
PROVIDING PHYSICAL THERAPY IN THE HOME
PROVIDING PHYSICAL THERAPY IN THE HOME
This comprehensive successor to the APTA Home Health Section’s popular
Guidelines for the Provision of Physical Therapy in the Home reflects the
expanding roles of physical therapists and physical therapist assistants in the
home health setting, changes in reassessment requirements, and increased
public accountability for best practices and positive patient experiences.
Providing Physical Therapy in the Home provides timely guidance to elevate the
quality of physical therapist services in the home care setting to the highest
levels, consistent with the Vision Statement of APTA:
Transforming society by optimizing movement to improve the human experience.
www.APTA.org
Providing
PHYSICAL THERAPY
in the Home
www.homehealthsection.org
P-131
1014/200

Providing
PHYSICAL THERAPY
in the Home

iv
Providing Physical Therapy in the Home
©2014 American Physical Therapy Association. All rights reserved. No part of this publication may
be reproduced in any form or by any means—electronic, mechanical, or information storage retrieval
system—without written permission from the American Physical Therapy Association.
For more information about this and other APTA publications, contact the American Physical
Therapy Association, 1111 North Fairfax Street, Alexandria, VA 22314. www.apta.org.
Publication P-131
ISBN: 978-1-931369-87-9
1014/200
Mention of specific brand names or products in this publication does not imply endorsement or
recommendation by APTA or the Home Health Section.

v
Table of Contents
TABLE OF CONTENTS
Preface ...................................................................vii
Chapter 1. Roles of the Physical Therapist in Home Health Care ........................1
Chapter 2. Roles of the Physical Therapist Assistant in Home Health Care ................9
Chapter 3. Qualifications ...................................................... 15
Chapter 4. Orientation to the Agency ............................................25
Chapter 5. Referral Information .................................................41
Chapter 6. Timely Scheduling of the Home Visits ...................................47
Chapter 7. Physical Therapy Admissions and Evaluations .............................53
Chapter 8. Physical Therapist Plan of Care ........................................65
Chapter 9. Physical Therapists as Case Managers ..................................71
Chapter 10. Documentation Requirements in Home Health Care .......................81
Chapter 11. Home Health Physical Therapy Supplies/Equipment and Infection Control .......95
Chapter 12. Discharge Planning ................................................103
Chapter 13. The Patient Experience .............................................109
Chapter 14. Lifelong Learning and Continuing Competence ...........................117
Chapter 15. Home Health Physical Therapist Practice Resources and Reference ...........125

vii
Acknowledgements
Special thanks to:
Third Edition Task Force Project Leaders:
Jonathan S. Talbot, PT, MS, COS-C
Kenneth L. Miller, PT, DPT, CEEAA
Chapter Authors:
Aban Singh, PT, LLB
Barbara Piper, PT, DPT
Debbie Becker, PT
Judy Schank, PT, MS
Kathy Medlin, PT, MS, GCS
Kelly Bailey, PT, DPT
Laurie Page, PT, DPT
Lisa Marie Naeger, PT
Lynn Kelly, PT, DPT, MS
Medha Bansode Ram, PT, MHS, GCS, COS-C
Patricia Crowl Yoder, PT, DPT
Paula Graul, PT, MS, GCS, CEEAA
Sharon Bezner, PT, PhD
Sheri Yarbray, PT, MS
Tim Dunn, PT, DPT, GCS, COS-C
Project Advisors:
Diana “Dee” Kornetti, PT
Arlynn Hansell, PT, HCS-D, HCS-O, COS-C
Special thanks to members of the APTA Home Health Section Practice Committee for their insightful
feedback in producing this handbook.
ACKNOWLEDGMENTS

ix
Preface
Much has changed in the home health landscape since the second edition of Guidelines for the
Provision of Physical Therapy in the Home was published in 2007. Since that time, the roles of
physical therapists (PTs) and physical therapist assistants (PTAs) in the home health setting have
expanded, reassessment requirements have changed, and public accountability has increased for
the provision of best practices and the promotion of positive patient experiences. The American
Physical Therapy Association’s (APTA) revision of the Code of Ethics for the Physical Therapist and
Standards of Practice for the Physical Therapist Assistant in 2010 resulted from a recognition of these
evolving roles. Care coordination and interdisciplinary collaboration are now viewed as essential for
producing a value-based experience for patients and their caregivers. The third edition, now titled
Providing Physical Therapy in the Home, provides timely guidance to elevate the quality of physical
therapist services in the home care setting to the highest levels, consistent with the Vision Statement
of APTA.
Providing Physical Therapy in the Home includes several important revisions to its predecessor,
Guidelines for the Provision of Physical Therapy in the Home, second edition. Perhaps most important,
the model of the International Classification of Functioning, Disability, and Health (ICF), which was
endorsed by APTA in 2008, has been integrated with Chapter 7, “Physical Therapy Admissions
and Evaluation.” This handbook also addresses new and relevant subjects. For instance, it adds an
entire chapter, Chapter 9, dedicated to the role of physical therapists as case managers. Chapter 11,
“Home Health Physical Therapy Supplies/Equipment and Infection Control,” was derived from the
“Tools of the Trade” resource found in the second edition. Chapter 13, “The Patient Experience,” was
deemed appropriate given that the Home Health Consumer Assessment of Healthcare Providers
and Systems (HHCAHPS) was implemented in 2009 and is publically reported. The handbook adds
Chapter 14, “Lifelong Learning and Continuing Competence,” to inspire clinicians in home health
to consider a formal career development pathway that brings value to both their patients and their
personal ambitions. The final chapter, “Home Health Physical Therapist Practice References and
Resources,” was adapted from the “Online Resources” section in the second edition.
As currently organized, chapters 1 through 6 are written to be beneficial for PTs and PTAs working in
the field, as well as for home health agency administrative personnel. Chapters 7 through 12 provide
guidance specific to the actual provision of physical therapist services. Chapters 13 through 15
provide additional resource material for PTs and PTAs to improve quality of care for patients through
continued competence and effective use of available resources.
This handbook provides a foundation for the provision of physical therapy to patients in their place
of residence. The authors obtained input regarding the handbook from APTA staff members, Home
Health Section members, committee chairs, and the Home Health Section Executive Committee.
Consistent with APTA terminology, the handbook represents Home Health Section-approved,
nonbinding statements of advice pertaining to the specifics of home health care.
PREFACE

x
Providing Physical Therapy in the Home
The ongoing evolution of practice, research, and regulatory standards will influence home health
physical therapist practice. The focus of practice remains on meeting the needs of patients and
caregivers in their homes and communities. We recognize that this handbook does not reflect the
entire scope of requirements associated specifically with home health physical therapy because of
rules and regulations including, but not limited to:
• Federal rules and regulations such as Medicare Benefit Policy Manual Chapter 7, Medicare’s
conditions of participation, the prospective payment system, regional home health intermediary
local coverage determinations, and the Health Insurance Portability and Accountability Act
• Individual state rules and regulations such as professional licensure requirements and
public health regulations
• Municipal rules and regulations
• Referral relationships (APTA HOD P06-90-15-28)
• Accreditation bodies such as the Community Health Accreditation Program and
The Joint Commission
• Applicable agency policies and procedures
• Reimbursement requirements of third-party payers
• Quality initiatives and advances in professional practice
This handbook represents statements of conditions that reflect ideal performance criteria for
the administration of quality physical therapy in the home. These criteria may be used to assess
compliance with best practices for therapy services provided by home health agencies. This book
may be subject to changes and modifications to remain up-to-date with current home health rules
and regulations.
The Home Health Section Practice Committee anticipates that this edition will be a valuable resource
for home health agency leadership, physical therapists, and physical therapist assistants in providing
the highest standards of care for patients and their caregivers.
Jonathan S. Talbot, PT, MS, COS-C
Kenneth L Miller, PT, DPT, CEEAA
Third Edition Task Force Leaders
Home Health Section of the American Physical Therapy Association

CHAPTER 1
1
Chapter 1: Roles of the Physical Therapist in Home Health Care
ROLES OF THE PHYSICAL THERAPIST IN HOME HEALTH CARE
Introduction
Physical therapists working in the home health setting fulfill several valuable roles as they serve the
needs of patients and caregivers. The roles and responsibilities of home health physical therapists
have evolved over the years. The Guide to Physical Therapist Practice
1
and the American Physical
Therapy Association (APTA) Code of Ethics for the Physical Therapist identify 5 roles
2,3
in which
physical therapists may serve:
• Manager of patients and caregivers
• Consultant
• Educator
• Researcher (critical inquiry)
• Administrator
These roles pertain to the home health setting as follows.
The role of manager of patients and caregivers is well established in the home health setting at the
basic level of providing physical therapy care. This role has evolved to include case management
responsibilities. In the role of consultant, the physical therapist shares his or her expertise with patients
and caregivers, peers, and organizations to promote optimal health and function. Physical therapists
serve as educators, providing valuable training to patients and caregivers, and to peers via in-services.
As researchers, physical therapists in home health care participate in the process of critical inquiry
by using and interpreting standardized tests and measures to provide objective evidence about how
their services benefit individuals. Some clinicians may also participate in research by contributing to
the body of knowledge about how physical therapy benefits society at large. Finally, in the role of
administrator, physical therapists serve as decision makers to guide a group of clinicians with the
provision of quality and cost-effective care for the individuals served by their organization.
Physical therapists who fulfill their roles and responsibilities with professionalism
4
have the potential to
positively impact the society in which they live. The APTA Vision Statement for the Profession
5
pursues
a larger role for physical therapists of “transforming society by optimizing movement to improve the
human experience.” This vision statement highlights the unique expertise of physical therapists as
movement specialists and how they can affect societal health. Physical therapists serve in multiple
roles in the home health setting, so they are well positioned to lead the way toward accomplishing
this vision. The purpose of this chapter is to provide a guideline and criteria to help physical therapists
succeed in their various roles.

2
Providing Physical Therapy in the Home
GUIDELINE
In the pursuit of greater societal health, and in compliance with existing standards of care, policies,
and regulations, physical therapists serve with professionalism in multiple roles and with multiple
responsibilities in the home health setting, acting as patient care managers, consultants, educators,
researchers, and administrators.
CRITERIA
1. The physical therapist (PT) serves as a care manager by:
a. Admitting patients to home health services
b. Completing a comprehensive patient history and examination according to current
standards of best practice
c. Reviewing medication profiles
6
for accuracy and identifying possible concerns or
discrepancies for discussion with the physician and other members of the interdisciplinary
team
d. Developing and implementing appropriate plans of care based upon the following key
components from the International Classification of Functioning, Disability, and Health
(ICF)
7
:
i. Prior level of function
ii. Current and prior health condition(s)
iii. Impairments of body function and structure
iv. Activity limitations
v. Participation restrictions
vi. Environmental factors (eg, devices, medications, family support)
vii. Personal factors (eg, race, education, lifestyle, habits)
e. Submitting documentation that is timely, is accurate, and establishes the medical
necessity for skilled physical therapy
f. Collaborating regularly with the interdisciplinary team and recognizing the role of each
member to help achieve patient-centered goals
g. Supervising physical therapist assistants (PTAs) in compliance with all jurisdiction
requirements, agency policies, and best practices
8-11
h. Making timely reassessments, including updating/modifying the plan of care as needed in
response to patient condition
i. Employing objective tests and measures at multiple time-points during the episode
of care
j. Accurately completing the Outcome and Assessment Information Set (OASIS)
12
k. Respecting cultural diversity and patient choice(s)
13
l. Advocating for patient safety by addressing concerns about his or her environment,
social support, and emotional health
m. Formulating a discharge plan and subsequently discharging patients from physical
therapist services when skilled care is no longer indicated (see Chapter 12, “Discharge
Planning,” for explanation of the use of the term “discharge” throughout this publication)

3
Chapter 1: Roles of the Physical Therapist in Home Health Care
2. The PT serves as a consultant in the home health setting by sharing his or her expertise and
guidance with members of the interdisciplinary team and organizations regarding:
a. Enhancement of clinical skills
b. Promotion of value-based patient care
c. Patient-centered care
d. Improving the patient experience (eg, patient satisfaction)
e. Risk-management strategies
3. The PT serves as an educator in the home health setting for patients and caregivers, students,
community groups, and interdisciplinary teams by:
a. Providing in-service training
b. Serving as a mentor to students and clinicians
c. Explaining the benefits of home health physical therapist services
d. Planning for professional growth and continuing competence
4. The PT serves as a researcher by demonstrating critical inquiry in the home health setting by:
a. Analyzing and applying research findings to physical therapist practice and education
b. Disseminating the results of research
c. Evaluating the efficacy of new and established interventions/technologies
d. Participating in, planning, and conducting clinical, basic, or applied research
5. The PT serves as an administrator in the home health setting by being an organizational leader,
which may include the following responsibilities:
a. Serving in various leadership roles such as therapy director, agency administrator,
regional therapy director, chief clinical officer, or chief executive officer
b. Recruitment and retention of agency staff
c. Promoting adherence to best practices and evidence-based care
d. Ensuring regulatory compliance with the provision of home health services
e. Participating in quality improvement activities, such as chart audits and peer reviews
(home visits)
f. Monitoring the quality of the patient experience (eg, patient satisfaction)
g. Team building
h. Supporting the establishment of student clinical affiliations
i. Participating in community outreach events

4
Providing Physical Therapy in the Home
CASE SCENARIO
Tom is a physical therapist with 10 years of experience. He began his career working 3 years in an
outpatient setting, followed by 2 years in a hospital medical rehabilitation unit (MRU). He noticed
patients were being sent home sooner than they used to be, prior to the completion of their MRU
physical therapist plan of care, to receive home health services. A friend of his has been working for a
home health agency and encouraged Tom to give it a try. He has now been doing home health during
the past 5 years and has noticed a significant shift in his responsibilities during this time.
Initially, Tom didn’t have to do start-of-care visits (ie, admissions) because his agency policy was
to send nursing staff out to do all admissions. During the past 2 years, this policy has changed,
and he has had to start admitting patients to home health. Fortunately, he has obtained extensive
Outcome and Assessment Information Set (OASIS) and case management training, expanded his
understanding of pharmacology, learned to document according to the model provided by the
International Classification of Functioning, Disability, and Health (ICF), and increased use of evidence-
based testing to more objectively quantify patient function. Consequently, he has improved his
confidence with case managing patients with chronic diagnoses such as congestive heart failure (CHF)
and chronic obstructive pulmonary disease (COPD), and he has used this knowledge to coordinate
care to reduce re-hospitalization rates. His agency now boasts one of the lower re-hospitalization
rates in the region.
Tom previously deferred the assessment of skin integrity, temperature, heart and lung sounds, and
wound care to nursing staff, and routinely checked only blood pressure and pulse during visits. He
weighs patients with CHF every visit to check for water retention. Having received additional training
from his agency, he now routinely assesses all of these items with every patient, recognizing that this
information makes him more instrumental in protecting the health and well-being of his patients. He
plans reassessments carefully, and documents appropriately, to justify the ongoing need for skilled
physical therapist services, if appropriate. His roles and responsibilities in home health care have
changed, but he has proudly accepted these changes and it has challenged him to improve the
quality of his care.
PRACTICAL APPLICATION
• Vision Statement and Guiding Principles for Physical Therapists
• Roles and Responsibilities of the Home Health Physical Therapist

5
Chapter 1: Roles of the Physical Therapist in Home Health Care
Vision Statement and Guiding Principles for Physical Therapists
5
(Adopted by the American Physical Therapy Association in June 2013)
APTA Vision Statement for the Physical Therapy Profession
Transforming society by optimizing movement to improve the human experience.
Guiding Principles
Identity. Physical therapists will be responsible for evaluating and managing an individual’s movement
system throughout his or her lifespan to improve the health of society. The movement system is the
core of physical therapist practice, education, and research.
Quality. The physical therapy profession includes doctors of physical therapy who will commit to
evidence-based practices in treatments, education, and research as they work to achieve functional
outcomes while preventing adverse events to patient care and to society.
Collaboration. The physical therapy profession will collaborate with other health care providers,
consumers, organizations, and disciplines to provide consumer-centered care. Evidence from
research should translate to practice in order to help solve health-related challenges faced by society.
Value. The physical therapy profession will provide interventions that are safe, effective, patient
centered, timely, efficient, and equitable. Outcomes will be cost effective, and value will be
demonstrated in all settings. Accountability is an essential characteristic for demonstrating value.
Innovation. The physical therapy profession will offer creative and proactive solutions to enhance
health services delivery and to increase the value of physical therapy to society. Innovation for value-
based care will be assisted by new technology, care models, workforce needs, and delivery methods.
Consumer-centricity. The physical therapy profession will ensure that patient/client/consumer values
and goals will be prioritized in all efforts and care settings. Physical therapists will embrace cultural
competence as an important skill for ensuring that best practice is provided to all patients and clients.
Access/Equity. The physical therapy profession will recognize health inequities and disparities and
seek to resolve them via creative models for service delivery. Physical therapists will seek improved
access to health care for all members of society.
Advocacy. The physical therapy profession will advocate for health care systems based upon
consumer-centered care. Physical therapists will advocate for appropriate care for patients, clients,
and consumers both as individuals and as a population, in practice, education, and research settings.
Adapted with permission from the American Physical Therapy Association. Complete text may be found at
http://www.apta.org/Vision/.

6
Providing Physical Therapy in the Home
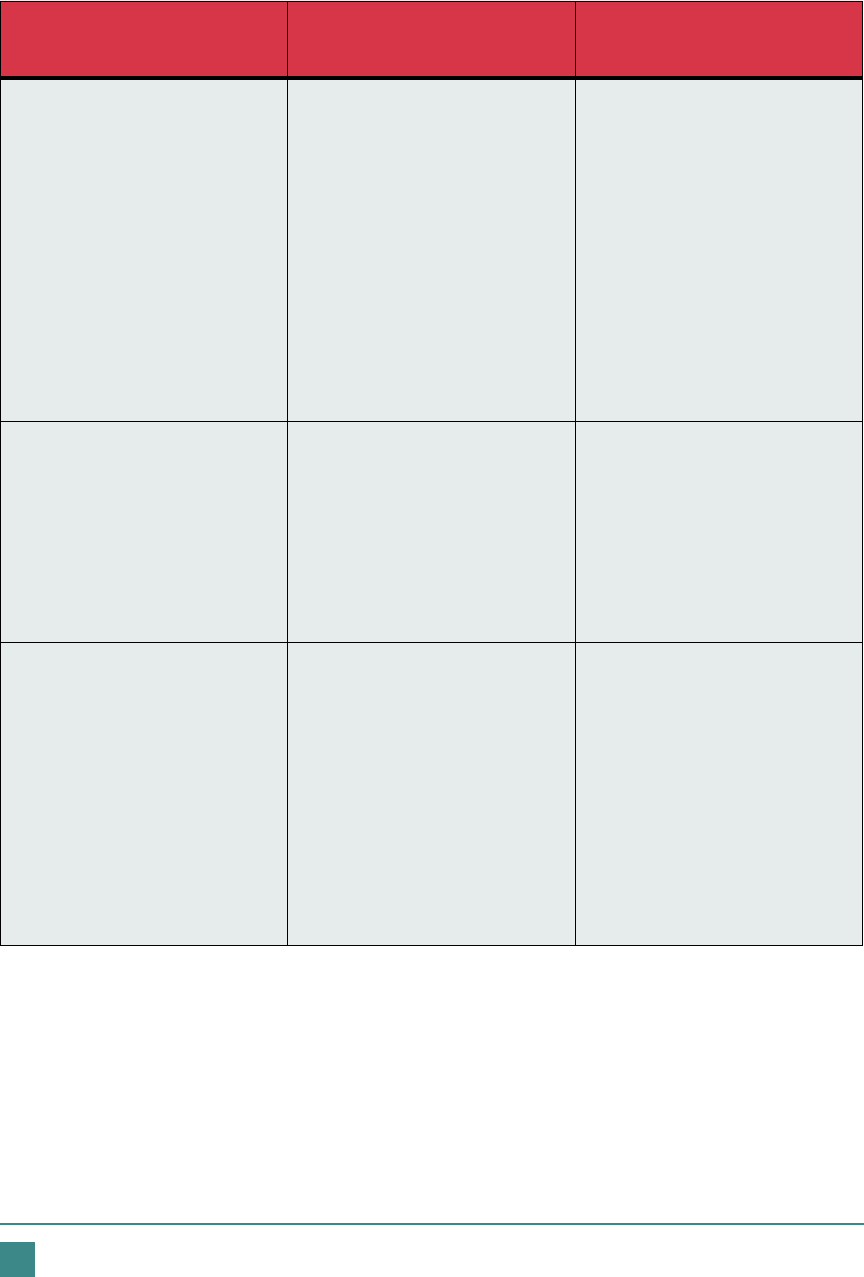
Table 1.1. Roles and Responsibilities of the Home Health
Physical Therapist
Patient Care
Manager
Consultant Educator Researcher Administrator
Admission
Care plan
development
Collaboration
Discharge planning
Documentation
Evaluation
Medication review
OASIS
Objective testing
Patient safety
PTA supervision
Reassessments
Regulatory
compliance
Respect
Clinical skills
Patient experience
Patient-centered
care
Risk management
Value-based care
Continuing
competence
In-services
Mentorship
Professional growth
Promotion of
physical therapy
Analysis
Critical inquiry
Research
participation
Treatment efficacy
Best practice
Community
outreach
Leadership
Patient experience
Quality improvement
Regulatory
compliance
Students
Team building
Derived from roles of the physical therapist as defined in the Guide to Physical Therapist Practice.
1
7
Chapter 1: Roles of the Physical Therapist in Home Health Care
References
1. Guide to Physical Therapist Practice 3.0. American Physical Therapy Association; 2014. http://
guidetoptpractice.apta.org/. Accessed August 20, 2014.
2. Swisher LL, Hiller P. The revised APTA code of ethics for the physical therapist and standards of ethical
conduct for the physical therapist assistant: theory, purpose, process, and significance. Phys Ther.
2010;90:803-824.
3. American Physical Therapy Association House of Delegates. Code of ethics for the physical therapist (HOD
S06-09-07-12). Alexandria, VA: American Physical Therapy Association; 2009. http://www.apta.org/
uploadedFiles/APTAorg/About_Us/Policies/Ethics/CodeofEthics.pdf. Accessed December 9, 2013.
4. American Physical Therapy Association Ethics and Judicial Committee. Guide for professional conduct.
Alexandria, VA: American Physical Therapy Association; 2010. http://www.apta.org/uploadedFiles/APTAorg/
Practice_and_Patient_Care/Ethics/GuideforProfessionalConduct.pdf. Accessed December 9, 2013.
5. American Physical Therapy Association House of Delegates. Vision statement for the physical therapy
profession (HOD P06-13-19-23). Alexandria, VA: American Physical Therapy Association; 2013. http://
www.apta.org/Vision/. Accessed December 9, 2013.
6. The role of physical therapists in medication management. Official statement. Alexandria, VA: American
Physical Therapy Association; 2010. http://www.apta.org/uploadedFiles/APTAorg/Payment/Medicare/
Coding_and_Billing/Home_Health/Comments/Statement_MedicationManagement_102610.pdf. Accessed
December 9, 2013.
7. ICF checklist, version 2.1a, clinician form for international classification of functioning, disability and health.
Geneva, Switzerland: World Health Organization; 2003. http://www.who.int/classifications/icf/training/
icfchecklist.pdf. Accessed December 16, 2013.
8. American Physical Therapy Association House of Delegates. Direction and supervision of the physical
therapist assistant (HOD P06-05-18-26). Alexandria, VA: American Physical Therapy Association; 2005.
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/HOD/Practice/Direction.pdf. Accessed
December 9, 2013.
9. PTA Patient care & supervision. American Physical Therapy Association website. http://www.apta.org/
PTA/PatientCare/. Updated February 20, 2013. Accessed December 9, 2013.
10. Practice acts by state. American Physical Therapy Association website. http://www.apta.org/Licensure/
StatePracticeActs/. Updated April 20, 2014. Accessed May 30, 2014.
11. PT/PTA teamwork: models in delivering patient care. American Physical Therapy Association website. http://
www.apta.org/SupervisionTeamwork/Models/. Updated June 20, 2013. Accessed December 9, 2013.
12. Outcome and assessment information set (OASIS). Centers for Medicare and Medicaid Services website.
http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/OASIS/index.html.
Updated April 5, 2012. Accessed December 28, 2013.
13. Policies & guidelines related to cultural competence and diversity. American Physical Therapy Association
website. Updated September 12, 2013. http://www.apta.org/CulturalCompetence/Policies/. Accessed
December 9, 2013.

CHAPTER 2
9
Chapter 2: Roles of the Physical Therapist Assistant in Home Health Care
ROLES OF THE PHYSICAL THERAPIST ASSISTANT IN HOME
HEALTH CARE
Introduction
Home health is a unique environment where the physical therapist assistant (PTA) may implement
physical therapist plans of care in a patient’s residence under the supervision of a physical therapist
(PT). Physical therapist assistants are graduates of education programs accredited by the Commission
on Accreditation in Physical Therapy Education (CAPTE).
1
The role of the PTA has been developing
since the 1960s, when very few physical therapists were available to fill the growing demand for
physical therapist services. Although PTAs may help expand access to home health physical therapy,
the actual use of PTAs varies between jurisdictions due to licensure limitations.
In jurisdictions where PTAs are permitted to provide home health physical therapy, they fulfill several
important roles.
2
Some of these roles include:
• Providing direct patient care under physical therapist supervision
• Documenting patient interventions and objective measurements
• Educating patients and caregivers to ensure safety
• Monitoring patient status and reporting changes
• Communicating and collaborating with the physical therapist and the interdisciplinary team
Physical therapist assistants serve in these roles to enhance quality, patient-centered care as
contributing members of the home health interdisciplinary team.

10
Providing Physical Therapy in the Home
GUIDELINE
Under the supervision of a physical therapist, and in compliance with existing standards of care,
policies, and regulations, the physical therapist assistant provides patient care, documents services,
educates patients and caregivers, monitors progress, and communicates with the interdisciplinary
team.
CRITERIA
1. The physical therapist assistant (PTA) provides patient care by:
a. Implementing the plan of care under the supervision
3,4
of the physical therapist
b. Modifying interventions appropriately within the framework of the plan of care to progress
patients toward goals
c. Respecting cultural diversity and providing quality services to patients and caregivers in a
nonjudgmental manner, regardless of the nature of their health problems
5,6
d. Maintaining confidentiality of patient information per state and federal regulations
7
e. Complying with the American Physical Therapy Association’s (APTA) Standards of
Practice for Physical Therapy
8
f. Complying with APTA’s Standards of Ethical Conduct for the Physical Therapist
Assistant
9-11
2. The PTA documents skilled patient care by:
a. Recording patient statements about functional difficulties and improvements noted
during the course of care
b. Describing teaching provided to patient and caregivers
c. Describing specifically the interventions provided
d. Recording patient and caregiver response to interventions
e. Comparing patient performance with prior visits and/or goals
f. Describing planned intervention modifications for the subsequent visit
g. Submitting documentation to the agency in a timely manner
3. The PTA educates patients and caregivers by:
a. Instructing in a home exercise program (HEP)
b. Teaching safety principles
c. Using appropriate modes of instruction (eg, verbal, demonstration) to facilitate optimal
patient and caregiver understanding
d. Providing preventive education regarding health and wellness
e. Informing about care transition resources
f. Participating in professional growth and continuing competence activities

11
Chapter 2: Roles of the Physical Therapist Assistant in Home Health Care
4. The PTA monitors patient status by:
a. Performing objective tests and documenting results
b. Modifying interventions in response to patient progress, per direction of the supervising
physical therapist
5. The PTA communicates with the interdisciplinary team by:
a. Reporting the need for reassessment to the supervising physical therapist and preparing
patients for discharge
b. Conferencing with the supervising physical therapist regarding significant changes in the
patient’s condition
c. Reporting observations of environmental issues and abusive situations to the supervising
physical therapist and case manager
d. Participating in multidisciplinary care conferences and quality improvement activities
12

12
Providing Physical Therapy in the Home
CASE SCENARIO
Jessica is a physical therapist assistant (PTA) who previously worked in a skilled nursing facility (SNF)
for 6 years. She has begun working in the home health setting. She loves the geriatric population
and enjoys home health because she gets to work 1-on-1 with patients. She is a self-starter and
appreciates the ability to manage her patient schedule. During the past year, she has learned the
importance of recording blood pressure, respiratory rate, pulse, and temperature every visit. On
several occasions, she has reported to her supervising PT when vital signs were found to be outside
parameters, enabling the team of therapists, nurses, and the patient’s physician to coordinate an
appropriate response to help prevent re-hospitalization. She also discusses her patient’s pain level
on every visit, and inquires about whether there are any changed medications or any side effects to
medications. She reports any changes or problems to her supervising PT and other members of the
interdisciplinary team.
Jessica effectively implements plan-of-care interventions within the scope of her license, using
evidence-based techniques to optimize outcomes. For example, she uses the appropriate resistance
for strengthening exercises, based on principles of safe overloading. She educates on a home
exercise program effectively, requiring the patient and/or caregiver to teach back learning and provide
return demonstration. She promptly contacts her supervising PT regarding any changes in patient
condition to discuss an appropriate response. She and her supervising PT conference weekly to
discuss each patient’s status relative to the plan of care goals. They consider how many therapy
disciplines are involved and verify timely scheduling of the next reassessment. She values her ability
to make a difference in the lives of her patients and is honored by the high patient satisfaction scores
that her agency receives.
PRACTICAL APPLICATION
• Roles of the Physical Therapist Assistant in the Home Health Setting
• Appropriate PTA Responses to Changes in Patient Condition

13
Chapter 2: Roles of the Physical Therapist Assistant in Home Health Care
Roles of the Physical Therapist Assistant in the Home Health Setting
• Provide patient care
• Document appropriately and timely
• Educate to ensure safety
• Monitor patient progress/changes
• Communicate patient status to supervising PT and collaborate with interdisciplinary team
Figure 2.1. Appropriate PTA responses to changes in patient condition.
INDICATIONS
FOR PT–PTA
CONFERENCING
Vital signs outside
of parameters,
but patient
asymptomatic
A plan-of-care goal
met or exceeded
Next planned
visit is a
reassessment
or discharge
INDICATIONS
FOR EMERGENCY
ACTION
(Call 911, call PT, notify
agency, notify physician)
Vital signs critically
abnormal
Patient falls at
home with injury
Very unusual
change in patient
status

14
Providing Physical Therapy in the Home
References
1. Evaluative Criteria: PTA Programs. Alexandria, VA: Commission on Accreditation in Physical Therapy
Education; 2013. http://www.capteonline.org/uploadedFiles/CAPTEorg/About_CAPTE/Resources/
Accreditation_Handbook/EvaluativeCriteria_PTA.pdf. Accessed December 17, 2013.
2. Role of a physical therapist assistant (PTA). American Physical Therapy Association website. http://www.
apta.org/PTACareers/RoleofaPTA/. Updated March 28, 2013. Accessed December 17, 2013.
3. American Physical Therapy Association House of Delegates. Levels of supervision (HOD P06-00-15).
Alexandria, VA: American Physical Therapy Association; 2000. http://www.apta.org/uploadedFiles/
APTAorg/About_Us/Policies/Terminology/LevelsSupervision.pdf. Accessed December 17, 2013.
4. PTA patient care & supervision. American Physical Therapy Association website. http://www.apta.org/
PTA/PatientCare/. Updated February 20, 2013. Accessed December 17, 2013.
5. Policies & guidelines related to cultural competence and diversity. American Physical Therapy Association
website. http://www.apta.org/CulturalCompetence/Policies/. Updated September 12, 2013. Accessed
December 17, 2013.
6. American Physical Therapy Association House of Delegates. Nondiscrimination in the provision of physical
therapy services (HOD P06-03-24-21). Alexandria, VA: American Physical Therapy Association; 2003.
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/HOD/Health/Nondiscrimination.pdf.
Accessed December 17, 2013.
7. Health information privacy. US Department of Health and Human Services website. http://www.hhs.gov/
ocr/privacy/. Accessed December 17, 2013.
8. American Physical Therapy Association House of Delegates. Standards of practice for physical therapy
(HOD P06-13-22-15). Alexandria, VA: American Physical Therapy Association; 2013. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Practice/StandardsPractice.pdf. Accessed December 17,
2013.
9. American Physical Therapy Association House of Delegates. Standards of ethical conduct for the physical
therapist assistant (HOD S06-09-20-18). Alexandria, VA: American Physical Therapy Association; 2009.
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/StandardsEthicalConductPTA.pdf.
Accessed December 17, 2013.
10. American Physical Therapy Association Ethics and Judiciary Committee. Guide for conduct of the physical
therapist assistant. Alexandria, VA: American Physical Therapy Association; 2010. http://www.apta.org/
uploadedFiles/APTAorg/Practice_and_Patient_Care/Ethics/GuideforConductofthePTA.pdf. Accessed
December 17, 2013.
11. American Physical Therapy Association Department of Physical Therapist Assistant Services and
Department of Academic/Clinical Education Affairs. Values-based behaviors for the physical therapist
assistant. Alexandria VA: American Physical Therapy Association; 2011. http://www.apta.org/
uploadedFiles/APTAorg/PTAs/Careers/Values/ValuesBasedBehaviorsforPTA.pdf. Accessed December 17,
2013.
12. PT/PTA teamwork: models in delivering patient care. American Physical Therapy Association website. http://
www.apta.org/SupervisionTeamwork/Models/. Updated June 20, 2013. Accessed December 9, 2013.

CHAPTER 3
15
Chapter 3: Qualifications
QUALIFICATIONS
Introduction
The task of hiring and training a new physical therapist or physical therapist assistant can be
challenging for home health agencies. It is imperative that therapists chosen to represent the agency
or provider have the appropriate qualifications and skills to safely manage patients. Patients receiving
home health physical therapy should benefit from a quality standard of care that inspires confidence
in the ability of their therapist(s) to safely and effectively manage their health care needs.
Most agencies recognize the importance of finding therapists who are a “good fit” for their organizational
goals for quality patient care. To this end, they may consider the mission of the organization and the
unique needs of their patient population (eg, therapist compatibility with company culture, specialized
training/qualifications, languages spoken). Meanwhile, the provision of home health services requires
that a quality standard be maintained. The information in this chapter provides valuable guidance
to agencies and clinicians to help ensure that the providers of home health services are adequately
prepared prior to patient care, and that skills and knowledge are sufficiently maintained for quality
care on an ongoing basis.

16
Providing Physical Therapy in the Home
GUIDELINE
Appropriately qualified professionals provide home health physical therapist services in accordance
with best practice standards.
CRITERIA
1. The physical therapist (PT) and physical therapist assistant (PTA) are health care professionals
who have met the criteria for licensure as defined by federal guidelines.
1,2
2. The PT and PTA are licensed to practice in the jurisdiction(s) in which the therapist provides care as
required by law and, where applicable, meet all licensure requirements as defined by the jurisdiction.
3,4
3. The PT and PTA comply with any jurisdiction-specific requirements for home health and, where
applicable, reference and comply with the standards established by the jurisdiction’s Department
of Health.
5,6
4. The PT and PTA are certified in basic life support (BLS)
7
in accordance with the certifying agency’s
guidelines and state regulations (eg, American Red Cross CPR/AED for Professional Rescuers
and Health Care Providers
8
and American Heart Association Basic Life Support
9
).
5. The PT and PTA comply with applicable infection control guidelines
developed by:
a. The Centers for Disease Control and Prevention (eg, health care associated infections,
10
bloodborne pathogens
11
)
b. The Occupational Safety and Health Administration (eg, personal protective equipment,
12
respiratory protection,
13
exposure to tuberculosis
14
)
c. Agency policies and procedures
6. The PT and PTA are obligated to:
a. Practice/work at or above the level determined to be the minimal acceptable standard
that will ensure safe patient practice
b. Participate in ongoing professional/career development that maintains the expected level
of clinical practice/competency
15-19
7. Related physical therapy experience is recommended for PTs and PTAs entering home health
care to ensure that knowledge and skills are sufficient to safely provide physical therapist services
to patients.
20
Agencies may promote ongoing therapist qualification for safe and appropriate
patient care by:
a. Performing pre-hire or pre-contract interviews with clinicians in which topics of clinical
competency are discussed in detail specific to the needs of patients served by the home
health agency
b. Formally assessing clinical competencies post-hire or post-contract and prior to the
provision of patient care
c. Providing additional mentoring and training resources for clinicians new to home health care
d. Supporting continuing competence and educational opportunities to promote lifelong
learning
e. Completing regularly scheduled clinician performance evaluations

17
Chapter 3: Qualifications
CASE SCENARIO
Tom and Jessica were each interviewed by the home health agency. The interviews included
discussions of the clinical needs of the patients served by the agency and a background check to
ensure that both Tom and Jessica were properly licensed. During the interview process, the agency
representative noted that both have the flexibility to provide home health services and determined that
they have the organizational ability to manage patient schedules appropriately. From their respective
conversations, Tom and Jessica made clear that they looked at patients holistically, considering
all aspects of a patient’s needs including their diagnoses, home safety, living situation, caregiver
availability, social support network, and transportation needs. It was also evident that they were
already in the habit of performing PT–PTA conferences regularly and coordinating care with the
physician and with other disciplines when appropriate. They both verbalized understanding of how to
identify problems with medication management and respond appropriately.
Tom has some experience and training with providing wound care and is certified for lymphedema
management. The home health agency explained to Tom that they would require that he provide
evidence of training and competency in these areas prior to treating patients with these conditions.
Tom and Jessica reported being comfortable using the modalities that the agency has available (eg,
electrical stimulation, ultrasound), but the agency plans to have a preceptor therapist meet with them
to have them demonstrate competency. This preceptor will assist with orientation and discuss other
competencies identified by the agency as important for safe patient care, and report back to agency
leadership when Tom and Jessica are cleared for patient care.
PRACTICAL APPLICATION
• Home Health Qualifications for PTs and PTAs
• Home Health PTA Supervision Requirements by Jurisdiction
18
Providing Physical Therapy in the Home
Table 3.1. Home Health Qualifications for PTs and PTAs
Criteria
Application for Home
Health Agency
References
1. Licensure/Certification/
Registration
The physical therapist (PT)
and physical therapist
assistant (PTA) are health
care professionals who have
met the criteria for licensure as
defined by federal guidelines.
Agency verifies licensure as
required in the jurisdictions within
the area of coverage of the home
health agency.
Agency performs required
background checks (eg, criminal,
Medicare exclusion, disciplinary
actions).
Agency verifies other requirements
as needed (eg, liability insurance,
automobile insurance, driver’s
license).
US Government Printing Office.
42 CFR 484.4—Personnel
qualifications.
1
American Physical Therapy
Association House of Delegates.
Consumer protection in the
provision of physical therapist
services: qualifications of persons
providing physical therapist
services (HOD P06-01-20-20).
2
2. PT and PTA Licensure
Requirements
The PT and PTA are licensed
to practice in the jurisdiction(s)
in which the therapist provides
care and meet all licensure
requirements as defined by
the jurisdiction.
Agency verifies that therapists
meet requirements for active
licensure, including continuing
education.
Practice acts by state. American
Physical Therapy Association.
3
Licensure reference guide. The
Federation of State boards of
Physical Therapy.
4
3. PT and PTA Jurisdiction
Requirements
PT and PTA comply with
any jurisdiction-specific
requirements for home
health and, where applicable,
reference and comply with
the standards established by
the jurisdiction’s Department
of Health.
Agency verifies adequate PTA
supervision by the PT according
to the requirements of the state/
jurisdiction and the professional
judgment of supervising PT.
Agency determines if any payer
restrictions are relevant to use of
PTA services.
US Government Printing Office.
42 CFR 484.12—Condition
of participation: compliance
with federal, state, and local
laws, disclosure and ownership
information, and accepted
professional standards and
principles.
5
State health departments
and services. State and Local
Government on the Net.
6

19
Chapter 3: Qualifications
4. Basic Life Support and
Cardiopulmonary Resuscitation
PT and PTA are certified in
basic life support (BLS) in
accordance with the certifying
agency’s guidelines and state
regulations.
PT and PTA complete BLS training
prior to providing patient care.
Agency verifies that BLS training
meets its requirements (eg,
American Red Cross CPR/AED for
Professional Rescuers and Health
Care Providers, American Heart
Association Basic Life Support,
or equivalent).
American Physical Therapy
Association House of Delegates.
Cardiopulmonary resuscitation
(HOD P06-06-12-09).
7
American Red Cross. First aid,
CPR, and AED certification.
8*
American Heart Association. Basic
life support.
9*
*Inclusion of these references
should not be interpreted as
endorsement by APTA or the
Home Health Section.
5. Infection Control Guidelines
The PT and PTA comply with
applicable infection control
guidelines developed by:
a.) The Centers for Disease
Control (CDC);
b.) The Occupational Safety
and Health Administration
(OSHA); and
c.) Agency-specific policies
and procedures.
PT and PTA demonstrate
compliance with standards of
infection control, including bag
technique and hand washing.
PT and PTA to follow agency-
specific infection control
guidelines.
Centers for Disease Control and
Prevention. Healthcare associated
infections (HIAs).
10
US Dept of Labor. Bloodborne
pathogens.
11
US Dept of Labor. Personal
protective equipment.
12
US Dept of Labor. Respiratory
protection.
13
US Dept of Labor. Enforcement
procedures and scheduling
for occupational exposure to
tuberculosis.
14
Table 3.1. (Continued)

20
Providing Physical Therapy in the Home
6. PT and PTA Standards
of Practice
The PT and PTA are
obligated to:
a.) Practice/work at or above
the level determined to be
the minimal acceptable
standard that will ensure
safe and effective patient
practice; and
b.) Participate in ongoing
professional/career
development that maintains
a level of clinical practice/
competence consistent
with minimal acceptable
standards.
PT and PTA provide care that is
culturally sensitive, professional,
and compassionate.
PT and PTA provide care based
upon evidence-based practice,
including use of valid standardized
tests and clinical practice
guidelines (CPGs).
PT and PTA demonstrate core
values identified by APTA,
including:
1. Accountability
2. Compassion/caring
3. Excellence
4. Integrity
5. Professional duty
6. Social responsibility
PT and PTA demonstrate
behaviors consistent with the
Code of Ethics for the Physical
Therapist and Standards of
Ethical Conduct for the Physical
Therapist Assistant.
American Physical Therapy
Association Board of Directors.
Professionalism in physical
therapy: core values (BOD 05-04-
02-03).
15
American Physical Therapy
Association House of Delegates.
Code of ethics for the physical
therapist (HOD S06-09-07-12).
16
American Physical Therapy
Association House of Delegates.
Standards of ethical conduct for
the physical therapist assistant
(HOD-S06-09-20-18).
17
American Physical Therapy
Association House of Delegates.
Standards of practice for physical
therapy (HOD-S06-13-22-15).
18
American Physical Therapy
Association House of Delegates.
Nondiscrimination in the provision
of physical therapy services (HOD
P06-03-24-21).
19
Table 3.1. (Continued)

21
Chapter 3: Qualifications
7. Knowledge and Skills
Competency
Related physical therapy
experience is recommended
for PTs and PTAs entering
home health care to ensure
that knowledge and skills are
sufficient to safely provide
physical therapist services
to patients. Agencies may
promote ongoing therapist
qualification for safe and
appropriate patient care by:
a.) Performing pre-hire or
pre-contract interviews
with clinicians in
which topics of clinical
competency are discussed
in detail specific to the
needs of patients served
by the home health agency
b.) Formally assessing clinical
competencies post-hire or
post-contract and prior to
the provision of patient care
c.) Providing additional
mentoring and training
resources for clinicians new
to home health care
d.) Supporting continuing
competence/educational
opportunities to promote
lifelong learning
e.) Completing regularly
scheduled clinician
performance evaluations
Agency completes competency
assessments prior to PT or PTA
providing patient care. Agency
provides further education or
mentoring for any deficits noted.
Agency provides mentoring
resources to any new clinician in
home health to ensure effective
preparation for his or her role.
Agency supports continuing
competence/education
opportunities to promote
enhanced knowledge base among
therapy staff.
Agency completes performance
evaluations that hold PT and PTA
to standard of care consistent with
safe patient care and timely and
appropriate documentation.
Career management. American
Physical Therapy Association
website.
20
Table 3.1. (Continued)

22
Providing Physical Therapy in the Home
Home Health PTA Supervision Requirements by Jurisdiction
The level of physical therapist assistant (PTA) supervision varies from one jurisdiction to another.
Physical therapists (PTs), PTAs, and home health agencies need to know how the regulations for
their jurisdiction affect PTA utilization in the home health setting. The Federation of State Boards of
Physical Therapy and APTA provide valuable reference information for identifying PTA supervision
requirements by jurisdiction. Reference information is provided below, but clinicians are responsible
for recognizing that this reference material may not be updated as quickly as the various practice
regulations around the country. Therefore, this reference material should not take precedence over
having a good working knowledge of the most up-to-date practice regulations applicable to the
jurisdiction where one is licensed to practice.
PTA Supervision Requirements by Jurisdiction
The Federation of State Boards of Physical Therapy
https://www.fsbpt.org/Portals/0/documents/free-resources/JLRGSupervisionRequirements_201006.pdf.
Physical Therapy Practice Acts by State
American Physical Therapy Association
http://www.apta.org/Licensure/StatePracticeActs/

23
Chapter 3: Qualifications
References
1. US Government Printing Office. 42 CFR 484.4—Personnel qualifications. http://www.gpo.gov/fdsys/
granule/CFR-2011-title42-vol5/CFR-2011-title42-vol5-sec484-4/content-detail.html. Accessed December
20, 2013.
2. American Physical Therapy Association House of Delegates. Consumer protection in the provision of
physical therapy services: qualifications of persons providing physical therapy services (HOD P06-01-20-
20). Alexandria, VA: American Physical Therapy Association; 2001. http://www.apta.org/uploadedFiles/
APTAorg/About_Us/Policies/HOD/Practice/ConsumerProtection.pdf. Accessed December 20, 2013.
3. Practice acts by state. American Physical Therapy Association website. http://www.apta.org/Licensure/
StatePracticeActs/. Updated April 20, 2014. Accessed May 30, 2014.
4. Licensure reference guide. The Federation of State Boards of Physical Therapy website. http://www.fsbpt.
org/FreeResources/RegulatoryResources/LicensureReferenceGuide.aspx. Accessed December 28, 2013.
5. US Government Printing Office. 42 CFR 484.12—Condition of participation: compliance with federal,
state, and local laws, disclosure and ownership information, and accepted professional standards and
principles. http://www.gpo.gov/fdsys/granule/CFR-2011-title42-vol5/CFR-2011-title42-vol5-sec484-12/
content-detail.html. Accessed December 20, 2013.
6. State health departments and services. State and Local Government on the Net website.
http://www.statelocalgov.net/50states-health.cfm. Accessed December 28, 2013.
7. American Physical Therapy Association House of Delegates. Cardiopulmonary resuscitation (HOD
P06-06-12-09). Alexandria, VA: American Physical Therapy Association; 2006. http://www.apta.org/
uploadedFiles/APTAorg/About_Us/Policies/Health_Social_Environment/CardiopulmonaryResuscitation.
pdf#search=%22cardiopulmonary_resuscitation%22. Accessed December 20, 2013.
8. First aid, CPR, and AED certification. American Red Cross website. http://www.redcross.org/CPR-
Training. Accessed August 14, 2014.
9. Basic life support. American Heart Association website. http://www.heart.org/HEARTORG/CPRAndECC/
HealthcareProviders/BasicLifeSupportBLS/Basic-Life-Support-BLS_UCM_001281_SubHomePage.jsp.
Accessed August 14, 2014.
10. Healthcare associated infections (HIAs). Centers for Disease Control and Prevention website.
http://www.cdc.gov/hai/prevent/prevent_pubs.html. Updated January 27, 2014. Accessed May 30, 2014.
11. Standards 29 CFR 1910.1030 Bloodborne pathogens. US Department of Labor website.
https://www.osha.gov/SLTC/bloodbornepathogens/. Accessed April 30, 2014.
12. US Department of Labor. Personal protective equipment. Website. https://www.osha.gov/pls/oshaweb/
owadisp.show_document?p_table=STANDARDS&p_id=9777. Accessed December 28, 2013.
13. US Department of Labor. Respiratory protection. Website. https://www.osha.gov/pls/oshaweb/owadisp.
show_document?p_table=STANDARDS&p_id=9777 . Accessed December 28, 2013.

24
Providing Physical Therapy in the Home
14. US Department of Labor. Enforcement procedures and scheduling for occupational exposure
to tuberculosis. Website. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_
table=DIRECTIVES&p_id=1586&p_text_version=FALSE. Accessed December 28, 2013.
15. American Physical Therapy Association Board of Directors. Professionalism in physical therapy: core
values (BOD 05-04-02-03). Alexandria, VA: American Physical Therapy Association; 2004. http://www.
apta.org/uploadedFiles/APTAorg/About_Us/Policies/BOD/Judicial/ProfessionalisminPT.pdf. Accessed
December 28, 2013.
16. American Physical Therapy Association House of Delegates. Code of ethics for the physical therapist
(HOD S06-09-07-12). Alexandria, VA: American Physical Therapy Association; 2009. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/CodeofEthics.pdf. Accessed December 28, 2013.
17. American Physical Therapy Association House of Delegates. Standards of ethical conduct for the physical
therapist assistant (HOD-S06-09-20-18). Alexandria, VA: American Physical Therapy Association; 2009.
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/StandardsEthicalConductPTA.pdf.
Accessed December 28, 2013.
18. American Physical Therapy Association House of Delegates. Standards of practice for physical therapy
(HOD-S06-13-22-15). Alexandria, VA: American Physical Therapy Association; 2013. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Practice/StandardsPractice.pdf. Accessed December 28,
2013.
19. American Physical Therapy Association House of Delegates. Nondiscrimination in the provision of
physical therapy services (HOD P06-03-24-21). Alexandria, VA: American Physical Therapy Association;
2003. http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Health_Social_Environment/
NonDiscriminationProvisionPTServices.pdf. Accessed December 28, 2013.
20. Career management. American Physical Therapy Association website. http://www.apta.org/
CareerManagement/. Updated December 30, 2013. Accessed May 30, 2014.

CHAPTER 4
25
Chapter 4: Orientation to the Agency
ORIENTATION TO THE AGENCY
Introduction
The task of orienting and training a new physical therapist (PT) or physical therapist assistant (PTA)
has become increasingly important as home health providers seek to improve the quality of therapy
services. Training new clinicians is costly, and well-planned orientation can enhance retention. A
comprehensive and organized orientation process is essential for building a strong therapy team and
furthering the mission and objectives of the home health agency.
Although field therapists can learn from experience, they will make many mistakes that are
unnecessary and potentially damaging to the agency’s reputation. Agency orientation programs fail for
several reasons:
• The orientation was not planned.
• The clinician was unaware of the home health job requirements and protocols.
• The therapist does not feel welcomed or supported with administrative issues.
• The field therapist hired does not meet qualification standards as set by APTA to practice
in this setting.
Effective orientation should include familiarizing new PTs and PTAs with agency operations, with
an overall design to inspire their support for the unique mission of the organization. Clinicians must
also be oriented to regulatory requirements related to the provision of home health services. The
orientation also should include training to facilitate direct patient care that is evidence based and
implements best practices. Precepting/mentoring is an effective approach for assisting agencies
with providing a quality orientation, which in turn may contribute to improved clinician retention.
1-3
The guideline and criteria in this chapter provide direction on how to customize a comprehensive
orientation for therapy field staff.

26
Providing Physical Therapy in the Home
GUIDELINE
The PT and PTA receive a comprehensive agency orientation that at a minimum includes training on
policies and procedures involving agency administration and on the safe provision of direct patient
care.
CRITERIA
1. The agency provides orientation regarding administrative policies and procedures that include,
but are not limited to:
a. Agency philosophy, which may include a statement of the company’s mission, values,
and/or vision
b. Agency organizational structure, including:
i. Hierarchy, including ownership
ii. Reporting structure, including:
1. Clinical reporting
2. Administrative reporting
iii. Corporate compliance, including:
1. Regulatory compliance (eg, Health Insurance Portability and Accountability Act
[HIPAA], Medicare Conditions of Participation)
2. Ethical compliance
iv. List of agency contact information
c. Policy and procedure manual
i. Physical therapist (PT) and physical therapist assistant (PTA) review and sign all
appropriate forms of acknowledgment as required by agency
ii. Employee handbook, if available, is issued to PT and PTA
d. Risk management and quality improvement efforts, including:
i. Occurrence reporting
ii. Complaint response process
iii. Quality improvement initiatives, including efforts to improve:
1. Outcomes
2. Patient experience
iv. If applicable, accrediting agency requirements (eg, Joint Commission, Community
Health Accreditation Program)
e. Regulatory overview

27
Chapter 4: Orientation to the Agency
i. Applicable municipal, state, and federal rules and regulations (eg, conditions
of participation, prospective payment system, local coverage determinations)
ii. Patient privacy (HIPAA)
iii. Reimbursement source/third-party payer requirements
iv. Quality assurance, improvement programs, and public reporting
1. Outcome-Based Quality Improvement (OBQI) / Outcome-Based Quality
Monitoring (OBQM)
2. OASIS Quality and Process Measures
3. Home Health Compare
4. HHCAHPS Survey
f. Services provided by the agency, including:
i. Nursing
ii. Physical therapy
iii. Occupational therapy
iv. Speech therapy
v. Home health aide
vi. Social work
vii. Dietician
viii. Care sitting
g. Hours of operation, including:
i. Regular service hours
ii. On-call service, including plans for staffing weekends and holidays (eg, on-call
schedule)
h. Time-off/vacation requests
i. Request policy/procedure and approval considerations
ii. Coverage planning/expectations, including procedure for ensuring adequate PTA
supervision is maintained (where applicable)
i. Payroll instructions/processes
j. Performance evaluations, including a review of key performance expectations and
evaluation schedule/frequency
k. Professional responsibilities/expectations, which may include:
i. Continuing competence
ii. Professional growth/development
iii. Mentoring clinicians new to home care
iv. Mentoring students (if applicable)
l. Employee benefits information (per agency)

28
Providing Physical Therapy in the Home
m. Job description, which may include:
i. Required work hours
ii. Productivity expectations
iii. Physical job demands
iv. In-home visit time expectations
v. Documentation expectations
vi. Required meeting attendance
vii. Interdisciplinary communication
viii. On-call expectations for weekends/holidays
n. Agency interdisciplinary communication processes (eg, team meetings, initial case report,
status report, discharge notification, reassessment planning), including:
i. Communication logistics (eg, onsite meeting, phone call, e-mail)
ii. Documentation requirements
iii. Meeting frequency and expected duration
iv. Attendance and participation requirements and expectations
v. Meeting preparation
2. The agency provides orientation regarding the safe provision of direct patient care following best
practices and current evidence. Orientation may include education on:
a. Patient care processes for:
i. Timely management of new referrals
ii. Appointment scheduling
iii. Verification of appropriate visit types (eg, OASIS vs PT evaluation only)
iv. Securing additional orders from the physician
b. Patient admission/start-of-care forms, and policies and procedures, including:
i. Home folder contents
ii. Consent forms
iii. Patient rights and responsibilities
iv. Privacy
v. Complaint procedure
c. Chart review to include locating patient demographics, advance directives, physician
orders, medication profile, diagnoses/coding, and homebound status
d. Clinical competency/skills assessment, which may include:
i. Clinician self-assessment of skills and certifications

29
Chapter 4: Orientation to the Agency
ii. Competency ensured via written testing and/or demonstration of techniques for:
1. Clinical skills
2. Tests and measures
3. OASIS
4. Oxygen safety
5. Infection control
iii. Training to recognize abuse and neglect, and reporting procedures
iv. Field observation
v. Competency testing
vi. Other requirements per agency policy
e. Basic life-support training requirements
f. Infection control
g. Dress code and personal appearance
h. Physician orders/communication, including:
i. Organizing communication to physician using standardized method for efficiency
(eg, Situation Background Assessment Recommendation [SBAR])
ii. Obtaining and appropriately documenting receipt of verbal orders
iii. Timely communication regarding sudden changes in patient status (eg, vital signs
outside parameters, falls, emergency care)
iv. Managing hold orders (eg, hospital hold, patient request)
i. Homebound status
j. OASIS instructions, time points, and management
k. Clinical documentation requirements:
i. Types of forms/format required (eg, electronic record, paper forms)
ii. Approved abbreviation list (including list of “do not use” abbreviations)
iii. Physician orders
iv. Expectations regarding content, including compliance with third-party payer
requirements (eg, local coverage determination)
v. Requirements for timely submission
vi. Instructions for correct application of clinical instruments, and tests and measures
(eg, OASIS, standardized tests, evidence-based measures)
vii. Change of service/discharge notification (eg, patient notification)
viii. Home logbook documentation
ix. Agency policy regarding patient/clinician signatures on visit notes
x. Other requirements per agency policy
l. Plan of care development and visit scheduling per evaluation findings, safety
considerations, prior level of function, patient and caregiver goals, and recommended
evidence-based interventions

30
Providing Physical Therapy in the Home
m. Supervision requirements for PTs, including:
i. PTA supervision
ii. Home health aide supervision
n. Patient and caregiver safety, including:
i. Protocol for requesting emergency care
ii. Identification of home safety concerns
iii. Falls prevention education
iv. Medication profile management/reconciliation
v. Procedures for minimizing re-hospitalization
vi. Oxygen safety
o. Diagnoses coding
p. Discharge planning, including advance notification, forms, and procedures (eg,
interdisciplinary coordination)
q. Emergency preparedness and disaster response plan, including priority codes and
triaging process
r. Workplace safety, including:
i. Driving safety
ii. Auto insurance
iii. Visit safety (eg, animals, weapons)
iv. Community safety
v. Personal protection equipment (PPE)
vi. Hazardous materials and Safety Data Sheet (SDS) location
s. Therapy supplies and equipment, including:
i. Description of therapy supplies issued by agency for clinician use during visits
ii. Policies regarding issuance of supplies/equipment to patients or caregivers
iii. Process for checking out and caring for therapy modalities (eg, ultrasound,
neuromuscular electrical nerve stimulation [NMES])
iv. Infection control with equipment use

31
Chapter 4: Orientation to the Agency
CASE SCENARIO
The agency for which Tom and Jessica work has a 2-week orientation, an assigned preceptor, and
a 3-month probation period. They received some initial training in the office and then were assigned
to ride with their preceptor for field training. Competencies were discussed and rated, and the
preceptor was instructed to follow up and verify competency. The preceptors determined the new
clinicians’ readiness for beginning to perform their own visits and provided training reports to the
agency supervisor. The preceptors instructed the patient scheduler to follow a “ramp-up” scheduling
plan to avoid overwhelming Tom and Jessica during their first 2 or 3 weeks of treating patients. The
availability of the preceptors to answer many routine questions from Tom and Jessica lightened the
burden on the agency supervisor while promoting a helpful and encouraging experience for these new
clinicians. Tom and Jessica commented to one another that this was the best orientation they have
ever had, and they are pleased with the support they have felt. Most important, they are satisfied with
their decision to work for this agency and view this as a long-term decision. Agency management has
noticed a 15% reduction in clinician turnover since implementing this comprehensive orientation plan
2 years ago, and their patient satisfaction scores have been climbing steadily.
PRACTICAL APPLICATION
• Home Health Agency PT/PTA Orientation: Administrative Policies and Procedures
• Home Health Agency PT/PTA Orientation: Direct Patient Care Policies and Procedures
• Orientation/Human Resources: Common Resources

32
Providing Physical Therapy in the Home
Table 4.1. Home Health Agency PT/PTA Orientation: Administrative
Policies and Procedures
Administrative Policies
And Procedures
Description
£
Agency philosophy
• Mission statement
• Company values
• Company’s vision
£
Agency organizational
structure
• Hierarchy/ownership
• Reporting structure for clinical and administrative issues
• Corporate compliance with regulatory and ethical matters
• List of agency contact information
£
Policy and procedure manual
• Agency-specific forms for PT/PTA signature
• Employee handbook
£
Risk management and quality
improvement efforts
• Occurrence reporting
• Complaint response process
• Quality improvement initiatives (eg, outcomes,
patient experience)
• Accrediting agency requirements (if applicable)
£
Regulatory overview
• Municipal, state, and federal rules and regulations
• HIPAA
• Reimbursement source/third-party payer requirements
• Quality assurance, improvement programs, and
public reporting
• (OBQI/OBQM, OASIS Quality/Process Measures, Home Health
Compare, HHCAHPS)
£
Services provided by the
agency
• Nursing, PT, OT, SLP, social work, dietetics, care sitting, etc
£
Hours of operation
• Regular service hours
• On-call service, including plans for staffing weekends and
holidays (eg, on-call schedule)
£
Time-off/vacation requests
• Request policy/procedure and approval considerations
• Coverage planning/expectations, including procedure for
ensuring adequate PTA supervision is maintained (where
applicable)
£
Payroll instructions/processes
• Due dates, timesheets, and submission process
£
Performance evaluations
• Key performance expectations
• Evaluation schedule/frequency

33
Chapter 4: Orientation to the Agency
£
Professional responsibilities/
expectations
• Continuing competence
• Professional growth/development
• Mentoring clinicians new to home care
• Mentoring students
£
Employee benefits information
• Per agency
£
Job description
• Required work hours
• Productivity expectations
• Physical job demands
• In-home visit time expectations
• Documentation expectations
• Required meeting attendance
• Interdisciplinary communication
• On-call expectations for weekends/holidays
• Other agency-specific items
£
Agency interdisciplinary
communication processes
• Team meetings, initial case report, status report, discharge
notification, and reassessment planning
• Communication logistics (eg, onsite meeting,
phone call, e-mail)
• Documentation requirements
• Meeting frequency and expected duration
• Attendance/participation requirements and expectations
• Meeting preparation
Table 4.1. (Continued)

34
Providing Physical Therapy in the Home
Table 4.2. Home Health Agency PT/PTA Orientation: Direct Patient Care
Policies and Procedures
Direct Patient Care
Policies and Procedures
Description
£
Patient care processes
• Timely management of new referrals
• Appointment scheduling
• Verification of appropriate visit types
• Securing additional orders from the physician
• Patient admission information, including start-of-care
contents, consent forms, home folder contents (eg, rights and
responsibilities, privacy, complaint procedure)
£
Patient admission/start-of-
care forms and policies/
procedures
• Home folder contents
• Consent forms
• Patient rights and responsibilities
• Privacy
• Complaint procedure
£
Chart review
• Locating patient demographics
• Advance directives
• Physician orders
• Medication profile
• Diagnoses/coding
• Homebound status
• Other
£
Clinical competency/skills
assessment
• Clinician self-assessment of skills and certifications
• Competency verification by supervisor/preceptor, with regard to
clinical skills, tests and measures, OASIS, oxygen safety, infection
control, etc
• Training to recognize abuse and neglect, and reporting
procedures
• Field observation
• Competency testing
• Other competency requirements per agency policy
£
Basic life support training
requirements
• Refer to APTA guidance
• Specify requirements (hands-on vs online) for both initial
certification and renewal
£
Infection control
• Universal precautions
• Hand washing
• Bag technique
• Equipment management/cleaning
£
Dress code and
appearance
• Per agency policy

35
Chapter 4: Orientation to the Agency
£
Physician orders/
communication
• Organizing communication to physician with standardized
method for efficiency (eg, SBAR)
• Obtaining and appropriately documenting receipt of verbal orders
• Timely communication regarding sudden changes in patient
status (eg, vital signs outside parameters, falls, emergency care)
• Managing hold orders (eg, hospital hold, patient request)
£
Homebound status
• Per payer requirements for coverage
£
OASIS instructions, time-
points, and management
• Per CMS training materials regarding OASIS
£
Clinical documentation
requirements
• Types of forms/format required (eg, electronic record,
paper forms)
• Approved abbreviation list (including list of “do not use”
abbreviations)
• Physician orders
• Expectations regarding content, including compliance with third-
party payer requirements (eg, local coverage determinations)
• Requirements for timely submission
• Instructions for correct application of clinical instruments, and
tests and measures (eg, OASIS, standardized tests, evidence-
based measures)
• Change of service/discharge notification (eg, patient notification)
• Home logbook documentation
• Agency policy regarding patient/clinician signatures on visit notes
• Other requirements per agency policy
£
Plan of care development
and visit scheduling
• Per evaluation findings, safety considerations, prior level of
function, patient and caregiver goals, and recommended
evidence-based interventions
£
Supervision requirements
for PTs
• PTA supervision (if applicable)
• Home health aide supervision (if applicable)
£
Patient and caregiver safety
• Protocol for requesting emergency care
• Identification of home safety concerns
• Falls prevention education
• Medication profile management/reconciliation
• Procedures for minimizing re-hospitalization
• Oxygen safety
• Competency requirements (eg, field observation,
competency testing)
£
Diagnoses coding
• Per agency policy and training
Table 4.2. (Continued)

36
Providing Physical Therapy in the Home
£
Discharge planning
• Advance patient and caregiver notification
• Discharge instruction forms
• Discharge procedures (eg, interdisciplinary coordination)
£
Emergency preparedness
and disaster response plan
• Review priority codes and triaging process
£
Workplace safety
• Driving safety
• Visit safety (eg, animals, weapons)
• Community safety
• Personal protection devices (PPD)
• Auto insurance
• Hazardous materials and Safety Data Sheet (SDS) location
• Emergency preparedness and disaster response plan
£
Therapy supplies and
equipment
• Description of therapy supplies issued by agency for clinician use
during visits
• Policy regarding issuance of supplies/equipment to patients/
caregivers
• Process for checking out/caring for therapy modality equipment
(eg, ultrasound, NMES)
• Infection control with equipment use
Table 4.2. (Continued)

37
Chapter 4: Orientation to the Agency
Orientation/Human Resources: Common Resources
Centers for Medicare and Medicaid Services (CMS)
Provides health coverage through Medicare, Medicaid, and the Children’s Health Insurance Program
www.cms.gov, www.cms.gov/Medicare/Medicare.html (specific to Medicare, Medicare Advantage
plans, home health quality initiatives, and home health agency centers)
US Department of Health and Human Services (HHS)
Principal federal agency for protecting Americans’ health and providing essential human services,
especially for those least able to help themselves
www.hhs.gov
The Joint Commission
An independent, not-for-profit organization that accredits and certifies health care organizations and
programs in the United States that commit to meeting certain performance standards
www.jointcommission.org
Community Health Accreditation Program (CHAP)
Surveys agencies providing home health, hospice, and home medical equipment services, to
determine if they meet the Medicare conditions of participation and CMS quality standards
www.chapinc.org
OASIS Answers
Includes questions and answers to guide completion of OASIS questions
www.oasisanswers.com
Home Health Compare
Quality of care ratings per OASIS and Medicare quality measures
www.medicare.gov/homehealthcompare
Consumer Assessment of Healthcare Providers and Systems (CAHPS)
Consumer survey to measure the experience of people receiving home health care from Medicare-
certified home health agencies.
www.homehealthcahps.org

38
Providing Physical Therapy in the Home
American Physical Therapy Association
Information relevant to physical therapist practice in home health, though APTA and its specialty sections
www.apta.org
www.homehealthsection.org
www.geriatricspt.org
www.neuropt.org (outcome measure recommendations for stroke, multiple sclerosis, spinal cord
injury, traumatic brain injury)
www.ptnow.org (APTA resource for evidence-based practice)
Rehabilitation Measures Database
Identification and summaries of reliable and valid measurement instruments
www.rehabmeasures.org
NOTE: This is not a comprehensive list, but it includes several established resources to ensure that orientation
material is accurate and appropriate.

39
Chapter 4: Orientation to the Agency
References
1. Accountemps survey: one in three employers lacks orientation program for new hires [news release].
Menlo Park, CA: Accountemps, a division of Robert Half; March 20, 2012. http://accountemps.rhi.
mediaroom.com/orientation. Accessed May 30, 2014.
2. Wallace K. Creating an effective new employee orientation program. Library Leadership & Management.
2009;23(4):168-176. http://journals.tdl.org/llm/index.php/llm/issue/view/116. Accessed May 30, 2014.
3. Lindo DK. New employee orientation is your job! Supervision. August 1999;60(8):6-9. .

CHAPTER 5
41
Chapter 5: Referral Information
REFERRAL INFORMATION
Introduction
Referral information should provide the agency with diagnostic information to assist the physical
therapist with the evaluation process and the development of an appropriate plan of care to address
the patient’s functional deficits. Referral information is received via diverse sources (eg, phone
contact, e-mail, facsimile, databases, tablets). It is important for the agency to pursue a basic set of
information upon receipt of the referral. The physical therapist plays an important role in this process.
The physical therapist should review the orders upon referral and seek clarification from and/or
provide feedback to the physician as indicated. This communication influences the quality of the
plan of care through order clarification. Furthermore, it enhances effective case management and
encourages interdisciplinary dialogue. This chapter provides guidance for agencies and therapists
about essential referral information.

42
Providing Physical Therapy in the Home
GUIDELINE
The physical therapist has available pertinent and legible information from referral sources prior
to the initial patient encounter/visit in order to provide effective case management, inclusive of
comprehensive examination, evaluation, and ongoing intervention.
CRITERIA
1. The information received from the referral source should include:
1
a. Patient information:
i. Name
ii. Date of birth (DOB)
iii. Address and phone number
iv. Languages spoken
1. Interpreter needs, and, if applicable, the name of the interpreter
v. Diagnoses (eg, ICD code, date of onset or exacerbation)
vi. Reason for physical therapy referral
vii. Referral physician order
viii. Date of referral
1. If ordered by the physician, date for physical therapist evaluation
ix. Medical/surgical history (including surgical procedures)
x. Code status
xi. Precautions/restrictions
1. Weight-bearing status
2. Infection control precautions
3. Range of motion restrictions
4. Other precautions/restrictions
xii. Medication profile
xiii. Durable medical equipment (DME) needs (if known)
xiv. Home environment unusual issues
b. Caregiver information
i. Name
ii. Phone numbers (at least 2, if possible)
iii. Relationship to the patient
iv. Availability

43
Chapter 5: Referral Information
v. Health care proxy
1. Emergency contact
a. Name
b. Phone number
c. Payer source information from all payers
i. Payer name(s)
ii. Identification number(s)
d. Referral source/physician information
i. Name (eg, name of the hospital, skilled nursing facility, or physician office)
ii. Discharge date from skilled nursing facility or hospital
e. Duration of stay in the facility
f. Date of last face-to-face encounter, if applicable
g. Information of physician signing plan of care for physical therapy
i. Name
ii. Address
iii. Phone number

44
Providing Physical Therapy in the Home
CASE SCENARIO
A referral with the following information is received June 6 from the intake department of the home
health agency. The agency director agrees to accept the patient and instructs the office patient
scheduler to contact Tom to admit the patient to services with his physical therapy evaluation. Tom
agrees to see this patient, and the information below is securely faxed to his agency office. He tries
to contact the patient but does not get an answer. He then tries contacting the patient’s daughter,
Susan, who replies and tells him that her mother is hard of hearing and sometimes doesn’t answer
the phone. She indicates that Tom can stop by at 3:00 pm today to admit the patient to home health
services. She says that her mother is looking forward to getting stronger.
Orders: PT evaluate & treat, assess for home health aide, occupational therapist
Patient: Mary Jones
MR#: 012345678910
Address: 37 Main Street
Phone: xxx-283-4489
Emergency Contacts: Patient’s daughter, Susan, staying with mother for next week
Emergency Phone: Susan, Home: xxx-609-1245; Mobile: xxx-609-9876
DOB: 1/22/1942 (age 72)
Hospital stay: 5/29/2013 – 5/31/2013
Subacute Rehab: 5/31/2013 – 6/7/2013
D/C home date: 6/7/2013
Dx: s/p fall in home L hip fx ORIF, WBAT LLE
Comorbidities: CHF, DM, HTN
Meds (current): Metoprolol, Hydrocodone, Lisinopril, Lasix
Allergies: NKA
Attending MD: Dr Oz, 46 High St, Phone: 837-6733
Primary Insurance: Medicare
Secondary Insurance: None
Copay: $0/visit
Comments: Please call daughter to schedule
PRACTICAL APPLICATION
• Essential Referral Information

45
Chapter 5: Referral Information
Essential Referral Information
The process of obtaining a history is a vital component of the examination process. If the referral
information is unclear or illegible, the physical therapist is responsible for obtaining clarification directly
from the referral source or via agency resources. The key is to ensure that the physical therapist
has the required information to evaluate the patient and determine an appropriate plan of care for
the patient.
Table 5.1. Essential Referral Information
Primary Information
Patient Name/DOB
Referral Source/
Physician
Payer Source Information
Address/Social Security # Address Insurance #
Phone number Phone number Preauthorization required
Diagnoses Date of referral Copay information
Date of onset SOC date Other pertinent data from insurance
Medical information
Requested date for PT
consult
Multiple payers
Medical/surgical procedures Urgency of initial visit Deductibles/copays
Precautions Physician orders
Evaluation and treat
Secondary Information
Emergency Contact Facility D/C
Home
Environment
Medications
Primary caregiver Length of stay Unusual circumstances List
Contact designee Diagnostic reports Prior level of function
Frequency/
dosages
Power of attorney (POA) Specific care DME needs Special instructions
Health care proxy (HCP) Episode status
Weight-bearing status

CHAPTER 6
47
Chapter 6: Timely Scheduling of the Home Visits
TIMELY SCHEDULING OF THE HOME VISITS
Introduction
Seeing patients in a timely manner is one of the hallmarks of clinical professionalism. It contributes
to improved patient and caregiver experience,
1
improved compliance with regulations/policies,
2
and
positive feedback from referral sources. Patients and caregivers quickly become concerned about
the impact on outcomes when care is delayed, so it is important for agencies and clinicians to
address this issue proactively and responsibly.
Delays in care have various causes. Home health agencies and their field clinicians need to analyze
this issue and determine solutions for minimizing delays, and then implement those solutions. The
seeds of a successful relationship with the patient and caregiver are planted when the patient
recognizes that the physical therapist (PT) truly understands the patient’s medical journey and values
the patient’s time. This level of compassion by the PT is associated with timely and appropriate care,
which results in a positive patient experience. No one is surprised when positive outcomes occur
under these circumstances.

48
Providing Physical Therapy in the Home
GUIDELINE
The physical therapist performs the initial examination and evaluation, and conducts subsequent
visits in a timely manner in coordination with the patient and caregiver.
CRITERIA
1. The physical therapist (PT) or agency managerial designee makes initial telephone contact with
the patient within 24 hours of referral acceptance.
2. The PT contacts the patient and caregiver within 24 hours of being assigned responsibility for
the patient’s initial evaluation and schedules the initial evaluation and examination visit in a timely
manner:
a. In compliance with regulatory and payer requirements
b. In compliance with agency requirements
c. In compliance with physician orders
d. In consideration of the needs of the patient and caregiver
3. If the initial examination and evaluation aren’t provided within the expected timeframe, the PT
contacts the referring physician to coordinate care.
4. Prior arrangements, exceptions, or expectations should be documented and communicated
by the:
a. Referral source
b. Patient
c. Patient’s caregiver(s)
d. Appropriate agency personnel
5. The PT thoroughly reviews referral information to ensure that involved caregivers are made aware
of the appointment (eg, medical power of attorney, surrogate decision maker).

49
Chapter 6: Timely Scheduling of the Home Visits
CASE SCENARIO
Tom is assigned by his home health agency to perform a physical therapy start of care (SOC) on a
patient named Helen. The date of the referral is June 7, so Tom recognizes that the SOC visit must
be performed within 48 hours of this referral in order to be compliant with the Medicare Conditions
of Participation. Meanwhile, the designated office personnel responsible for referral intake verifies
the accuracy of patient insurance, address, and phone number as provided with the referral. Tom
contacts Helen on June 7 to schedule an appointment for 10:00 am on June 8. Tom explains that the
visit will take approximately 1-2 hours and asks that the patient have all of her medications together
for review so that the medication profile can be updated. The phone call is documented in the
electronic medical record (EMR). Tom notes that Helen’s daughter is the medical power of attorney,
so he also calls her to inform her of the visit time and to invite her to attend the appointment.
On June 8, Tom runs a little behind with an earlier appointment, so he calls Helen and her daughter at
9:45 am to let them know he won’t make it there until about 10:15 am. When Tom arrives at 10:15,
Helen and her daughter are welcoming and appreciate him letting them know about the small delay.
Tom completes the admission visit in 90 minutes and, before leaving, confirms the next visit for 10:00
am on June 10. He promises to call and remind Helen the evening before. After he leaves, Helen and
her daughter comment to one another how professional Tom has been, and how glad they are that
they selected his agency to provide home health services.
PRACTICAL APPLICATION
• Scheduling for Patient Satisfaction

50
Providing Physical Therapy in the Home
Scheduling for Patient Satisfaction
In caring for patients within their homes, physical therapists (PTs) function as guests just as much as
clinicians. Part of that privilege necessitates upholding the core values of altruism, compassion, and
professional duty. PTs are to act in the best interests of patients. Three simple rules for scheduling
home visits will assist the PT in being a successful home health clinician.
1. Call the patient to schedule the visit.
2. Set a time and date for the visit.
3. Arrive on time.
Figure 6.1. Patient scheduling timeline.
Changes to schedule are
clearly communicated
to patient.
Interdisciplinary
communication is
coordinated and
documented.
Referral
Initial
Patient
Contact
Date of
Evaluation
Follow-Up
Care at
Regular
Scheduled
Intervals
PTs can gain further insight into a patient’s situation and preferences by examining the referral.
• Does the patient prefer to be addressed by a specific name?
• Is there a time of day that the PT should not call or schedule a visit?
• Should visit dates and times be scheduled with someone other than the patient?
Mindful attention to details will help the PT succeed as a home health clinician.

51
Chapter 6: Timely Scheduling of the Home Visits
References
1. About home health care CAHPS survey. Centers for Medicare and Medicaid Services website.
https://homehealthcahps.org/GeneralInformation/AboutHomeHealthCareCAHPSSurvey.aspx. Accessed
December 16, 2013.
2. State operations manual, appendix B—guidance to surveyors: home health agencies. Centers for
Medicare and Medicaid Services. http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/
GuidanceforLawsAndRegulations/Downloads/som107ap_b_hha.pdf. Updated
August 12, 2005. Accessed December 15, 2013.

CHAPTER 7
53
Chapter 7: Physical Therapy Admissions and Evaluations
PHYSICAL THERAPY ADMISSIONS AND EVALUATIONS
Introduction
The physical therapist (not the physical therapist assistant) is responsible for performing a
comprehensive assessment of the home care patient. The Guide to Physical Therapist Practice
provides insight into the evaluation process with the statement: “To establish the individual’s specific
diagnosis, prognosis, and plan of care through the evaluation process, physical therapists synthesize
the collected examination data …”
1
Also, APTA has endorsed use of the International Classification of
Functioning, Disability, and Health (ICF) as a valuable model for assessing patient function in a holistic
manner.
2
This endorsement provides insight into how the physical therapist evaluation process
continues to evolve toward standardizing and improving the quality of services for the patients served
by our profession.
Clinicians not yet familiar with the ICF model and terminology should educate themselves about it and
begin using it as a means to improve the quality of their evaluations and care planning. In the future,
use of the ICF model and its terminology may be required.
3
The World Health Organization (WHO)
has already prepared a checklist to help clinicians learn to apply the concepts of the ICF.
4
Some of
the key terms associated with the ICF model include:
• Health condition(s)
• Body function and structure (impairments)
• Activity (limitations)
• Participation (restrictions)
• Environmental factors
• Personal factors
Full consideration of these elements, and use of standardized testing to objectively quantify them
wherever possible, should be viewed as the standard for a quality physical therapist evaluation. This
chapter will help physical therapists align their evaluations to this standard, and enhance their case
management skills when they are tasked with admitting patients to home care services.

54
Providing Physical Therapy in the Home
GUIDELINE
The physical therapist meets the needs of patients, caregivers, and referral sources during the initial
examination and evaluation by applying principles of best practice consistent with the Guide to
Physical Therapist Practice. This includes an evidence-based approach that involves an appropriate
and adequate selection of standardized tests for objective measurement and a documented
explanation of the patient’s current functional status using terminology consistent with the ICF model.
CRITERIA
Physical therapists are prepared to address the following areas as appropriate, per the Guide to
Physical Therapist Practice
1
by documenting patient status for any of the following items applicable
to patient status:
1. Health Conditions
a. History, to include relevant:
i. Medical history
ii. Surgical history
b. Diagnoses
i. Primary and secondary
ii. Verify that coded diagnoses are accurate and support medical necessity for
physical therapist services
2. Body Function and Structure
a. Aerobic capacity and endurance
b. Anthropometric measures
i. Height, weight, girth/circumference, and limb length(s)
c. Balance
i. Use of standardized, evidence-based, and objective assessments
d. Circulation
i. Vital sign assessment of blood pressure, respiratory rate, pulse, and temperature
ii. Oxygen saturation readings with patients requiring monitoring in response to activity
iii. Use of standardized, evidence-based, and objective assessments (refer to Practical
Application section of this chapter)
iv. Assessment for signs and symptoms of embolus or deep vein thrombosis (DVT) for
postoperative and sedentary patients
e. Cranial and peripheral nerve testing and reflex integrity
i. Auditory, visual, and vestibular function
ii. Light touch, position sense
iii. Deep tendon reflexes (DTR)

55
Chapter 7: Physical Therapy Admissions and Evaluations
f. Gait and locomotion
i. Gait analysis, including objective measures of walking speed and distance, as well
as description of deviations
ii. All applicable surfaces (eg, level, uneven, sloped, stairs)
iii. Weight-bearing status
iv. Assistive device(s)
v. Human assistance needed
vi. Footwear and other devices (eg, orthotics/prosthetics)
g. Integumentary integrity
i. Skin color/pallor, temperature, turgor, nail beds, hair
ii. Lesions/abnormalities
iii. Wound assessment/measurement, including signs and symptoms of potential
wound infection
iv. Pressure ulcer risk assessment
h. Joint integrity and mobility testing, and range of motion
i. Special testing as indicated
ii. Active range of motion (AROM)
iii. Passive range of motion (PROM)
i. Mental functions
i. Ability to learn/process commands
ii. Communication skills
iii. Orientation to person, place, and time
iv. Short-term and long-term memory
j. Motor function and muscle performance
i. Dexterity
ii. Muscle endurance
iii. Fine and gross motor control
iv. Manual muscle tests
v. Muscle performance tests
vi. Dynamometry
vii. Physical capacity tests
k. Neuromotor development and sensory processing
i. Babinski/clonus
ii. Tone
iii. Reflex integration/abnormal reflexes

56
Providing Physical Therapy in the Home
l. Pain
i. Use of a standardized measure of pain
ii. Assessment of impact of pain on activity and participation
m. Posture/body mechanics
i. Resting posture (supine, sitting, standing)
ii. Posture during functional activities
3. Activities
a. Learning and applying knowledge
b. Communication
c. Mobility
d. Self-care, home management, and domestic life
i. Activities of daily living (ADLs)
ii. Instrumental activities of daily living (IADLs)
4. Participation
a. Identification of roles for participation in:
i. Community (eg, pharmacy, physician appointment, church)
ii. Leisure integration (eg, shopping)
iii. Social interaction (eg, family reunions)
iv. Work/employment (eg, performing job duties, yard work)
v. Educational pursuits (eg, attending school)
5. Environmental factors
a. Products/technology
i. Food/nutrition
ii. Medication profile
iii. Ability to use telephone
iv. Assistive, adaptive, supportive, and protective devices
1. Identification of durable medical equipment (DME) and assistive devices used
2. Identification of DME and assistive devices needed for safe function, including
orthotic/prosthetic requirements
v. Presence of or need for ramps to help access home environment safely
b. Home environment
i. Adaptations (eg, bed, furniture risers, modifications, ergonomics)
ii. Lighting
iii. Room temperature
iv. Safety hazards (eg, fire safety)
v. Architectural barriers and falls risk factors
57
Chapter 7: Physical Therapy Admissions and Evaluations
c. Social support and health services
i. Home health agency staff
ii. Family/caregivers
iii. Sitters
d. Attitudes
i. Family
ii. Caregivers
iii. Friends
e. Community services and transportation
6. Personal factors
a. Lifestyle and habits
b. Socioeconomic status and possible impact on care
c. Education level and ability to comprehend instructions
d. Effect of life events on function
e. Race/ethnicity/sexual orientation
f. Emotional state and depression
i. Depression assessment per best practice (eg, OASIS)

58
Providing Physical Therapy in the Home
CASE SCENARIO
Tom arrives at the home of the patient, Mary, introduces himself, and talks with Mary and her daughter
to determine Mary’s prior level of function (PLOF), the details of the fall, and her hospital and rehab
stay. He takes vitals, does a functional assessment, and then focuses on specific neuromuscular
areas. He reviews all the medications that Mary is taking. He also takes a photo of the surgical
wound, assessing the wound and noting the wound care as prescribed by the physician.
During the assessment, Tom instructs Mary in the proper use of her walker. She was using it to stand
and placing it too far in front of her during ambulation. He also adjusts it to the proper height and
reverses the wheels so that it will fit through the doorways in her home. He instructs her in ankle
pumps to help decrease the edema in her left foot and ankle. She is able to perform these correctly.
During the start of care (SOC) visit, Tom determines that Mary has medications in her home from
before her hospitalization. The dosage for Lisinopril was different from what came home from the
SAR, and Lasix had been added. Mary had some questions about that. The medication will be
clarified by the primary care physician (PCP) and an order/referral made for the nurse.
Telehealth screen: With her diagnosis of congestive heart failure (CHF), Tom recommended telehealth,
and Mary and her daughter were agreeable. Tom made a call to the telehealth nurse to begin setup.
Tom left Mary a folder with her patient rights, falls prevention precautions, agency contact numbers,
and a calendar. He scheduled 2 more visits this week, explaining that he would be bringing Jessica,
a PTA, to work with Mary on the next visit. He wrote both dates on Mary’s calendar. He explained that
the OT, nurse, and HHA office would be calling to schedule visits with her.
PRACTICAL APPLICATION
• Standardized Testing Considerations for Home Health Patients
• Using the ICF Model to Complete a Home Health Physical Therapist Evaluation

59
Chapter 7: Physical Therapy Admissions and Evaluations
Table 7.1. Standardized Testing Considerations for Home Health
Patients
5
Category Tests References
Endurance Tests
and Measures
6-Minute Walk Test American Thoracic Society. Guidelines for the six-minute
walk test. Am J Respir Crit Care Med. 2002;166:111-117.
Lusardi MM, Pellecchia GL, Schulman M. Functional
performance in community living older adults. J Geriatr
Phys Ther. 2003;26(3):14-22.
Borg Rating of Perceived
Exertion Scale
Borg GAV. Psycho-physical bases of perceived exertion.
Med Sci Sports Exerc. 1982;14:377–381.
2-Minute Step Test Jones CJ, Rikli RE. Measuring functional fitness of older
adults. J Active Aging. March/April 2002:24-30.
Strength Tests 30-Second Chair Stand
Test and
30-Second Arm Curl Test
Jones CJ, Rikli RE. Measuring functional fitness of older
adults. J Active Aging. March/April 2002:24-30.

60
Providing Physical Therapy in the Home
Gait/Balance
and
Falls Risk
Walking Speed (also
called Comfortable Gait
Speed and Fast Gait
Speed)
Fritz S, Lusardi M. White paper: walking speed: the sixth
vital sign. J Geriatr Phys Ther. 2009;32(2):2-5.
Berg Balance Scale Muir S, Berg K, Chesworth B, et al. Use of the Berg
Balance Scale for predicting multiple falls in community-
dwelling elderly people: a prospective study. Phys Ther.
2008;88:449-459.
Unipedal Stance Test
(also called One-Leg
Stance Test)
Springer BA, Marin R, Cyhan T, et al. Normative values
for the unipedal stance test with eyes open and closed.
J Geriatr Phys Ther. 2007;30(1):8-15.
Timed Up and Go Shumway-Cook A, Brauer S, Woollacott M. Predicting
the probability for falls in community-dwelling older adults
using the timed up & go test. Phys Ther. 2000;80(9):896-
903.
Functional Reach Duncan PW, et al. Functional reach: a new clinical
measure. J Ger. 1990;45:M192-197.
Duncan PW, et al. Functional reach: predictive validity in a
sample of elderly male veterans. J Ger. 1992;47:M93-98.
Sitting Functional Reach
(Forward/Lateral)
Thompson M, Medley A. Forward and lateral sitting
functional reach in younger middle-aged and older
adults. J Geriatr Phys Ther. 2007;30(2):43-48.
Four-Square Step Test Dite W, Temple VA. A clinical test of stepping and change
of direction to identify multiple falling older adults. Arch
Phys Med Rehabil. 2002;83:1566-1571.
Modified Clinical Test of
Sensory Integration on
Balance
Shumway-Cook A, Horak FB. Assessing the influence of
sensory interaction on balance: suggestion from the field.
Phys Ther. 1986;66:1548-1550.
Cohen H, Blatchly CA, Gombash LL. A study of the
clinical test of sensory interaction and balance.
Phys Ther. 1993;73:346-51.
Missouri Alliance for
Home Care Fall Risk
Assessment Tool
Calys M, Gagnon K, Jernigan S. A validation study of
the Missouri Alliance for Home Care fall risk assessment
tool. Home Health Care Management and Practice.
April 2013;25(2):39-44.
Table 7.1. (Continued)

61
Chapter 7: Physical Therapy Admissions and Evaluations
Pain Wong-Baker Faces
Visual Analog Scale
PAINAD
Hockenberry MJ, Wilson D, Winkelstein ML. Wong’s
Essentials of Pediatric Nursing. 7th Ed. St Louis,
2005:1259.
Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies
comparing numerical rating scales, verbal rating scales,
and visual analogue scales for assessment of pain
intensity in adults. J Pain and Symptom Management.
2010;41(6):1073-1093.
Jordan A, Hughes J, Pakresi M, et al. The utility of
PAINAD in assessing pain in a UK population with severe
dementia. Int J Geriatr Psychiat. 2011;26(2):118-126.
Vestibular 4-Item Dynamic
Gait Index
Marcheti G, Whitney S. Construction and validation
of the 4-item Dynamic Gait Index. Phys Ther. 2006;
86:1651-1660.
Table 7.1. (Continued)

62
Providing Physical Therapy in the Home
Figure 7.1. Using the ICF Model to complete a home health physical
therapist evaluation.
6
Products/technology
Food, meds,
telephone use
Assistive devices,
ramps
Lighting, room
temperature,
fire safety
Social support and
health services
Attitudes
Community services/
transportation
Barriers
(job/school/play)
BODY FUNCTION
AND STRUCTURE
(Impairments)
Aerobic capacity
and endurance
Anthropometric measures
Balance
Circulation
Cranial/peripheral
nerve and reflex integrity
Gait and locomotion
Integumentary integrity
Joint integrity/mobility
and range of motion
Mental functions
Motor function/
muscle performance
Neuromotor development
and sensory processing
Posture/body mechanics
Past medical/surgical
history
Primary and secondary
diagnoses
Prior level of function
HEALTH CONDITIONS
Learning/applying
knowledge
Communication
Mobility
Self-care, home
management,
and domestic life
(ADLs/IADLs)
ACTIVITY
(Limitations)
PARTICIPATION
(Restrictions)
Ability to safely engage in
roles associated with
the following activities:
Community
Leisure integration
Social
Work
Education
Examples:
Shopping at
grocery store
Attending church
Going to pharmacy
Physician appointments
Family reunions
Doing yard work
Attending school
Lifestyle/habits
Socioeconomics
Education level
Life events
Race/ethnicity/
sexual orientation
Emotions/depression
PERSONAL FACTORS
ENVIRONMENTAL
FACTORS

63
Chapter 7: Physical Therapy Admissions and Evaluations
References
1. Guide to Physical Therapist Practice 3.0. American Physical Therapy Association; 2014. http://
guidetoptpractice.apta.org/. Accessed August 20, 2014.
2. Bemis-Dougherty A. Practice matters: what is the ICF? PT—Magazine of Physical Therapy. 2009;
17(1):44-46. http://www.apta.org/PTinMotion/2009/2/Feature/PracticeMatters/ICF/. Accessed February
26, 2014.
3. Langham B. International classification of functioning: a common language for case management in a
changing home health environment. The Quarterly Report, Home Health Section of the American Physical
Therapy Association. 2013;48(3):15-18.2.
4. ICF checklist, version 2.1a, clinician form for international classification of functioning, disability and health.
Geneva, Switzerland: World Health Organization; 2003. http://www.who.int/classifications/icf/training/
icfchecklist.pdf. Accessed December 16, 2013.
5. The Home Health Section Toolbox of Standardized Tests and Measures. Home Health Section website.
2013. https://c.ymcdn.com/sites/hhsapta.site-ym.com/resource/resmgr/practice/toolbox_final_9-2013.
pdf. Accessed May 22, 2014.
6. Towards a common language for functioning, disability and health: ICF—the international classification of
functioning, disability and health. Geneva, Switzerland: World Health Organization; 2002. http://www.who.
int/classifications/icf/training/icfbeginnersguide.pdf. Accessed December 16, 2013.

CHAPTER 8
65
Chapter 8: Physical Therapist Plan of Care
PHYSICAL THERAPIST PLAN OF CARE
Introduction
“The development, implementation, management, and evaluation of a patient care plan based on the
physician’s orders constitute skilled therapy services when, because of the patient’s condition, those
activities require the skills of a qualified therapist to ensure the effectiveness of the treatment goals
and ensure medical safety.”
—Medicare Benefit Policy Manual, Chapter 7, Section 40.2.1
1
After the initial examination and evaluation are completed, the physical therapist develops a plan of
care (POC). The POC directs treatment throughout the home health episode. Returning a patient
to his or her prior level of function or maximum functional status is the focus of the POC. During
the initial physical therapist evaluation visit, the physical therapist should review the POC with the
patient or an authorized representative to obtain informed consent. Collaborative care planning may
positively impact patient and caregiver adherence, satisfaction, and outcomes. This chapter provides
guidance for designing and implementing a quality plan of care.

66
Providing Physical Therapy in the Home
GUIDELINE
Consistent with APTA’s Guide to Physical Therapist Practice,
2
and in collaboration with the patient
and caregiver, the physical therapist develops a plan of care (POC) that is based upon principles
of evidence-based practice, that optimizes the functional needs, and that addresses the safety
concerns of the patient and caregiver.
CRITERIA
1. The physical therapist (PT) develops the plan of care (POC), which includes:
a. Specific, functional, and measurable goals developed in collaboration with the patient/
family/caregiver
b. Frequency and duration of physical therapist services
c. Treatments or interventions to be provided to optimize patient participation in ADLs and
IADLs
d. Anticipated plans for discharge
e. Prognosis/rehabilitation potential
2. The PT reviews the POC with the patient/caregiver.
3. The physician approves the POC with either written or verbal permission.
4. The PT provides appropriate supervision of POC treatments being provided by a PTA and/or
home health aide, in compliance with APTA policy and state and federal regulations.
5. At each visit, the PT assesses and documents the skilled services provided and objectively
measures the patient’s response to the interventions provided. The PT implements program
changes at each visit, as indicated by the inherent complexity of the patient/caregiver.
6. The PT reviews and updates the POC as determined by patient need and regulatory/payer/
agency requirements.

67
Chapter 8: Physical Therapist Plan of Care
CASE SCENARIO
Mary Jones
PT 3w1, 2w3
OT Eval 1w1
SN Assess medications/patient education 1w1
HHA 2w4 assist with personal care
Interventions: Transfer training, gait training, safety education, and therapeutic exercise for LE strengthening
Short-term goals (provide expected date or timeframe for achievement):
1. Improve bilateral lower extremity strength in the hips and knees to 4/5 to improve patient’s ability
to transfer safely and independently
2. Improve transfers from minimum assistance to independent to improve safety and independence
in the home
Long-term goals (provide expected date or timeframe for achievement):
1. Patient to ambulate 200 ft independently using appropriate device to enable patient to access
entire home
2. Improve patient’s ability to ascend and descend 4 stairs using railing and cane, requiring
supervision level assistance to enter/exit home safely
3. Improve patient’s 30-Second Chair Stand score to 12 reps to reflect improved functional strength
for safe transfers and reduce falls risk
4. Improve patient’s walking speed to 2.5 ft/sec (within age/gender normal values) to decrease risk
of falls and hospitalization
Rehab Potential: Good for the above goals
Discharge Plan: Outpatient therapy
Following the visit, Tom calls the attending physician for verbal approval of the POC. Tom writes
the orders; he creates a 485 and sends it to the physician electronically or by fax. Tom provides the
referrals for the other disciplines to the appropriate scheduler.
PRACTICAL APPLICATION
• Using the ICF to Construct an Appropriate Plan of Care

68
Providing Physical Therapy in the Home
Using the ICF to Construct an Appropriate Plan of Care
The International Classification of Functioning, Disability, and Health (ICF) is the World Health
Organization’s framework for measuring health and disability. It emphasizes the functioning of
individuals in their environment and the community. The framework can help determine an individual’s
health care and rehabilitative needs. The table below shows how identifying the functional deficits
in terms of activity and participation is helpful for selecting appropriate plan of care interventions,
objective measures, and goals.
Table 8.1. Using the ICF to Construct an Appropriate Plan of Care
3
Activity/
Participation
Problems
Intervention
Considerations
Objective
Measure(s)*
Short-Term (STG)
and Long-Term
(LTG) Goal(s)
Fatigue limits access
to the bedroom and
bathroom located on
the second floor, which
prevents the patient
from showering/bathing.
• Gait/stair training
• Transfer training
• Strengthening
• Home modifications/
DME
• 30-Second Chair
Stand Test (30
SCST)
• 2-Minute Step Test
STG: Patient to perform
30 SCST x 12 reps
to achieve strength to
perform stair-climbing with
supervision by [DATE].
LTG: Patient to complete
50 reps of 2-Minute
Step Test to increase
endurance for safe access
to bathroom by [DATE].
Caregiver doesn’t know
how to safely transport
patient to a physician
appointment because
patient is unsteady.
• Car transfer training
• Balance training
• Berg Balance Test STG: Berg score to
increase from 45/56 to
50/56 to reduce falls risk
by [DATE].
LTG: Caregiver to
demonstrate safe ability
to assist patient with car
transfers by [DATE].

69
Chapter 8: Physical Therapist Plan of Care
Patient is unable to use
walker to get from the
living room to the toilet
safely and timely due to
narrow doorways and
multiple throw rugs.
• Gait training
• Education regarding
timing voiding
• Home modification
(eg, removal of throw
rugs)
• Device/DME training
(eg, change walker
wheels to inside)
• Timed Up and Go
(TUG)
• Walking Speed
STG: All throw rugs
removed in 2 days.
STG: TUG score to
improve from 25 to 18
seconds to decrease falls
risk by [DATE].
LTG: Walking speed to
improve from 1.20 ft/sec
to 2.00 ft/sec so patient
can reach toilet safely and
timely by [DATE].
Patient is unable to
safely walk 800 feet
from apartment to
assisted living facility
dining area due to
fatigue, poor step
clearance, and impaired
balance.
• Cardiovascular
endurance training/
conditioning
• Balance training
• Gait training
• Strengthening
• 6-Minute Walk Test
(6MWT)
• 30-Second Chair
Stand Test (30
SCST)
LTG: Patient to improve
6MWT distance from 200'
to 800' to improve safe
access to dining area by
[DATE].
LTG: 30 SCST score
to improve to 12 reps
to reduce falls risk and
improve step clearance by
[DATE].
Table 8.1. (Continued)

70
Providing Physical Therapy in the Home
References
1. Chapter 7—home health services. In: Medicare Benefit Policy Manual, Rev 179. Washington DC: Centers
for Medicare and Medicaid Services. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/
downloads/bp102c07.pdf. Updated January 14, 2014. Accessed May 30, 2014.
2. Guide to Physical Therapist Practice 3.0. American Physical Therapy Association; 2014.
http://guidetoptpractice.apta.org/. Accessed August 20, 2014.
3. Towards a common language for functioning, disability and health: ICF—the international classification
of functioning, disability and health. Geneva, Switzerland: World Health Organization; 2002.
http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf. Accessed December 16, 2013.

CHAPTER 9
71
Chapter 9: Physical Therapists as Case Managers
PHYSICAL THERAPISTS AS CASE MANAGERS
Introduction
Physical therapists have sufficient knowledge and skills to serve as front line health care providers
and are prepared to be case managers in the home health setting. They admit patients to home
health care with a comprehensive evaluation and examination, performance of a medication
review, coordination of needed services, and management of discharge planning/care transitions.
According to an official statement of the American Physical Therapy Association (APTA) regarding
the role of physical therapists with medication management, physical therapists should be proficient
in “screening, evaluation, collection of information, identification of adverse events/reactions, and
education.”
1
Physical therapists also recognize that patients derive the greatest value from achieving
safe and optimal function both at home and in the community. The purpose of this chapter is to
support home health physical therapists with the guidance and criteria needed to better understand
how to case manage high-quality home health services.

72
Providing Physical Therapy in the Home
GUIDELINE
Home health physical therapists serve as holistic case managers by assuming full responsibility for
each patient’s needs via comprehensive assessments, medication reviews, coordination of services,
education, and timely discharge planning.
CRITERIA
1. Physical therapists (PTs) initiate case management responsibilities via a comprehensive evaluation
and examination consistent with the tenets of the International Classification of Functioning,
Disability, and Health (ICF),
2
which includes consideration of:
a. Health condition
b. Body function and structure
c. Safety with activities at home
d. Safety with community participation outside the home
e. Environmental factors
f. Personal factors
2. PTs deemed competent to do so by their agency may enhance patient safety and prevent adverse
consequences by performing medication reviews, as allowed by state and federal regulations,
to assess for:
a. Accuracy of the medication profile
b. Allergies
c. High-risk medications
d. Medication adherence
e. Medication dosage and frequency
f. Medication interactions
g. Medication knowledge deficit
h. Medication purposes, action, and side effects
i. Oxygen use
j. Polypharmacy
k. Prescription and nonprescription medications, including supplements and ointments/
creams
l. Need for coordination with the appropriate health care provider for resolving any
concerns about medications

73
Chapter 9: Physical Therapists as Case Managers
3. The PT coordinates care with the physician and the interdisciplinary team to provide best
practices with:
a. Risk management, including:
i. Falls risk
ii. Depression
iii. Pressure ulcer risk
iv. Wounds/infection
v. Abuse (physical/emotional/drug)
vi. Environmental hazards, including durable medical equipment (DME) needs
b. Chronic illnesses such as diabetes, congestive heart failure (CHF), and chronic
obstructive pulmonary disease (COPD), by providing:
i. Education about disease management, including typical signs and symptoms
ii. Protocols to follow when signs and symptoms are outside of predefined parameters
(eg, call physician, emergency care)
iii. Education regarding prescribed programs (eg, exercise, positioning, safety)
iv. Coordination of alternative therapies/services
v. Recommendations for equipment to improve safety and quality of life
vi. Information about community resources
c. Pain management
i. Review of pharmacological and nonpharmacological interventions for managing
pain
ii. Instruction in relaxation techniques (eg, breathing exercises, tai chi)
iii. Education to manage pain in coordination with therapy services to improve exercise
tolerance
4. PTs coordinate discharge planning with the interdisciplinary team by:
a. Initiating discharge planning at the time of patient admission
b. Revising/updating goals as needed
c. Avoiding underutilization and overutilization, consistent with the APTA Code of Ethics for
the Physical Therapist
3
d. Arranging the most appropriate care transition after completion of home health services

74
Providing Physical Therapy in the Home
CASE SCENARIO
Tom is the PT case manager for Mary, and Jessica, the PTA, will provide continuing care under
Tom’s supervision. They instruct Mary in transfers, exercises, and correct gait pattern using her
rolling walker. Jessica will continue to progress Mary’s program, adding more exercises, working on
balance, gait, and the stairs. Tom will periodically assess Mary’s progress. Mary is given a written
home exercise program to be performed daily.
The occupational therapist (OT) evaluates the patient on June 11 and sets a frequency of 1w3 to get
Mary a tub transfer bench, instruct her in using it safely, and obtain equipment for helping Mary to
don and doff her own socks and shoes. Tom secures physician orders for home health aide (HHA)
services 2w4 to assist with personal care.
A nurse comes in and assists with getting the proper medications and setting up a medi-planner to
increase Mary’s safety and independence. She helps Mary to understand the status of her disease
and instructs her in the signs and symptoms that indicate the need to call a physician. Mary becomes
proficient with the use of telehealth and is independent within 3 weeks.
Tom manages the case by ensuring that all of Mary’s needs are met and that orders are up-to-date.
Tom is required by his state regulations to assess the patient periodically. Jessica and Tom keep in
touch weekly by e-mail or phone regarding progress and respond in a timely manner to any problems
that arise.
During the third week of care, Jessica finds that Mary has a very low blood pressure and is complaining
of feeling lightheaded and dizzy. Jessica calls the physician, who decreases the Lasix dosage. Jessica
informs Tom about the change and Tom adjusts the medical record to reflect the change.
A PT reassessment is done after 4 weeks. Mary has made significant progress but is still in need of
continued physical therapy and HHA services. The OT has met their goals and is discharged. Tom
determines that skilled services will continue another 4 weeks until the end of the certification period.
Mary has made great progress at 7 weeks after SOC, which was the 19th visit reassessment. She
is able to get in and out of bed, on and off the toilet, and shower independently. Mary still needs
assistance with her IADLs and groceries. The HHA is discharged. Mary is walking with a single point
cane independently in the home, but the physician does not approve driving yet. Mary’s final goal is to
be able to use the stairs independently with a single-point cane. Her wonderful neighbor is willing to
drive her to outpatient physical therapy. On August 6, the PT explains the advance beneficiary notice
of noncoverage form, which Mary signs, agreeing that she will be discharged on August 13.

76
Providing Physical Therapy in the Home
Medication Management
Documentation of medications should always include:
• name of drug
• dose
• type (capsules, tablets, gelcaps)
• route
• frequency
Dose is the measure of drug taken at a time and should, at a minimum, include:
• weight (mg)
• volume (ml)
• number of dosage forms (unit, puff, vial, suppository)
Common medication routes include but are not limited to:
• drops
• inhaled (nebulizer, oxygen, inhaler device)
• injections
• intravenous (IV)
• oral
• parenteral
• rectal and vaginal (suppositories)
• sprays (nasal)
• topical (ointments, pastes, creams, lotions)
• transdermal (patches)
Frequency should be documented as follows, without abbreviations:
• daily
• __ times a day
• every __ hours
• in morning, at bedtime
• before meals, after meals, with meals
• as needed (PRN) for _________ (must state reason; eg, pain, shortness of breath, special
instructions)
• sliding scales
NOTE: The role of physical therapists in medication management is regulated by state licensing boards. It is the
responsibility of each therapist to review and comply with his or her state regulations.

77
Chapter 9: Physical Therapists as Case Managers
OASIS Process Measures Reported to Home Health Compare
Table 9.1. Case Managerial Considerations for the Physical Therapist:
OASIS Quality Process Measures
4
Start of Care (SOC)/Resumption of Care (ROC) OASIS Visits*
OASIS Item Description Process Type
(QM) MO102 Timely initiation of care Timely care
(QM) M1240 Pain assessment conducted Assessment
(QM) M1300 Pressure ulcer risk assessment conducted Assessment
(QM) M1730 Depression assessment conducted Assessment
(QM) M1910 Multifactor falls risk assessment conducted Assessment
(QM) M2250(f) Pressure ulcer prevention in plan of care Care planning
Transfer to Inpatient Facility (TIF)/Discharge (DC) OASIS Visits*
OASIS Item Description Process Type
(QM) M1500 Heart failure symptoms addressed Care plan
implementation
(QM) M2400(a) Diabetic foot care and patient and caregiver education
implemented
Care plan
implementation
(QM) M2400(d) Pain interventions implemented Care plan
implementation
(QM) M2015 Drug education on all medications provided to patient and
caregiver
Education
(QM) M1040/45 Influenza immunization received (flu season) Prevention
(QM) M1050/55 Pneumococcal polysaccharide vaccine received Prevention
(QM) M2400(e) Pressure ulcer prevention implemented Prevention

78
Providing Physical Therapy in the Home
Best Practice Assessments and Intervention Planning
Providing best practice under the current OASIS Quality Process Measures categories requires
fulfillment of the physical therapist’s role to perform best practice assessments on all patients.
Following the assessment, appropriate interventions should be included in the physician-ordered
plan of care, implemented as ordered within the required time frame, and clearly documented in the
medical record. Note that OASIS item guidance allows for preventive interventions to be provided
even if the formal assessment finds the patient not to be at risk for that item.
Figure 9.1. Best practice assessments and intervention planning.
Depression monitoring and care coordination
Falls prevention program and safety education
Pain management interventions and education
Pressure ulcer preventive positioning and education
Diabetic foot care interventions, monitoring, and education
Medication education and care coordination
ASSESSMENT
Depression (eg, PHQ-2)
Multifactor falls risk (eg, MAHC-10)
Pain (eg, numerical scale)
Pressure ulcer risk (eg, Braden Scale)
Diabetic feet/protective sensation
(Semmes Weinstein 5.07g monofilament)
Medications review (identify interactions)
PREVENTION
MEASURES
Falls prevention programs
Pressure ulcer risk precautions and education
Timely care coordination with physician to resolve concerns
Potential medication issues identified and discussed
with physician
Interdisciplinary collaboration to achieve patient/
caregiver goals
POTENTIAL
PLAN OF CARE
INTERVENTIONS

79
Chapter 9: Physical Therapists as Case Managers
References
1. The role of physical therapists in medication management. Official statement. Alexandria, VA: American
Physical Therapy Association; 2010. http://www.apta.org/uploadedFiles/APTAorg/Payment/Medicare/
Coding_and_Billing/Home_Health/Comments/Statement_MedicationManagement_102610.pdf. Accessed
December 9, 2013.
2. Towards a common language for functioning, disability and health: ICF—the international classification
of functioning, disability and health. Geneva, Switzerland: World Health Organization; 2002.
http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf. Accessed December 16, 2013.
3. American Physical Therapy Association House of Delegates. Code of ethics for the physical therapist (HOD
S06-09-07-12). Alexandria, VA: American Physical Therapy Association; 2009. http://www.apta.org/
uploadedFiles/APTAorg/About_Us/Policies/Ethics/CodeofEthics.pdf. Accessed December 9, 2013.
4. Home health quality measures – process [table]. Quality measures. Centers for Medicare and Medicaid
Services website. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/
HomeHealthQualityInits/HHQIQualityMeasures.html. July 2013. Accessed December 17, 2013.

CHAPTER 10
81
Chapter 10: Documentation Requirements in Home Health Care
DOCUMENTATION REQUIREMENTS IN HOME HEALTH CARE
Introduction
Documentation by home health physical therapists serves multiple purposes as a clinical record, a
business document, a legal document, and a source of potential outcomes data for research and
education.
1
In other words, physical therapists and physical therapist assistants are responsible for
producing documentation that meets professional standards,
2
meets payer source requirements for
reimbursement,
3
and complies with legal requirements for licensure within their jurisdiction.
4
The
documentation of skilled services should clearly illustrate the clinical decision-making and problem-
solving processes consistent with contemporary, evidence-based practice.
Given the time and travel constraints associated with home health care, producing documentation
that consistently and efficiently satisfies these requirements can be challenging. Nevertheless, the
standard for quality documentation has been established, and clinicians are obligated to continuously
pursue achievement of that standard. Fortunately, many resources are available to assist clinicians
with this pursuit. For instance, APTA’s Guide to Physical Therapist Practice,
5
the APTA Code of Ethics,
6
Standards of Ethical Conduct,
7
APTA online resources,
2
and the ICF model
8
provide valuable guidance
and instruction. The ICF model, in particular, assists clinicians with a method for consistently framing
their documentation with information that is considered essential for the justification of skilled physical
therapist services. This chapter provides a guideline and criteria for home health documentation
that is general to all visit types, documentation that is unique to specific visit types (eg, evaluation,
reassessments, discharges), and nonvisit documentation.

82
Providing Physical Therapy in the Home
GUIDELINE
The physical therapist and physical therapist assistant complete timely documentation for each visit
performed, providing clear justification for services rendered that is consistent with the essential
requirements specified by APTA, state and federal regulations, home health agency policy, and payer
sources.
CRITERIA
1. Physical therapists (PTs) and physical therapist assistants (PTAs) follow general principles of
documentation,
2
which include but are not limited to:
a. Abbreviations—minimal use, “do not use,” per home health agency policy
b. Addendums/errors—documentation errors must be corrected by drawing a single
line through the error and initialing and dating the error or through the appropriate
mechanism for electronic documentation
c. Functional progress—document status regularly
d. Skilled care—includes problem solving, clinical decision making, objectively measuring
patient response, and standardized testing
e. Timeliness—documentation should be completed the same day as the encounter/visit
f. Terms/phrases to avoid—Avoid generalized statements such as “tolerated treatment
well,” “continue POC,” and “as above”
2. Documentation required for all visits
a. Name of patient
b. Visit date and start/end times
c. Objective tests and measures
d. Vital signs
e. Homebound status, if applicable
f. Medication review (eg, changes, side effects, new medications)
g. Physical therapist intervention(s), including:
i. Rationale/explanation for intervention(s)
ii. Education/cueing (eg, mobility training, body mechanics, safety, home exercise
program, medication effects on exercise and physical activity)
iii. Detailed description of treatment(s)
iv. Objective measure of patient response (eg, Borg scale, vital signs)
v. Assistance required
h. Comparative statement(s) to identify patient progress or lack thereof
i. Current visit vs prior visit
ii. Current visit vs goals
iii. Existing impairments/functional limitations vs prior level of function

83
Chapter 10: Documentation Requirements in Home Health Care
i. Identification of barriers to progress, if applicable
j. Plan for next visit, to include specific modifications/progression of interventions for unmet
goals
k. Modification/update of discharge plan as needed
l. Applicable physician/interdisciplinary communication
m. Appropriate signature(s) that include:
i. Legible physical therapist/physical therapist assistant signature, with full name and
designation
2
ii. If required by home health agency policy, signature of patient or caregiver/power of
attorney
3. Additional documentation pertaining to evaluation visits
a. Start of care/admission visits include:
i. Signed consent forms
ii. Explanation of services
iii. Outcome Assessment Information Set (OASIS)
iv. Acuity/priority status
v. Education regarding advance directives and privacy rights (HIPAA)
b. Initial evaluation/examination visits include:
i. Medical history
ii. Current medical status and diagnoses (eg, medical, rehab)
iii. Medication review/allergies
iv. Prior vs current level of function
v. Impairments and functional limitations
vi. Activity limitations/participation restrictions
vii. Environment/equipment and personal factors
viii. Interventions provided
ix. Patient-centered goals with expected time frame for achievement
x. Rehab potential to achieve plan-of-care goals
xi. Planned interventions and frequency/duration of visits
xii. Discharge plan
c. Reassessment
i. Reassessments performed by PTs in association with the following visits:
1. Resumption of care (ROC)
2. Follow-up to change of patient condition
3. Recertification
4. Functional reassessment required by state/federal regulations

84
Providing Physical Therapy in the Home
ii. Reassessment documentation should include:
1. Standardized testing with explanation of relevance to goals
2. Summary of progress toward goals, or lack thereof
3. Summary of barriers to progress toward goals
4. Justification for why patient requires continued treatment
5. Rationale for any plan of care modifications, including updated goals and visit
frequency changes
d. Discharge visits should include the following components:
i. OASIS assessment when needed
ii. Current level of function with objective measures
iii. Interventions received
iv. Discharge disposition
v. Discharge instructions/discharge notice provided per regulatory requirement
vi. Medication reconciliation
vii. Goals met
viii. Explanation for any unmet goals
ix. Communication with physician regarding recommendations for any ongoing care
4. Nonvisit documentation
a. Supervision
i. PTA supervision may be done with or without a visit per state requirements
ii. Documentation of onsite observation of PTA visit or review and follow-up of PT plan
of care of PTA notes
iii. Ongoing PT and PTA communication regarding patient care and any medical issues
that come up during visits made by PTA
b. Care coordination
i. Conferencing to include communication with physician, interdisciplinary team, and
equipment companies
ii. Missed visit/refusal, including date, time, reason, and physician notification
iii. Patient visit scheduling
c. Nonvisit OASIS
i. Transfer to inpatient facility
ii. Nonvisit discharge

85
Chapter 10: Documentation Requirements in Home Health Care
CASE SCENARIO
The home health agency for which Tom works recently received an Additional Documentation Request
(ADR) from Medicare. The agency needs to provide documentation to demonstrate the medical
necessity for the physical therapist services provided. Fortunately, Tom has been documenting
consistent with the ICF model. His documentation clearly identifies the reason for referral and contains
a specific description of the patient’s prior level of function. His documentation includes details about
environmental factors such as devices/equipment being used, and the degree to which the patient
could effectively participate in community functions prior to this episode. He clearly identifies the
patient’s goals, which are integrated into the goals of the physical therapist plan of care. He has
objectively measured impairments of body functions and structures and detailed their impact on
functional mobility/activity participation. He has selected appropriate standardized tests to provide a
baseline status and to evidence progress or the lack thereof in response to the plan of care.
The rationale for selected interventions is based on principles of best practice and current evidence.
Functional mobility training includes both a description of deviations and the teaching provided to
correct them. Therapeutic exercises for strengthening include appropriate resistance based upon
the overload principle. Tom has instructed the patient in a home exercise program, including details
about safe and correct technique. Objective measures of patient response to interventions guide
appropriate intensity and activity progression. Tom regularly documents patient progress toward
goals and completes timely reassessments, updating the plan of care as indicated. He has clearly
documented care coordination with other team members and the physician throughout the episode
of care.
The agency finds that Tom’s documentation makes it easy to prepare a response to this ADR.
The elements of the ICF model are easily identified in the medical record. As a result, the agency
successfully demonstrates that the care provided was skilled and medically necessary to address the
patient’s health condition. Medicare agrees to cover these services in their entirety.
PRACTICAL APPLICATION
• Checklist for Integrating ICF Model With Initial Physical Therapist Evaluation Documentation
• Home Health Physical Therapy Documentation Q&A
• Home Health Skilled Documentation Components by Visit Type
• Highlights From APTA’s Defensible Documentation

86
Providing Physical Therapy in the Home
Table 10.1. Checklist for Integrating ICF Model With Initial Physical
Therapist Evaluation Documentation
8
Checklist Categories Examples
£ Reason for referral (health
condition)
Primary diagnoses
£ Comorbidities
Secondary diagnoses
Medical/surgical history
£ Prior level of function
Community access
Transportation method(s)
Mobility devices used
Human assistance needed
Status with ADLs/IADLs
Patient referred for physical therapy s/p CVA with left
hemiparesis in July 2013. Patient has hypertension and
controls diabetes with his diet. Surgical history includes left
total hip replacement in 2010. Prior to CVA, patient was
independent with all community access using personal
vehicle, using a single-point cane for ambulation. Managed
all ADLs and IADLs independently.
£ Impaired body functions and
structures
Specify involved body system(s)
and structural deficits
Left side of body with neurologic impairment involving
abnormal tone, synergistic movement patterns, and
musculoskeletal weakness. Musculoskeletal range of
motion (ROM) deficit with 80 degrees of passive left
shoulder flexion and abduction. Left shoulder joint subluxed
and painful, rated 4/10 at rest. Impaired gait with deviations
including short left foot stance time, left foot drop, and
slow walking speed (1.20 ft/sec). Endocrine system with
impaired insulin resistance. Cardiovascular impairment:
right upper arm blood pressure 160/90.
£ Activity limitations
Deficits with ADLs/IADLs
Deficits with transfers
Deficits with gait
Home management
£ Environmental factors
Medications, food
DME/devices used
Social support
Attitudes
£ Participation restrictions
Community integration
Social involvement
Patient requires moderate assistance with bathing and
hygiene, and minimal assistance with bed mobility. Requires
minimal assistance and a hemi-walker for safe ambulation.
Fatigue limits ambulation distance to 20 feet. Requires
moderate assistance to reach clothing or dress self.
Patient unable to attend church services, and his daughter
manages grocery shopping, medications, and finances. He
is unable to safely access bathroom due to low toilet and
narrow doorway, and doesn’t have a bedside commode.
Daughter plans to arrange for Meals on Wheels. Patient
is agreeable to participate in therapy. Daughter states she
doesn’t have time to help patient with exercises.

87
Chapter 10: Documentation Requirements in Home Health Care
£ Personal factors
Patient goals
Medication profile
Patient is frustrated with situation and depressed about
lack of independence. He doesn’t want to be a burden for
his daughter.
£ Rehab potential (to meet goals)
£ Plan of care
Frequency/duration
Interventions
Short- and long-term goals
Discharge plan
Good rehab potential to meet stated goals of plan of care.
Physical therapy 3w4, 2w4 effective week of [DATE] to
provide training to address deficits with gait, transfers, bed
mobility, home safety, falls risk, and neuromuscular function.
Coordinate medication management with physician and
with patient and caregiver. Order bedside commode.
Request evaluations by OT and MSW and plan to discharge
patient to independent function at home.
(List objective short- and long-term goals with expected
achievement dates.)
Table 10.1. (Continued)

88
Providing Physical Therapy in the Home
Home Health Physical Therapy Documentation Q&A
Q. Sometimes I am too busy and forget to perform any standardized testing during evaluation visits,
and so I don’t have any objective measures documented. Is that okay?
A. Therapists must include objective measures to quantify impairments on evaluation to form a
baseline. Without an objective baseline, it is difficult to substantiate any changes in patient status
during subsequent reassessments. A documented explanation of the significance of these tests and
measures provides valuable support to justify the physical therapist plan of care. If these tests aren’t
performed during the initial evaluation, the physical therapist should arrange to complete such testing
during the next visit.
Q. What are some examples of objective measures that I should use routinely?
A. Objective measures should be selected carefully based upon their ability to provide a baseline
of the patient’s condition. The Centers for Medicare and Medicaid Services (CMS) recommends
that clinicians seek guidance from their professional associations.
9
The American Physical Therapy
Association has developed www.ptnow.org as a resource for this type of guidance.
Q. My documentation shows that the patient performed more reps with exercises today compared
with the prior visit. Isn’t that enough to show skilled care?
A. It is very important for the documentation to establish that the inherent complexity of the exercises
is such that they could not be performed by a nonskilled caregiver. For example, documenting why
the number of reps was appropriate helps to demonstrate client response (eg, Borg/RPE scale).
Furthermore, skilled care is demonstrated by documenting the education required to ensure safe
exercise performance, including instructions/guidance about when to rest.
Q. If I modify performance of a standardized test due to patient difficulty (eg, has to use arms to stand
up from a chair for 30-Second Chair Stand Test), may I still compare the results with normative values?
A. No. The normative values should only be compared with tests performed exactly as described in
the literature. However, if the modification is consistent from one test to another, you may compare
the results between those tests to demonstrate progress. For example, a patient who uses her arms
to complete the 30-Second Chair Stand Test can show progress if the number of reps changed from
4 to 7 between assessments.

89
Chapter 10: Documentation Requirements in Home Health Care
Q. If the patient achieves a goal prior to the end of the plan of care, is it okay to continue with that
intervention without modifying the goal?
A. In general, if the goal has been met, justifying the medical necessity for providing the same
interventions with a restorative plan of care is difficult. If concerns exist about patient safety and/or
the patient’s ability to maintain that status, the evaluating clinician should determine whether a skilled
maintenance plan of care is appropriate. In the absence of a skilled need for maintenance therapy,
the goal should be updated or the intervention should be discontinued.
Q. Does documenting improvements in ambulation distance demonstrate medical necessity for
skilled therapy services?
A. In general, medical necessity and skill may not be demonstrated if distance is the only factor
documented. For example, the medical necessity and skill associated with gait training depends
upon documentation of teaching being provided to correct gait deviations, the patient’s ability to
safely access his or her home environment/community (including human assistance needed), and the
appropriateness of devices being used for ambulation. Goals for ambulation distance should reflect
the documented needs of the patient’s home environment and community participation.
Q. My agency uses an electronic medical record, which allows me to copy and paste the same
intervention text from one visit note to the next. This saves a lot of documentation time. Is this okay?
A. This is very risky. Intervention documentation for each visit should stand alone with the unique
documentation of services and teaching provided during that visit. Clinicians must be cautious to avoid
duplicating documentation from one visit to another, which presents a “cookie-cutter” appearance
that makes it difficult to substantiate ongoing skilled services. It is critical to refrain from copying and
pasting any assessment information from one visit note to another. This is unprofessional and fails to
denote that any ongoing skilled assessment is occurring. CMS is expected to scrutinize this further
with the expanded use of electronic health records.
10

90
Providing Physical Therapy in the Home
Home Health Skilled Documentation Components by Visit Type
Comprehensive Assessments (Start of Care, Resumption of Care, Recertification)
Purpose: Design and individualize plan of care for payment episode
Qualified clinician: PT
Elements:
• Patient demographics
• Informed consent
• OASIS (if required)
• Medical history and comorbidities
• Vital signs
• Health condition, with reason for referral and diagnoses
• Prior level of function
• Personal factors, including medication review/allergies
• Impairment measures (eg, strength, ROM, balance)
• Standardized tests for functional mobility
• Environmental factors, including safety concerns and equipment used/needed
• Clinical judgment and interpretation
• Rationale for skilled interventions
• Objective measures of response to interventions (eg, Borg, pain, vital signs)
• Participation restrictions
• Care coordination
• Visit frequency/duration
• Discharge plan
Visit Note
Purpose: Document interventions, status, and progress toward goals
Qualified clinician(s): PT or PTA
Elements:
• Vital signs
• Pain: pre- and post-treatment
• Interventions designed to achieve functional goals; should include:
Skilled teaching (eg, technique, verbal cues)
Specific description (eg, reps, weights, distance)
Objective patient response (eg, Borg, pain, vital signs)
• Document evidence of progress toward goals or lack thereof

91
Chapter 10: Documentation Requirements in Home Health Care
• Comparison of performance to prior visit(s)
• Description of residual impairments, functional limitations, and education needs
• Equipment training
• Environmental safety education
• Care coordination/conferencing
• Focus/plan for next visit
Reassessments
Purpose: Assess functional progress and modify plan of care as indicated
Qualified clinician(s): PT
Elements:
• Complete both regular visit note documentation and the reassessment
• Complete timely reassessments as required by regulations, payers, and patient need(s)
• Perform standardized testing and objectively quantify patient function
• Explain results of standardized testing, comparing with normative values as appropriate
• Document barriers to progress
• Document summary of progress supported by objective measurements
• Document status with regard to plan of care goals
• If not discharging patient, provide justification for why continued skilled care is indicated,
including rehab potential if goals have changed
• Communicate plan of care changes to physician, including changes to frequency/duration
and goals
Discharge Note
Purpose: Summarize patient’s response to PT plan of care
Qualified clinician(s): PT
Elements
• Ensure patient was notified appropriately of discharge plan
• Complete regular visit note documentation and discharge reassessment
• Justify discharge visit with documentation of skilled interventions provided during that visit
• Coordinate with care team to determine if discharge OASIS is required
• Perform standardized testing and objectively quantify patient function
• Explain results of standardized testing, comparing with normative values as appropriate
• List goals met and explain any unmet goals
• Summarize interventions received
• Document discharge disposition
• Communicate discharge status to care team and physician

92
Providing Physical Therapy in the Home
Table 10.2. Highlights From APTA’s “Defensible Documentation”
2
Tips for
Documenting
Progress
Tips for
Documenting
Evidence-Based
Care
Top 10 Payer
Complaints
About
Documentation
Avoid
• Update patient goals
periodically
• Highlight patient
progress toward goals
• Show comparisons
from previous date to
current date
• Show a focus on
function
• Reassess when
clinically indicated
and according
to regulatory
requirements
• Keep up-to-date with
research through
journal articles and
reviews, ArticleSearch
on PTNow at
PTNow.org
• Include valid and
reliable tests and
measures as
appropriate
• Include standardized
tests and
measures in
clinical documentation
• Poor legibility
• Incomplete
• Date of service not
documented
• Abbreviations—
too many and/or can’t
understand
• Documentation
doesn’t support billing
(coding)
• Skilled care not
demonstrated
• Medical necessity not
demonstrated
• Progress not
demonstrated
(restorative plan of
care)
• Repetitious daily
notes without change
in patient status
• Interventions without
clarification of time,
frequency, or duration
• “Patient tolerated
treatment well”
• “Continue per plan”
• “As above”
• Unknown or confusing
abbreviations
• Adverbs such as
slightly, likely
• Adjectives such as
good, fair, well
• Words “minimal,”
“moderate,” and
“maximal”
Adapted with permission from the American Physical Therapy Association.

93
Chapter 10: Documentation Requirements in Home Health Care
References
1. American Physical Therapy Association. Documentation: tips for improvement. PT—Magazine of Physical
Therapy. January 2006. http://www.apta.org/PTinMotion/2006/1/Feature/GoodTipsDocumentation/.
Accessed December 17, 2013.
2. Defensible documentation for patient/client management. American Physical Therapy Association
website. http://www.apta.org/Documentation/DefensibleDocumentation/. Updated March 28, 2012.
Accessed January 29, 2014.
3. Chapter 7—home health services. In: Medicare Benefit Policy Manual, Rev 179. Washington DC: Centers
for Medicare and Medicaid Services. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/
downloads/bp102c07.pdf. Updated January 14, 2014. Accessed May 30, 2014.
4. Practice acts by state. American Physical Therapy Association website. http://www.apta.org/Licensure/
StatePracticeActs/. Updated April 20, 2014. Accessed May 30, 2014.
5. Guide to Physical Therapist Practice 3.0. American Physical Therapy Association; 2014.
http://guidetoptpractice.apta.org/. Accessed August 20, 2014.
6. American Physical Therapy Association House of Delegates. Code of ethics for the physical therapist
(HOD S06-09-07-12). Alexandria, VA: American Physical Therapy Association; 2009. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/CodeofEthics.pdf. Accessed December 9, 2013.
7. American Physical Therapy Association House of Delegates. Standards of ethical conduct for the physical
therapist assistant (HOD S06-09-20-18). Alexandria, VA: American Physical Therapy Association; 2009.
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/StandardsEthicalConductPTA.pdf.
Accessed December 17, 2013.
8. Towards a common language for functioning, disability and health: ICF—the international classification of
functioning, disability and health. Geneva, Switzerland: World Health Organization; 2002. http://www.who.
int/classifications/icf/training/icfbeginnersguide.pdf. Accessed December 16, 2013.
9. Therapy questions and answers (Q&A #15). Centers for Medicare and Medicaid Services. http://www.
cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HomeHealthPPS/downloads/therapy_questions_
and_answers.pdf. Revised February 28, 2013. Accessed January 27, 2014.
10. Levinson D. CMS and its contractors have adopted few program integrity practices to address
vulnerabilities in EHRs (OEI-01-11-00671). Department of Health and Human Services, Office of the
Inspector General. January 2014. http://oig.hhs.gov/oei/reports/oei-01-11-00571.pdf. Accessed January
29, 2014.

CHAPTER 11
95
Chapter 11: Home Health Physical Therapy Supplies/Equipment and Infection Control
HOME HEALTH PHYSICAL THERAPY SUPPLIES/EQUIPMENT
AND INFECTION CONTROL
Introduction
Physical therapists and physical therapist assistants working in the home health setting need to
be prepared with the necessary supplies and equipment for providing patient care. Many clinicians
store supplies in their vehicles and use a bag to bring supplies into the patient’s home. Some home
health agencies provide supplies, but sometimes clinicians need to assemble their own collection of
supplies and equipment for patient care.
In 2002, the United States saw an estimated 1.2 million infections involving 8 million adult and pediatric
patients receiving home health services.
1
With the expected growth and prevalence of multiple-drug-
resistant organisms, agencies and clinicians need to ensure that policies and procedures are in
place to minimize risk for both themselves and the patients they serve.
2
Clinicians are responsible for
ensuring that their equipment is safe for use with patients. This involves following infection control
measures and ensuring that equipment is serviced appropriately and in a timely way. Clinicians
should use proper bag technique in patients’ homes.
3
Clinicians also should be prepared with all of
the essential forms/documents that may be required during patient visits or encounters. This chapter
provides guidance and criteria for achieving these objectives as part of providing a safe and valuable
patient experience.

96
Providing Physical Therapy in the Home
GUIDELINE
The home health physical therapist and physical therapist assistant prepare and organize their
supplies and equipment, follow infection control procedures, and maintain patient safety.
CRITERIA
1. Physical therapists (PTs) and physical therapist assistants (PTAs) organize supplies and equipment
in their vehicles and supply bags with “clean” and “dirty” areas.
2. PTs and PTAs carry supplies in the following categories (refer to Table 11.1 in the Practical
Application section of this chapter):
a. General
b. Health assessment
c. Quantitative measures
d. Interventions
3. PTs and PTAs apply infection control measures by:
a. Washing hands or using hand sanitizer
b. Following universal precautions with potential contact with blood and other body fluids
c. Maintaining supply bags in clean and orderly state
d. Following appropriate bag technique by not placing supply bags on the floor and by
using a barrier when placing the bag on other surfaces
e. Cleaning/disinfecting reusable supplies and equipment after use
4. PTs and PTAs help to maintain patient safety by:
a. Being prepared to use the following equipment as indicated:
i. CPR pocket mask
ii. Personal protective equipment (PPE), including gloves, gown, and mask
iii. Wrench and screwdrivers (for equipment adjustment)
b. Ensuring that electrical equipment is serviced and calibrated on a timely schedule

97
Chapter 11: Home Health Physical Therapy Supplies/Equipment and Infection Control
CASE SCENARIO
Tom and Jessica are provided some supplies and equipment by the home health agency that employs
them. The agency educates them in infection control, including hand hygiene and bag technique.
Prior to seeing patients, they are issued a supply bag containing:
• CPR pocket mask
• Dressing supplies (bandages, 4x4 gauze, tape)
• Goniometers (8” and 12” sizes)
• Gown, gloves, and mask
• Hand sanitizer and soap
• Oral thermometer and sheaths
• Pulse oximeter
• Sphygmanometer and stethoscope
• Stopwatch
• Elastic band
• Wax paper, drape, or paper towel to be used as a barrier
The supply bag is large enough to hold essential supplies and a laptop. The polyester covering
is easy to sanitize with wipes. In addition to the agency-issued supplies, Tom and Jessica each
purchase a balance pad for advanced balance training and a rolling tape measure to accurately
measure distances and calculate walking speed. They purchase their own sets of adjustable ankle
weights to provide resistance training during strengthening exercises.
Both clinicians perform hand hygiene before and after providing patient care, and prior to entering
their home health bag’s clean section. They also place a barrier between their supply bag and the
couch where they set the bag. Sometimes they hang the bag from a door handle if no surface is
suitable for resting the bag. They also use the barrier, such as wax paper, drape, or paper towel,
between ankle weights and the patient’s skin.
During every visit, they check patient temperature, blood pressure, pulse, respiratory rate, and pain
levels. Tom occasionally checks out an ultrasound unit from the office and ensures that it has been
serviced and calibrated annually. They are prepared to document occurrence reports, provide home
exercise programs, complete Advance Beneficiary Notice of Noncoverage forms, and notes for
physicians.
Tom and Jessica feel prepared with the supplies and equipment needed to provide optimal care for
their patients.

99
Chapter 11: Home Health Physical Therapy Supplies/Equipment and Infection Control
Table 11.1. Supplies/Equipment Considerations for Home Health
Physical Therapy
4
General
Health
Assessment
Quantitative
Measuring
Interventions
• Alcohol wipes
• Antibacterial wipes
• Barriers (eg, wax
paper, paper towels,
plastic wrap)
• CPR pocket mask
• Essential forms and/
or equipment for
documentation
• Garbage bags (for
disposables)
• Hand sanitizer and
antibacterial soap
• Personal protective
equipment (PPE):
Disposable gloves
Goggles
Gown
Mask
Shoe covers
• Spill kit
• Supply bag with
“clean” and “dirty”
compartments
• Wrench/screwdriver
• 5.07 monofilament
• Flashlight
• Mirror
• Pulse oximeter
• Reflex hammer
• Sharp/dull instruments
• Sphygmanometer
• Stethoscope
• Thermometer (with
disposable sheaths)
• Tuning fork
• Distance measuring
wheel
• Dynamometer
• Goniometers (8" and
12")
• Stopwatch
• Tape measure
(disposable)
• Balance board
• Cuff weights
• Dumbbells
• Elastic bands/tubing
• Foam balance pad
• Foldable step stool/
riser
• Gait belt
• Home exercise
programs
• Modalities:
Electrical stimulator
Laser
TENS
Ultrasound
• Pedal exerciser
(pedaler)
• Shoulder pulleys
• Transfer board
• Wound care:
Bandages
Scissors
Suture/staple
removal kit

100
Providing Physical Therapy in the Home
Table 11.2. Spaulding’s Scheme for Infection Control
4
Critical Items Semi-Critical Items Non-Critical Items
Devices that enter sterile tissue
or spaces and must be sterile for
use:
Devices that contact mucous
membranes and non-intact skin:
Equipment that contacts intact
skin and thus should be clean
for use or undergo low-level
disinfection:
• IV therapy catheters
• Needles
• Indwelling urinary catheters
• Oral suction catheters
• Thermometers
• Stethoscopes
• Blood pressure cuffs
(sphygmanometers)
• Pulse oximeters
How to manage infection control
in home care:
How to manage infection control
in home care:
How to manage infection control
in home care:
• Sterilize by steam sterilization
• If heat sensitive, ethylene
oxide
• Other liquid sterilants
• High-level disinfection
• Chemical disinfectants (eg,
chlorine, hydrogen peroxide)
• Wipe down with alcohol wipes/
swabs and allow
to dry before use
• Follow manufacturer’s
instructions

101
Chapter 11: Home Health Physical Therapy Supplies/Equipment and Infection Control
References
1. Association for Professionals in Infection Control and Epidemiology (APIC) and Healthcare Infection
Control Practices Advisory Committee (HICPAC). APIC-HICPAC surveillance definitions for home
health care and home hospice infections. HICPAC. February 2008. http://www.apic.org/resource_/
tinymcefilemanager/practice_guidance/hh-surv-def.pdf. Accessed October 8, 2013.
2. Kenneley I. Infection control in home healthcare: an exploratory study of issues for patients and providers.
Home Healthc Nurse. April 2012;30(4);235-245.
3. McGoldrick M. Bag technique: preventing and controlling infections in home care and hospice. Home
Healthc Nurse. January 2014;32(1):39-45.
4. Rhinehart E, McGoldrick M. Infection Control in Home Care and Hospice. 2nd ed. Sudbury, MA: Jones
and Bartlett; 2005:121-125.

CHAPTER 12
103
Chapter 12: Discharge Planning
DISCHARGE PLANNING
Introduction
The dynamic process of discharge planning begins with the initial physical therapist evaluation and
continues until physical therapist services are no longer indicated. The Guide to Physical Therapist
Practice, 2
nd
edition, defines discharge as the “process of ending physical therapy services that have
been provided during a single episode of care, when the anticipated goals and expected outcomes
have been achieved.”
1(678)
The Guide differentiates this from discontinuation, which is a situation
when “termination of physical therapy service occurs prior to achievement of anticipated goals and
expected outcomes.”
1(678)
In June 2013, the American Physical Therapy Association (APTA) House of
Delegates (House) voted to adopt the phrase “conclusion of the episode of care”
2
as a replacement
for the terms discharge and discontinuation. (Language in versions of the Guide to Physical Therapist
Practice published after 2013 follows the House policy, and “discharge” is not used.) However, to
avoid confusion with the specific implications of the concept of ending an episode of care within
home health care, Providing Physical Therapy in the Home uses the term “discharge” in reference to
the above terminology.
A comprehensive discharge plan focuses on achieving patient and caregiver goals by adequately
considering diagnoses, impairments, functional limitations, societal resources, environmental
safety, risk reduction/prevention, community access, and care transition. Discharge planning
involves a collaborative effort with an interdisciplinary team and leads to improved patient
outcomes and satisfaction.
3
This chapter provides guidance and criteria for developing a patient-
centered discharge plan.

104
Providing Physical Therapy in the Home
GUIDELINE
The physical therapist coordinates an appropriate discharge plan to address patient and caregiver
goals.
CRITERIA
1. The physical therapist (PT) considers the impact of the following factors and addresses them
within the discharge plan:
a. Patient diagnoses
b. Physical impairments
c. Functional limitations
d. Societal resources
e. Environmental safety
f. Risk reduction/prevention
g. Community access
h. Care transition(s)
2. The PT evaluates the appropriateness for discharge based upon:
a. Physician changes to the ordered services
b. Patient refusal or change in homebound status
c. Financial concerns
d. Patient progress toward goals of the plan of care, or lack thereof
e. Patient adherence to safety recommendations
3. The PT coordinates discharge planning with the patient and caregiver and the interdisciplinary
team.
4. The PT ensures that the patient/caregiver receives adequate advance notice of planned discharge
date, per regulatory requirements.
5. The PT documents a discharge summary that includes:
a. The reason for referral
b. The number of visits provided
c. A list of therapeutic interventions and education provided
d. Objective measures of the patient’s initial status compared with discharge status
e. Progress toward goals of the plan of care
f. Explanation for unmet goals, including a summary of comorbidities
g. Description of environmental and personal factors
h. Discharge disposition (eg, care transition to other setting, self-care at home)

105
Chapter 12: Discharge Planning
CASE SCENARIO
During the initial physical therapist evaluation with his patient, Mary, Tom reviews her diagnoses
to identify any comorbidities that could affect her rehab potential. Tom evaluates Mary’s physical
impairments and functional limitations and explains to her what he feels would be a realistic outcome.
Tom recommends that Mary have grab bars installed prior to the conclusion of therapy services
so that he can work with her on using them to improve safety with bathroom transfers. Tom also
recommends that they have the railing fixed by the 3 steps exiting the home. Her daughter Susan
indicates that her husband will take care of that.
The goals of the plan of care were established in collaboration with Mary and her daughter Susan.
The goals accounted for Mary’s desire to be able to go out to eat with her friends twice a month,
which would require some assistance from Susan for transportation since Mary doesn’t drive. Susan
plans to transport Mary to and from outpatient physical therapist services after she is discharged
from home health care. In preparation for the conclusion of her home health plan of care, Tom
verifies the outpatient clinic with Mary and reaches out to the physical therapist there to coordinate
the care transition. Tom also ensures that Mary can safely demonstrate the ability to independently
manage bathroom transfers with her new grab bars, and safely exit and enter the home with the new,
sturdy railing.
PRACTICAL APPLICATION
• Considerations for Planning a Safe Patient Discharge
• Documenting an Appropriate Discharge Summary

106
Providing Physical Therapy in the Home
Figure 12.1. Considerations for planning a safe patient discharge.
SAFE PATIENT
DISCHARGE
Diagnoses
Physical
impairments
Functional
limitations
Risk
reduction
and
prevention
Community
access
Care
transaction(s)
Environmental
safety
Societal
resources

107
Chapter 12: Discharge Planning
Documenting an Appropriate Discharge Summary
Discharge date: 8/20/2013
Patient was referred for physical therapy
a
s/p fall with resultant left hip fracture requiring ORIF. Patient
received 12 physical therapy visits
b
beginning on 7/15/2013.
Skilled interventions/education
c
provided were therapeutic exercise, bed mobility training, transfer training,
gait training, and home safety instructions. Patient is doing home exercise program as instructed.
Status of goals:
• 30-Second Chair Stand Test score improved from 3 to 12 reps, indicating improved functional
lower extremity strength and safety during transfers.
d
GOAL MET
e
• Walking speed improved from 1.20 ft/sec to 2.00 ft/sec, indicating reduced risk for falls and
hospitalization. GOAL MET
• Ascending/descending 3 steps to egress house improved from unable to min assist. GOAL
UNMET (arthritic knee pain and poor safety awareness)
f
Patient has good family support
g
with daughter checking on her several times/week. Daughter will be
transporting patient to/from outpatient physical therapist services
h
effective next week.
Key Elements of a Discharge Summary:
a. The reason for referral
b. The number of visits provided
c. A list of therapeutic interventions and education provided
d. Objective measures of the patient’s initial status compared with discharge status
e. Progress toward goals of the plan of care
f. Explanation for unmet goals, including a summary of comorbidities
g. Description of environmental and personal factors
h. Discharge disposition (eg, care transition to other setting, self-care at home)
Note: This is a guideline. Agencies, payers, and licensing bodies may have more or less stringent requirements
for discharge documentation. Clinicians are responsible for knowing what is required. More comprehensive
documentation may be required when the patient is being discharged from all home health agency services, to
reflect appropriate case management.

108
Providing Physical Therapy in the Home
References
1. Guide to Physical Therapist Practice. Rev 2nd ed. Alexandria, VA: American Physical Therapy
Association; 2003.
2. American Physical Therapy Association House of Delegates. Standards of practice for physical therapy
(HOD P06-13-22-15). Alexandria, VA: American Physical Therapy Association; 2013. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Practice/StandardsPractice.pdf. Accessed February 26,
2014.
3. Hearn J, Higginson IJ. Do specialist palliative care teams improve outcomes for cancer patients? A
systematic literature review. Pall Med. 1998;12:317-332.

CHAPTER 13
109
Chapter 13: The Patient Experience
THE PATIENT EXPERIENCE
Introduction
Receiving positive feedback from patients and caregivers is one of the most rewarding aspects of
the physical therapy profession. In the home health setting, clinicians need to recognize that they
are truly guests in the homes of patients and caregivers. The American Physical Therapy Association
produced the Code of Ethics for the Physical Therapist
1
and the Standards of Ethical Conduct for
the Physical Therapist Assistant
2
to inspire the highest standards of care. These documents obligate
physical therapists and physical therapist assistants to act in a “respectful manner toward each
person,” employ “compassionate and caring behaviors,” and collaborate with patients/caregivers
about their health care decisions. Fulfillment of these obligations establishes the foundation for a
positive patient experience.
Various methods exist for collecting, analyzing, and reporting patient satisfaction data. For example,
the Home Health Consumer Assessment of Health Providers and Systems (HHCAHPS) was developed
by the Centers for Medicare and Medicaid Services (CMS) to produce comparable patient satisfaction
data, incentivize agencies to improve quality, and enhance public accountability by increasing the
transparency of services being provided.
3
Another method for collecting information is for home
health agencies to make follow-up phone calls to patients and caregivers. This chapter helps physical
therapists and physical therapist assistants understand their role in helping their agency attain the
highest levels of patient satisfaction.

110
Providing Physical Therapy in the Home
GUIDELINE
The physical therapist and physical therapist assistant provide quality services to patients and
caregivers in the home setting and accept responsibility for contributing to a positive patient
experience.
CRITERIA
1. Physical therapists (PTs) and physical therapist assistants (PTAs) contribute to positive patient
and caregiver satisfaction with home health services by:
a. Providing compassionate care, including:
i. Staying informed about all the care and treatment being provided via regular
collaboration with other care providers
ii. Treating patients as gently as possible
iii. Treating patients/caregivers with courtesy and respect
iv. Understanding and respecting cultural differences
v. Promptly managing patient/caregiver concerns to minimize problems with care
b. Communicating appropriately with patients/caregivers, including:
i. Establishing informed consent for the services to be provided
ii. Ensuring they are consistently aware of arrival times
iii. Educating in easy-to-understand terms
iv. Listening carefully
v. Assisting office personnel with helpful and timely resolution of concerns
c. Managing specific care issues, including but not limited to:
i. Discussing safety in the home environment
ii. Talking about pain, pain management, and its impact on function
iii. Asking to see and then talking with patient/caregiver about all prescription and over-
the-counter (OTC) medications
iv. Inquiring about new/changed prescription and OTC medications and then providing
instruction as indicated regarding:
1. Purpose
2. Timing/scheduling
3. Side effects
v. Following best practices for chronic conditions (eg, heart failure, chronic obstructive
pulmonary disease, diabetes)
vi. Preventive care to minimize pressure ulcer risk
vii. Follow-up questions regarding immunizations (eg, influenza, pneumonia)

111
Chapter 13: The Patient Experience
CASE SCENARIO
A few weeks after her discharge from home care services, Mary receives a survey asking about the
care that she received from the home health agency. She was very happy and gives high marks for
how she was treated by the staff. Everyone was respectful and treated her as gently as possible.
She always knew when to expect a clinician, which made it easier for her to manage her day. When
she had a problem or question she felt that the staff was very well informed, and she was confident
in the answers provided. Mary was glad that the nurses and therapists took the time to discuss
her medications, educate on disease processes, and make home safety recommendations. Jessica
showed her pictures of her hip and provided education about the healing process.
Both Tom and Jessica prepared the patient for the expected muscle soreness associated with the
rehabilitation process and regularly requested feedback about pain/soreness pre- and post-treatment
sessions. Mary gives a glowing report to her friends and family about the quality of care she received.
She reports that the agency was great and helped her get back to normal. Two months later, her
neighbor asks her surgeon for services from this same agency based upon Mary’s recommendation.
PRACTICAL APPLICATION
• How Physical Therapists Can Promote Better Patient Satisfaction Ratings on
HHCAHPS Survey
• Understanding Patient Care Factors that Contribute to High Global Scores on the
HHCAHPS Survey

112
Providing Physical Therapy in the Home
Table 13.1. How Physical Therapists Can Promote Better Patient
Satisfaction Ratings on Home Health Consumers of Healthcare
Providers and Services (HHCAHPS) Survey
Category: Care of Patients Physical Therapist Actions
Were home health providers informed
and up-to-date about the patient’s care/
treatment? (Question 9)
• Communicate with other team members
• Secure understanding of how each discipline contributes
to patient goals
• Collaborate weekly with other team members about
ongoing plans and discharge planning
Was the patient treated as gently as
possible? (Question 16)
• Explain what you are going to do
• Instruct patients to take pain meds prior to therapy visits
to reduce pain
• Ask if they need anything prior to leaving the
patient's home
Was the patient/caregiver treated with
courtesy and respect? (Question 19)
• Treat patients and caregivers the way that you would like
to be treated
• Be respectful of cultural and personal preferences (eg,
removal of shoes, greetings)
• When leaving, replace all items as you found them
Did the patient have any problems with
care received? (Question 24)
• Respond to concerns and implement solutions quickly
Category: Communications
Between Providers and
Patients/Caregivers
Physical Therapist Actions
Was the patient/caregiver informed about
all care to be provided at the SOC?
(Question 2)
• Explain rationale for services to be provided (eg, SN, OT,
HHA, MSW, RD) to patient and caregiver during
SOC visit
Was the patient/caregiver informed about
arrival times? (Question 15)
• Schedule visits on the patient’s calendar
• Inform patients of timeframe for arrival; promptly notify
if running late
Were explanations to patient and caregiver
given in easy-to-understand terms?
(Question 17)
• Use layman’s terminology
• Verify patient understanding
Did providers listen carefully to patient and
caregiver? (Question 18)
• Verbalize understanding
• Respond promptly to address concerns
Did office staff provide timely assistance
and advice? (Questions 22 & 23)
• Build good communicative relationships with office staff
• Promptly communicate changes of patient status, case
manager assignments, scheduling changes, etc

113
Chapter 13: The Patient Experience
Category: Specific Care
Issues
Physical Therapist Actions
Upon admission, did the provider discuss
home safety with the patient/caregiver?
(Question 3)
• Provide safety education (eg, falls prevention, devices)
• Recommend environmental changes
Did the provider ask to see and then
discuss prescription and over-the-counter
(OTC) medications? (Questions 4 & 5)
• Ask to see all medications, ointments/creams, vitamins,
and herbal remedies
• Discuss schedule, purpose, action, and side effects
of medications
• Inquire about medication changes every visit
Did the provider(s) ask about any new or
changed prescription medications and
educate as indicated? (Questions 12,
13, & 14)
• Discuss schedule, purpose, action, and side effects
of medications
• Inquire about medication changes every visit
• Review information/pharmacy handouts
Global Survey Questions
How would the patient/caregiver rate
the home health agency from 0-10?
(Question 20)
Would the patient/caregiver recommend
this agency to family or friends for home
health care? (Question 25)
HHCAHPS questions shown to most strongly influence
positive global survey scores are:
• Care of patients: 9, 16, 19, and 24
• Communication: 15, 17, and 18
Table 13.1. (Continued)

114
Providing Physical Therapy in the Home
Figure 13.1. Understanding patient care factors that contribute to high
global scores on the HHCAHPS
3
survey.
Informed and up-to-date*
Treated gently*
Treated with courtesy/respect*
No problems with care*
Care providers informed/
up-to-date*
Keep patients informed
about arrival times*
Explain in layman’s terms
Listen carefully*
Oce was helpful with advice
Oce help was timely
Discussed home safety
Talked about pain
Talked about Rx/
OTC medications
Asked to see medications
Talked about purpose, side
eects, and schedules for
new/changed medications
PATIENT CARE COMMUNICATION SPECIFIC CARE ISSUES
GLOBAL SCORES
Rate agency 9-10 out of 10
and
definitely refer to
family and friends
*Identified as “key drivers” by Fazzi
4
for improving global scores involving agency rank and patient/
caregiver sentiment for “definitely” recommending agency to family and friends.

115
Chapter 13: The Patient Experience
References
1. American Physical Therapy Association House of Delegates. Code of ethics for the physical therapist
(HOD S06-09-07-12). Alexandria, VA: American Physical Therapy Association; 2009. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/CodeofEthics.pdf. Accessed December 9, 2013.
2. American Physical Therapy Association House of Delegates. Standards of ethical conduct for the physical
therapist assistant (HOD S06-09-20-18). Alexandria, VA: American Physical Therapy Association; 2009.
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/StandardsEthicalConductPTA.pdf.
Accessed December 17, 2013.
3. About home health care CAHPS survey. Centers for Medicare and Medicaid Services website. https://
homehealthcahps.org/GeneralInformation/AboutHomeHealthCareCAHPSSurvey.aspx. Accessed
December 16, 2013.
4. Mazza G. Key drivers for improving HHCAHPS results. Fazzi.com website. http://www.fazzi.com/Key_
Drivers_for_Improving_HHCAHPS_Results.html. Accessed May 1, 2014.

CHAPTER 14
117
Chapter 14: Lifelong Learning and Continuing Competence
LIFELONG LEARNING AND CONTINUING COMPETENCE
Introduction
The health care arena is rapidly changing. Physical therapists and physical therapist assistants
keep up with these changes by accepting the responsibility for lifelong learning and continued
professional competence. In 2007, the American Physical Therapy Association defined continuing
competence as “the ongoing possession and application of contemporary knowledge, skills, and
abilities commensurate with an individual’s (physical therapist or physical therapist assistant) role
within the context of public health, welfare, and safety and defined by a scope of practice and
practice setting.”
1
APTA’s Code of Ethics for the Physical Therapist
2
provides valuable guidance on
how to fulfill this responsibility. It tasks physical therapists to “achieve and maintain professional
competence” through “critical self-assessment,” continued education, and following best practices
by evaluating the “strength of evidence” for interventions provided.
Professional excellence and continued competence may involve several pathways.
3
For example,
some may pursue clinical specialization and/or certification while others may pursue higher levels
of education. Physical therapists also can take opportunities to participate in research or serve in
positions of leadership that promote the profession of physical therapy. These various roles are
important for demonstrating the role of physical therapists in promoting a healthy society. This chapter
encourages physical therapists and physical therapist assistants to fulfill their obligation to society via
a pathway of lifelong learning and continued competence.

118
Providing Physical Therapy in the Home
GUIDELINE
The physical therapist and physical therapist assistant are committed to lifelong learning and
continuing competence.
CRITERIA
1. Physical therapists (PTs) and physical therapist assistants (PTAs) demonstrate their commitment
to lifelong learning and continuing competence by:
a. Fulfilling their roles as health care professionals who promote quality health and wellbeing
in society
b. Complying with contemporary standards of best practice, including reliance on evidence
for clinical decision-making
c. Practicing autonomously in the home health setting, which minimally includes:
i. Collaboration with the physician and the interdisciplinary team
ii. Case management efforts centered on value-based care for patients, including:
1. Supervision of medication management
2. Monitoring emotional health of patients/caregivers
3. Assessing environmental risks and needs for safety modifications
4. Identifying the need for additional services
5. Promotion of functional recovery and societal participation for patients
and caregivers
6. Active participation in care planning meetings
d. Exhibiting the 7 core values of professionalism
4
:
i. Accountability
ii. Altruism
iii. Compassion/caring
iv. Excellence
v. Integrity
vi. Professional duty
vii. Social responsibility
e. Practicing in compliance with the following:
i. Guide to Physical Therapist Practice
5
ii. Standards of Practice for Physical Therapy
6
and Guide for Conduct of the Physical
Therapist Assistant
7
iii. Code of Ethics for the Physical Therapist
2
and Standards of Ethical Conduct for the
Physical Therapist Assistant
8

119
Chapter 14: Lifelong Learning and Continuing Competence
f. Integrating the APTA vision for the profession,
9
which includes the following principles:
i. Identity
ii. Quality
iii. Collaboration
iv. Value
v. Innovation
vi. Consumer-centricity
vii. Access/equity
viii. Advocacy
g. Participating in or supporting clinical research
2. PTs and PTAs regularly perform self-reflection as part of their professional development,
which includes:
a. Determining their current levels of competence
b. Identifying opportunities for growth and development
c. Pursuing higher levels of excellence within their scope of practice; obtaining enhanced
knowledge and skills
d. Participating in opportunities that promote and advance the physical therapy profession
e. Collaborating with professional peers and interdisciplinary teams to optimize
value-based care
f. Establishing short-term and long-term professional goals as part of a lifelong learning
pathway, which may include advanced degrees, specialization, and/or certification

120
Providing Physical Therapy in the Home
CASE SCENARIO
Shortly after beginning to work in the home health setting, Tom recognizes that he needs some
additional training to enhance his case management knowledge and skills. He is particularly interested
in becoming more confident with reviewing the medication profile.
He identifies and completes a pharmacology course for physical therapists. A few months after
completing this training, he determines that one of his patients has been taking both a generic
and a brand name version of the same medication without realizing it. Tom contacts the physician
to seek clarification, and the physician asks that the patient be instructed to discontinue one of
those medications. The physician compliments Tom on his thorough assessment and says that this
could have been hazardous for the patient if it had continued too long. This proves to be a valuable
experience for understanding Tom’s role as a case manager.
Tom subsequently pursues and completes OASIS certification, which he finds to be extremely helpful
for accurately scoring OASIS items. He also completes some training on the use of standardized
tests, which proves to be beneficial for completing reassessments that justify care with sound clinical
evidence. He maintains his membership with the American Physical Therapy Association and the
Home Health Section, which lead to volunteer opportunities and community education activities. Tom
decides to continue on a career path in the home health setting, and plans to pursue further training
to obtain specialization in geriatric care.
PRACTICAL APPLICATION
• Professional Development Pathways for Physical Therapists and Physical Therapist Assistants

121
Chapter 14: Lifelong Learning and Continuing Competence
Table 14.1. Professional Development Pathways for Physical Therapists
and Physical Therapist Assistants
3
Credentialed Clinical
Instructor Program (CCIP)
The CCIP career development pathway is appropriate for PTs and PTAs
working in a clinical setting who seek to develop their teaching skills.
They learn to provide a challenging and educational clinical experience for
students.
Obtain additional information at: www.apta.org/CCIP/
Research
The Foundation for Physical Therapy provides funding for physical therapy
research, supports evidence-based practice, enhances the value of patient
services, and contributes to the development of the next generation of
researchers. Funding supports areas of scientific, clinical, and health
services research. Many of the sections within APTA also award grants that
support research.
Obtain additional information at: http://foundation4pt.org/
Board-Certified Clinical
Specialization
Specialist certification enables a physical therapist to obtain advanced
professional education and proficiency in a selected area of practice.
Clinical specialization focuses on a specific field of practice, requiring
additional knowledge, skill, and experience beyond that of an entry-
level physical therapist. The American Board of Physical Therapy
Specialties (ABPTS) recognizes clinicians who attain this level of advanced
specialization.
Obtain additional information at: www.abpts.org/home.aspx
Postprofessional Degree
There are multiple opportunities for postprofessional degrees, including
postdoctoral, doctoral/graduate programs, transitional doctor of physical
therapy (DPT), and PhD and ScD programs.
Obtain additional information at: www.apta.org/PostprofessionalDegree/
Residency and Fellowship
Programs
Residency and fellowship programs consist of clinical or nonclinical
opportunities for postprofessional mentoring and training. Based on
a foundation in scientific inquiry, they include written and live practical
examinations and evidence-based practice. A physical therapist clinical
fellowship program is similar to the medical model. Fellowship training is not
appropriate for new physical therapist graduates.
Obtain additional information at: www.abptrfe.org/home.aspx
Leadership Development
APTA offers multiple programs and opportunities to develop leadership
skills. For example, a variety of leadership meetings
take place at APTA Combined Sections Meeting (CSM) and
NEXT Conference and Exposition.
Obtain additional information at: www.apta.org/LeadershipDevelopment/

122
Providing Physical Therapy in the Home
PTA Recognition of
Advanced Proficiency
Physical therapist assistants who meet minimum eligibility requirements
may receive APTA's Recognition of Advanced Proficiency for the Physical
Therapist Assistant.
Obtain additional information at: www.apta.org/PTARecognition/
PTA Advanced Proficiency
Pathways (APP)
PTAs can gain advanced proficiency knowledge and skill in a selected
area of work. Participants take online core courses common to all of the
APPs, take content-specific courses for the selected area of work, and
have mentoring experiences with a qualified mentor of the participant's
choosing.
Obtain additional information at: www.apta.org/APP/
Table 14.1. (Continued)

123
Chapter 14: Lifelong Learning and Continuing Competence
References
1. American Physical Therapy Association House of Delegates. Professional development, lifelong learning,
and continuing competence in physical therapy (HOD P05-07-14-14). Alexandria, VA: American Physical
Therapy Association; 2007. http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/HOD/
Professional_Development/ProfessionalDev.pdf. Accessed January 20, 2014.
2. American Physical Therapy Association House of Delegates. Code of ethics for the physical therapist
(HOD S06-09-07-12). Alexandria, VA: American Physical Therapy Association; 2009. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/CodeofEthics.pdf. Accessed December 9, 2013.
3. Career development. American Physical Therapy Association website. http://www.apta.org/
CareerDevelopment/. Updated July 11, 2013. Accessed November 5, 2013.
4. American Physical Therapy Association House of Delegates. Core values (HOD P05-07-19-19).
Alexandria, VA: American Physical Therapy Association; 2007. http://www.apta.org/uploadedFiles/
APTAorg/About_Us/Policies/Ethics/CoreValuesEndorsement.pdf. Accessed December 28, 2013.
5. Guide to Physical Therapist Practice 3.0. American Physical Therapy Association; 2014.
http://guidetoptpractice.apta.org/. Accessed August 20, 2014.
6. American Physical Therapy Association House of Delegates. Standards of practice for physical therapy
(HOD P06-13-22-15). Alexandria, VA: American Physical Therapy Association; 2013. http://www.apta.
org/uploadedFiles/APTAorg/About_Us/Policies/Practice/StandardsPractice.pdf. Accessed January 20,
2014.
7. American Physical Therapy Association Ethics and Judiciary Committee. Guide for conduct of the physical
therapist assistant. Alexandria, VA: American Physical Therapy Association; 2010. http://www.apta.org/
uploadedFiles/APTAorg/Practice_and_Patient_Care/Ethics/GuideforConductofthePTA.pdf. Accessed
December 17, 2013.
8. American Physical Therapy Association House of Delegates. Standards of ethical conduct for the physical
therapist assistant (HOD S06-09-20-18). Alexandria, VA: American Physical Therapy Association; 2009.
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/StandardsEthicalConductPTA.pdf.
Accessed December 17, 2013.
9. American Physical Therapy Association House of Delegates. Vision statement for the physical therapy
profession (HOD P06-13-19-23). Alexandria, VA: American Physical Therapy Association; 2013. http://
www.apta.org/Vision/. Accessed January 20, 2014.

CHAPTER 15
125
Chapter 15: Home Health Physical Therapist Practice Resources and References
HOME HEALTH PHYSICAL THERAPIST PRACTICE RESOURCES
AND REFERENCES
Introduction
In any setting, the physical therapist is responsible for keeping current with evidence-based practice
and staying aware of rules and regulations affecting that practice. In home health, where the physical
therapist practices autonomously, it is essential for the physical therapist to have the resources readily
available to provide timely care for patients. As case manager, the physical therapist is responsible
for identifying all needs of the patient. This includes medication reconciliation and obtaining referrals
for other disciplines.
This chapter provides a list of online resources for physical therapy, rules and regulations affecting
home health, and resources for community support for patients and their families. Also, for the
modern smartphone user, this chapter lists a sampling of free apps available for quick reference to
medications, anatomy, coding, and more.
Online Resources
Physical Therapy Resources
• APTA Advocacy: www.apta.org/advocacy/
• APTA Code of Ethics: www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/
CodeofEthics.pdf
• APTA Guide to Physical Therapist Practice: http://guidetoptpractice.apta.org/
• APTA Policies and Bylaws: www.apta.org/policies/
• Federation of State Boards of Physical Therapy (FSBPT): www.fsbpt.org/index.asp
• FSBPT Licensing Authorities: www.fsbpt.org/licensingAuthorities/index.asp
• Home Health Section of APTA: www.homehealthsection.org/
• PTNow (Evidence-Based Practice): www.ptnow.org/
• State Physical Therapy Practice Acts: www.apta.org/Licensure/StatePracticeActs/

126
Providing Physical Therapy in the Home
Regulatory Resources
• Accreditation for Health Care: www.achc.org/
• CMS Home Health Agency Center: www.cms.hhs.gov/center/hha.asp
• Community Health Accreditation Program: www.chapinc.org/
• CMS Conditions of Participation: http://www.gpo.gov/fdsys/pkg/FR-1997-03-10/pdf/97-5316.pdf
• Home Health PPS: www.cms.hhs.gov/HomeHealthPPS/
• Home Health Quality Initiatives: www.cms.hhs.gov/HomeHealthQualityInits/01_Overview.
asp#TopOfPage
• The Joint Commission: www.jointcommission.org/accreditation/home_care_accreditation.aspx
• Occupational Safety and Health Administration (OSHA): www.osha.gov
Industry Resources
• Alzheimer’s Association: www.alz.org/
• American Heart Association: http://www.heart.org/HEARTORG/
• American Stroke Association: www.strokeassociation.org/STROKEORG/
• Defensible Documentation: www.apta.org/Documentation/DefensibleDocumentation/
• Home Health Compare: http://www.medicare.gov/homehealthcompare/search.html
• National Association for Home Care and Hospice (NAHC): www.nahc.org/
• National Council on Aging: www.ncoa.org
• OASIS Answers Inc: http://www.oasisanswers.com/
• Outcome and Assessment Information Set (OASIS): www.cms.hhs.gov/oasis/
• Parkinson’s Association: www.parkinson.org/ and www.apdaparkinson.org/
• Quality Improvement Organizations: www.cms.gov/Medicare/Quality-Initiatives-Patient-
Assessment-Instruments/QualityImprovementOrgs/index.html
• Services for Seniors—Eldercare Locator: www.eldercare.gov

127
Chapter 15: Home Health Physical Therapist Practice Resources and References
Free Smartphone Apps
(Not all-inclusive, and listing does not imply endorsement by APTA or the Home Health Section)
• iPharmacy: Drug guide and pill identifier
• Micromedex: Drug information
• Epocrates: Drug, disease, and diagnostic information
• Medscape: Mobile WebMD
• iTriage: Health, doctor, symptoms, and health care search
• Visual Anatomy: Interactive reference and education tool
• Find-a-Code ICD10/ICD9+GEMS: Code sets and general equivalency mappings between
ICD-10 and ICD-9
• Educus ICD-9 codes, Version 2011
• ICD 10 Lite 2012: ICD 10 codes

PROVIDING PHYSICAL THERAPY IN THE HOME
PROVIDING PHYSICAL THERAPY IN THE HOME
This comprehensive successor to the APTA Home Health Section’s popular
Guidelines for the Provision of Physical Therapy in the Home reflects the
expanding roles of physical therapists and physical therapist assistants in the
home health setting, changes in reassessment requirements, and increased
public accountability for best practices and positive patient experiences.
Providing Physical Therapy in the Home provides timely guidance to elevate the
quality of physical therapist services in the home care setting to the highest
levels, consistent with the Vision Statement of APTA:
Transforming society by optimizing movement to improve the human experience.
www.APTA.org
Providing
PHYSICAL THERAPY
in the Home
www.homehealthsection.org
P-131
1014/200



