traumatic stress disorder (pp. 167–170). Chichester, UK: John Wiley and Sons,
Inc.
Stein, M. B., Roy-Byrne, P. P., Craske, M. G., Bystritsky, A., Sullivan, G., Pyne, J. M. et al. (2005).
Functional impact and health utility of anxiety disorders in primary care outpatients. Medical Care,
43, 1164–1170.
Stein, M. B., Walker, J. R., Hazen, A. L., & Forde, D. R. (1997). Full and partial posttraumatic stress
disorder: Findings from a community survey. American Journal of Psychiatry, 154, 1114–1119.
Stewart, R. E. & Chambless, D. L. (2009). Cognitive–behavioral therapy for adult anxiety disorders in
clinical practice: A meta-analysis of effectiveness studies. Journal of Consulting and Clinical
Psychology, 77, 595–606.
Stewart, S. (2005). Suicidality, interpersonal trauma and cultural diversity: A review of the literature.
AeJAMH (Australian e-Journal for the Advancement of Mental Health), 4(2).
Stewart, S. H. & Conrod, P. J. (2003). Psychosocial models of functional associations between
posttraumatic stress disorder and substance use disorder. In P. Ouimette & P. J. Brown (Eds.),
Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders (pp. 29–
55). Washington, DC: American Psychological Association.
Stewart, S. H., Ouimette, P. C., & Brown, P. J. (2002). Gender and the comorbidity of PTSD with
substance use disorders. In R. Kimerling, P. C. Ouimette, & J. Wolfe (Eds.), Gender and PTSD (pp.
233–270). New York: Guilford Press.
Stinson, F. S., Dawson, D. A., Goldstein, R. B., Chou, S. P., Huang, B., Smith, S. M. et al. (2008).
Prevalence, correlates, disability, and comorbidity of DSM-IV narcissistic personality disorder:
Results from the Wave 2 National Epidemiologic Survey on alcohol and related conditions. Journal
of Clinical Psychiatry, 69, 1033–1045.
Stirman, S. W. (2008). The applicability of randomized controlled trials of psychosocial treatments for
PTSD to a veteran population. Journal of Psychiatric Practice, 14, 199–208.
Stockdale, S. E., Wells, K. B., Tang, L., Belin, T. R., Zhang, L., & Sherbourne, C. D. (2007). The
importance of social context: Neighborhood stressors, stress-buffering mechanisms, and alcohol,
drug, and mental health disorders. Social Science & Medicine, 65, 1867–1881.
Stokols, D. (1996). Translating social ecological theory into guidelines for community health promotion.
American Journal of Health Promotion, 10, 282–298.
Trauma-Informed Care in Behavioral Health Services 3-101
Stover, C. S. (2005). Domestic violence research: What have we learned and where do we go from here?
Journal of Interpersonal Violence, 20, 448–454.
Stride, S., Geffner, R., & Lincoln, A. (2009). The physiological and traumatic effects of childhood
exposure to intimate partner violence. In R. Geffner, D. Griffin, & J. Lewis, III (Eds.), Children
exposed to violence: Current issues, interventions and research (pp. 80–97). New York:
Routledge/Taylor & Francis Group.
Subcommittee on Posttraumatic Stress Disorder of the Committee on Gulf War and Health: Physiologic,
Psychologic, and Psychosocial Effects of Deployment-Related Stress (2006). Posttraumatic stress
disorder: Diagnosis and assessment. Washington, DC: The National Academies Press.
Substance Abuse and Mental Health Services Administration (2007). Prolonged exposure therapy for
posttraumatic stress disorders. Rockville, MD: Substance Abuse and Mental Health Services
Adminsitration.
Substance Abuse and Mental Health Services Administration (2010). Eye movement desensitization and
reprocessing. Rockville, MD: Substance Abuse and Mental Health Services Adminstration.
Substance Abuse and Mental Health Services Administration (2011). Leading change: A plan for
SAMHSA’s roles and actions 2011 – 2014 . Rockville, MD: Substance Abuse and Mental Health
Services Adminstration.
Substance Abuse and Mental Health Services Administration. (2011a). Addressing viral hepatitis in people
with substance use disorders. Treatment Improvement Protocol (TIP) Series 53. (HHS Publication
No. SMA 11-4656). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (2011b). Managing chronic pain in adults
with or in recovery from substance use disorders. Treatment Improvement Protocol (TIP) Series 54.
(HHS Publication No. SMA 11-4661). Rockville, MD: Substance Abuse and Mental Health Services
Administration.
Substance Abuse and Mental Health Services Administration. (2013a). Addressing the specific behavioral
health needs of men. Treatment Improvement Protocol (TIP) Series 56. (HHS Publication No. SMA
13-4736). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (2013b). Behavioral health services for
people who are homeless. Treatment Improvement Protocol (TIP) Series 55. (HHS Publication No.
SMA 13-4734). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned a). Behavioral health services:
Building health, wellness, and quality of life for sustained recovery. Treatment Improvement Protocol
(TIP) Series. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned b). Behavioral health services for
American Indians and Alaska Natives. Treatment Improvement Protocol (TIP) Series. Rockville, MD:
Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned c). Improving cultural competence.
Treatment Improvement Protocol (TIP) Series. Rockville, MD: Substance Abuse and Mental Health
Services Administration.
3-102 Part 3, Section 3—General Bibliography
Substance Abuse and Mental Health Services Administration. (planned d). Managing anxiety symptoms in
behavioral health services. Treatment Improvement Protocol (TIP) Series. Rockville, MD: Substance
Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned e). Relapse prevention and
recovery promotion in behavioral health services. Treatment Improvement Protocol (TIP) Series.
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned f). Reintegration-related
behavioral health issues in veterans and military families. Treatment Improvement Protocol (TIP)
Series. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (planned h). Using telephone- and Web-
based technologies in behavioral health settings. Treatment Improvement Protocol (TIP) Series.
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration, Center for Mental Health Services (2007).
Promotion and prevention in mental health: Strengthening parenting and enhancing child resilience.
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration & Office of Applied Studies (2008). Impact
of hurricanes Katrina and Rita on substance use and mental health. (Rep. No. January 31). Rockville,
MD: Substance Abuse and Mental Health Services Administration & Office of Applied Studies.
Substance Abuse and Mental Health Services Administration, Trauma and Justice Strategic Initiative
(2012). SAMHSA's working definition of trauma and guidance for trauma-informed approach.
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Sudaryo, M. K., Besral, Endarti, A. T., Rivany, R., Phalkey, R., Marx, M. et al. (2012). Injury, disability
and quality of life after the 2009 earthquake in Padang, Indonesia: A prospective cohort study of adult
survivors. Global Health Action, 5.
Sullivan, G. M. & Neria, Y. (2009). Pharmacotherapy in post-traumatic stress disorder: Evidence from
randomized controlled trials. Current Opinion in Investigational Drugs, 10, 35–45.
Sullivan, P. M. & Knutson, J. F. (2000). Maltreatment and disabilities: A population-based
epidemiological study. Child Abuse & Neglect, 24, 1257–1273.
Summey, J. R. (2001). The prevention, treatment and mitigation of secondary traumatic stress in
emergency personnel dealing with disasters. Annals of the American Psychotherapy Assn, 4, 18–21.
Sumter, M. (2006). Domestic violence and diversity: A call for multucultural services. Journal of Health
and Human Services Administration, 29, 173–190.
Suris, A., Lind, L., Kashner, T. M., & Borman, P. D. (2007). Mental health, quality of life, and health
functioning in women veterans: Differential outcomes associated with military and civilian sexual
assault. Journal of Interpersonal Violence, 22, 179–197.
Suvak, M., Maguen, S., Litz, B. T., Silver, R. C., & Holman, E. A. (2008). Indirect exposure to the
September 11 terrorist attacks: Does symptom structure resemble PTSD? Journal of Traumatic
Stress, 21, 30–39.
Swarbrick, M. (2006). A wellness approach. Psychiatric Rehabilitation Journal, 29, 311–314.
Trauma-Informed Care in Behavioral Health Services 3-103
Swinbourne, J. M. & Touyz, S. W. (2007). The co-morbidity of eating disorders and anxiety disorders: A
review. European Eating Disorders Review, 15, 253–274.
Symes, L., McFarlane, J., Frazier, L., Henderson-Everhardus, M. C., McGlory, G., Watson, K. B. et al.
(2010). Exploring violence against women and adverse health outcomes in middle age to promote
women’s health. Critical Care Nursing Quarterly, 33, 233–243.
Taft, C. T., Vogt, D. S., Mechanic, M. B., & Resick, P. A. (2007). Posttraumatic stress disorder and
physical health symptoms among women seeking help for relationship aggression. Journal of Family
Psychology, 21, 354–362.
Taft, C. T., Walling, S. M., Howard, J. M., & Monson, C. (2011). Trauma, PTSD, and partner violence in
military families. In Risk and resilience in U.S. military families (pp. 195–212). New York: Springer
Publishing Science + Business Media.
Tagay, S., Herpertz, S., Langkafel, M., & Senf, W. (2005). Posttraumatic stress disorder in a
psychosomatic outpatient clinic. Gender effects, psychosocial functioning, sense of coherence, and
service utilization. Journal of Psychosomatic Research, 58, 439–446.
Tam, T. W., Zlotnick, C., & Robertson, M. J. (2003). Longitudinal perspective: Adverse childhood events,
substance use, and labor force participation among homeless adults. American Journal of Drug and
Alcohol Abuse, 29, 829–846.
Tanielian, T. & Jaycox, L. H. (2008). Invisible wounds of war: Psychological and cognitive injuries, their
consequences, and services to assist recovery. Santa Monica, CA: RAND Corporation.
Tanielian, T. L., Jaycox, L. H., Schell, T. L., Marshall, G. N., Burnam, M. A., Eibner, C. et al. (2008).
Invisible wounds of war: Summary and recommendations for addressing psychological and cognitive
injuries. Santa Monica, CA: RAND Corporation.
Tarakeshwar, N., Hansen, N. B., Kochman, A., Fox, A., & Sikkema, K. J. (2006). Resiliency among
individuals with childhood sexual abuse and HIV: Perspectives on addressing sexual trauma. Journal
of Traumatic Stress, 19, 449–460.
Taylor, B., Irving, H. M., Kanteres, F., Room, R., Borges, G., Cherpitel, C. et al. (2010). The more you
drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption
and injury or collision risk increase together. Drug and Alcohol Dependence, 110, 108–116.
Taylor, L. A., Kreutzer, J. S., Demm, S. R., & Meade, M. A. (2003). Traumatic brain injury and substance
abuse: A review and analysis of the literature. Neuropsychological Rehabilitation, 13, 165–188.
Teicher, M. H. (2002). Scars that won’t heal: The neurobiology of child abuse. Scientific American, 286,
68–75.
Teplin, L. A., McClelland, G. M., Abram, K. M., & Weiner, D. A. (2005). Crime victimization in adults
with severe mental illness: Comparison with the National Crime Victimization Survey. Archives of
General Psychiatry, 62, 911–921.
Terrio, H. P., Nelson, L. A., Betthauser, L. M., Harwood, J. E., & Brenner, L. A. (2011). Postdeployment
traumatic brain injury screening questions: Sensitivity, specificity, and predictive values in returning
soldiers. Rehabilitation Psychology, 56, 26–31.
The APSAC handbook on child maltreatment (2nd ed.) (2002). Thousand Oaks, CA: Sage Publications,
Inc.
3-104 Part 3, Section 3—General Bibliography
The National Child Traumatic Stress Network (2012). Psychological first aid. Los Angeles, CA: National
Child Traumatic Stess Network.
Thompson, E. M. & Abel, W. D. (2009). Risk and protective factors in the development of post-traumatic
stress disorder symptoms among a cohort of students in two tertiary institutions post Hurricane Ivan.
West Indian Medical Journal, 58, 179–180.
Thompson, M. P. & Kingree, J. B. (1998). The frequency and impact of violent trauma among pregnant
substance abusers. Addictive Behaviors, 23, 257–262.
Thompson, R. A. (2004). Crisis intervention and crisis management: Strategies that work in schools and
communities. New York: Brunner-Routledge.
Thorp, S. R. & Stein, M. B. (2005). Posttraumatic stress disorder and functioning. PTSD Research
Quarterly, 16, 1–7.
Tjaden, P. & Thoennes, N. (2000). Extent, nature, and consequences of intimate partner violence.
Washington, DC: U.S. Department of Justice.
Tolin, D. F. & Foa, E. B. (2006). Sex differences in trauma and posttraumatic stress disorder: A
quantitative review of 25 years of research. Psychological Bulletin, 132, 959–992.
Torchalla, I., Nosen, L., Rostam, H., & Allen, P. (2012). Integrated treatment programs for individuals
with concurrent substance use disorders and trauma experiences: A systematic review and meta-
analysis. Journal of Substance Abuse Treatment, 42, 65–77.
Torchalla, I., Strehlau, V., Li, K., Schuetz, C., & Krausz, M. (2012). The association between childhood
maltreatment subtypes and current suicide risk among homeless men and women. Child
Maltreatment, 17, 132–143.
Toumbourou, J. W., Hemphill, S. A., Tresidder, J., Humphreys, C., Edwards, J., & Murray, D. (2007).
Mental health promotion and socio–economic disadvantage: Lessons from substance abuse, violence
and crime prevention and child health. Health Promotion Journal of Australia, 18, 184–190.
Toussaint, D. W., VanDeMark, N. R., Bornemann, A., & Graeber, C. J. (2007). Modifications to the
trauma recovery and empowerment model (TREM) for substance-abusing women with histories of
violence: Outcomes and lessons learned at a Colorado substance abuse treatment center. Journal of
Community Psychology, 35, 879–894.
Trauma (2012). Retrieved July 5, 2013, from: http://www.merriam-webster.com/dictionary/trauma
Treating compassion fatigue (2002). New York: Brunner-Routledge.
Treating complex traumatic stress disorders: An evidence-based guide (2009). New York: Guilford Press.
Tri-County Mental Health Services (2008). You and TRI County: Consumer rights and concerns.
Lewiston, ME: Tri-County Mental Health Services.
Triffleman, E. (2000). Gender differences in a controlled pilot study of psychosocial treatment in
substance dependent patients with post-traumatic stress disorder: Design considerations and
outcomes. Alcoholism Treatment Quarterly, 18, 113–126.
Triffleman, E. (2002). Implementing substance dependence posttraumatic stress disorder therapy in a
community-based methadone clinic. In J. L. Sorensen, R. A. Rawson, J. Guydish, & J. E. Zweben
Trauma-Informed Care in Behavioral Health Services 3-105
(Eds.), Research to practice, practice to research: Promoting scientific clinical interchange in drug
abuse treatment. (pp. 227–248). Washington, DC: American Psychological Association.
Triffleman, E. (2003). Issues in implementing posttraumatic stress disorder treatment outcome research in
community-based treatment programs. In J. L. Sorensen, R. A. Rawson, J. Guydish, & J. E. Zweben
(Eds.), Drug abuse treatment through collaboration: Practice and research partnerships that work
(pp. 227–247). American Psychological Association: Washington.
Triffleman, E. G. & Pole, N. (2010). Future directions in studies of trauma among ethnoracial and sexual
minority samples: Commentary. Journal of Consulting and Clinical Psychology, 78, 490–497.
Triffleman, E. G., Marmar, C. R., Delucchi, K. L., & Ronfeldt, H. (1995). Childhood trauma and
posttraumatic stress disorder in substance abuse inpatients. Journal of Nervous & Mental Disease,
183, 172–176.
Trippany, R. L., Kress, V. E. W., & Wilcoxon, S. A. (2004). Preventing vicarious trauma: What counselors
should know when working with trauma survivors. Journal of Counseling & Development, 82, 31–
37.
Trippany, R. L., Wilcoxon, S. A., & Satcher, J. F. (2003). Factors influencing vicarious traumatization for
therapists of survivors of sexual victimization. Journal of Trauma Practice, 2, 47–60.
Truman, J. L. (2011). Criminal Victimization, 2010.
Tsakanikos, E., Bouras, N., Costello, H., & Holt, G. (2007). Multiple exposure to life events and clinical
psychopathology in adults with intellectual disability. Social Psychiatry and Psychiatric
Epidemiology, 42, 24–28.
Tucker, P. & Trautman, R. (2000). Understanding and treating PTSD: Past, present, and future. Bulletin of
the Menninger Clinic, 64, A37–A51.
Tucker, P. M., Pfefferbaum, B., North, C. S., Kent, A., Burgin, C. E., Parker, D. E. et al. (2007).
Physiologic reactivity despite emotional resilience several years after direct exposure to terrorism.
The American Journal of Psychiatry, 164, 230–235.
Tull, M. T., Gratz, K. L., Aklin, W. M., & Lejuez, C. W. (2010). A preliminary examination of the
relationships between posttraumatic stress symptoms and crack/cocaine, heroin, and alcohol
dependence. Journal of Anxiety Disorders, 24, 55–62.
Tummala-Narra, P. (2007). Conceptualizing trauma and resilience across diverse contexts: A multicultural
perspective. Journal of Aggression, Maltreatment & Trauma, 14, 33–53.
Turnbull, G. J. (1998). A review of post-traumatic stress disorder; part I: Historical development and
classification. Injury, 29, 87–91.
Twamley, E. W., Allard, C. B., Thorp, S. R., Norman, S. B., Cissell, S. H., Berardi, K. H. et al. (2009).
Cognitive impairment and functioning in PTSD related to intimate partner violence. Journal of the
International Neuropsychological Society, 15, 879–887.
U.S. Committee For Refugees and Immigrants (2006). World Refugee Survey 2006: Risks and rights.
Washington, DC: U.S. Committee for Refugees and Immigrants.
U.S. Committee For Refugees and Immigrants (2009). World Refugee Survey: 2009. Washington, DC:
U.S. Committee for Refugees and Immigrants.
3-106 Part 3, Section 3—General Bibliography
U.S. Department of Health and Human Services (2003). Developing cultural competence in disaster
mental health programs: Guiding principles and recommendations. (Rep. No. HHS Pub. No. SMA
3828). Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health
Services Administration.
U.S. Department of Health and Human Services, Administration for Children and Families,
Administration on Children, Youth and Families, Children’s Bureau. (2010). Child maltreatment
2008. Washington, DC: U.S. Government Printing Office.
U.S. Department of Health and Human Services, Administration for Children and Families,
Administration on Children, Youth and Families, Children’s Bureau. (2011). Child maltreatment
2010. Washington, DC: U. S. Government Printing Office.
U.S. Department of Health and Human Services, Health Resources and Services Administration (2006).
Model trauma system: Planning and evaulation. Washington, DC: U.S. Department of Health and
Human Services.
U.S. Department of Housing and Urban Development & Office of Community Planning and Development
(2007). The annual homeless assessment report to Congress. Washington, DC: U.S. Department of
Housing and Urban Development.
U.S. Department of Justice (2010). Criminal victimization in the United States, 2008: Statistical Tables.
Washington, DC: U. S. Department of Justice.
U.S. Fire Administration (2007). I-35W bridge collapse and response. Washington, DC: U.S. Department
of Homeland Security.
Ullman, S. E. & Filipas, H. H. (2001). Predictors of PTSD symptom severity and social reactions in sexual
assault victims. Journal of Traumatic Stress, 14, 369–389.
Ullman, S. E., Filipas, H. H., Townsend, S. M., & Starzynski, L. L. (2007). Psychosocial correlates of
PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress, 20, 821–831.
Ulmer, C. S., Edinger, J. D., & Calhoun, P. S. (2011). A multi-component cognitive–behavioral
intervention for sleep disturbance in veterans with PTSD: A pilot study. Journal of Clinical Sleep
Medicine, 7, 57–68.
Unger, W. S., Wattenberg, M. S., Foy, D. W., & Glynn, S. M. (2006). Trauma-focus group therapy: An
evidence-based group approach to trauma with adults. In L. A. Schein, H. I. Spitz, G. M. Burlingame,
& P. R. Muskin (Eds.), Psychological effects of catastrophic disasters: Group approaches to
treatment (pp. 731–786). New York: Haworth Press.
United States Department of Veterans Affairs, National Center for PTSD (2011). Mental health effects
following disaster: Risk and resilience factors. White River Junction, VT: National Center for PTSD.
University of South Florida, College of Behavioral and Community Sciences (2012). Creating trauma-
informed care environments: An organizational self-assessment.Tampa, FL: Central Florida
Behavioral Health Network.
Uomoto, J. M. & Williams, R. M. (2009). Post-acute polytrauma rehabilitation and integrated care of
returning veterans: Toward a holistic approach. Rehabilitation Psychology, 54, 259–269.
Trauma-Informed Care in Behavioral Health Services 3-107
Updegraff, J. A., Silver, R. C., & Holman, E. A. (2008). Searching for and finding meaning in collective
trauma: Results from a national longitudinal study of the 9/11 terrorist attacks. Journal of Personality
and Social Psychology, 95, 709–722.
Urlic, I. & Simunkovic, G. T. (2009). Working through shame in groups for victims of trauma and war.
International Journal of Group Psychotherapy, 59, 165–178.
Urquiza, A. J. & Goodlin–Jones, B. L. (1994). Child sexual abuse and adult revictimization with women of
color. Violence and Victims, 9, 223–232.
Vaishnavi, S., Connor, K., & Davidson, J. R. T. (2007). An abbreviated version of the Connor–Davidson
Resilience Scale (CD–RISC), the CD–RISC2: Psychometric properties and applications in
psychopharmacological trials. Psychiatry Research, 152, 293–297.
Valdez, C., Kimerling, R., Hyun, J. K., Mark, H. F., Saweikis, M., & Pavao, J. (2011). Veterans Health
Administration mental health treatment settings of patients who report military sexual trauma.
Journal of Trauma & Dissociation, 12, 232–243.
Valent, P. (2002). Diagnosis and treatment of helper stresses, traumas, and illnesses. In C. R. Figley (Ed.),
Treating compassion fatigue (pp. 17–38). New York: Brunner-Routledge.
Valentiner, D. P., Foa, E. B., Riggs, D. S., & Gershuny, B. S. (1996). Coping strategies and posttraumatic
stress disorder in female victims of sexual and nonsexual assault. Journal of Abnormal Psychology,
105, 455–458.
Van Ameringen, M. & Patterson, B. (2011). Shortcomings and future directions of the pharmacotherapy of
PTSD. In D. J. Stein, M. J. Friedman, & C. Blanco (Eds.), Post-traumatic stress disorder (pp. 164–
166). Chichester, UK: John Wiley and Sons, Inc.
Van Breda, A. D. (2001). Resilience theory: A literature review. Pretoria, South Africa: South African
Military Health Service.
van den Berg, D. P. G. & van der Gaag, M. (2012). Treating trauma in psychosis with EMDR: A pilot
study. Journal of Behavior Therapy and Experimental Psychiatry, 43, 664–671.
van der Kolk, B. A., Herron, N., & Hostetler, A. (1994). The history of trauma in psychiatry. Psychiatric
Clinics of North America, 17, 583–600.
van der Kolk, B. A., McFarlane, A. C., & Van der Hart, O. (1996). A general approach to treatment of
posttraumatic stress disorder. In B. A. van der Kolk, A. C. McFarlane, & L. Weisaeth (Eds.),
Traumatic stress: The effects of overwhelming experience on mind, body, and society (pp. 417–440).
New York: Guilford Press.
van der Kolk, B. A., Spinazzola, J., Blaustein, M. E., Hopper, J. W., Hopper, E. K., Korn, D. L. et al.
(2007). A randomized clinical trial of eye movement desensitization and reprocessing (EMDR),
fluoxetine, and pill placebo in the treatment of posttraumatic stress disorder: Treatment effects and
long–term maintenance. Journal of Clinical Psychiatry, 68, 37–46.
van der Kolk, B., Roth, S., Pelcovitz, D., & Mandel, F. (1993). Complex PTSD: Results of the PTSD field
trials for DSM-IV. Washington, DC: American Psychiatric Association.
van der Velden, P. G. & Wittmann, L. (2008). The independent predictive value of peritraumatic
dissociation for PTSD symptomatology after type I trauma: A systematic review of prospective
studies. Clinical Psychology Review, 28, 1009–1020.
3-108 Part 3, Section 3—General Bibliography
van der Velden, P. G., Kleber, R., Fournier, M., Grievink, L., Drogendijk, A., & Gersons, B. P. R. (2007).
The association between dispositional optimism and mental health problems among disaster victims
and a comparison group: A prospective study. Journal of Affective Disorders, 102, 35–45.
Van Emmerik, A. A. P., Kamphuis, J. H., Hulsbosch, A. M., & Emmelkamp, P. M. G. (2002). Single
session debriefing after psychological trauma: A meta-analysis. Lancet, 360, 766–771.
Van, A. M., Mancini, C., Simpson, W., & Patterson, B. (2010). Potential use of Internet-based screening
for anxiety disorders: A pilot study. Depression and Anxiety, 27, 1006–1010.
VanDeusen, K. M. & Way, I. (2006). Vicarious trauma: An exploratory study of the impact of providing
sexual abuse treatment on clinicians’ trust and intimacy. Journal of Child Sexual Abuse, 15, 69–85.
Varra, A. A. & Follette, V. M. (2005). ACT with posttraumatic stress disorder. In S. C. Hayes (Ed.), A
practical guide to acceptance and commitment therapy (pp. 133–152). New York: Springer
Publishing Science + Business Media.
Vasterling, J. J., Verfaellie, M., & Sullivan, K. D. (2009). Mild traumatic brain injury and posttraumatic
stress disorder in returning veterans: Perspectives from cognitive neuroscience. Clinical Psychology
Review, 29, 674–684.
Vaughn, M. G., Fu, Q., DeLisi, M., Beaver, K. M., Perron, B. E., & Howard, M. O. (2010). Criminal
victimization and comorbid substance use and psychiatric disorders in the United States: Results from
the NESARC. Annals of Epidemiology, 20, 281–288.
Verger, P., Dab, W., Lamping, D. L., Loze, J. Y., Deschaseaux-Voinet, C., Abenhaim, L. et al. (2004). The
psychological impact of terrorism: An epidemiologic study of posttraumatic stress disorder and
associated factors in victims of the 1995–1996 bombings in France. The American Journal of
Psychiatry, 161, 1384–1389.
Vermetten, E. & Lanius, R. A. (2012). Biological and clinical framework for posttraumatic stress disorder.
Handb. Clin. Neurol., 106, 291–342.
Verschuur, M. J., Maric, M., & Spinhoven, P. (2010). Differences in changes in health-related anxiety
between Western and non–Western participants in a trauma-focused study. Journal of Traumatic
Stress, 23, 300–303.
Vest, J. R., Catlin, T. K., Chen, J. J., & Brownson, R. C. (2002). Multistate analysis of factors associated
with intimate partner violence. American Journal of Preventive Medicine, 22, 156–164.
Vickerman, K. A. & Margolin, G. (2009). Rape treatment outcome research: Empirical findings and state
of the literature. Clinical Psychology Review, 29, 431–448.
Villagonzalo, K. A., Dodd, S., Ng, F., Mihaly, S., Langbein, A., & Berk, M. (2011). The relationship
between substance use and posttraumatic stress disorder in a methadone maintenance treatment
program. Comprehensive Psychiatry, 52, 562–566.
Vlahov, D., Galea, S., Ahern, J., Resnick, H., & Kilpatrick, D. (2004). Sustained increased consumption of
cigarettes, alcohol, and marijuana Among Manhattan residents after September 11, 2001. American
Journal of Public Health, 94, 253–254.
Vo, N. M. (2006). The Vietnamese boat people, 1954 and 1975–1992. Jefferson, NC: McFarland &
Company.
Trauma-Informed Care in Behavioral Health Services 3-109
Vogt, D. S. & Tanner, L. R. (2007). Risk and resilience factors for posttraumatic stress symptomatology in
Gulf War I veterans. Journal of Traumatic Stress, 20, 27–38.
Vogt, D. S., King, D. W., & King, L. A. (2007). Risk pathways for PTSD: Making sense of the literature.
In M. J. Friedman, T. M. Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice
(pp. 99–115). New York: Guilford Press.
Vogt, D. S., Pless, A. P., King, L. A., & King, D. W. (2005). Deployment stressors, gender, and mental
health outcomes among Gulf War I veterans. Journal of Traumatic Stress, 18, 272–284.
Vogt, D., Bruce, T. A., Street, A. E., & Stafford, J. (2007). Attitudes toward women and tolerance for
sexual harassment among reservists. Violence Against Women, 13, 879–900.
Vogt, D., Vaughn, R., Glickman, M. E., Schultz, M., Drainoni, M. L., Elwy, R. et al. (2011). Gender
differences in combat-related stressors and their association with postdeployment mental health in a
nationally representative sample of U.S. OEF/OIF veterans. Journal of Abnormal Psychology, 120,
797–806.
Von Rueden, K. T., Hinderer, K. A., McQuillan, K. A., Murray, M., Logan, T., Kramer, B. et al. (2010).
Secondary traumatic stress in trauma nurses: Prevalence and exposure, coping, and
personal/environmental characteristics. Journal of Trauma Nursing, 17, 191–200.
Voss Horrell, S. C., Holohan, D. R., Didion, L. M., & Vance, G. T. (2011). Treating traumatized OEF/OIF
veterans: How does trauma treatment affect the clinician? Professional Psychology: Research and
Practice, 42, 79–86.
Waelde, L. C., Pennington, D., Mahan, C., Mahan, R., Kabour, M., & Marquett, R. (2010). Psychometric
properties of the Race-related Events Scale. Psychological trauma: Theory, research, practice, and
policy, 2, 4–11.
Wagner, K. D., Brief, D. J., Vielhauer, M. J., Sussman, S., Keane, T. M., & Malow, R. (2009). The
potential for PTSD, substance use, and HIV risk behavior among adolescents exposed to Hurricane
Katrina. Substance Use & Misuse, 44, 1749–1767.
Wagnild, G. M. & Young, H. M. (1993). Development and psychometric evaluation of the Resilience
Scale. Journal of Nursing Measurement, 1, 165–178.
Waldrop, A. E., Back, S. E., Verduin, M. L., & Brady, K. T. (2007). Triggers for cocaine and alcohol use
in the presence and absence of posttraumatic stress disorder. Addictive Behaviors, 32, 634–639.
Waldrop, A. E., Santa Ana, E. J., Saladin, M. E., McRae, A. L., & Brady, K. T. (2007). Differences in
early onset alcohol use and heavy drinking among persons with childhood and adulthood trauma. The
American Journal on Addictions, 16, 439–442.
Walker, R. L., Clark, M. E., & Sanders, S. H. (2010). The postdeployment multi-symptom disorder: An
emerging syndrome in need of a new treatment paradigm. Psychological Services, 7, 136–147.
Wall, T. (2009). Beyond survival: Facing the past, claiming the present. Cross Currents Vol.12 No.3.
Walser, R. D. & Westrup, D. (2007). Acceptance & commitment therapy for the treatment of post-
traumatic stress disorder & trauma-related problems: A practitioner’s guide to using mindfulness &
acceptance strategies. Oakland, CA: New Harbinger Publications.
3-110 Part 3, Section 3—General Bibliography
Walser, R. D. (2004). Disaster Response: Professional and Personal Journeys at the Pentagon New York:
The Association for the Advancement of Behavior Therapy.
Walsh, F. (2006). Strengthening family resilience (2nd ed.). New York: Guilford Press.
Walsh, F. (2007). Traumatic loss and major disasters: Strengthening family and community resilience.
Family Process, 46, 207–227.
Walsh, K., Blaustein, M., Knight, W. G., Spinazzola, J., & van der Kolk, B. A. (2007). Resiliency factors
in the relation between childhood sexual abuse and adulthood sexual assault in college-age women.
Journal of Child Sexual Abuse, 16, 1–17.
Walter, K. H., Horsey, K. J., Palmieri, P. A., & Hobfoll, S. E. (2010). The role of protective self-cognitions
in the relationship between childhood trauma and later resource loss. Journal of Traumatic Stress, 23,
264–273.
Wan, J. J., Morabito, D. J., Khaw, L., Knudson, M. M., & Dicker, R. A. (2006). Mental illness as an
independent risk factor for unintentional injury and injury recidivism. Journal of Trauma, 61, 1299–
1304.
Way, I., VanDeusen, K. M., & Cottrell, T. (2007). Vicarious trauma:predictors of clinicians’ disrupted
cognitions about self-esteem and self-intimacy. Journal of Child Sexual Abuse, 16, 81–98.
Way, I., VanDeusen, K. M., Martin, G., Applegate, B., & Jandle, D. (2004). Vicarious trauma: A
comparison of clinicians who treat survivors of sexual abuse and sexual offenders. Journal of
Interpersonal Violence, 19, 49–71.
Weathers, F. W., Keane, T. M., & Foa, E. B. (2009). Assessment and diagnosis of adults. In E. B. Foa, T.
M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines
from the International Society for Traumatic Stress Studies (2nd ed.) (pp. 23–61). New York:
Guilford Press.
Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993). The PTSD Checklist:
Reliability, validity, and & diagnostic utility. Paper presented at the Annual Meeting of the
International Society for Traumatic Stress Studies, San Antonio, TX, October.
Wee, D. F. (2007). Review of trauma and dissociation in a cross-cultural perspective: Not just a North
American phenomenon. Traumatology, 13, 39–40.
Weinbaum, Z., Stratton, T. L., Chavez, G., Motylewski-Link, C., Barrera, N., & Courtney, J. G. (2001).
Female victims of intimate partner physical domestic violence (IPP–DV), California 1998. American
Journal of Preventive Medicine, 21, 313–319.
Weine, S., Danieli, Y., Silove, D., Ommeren, M. V., Fairbank, J. A., & Saul, J. (2002). Guidelines for
international training in mental health and psychosocial interventions for trauma exposed populations
in clinical and community settings. Psychiatry, 65, 156–164.
Weine, S., Kulauzovic, Y., Klebic, A., Besic, S., Mujagic, A., Muzurovic, J. et al. (2008). Evaluating a
multiple–family group access intervention for refugees with PTSD. Journal of Marital and Family
Therapy, 34, 149–164.
Weiss, D. & Marmar, C. (1997). The Impact of Event Scale–revised. In J. Wilson & T. Keane (Eds.),
Assessing psychological trauma and PTSD. (pp. 399–411). New York: Guildford Press.
Trauma-Informed Care in Behavioral Health Services 3-111
Weiss, L., Fabri, A., McCoy, K., Coffin, P., Netherland, J., & Finkelstein, R. (2002). A vulnerable
population in a time of crisis: Drug users and the attacks on the World Trade Center. Journal of
Urban Health: Bulletin of the New York Academy of Medicine, 79, 392–403.
Weiss, T., Skelton, K., Phifer, J., Jovanovic, T., Gillespie, C. F., Smith, A. et al. (2011). Posttraumatic
stress disorder is a risk factor for metabolic syndrome in an impoverished urban population. General
Hospital Psychiatry, 33, 135–142.
Weissbecker, I. & Clark, C. (2007). The impact of violence and abuse on womens physical health: Can
trauma-informed treatment make a difference? Journal of Community Psychology, 35, 909–923.
Wenzel, S. L., Tucker, J. S., Elliott, M. N., Hambarsoomians, K., Perlman, J., Becker, K. et al. (2004).
Prevalence and co-occurrence of violence, substance use and disorder, and HIV risk behavior: A
comparison of sheltered and low-income housed women in Los Angeles County. Preventive
Medicine, 39, 617–624.
Wessely, S. (2003). The role of screening in the prevention of psychological disorders arising after major
trauma: Pros and cons. In Terrorism and disaster: Individual and community mental health
interventions (pp. 121–145). New York: Cambridge University Press.
Wessely, S., Bryant, R. A., Greenberg, N., Earnshaw, M., Sharpley, J., & Hughes, J. H. (2008). Does
psychoeducation help prevent posttraumatic psychological distress? Psychiatry: Interpersonal and
Biological Processes, 71, 287–302.
Westermeyer, J. (2004). Cross-cultural aspects of substance abuse. In M. Galanter & H. D. Kleber (Eds.),
The American Psychiatric Publishing textbook of substance abuse treatment (3rd. ed.) (pp. 89–98).
Washington, DC: American Psychiatric Publishing.
Westermeyer, J., Hollifield, M., Spring, M., Johnson, D., & Jaranson, J. (2011). Comparison of two
methods of inquiry for torture with East African refugees: Single query versus checklist. Torture., 21,
155–172.
Westphal, M., Olfson, M., Gameroff, M. J., Wickramaratne, P., Pilowsky, D. J., Neugebauer, R. et al.
(2011). Functional impairment in adults with past posttraumatic stress disorder: Findings from
primary care. Depression and Anxiety., 28, 686–695.
Whitbeck, L. B., Chen, X., Hoyt, D. R., & Adams, G. W. (2004). Discrimination, historical loss and
enculturation: Culturally specific risk and resiliency factors for alcohol abuse among American
Indians. Journal of Studies on Alcohol, 65, 409–418.
White, M. (2004). Narrative therapy. New Zealand: Massey University.
Whitfield, C. L., Anda, R. F., Dube, S. R., & Felitti, V. J. (2003). Violent childhood experiences and the
risk of intimate partner violence in adults: Assessment in a large health maintenance organization.
Journal of Interpersonal Violence, 18, 166–185.
Widom, C. S. & Morris, S. (1997). Accuracy of adult recollections of childhood victimization, Part 2:
Childhood sexual abuse. Psychological Assessment, 9, 34–46.
Widom, C. S., DuMont, K., & Czaja, S. J. (2007). A prospective investigation of major depressive disorder
and comorbidity in abused and neglected children grown up. Archives of General Psychiatry, 64, 49–
56.
3-112 Part 3, Section 3—General Bibliography
Wiechelt, S. A. & Gryczynski, J. (2012). Cultural and historical trauma among Native Americans. In S.
Ringel & J. R. Brandell (Eds.), Trauma: Contemporary directions in theory, practice, and research.
(pp. 191–222). Thousand Oaks, CA: Sage Publications.
Wilcox, J., Briones, D., & Suess, L. (1991). Auditory hallucinations, posttraumatic stress disorder, and
ethnicity. Comprehensive Psychiatry, 32, 320–323.
Wilkinson, D. M., Blacker, S. D., Richmond, V. L., Horner, F. E., Rayson, M. P., Spiess, A. et al. (2011).
Injuries and injury risk factors among British army infantry soldiers during predeployment training.
Injury Prevention, 17, 381–387.
Williams, L. M. (1994). Recall of childhood trauma: A prospective study of women’s memories of child
sexual abuse. Journal of Consulting and Clinical Psychology, 62, 1167–1176.
Wilson, D. R. (2010). Health consequences of childhood sexual abuse. Perspectives in Psychiatric Care,
46, 56–64.
Wilson, J. P. & Keane, T. M. (2004). Assessing psychological trauma and PTSD. (2nd ed.) New York:
Guilford Press.
Wilson, J. P. & Tang, C. S. (2007). Cross-cultural assessment of psychological trauma and PTSD. New
York: Springer Publishing.
Wilson, J. P. (2007). The lens of culture: Theoretical and conceptual perspectives in the assessment of
psychological trauma and PTSD. In J. P. Wilson & C. S. Tang (Eds.), Cross-cultural assessment of
psychological trauma and PTSD (pp. 3–30). New York: Springer Publishing Science + Business
Media.
Wilson, J. P. (2008). Culture, trauma, and the treatment of post-traumatic syndromes: A global
perspective. In A. J. Marsella, J. L. Johnson, P. Watson, & J. Gryczynski (Eds.), Ethnocultural
perspectives on disaster and trauma: Foundations, issues, and applications (pp. 351–375). New
York: Springer Publishing Science + Business Media.
Wingo, A. P., Wrenn, G., Pelletier, T., Gutman, A. R., Bradley, B., & Ressler, K. J. (2010). Moderating
effects of resilience on depression in individuals with a history of childhood abuse or trauma
exposure. Journal of Affective Disorders, 126, 411–414.
Wittchen, H. U., Schonfeld, S., Thurau, C., Trautmann, S., Galle, M., Mark, K. et al. (2012). Prevalence,
incidence and determinants of PTSD and other mental disorders: Design and methods of the PID–
PTSD+(3) study. International Journal of Methods in Psychiatric Research
Wolf, G. K., Reinhard, M., Cozolino, L. J., Caldwell, A., & Asamen, J. K. (2009). Neuropsychiatric
symptoms of complex posttraumatic stress disorder: A preliminary Minnesota Multiphasic
Personality Inventory scale to identify adult survivors of childhood abuse. Psychological Trauma:
Theory, Research, Practice, and Policy, 1, 49–64.
Wolfe, J. & Kimerling, R. (1997). Gender issues in the assessment of posttraumatic stress disorder. In J. P.
Wilson & T. M. Keane (Eds.), Assessing Psychological Trauma and PTSD (pp. 192–238). New York:
Guilford Press.
Wolpe, J. & Abrams, J. (1991). Post-traumatic stress disorder overcome by eye-movement desensitization:
A case report. Journal of Behavior Therapy and Experimental Psychiatry, 22, 39–43.
Wolpe, J. (1958). Psychotherapy by Reciprocal Inhibition. Stanford, CA: Stanford University Press.
Trauma-Informed Care in Behavioral Health Services 3-113
Wong, E. C., Schell, T. L., Marshall, G. N., Jaycox, L. H., Hambarsoomians, K., & Belzberg, H. (2009).
Mental health service utilization after physical trauma: The importance of physician referral. Medical
Care, 47, 1077–1083.
Wong, P. T. P. & Wong, L. C. J. (2006). Handbook of multicultural perspectives on stress and coping.
Dallas, TX: Spring Publications.
Woodhead, C., Rona, R. J., Iversen, A., MacManus, D., Hotopf, M., Dean, K. et al. (2011). Mental health
and health service use among post-national service veterans: Results from the 2007 Adult Psychiatric
Morbidity Survey of England. Psychological Medicine: A Journal of Research in Psychiatry and the
Allied Sciences, 41, 363–372.
Woods, S. J. (2005). Intimate partner violence and post-traumatic stress disorder symptoms in women:
what we know and need to know. Journal of Interpersonal. Violence, 20, 394–402.
Woodward, A. T., Taylor, R. J., Bullard, K. M., Aranda, M. P., Lincoln, K. D., & Chatters, L. M. (2011).
Prevalence of lifetime DSM-IV affective disorders among older African Americans, Black
Caribbeans, Latinos, Asians and non-Hispanic White people. International Journal of Geriatric
Psychiatry.
Woon, F. L. & Hedges, D. W. (2009). Amygdala volume in adults with posttraumatic stress disorder: A
meta-analysis. Journal of Neuropsychiatry and Clinical Neurosciences, 21, 5–12.
World Health Organization (1992). International statistical classification of diseases and related health
problems. (10th revision ed.) Geneva: World Health Organization.
Wrenn, G. L., Wingo, A. P., Moore, R., Pelletier, T., Gutman, A. R., Bradley, B. et al. (2011). The effect
of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients.
Journal of the National Medical Association, 103, 560–566.
Wright, D. C., Woo, W. L., Muller, R. T., Fernandes, C. B., & Kraftcheck, E. R. (2003). An investigation
of trauma-centered inpatient treatment for adult survivors of abuse. Child Abuse & Neglect, 27, 393–
406.
Wyatt, G. E., Guthrie, D., & Notgrass, C. M. (1992). Differential effects of women’s child sexual abuse
and subsequent sexual revictimization. Journal of Consulting and Clinical Psychology;Journal of
Consulting and Clinical Psychology, 60, 167–173.
Xian, H., Chantarujikapong, S. I., Scherrer, J. F., Eisen, S. A., Lyons, M. J., Goldberg, J. et al. (2000).
Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence
in twin pairs. Drug and Alcohol Dependence, 61, 95–102.
Xie, Y. & Greenman, E. (2005). Research report: Segmented assimilation theory: A reformulation and
empirical test. Ann Arbor, MI: University of Michigan.
Yanos, P. T., Czaja, S. J., & Widom, C. S. (2010). A prospective examination of service use by abused and
neglected children followed up into adulthood. Psychiatric Services, 61, 796–802.
Yehuda, R. & Flory, J. D. (2007). Differentiating biological correlates of risk, PTSD, and resilience
following trauma exposure. Journal of Traumatic Stress, 20, 435–447.
Yehuda, R. (2004). Risk and resilience in posttraumatic stress disorder. Journal of Clinical Psychiatry, 65
Supplement 1, 29–36.
3-114 Part 3, Section 3—General Bibliography
Yehuda, R., Bryant, R., Zohar, J., & Marmar, C. R. (2007). Neurobiological and behavioral consequences
of terrorism: Distinguishing normal from pathological responses, risk profiling, and optimizing
resilience. In B. Bongar, L. M. Brown, L. E. Beutler, J. N. Breckenridge, & P. G. Zimbardo (Eds.),
Psychology of terrorism (pp. 273–287). New York: Oxford University Press.
Yehuda, R., Halligan, S. L., & Bierer, L. M. (2001). Relationship of parental trauma exposure and PTSD
to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research, 35, 261–
270.
Yehuda, R., Halligan, S. L., & Grossman, R. (2001). Childhood trauma and risk for PTSD: Relationship to
intergenerational effects of trauma, parental PTSD, and cortisol excretion. Development and
Psychopathology, 13, 733–753.
Yellow Horse, S. & Brave Heart, M. Y. H. (2005). Chapter 3: Native American children. Colorado
Springs, CO: White Bison, Inc.
Yoder, M., Tuerk, P. W., Price, M., Grubaugh, A. L., Strachan, M., Myrick, H. et al. (2012). Prolonged
exposure therapy for combat-related posttraumatic stress disorder: Comparing outcomes for veterans
of different wars. Psychological Services, 9, 16–25.
Yoshioka, M. R. & Choi, D. Y. (2005). Culture and interpersonal violence research: Paradigm shift to
create a full continuum of domestic violence services. Journal of Interpersonal Violence, 20, 513–
519.
Young, B. H. (2006). The immediate response to disaster: Guidelines for adult psychological first aid. In
E.C.Ritchie, P. J. Watson, & M. J. Friedman (Eds.), Interventions following mass violence and
disasters: Strategies for mental health practice (pp. 134–154). New York: Guilford Press.
Young, L. (2009). Focus: “Hear me, don’t hurt me”: Survivors teach powerful lessons in trauma and
transformation. Cross Currents, 12.
Young, M. A. (2001). The community crisis response team training manual. Washington, DC: Office for
Victims of Crime.
Yuan, C., Wang, Z., Inslicht, S. S., McCaslin, S. E., Metzler, T. J., Henn–Haase, C. et al. (2011).
Protective factors for posttraumatic stress disorder symptoms in a prospective study of police officers.
Psychiatry Research, 188, 45–50.
Zatzick, D. F., Jurkovich, G. J., Gentilello, L., Wisner, D., & Rivara, F. P. (2002). Posttraumatic stress,
problem drinking, and functional outcomes after injury. Archives of Surgery, 137, 200–205.
Zayfert, C. & Becker, C. B. (2000). Implementation of empirically supported treatment for PTSD:
Obstacles and innovations. Behavior Therapist, 23, 161–168.
Zayfert, C. & DeViva, J. C. (2010). Avoiding treatment failures in PTSD. In Avoiding treatment failures in
the anxiety disorders (pp. 147–168). New York: Springer Publishing Science + Business Media.
Zemore, S. E. (2005). Re-examining whether and why acculturation relates to drinking outcomes in a
rigorous, national survey of Latinos. Alcoholism: Clinical & Experimental Research, 29, 2144–2153.
Zinzow, H. M., Resnick, H. S., Amstadter, A. B., McCauley, J. L., Ruggiero, K. J., & Kilpatrick, D. G.
(2010). Drug-or alcohol-facilitated, incapacitated, and forcible rape in relationship to mental health
among a national sample of women. Journal of Interpersonal Violence, 25, 2217–2236.
Trauma-Informed Care in Behavioral Health Services 3-115
Zivin, K., Bohnert, A. S. B., Mezuk, B., Ilgen, M. A., Welsh, D., Ratliff, S. et al. (2011). Employment
status of patients in the VA health system: Implications for mental health services. Psychiatric
Services, 62, 35–38.
Zoellner, L. A., Feeny, N. C., Eftekhari, A., & Foa, E. B. (2011). Changes in negative beliefs following
three brief programs for facilitating recovery after assault. Depression and Anxiety, 28, 532–540.
Zohar, J., Fostick, L., Cohen, A., Bleich, A., Dolfin, D., Weissman, Z. et al. (2009). Risk factors for the
development of posttraumatic stress disorder following combat trauma: A semiprospective study.
Journal of Clinical Psychiatry, 70, 1629–1635.
Zohar, J., Juven-Wetzler, A., Sonnino, R., Cwikel-Hamzany, S., Balaban, E., & Cohen, H. (2011). New
insights into secondary prevention in post-traumatic stress disorder. Dialogues in Clinical
Neuroscience, 13, 301–309.
Zohar, J., Sonnino, R., Juven-Wetzler, A., & Cohen, H. (2009). Can posttraumatic stress disorder be
prevented? CNS Spectrums, 14, 44–51.
Zweig, J. M., Yahner, J., & Rossman, S. B. (2012). Does recent physical and sexual victimization affect
further substance use for adult drug-involved offenders? Journal of Interpersonal Violence, 27(12),
2348–2372.
