
For Employees Living in All States Except Arizona and Ohio
What’s Inside:
About the JPMorgan Chase U.S. Benefits Program ..........2
Benefits at a Glance .........................................................3
New Employee Action Checklist for the Health Care
and Insurance Plans ........................................................9
The Health Care and Insurance Plans ............................. 11
Medical Plan ..........................................................................11
Dental Plan ...........................................................................26
Vision Plan ...........................................................................28
Spending Accounts — Health Care, Dependent Care,
Transportation (Transit/Parking) .......................................29
Long-Term Disability (LTD) Plan ..........................................32
Life and Accident Insurance Plans ...................................... 33
Group Personal Excess Liability Insurance Plan ...............35
Group Legal Services Plan ..................................................36
The Retirement Savings Program ................................. 37
401(k) Savings Plan .............................................................37
Pension Plan
1
.......................................................................39
Employee Stock Purchase Plan ......................................... 40
Additional Programs/Services ..................................... 40
Who to Call With Benefits Questions ............................. 41
Additional Reminders ....................................................43
Your Privacy Is Important ...................................................43
Appendix ...................................................................... 44
Special Notice for Employees Who Have Been
Reinstated by JPMorgan Chase Within 31 Days ................. 44
Important Definitions ...................................................45
1
For employees hired on or after December 2, 2017, this plan does not apply to you.
EFFECTIVE
January 1, 2023
Highlights of the 2023 JPMorgan Chase
U.S. Benefits Program
Health. Balance. Finances.

2
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
About the JPMorgan Chase
U.S. Benefits Program
JPMorgan Chase is committed to providing a comprehensive set of benefits choices to meet
different employee needs and lifestyles. In return, we ask our employees to take an active role
in designing a personal strategy to help meet their short-term and long-term “health care and
insurance” and “retirement savings” objectives. This brochure provides an overview of the
JPMorgan Chase U.S. Benefits Program, which is applicable to employees except those living in
Arizona or Ohio. For more detailed information about the benefits described
here, please refer to
the Summary Plan Descriptions found on
My Health > Benefits Enrollment > 2023 Benefits
Resources > Benefit Plan Details (Summary Plan Descriptions).
JPMorgan Chase is committed to your wellness, which is why we offer a Wellness Program to
help you and your family get healthy and stay healthy. Because wellness is so much a part of
our culture, we’ve integrated it with our Medical Plan. Your Wellness Program will provide
access to programs such as health coaching, condition management and maternity support.
You’ll also have access to onsite support (where available) from JPMorgan Chase to help you get
the health care you need when you’re at work to supplement the direction you receive from
your doctor. Learn more about the Wellness Program in this brochure and on My Health.
For the definitions used in the tables on the following pages and throughout this brochure,
please see page 45.
About Eligibility
The JPMorgan Chase U.S. Benefits Program described in this brochure is generally available
in whole or in part to most employees on a U.S. payroll who are:
•
Paid salary/regular pay, draw, commissions or production overrides;
•
Employed by JPMorgan Chase & Co. or one of its subsidiaries to the extent that such
subsidiary has adopted the JPMorgan Chase U.S. Benefits Program;
•
Regularly scheduled to work 20 or more hours per week; and
•
On a U.S. payroll of your employer and are subject to FICA taxes.
You are considered a full-time, U.S. benefits-eligible employee if you meet the criteria above
and are regularly scheduled to work 40 hours per week.
You are considered a part-time, U.S. benefits-eligible employee if you meet the criteria above
and are regularly scheduled to work at least 20 but less than 40 hours per week.
Visit My Health — your
centralized online
resource for health care
and wellness benefits
information.
From work: Type “go/myhealth”
into your intranet browser.
From home: Visit
myhealth.jpmorganchase.com.
The JPMorgan Chase U.S. Benefits Program generally is available to most employees on a U.S. payroll who are regularly scheduled to
work 20 hours or more a week and who are employed by JPMorgan Chase & Co. or one of its subsidiaries to the extent that such
subsidiary has adopted the JPMorgan Chase U.S. Benefits Program. This information does not include all of the details contained in the
applicable insurance contracts, plan documents, and trust agreements. If there is any discrepancy between this information and the
governing documents, the governing documents will control. JPMorgan Chase & Co. expressly reserves the right to amend, modify,
reduce, change, or terminate its benefits and plans at any time. The JPMorgan Chase U.S. Benefits Program does not create a contract
or guarantee of employment between JPMorgan Chase and any individual. JPMorgan Chase or you may terminate the employment
relationship at any time.
Making Changes During
the Year
The Health Care and Insurance Plans
elections you make during your Benefits
Enrollment will stay in effect through the
next plan year (or the current plan year if
you enroll during the year as a newly
eligible employee). However, you may be
permitted to change your elections before
the next Annual Benefits Enrollment if
you have a qualified change in status. A
qualified change in status does not permit
you to change your health care company
during the year under the Health Care
and Insurance Plans. Please note: Any
changes you make during the year must
be consistent with your qualified change
in status.
You need to enroll and/or add your
eligible dependents within 31 days of the
qualifying event (90 days if the qualifying
event is the birth or adoption of a child)
for benefits to be effective on the date of
the event.
2
To make these election changes, go to
My Health > Benefits Web Center. Or
through HR Answers.
1
If your newly eligible dependent passes away within
this 90-day period, please contact HR Answers.
2
For employees hired on or after December 2, 2017,
this plan does not apply to you.
Have You Worked...
…for JPMorgan Chase or any of its
predecessor organizations in the past?
If yes, then your prior service may count
toward your eligibility and vesting for
certain JPMorgan Chase benefits plans.
For more specific information, please
see page 44.
Do you live in Arizona or Ohio?
Please refer to the brochure titled “Highlights of the 2023 JPMorgan Chase U.S. Benefits Program —
For Employees Living in Arizona and Ohio” for information about the benefits available to you.

3
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
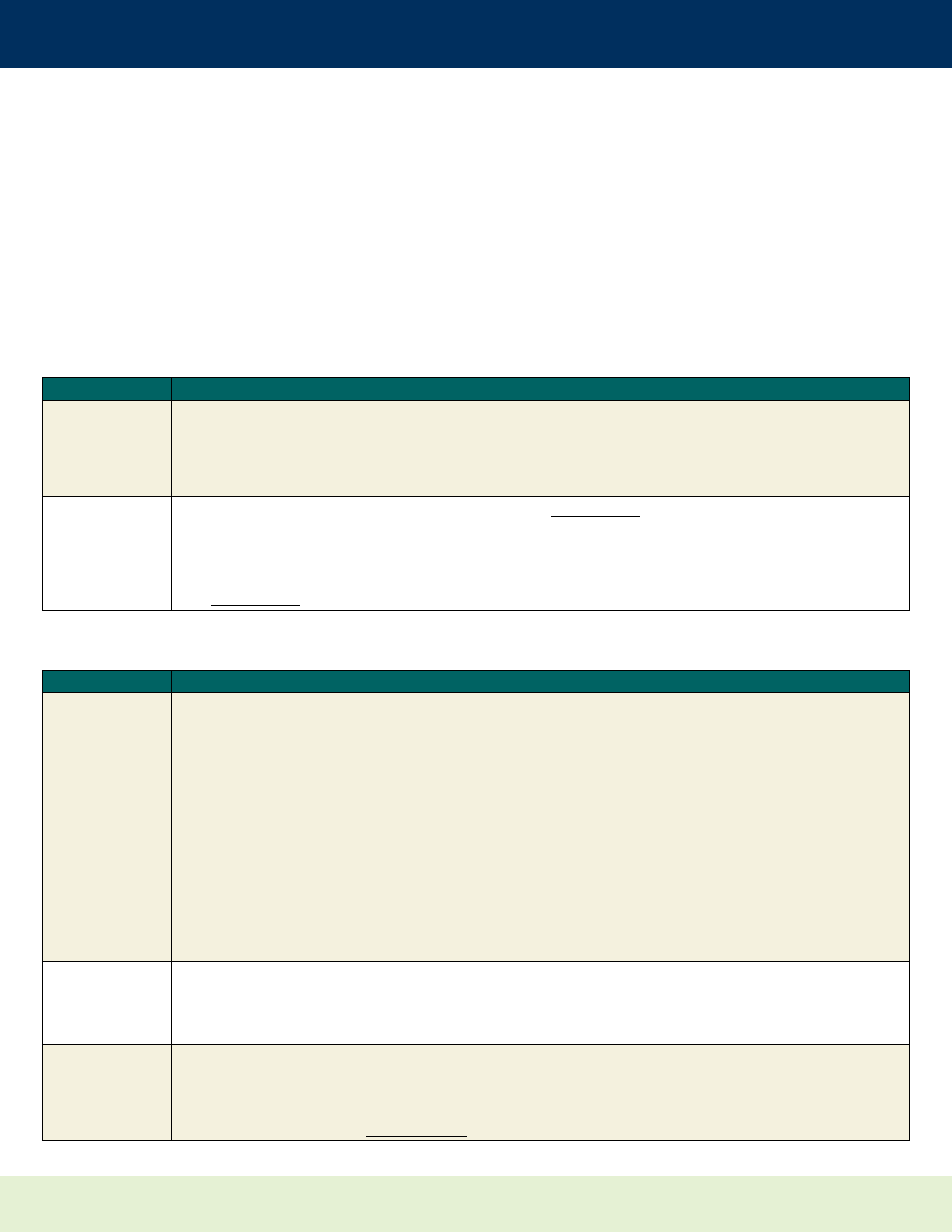
Health Care and Insurance Plans Benefits at a Glance
Benefit Benefits Coverage Summary
When Participation
Begins for New Hires
1
Medical Options 1
and 2
(For all employees
except those in
Arizona and Ohio)
• Two Consumer Driven Health Plan (CDHP) coverage options with a Medical Reimbursement
Account (MRA) feature:
— Option 1 (has higher payroll contributions but lower annual deductibles and coinsurance
maximums)
— Option 2 (has lower payroll contributions but higher annual deductibles and coinsurance
maximums)
— Both options are offered by Aetna and Cigna
• The Medical Reimbursement Account (MRA) helps you pay your share of eligible
out-of-pocket medical and prescription drug expenses. All employees who are enrolled in
the plan can earn funding by participating in certain wellness activities. When your
covered spouse/domestic partner completes certain wellness activities, you earn
additional MRA funding.
• No exclusions for pre-existing conditions
• Eligible in-network preventive care (including annual physical exams and recommended
preventive screenings) and eligible preventive drugs covered at 100% with no deductible,
coinsurance or copayments
• In-network primary care office visits are covered at 90% with no deductible;
— In-network psychologist/therapist office visits are covered at 90% with no deductible
— In-network psychiatrist office visits are covered at 80% with no deductible
• Medical virtual doctor visits are available to you for approximately $5 per virtual visit with
no deductible
• Out-of-network care covered at 50%
• Prescription drug coverage (retail and mail-order) administered by CVS Caremark
— Prescription drug coverage has a completely different plan design than the other
Medical Plan features and is not subject to the same deductibles or coinsurance
maximums.
— Eligible preventive brand and generic drugs are covered at 100% with no deductibles,
copayments or coinsurance. The Mandatory Generic Program applies.
— If you fill a prescription for a brand-name medication when a direct generic equivalent is
available, you will pay the difference in cost between the brand-name drug and generic
drug, plus the generic copay.
— Certain drugs are excluded from coverage.
• Employee and dependent coverage
• JPMorgan Chase and employee cost sharing
• Employee contributions on a before-tax basis are generally determined based on:
— Your level of Total Annual Cash Compensation (excluding overtime)
— The Medical Plan option chosen
— Your geographic location
— Number and type of dependents you cover
— Whether you and/or your covered spouse/domestic partner use tobacco, and
— Whether you and/or your covered spouse/domestic partner complete Initial Wellness
Activities (see page 18)
• You will pay for medical coverage for each covered family member individually
(i.e., employee, spouse/domestic partner and/or each child).
• Full-time employees:
First day of employment
with JPMorgan Chase
• Part-time employees:
First day of the month
following 60 days from
your date of hire
Kaiser HMO Medical
Option
(Additional option
for employees living
in California)
• A primary care physician (PCP) is responsible for wholly managing your care and your
family’s care, including the coordination of care with other providers, such as specialists.
• The Medical Reimbursement Account (MRA) helps you pay your share of eligible
out-of-pocket medical and prescription drug expenses. All employees who are enrolled
in the plan can earn funding by participating in Initial Wellness Activities. When your
covered spouse/domestic partner completes Initial Wellness Activities, you earn additional
MRA funding. The Kaiser HMO Option does not offer incentives for completing Additional
Wellness Activities.
• Most preventive care services are covered at 100% with no deductible. For most services,
like doctor’s office visits, urgent care visits, X-rays, lab work and imaging, you have copays
with no deductible to meet.
• Medical virtual doctor visits are covered at 100%
• Out-of-network care is not covered under the Kaiser HMO Option, except for emergencies
• $1,000 deductible that only applies to a small subset of services (e.g., hospital care,
outpatient surgery), then you’ll share in the cost by paying coinsurance
• See Medical
Options 1 and 2
1
Indicates when participation begins if you enroll when first eligible. If you do not enroll when you are first eligible, your participation will not begin unless you enroll due to a qualified status
change or during subsequent annual benefits enrollment periods. However, you are able to elect to participate at any time under the Transportation Spending Accounts and 401(k) Savings Plan.

4
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Health Care and Insurance Plans Benefits at a Glance
(continued)
Benefit Benefits Coverage Summary
When Participation
Begins for New Hires
1
Kaiser HMO Medical
Option
(continued)
• Employee and dependent coverage
• Prescription drug coverage
— Prescription drug coverage is part of the Kaiser HMO and is administered by Kaiser
Permanente
— Kaiser has its own pharmacies, which must be used to fill your prescription drugs. There
is no prescription deductible
— Eligible preventive generic and brand drugs are covered at 100% at no cost to you
— Kaiser’s list of covered drugs (formulary) is different from CVS Caremark’s
• JPMorgan Chase and employee cost sharing
• Employee contributions on a before-tax basis are generally determined based on:
— Your level of Total Annual Cash Compensation (excluding overtime)
— Number and type of dependents you cover
— Whether you and/or your covered spouse/domestic partner use tobacco, and
— Whether you and/or your covered spouse/domestic partner complete Initial Wellness
Activities (see page 18)
• The deductible and out-of-pocket maximums are fixed for all individuals, regardless of
Total Annual Cash Compensation tier. However, payroll contributions will continue to vary
based on Total Annual Cash Compensation.
• You will pay for medical coverage for each covered family member individually
(i.e., employee, spouse/domestic partner and/or each child).
• MRA and any spending accounts you participate in will be administered by Cigna
Dental
*Independent of the
health care company you
choose for Medical.
• Three coverage options depending on your home zip code:
— Preferred Dentist Program (PDP) Option (MetLife)
— Dental Maintenance Organization (DMO) Option (Aetna*)
— Dental Health Maintenance Organization (DHMO) Option (Cigna*)
• Employee and dependent coverage
• JPMorgan Chase and employee cost sharing
— Employee contributions on a before-tax basis
• See Medical
Vision
• Coverage through EyeMed for eligible vision expenses, such as eye exams, lenses
(including contacts) and eyeglass frames
• Employee and dependent coverage
• You pay the full cost of coverage on a before-tax basis
• See Medical
Spending
Accounts
— Health Care
— Dependent Care
— Transportation
(Transit/Parking)
• Health Care Spending Account — Contributions up to $3,050 annually; up to $610 in
unused funds can carry over for use in the following plan year
• Dependent Care Spending Account — Contributions generally up to $5,000 annually
($2,500 if married and filing separately)
• Transportation Spending Accounts — Contributions for work commuting expenses for
transit and parking. The monthly before-tax limits are $300 for transit and $300 for
parking expenses.
• You pay the full cost of coverage
• See Medical
Long-Term
Disability (LTD)
• For employees earning less than $60,000 in Total Annual Cash Compensation:
— Company-provided coverage of 60% of your Total Annual Cash Compensation
— Fully paid for by JPMorgan Chase
• For employees whose Total Annual Cash Compensation is $60,000 or more:
— Replacement of 50% of Total Annual Cash Compensation; or
— Replacement of 60% of Total Annual Cash Compensation
— Maximum monthly LTD benefit of $20,000
— Tobacco user rates apply
— You pay the full cost of coverage on an after-tax basis
• For employees whose Total Annual Cash Compensation is greater than $400,000:
— Ability to purchase additional LTD coverage under an Individual Disability
Insurance (IDI) policy
— IDI policy provides an additional maximum monthly LTD benefit of up to $15,000
— Fully portable
— Tobacco user rates apply
— You pay the full cost of coverage on an after-tax basis
• See Medical
1
Indicates when participation begins if you enroll when first eligible. If you do not enroll when you are first eligible, your participation will not begin unless you enroll due to a qualified status change or
during subsequent annual benefits enrollment periods. However, you are able to elect to participate at any time under the Transportation Spending Accounts and 401(k) Savings Plan.

5
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Health Care and Insurance Plans Benefits at a Glance
Benefit Benefits Coverage Summary
When Participation Begins
for New Hires
1
Basic Life
Insurance
• Company-provided employee coverage equal to one times Total Annual Cash
Compensation (rounded up to next $1,000) to a maximum of $100,000
• Additional features of the Basic Life Insurance Plan include:
— SurvivorSupport® Financial Counseling Service
— Identity (ID) Theft Assistance Program
— Travel Assistance and Emergency Evacuation Services
— Funeral Concierge Services
• Fully paid for by JPMorgan Chase
• See Medical
Business Travel
Accident Insurance
• Company-provided employee coverage equal to six times annual base salary/
regular pay (minimum of $50,000 and maximum of $3 million)
• Fully paid for by JPMorgan Chase
First day of work with
JPMorgan Chase
Employee and
Dependent
Supplemental Term
Life Insurance
• Employee coverage up to 10 times Total Annual Cash Compensation in $10,000
increments, up to a maximum of $3 million
• Spouse/domestic partner coverage from $10,000 to $300,000 in $10,000
increments
• Child coverage equal to $5,000, $10,000, $15,000 or $20,000 per child
• Employee and spouse/domestic partner tobacco user rates apply
• You pay the full cost of coverage on an after-tax basis
• See Medical
Employee and
Dependent Accidental
Death and
Dismemberment
(AD&D) Insurance
• Employee coverage up to 10 times Eligible Compensation in $10,000 increments, up
to a maximum of $3 million
• Spouse/domestic partner coverage from $10,000 to $600,000 in $10,000
increments
• Child coverage from $10,000 to $100,000 in $10,000 increments per child
• You pay the full cost of coverage on an after-tax basis
• See Medical
Group Personal
Excess Liability
Insurance
• Provides additional liability coverage in excess of the limits carried on your
personal insurance policies, such as homeowners or renters, automobile,
watercraft
• You choose from among three levels of coverage:
— $2 million
— $5 million
— $10 million
• You pay the full cost of coverage on an after-tax basis
• See Medical
Group Legal
Services
• Coverage for attorneys’ fees for routine legal services related to personal and
family legal issues
• Employee and dependent coverage
• You pay the full cost of coverage on an after-tax basis
• See Medical
1
Indicates when participation begins if you enroll when first eligible. If you do not enroll when you are first eligible, your participation will not begin unless you enroll due to a qualified status change or
during subsequent annual benefits enrollment periods. However, you are able to elect to participate at any time under the Transportation Spending Accounts and 401(k) Savings Plan.
(continued)

6
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Retirement Savings Program Benefits at a Glance
Benefit Benefits Coverage Summary
When Participation
Begins for New Hires
401(k) Savings
• Automatic enrollment for new hires at a before-tax per-pay rate of 3% of Ongoing
Compensation, with a 1% annual automatic increase up to a total contribution rate of 10%
unless you elect otherwise. The per-pay contribution rate will apply to your Ongoing
Compensation, which includes base salary/regular pay and any non-annual cash incentives
you receive. Contributions will be invested in a Target Date Fund, based on your age and an
assumed retirement date of 65. These elections will take effect if no action is taken within 31
days of hire/eligibility date
• You can otherwise choose before-tax and/or Roth after-tax contributions up to 50% of
Ongoing Compensation and/or Annual Incentive Compensation
• The maximum IRS contribution limit for all 401(k) employee contributions is $22,500 in 2023
($30,000 for individuals age 50 or older)
• There are two types of company contributions to employees once they complete one year of
total service:
— Automatic pay credits:
• Credits equal 3% of Eligible Compensation (capped at $100,000 annually)
1
regardless of
whether you contribute to the plan
— Matching contributions:
• Dollar-for-dollar up to 5% of Eligible Compensation contributed to the plan for participants
that have Total Annual Cash Compensation of less than $250,000
• Timing and vesting of company contributions:
— Deposited into eligible employees’ accounts annually, following the end of each calendar
year. Employees must generally be employed on December 31 of that year to receive the
company contributions
— 100% vested after three years of total service
— Invested in the same manner as your own employee contributions (for automatic pay
credits, if you have no investment elections on file, the pay credits are invested in the
Target Date Fund that most closely aligns with the year in which you will turn age 65)
• You can choose to invest in a Target Date Fund or among the Core Fund lineup
• When you leave JPMorgan Chase, your vested account balance is generally payable in the
form of a single lump sum, rollover to an IRA or another qualified plan, or installment
payments
• Full-time employees:
Eligible as of your first
day of employment with
JPMorgan Chase
• Part-time employees:
Eligible as of the first day
of the month following
the completion of 60
days of total service
• Automatic enrollment:
Employees will be
automatically enrolled
in the plan 31 days after
their hire/eligibility
date, with payroll
deductions beginning
shortly thereafter,
unless they make other
elections (e.g., to enroll
sooner) or choose not to
participate (e.g., “opt
out”)
• Automatic pay credits
and matching
contributions:
Participants become
eligible on the first day
of the month following
the completion of one
year of total service
Pension Plan
(Please note:
For employees hired
on or after
December 2, 2017,
this plan does
not apply to you)
• For employees hired before December 2, 2017, participation began automatically after one
year of total service
• A notional account was established in your name that grew with pay credits through
December 31, 2019, and interest credits
• Effective January 1, 2020, any existing balances in the Pension Plan continue to earn interest
credits, but no longer earn monthly pay credits
• Instead employees earn automatic pay credits in the 401(k) Savings Plan
• When you leave JPMorgan Chase, your vested account balance is generally payable in the form of a
single lump sum, a rollover to an IRA or another qualified plan, or a variety of annuity options
• Fully paid for by JPMorgan Chase
• Closed to new hires
Employee Stock
Purchase Plan
• Purchase JPMorgan Chase common stock quarterly at a 5% discount
• Contributions are subject to an annual maximum share purchase of $25,000
• Dividends can be automatically reinvested in the Plan at 100% of the FMV on the dividend
payable date, or paid in the form of a cash equivalent (e.g., check)
• No brokerage or commission fees on shares purchased
• Employee salary contributions on an after-tax basis up to 20% of Eligible Compensation per
pay period
• Employees with Total Annual Cash Compensation of $250,000 or more are not eligible
to participate
• Must be hired on or
before September 30
to participate in the
following calendar year
• Election to participate
only during an annual
benefits enrollment
period
Designating Beneficiaries
You may designate beneficiaries for the Life and Accident Insurance Plans, 401(k) Savings Plan and the Pension Plan (for employees with a balance) through
the Online Beneficiary Designations site. This website, which is open to all employees eligible for the JPMorgan Chase U.S. Benefits Program, allows you to
designate beneficiaries electronically. Beneficiary designations made on this site can be reviewed and updated as needed, for instance, in the event of a
status change (divorce, marriage or the birth/adoption of a child).
To access the site:
From work: go/myhealth > Online Beneficiary Designation Site From home: https://beneficiary.jpmorganchase.com
1
For benefits-eligible employees as of December 31, 2018, who are continuously employed, automatic pay credits are equal to 3% to 5% of Eligible Compensation (capped at $100,000 annually)
based on years of pay credit service.
7
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Wellness Program
Nothing is more important than the health of you and your family. That’s why JPMorgan Chase offers a Wellness Program for you and your
enrolled spouse/domestic partner. Our Wellness Program provides resources and services that can help you take charge of your health
and make informed health care decisions for you and your family, including online and telephonic resources.
Wellness is a core part of our culture at JPMorgan Chase. That’s why we’ve integrated it with our Medical Plan.
Earn Wellness Rewards!
When you enroll in the JPMC Medical Plan, you are eligible to earn Wellness Rewards in your Medical Reimbursement Account (MRA) that
you can use to pay for eligible out-of-pocket medical and prescription drug expenses. JPMorgan Chase contributes money to your MRA
when you and/or your covered spouse/domestic partner participate in certain wellness activities each year.
Initial Wellness Activities: If you enroll in the JPMC Medical Plan, you and your covered spouse/domestic partner can earn funds in your
MRA by completing both the biometric Wellness Screening and online Wellness Assessment.
Program Description
Biometric
Wellness
Screening
• Use the Wellness Screening Portal to schedule your appointment at an onsite screening event or JPMC Health &
Wellness Center (where available). Or download a Wellness Screening form to get a free biometric screening at a local
Quest Patient Service Center or lab, CVS MinuteClinic or your in-network doctor’s office.
• For more information about the Wellness Screening and registering on the Portal, go to My Health > How to complete
your biometric Wellness Screening.
Online Wellness
Assessment
• A simple health and lifestyle questionnaire is available on my.cigna.com, even if Aetna or Kaiser Permanente is
your health care company. After you complete the online Wellness Assessment, you’ll see a summary of what
you’re doing well and opportunities to improve. When you finish taking the online Wellness Assessment, be sure to
print the completion page to keep for your records.
• Find the Wellness Assessment on Cigna’s website through My Health > Wellness Activities & Services or go directly
to my.cigna.com.
Additional Wellness Activities: If you enroll in Option 1 or 2 of the JPMC Medical Plan, you and your covered spouse/domestic partner
can choose the activities you want to complete to earn additional funds in your 2023 MRA, including:
Program Description
Health Coaching,
Personal
Action Call,
Condition
Management,
Maternity
Support,
Treatment
Decision
Support and
Online Learning
Programs
• Health coaches can help you set goals to address certain potential health risks — such as creating an exercise
program, developing a healthy eating plan, or building a plan to lower your blood pressure or cholesterol.
• You can discuss the results of your Wellness Screening and Wellness Assessment and create a plan during your
Personal Action Call with your health care company.
• Your health care company will also help you manage a health condition, such as asthma, coronary artery disease,
congestive heart failure, COPD or diabetes.
• Nurses (available through your health care company) can be accessed 24 hours a day, seven days a week to answer
your health questions and give advice.
• Enrollment in the Maternity Support Program must be during your first trimester or within 31 days of your benefits
effective date (and before the child’s birth).
• Get help from your health care company or Included Health with choosing the most appropriate treatment for many
conditions along with names of high-quality, cost-effective physicians near you.
• Two Online Learning Programs are available: Choosing Care Wisely and Planning Your Finances Wisely.
• See pages 20-21 for more information.
Preventive Care
• Preventive care can help you detect a condition early on. The earlier a condition is diagnosed, the sooner you can treat it.
• All age- and gender-appropriate screenings that apply to you are covered 100% in-network.
• You can get a physical, cervical or prostate cancer screening, mammogram or a colonoscopy each year and receive
funds in your MRA.
Expert Medical
Advice
• A voluntary and free service through Included Health, an independent company, that provides employees enrolled
in the U.S. Medical Plan and their covered family members with access to advice from nationally recognized
experts — no matter where you live.
• Get Expert Medical Advice when you and your covered family members want a second expert medical opinion on a
documented diagnosis. Visit Included Health (formerly Ground Rounds) or call 1-888-868-4693.
Wellness Program Benefits at a Glance

8
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Program Description
meQuilibrium Mindfully Managing Stress: Complete an online training program through meQuilibrium to learn about the powerful science
of resilience and cornerstone technique that will help you gain control over your emotions, thoughts and stress.
meQuilibrium Resilience Program: meQuilibrium is a personalized resilience program designed to help you feel more
balanced and capable, no matter what your day brings. Develop new skills with tips, tools, easy-to-do activities and short
videos that will help you practice behaviors to better handle life’s competing demands.
My Finances
and Me
This benefit, which is fully paid for by the firm, provides tools, resources and help to be at your financial best.
• Get a Financial Wellness Score™ and Action Plan; and
• Attend a group education session on a variety of topics, such as paying off debt, managing cash flow, and estate and
retirement planning.
The administration of the Wellness Program is provided by Cigna, even if you have selected Aetna or Kaiser Permanente as your
health care company. However, if you select Aetna, Aetna will maintain your MRA account and administer certain components of
your Wellness Program. If you select Kaiser Permanente, Cigna will administer your MRA.
If you do not enroll in the JPMC Medical Plan, your Wellness Program will be administered by Cigna, and any Wellness Rewards you earn will be paid
to you via JPMorgan Chase payroll (if you’re actively employed at JPMorgan Chase at that time) and will be taxable. Note: You are not eligible to earn
Wellness Rewards for all the activities shown above (see page 19 for details). (Your spouse/domestic partner is not eligible for Wellness Rewards if
you do not enroll in the JPMC Medical Plan.)
Other Wellness Programs and Services (Not Eligible for Wellness Rewards)
You can also take advantage of these Wellness Programs:
Program Description
Health Advocate • This independent health advocacy company can help you find solutions to your health care or insurance-related
issues, such as:
— Locating and researching treatments for a
medical condition
— Resolution of any benefits claims issues
— Scheduling appointments with hard-to-reach specialists
— Answering questions on health care reform, and more
Employee
Assistance
and Work-Life
Program
• The Employee Assistance and Work-Life Program (EAP) is a professional counseling, consultation and referral service
available to help our employees and their family members find solutions to the many challenges faced in managing
work and personal lives.
• The program includes referrals for professional, confidential and free counseling; assistance with child care or adoption
services; adult and elder professional care management; parenting resources and information; financial and legal
consultations; relocation resources; pet care; and more.
• EAP services are free, confidential and available 24 hours a day, seven days a week.
Financial
Coaching
• Unlimited one-on-one telephonic financial coaching with a Certified Financial Planner™. You can reach a coach at
1-833-283-0031 Monday to Friday from 9 a.m. to 8 p.m. Eastern Time. This benefit is fully paid for by JPMorgan Chase.
Wellness Program Benefits at a Glance
(continued)
Take Advantage of JPMorgan Chase Onsite Health &
Wellness Centers (where available)
At the onsite JPMorgan Chase Health & Wellness Centers, you have access to basic
medical services and educational resources — at no cost to you. The centers provide
medical care, treatment and resources when you need them at work to supplement the
care and direction you get from your own doctor. Onsite nurses are available to act as
advisors and help you connect with your health care company’s coaching programs.
Doctors are also available at many locations to provide onsite care when you need it.
Please note: Some Health & Wellness Centers offer additional services that may result
in a cost, such as bloodwork ordered by your primary care physician that is sent to a
lab for processing, physician specialists and physical therapists who are offering
services onsite for your convenience. For these services, a claim will be submitted to
your insurance company, and costs will be covered according to your Medical Plan. While
the JPMorgan Chase Health & Wellness Centers are staffed with nurses who are
employed by the firm, as medical professionals, they cannot disclose your personal
information to anyone outside the centers without your written permission.
Access All Your Health Information
in One Place
My Health is your centralized online resource where
you and your family can go to educate yourselves
about the Medical Plan, research doctors, link to your
health care company, and more.
You can access the site from work or home. And the
Single Sign-On feature gets you around without the need
to remember passwords. Here’s how you can get there:
•
From work: type “go/myhealth” into your intranet
browser or from me@jpmc > My Health
•
From home: myhealth.jpmorganchase.com
(also available for your covered spouse/domestic
partner)

9
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
New Employee Action Checklist for the
Health Care and Insurance Plans
If you are a new employee, this brochure provides information and tools to help you make your
Health Care and Insurance Plan elections as a new employee. This checklist outlines the actions
to take to enroll for your benefits.
Important Enrollment Information to Know
•
Enrollment Deadline. The enrollment deadline and plan effective date for most of the Health
Care and Insurance Plans are based on your status as a full-time or part-time employee as follows
:
If You Are a… When Participation Begins… Enrollment Deadline…
Full-time employee
(regularly scheduled to
work 40 hours per week)
You are eligible to participate
in the plans as of your date of
hire.
You have 31 days from your
date of hire to make your
enrollment elections. Coverage
is effective retroactive to your
date of hire.
Part-time employee
(regularly scheduled to
work at least 20 hours
but less than 40 hours
per week)
You are eligible to participate
in the plans on the first day of
the month following 60 days
from your date of hire.
You have 31 days prior to your
eligibility date to make your
enrollment elections. Coverage
is effective as of your
eligibility date.
If you don’t enroll, you won’t be able to enroll until the next annual benefits enrollment
period (unless you have a qualifying event), and you will be assigned No Coverage, except for
Company-provided benefits, such as basic life insurance.
Please note: If you enroll before the end of your 31-day new hire enrollment period
via the Benefits Web Center and would like to change your coverage election once you
have confirmed your elections, you must call HR Answers and speak with a Service
Representative — as long as you are still within your 31-day enrollment deadline. While
you will be able to change your health care company, you will not be able to change the
administrator of your spending accounts (HCSA, DCSA) or your Medical Reimbursement
Account
1
(MRA), which will remain with the health care company you initially chose. As an
example, if you initially elected Cigna and change to Aetna within 31 days, your health care
company would now be Aetna, but your spending accounts would remain at Cigna (for the
current plan year). Additionally, automatic claim payment will not be available to you if your
health care company is different than your spending account administrator.
•
Enroll Online. You can access additional enrollment information and/or make your election
via the Benefits Web Center on My Health:
— From work: type “go/myhealth” into your intranet browser
— From home: myhealth.jpmorganchase.com
Once on My Health, select “Benefits Web Center” to access the Benefits Web Center.
You will be prompted for your Standard ID and a password.
•
Ask questions or enroll through HR Answers. If you have questions about your benefits
coverage or the enrollment process, send a message to HR Answers on me@jpmc, or if
you don’t have Internet access from work or home, call HR Answers at 1-877-JPMChase
(1-877-576-2427) or 1-212-552-5100 if calling from outside the United States. You will be
prompted to enter your Standard ID. Your default PIN is your date of birth in MM/DD/YY
format, using two numbers for each.
1
If you have a remaining balance in your MRA, you can request to transfer your MRA balance to your new health care company.
Contact your health care company (Aetna or Cigna) for more information.
Quick Path:
— Enter your Standard ID or Social
Security number, and follow the
prompts to confirm.
— Select Option 2, then Option 0,
then Option 1.

10
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Steps to Take to Make Your Health and Insurance Plan Elections
Action Steps
Review… • The Health Care and Insurance Plan benefits options available to you and costs for coverage online via the Benefits
Web Center on My Health.
• The dependent eligibility rules on My Health. You must make any election changes before the end of your
31-day new hire benefits enrollment period or within 31 days of a qualified status change (90 days if the
qualifying event is the birth or adoption of a child). You will also be asked to provide supporting documentation for
any dependents who are covered under your plans. Please Note: To add a dependent child over the age of 26 who
is unable to support themselves due to a mental or physical disability, you must do so within your 31-day new hire
enrollment period by contacting HR Answers. You will not be able to enroll a disabled dependent who is over the age
of 26 after your initial 31-day enrollment period.
• Details about how the Medical Plan works by reviewing this brochure and accessing the Tip Sheets on
My Health.
• Details about how your benefits options work, which are described in the Summary Plan Descriptions —
available on My Health > Benefits Enrollment > 2023 Benefits Resources > Benefit Plan Details (Summary Plan
Descriptions).
• If you and/or your covered spouse/domestic partner are tobacco users, get details about how you can quit a
tobacco habit and get help creating an easy-to-follow plan, as well as information on how you can pay lower,
non-tobacco user rates for the Medical Plan, the Supplemental Term Life Insurance Plan and the Long-Term
Disability Plan.
Compare…
• Your Medical Plan and Dental Plan options through the Health Plan Comparison Charts by going to
My Health and accessing the Benefits Web Center. From there, click “Compare medical details” and “Compare
dental plan details” in the enrollment process. You should also compare your options with any other plans — such
as plans available through your spouse’s/domestic partner’s employer or other options available to your child(ren).
• The doctors, dentists, hospitals and other health care providers who participate in the Medical Plan, Dental Plan
and Vision Plan options available to you by going to My Health and accessing the Benefits Web Center. You can
also access each health care company’s website through My Health > Benefits Enrollment > 2023 Benefits
Resources.
Plan…
• How you will build your 2023 Medical Reimbursement Account (MRA) by reviewing the Initial and Additional
Wellness Activities in which you want to participate in 2023. If enrolled in Option 1 or 2 with Aetna or Cigna, you
have the opportunity to earn up to $1,000 in funds for your 2023 MRA, as well as up to $400 in funds for your
2023 MRA when your covered spouse/domestic partner completes wellness activities. If you enroll in the Kaiser
HMO Option, you can earn up to $200 in your MRA for completing Initial Wellness Activities — plus an additional
$100 when your spouse/domestic partner completes their activities, too.
Determine…
• How much you want to contribute with before-tax dollars to the Health Care and/or Dependent Care Spending
Accounts by going to My Health and accessing the Benefits Web Center. From there, click on “Enroll in Your
Benefits” > Click on “Estimate your potential tax savings” to estimate your potential tax savings with a Health Care
Spending Account.
Choose…
• The benefits options that meet your and your family’s needs.
• Your primary care dentist if you are enrolling in the Dental Maintenance Organization (DMO) or Dental Health
Maintenance Organization (DHMO) Option.
Enroll…
• In most Health Care and Insurance Plan benefits online via My Health by accessing the Benefits Web Center. If you
don’t have Internet access from work or home, please call HR Answers and speak with a Service Representative to
make your elections.
• In the Transportation Spending Accounts (Transit/Parking) at any time after your date of hire or on a monthly basis
via the Transportation Spending Accounts Web Center on My Rewards.
Confirm…
• Your choices after completing your enrollment on the Benefits Web Center. Once you complete your new hire
enrollment, you’ll receive a confirmation email.
Complete…
• Your Beneficiary Designations online. Go to https://beneficiary.jpmorganchase.com.

11
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
The Health Care and Insurance Plans
Maintaining good health and protecting your income in case you’re unable to work are
important priorities in your life. That’s why JPMorgan Chase offers a variety of options under
our Health Care and Insurance Plans — such as the Medical, Dental, Vision, Spending Accounts,
Long-Term Disability, Life and Accident Insurance, Group Personal Excess Liability Insurance
and Group Legal Services Plans — to provide you with the opportunity to select health care
and insurance benefits that best suit your needs and those of your eligible dependents.
Medical Plan
JPMorgan Chase offers two Consumer Driven Health Plan (CDHP) options — Option 1 and
Option 2 with Aetna or Cigna — which means they are high-deductible plans paired with an
integrated Health Reimbursement Account, known as the Medical Reimbursement Account
(MRA). The MRA is used for eligible out-of-pocket medical and prescription drug expenses and is
funded by JPMC when the employee and their covered spouse/domestic partner complete
certain wellness activities. This plan is offered to employees nationally, except employees who
live in Arizona and Ohio.
1
For employees who live in California, the JPMC Medical Plan offers a third medical option,
Kaiser HMO (administered by Kaiser Permanente) — in addition to Options 1 and 2 with Aetna
or Cigna. It is also paired with an MRA. Note: The Kaiser Permanente Health System offers
services in most — but not all — California ZIP codes. If available in your area, Kaiser HMO will
be one of the options you see when visiting the
Benefits Web Center during your benefits
enrollment period. If you live in an area where Kaiser does not offer services, you will see only
Options 1 and 2 with Aetna or Cigna.
In-network preventive care services are fully covered (there is no annual deductible,
coinsurance or copay; subject to age and frequency guidelines). See the following pages for a
brief overview of the Medical Plan provisions.
JPMC’s Prescription Drug Plan is part of the JPMC Medical Plan, no matter which option you
choose. You won’t need to make a separate election for prescription drug coverage. The
Prescription Drug Plan for Options 1 and 2 is administered by CVS Caremark. The Kaiser HMO
Option (CA only) includes its own Prescription Drug Plan that is administered by Kaiser.
Option 1 and Option 2 with Aetna or Cigna
The Medical Plan offers two “Consumer Driven Health Plan” options, and you choose whether
your coverage is provided through Aetna or Cigna. Both options offer the same coverage for
medically necessary services and supplies, including prescription drugs. The key difference
between the two options is the level of payroll contributions versus deductibles and coinsurance
maximums.
Here’s how the two Medical Plan options compare:
•
Option 1 — Higher medical payroll contributions; lower annual deductibles and annual
coinsurance maximums.
•
Option 2 — Lower medical payroll contributions; higher annual deductibles and annual
coinsurance maximums.
1
For employees residing in Arizona and Ohio, please refer to the “Highlights of the 2023 JPMorgan Chase U.S. Benefits Program for
Employees Living in Arizona and Ohio” brochure for information about the benefits available to you.
Committed to Your Health
Our Medical Plan is built on the principle
of a shared commitment to health.
JPMorgan Chase demonstrates its
commitment by providing valuable
benefits, programs and access to a suite
of tools and resources. These are all
designed to help you get and pay for the
treatment you need, manage your health
care expenses and, most importantly,
take care of yourself.
Your commitment is required, too. Your
role is to take responsibility for the
controllable aspects of your health care
and health care spending. You can do this
by getting preventive care, maintaining a
proper diet and exercise regimen,
carefully selecting your doctors and
hospitals, as well as understanding your
treatment alternatives and their costs. Go
to My Health to research quality ratings
of medical providers, connect to your
health care company, find out about ways
to lower your prescription drug costs,
and more.
In addition, when you take the right
steps, such as participating in Wellness
Programs, you get funds from
JPMorgan Chase added to your MRA to
help pay your eligible out-of-pocket
medical and prescription drug expenses
(deductibles, coinsurance and
copayments) — tax-free.

12
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
How the Plan Works
Plan benefits are offered through a network of participating health care providers (for example, doctors, hospitals, labs and outpatient
facilities). While the most cost-effective care will always be available through in-network providers, you can choose to go in- or
out-of-network each time you need care.
You generally must meet an annual deductible — a set amount that you pay out of pocket — before the plan shares in the costs for care.
You should note there are separate deductibles for in-network and out-of-network care.
Here are some other important differences in cost:
•
If you choose to go in-network: Preventive care, including physical exams and recommended preventive screenings, is covered at
100% with no deductible or coinsurance. In-network primary care office visits are covered at 90% with no deductible. (Primary care
includes family practitioners, internists,
1
pediatricians, OB/GYNs and convenience care clinics.) Medical virtual doctor visits are also
available to you for approximately $5 per virtual visit with no deductible. In-network psychologist/therapist office visits are covered at
90% with no deductible; in-network psychiatrist office visits are covered at 80% with no deductible.
•
If you choose to go out-of-network: Out-of-network charges do not apply toward the in-network annual deductible or coinsurance
maximum. The same applies with in-network charges — they do not apply toward the out-of-network deductible or coinsurance
maximum.
For other services, the plan pays a percentage (generally 80% in-network and 50% out-of-network) of the cost once you meet the
annual deductible. Your share — called coinsurance, which is the amount you and the plan share for certain expenses after the deductible —
is typically 20% of the cost for in-network care and 50% of the cost for out-of-network care.
The plan’s coinsurance maximum — your financial “safety net” — limits the amount you are required to pay in coinsurance each year. There
are separate coinsurance maximums for in-network and out-of-network charges. Prescription drug coverage is subject to an entirely
separate plan design and is managed by CVS Caremark (see pages 14-15 for coverage details).
ANNUAL DEDUCTIBLE
Coverage Levels Option 1 Option 2
In-Network Out-of-Network In-Network Out-of-Network
Total Annual Cash Compensation: under $60,000
Employee $500 $2,750 $1,500 $4,750
Employee + Spouse/Domestic Partner or Child(ren) $1,375 $4,125 $2,875 $7,125
Employee + Spouse/Domestic Partner + Child(ren) $2,250 $5,500 $4,250 $9,500
Total Annual Cash Compensation: $60,000 and over
Employee $1,250 $2,750 $2,250 $4,750
Employee + Spouse/Domestic Partner or Child(ren) $2,125 $4,125 $3,625 $7,125
Employee + Spouse/Domestic Partner + Child(ren) $3,000 $5,500 $5,000 $9,500
ANNUAL COINSURANCE MAXIMUM (DOES NOT INCLUDE DEDUCTIBLE)
Coverage Levels Option 1 Option 2
In-Network Out-of-Network In-Network Out-of-Network
Total Annual Cash Compensation: under $60,000
Employee $1,500 $6,000 $3,250 $6,000
Employee + Spouse/Domestic Partner or Child(ren) $2,000 $8,000 $4,625 $8,000
Employee + Spouse/Domestic Partner + Child(ren) $2,500 $12,000 $6,000 $12,000
Total Annual Cash Compensation: $60,000 – $149,999
Employee $2,000 $6,000 $3,550 $6,000
Employee + Spouse/Domestic Partner or Child(ren) $2,750 $8,000 $5,075 $8,000
Employee + Spouse/Domestic Partner + Child(ren) $3,500 $12,000 $6,600 $12,000
Total Annual Cash Compensation: $150,000+
Employee $2,750 $6,000 $3,550 $6,000
Employee + Spouse/Domestic Partner or Child(ren) $3,875 $8,000 $5,075 $8,000
Employee + Spouse/Domestic Partner + Child(ren) $5,000 $12,000 $6,600 $12,000
1
Internists must be contracted with Aetna or Cigna as a primary care physician (PCP). Go to Aetna’s or Cigna’s website through My Health to search for PCPs/primary care.

13
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
The “Per Person” Rule
For both deductibles and coinsurance maximums, the “per person” rule allows the employee or any covered dependent(s) (e.g., spouse/domestic
partner or child) to reach an individual deductible or coinsurance maximum, after which the deductible or coinsurance maximum is satisfied for
the year for that person. Covered individuals who have not met the deductible or coinsurance maximum may combine to meet the remainder of
the deductible or coinsurance maximum for that particular coverage level. If no one person has met the individual deductible or coinsurance
maximum, the expenses of all covered individuals can combine to meet the deductible or coinsurance maximum for that coverage level.
Medical Benefit Provisions Coverage for Option 1 and Option 2
In-Network Out-of-Network
1
Preventive Care (age- and gender-appropriate exams
such as physicals, cervical and prostate cancer
screenings, mammograms or colonoscopies)
100% before deductible 50% after deductible
Primary Care Office Visit (family practitioner, internist,
2
pediatrician, OB/GYN or convenience care clinic)
90% before deductible 50% after deductible
Medical Virtual Office Visit
(through MDLive or Teladoc)
90% before deductible
(approximately $5 per visit)
Not applicable
Psychologist, Therapist or Social Worker Office Visit 90% before deductible 50% after deductible
Psychiatrist Office Visit 80% before deductible 50% after deductible
Specialist Office Visit 80% after deductible 50% after deductible
Other Medical Costs (hospitalizations, labs, etc.) 80% after deductible 50% after deductible
Emergency Care (true emergency
3
) 80% after in-network deductible is met 80% after in-network
deductible is met
Emergency Care (not a true emergency
3
) 50% after in-network deductible is met 50% after out-of-network deductible
is met
1
Percentages do not include amounts above reasonable and customary (R&C) limits that you may owe. R&C is the amount health care companies have determined is a normal range of payment
for a specific health-related service or medical procedure within a given geographic area. Amounts owed above R&C, if any, are fully payable by you.
2
Internists must be contracted with Aetna or Cigna as a primary care physician (PCP). Go to Aetna’s or Cigna’s website through My Health to search for PCPs/primary care.
3
True emergency based on what a prudent person would consider an emergency; not a final diagnosis reached by a physician.
Please note: This chart presents an overview of plan design features — for more detailed information, please contact your health care
company or use the Health Plan Comparison Charts on the Benefits Web Center, which you can access through My Health. With the Health
Plan Comparison Charts, you can easily compare specific features (e.g., costs, deductibles, coinsurance) of the available Medical Plan options.
Also refer to the Summary Plan Descriptions available on My Health > Benefits Enrollment > 2023 Benefits Resources > Benefit Plan Details
(Summary Plan Descriptions).
Note: If enrolled in Option 1 or 2, you must contact a coach/nurse at your health care company (Aetna or Cigna) before you have bariatric surgery
to be eligible for benefits under the Medical Plan. Contact your health care company for details. For Family Building Benefits, enroll with
WINFertility and complete a nurse consultation to have access to a $30,000 medical lifetime maximum benefit ($10,000 medical benefit without
WINFertility engagement). Call WINFertility at 1-833-439-1517, Monday – Friday, 9 a.m. – 7:30 p.m. ET.
For contact information, see Who to Call With Benefits Questions at the end of this document.
Important Note About Providers Leaving Networks
When considering your options under the Medical Plan, remember that if your doctor leaves a network, it does not qualify as an event that allows you to
change coverage during the year. You may want to check with your provider to ensure that he or she plans to continue to participate in the network of
the health care company you decide to choose.
Prescription Drug Coverage for Option 1 and 2
If you are enrolled with Aetna or Cigna, your Prescription Drug Plan is part of the Medical Plan and is administered by CVS Caremark.
Though it is part of the Medical Plan, it has a different plan design, with separate deductibles and a separate safety net for covered
prescriptions in the form of per-prescription maximums and annual out-of-pocket maximums. You will receive two separate ID cards
(one for medical services from your health care company and one for prescription drug coverage from CVS Caremark). This coverage
gives you the option of having prescriptions filled through a convenient mail-order program or at a network of retail pharmacies.

14
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Prescription Drug Benefit Provisions
1
Coverage for Option 1 and Option 2
Retail (up to a 30-day supply)
Preventive drugs Covered 100% for eligible brand and generic drugs.
Mandatory Generic Program applies.
Generic drugs • Non-specialty: You pay $10 with no deductible
• Specialty: You pay 30% after deductible, up to
$200 max
Preferred brand-name drugs Non-specialty/specialty: You pay 30% after deductible,
up to $200 max
Non-preferred brand-name drugs Non-specialty/specialty: You pay 45% after
deductible, up to $250 max
Annual deductible
(employee
2
/employee + spouse/domestic partner or
children/employee + spouse/domestic partner +
children)
$100/$200/$300
Mail Order (up to a 90-day supply)
Preventive drugs Covered 100% for eligible brand and generic drugs.
Mandatory Generic Program applies.
Generic drugs • Non-specialty: You pay $20 with no deductible
• Specialty: You pay 30% after deductible, up to
$500 max
Preferred brand-name drugs Non-specialty/specialty: You pay 30% after
deductible, up to $500 max
Non-preferred brand-name drugs Non-specialty/specialty: You pay 45% after
deductible, up to $625 max
Annual deductible N/A
Annual Prescription Out-of-Pocket Maximum
(employee
2
/employee + spouse/domestic partner or
children/employee + spouse/domestic partner +
children)
$1,150/$1,750/$2,300; includes copays and
coinsurance for covered drugs; does not include
annual retail deductible or costs for non-covered
drugs
1
The prescription drug copay and coinsurance amounts are maximums; if the cost of the drug is less than the copay/coinsurance,
then you pay the cost of the drug.
2
For both the annual deductible and out-of-pocket maximum, the “per person” rule applies. Please see page 13 for additional
information.
Mandatory Generic Program
The plan contains a mandatory generic drug program in which generic drugs are substituted
for certain brand-name prescription drugs. If you fill your prescription with a brand-name
drug when a direct generic equivalent is available, you will pay the entire cost difference
between the brand-name and generic drug plus the non-specialty generic drug copay. Please
note: These cost differences will not be limited by per-prescription maximums or annual
out-of-pocket maximum limits. Your physician can contact CVS Caremark to seek a medical
exception review for possible approval for specific clinical reasons.
Fill Long-Term Prescription Drugs through Mail Order
One of the features of Option 1 and 2 is the discount available for long-term maintenance
prescriptions purchased in bulk by CVS Caremark and fulfilled through the mail-order
prescription service. This program, known as the CVS Caremark Maintenance Choice® Program,
saves both you and JPMorgan Chase money.
If you are taking a long-term medication, this program allows you the flexibility to receive your
90-day supply by mail through CVS Caremark’s mail-order prescription service or by picking
up your 90-day supply at a CVS retail pharmacy. If you prefer not to participate in the
CVS Caremark Maintenance Choice Program, you may opt out and obtain a 90-day supply
(or a 30-day supply) at any participating network pharmacy, but you may have to pay more.
Please keep in mind that it may be more cost-effective for you to use the CVS Caremark
Maintenance Choice Program.
Important Notes
• Your Prescription Drug Plan uses
CVS Caremark’s standard drug lists
(Specialty and Non-Specialty) of covered
and excluded (not covered) drugs. These
lists are subject to change quarterly by
CVS Caremark. An independent
committee made up of pharmacists,
physicians and medical ethicists reviews
and approves these drug lists (also
known as a Formulary). To access these
drug lists, visit the CVS Caremark
website at https://www.caremark.com
or via My Health.
•
If you choose to take a non-covered drug,
you will pay the full cost of the drug. This
could be a costly option. Be sure to
carefully consider how the costs of taking
a non-covered drug could add up.
•
Your prescription drug plan may have
special programs associated with specific
drug therapies. Some medications may
require prior authorization, have quantity
limits associated with them or be
excluded from coverage.
DON’T FORGET: You can use your Medical
Reimbursement Account (MRA) to help
pay for prescription drug deductibles,
copayments and coinsurance.
Free Preventive Drugs
To encourage preventive care, eligible
preventive brand and generic drugs on
CVS Caremark’s standard preventive drug
list are covered at 100% with no copays.
Preventive drugs are medications that can
help prevent the onset of a condition if
you are at risk or help you manage your
health if you have a condition. If you enroll
in Option 1 or 2, see the Preventive Drug
List for a list of drugs covered at 100%, as
determined by CVS Caremark. The list can
be found on CVS Caremark’s website, on
the Covered Drug List (Formulary) section
of the Plan & Benefits tab, through My
Health. Please note: Some strengths or
dosage forms may not be included in the
Brand and Generic Preventive Therapy
Drug list, and certain drugs, products or
categories may not be covered regardless
of their appearance on this list. Certain
drugs are subject to step therapy, prior
authorization or quantity limits. For the
latest coverage information, please
contact CVS Caremark.
The Mandatory Generic Drug Program
applies.If you fill a prescription for a
brand-name drug when a direct generic
equivalent is available (e.g., if you fill
Lipitor instead of atorvastatin), you will
pay the entire cost difference.

15
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Kaiser HMO Option (Additional Option for Employees Living in California)
The Kaiser HMO Option is offered through Kaiser Permanente, a fully integrated health system that employs physicians and other medical staff
and owns hospitals, facilities and pharmacies. As is common in an HMO, a primary care physician (PCP) will be responsible for wholly managing
your care and your family’s care, including the coordination of care with other providers, such as specialists.
What’s important to note is that out-of-network care is not covered under the Kaiser HMO, except for emergencies. If you enroll in the
Kaiser HMO, you will need to receive all non-emergency services from Kaiser doctors, facilities and affiliated providers. Non-emergency services
you receive from non-Kaiser doctors, facilities and affiliated providers will not be covered by the Kaiser HMO. Therefore, you should strongly
consider the appropriateness of electing Kaiser if you are in active treatment for a serious medical condition (e.g., chemotherapy for cancer) or
are pregnant and are unwilling to change all of your doctors and facilities where you receive care.
If you’re considering enrolling in the Kaiser HMO and covering a dependent who resides outside of California (for example, a child attending
college), there are limited covered services available to this dependent while outside of California — primarily virtual doctor visits and emergency
care. Given this, you should carefully consider whether the Kaiser HMO Option will meet the needs of you and your family.
How the Plan Works
Plan benefits are offered through Kaiser Permanente’s network of doctors, hospitals, labs, outpatient facilities and pharmacies.
•
You will need to select a Kaiser PCP for each covered family member and will generally need referrals to see a specialist.
•
Similar to Options 1 and 2, most preventive care services are covered at 100% at Kaiser facilities. Virtual doctor visits are also covered
at 100%.
•
For most services, like doctor’s office visits, urgent care visits, X-rays, lab work and imaging, you have copays — a fixed amount that you
pay for covered services — with no deductible to meet.
•
Kaiser administers the Prescription Drug Plan (rather than CVS Caremark for Options 1 and 2), which determines the types of drugs
covered by the plan, as well as where you can fill prescriptions (see page 16 for coverage details).
•
There is a $1,000 individual deductible ($2,000 for family) that applies to a small subset of services (e.g., hospital care, outpatient
surgery).
•
The Kaiser HMO’s out-of-pocket maximum — your financial “safety net” — limits the total amount you are required to pay out of pocket
each year. The out-of-pocket maximum includes the deductible as well as both medical and prescription drug amounts (i.e., a combined
maximum).
Coverage Levels Annual Deductible
1
Annual Out-of-Pocket Maximum
1
Inclusive of deductible and medical & prescription drug amounts
Employee $1,000 $2,000
Family $2,000 $4,000
1
Same annual deductible and annual out-of-pocket maximum for all TACC levels. Similar to Options 1 and 2, the “per person” rule applies to both the annual deductible and annual
out-of-pocket maximum. See page 13 for additional information.
Medical Benefit Provisions Coverage for Kaiser HMO
Only in-network care is covered
Preventive Care (age- and gender-appropriate exams such as
physicals, cervical and prostate cancer screenings, mammograms or
colonoscopies)
100% before deductible
Primary Care Office Visit (family practitioner, internist,
pediatrician,
OB/GYN or convenience care clinic)
You pay $20 with no deductible
Virtual Office Visit 100% before deductible
Specialist Office Visit You pay $30 with no deductible
X-rays and Lab Tests You pay $10 with no deductible
Outpatient Surgery 80% after deductible
Hospitalization 80% after deductible
Emergency Care (true emergency
1
) 80% before deductible
1
True emergency based on what a prudent person would consider an emergency; not a final diagnosis reached by a physician.

16
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Please note: This chart presents an overview of plan design features — for more detailed
information, please contact Kaiser Permanente or use the Health Plan Comparison Charts on the
Benefits Web Center, which you can access through My Health. With the Health Plan Comparison
Charts, you can easily compare specific features (e.g., costs, deductibles, coinsurance) of the
available Medical Plan options. Also refer to the Summary Plan Descriptions available on
My Health > Benefits Enrollment > 2023 Benefits Resources > Benefit Plan Details (Summary Plan
Descriptions).
Prescription Drug Coverage
The Kaiser HMO prescription drug coverage is managed by Kaiser Permanente. There is
no prescription deductible, and prescription drug copays and coinsurance count toward
a combined medical and prescription drug out-of-pocket maximum. Kaiser has its own
pharmacies, which must be used. You generally do not have the flexibility to fill a prescription
at a local retail pharmacy (for example, CVS retail pharmacies). Most prescriptions can be
filled through mail order or online for home delivery or same-day pickup. When selecting
mail order, you will receive up to a 100-day supply. Additionally, not all pharmaceutical
manufacturer coupon or copay assistance cards are accepted at Kaiser pharmacies. Contact
Kaiser Permanente at 1-800-204-6561 if you have questions or visit my.kp.org/jpmc.
If you enroll in Kaiser, your Prescription Drug Plan uses Kaiser’s standard drug lists of
covered and excluded (not covered) drugs, which are subject to change by Kaiser. To access
the covered drug list, visit Kaiser’s website at my.kp.org/jpmc or via My Health. If you
choose to take a non-covered drug, you will pay the full cost of the drug. This could be a
costly option. Be sure to carefully consider how the costs of taking a non-covered drug
could add up.
To encourage preventive care, eligible generic and brand-name preventive drugs are covered
at 100% with no copays. Preventive drugs are medications that can help prevent the onset of
a condition if you are at risk or help you manage your health if you have a condition. Under
the Kaiser HMO, Kaiser maintains its own list of generic and brand-name preventive drugs
covered at 100%. Information can be found at my.kp.org/jpmc or by contacting Kaiser.
Prescription Drug Benefit Provisions
1
Coverage for Kaiser HMO
Retail (up to a 30-day supply)
Preventive drugs Covered 100% for generics and brand
Generic drugs • Non-specialty: You pay $10
• Specialty: You pay 20% up to $150 max
Preferred brand-name drugs • Non-specialty: You pay $30
• Specialty: You pay 20% up to $150 max
Non-preferred brand-name drugs Not covered; pays at generic, brand, specialty cost if
approved exception
Mail Order (up to a 100-day supply)
Preventive drugs Covered 100% for generics and brand
Generic drugs • Non-specialty: You pay $20
• Specialty: You pay 20% up to $150 max
Preferred brand-name drugs • Non-specialty: You pay $60
• Specialty: You pay 20% up to $150 max
Non-preferred brand-name drugs Not covered; pays at generic, brand, specialty cost if
approved exception
Annual Deductible & Annual Out-of-Pocket
Maximum
• Annual Deductible: Not applicable
• Annual Out-of-Pocket Maximum: Combined with
Medical Out-of-Pocket Maximum - please refer to
page 15
1
The prescription drug copay and coinsurance amounts are maximums; if the cost of the drug is less than the copay/coinsurance,
then you pay the cost of the drug.

17
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Expert Medical Advice (All Medical Options)
Get Expert Medical Advice through Included Health (formerly Grand Rounds) — an
independent company
— when you and/or your covered family members want an Expert
Second Medical Opinion or Additional Expert Medical Advice Services. This service is
available to participants in any medical option through the JPMC Medical Plan.
Expert Second Medical Opinion
1
An expert second medical opinion through Included Health allows you to receive medical
guidance from a national leading expert on a documented diagnosis — without leaving your
home. Leading expert physicians are available to review documentation on:
•
An initial diagnosis and/or medical records from a physician or specialist
•
Treatment plans that have been recommended for your condition or diagnosis
•
Complex medical conditions you may be facing
•
Scheduled surgeries or major procedures
•
Medications you are taking
Additional Expert Medical Advice Services
In additional to second medical opinions, you can ask for Expert Medical Advice when you want:
•
To find a doctor
2
— a Care Coordinator will help you find a highly rated primary care
physician or specialist who’s in your health care company’s network.
•
A call with a clinician (Treatment Decision Support
1, 3
) — a staff clinician will answer your
health-related questions by phone or video chat to help you better understand your
current treatment options.
•
To get hospital support
1, 3
— the Included Health care team can quickly provide support by
connecting with you and your family to help answer questions as part of the Treatment
Decision Support service.
Family Building Benefits (All Medical Options)
For employees and their dependents enrolled in the JPMC U.S. Medical Plan, the following
bundle of services make up our Family Building Benefits:
•
Fertility treatments such as in vitro fertilization (IVF) and intrauterine insemination (IUI),
whether or not you have a medical diagnosis of infertility
•
Elective fertility preservation (egg and sperm freezing with 12 months of storage)
•
Associated prescription medications
Family Building Benefits can provide up to $30,000 for medical and $10,000 for prescription
drugs (enrollment with WINFertility and completion of a nurse consultation required to unlock
this benefit level; otherwise, medical benefit is $10,000).
Please note: Those enrolled in the Kaiser HMO Option have access to similar Family Building Benefits
through their plan and do not need to contact WINFertility to unlock access to the benefit (however,
they are welcome to consult with WINFertility for guidance and support). Contact Kaiser Permanente
at 1-800-204-6561 for more information about Family Building Benefits under the Kaiser HMO.
Learn more at: go/myhealth > Medical Specialty Services > Go to Family Building Benefits.
LGBT+ Health Concierge Service through Included Health
(All Medical Options)
Available at no additional cost to all employees and their dependents enrolled in the JPMC U.S.
Medical Plan, this LGBT+ friendly service is tailored to the needs of the LGBT+ community to help them:
•
Find in-network, LGBT+ affirming providers
•
Understand their benefits and coverage that may pertain to them, such as PrEP
(HIV preventive medication) and gender-affirming procedures
•
Navigate gender-affirming care
•
Connect with community support and resources
Learn more at: go/myhealth > Medical Specialty Services > Go to LGBT+ Health Concierge Service
Visit the new LGBT+ Benefits
Resources page at me@jpmc >
Health, Life & Parenting >
LGBT+Benefits@jpmc.
1
Services listed here may be eligible for Wellness
Rewards if enrolled in Option 1 or 2. You must
complete the entire expert second medical opinion
process to be eligible for Wellness Rewards in your
Medical Reimbursement Account (MRA). Please see
the “Your 2023 MRA Funding at a Glance” section
for more information.
2
These services are not eligible for Wellness
Rewards.
3
If enrolled in the Kaiser HMO Option, your medical
team can also support these services.

18
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
The Medical Reimbursement Account (MRA)
A key feature of the Medical Plan is the Medical Reimbursement Account (MRA).
JPMorgan Chase contributes money to your MRA to help you pay for eligible out-of-pocket
medical and prescription drug expenses.
JPMorgan Chase wants to reward you for taking healthy actions and leading a healthier lifestyle.
That’s why we contribute money to your MRA when you complete certain wellness activities,
including a biometric Wellness Screening and an online Wellness Assessment. When you do,
you’ll get a snapshot of important indicators of your health, as well as any potential risk factors
you may have. This information can help you take steps to either keep up the good work or
make changes so you can be the best you can be.
Initial Wellness Activity(ies)
When JPMC employees complete an annual biometric Wellness Screening and an online Wellness
Assessment by a certain deadline, they save on their next year’s medical payroll contributions and
earn money in their next year’s MRA.
The Initial Wellness Activity(ies) you must complete in 2023 to save and earn in 2024 have not yet
been determined, and the deadline has not yet been communicated.
Please note: If you became eligible for benefits coverage on or before September 1, 2022,
you were able to earn $200 in your 2023 Medical Reimbursement Account (MRA) and save
$500 on medical payroll contributions in 2023 if you completed both a biometric Wellness
Screening and an online Wellness Assessment questionnaire between November 20, 2021,
and November 18, 2022.* And you were able to earn an additional $100 in your 2023 MRA
and save an additional $500 on 2023 medical payroll contributions if your covered spouse/
domestic partner also completed both the Wellness Screening and Wellness Assessment
during the same period.
•
Employees who became eligible for benefits coverage — and/or add a spouse/domestic
partner to medical coverage — after September 1, 2022, will automatically save $500 (or
$1,000 if covering a spouse/domestic partner) on both 2022 and 2023 medical payroll
contributions without completing the Initial Wellness Activities in 2022. They will have
until the 2023 Initial Wellness Activity(ies) deadline (to be communicated in 2023) to earn
2023 MRA dollars for completing the Initial Wellness Activities; however, if they completed
the Initial Wellness Activities by November 18, 2022, they not only earned Wellness
Rewards for their 2022 MRA, but for their 2023 MRA too.
•
Employees who were on an approved leave of absence for 45 consecutive days between
September 1 and November 18, 2022, and did not complete a Wellness Screening and
Wellness Assessment during that time will automatically save $500 in 2023 on their
medical payroll contributions (or $1,000 if they cover a spouse/domestic partner). Other
provisions of the JPMorgan Chase Medical Plan and Wellness Program will continue to
apply, including the opportunity for employees and covered spouses/domestic partners
to earn MRA funds for completing Additional Wellness Activities.
* You have until June 30, 2023, to open a case with Cigna if you believe your Initial Wellness Activities were completed by the
deadline and not reflected in your medical payroll contributions.
If You Don’t Enroll in the
JPMorgan Chase Medical
Plan for 2023
If you choose to not enroll in the
JPMorgan Chase Medical Plan,
you can still earn up to $600 in
2023 Wellness Rewards (payable
in your 2023 pay and taxable).
Here’s how:
•
If you became eligible for
benefits on or before
September 1, 2022, you
needed to complete both
your biometric Wellness
Screening and online
Wellness Assessment by
November 18, 2022, to earn
$200 in 2023. However, you
can earn $400 for completing
Additional Wellness Activities
during 2023.
•
If you became eligible
for benefits after
September 1, 2022,
you can earn $200 for
completing both the
biometric Wellness Screening
and online Wellness
Assessment by the Initial
2023 Wellness Activities
deadline (to be
communicated in 2023).
You can also earn
an additional $400 for
completing Additional
Wellness Activities
during 2023.
Keep in mind that your spouse/
domestic partner is not eligible to
earn Wellness Rewards.

19
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
The 2023 MRA Action Plan
For employees and spouses/domestic partners enrolled in the JPMorgan Chase Core
Medical Plan (excludes employees residing in Arizona and Ohio
1
)
Complete Additional Wellness Activities in the areas of health, balance and finances to help
improve your well-being and earn money in your Medical Reimbursement Account (MRA)!
Choose Your 2023 Additional Wellness Activities
Complete these activities between January 1 and December 31, 2023 (see full descriptions and
dollar values on the following pages).
Make a Personal Action Call
2
Get preventive care
Meet biometric guidelines Engage in health coaching
2
Take online learning programs Get Expert Medical Advice
Use meQuilibrium
3
Enroll in maternity support
Manage a health condition
with condition management
2
Reach out for treatment decision support
Participate in My Finances and Me
3
Note: Upon completion of Additional Wellness Activities, allow two to three weeks for processing
before funds are deposited in your MRA.
Not Enrolled In the JPMorgan Chase Medical Plan?
No worries! You can still earn 2023 Wellness Rewards, payable (and taxable) through
JPMorgan Chase payroll, and administered by Cigna (1-800-790-3086). Visit My Health >
Not enrolled in JPMC Medical? > 2023 Wellness Rewards Action Plan.
1
Also excludes employees residing in California enrolled in the Kaiser HMO Option.
2
December 29, 2023, is the deadline for completing this activity, which may involve several weekly sessions. Also, coaching capacity is
often limited in November and December.
3
Not applicable to covered spouses/domestic partners.
Earn up to $800
in your MRA when you complete
Additional Wellness Activities
between January 1 and December
31, 2023.
Earn up to an additional $300
in your MRA when your covered
spouse/domestic partner
completes Additional Wellness
Activities between January 1 and
December 31, 2023.

20
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
How Your 2023 MRA Additional Wellness Activities Add Up
MRA Activity
Funds Earned in
Employee’s 2023 MRA
1
Frequency Details
Additional Wellness Activities You Covered Spouse/
Domestic Partner
Earn funds
up to this many
times for each
activity in
2023
Complete activities
between January 1 and
December 31, 2023
Complete activities of your choice
Earn up to
a maximum
of $800
Earn up to
a maximum
of $300
Preventive Care. Get a physical, cervical or prostate cancer
screening, mammogram or colonoscopy.
$200 $100 1x
Take advantage of all the age- and
gender-appropriate screenings that
apply to you (each is covered at 100%
in-network).
Biometric Outcomes:xq
These activities are typically
completed when you get a biometric
Wellness Screening. For details, see
Wellness Rewards for Body Mass
Index and Wellness Rewards for
Blood Pressure.
• Body Mass Index (BMI) under 25 or a 5% weight loss
since your last Wellness Screening.
2
$200 $100 1x
• Blood Pressure 120/80
2
or less, or alternative activities. $200 $100 1x
Personal Action Call
4
with your health care company to
discuss your Wellness Screening and Assessment results,
understand tools and resources available.
$50 $50 1x Call your health care company.
3, 4
Participate in as many Health Coaching
Programs as you want, such as blood pressure and/or
heart health, stress management, weight management
and nutrition
Go to My Medical Plan Website
(or go directly to aetna.com or
mycigna.com). Call your health care
company.
3
• Online $100 $50 1x
• Telephonic
4
$200 $100 2x
Online learning: Choosing Care Wisely — Become a good
health care purchaser using tools and resources available
on your health care company’s website.
$50 $50 1x
Go to My Medical Plan Website (or
go directly to mycigna.com)
Maternity Support
Maternity Support through your health care company
(Aetna or Cigna) provides health assessments, customized
educational materials and maternity nurse support
throughout your pregnancy.
$200 $100 1x
You must enroll during your first
trimester or within 31 days of the
effective date of your medical plan
coverage. For details, go
to Maternity Support.
Condition Management
4
Receive help managing a health condition, such as asthma,
diabetes, heart failure, chronic obstructive pulmonary
disease (COPD) and coronary artery disease (CAD).
$300 $150 2x Call your health care company.
3, 4
Expert Medical Advice
Get an expert second medical opinion through Included
Health (formerly Grand Rounds) when you complete a
second opinion on your documented diagnosis. Leading
experts are available to review documentation on treatment
plans, complex medical conditions, scheduled surgeries or
major procedures, and medications you’re taking.
$300 $150 1x Go to Expert Medical Advice
for details.
Visit Included Health or call
1-888-868-4693.
1
Allow two to three weeks for processing before funds are deposited in your MRA.
2
If it is unreasonably difficult due to a medical condition for you and/or your covered spouse/domestic partner to achieve the standards for the reward under this
program, contact your health care company to work with you (and, if you wish, with your doctor) on an alternative.
3
Aetna: 1-800-468-1266; 8 a.m. to 8 p.m., all time zones, Monday through Friday. Cigna: 1-800-790-3086; 24/7.
4
December 29, 2023, is the deadline for completing this activity, which may involve several weekly sessions. Also, coaching capacity is often limited in November
and December.

21
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
MRA Activity
Funds Earned in
Employee’s 2023 MRA
1
Frequency Details
Additional Wellness Activities You Covered Spouse/
Domestic Partner
Earn funds
up to this many
times for each
activity in
2023
Complete activities
between January 1 and
December 31, 2023
Complete activities of your choice
Earn up to
a maximum
of $800
Earn up to
a maximum
of $300
Treatment Decision Support
When dealing with one of many conditions, such as
coronary artery disease (CAD), knee/hip/lower-back
osteoarthritis, breast cancer, prostate cancer, benign
uterine conditions and obesity, that have different
treatment options, reach out to a clinician for detailed
information to help you choose the most appropriate
treatment option(s) along with names of high-quality,
cost-effective physicians near you and questions to ask
your doctor.
$200 $100 1x
Call Included Health at
1-888-868-4693. Or call
your health care company.
2
Financial Well-being
• Planning Your Finances Wisely, online
learning program — Learn more about how to
be financially well by using tools and resources that
JPMorgan Chase provides.
$50 $50 1x
Click here (or go directly to
mycigna.com)
• My Finances and Me: (1) get a Financial Wellness Score™
and Action Plan and (2) attend a group education
session on a variety of financial topics, such as basic
money management, navigating student loans and
retirement planning. Your spouse/domestic partner can
participate, but cannot earn MRA dollars for doing so.
$50 Not applicable 1x
Visit the Financial Finesse Hub
To receive credit for a group
education session, you must attend
using your JPMC Zoom account.
meQuilibrium (meQ)
Online and mobile program designed to help you
manage stress, feel your best and become more resilient.
You must register for meQ and take the meQ assessment
to complete:
Start today at
meQuilibrium.
• The required activities to earn four gold badges. $100 Not applicable 1x
• The online training, Mindfully Managing Stress, for help
gaining control over your emotions, thoughts and stress.
$50 Not applicable 1x
TOTAL MAXIMUM 2023 MRA FUNDS $1,000
($200
3
+
$800)
$400
($100
3
+
$300)
$1,400 if the JPMorgan Chase
employee and covered spouse/
domestic partner complete Initial +
Additional Wellness Activities within
required time frames.
How Your 2023 MRA Additional Wellness Activities Add Up (Continued)
1
Allow two to three weeks for processing before funds are deposited in your MRA.
2
Aetna: 1-800-468-1266; 8 a.m. to 8 p.m., all time zones, Monday through Friday.
Cigna: 1-800-790-3086; 24/7.
3
This amount assumes you and/or your covered spouse/domestic partner completed both the
Wellness Screening and Assessment between November 20, 2021, and November 18, 2022.
Please read these important disclaimers.
To see a list of your completed/available
Additional Wellness Activities and your MRA
balance, go to My Health > View MRA &
Spending Account.

22
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Paying Expenses Through Your MRA
When you enroll in the Medical Plan, you can pay for eligible expenses by using your MRA and Health Care Spending Account (HCSA). If
you enroll in Option 1 or 2, you will be able to choose whether you want automatic claim payment or a debit card to pay claims from your
MRA and HCSA. Your debit card will be issued by your health care company — Cigna or PayFlex (for Aetna enrollees). If you enroll in the
Kaiser HMO Option, your payment method will default to a debit card as automatic claim payment is not available and your debit card
will be issued by Cigna. Learn more about paying your expenses through your MRA by accessing the MRA, HCSA and Payment Options
Tip Sheet through My Health.
Please note: If you elect to participate in the HCSA, the payment method you choose for your MRA will also be used for your HCSA. In
addition, if you don’t make a payment election, your payment method will default to automatic claim payment and generally cannot be
changed until the next Annual Benefits Enrollment. For the Kaiser HMO Option, the only available payment option is a debit card. For
claim forms or to check your MRA and HCSA balances, go to My Health.
Payment Method How It Works
Automatic
Claim Payment
(Available for
Options 1 and 2
only)
After your health care company pays its share of the cost of care, your health care company will pay your doctor/
pharmacy your share of the eligible cost. They’ll use your MRA funds first, then your HCSA funds (if applicable).
Once both MRA and HCSA funds are gone, you’ll pay any remaining expenses out of your pocket when billed by
your doctor. If you’re filling a prescription, you’ll pay any remaining balance not covered by funds in your MRA
and/or HCSA at the time you purchase the drug. The pharmacy will let you know about any amount you owe.
If you’re using your HCSA to pay for eligible dental and vision expenses not payable under your plans
(e.g.,
coinsurance for dental services, eyeglasses), you’ll need to pay out of your own pocket, then submit an
online claim form (via your health care company website) or a paper claim form (via mail or fax) to access
your HCSA balance.
Debit Card After your health care company pays its share of the cost of care, you can use your debit card to pay your share of
the eligible out-of-pocket medical and prescription drug expenses from your MRA and then your HCSA. (Give your
debit card number to your doctor when you are billed for services or your pharmacy when you purchase a
prescription drug, and your share of the expenses will automatically be taken out of your accounts.)
You can also use your debit card to pay for eligible out-of-pocket dental and vision expenses out of your HCSA, as
long as your provider accepts debit cards.
You can also pay out-of-pocket and later submit a paper claim form to Aetna or Cigna, available on My Health >
Medical, Rx, MRA, & Spending Account > Claims and Other Forms, or complete an online claim form (via your
health care company website).
Information on Wellness Rewards for Blood Pressure
If you enroll in Option 1 or 2, you can earn Wellness Rewards for Blood Pressure in the following manner:
•
If your blood pressure is 120/80 or less, you earn $200 in Wellness Rewards for Blood Pressure.
•
If your blood pressure is greater than 120/80 but less than 160/100, you can earn $200 in Wellness Rewards in one of two ways:
1. You can make an appointment at an onsite JPMC Health & Wellness Center (where available) to retake your blood pressure for
in-person health coaching regarding the risks of high blood pressure. After completion of your coaching session, the JPMC
nurse will notify your health care company that the coaching took place, and your health care company will authorize
Wellness Rewards for Blood Pressure.
2. You can call your health care company (Aetna or Cigna) and complete Health Coaching that will be focused on your blood
pressure or a related topic such as Heart Health. Your health care company will authorize your Wellness Rewards.
Please note: The incentive for completing this Blood Pressure activity will be recorded under “Health Coaching,” not
“Blood Pressure.”
•
If your blood pressure is 160/100 or greater, you can still earn $200 in Wellness Rewards by calling Aetna or Cigna or going to a
JPMC Health & Wellness Center (where available) to obtain the Wellness Screening Outcomes Exemption Form and taking it to your
personal health care provider. Your health care provider can determine if medication adjustment or information regarding your blood
pressure risks is appropriate for you. Your provider can then complete the form and fax it to Cigna as evidence that you are currently
under medical care for your blood pressure. Your health care company will then award Wellness Rewards for Blood Pressure.

23
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Eligible Dependents
In addition to employee coverage, your dependents are also generally eligible for coverage
under the JPMorgan Chase Medical Plan. When you enroll for coverage, you need to certify
online that your dependent meets the eligibility requirements. You will then be asked to provide
acceptable documentation supporting eligibility. Eligible dependents generally include:
•
Your spouse
1
or domestic partner; and
•
Your and/or your spouse’s/domestic partner’s children
— Up to the end of the month in which they turn 26
— Can be covered regardless of student or marital status, financial dependence on parents,
residency with parents or eligibility for coverage under another health plan
1
Same- and opposite-sex spouses
Please note: You may continue coverage beyond age 26 for an unmarried child who (1) is not capable of supporting himself or
herself due to a mental or physical disability that began before age 26, (2) is dependent on you for financial support, and (3) was
covered as a dependent at the time of turning age 26. If you are a new hire, you have 31 days from your eligibility date to add new
dependents who are over age 26 and meet the first two criteria. You will not be able to enroll a disabled dependent over the age of
26 after your initial 31-day enrollment period in any JPMorgan Chase plan. Please call HR Answers if this situation applies to you.
Overview of the Payment Methods
Below are some examples to help you learn more about the debit card and automatic
claim payment:
Automatic Claim Payment May Be Better
For You If You…
The Debit Card May Be Better For You
If You…
• Have doctors and providers who don’t
accept credit/debit cards.
• Want to avoid the substantiation process,
which requires you to provide receipts
when your health care company can’t
match expenses to a claim.
• Don’t have coverage through another
medical plan.
Please note: You are not able to apply any
other form of payment at the time of your
transaction if you elect the automatic claim
payment option. This option is available for
Options 1 and 2 only.
• Would like to review payments before any
MRA/HCSA funds are taken out of your
account.
• Elect the HCSA and want to use that
account at the time of service to pay for
dental and vision expenses.
• Use a prescription drug discount card
provided by a drug manufacturer or
foundation.
• Also have coverage through another
medical plan, such as your spouse’s plan,
Medicare or Medicaid.
• Visit providers or facilities that require
you to pay at the point of service.
Please keep in mind that automatic claim payment assumes you did not pay your portion of
your eligible medical expense at the time of service and pays your provider/facility your
portion directly. If you pay your portion at the time of service, your provider/facility will be
double-paid — once from you at the point of service and once from your MRA/HCSA
(assuming funds are available). It will be your responsibility to recoup the overpayment from
your provider/facility (although your health care company can try to assist you). Therefore, if
the providers or facilities you visit are requiring you to pay at the point of service, the
automatic claim payment method may not be right for you; you should consider the debit
card payment method.
For Options 1 and 2, you can select your payment option when you first enroll in benefits or
during Annual Benefits Enrollment. If during the year, you begin taking a prescription drug
and have a manufacturer coupon or discount card, you can contact HR Answers and request
a one-time change from automatic claim payment to debit card payment (prospectively).
Be Sure Your Dependents
Are Eligible
You are responsible for understanding
the dependent eligibility rules and
abiding by them as well as providing
acceptable documentation when
requested. When you first enroll and
each year during your designated
enrollment period, or within 31 days
following a qualified status change
(90 days if the qualifying event is the
birth or adoption of a child), it is
important that you review both the
dependent eligibility rules and the
status of your covered dependents to
ensure that you cover only eligible
dependents. Review dependent
eligibility requirements on My Health,
and do not enroll any ineligible
dependents.
Please note: You will be required to
provide documentation for the
dependents you cover under the plan.
If you do not provide documentation
within the specified time period,
your dependents will be dropped
from coverage.
Dependents’ Social
Security Numbers
Required
If you cover dependents under your
JPMorgan Chase plans, be sure their
names, addresses and Social Security
numbers are up to date. This information
is important for us to have and is required
by the Affordable Care Act. In addition, if
you’re adding a dependent to your
coverage, you’ll need to provide that
dependent’s Social Security number. Just
go to the Benefits Web Center, and you
will be prompted for the Social Security
number when adding each dependent
for coverage.
If you do not enter your dependent’s
Social Security number when prompted,
you will not be able to enroll your
dependent on the Benefits Web Center
and will need to enroll him or her by
calling HR Answers.

24
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Coverage Categories
The JPMorgan Chase Medical Plan offers four coverage categories to help match your
coverage needs:
•
Employee Only
•
Employee Plus One Adult
(spouse or domestic partner)
•
Employee Plus Child(ren)
•
Employee Plus Family
(spouse or domestic partner plus child[ren])
Cost for Coverage
You and JPMorgan Chase share the cost of coverage under the Medical Plan. Your
contributions are deducted from your pay on a before-tax basis — before federal (and, in
most cases, state and local) income taxes are withheld. The amount you pay depends on the
level of your Total Annual Cash Compensation, the medical option you choose, where you
live, the number and type of eligible dependents you cover, if you and your covered spouse/
domestic partner use tobacco and if you and your covered spouse/domestic partner
complete Initial Wellness Activity(ies). You will have a higher cost for coverage if your Total
Annual Cash Compensation is higher, you cover more dependents under your Medical Plan
option, and/or costs in your geographic area are higher than average.
Please note: You will be provided lower rates for the Medical Plan in your first year of hire even
if you do not complete the Initial Wellness Activity(ies) or if you use tobacco.
The following chart shows the Total Annual Cash Compensation levels currently used to determine
employee before-tax contributions under the Medical Plan. Note: Employees whose Total Annual
Cash Compensation is less than $60,000 (Levels 1 & 2 below) will receive the highest subsidy from
the firm, which means they’ll pay the lowest medical payroll contributions. (Specific contribution
rates for each of your available Medical Plan options will be communicated during your designated
enrollment period.) Please see page 45 for the definition of Total Annual Cash Compensation.
Total Annual Cash Compensation Levels Used to Determine
Medical Plan Contributions
Level
Total Annual Cash Compensation
(excluding overtime)
Employee Pays
1
2
3
4
5
6
7
< $45,000
$45,000 – $59,999
$60,000 – $79,999
$80,000 – $149,999
$150,000 – $249,999
$250,000 – $349,999
$350,000 and above
Least
Most
Domestic Partners
To qualify as an eligible dependent under the JPMorgan Chase U.S. Benefits Program, you
and your domestic partner must meet all the following conditions:
1. Be age 18 or older; and
2. Not be legally married to, or the domestic partner of, anyone else; and
3. Have lived together for at least 12 months; are currently living together; and have a serious,
committed, romantic relationship; and
4. Be financially interdependent (share responsibility for household expenses); and
5. Not be related to each other in a way that would prohibit legal marriage; OR
Have registered as domestic partners pursuant to a domestic partnership ordinance or law
of a state or local government, or under the laws of a foreign jurisdiction.
For additional information on covering domestic partners, please review the information on
My Health, including the Covering a Domestic Partner Tip Sheet.

25
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Contribution Costs for Each Covered Family Member
To more accurately reflect the true cost of coverage and to fairly
distribute that cost among employees, you will pay for each family
member that you cover under a JPMorgan Chase Medical Plan
option, including each child. You will be charged for a maximum
of four children (three children for the Kaiser HMO option), even if
you cover more than that under your plan. (You can cover all of
your children, as long as they meet eligibility requirements. You will
only pay the per-child costs for the first four children (three
children for the Kaiser HMO option) you choose to cover.) This
itemized pricing will not only help you evaluate the cost of each
family member’s coverage, but will also give you information to
more accurately compare your Medical Plan options and costs.
Contributions will also depend on the variables described on the
prior page.
Higher Rates for Tobacco Users for
Certain Benefits Coverage
All U.S. benefits-eligible employees (and their covered spouses/
domestic partners, where applicable) who use tobacco will pay
higher rates under the following Health Care and Insurance Plans:
•
Medical Plan (employee and spouse/domestic partner coverage);
•
Supplemental Term Life Insurance Plan (employee and spouse/
domestic partner coverage);
•
Long-Term Disability Plan (employee coverage); and
•
Individual Disability Insurance.
If you use tobacco, you will pay an additional $80 per month (or
$960 per year) under the Medical Plan. If your covered spouse/
domestic partner also uses tobacco, you will pay an additional $80
per month (or $960 per year) under the Medical Plan.
Under the JPMorgan Chase Medical Plan, a “tobacco user” (for
a plan year) is any person who has used any type of tobacco
products (i.e., cigarettes, cigars, chewing tobacco, snuff or a
pipe) regardless of the frequency or location (this includes daily,
occasionally, socially, at home only, etc.) in the 12 months
preceding January 1 of the plan year.
When you enroll as a newly eligible employee or during a
subsequent annual enrollment period, you will declare a
non-tobacco user/tobacco user status for yourself and your
covered spouse/domestic partner. The status you report will
remain in effect for the calendar year. After you (and/or your
covered spouse/domestic partner) have been tobacco-free for
12 months (as of January 1 each year) or completed the Quit For
Life Tobacco Cessation Program by the applicable deadline (as
part of the annual benefits enrollment process), you’ll be eligible
for lower non-tobacco user rates beginning January 1 of the
following year.
If you become eligible for benefits coverage before September 1, you
will be assigned non-tobacco user rates
2
for the current calendar year
for you and your covered spouse/domestic partner even if you
declare yourself and/or your spouse/domestic partner a tobacco user,
because you and/or your spouse/domestic partner may not have had
an opportunity to complete a Tobacco Cessation Program in order to
qualify for the lower non-tobacco user rates. You’ll receive more
information regarding the opportunity to update your tobacco user
status during the annual benefits enrollment period. More information
on Tobacco Cessation Programs and requirements is available on
My Health > Wellness Activities & Services > Tobacco Cessation.
If you become eligible for benefits coverage after September 1, for
the current plan year and the following plan year you will be
assigned non-tobacco user rates for your and your spouse’s/
domestic partner’s coverage for certain benefits.
Example 2
1
Joseph wants to cover himself, his wife and their six children under
Medical Option 1. He will pay one price for himself, one price for his
wife, and one price for each of four of his children. He will not pay
an additional per-child price for his fifth and sixth children because
per-child costs apply only up to four children, even though he will
have coverage for his six children.
Joseph’s employee-only rate + wife’s rate + (per-child rate x 4) =
Joseph’s total monthly contribution for medical coverage.
[$83 + $265 + ($62 x 4)] = $596
Example 1
1
Deborah wants to provide coverage for herself, her husband
and their three children under Medical Option 2. She will pay
one price for herself, one price for her husband, and one
price for each of her three children. When combined, this will
equal her total contribution for medical coverage.
Deborah’s employee-only rate + husband’s rate + (per-child
rate x 3) = Deborah’s total monthly contribution for medical
coverage.
[$23 + $198 + ($33 x 3)] = $320
1
These examples are for illustrative purposes only and represent participation in Medical Option 1 and 2, average geographical price region, and Total Annual Cash Compensation of < $60,000.
Your actual rates could be different from those represented here. These examples also assume the employee and covered spouse complete a biometric Wellness Screening and an online Wellness
Assessment and are not tobacco users.
Here’s how it works:
2
Upon enrolling in Individual Disability Insurance (IDI), employees will be asked their tobacco user status to determine their rate for coverage. Those who are tobacco free for 12 months at
enrollment will have the non-tobacco user rate. All others may qualify for the lower non-tobacco user rate in the future by completing the Quit for Life Tobacco Cessation Program or being
tobacco free for 12 months.

26
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Dental Plan
JPMorgan Chase offers three dental coverage options based on where you live. All options provide coverage for preventive care, basic
and major restorative care. Here’s a brief overview of each Dental Plan option:
Dental Options at a Glance
Provision
Preferred Dentist Program
(PDP) Option — MetLife Dental Maintenance
Organization (DMO)
Option — Aetna
(in-network only)
Dental Health
Maintenance
Organization
(DHMO) Option —
Cigna (in-network only)In-Network Out-of-Network
Annual Deductible
Preventive None None None None
Restorative
(basic and major)
$50 individual,
$150 family
$100 individual,
$300 family
None None
Covered Services
Preventive
(exams, cleanings,
X-rays, sealants)
(no deductible)
100% coverage 90% coverage 100% coverage 100% coverage
Basic restorative
(fillings, extractions,
periodontal, oral
surgery, anesthesia)
80% coverage after
deductible
70% coverage after
deductible
90% coverage 90% coverage
Major restorative
(dentures, bridges,
root canals, inlays,
onlays, crowns)
60% coverage after
deductible
50% coverage after
deductible
60% coverage 60% coverage
Orthodontia
Child (under age 19) 50% coverage
no deductible
50% coverage
no deductible
50% coverage 50% coverage
Adult None None 50% coverage 50% coverage
Maximum Benefits
Combined annual for
preventive and restorative
Maximum $2,000
1
Maximum $1,500
1
No maximum No maximum
Lifetime for orthodontia Maximum $2,500
1
Maximum $2,000
1
Limited to one course
of treatment
per individual per
lifetime
24 months of
interceptive and/
or comprehensive
treatment (cases
beyond 24 months or
atypical cases require
additional payment by
the patient)
All in-network percentages above apply to dentists’ negotiated fees. All other percentages generally apply to reasonable and customary charges. Frequency limits may apply to certain services.
1
Combined in- and out-of-network, includes any benefits already applied to any lifetime maximum for orthodontia under the Dental Plan.

27
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Preferred Dentist Program Option
The Preferred Dentist Program (PDP) Option, administered by MetLife, offers you the
flexibility to choose between in-network and out-of-network dental care. Under this option,
networks of participating dental providers offer their services for lower, prenegotiated
rates. Here’s how it works:
•
When you need care, you can choose to visit a network provider or go out of network.
•
In general, when you obtain care from an in-network dentist, your out-of-pocket costs will
be lower; when you receive out-of-network care, your out-of-pocket costs will be higher.
•
Once you pay a deductible, you and JPMorgan Chase share the discounted costs for
in-network covered expenses, subject to plan maximums. In the case of out-of-network
covered expenses, a higher deductible applies and the plan pays a lower level of benefits
up to reasonable and customary limits and plan maximums.
•
No deductibles apply to in-network or out-of-network preventive services.
Dental Maintenance Organization/
Dental Health Maintenance Organization Option
When you enroll in the Dental Maintenance Organization (DMO) or Dental Health Maintenance
Organization (DHMO) Option, administered by Aetna and Cigna, respectively:
•
You receive care solely from dentists who are associated with the DMO/DHMO network.
•
All of your care within the network is coordinated through a primary dentist. You must go
through your primary dentist to receive benefits from the plan and for specialist referrals.
•
There are no deductibles.
•
You pay nothing for preventive care and share in the cost of care for basic and restorative
care. You pay a percentage of discounted costs.
Eligible Dependents
You can cover the same eligible dependents under the Dental Plan as under the
JPMorgan Chase Medical Plan (please see page 23).
Cost for Coverage
You and JPMorgan Chase share the cost of coverage under the Dental Plan. Your contributions
are deducted from your pay on a before-tax basis. The amount you pay depends on the option
you choose and the type of eligible dependents you cover.

28
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Vision Plan
The JPMorgan Chase Vision Plan, administered by EyeMed, helps you pay for covered vision
expenses, such as eye examinations, lenses (including contact lenses) and eyeglass frames.
When you seek care from a vision care professional within the plan’s network, you will have no
copayment for your vision exam. If you choose to seek care outside the network, you will be
reimbursed up to a specified dollar limit. EyeMed offers vision care coverage through a network
of independent vision care providers nationwide, including retail chains, such as Lenscrafters,
Target and most Pearl Vision locations.
Vision Plan at a Glance
EyeMed In-Network Coverage
Service
EyeMed Doctors and Participating
Retail Chains
Copay Frequency
WellVision Exam® Exam is available once every
calendar year
$0
Every
calendar
year
Frames
• $150 allowance $0
Lenses
• Single vision, lined bifocals or lined
trifocals
• Tints, scratch-resistant coating and
polycarbonate lenses are covered
in full.
$10
Contact Lenses
(instead of
eyeglass lenses)
$150 allowance $0
Contact
Lens Exam
Fully covered, after copay
No more
than $55
Retinal Screening An enhancement to your
WellVision Exam®
$39
Your Coverage with Out-of-Network Providers
Exam
Frame
Contacts
up to $45
up to $75
up to $120
Single Vision
Lined Bifocal
Lenses
Tints
up to $35
up to $50
up to $11
Lined Trifocal
Lenses
Progressive
Lenses
up to $65
up to $50
Cost for Coverage
Your contributions for Vision Plan coverage are deducted from your pay on a before-tax
basis. Your cost for coverage depends on the type of dependents you cover.
Eligible Dependents
You can cover the same eligible
dependents under the Vision Plan as
under the JPMorgan Chase Medical Plan
(please see page 23).
Get Preventive Care!
We believe preventive care is
so important that it’s covered
100% when you receive
in-network care under the
JPMorgan Chase Medical Plan,
Dental Plan and Vision Plan.

29
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Spending Accounts
Spending accounts allow you to set aside before-tax money to help pay for eligible health
care, dependent care and transportation expenses. JPMorgan Chase offers three spending
accounts — the Health Care Spending Account, the Dependent Care Spending Account and
the Transportation Spending Accounts (Transit/Parking).
Health Care Spending Account
You can generally contribute up to $3,050 a year on a before-tax basis to pay for eligible
out-of-pocket health care expenses. You may use your Health Care Spending Account for
eligible expenses such as:
•
Medical and prescription drug deductibles, copayments
and coinsurance after your MRA funds are used
•
Costs for non-covered prescription drugs, such as
non-sedating antihistamines (e.g., Clarinex, Allegra) with
a prescription from your doctor
•
Certain over-the-counter drugs without a prescription
from your doctor
•
Dental deductibles and coinsurance not covered under
any dental plan you may be enrolled in
•
Eyeglasses and contact lenses for amounts not covered
under any vision plan you may be enrolled in
Your health care company (Aetna or Cigna) will be the
administrator of your Health Care Spending Account. If your
health care company is Kaiser or if you do not enroll in the
JPMorgan Chase Medical Plan, Cigna will administer your Health Care Spending Account.
Please note: Generally, your medical and/or dental HCSA claims will be automatically
substantiated if you enroll in a medical or dental plan option with the same health care
company that administers your HCSA (Aetna or Cigna).
Coordinating Your MRA and Health Care Spending Account
Keep in mind that you have to use all the funds in your MRA before you can use the money in
your Health Care Spending Account for eligible out-of-pocket medical and prescription drug
expenses. However, you can also use your Health Care Spending Account to reimburse yourself
for eligible out-of-pocket dental and vision expenses, which are not eligible for reimbursement
under the MRA.
Here’s a look at how your eligible expenses are paid from your MRA and Health Care
Spending Account:
•
Your MRA pays first for eligible out-of-pocket medical and prescription drug expenses.
•
Your Health Care Spending Account pays for eligible out-of-pocket medical and prescription
drug expenses after MRA funds are depleted.
•
Your Health Care Spending Account pays for eligible out-of-pocket dental and vision care
expenses, as well as over-the-counter medicines for which you have a prescription and all
forms of insulin even if available without a prescription (cannot be paid by your MRA). Certain
over-the-counter supplies are covered without a prescription.
For more details about how your eligible expenses are paid from your MRA and Health Care
Spending Account, take a look at the MRA, HCSA and Payment Options Tip Sheet on My Health.
Important Details About
Participation in the Health
Care Spending Account
•
Carryover Funds: If you elect to
participate in the Health Care
Spending Account, you can carry
over up to $610 of unused Health
Care Spending Account funds from
year to year to continue to pay for
eligible expenses. Unused balances
less than $25 will be forfeited if you
do not choose to contribute to the
HCSA for the following plan year.
•
Estimate Your Contributions and plan
carefully: Use the Health Care
Spending Account Contribution
Estimator and MRA Value Estimator on
the Benefits Web Center to model your
expenses, so that you can estimate the
amount of before-tax dollars to
contribute to the Health Care Spending
Account. (The MRA Value Estimator
will show how much you can earn by
completing certain wellness activities.)
Please note: If you enroll in the
JPMorgan Chase Medical Plan, your
MRA funds will be used to pay for
eligible out-of-pocket medical and
prescription drug expenses before
your Health Care Spending Account
funds. So, be sure to plan your
contribution amount carefully.
•
Eligible Tax Dependents: You can pay
expenses from your Health Care
Spending Account for eligible tax
dependents only, including your
spouse, a tax-qualified domestic
partner, parents and your dependent
children, including the children of
your domestic partner if they are your
tax dependents.
•
Coordinating with Your Spouse:
If your spouse has a Health Care
Spending Account at JPMorgan Chase
or at another employer, by law you
cannot claim reimbursement for any
expense your spouse has claimed.
•
Certain expenses, such as those for
cosmetic surgery or health care
premiums, are not reimbursable
under the Health Care Spending
Account.
Don’t Lose Out: If you elect
to participate in the Health
Care Spending Account, you will
lose any balance exceeding
$610 remaining in your account
at the end of the plan year
(December 31). You have until
March 31 of the following plan
year to submit eligible claims
for reimbursement. If you do
not choose to contribute to the
HCSA in a given plan year, any
balance you carried over from a
prior year will be forfeited at
the end of the year if you do
not use it.

30
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
A listing of eligible expenses under the Health Care Spending Account is available on Aetna’s or Cigna’s website if you enrolled in
Option 1 or 2 and on Cigna’s website if you enrolled in the Kaiser HMO Option or if you waived medical coverage.
Your HCSA expenses will be paid in the same manner as the way you choose to have your expenses paid through your MRA: through
automatic claim payment or debit card. See pages 22-23 for details.
Dependent Care Spending Account
You can generally contribute up to $5,000 a year on a before-tax basis to pay for eligible out-of-pocket expenses to provide care
during working hours for eligible dependents. Eligible expenses are those that provide care so that you and your spouse (if you are
married) can work outside the home or so your spouse can attend school full-time. You must provide the Social Security number or tax
identification number of the care provider when filing for reimbursements. You may use your Dependent Care Spending Account for
eligible expenses including:
•
Child care expenses for dependent children under age 13, or older if disabled, and
•
Adult care expenses for your tax-qualified adult dependents.
The JPMorgan Chase Dependent Care Spending Account, which is administered by your health care company (Aetna or Cigna, or by
Cigna if you enroll in the Kaiser HMO or if you are not enrolled in the JPMorgan Chase Medical Plan) covers eligible expenses only up
to the balance credited to your account through payroll deductions at the time you request reimbursement. As your contributions are
deducted from your pay throughout the year, you’ll automatically be reimbursed for any outstanding expenses you’ve submitted, up to
the year-to-date amount already contributed (minus any previous reimbursements). Your account will only cover expenses for services
that have actually been incurred, not for future expected services.
Please note: Internal Revenue Service (IRS) rules impose limits on contributions to the Dependent Care Spending Account in certain
situations that involve highly compensated employees to help ensure that the plan doesn’t unfairly favor these employees. As a result,
it may be necessary to reduce contributions for some participants under these rules. You’ll be notified if you’re affected.
Important Details About Participation in the Dependent Care Spending Account
•
Don’t Lose Out: If you elect to participate in the Dependent Care Spending Account, you will lose any balance remaining in your
account at the end of the plan year (December 31). You have until March 31 of the following year to submit eligible claims for
reimbursement of expenses incurred during the previous year.
•
Change or Stop Contributions During the Year: If your dependent care needs change in 2023, you are able to change or stop
your Dependent Care Spending Account contributions during the year due to a qualifying status change.
•
Eligible Tax Dependents: You can pay expenses from your Dependent Care Spending Account for eligible tax dependents only,
including a tax-qualified disabled adult dependent; your dependent children, including the children of your domestic partner if
they are your tax dependents, as well as parents if they are your tax dependents.
•
Coordinating with Your Spouse: If your spouse’s employer offers a similar Dependent Care Spending Account, the most you and
your spouse can be reimbursed during a tax year is $5,000 on a combined basis. If you are married but file separate income tax
returns, your maximum contribution amount is $2,500 a year. Please note: Additional limits may apply.
•
Federal Income Tax Credit: The Internal Revenue Code prevents you from taking the federal dependent care tax credit on your
personal income tax form for expenses reimbursed through your Dependent Care Spending Account. You may wish to consult with
your personal financial advisor to determine which is better given your personal financial situation.
•
Calculate Back-Up Care: Calculate the value of your anticipated back-up child care use for the year when electing your coverage
amount. The Fair Market Value of a day of back-up child care is $60 minus your copayment amount.

31
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Transportation Spending Accounts (Transit/Parking)
Under the JPMorgan Chase Transportation Spending Accounts, you pay for eligible commuter and/or parking expenses related to
commuting to and from work through before-tax payroll deductions up to the legal limits. You may contribute before-tax dollars to two
different accounts — the Transit Account and/or the Parking Account. Limits for before-tax deductions for eligible transit and parking
expenses change from year to year. For 2023, the monthly before-tax limits are $300 for transit and $300 for parking expenses. After-tax
contributions are applicable to commuting and/or parking expenses that exceed before-tax monthly limits. For more information, please
refer to the Summary Plan Descriptions available on My Health > Benefits Enrollment > 2023 Benefits Resources > Benefit Plan Details
(Summary Plan Descriptions).
Important Details About Participation in the Transportation Spending Accounts
•
How Transit Expenses Are Paid: If you participate in the Transit Account, you simply order your commuter passes, tickets or
vouchers through HealthEquity, the plan administrator. You will be asked to specify whether your elections should carry over
month to month, or if you’d prefer, you may initiate a new election each month. Your commuter passes, tickets or vouchers are
then sent to your home address by the first of the month.
•
If Your Commuter Pattern Varies, the Transit Account Also Offers the Convenience of a Commuter Card for Your Transit
Expenses: This card can be used to purchase a pass and is available to participants in a location where the associated transit
agency accepts a debit card and/or credit card.
•
How Parking Expenses Are Paid: If you participate in the Parking Account, you must indicate how much you pay for parking, and
that amount will be paid to the parking provider (e.g., parking garage) directly for you.
•
If Your Monthly Parking Expenses Are Unpredictable: You can elect a Commuter Card, funded monthly by your TSA
(Transportation Spending Account) payroll contributions, to pay for parking directly (at participating garages), eliminating the need
to pay upfront and file claims or submit receipts for reimbursement. Alternatively, you can pay for parking each month and then
get reimbursed by submitting a claim.
•
When You Can Enroll: You may enroll for participation in the Transportation Spending Accounts on a monthly basis at any time
during the year. You must make your elections, changes or cancellations by the first day of the month prior to the month in which
expenses will be incurred. For example, if you make your enrollment elections between June 2 and July 1, your payroll deductions will
begin in July for the expenses you will incur in August.
•
Unused Before-Tax Dollars: The Transportation Spending Accounts are subject to different rules under the Internal Revenue Code
than the Health Care Spending Account and the Dependent Care Spending Account. So, you may enroll in one or both of the
Transportation Spending Accounts at any time and change or stop your contributions on a monthly basis. If your account reaches a
certain threshold, your contributions will be suspended until the balance is below that threshold.
New York City Area Commuters
A Premium Metro Card is available to New York City commuters, valid for 12 months, with unlimited 24/7 rides, all year long, including
holidays.
If you commute to work using either the Metro-North Railroad or Long Island Railroad, there are two steps you need to take when setting
up your account:
1. First, set up a Mail & Ride Account through the www.mta.info website.
2. Once you’ve set up your Mail & Ride Account, you can then set up your election by logging in to the Transportation Spending Accounts
Web Center. You can elect an amount up to the before-tax legal monthly limit or the full amount of your commuting cost. Your
deductions will then be forwarded directly to the agency to pay for your ticket.

32
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Long-Term Disability (LTD) Plan
The JPMorgan Chase Short-Term Disability Plan administered by Sedgwick provides eligible
employees with up to 26 weeks of time off (consisting of a one-week waiting period and up to
25 weeks of full or partial pay, if applicable) if you are ill or injured. If you are out of work for an
extended period of time (beyond 26 weeks), coverage is available under the LTD Plan (insured
and administered by Prudential) as follows:
•
If your Total Annual Cash Compensation (TACC) is less than $60,000, you will automatically
receive LTD coverage of 60% of your TACC fully paid by JPMorgan Chase.
•
If your TACC is $60,000 or more, you can elect employee-paid LTD coverage of 50% or 60%
of your TACC. The premiums you pay for coverage will be made on an after-tax basis. As a
result, any benefits you receive if you become disabled are tax-free. Keep in mind that if your
TACC decreases to less than $60,000, you will be defaulted into the Company-paid 60%
Option. The maximum monthly employee-paid LTD benefit is $20,000 (which generally limits
the benefit available to employees earning more than $400,000 per year if they elect the
60% Option and $480,000 per year if they elect the 50% Option). If you do not elect LTD
coverage, you will be assigned No Coverage for the plan year and will need to satisfy
evidence of good health if you enroll in the future.
Understand the Individual Disability Insurance (IDI)
Enrollment Process
Generally, if your TACC is more than $400,000, you are subject to the LTD Plan’s maximum
coverage limits and can purchase additional LTD coverage under a fully portable Individual
Disability Insurance (IDI) Policy insured by Unum (for which Covala Group is the administrative
service provider). This provides an additional maximum monthly LTD benefit of up to $15,000.
If you are eligible for the IDI benefit, you will receive information separately.
Important Details About Participation in the Long-Term
Disability (LTD) Plan
•
When You Can Enroll: You may only enroll in this benefit as a new employee or during
Annual Benefits Enrollment. You may not enroll due to a qualified status change.
•
Evidence of Insurability (EOI): If you are provided or enroll for coverage as a newly
hired employee, no EOI is required. However, EOI
1
does apply any time you want to
increase coverage or enroll in coverage at a later time. In these situations, if you
become disabled prior to approval of EOI, you will receive the value of coverage in effect
prior to your new election.
•
Actively at Work: You must be actively at work on the date your new coverage takes effect.
•
Tobacco User Rates for Coverage: Your tobacco user status will affect your contributions
under the LTD Plan. For more information on tobacco user premiums, please see page 25.
•
Pre-Existing Condition Exclusion: Long-Term Disability benefits will not be paid if both
statements below are true:
— During the first 12 consecutive months of your coverage, you become disabled; and
— You received treatment for that disabling condition during the six months before your
most recent coverage effective date.
1
You can complete an EOI form online through Prudential’s website (via the Benefits Web Center), which you can access through
My Health.
Why LTD Coverage
Is So Important
If you become disabled, you may be
eligible for Short-Term Disability benefits
or for unpaid short-term disability leave
for up to 26 weeks (including the
one-week waiting period). If your
disability continues beyond 26 weeks,
LTD coverage can provide you with
valuable income protection you may
need for you and your family. LTD
coverage also allows you to continue
your JPMorgan Chase Medical Plan and
certain other benefits coverage for
up to 24 months after your LTD benefits
effective date.
Did You Know?
More than one in four of today’s
20-year-olds can expect to be out of work
for at least a year
2
because of a disability
condition before reaching normal
retirement age. In addition, accidents are
not usually the cause of a long-term
disability — back injuries, cancer, heart
disease and other illnesses are usually the
reasons for most long-term absences.
Most Americans don’t have disability
insurance or enough emergency savings
to last 32.1 months, which is the duration
of the average long-term disability claim.
2
Now is the time to enroll for coverage
under the LTD Plan and have peace of mind
knowing that you have some financial
security in case you become disabled.
2
Source: Council for Disability Awareness, 2022

33
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Life and Accident Insurance Plans
JPMorgan Chase offers different types of life and accident insurance administered by
MetLife so you can choose the most appropriate coverage and survivor protection for your
personal situation. The Company automatically provides you with Basic Life Insurance that
pays benefits to your designated beneficiary(ies) if you die and Business Travel Accident
Insurance if you die or are injured while traveling on business for the Company.
Company-Paid Life and Accident Insurance Plans
JPMorgan Chase automatically provides the following protection at no cost to you:
•
Basic Life Insurance: JPMorgan Chase provides Basic Life Insurance equal to one
times your Total Annual Cash Compensation (rounded up to the next $1,000), up to
a maximum of $100,000. In the event of your death as an active employee, benefits
are paid to your designated beneficiary.
Additional benefits of the Basic Life Insurance Plan include:
— SurvivorSupport® Financial Counseling Service: Provides telephonic financial
counseling services to a surviving spouse or key adult survivor for six months after an
employee’s death
— Travel Assistance with ID Theft Solutions Services:
1
• Identity (ID) Theft Assistance Program: Provides identity theft protection
education and assistance to help guide you through the recovery process if your
identity or that of your dependents is compromised.
• Travel Assistance and Emergency Evacuation Services: Provides travel
assistance and emergency services for employees and their family members in
the event of an unexpected medical emergency when traveling 100 miles or more
from home.
• Mobile Assist: Provides information to help avoid expensive mobile telephone
charges and help effectively use overseas options.
— Funeral Concierge Services:
2
Provides information and assistance to employees and their
immediate family members for funeral-related issues anywhere in the United States.
— Grief Counseling:
2
Provides you and your dependents up to five private counseling
sessions either face-to-face or over the phone with a professional grief counselor to help
cope with a loss, no matter the circumstances, whether it’s a death, an illness or divorce.
•
Business Travel Accident Insurance: The Company provides Business Travel Accident
Insurance equal to six times your annual base salary/regular pay (minimum of $50,000
and maximum of $3 million). This coverage offers financial protection in the event of your
accidental death or certain accidental injuries sustained while traveling on business for
JPMorgan Chase. In the event of your death as an active employee, benefits are paid to
your designated beneficiary.
1
Travel Assistance services are offered and administered by AXA Assistance USA, Inc. Certain benefits provided under the Travel
Assistance program are underwritten by Certain Underwriters at Lloyd’s London (not incorporated) through Lloyd’s Illinois, Inc.
Neither AXA Assistance USA, Inc. nor the Lloyd’s entities are affiliated with MetLife, and the services and benefits they provide are
separate and apart from the insurance provided by MetLife.
2
Grief Counseling and Funeral Assistance services are provided through an agreement with LifeWorks, US Inc. LifeWorks is not an
affiliate of MetLife, and the services LifeWorks provides are separate and apart from the insurance provided by MetLife. LifeWorks has
a nationwide network of over 30,000 counselors. Counselors have master’s or doctoral degrees and are licensed professionals. The
Grief Counseling program does not provide support for issues such as: domestic issues, parenting issues or marital/relationship issues
(other than a finalized divorce). For such issues, please refer to My Health to understand the Employee Assistance Program and
Work-Life resources available to you. LifeWorks is available to insureds, their dependents and beneficiaries who have received a
serious medical diagnosis or suffered a loss. Events that may result in a loss are not covered under this program unless and until such
loss has occurred. Services are not available in all jurisdictions and are subject to regulatory approval. Not available on all policy forms.
Life and Accident
Insurance Beneficiaries
The Online Beneficiary Designations site
provides a convenient way to name,
review and update your beneficiary
information for your Life and Accident
Insurance Plan benefits, 401(k) Savings
Plan benefits, and your Pension Plan
(for employees with a balance).
You can access the site:
•
From work:
My Health > Online Beneficiary
Designation Site
•
From home:
https://beneficiary.
jpmorganchase.com
Total Annual Cash
Compensation
You can find the definition of Total Annual
Cash Compensation on page 45.

34
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Supplemental Term Life and Accident Insurance Plans
In addition to the Company-provided insurance described on the previous page, you can elect
to purchase Supplemental Term Life and Accident Insurance for yourself and/or your eligible
dependents through MetLife, the insurance carrier. You may have to provide evidence of
insurability (EOI) before certain levels of life insurance become effective. Your choices for
supplemental life and accident insurance include:
•
Employee Supplemental Term Life Insurance: You can purchase Supplemental Term Life
Insurance on an after-tax basis in increments of $10,000, up to 10 times your Total Annual Cash
Compensation (rounded to the next higher multiple of $10,000) to a maximum of $3 million.
•
Dependent Supplemental Term Life Insurance: You can also purchase Supplemental Term
Life Insurance for your eligible dependents on an after-tax basis. You can buy coverage for
your spouse/domestic partner from $10,000 to $300,000 (in $10,000 increments), subject to
approval by MetLife. In addition, you can buy $5,000, $10,000, $15,000 or $20,000 in
coverage for each dependent child through MetLife (as long as they meet the eligibility
requirements for dependent coverage). Please note: To purchase Supplemental Term Life
Insurance for your spouse/domestic partner or dependent child(ren), you do not need to
elect coverage for yourself.
•
The following services are included with Supplemental Term Life Insurance at no cost:
— Will Preparation Services:
1
Offers you and your spouse/domestic partner unlimited
face-to-face or telephonic meetings with an attorney from MetLife Legal Plans’ network of
over 174,000 participating attorneys.
— Estate Resolution Services:
1
Offers legal assistance from MetLife Legal Plans’ attorney
network with probating your and your spouse’s/domestic partner’s estates.
•
Employee Accidental Death and Dismemberment (AD&D) Insurance: You can purchase
AD&D Insurance on an after-tax basis for financial protection in case of accidental death or
certain accidental injuries. Coverage is available up to 10 times your Eligible Compensation
(in $10,000 increments) to a maximum of $3 million. Please note: Reduced coverage
amounts apply if you are age 75 or older.
•
Dependent Accidental Death and Dismemberment (AD&D) Insurance: You can
purchase AD&D Insurance for your eligible dependents on an after-tax basis. Coverage is
available for your spouse/domestic partner to a maximum of $600,000 (in $10,000
increments). Please note: Reduced coverage amounts also apply to dependents age 75
or older. In addition, you can buy coverage for a child from $10,000 to $100,000 (in
$10,000 increments) as long as the child meets the eligibility requirements for dependent
coverage. As long as you have company-paid Basic Life insurance, you may purchase AD&D
Insurance for your spouse/domestic partner or dependent child(ren), even if you do not
elect coverage for yourself.
If you leave JPMorgan Chase, generally employee and dependent Supplemental Term Life and
AD&D Insurance coverage is portable — meaning you can continue coverage through a direct
billing arrangement with MetLife at a higher rate.
1
Will Preparation and Estate Resolution Services are offered by MetLife Legal Plans, Inc., a MetLife company, Cleveland, Ohio. In certain
states, legal services benefits are provided through insurance coverage underwritten by Metropolitan General Insurance Company,
Warwick, Rhode Island. Tax Planning and preparation of Living Trusts are not covered by the Will Preparation Service. Certain services
are not covered by Estate Resolution Services, including matters in which there is a conflict of interest between the executor and any
beneficiary or heir and the estate; any disputes with the group policyholder, MetLife and/or any of its affiliates; any disputes involving
statutory benefits; will contests or litigation outside probate court; appeals; court costs, filing fees, recording fees, transcripts,
witness fees, expenses to a third party, judgments or fines; and frivolous or unethical matters.
Employee AD&D Insurance
Limit Due to Age
•
When you are age 75 or older, but less
than age 80, your amount of
Employee AD&D Insurance will be
reduced to a maximum amount
of $200,000.
•
When you are age 80 or older, your
amount of insurance will be further
reduced to a maximum amount
of $100,000.
•
If you reach age 75 or 80 while
insured, this limit will not apply until
the January 1 following the date you
reach that age.
Eligible Compensation
You can find the definition of Eligible
Compensation on page 45.

35
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Group Personal Excess Liability Insurance Plan
The JPMorgan Chase Group Personal Excess Liability Insurance Plan insured by Chubb and administered by Marsh McLennan Agency
Private Client Services provides additional liability protection for up to $10 million in coverage for damages and costs you or a covered
family member has to pay beyond the limits of liability provided by your primary auto, homeowners, renters, recreational vehicle,
motorcycle and watercraft insurance policies. Plan highlights include:
•
Covered Persons: If you enroll for coverage, the Plan provides coverage for you, your spouse or domestic partner and all eligible
dependent children.
•
Coverage Options and Costs: You pay for coverage with after-tax dollars. Your cost depends on the coverage level you choose. There
is a flat rate for coverage under this plan — your cost is the same regardless of how many dependents you cover. You can choose from
coverage of:
— $2 million
— $5 million
— $10 million
•
Services provided by Marsh McLennan Agency Private Client Services
— Complimentary Personal Risk Management Review: Elect to receive a complimentary personal risk analysis from a Marsh
McLennan Agency personal risk advisor. Through this consultation, a personal risk advisor will evaluate the adequacy of your
existing policies, identify exposures and determine whether there are sufficient underlying liability limits in your current coverage.
The advisor will also provide customized recommendations to improve the effectiveness of your coverage and ensure you have the
broadest coverage available for the best value.
— Liability Estimator Tool: You’ll have access to a confidential online liability estimator tool to quickly get a preliminary estimate of
the liability coverage amount that may be appropriate for you.
— Claims Advocacy: In the event of a claim, Marsh McLennan Agency will serve as your advocate throughout the claims process.
Important Details About Participation in the Life and Accident Insurance Plans
•
Evidence of Insurability (EOI): If you enroll in employee Supplemental Term Life Insurance when you are newly hired, you are
allowed to enroll for an amount up to the lesser of three times Total Annual Cash Compensation or $500,000 without having to
submit EOI. You can initially enroll a spouse/domestic partner for an amount up to $50,000 without having to submit EOI.
Elected amounts above these guaranteed issue amounts will be subject to EOI. If you do not enroll as a new hire or if you
subsequently increase coverage at a later date, all new coverage will be subject to EOI requirements at the time you make the
new election.
•
Dependent Child(ren) Coverage: If enrolling a child(ren) in Supplemental Term Life Insurance and/or AD&D Insurance, the
same rules for dependent eligibility apply as in the Medical Plan. Additionally, a child(ren) can be covered until age 26, unless
they are a disabled dependent. See the Dependent Eligibility Requirements Tip Sheet for details.
•
Non-Tobacco User Rates for Coverage: You pay for Supplemental Term Life Insurance and AD&D Insurance on an after-tax
basis. In addition, as explained on page 25, if you and/or your covered spouse/domestic partner enroll as a non-tobacco user or
complete an approved tobacco cessation course, you will pay lower, non-tobacco user rates for any Supplemental Term Life
Insurance you elect. For more information on non-tobacco user rates under the Supplemental Term Life Insurance Plan, please
see page 25.
•
Actively at Work: You must be actively at work on the date your new or newly approved coverage takes effect. Dependent
elections for Supplemental Term Life and AD&D coverages will take effect on the date of the qualifying status change or the
date that EOI requirements are satisfied (as applicable).

36
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Important Details About Participation in the Group Personal Excess Liability Insurance Plan
•
When You Can Enroll: You may only enroll in this benefit as a new employee or during Annual Benefits Enrollment. You may not
enroll due to a qualified status change.
•
Required Primary Underlying Liability Insurance Policies: There are certain minimum limits you must carry on your primary
underlying liability insurance policies in order to meet the eligibility requirements for this benefit, and failure to meet these
minimums will result in a gap in coverage for which you will be responsible in the event of a liability claim. Please refer to the
Summary Plan Descriptions available on My Health > Benefits Enrollment > 2023 Benefits Resources > Benefit Plan Details
(Summary Plan Descriptions).
•
If your primary underlying coverage is placed with Chubb, the maximum allowable underlying liability limit is $1,000,000.
•
How It Works: Coverage under this type of policy is always in excess of any other underlying insurance and is also known as
an “umbrella policy.” For example, in the case of a car accident, your primary auto insurance policy would provide the first level
of coverage, and the JPMorgan Chase Group Personal Excess Liability Insurance Plan would be available once primary limits
are exhausted.
Group Legal Services Plan
The JPMorgan Chase Group Legal Services Plan insured by MetLife offers you and your family access to an affordable network of
attorneys for routine legal services related to personal and family legal issues, such as wills and estate planning; real estate matters;
family law; juvenile matters; name changes; consumer protection; property protection; traffic matters; issues of incompetence; and more.
Most services are covered at 100% when you use network attorneys. A reimbursement schedule applies to fees charged by
out-of-network attorneys.
•
Covered Persons: If you elect to enroll, the plan automatically covers you, your spouse/domestic partner and all eligible dependent
children.
•
Coverage Costs: You pay for coverage on an after-tax basis. Your cost is the same regardless of how many dependents you cover under
the plan.
Important Details About Participation in the Group Legal Services Plan
•
When You Can Enroll: You may only enroll in this benefit as a new employee or during Annual Benefits Enrollment. You may not
enroll due to a qualified status change.
•
Pre-Existing Legal Matters: Any legal matter for which an attorney-client relationship existed prior to you becoming eligible for
services under the JPMorgan Chase Group Legal Services Plan will be excluded, and no benefits will apply.
•
Network Attorneys: The JPMorgan Chase Group Legal Services Plan offers access to a network of U.S. attorneys who provide a
wide range of legal services. In-network services are available only in the continental United States, U.S. Virgin Islands, Puerto Rico
and Hawaii, and attorneys will only provide services for U.S.-related issues.

37
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
The Retirement Savings Program
Building a financially secure future is a partnership between you and JPMorgan Chase.
That’s why the firm provides the 401(k) Savings Plan, one of the best and easiest ways to
save for your retirement. In this section you’ll also find information about the Pension Plan
(to the extent it applies to you) and the Employee Stock Purchase Plan.
401(k) Savings Plan
JPMorgan Chase believes that saving for retirement is important. That’s why the firm provides
annual automatic pay credits after one year of total service. In addition, to encourage saving,
the firm provides dollar for dollar matching contributions to most employees after they
complete one year of service. To take advantage of this benefit, begin by enrolling in the plan.
It’s easy — whether you’re automatically enrolled or you enroll on your own. Beyond that step,
you can make the most of the plan by saving and investing.
Enrolling
If you take no action within the first 31 days after your hire/eligibility date, you will be
automatically enrolled at a before-tax contribution rate of 3% of Ongoing Compensation,
which includes base salary/regular pay and non-annual cash incentives.
1
Your 3% before-tax contributions will be invested in a Target Date Fund based on your age and
an assumed retirement age of 65. Your contributions will increase by 1% annually, up to a total
contribution rate of 10%.
You may wish to consider whether this contribution rate will be enough to meet your financial
goals, and if not, choose a contribution rate that suits your needs. Keep in mind that the plan
offers two ways to save on a tax-advantaged basis.
If you don’t want to be enrolled automatically, you can either enroll yourself or you can opt out
of automatic enrollment via the 401(k) Savings Plan Call Center or Web Center prior to the end
of your 31-day grace period.
Your Contributions
You can contribute up to 50% of Ongoing Compensation on a before-tax and/or Roth basis (up to
the annual legal limit).
•
Before-tax contributions allow you to contribute to the plan before federal and, in
many cases, state and local taxes are withheld, which may help you lower your current
taxable income.
•
Roth contributions, which are made after federal, state and local taxes are withheld and
do not lower your current taxable income, may be right for you if you think your taxes may
be higher in retirement or at the time you take a withdrawal. Roth contributions and any
associated earnings can be withdrawn tax-free, assuming certain requirements are met.
You have the flexibility to contribute differently during the year, depending on what works best
for you. There are two types of 401(k) contribution rates:
•
Per-pay rate (1% to 50% on a before-tax and/or Roth basis) — applies to your Ongoing
Compensation, which is your base salary/regular pay, as well as any non-annual cash
incentives
2
you receive. You can adjust your per-pay rate as often as you’d like throughout
the year, and changes will be made on the next paycheck that is administratively possible.
•
Annual Incentive Compensation rate (1% to 50% on a before-tax and/or Roth basis) —
applies only to Annual Incentive Compensation, which is cash compensation awarded, if any,
under the firm’s Performance-Based Incentive Plan (generally paid in January) or Branch
Profitability Incentive Plan (generally paid in February).
You can contribute from your per-pay Ongoing Compensation, your Annual Incentive
Compensation (if any) or both, up to the annual legal limits (see sidebar).
Rolling Over from
Another Plan
Having multiple 401(k) plan accounts can
make tracking and monitoring of your
total savings difficult. Consider a rollover
to consolidate your retirement assets into
one account. The JPMorgan Chase 401(k)
Savings Plan accepts rollovers from most
employers’ 401(k) and other qualified
plans, as well as IRAs.
Know the 401(k) Savings
Plan Limits for 2023
Combined Before-Tax and Roth
401(k) Contributions:
•
Under Age 50: $22,500
•
Age 50 and Over: $30,000
Please note: These annual contribution
limits apply across the JPMorgan Chase
401(k) Savings Plan and any prior
employer’s plan in which you participated
during the calendar year. If you
participated in another employer’s plan
before joining JPMorgan Chase, it is your
responsibility to ensure that your total
contributions to all plans do not
exceed the annual legal limit for
401(k) contributions.
Access to Your Savings
Should a need arise requiring you to
borrow or withdraw from the plan, the
plan has options to take a loan or
withdrawal in certain circumstances.
For more information, refer to the Plan
Highlights available on the 401(k)
Savings Plan Web Center or contact the
401(k) Savings Plan Call Center.
Eligible Compensation
Your Eligible Compensation is your
Ongoing Compensation plus your
Annual Incentive Compensation, if any.
1
Non-annual cash incentive compensation includes cash incentives that are paid throughout the year, such as sales awards and monthly
and quarterly incentives. It also includes any cash incentives paid annually other than Annual Incentive Compensation.

38
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Automatic Pay Credits Contributed by JPMorgan Chase
After one year of total service, you will be eligible for automatic pay credits in the 401(k)
Savings Plan. The credits are equal to 3% of your Eligible Compensation (capped at $100,000
annually). Only the pay you earn beginning the first day of the month after completing one
year of service through the end of the calendar year will be used to determine your pay credits.
These automatic pay credits are in addition to any matching contributions (detailed below)
you’re eligible to receive and don’t require you to make any of your own contributions to the
401(k) Savings Plan. Automatic pay credits will be deposited into your 401(k) Savings Plan
account automatically on an annual basis and will be invested according to the investment
elections on file for your own future contributions to the 401(k) Savings Plan. If you have no
investment elections under the plan, the automatic pay credits will be invested in the Target
Date Fund that most closely aligns with the year in which you will turn age 65.
To be eligible to receive annual automatic pay credits for a given year, you generally need to be
employed as of December 31 of that year. You will become 100% vested in (meaning you have
a non-forfeitable right to) the value of any automatic pay credits you receive after completing
three years of total service.
Please note: For benefits-eligible employees as of December 31, 2018, who are continuously
employed, automatic pay credits are equal to 3% to 5% of Eligible Compensation (capped at
$100,000 annually) based on years of pay credit service. Please see table on the left for a
breakout of automatic pay credit rates based on completed years of pay credit service.
JPMorgan Chase Matching Contributions
JPMorgan Chase offers most employees who complete one year of service the opportunity to
boost their contributions with a dollar-for-dollar matching contribution up to 5% of Eligible
Compensation, which includes base salary/regular pay and annual and non-annual cash
incentives, that you contribute to the 401(k) Savings Plan. Matching contributions are calculated
and credited annually following the end of the calendar year.
Because the match is made on an annual basis, if your goal is to maximize the match, you need
to contribute at least 5% of your Eligible Compensation by year-end — and you have flexibility to
contribute differently during the year.
To be eligible to receive the annual matching contributions for a given year, you generally need
to be employed as of December 31 that year. Please note: Employees whose Total Annual Cash
Compensation is $250,000 or more are not eligible to receive matching contributions.
You will become 100% vested in (meaning you have a non-forfeitable right to) the value of any
matching contributions you receive after completing three years of total service.
Matching Contributions — Special Consideration for New Hires
When making contribution decisions (on your per-pay rate and/or Annual Incentive
Compensation rate), consider whether that compensation is match-eligible. Only contributions
you make — and compensation paid — beginning the first day of the month after completing
one year of service are eligible to be matched.
For example: Consider a full-time employee who is hired April 3, 2023. The employee is eligible
to contribute to the plan immediately; however, contributions made between April 3, 2023, and
April30, 2024, are not eligible for matching contributions. Any amounts up to 5% of Eligible
Compensation contributed from May 1, 2024, through the end of 2024 will be matched, assuming
the participant is employed as of December 31, 2024. These matching contributions will be
credited to the participant’s plan account in early 2025.
For benefits-eligible employees
as of December 31, 2018, who are
continuously employed, automatic pay
credits are equal to 3%–5% of Eligible
Compensation (capped at $100,000
annually), as follows:
Completed Years of
Pay Credit Service
Pay Credit
Percentage
1 – 9 3%
10 – 19 4%
20 or more 5%
My Rewards
All in one place and easy to navigate,
My Rewards gives you quick access to
information and resources to manage
your financial well-being. Enjoy a
consolidated view of your compensation
and retirement savings benefits, including
the 401(k) Savings Plan and Pension Plan
(for employees with a balance).
•
From work:
me@jpmc > MyRewards
•
From home:
myrewards.jpmorganchase.com
Contact Information
Obtain information and conduct plan
transactions by accessing the 401(k)
Savings Plan Web Center through
My Rewards.
For plan questions, please contact
the 401(k) Savings Plan Call Center.

39
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
A Note About Investment
Performance
Past performance does not guarantee
how any investment will perform in the
future. The plan’s investment funds are
not deposits or obligations of — nor
guaranteed by — JPMorgan Chase & Co.,
JPMorgan Chase Bank, N.A. or any of their
subsidiaries. Nor are they insured by the
Federal Deposit Insurance Corporation
(FDIC) or any other governmental agency.
Investments in the funds involve risks,
including the possible loss of principal.
Therefore, it’s important that you make
informed investment decisions only after
carefully reading all plan information
(including the prospectus for the
JPMorgan Chase Common Stock Fund).
You may also want to consult a financial
planner regarding an investment strategy
that’s right for you.
Investing
The plan offers two ways to invest to give you flexibility to choose how you make your
investment decisions — and the tools you’ll need to build a balanced retirement portfolio.
•
No Assembly Required: If you lack the time, interest or expertise to research, manage and
monitor your investments in the plan, you can select one of the Target Date Funds offered
under the plan. Each Target Date Fund corresponds to an expected “target” year — the year that
you plan to start withdrawing from your account (generally your retirement date). The funds are
already diversified with an asset mix that automatically becomes more conservative over time.
•
Do It Yourself: If you want a more hands-on approach, you can create your own diversified
investment mix by choosing a combination of the plan’s Core Funds.
To learn more about the plan’s investment options, visit the 401(k) Savings Plan Web Center.
You can find detailed fund information, including fund performance, fund fact sheets and a
prospectus for the Common Stock Fund. You will also find the Investment Fund Profiles
brochure, which explains the investment risks and strategies for each investment option within
the plan and provides a glossary of important investment terms. To receive paper copies of
the information provided online, free of charge, please call the 401(k) Savings Plan Call Center.
Payment Options When You Leave
When you leave JPMorgan Chase, your vested account balance is payable in the form of a single
lump sum, rollover to an IRA or another qualified plan, or installment payments. Please note:
If your vested account balance (including loans) is less than $1,000 when you leave and you do
not make a distribution election with respect to that balance, your benefit will be paid, as soon
as practicable, in a single cash payment in the form of a check.
My Finances and Me
JPMorgan Chase knows your finances are top of mind and personal to you. And we’re
committed to investing in our employees to provide you with tools, resources and help to be at
your financial best. That’s why we’ve partnered with Financial Finesse, a leader in financial
wellness, to bring you My Finances and Me, a benefit featuring guidance on a wide range of
topics, from paying off debt to managing cash flow to investing, and so much more.
My Finances and Me includes:
•
An online hub where you can access Aimee™, your virtual financial coach, to get prioritized
action steps and track your progress over time. There are also resources available such as
articles, calculators and more.
•
Group education sessions on a variety of topics.
•
Unlimited one-on-one telephonic financial coaching with a Certified Financial Planner.
This benefit is fully paid for by the firm and available to U.S. benefits-eligible employees.
You can also invite your spouse/domestic partner to participate through the hub.
Pension Plan — For Employees Hired Before
December 2, 2017
1
For employees with a balance in the Pension Plan, the plan works as follows:
•
Interest Credits: Your Pension Plan account balance grows by receiving interest credits each
month. The rate of the interest credit will be based on a one-year Treasury bill rate for October
of the prior year published by the IRS, plus 1% — with a minimum interest credit rate of 4.5%.
•
Payment Options: When you leave JPMorgan Chase, you have several payment options
available to you. You can take your vested account balance in a single lump sum, roll it
over to an Individual Retirement Account or another qualified plan, or elect to receive an
annuity from the plan. Please note: If your vested cash balance benefit is less than $5,000
when you leave and you do not make a distribution election with respect to that cash
balance benefit, your benefit will be paid, as soon as practicable, as follows:
— If your cash balance is less than $1,000, it will be paid to you in a single cash payment in
the form of a check;
— If your cash balance is $1,000 to $4,999.99, it will be paid in a direct rollover to an
Individual Retirement Account (IRA) established in your name at Empower.
1
For employees hired on or after December 2, 2017, this plan does not apply to you.
My Pension
Employees with a balance in the
Pension Plan can go to the My Pension
website for convenient access to
information about your plan benefit.
Go to My Pension from work or home
via My Rewards:
•
From work:
me@jpmc > My Rewards
•
From home:
myrewards.jpmorganchase.com
Please note: While employed by
JPMorgan Chase, you may not take a
distribution from your Pension Plan
account.

40
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Employee Financial
Services
Employees are eligible for special
savings and discounts on a variety of
JPMorgan Chase financial products,
such as checking and savings accounts,
mortgages and home equity loans, and
more. Military service personnel qualify
for even more benefits. For more
information, please go to the Employee
Financial Services website.
Employee Discount
Programs
As an active employee, you can also take
advantage of discounts on:
•
Arts and cultural events
•
Fitness and nutrition
•
Full-time child care
•
Travel
You’ll find Employee Discounts &
Benefits at me@jpmc > Benefits &
Rewards.
Additional Programs/Services
As a complement to the benefits plans and wellness programs described in this brochure,
JPMorgan Chase offers a variety of additional programs and services to help meet the diverse
needs of our employees. Some of the programs that may be available to you include:
•
Family Building Benefits
•
Back-Up Child Care
•
Business Resource Groups
•
Career Management
•
Elder and Adult Care
Program
•
Emergency Financial
Assistance
•
JPMorgan Chase Health
& Wellness Centers
•
Lactation Support
•
Legal & Financial
Consultation
•
Matching Gifts Program
•
parents@jpmc
•
Short-Term Disability Plan
•
Time Off Policies
(paid and unpaid)
•
Tuition Assistance Program
•
Volunteerism and Grants
•
Wellness/Work-Life
Seminars
•
SNOO infant smart sleeper
bassinet
•
LGBT+ Health Concierge
Service
For more information on these programs and services, please go to me@jpmc.
Employee Stock Purchase Plan
You are eligible to enroll in the Plan during each annual enrollment period that occurs in the
fourth quarter provided that you are a U.S. benefits-eligible employee and you were hired on
or before September 30 and your Total Annual Cash Compensation is less than $250,000.
(For the definition of Total Annual Cash Compensation, please see page 45.)
•
Payroll deductions: Contributions are deducted on an after-tax basis from each paycheck
based on your election of up to 20% of your Eligible Compensation per pay period. In
addition, contributions are subject to an annual maximum share purchase of $25,000.
•
Purchase dates: Stock purchases take place on first day of January, April, July and October
on which trading in JPMorgan Chase common stock is conducted on the New York Stock
Exchange.
•
5% Discount and no broker fees: Your payroll deductions are used to purchase
JPMorgan Chase common stock at a 5% discount without brokerage commissions or fees.
•
Dividends: Participants in the Plan have the option to either have dividends reinvested in
the Plan at 100% of the Fair Market Value (FMV) on the dividend payable date or paid in the
form of a cash equivalent (e.g., check). New participants will automatically have their
dividends reinvested.
•
Understand the risks: Participation in the Employee Stock Purchase Plan is optional and
does carry risk, including potential loss of your investment due to market fluctuations. You
decide whether or not to participate in the Plan and the level of your participation. Before
you elect to participate, carefully read the Employee Stock Purchase Plan Prospectus
(me@jpmc > My Rewards > Employee Stock Purchase Plan (ESPP)) for additional information
on the rewards and risks of participation.
•
Once enrolled: You can change the amount of your payroll deduction at any time, applicable
for the next administratively feasible pay date. However, if you change your deduction
amount to zero, it cannot be increased until you make an enrollment election during a
subsequent annual enrollment.
•
Preclearance: If you are subject to the firm-wide Personal Account Dealing Policy, you are
required to preclear the sale of any shares of JPMorgan Chase acquired under the Employee
Stock Purchase Plan via the iComply portal; however, there is no requirement at this time to
obtain preclearance approval for enrolling, electing dividend reinvestment or changing
contribution amounts in the Employee Stock Purchase Plan.
This document constitutes part of a prospectus covering securities that have been registered
under the Securities Act of 1933.
For questions about your:
• JPMC Medical Plan
• Medical Reimbursement Account (MRA)
• Health Care Spending Account (HCSA)
• Dependent Care Spending Account (DCSA)
• Nurseline (for health-related inquiries)
Aetna
PayFlex (the MRA, HCSA & DCSA administrator for Aetna)
1-800-468-1266; 8 a.m. to 8 p.m., all time zones, Mon. – Fri.
1-888-678-8242; 8 a.m. to 8 p.m. ET, Mon. – Fri.
Cigna (Cigna is also the HCSA & DCSA administrator for those
not enrolled in the JPMC Medical Plan)
1-800-790-3086; 24/7
Kaiser Permanente (the MRA, HCSA & DCSA administrator for
the Kaiser HMO Option is Cigna)
1-800-204-6561; 8 a.m. to 6 p.m. PT, Mon. – Fri.
For additional help when working with your health care company about:
• Claims
• Health-related inquiries
• Health care reform
Health Advocate 1-866-611-8298; 8 a.m. to 9 p.m. ET, Mon. – Fri.
Email: answers@HealthAdvocate.com
For Expert Medical Advice, including an expert medical second opinion on a documented diagnosis, treatment decision
support, help with finding a provider and additional services
Included Health 1-888-868-4693; 8 a.m. to 9 p.m. ET, Mon. – Fri.
For LGBT+ Health Concierge Service, including finding in-network, LGBT+ arming providers, navigating gender-arming
care as a transgender or non-binary person and more
Included Health 1-877-266-2861; 9 a.m. to 8 p.m. ET, Mon. – Fri.
For questions about Family Building Benefits, including fertility treatments and egg and sperm freezing
(If enrolled in the Kaiser HMO Option, contact Kaiser Permanente)
WINFertility 1-833-439-1517; 9 a.m. to 7:30 p.m. ET, Mon. – Fri.
For questions about your prescription drug coverage under the JPMC Medical Plan
CVS Caremark (Aetna/Cigna) 1-866-209-6093; 24/7 (TDD assistance: 1-800-863-5488)
Kaiser Permanente (Kaiser HMO Option) 1-800-204-6561; 8 a.m. to 6 p.m. PT, Mon. – Fri.
For questions about your Dental Plan
MetLife (PDP option) 1-888-673-9582; 8 a.m. to 11 p.m. ET, Mon. – Fri.
Aetna (DMO option) 1-800-843-3661; 8 a.m. to 6 p.m. ET, Mon. – Fri.
Cigna (DHMO option) 1-800-790-3086; 24/7
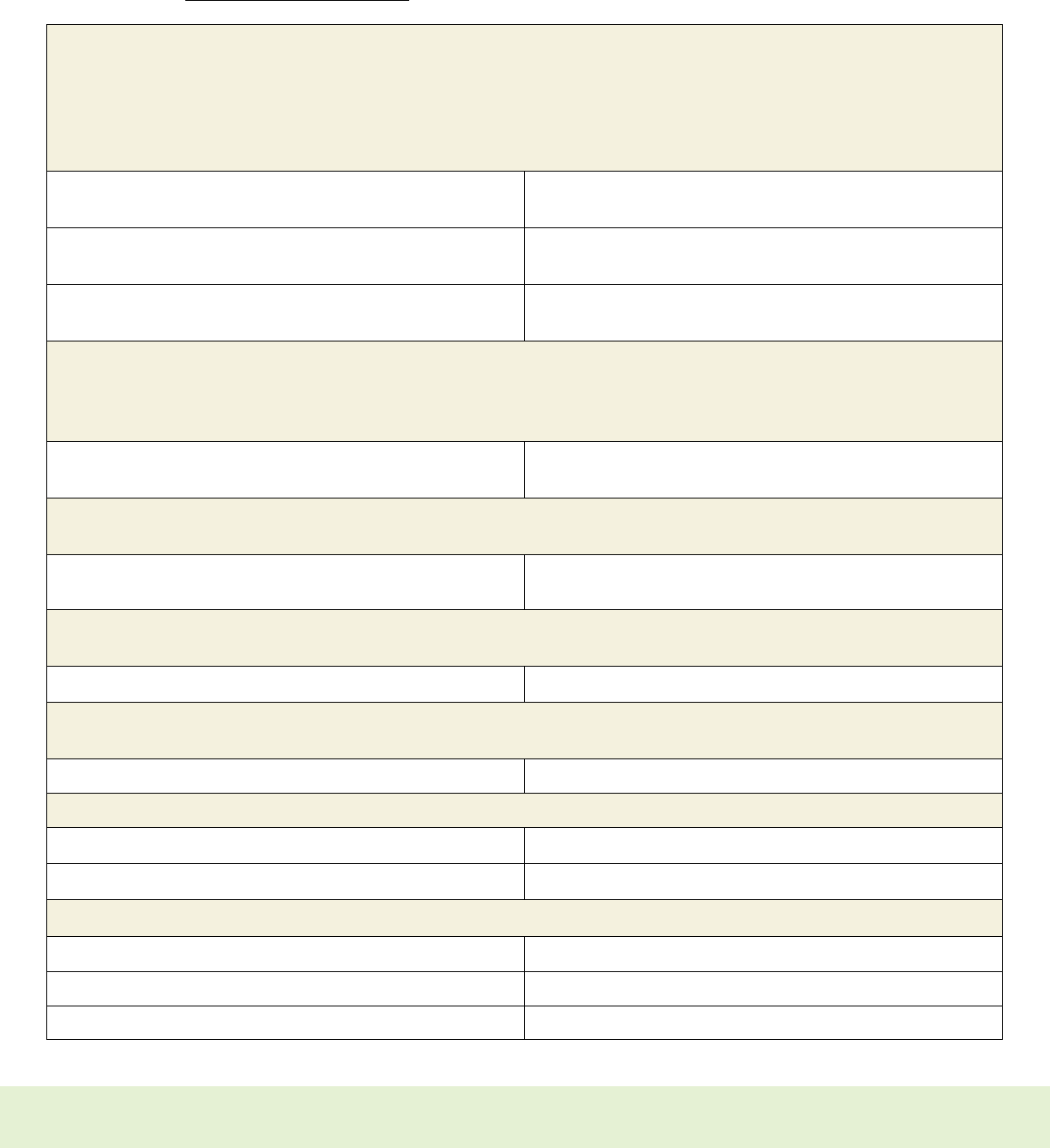
41
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Who to Call With Benefits Questions
Information to help you enroll in and use your benefits is available on My Health:
•
From work: Type “go/myhealth” into your Intranet browser
•
From home: Visit myhealth.jpmorganchase.com
For questions about your:
• JPMC Medical Plan
• Medical Reimbursement Account (MRA)
• Health Care Spending Account (HCSA)
• Dependent Care Spending Account (DCSA)
• Nurseline (for health-related inquiries)
Aetna
PayFlex (the MRA, HCSA & DCSA administrator for Aetna)
1-800-468-1266; 8 a.m. to 8 p.m., all time zones, Mon. – Fri.
1-888-678-8242; 8 a.m. to 8 p.m. ET, Mon. – Fri.
Cigna (Cigna is also the HCSA & DCSA administrator for those
not enrolled in the JPMC Medical Plan)
1-800-790-3086; 24/7
Kaiser Permanente (the MRA, HCSA & DCSA administrator for
the Kaiser HMO Option is Cigna)
1-800-204-6561; 8 a.m. to 6 p.m. PT, Mon. – Fri.
For additional help when working with your health care company about:
• Claims
• Health-related inquiries
• Health care reform
Health Advocate 1-866-611-8298; 8 a.m. to 9 p.m. ET, Mon. – Fri.
Email: answers@HealthAdvocate.com
For Expert Medical Advice, including an expert medical second opinion on a documented diagnosis, treatment decision
support, help with finding a provider and additional services
Included Health 1-888-868-4693; 8 a.m. to 9 p.m. ET, Mon. – Fri.
For LGBT+ Health Concierge Service, including finding in-network, LGBT+ arming providers, navigating gender-arming
care as a transgender or non-binary person and more
Included Health 1-877-266-2861; 9 a.m. to 8 p.m. ET, Mon. – Fri.
For questions about Family Building Benefits, including fertility treatments and egg and sperm freezing
(If enrolled in the Kaiser HMO Option, contact Kaiser Permanente)
WINFertility 1-833-439-1517; 9 a.m. to 7:30 p.m. ET, Mon. – Fri.
For questions about your prescription drug coverage under the JPMC Medical Plan
CVS Caremark (Aetna/Cigna) 1-866-209-6093; 24/7 (TDD assistance: 1-800-863-5488)
Kaiser Permanente (Kaiser HMO Option) 1-800-204-6561; 8 a.m. to 6 p.m. PT, Mon. – Fri.
For questions about your Dental Plan
MetLife (PDP option) 1-888-673-9582; 8 a.m. to 11 p.m. ET, Mon. – Fri.
Aetna (DMO option) 1-800-843-3661; 8 a.m. to 6 p.m. ET, Mon. – Fri.
Cigna (DHMO option) 1-800-790-3086; 24/7
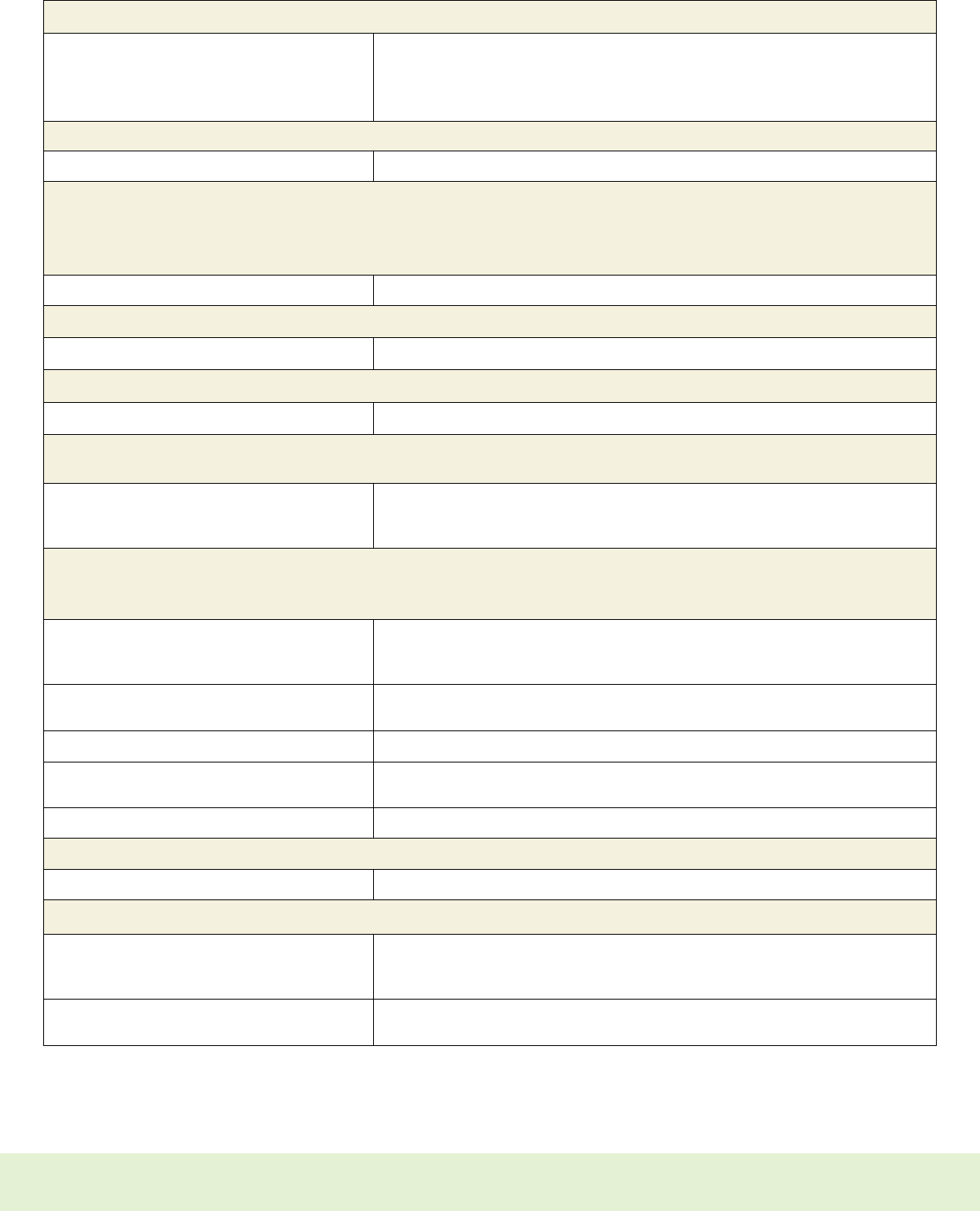
42
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
For complete plan details, see the Benefits Plan Details (Summary Plan Descriptions) on My Health.
For questions about your Vision Plan
EyeMed 1-833-279-4363
7:30 a.m. to 11 p.m. ET, Mon. – Fri.
8 a.m. to 11 p.m. ET, Sat.
11 a.m. to 8 p.m. ET, Sun.
For questions about your Transportation (Transit/Parking) Spending Account (TSA)
HealthEquity (formerly WageWorks) 1-877-924-3967; 8 a.m. to 8 p.m. ET, Mon. – Fri., except certain U.S. holidays.
For questions about your Life Insurance Plan
• Basic Life
• Optional Life
• Accidental Death and Dismemberment (AD&D)
MetLife 1-888-673-9582; 8 a.m. to 8 p.m. ET, Mon. – Fri.
For questions about your Group Personal Excess Liability (PEXL) Insurance Plan
Marsh McLennan Agency 1-855-426-1380; 9 a.m. to 5 p.m. ET, Mon. – Fri.
For questions about your Group Legal Services Plan
MetLife Legal Plans 1-800-821-6400; 8 a.m. to 8 p.m. ET, Mon. – Fri.
For questions about:
• General benefits, enrollment and Employee Stock Purchase Plan (ESPP)
HR Answers HR Answers widget on me@jpmc or
1-877-JPMChase (1-877-576-2427) or 1-212-552-5100 if calling from outside the
United States; 8 a.m. to 7 p.m. ET, Mon. – Fri.
For questions about Wellness:
• Wellness Activities
• Program Support
Initial Wellness Activities:
• Wellness Assessment
• Wellness Screening
Cigna: 1-800-790-3086, 24/7
Quest Patient Service Center: 1-888-606-3199
Additional Wellness Activities To see the activities you have completed or are available for you to complete,
go to My Health > Wellness Activities & Services
Virgin Pulse (Simplified) 1-833-568-3958; 8 a.m. to 9 p.m. ET, Mon. – Fri.
Newtopia (Simplified) 1-888-639-8181; 8 a.m. to 8 p.m. ET, Mon.; 8 a.m. to 10 p.m., Tue. – Thu.; 8 a.m. to
6 p.m., Fri.
meQuilibrium Email: support@mequilibrium.com
For questions about any financial topic, use the My Finances and Me benefit
Financial Finesse 1-833-283-0031; 9 a.m. to 8 p.m. ET, Mon. – Fri., except certain U.S. holidays.
For questions about retirement savings (not part of Annual Benefits Enrollment)
401(k) Savings Plan 1-866-JPMC401k (1-866-576-2401) or 1-303-737-7204 if calling from outside the U.S.,
8 a.m. to 10 p.m. ET, Mon. – Fri., except New York Stock Exchange holidays. The TTY
number is 1-800-345-1833.
Retirement Plan (pension) 1-877-JPMChase (1-877-576-2427) or 1-212-552-5100 if calling from outside the U.S.,
8 a.m. to 7 p.m. ET, Mon. – Fri., except certain holidays.

43
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Additional Reminders
•
Enrolling During Your 31-Day New Hire Health Care and Insurance Plans Enrollment
Period and Qualified Status Changes Throughout the Year. If you do not elect coverage
during your 31-day new hire Health Care and Insurance Plans enrollment period, you will not
have coverage for the remainder of the year. Your next opportunity to enroll for coverage will
be during an annual benefits enrollment period. Please note: To add a dependent child over
the age of 26 who is unable to support themselves due to a mental or physical disability, you
must do so within your 31-day new hire enrollment period. You will not be able to enroll them
in any plans after your 31-day enrollment period. You cannot change your health care company
or payment method during the year even if you have a qualified status change. If you
experience a qualified status change (such as marriage, divorce, or the birth or adoption of a
child), you must make eligible benefits changes through the Benefits Web Center or by calling
HR Answers within 31 days
1
of the qualifying event.
1
90 days if the qualifying event is the birth or adoption of a child. You will have 90 days from the qualified status change to add
any newly eligible dependent should that dependent pass away within this 90-day period. Please contact HR Answers if this
situation applies to you.
•
Newborns’ and Mothers’ Health Protection Act. In accordance with the Newborns’ and
Mothers’ Health Protection Act, group medical plans and health insurance issuers may not,
under federal law, restrict benefits for any hospital length of stay in connection with
childbirth for the mother or newborn child to less than 48 hours following a normal delivery,
or to less than 96 hours following a cesarean section. Further, the plan cannot require that
any medical provider obtain authorization from the plan or any insurance issuer for
prescribing a length of stay not in excess of these periods.
•
Medical Plan Post-Mastectomy Benefits. All options under the JPMorgan Chase Medical
Plan cover certain breast reconstructive benefits in conjunction with a mastectomy for
eligible participants. Coverage under the Medical Plan is available for:
— Reconstruction of the breast on which the mastectomy was performed;
— Surgery and reconstruction for the other breast to produce a symmetrical appearance;
and
— Prosthesis and treatment of physical complications for all stages of mastectomy, including
lymphedema.
This coverage is subject to all the terms of the Medical Plan option in which you participate,
including relevant deductibles and coinsurance provisions. For more information, please
contact your health care company.
•
HIPAA Privacy Rights and Protected Health Information. Federal legislation under the
Health Insurance Portability and Accountability Act (HIPAA) legally requires employers to
periodically communicate how certain protected health information under employee and
retiree health care plans may be used and disclosed, as well as how plan participants can
get access to their protected health information.
Accordingly, JPMorgan Chase will make available a Privacy Notice of Protected Health
Information Under the JPMorgan Chase Health Care Plans to you that describes in detail
how your personal health information may be used and your rights with regard to this
information. You can access a copy of the Privacy Statement on My Health.
Your Privacy
Is Important
The privacy of your health information is
important to you and to JPMorgan Chase.
We are committed to protecting your
personal health information and
complying with privacy laws, including
the Health Insurance Portability and
Accountability Act (HIPAA). This means
that when you complete a Wellness
Assessment, participate in any health
coaching activities or receive health care
treatment of any kind, your personal
health information is not disclosed to
anyone, including JPMorgan Chase,
without your authorization and except as
permitted by HIPAA. (For detailed
information about your HIPAA Privacy
Rights, please see the Privacy Notice
found on My Health.)

44
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Appendix
Special Notice for Employees Who Have Been Reinstated by
JPMorgan Chase Within 31 Days
If your employment has been reinstated with JPMorgan Chase within 31 days of your termination date, your coverage for certain benefits
under the JPMorgan Chase Benefits Program may be affected, as highlighted in the following chart:
Medical, Dental and Vision Plans You and your dependents will be assigned the same coverage you had prior
to your termination date.
Health Care Spending Account Your previously elected annual contribution amount will be reinstated and
prorated accordingly for the balance of the plan year.
Dependent Care Spending Account Your previously elected annual contribution amount will be reinstated and
prorated accordingly for the balance of the plan year.
Transportation Spending Accounts
(Transit/Parking)
There are no reinstatement provisions for these accounts. You will need to
make a new enrollment election.
Long-Term Disability (LTD) Plan You will be assigned the coverage level you had prior to your termination
date. Long-term disability benefits will not be paid if:
• During the first 12 consecutive months of your coverage, you become
disabled; and
• You received treatment for that disabling condition during the six months
before your most recent coverage effective date.
Please note: The 12 months of coverage will be reviewed based on the date
you were reinstated.
Supplemental Term Life (STL) Insurance Plan You and your dependents will be assigned the same coverage amount in
eect prior to your termination date.
Accidental Death and Dismemberment (AD&D)
Insurance Plan
You and your dependents will be assigned the same coverage amount in
eect prior to your termination date.
Group Personal Excess Liability Insurance Plan You will be assigned the same coverage amount in eect prior to your
termination date.
Group Legal Services Plan You will be assigned the same coverage amount in eect prior to your
termination date.
401(k) Savings Plan Your contribution rate and investment elections (if any) will be reinstated as
of your first pay period. If you were eligible for automatic pay credits, you
will receive automatic pay credits based on the same percentage of Eligible
Compensation (capped at $100,000 annually) as you would have otherwise
received had you not had a break in service.
Please note:
•
Any assigned coverage cannot be changed unless you experience a qualified status change. For more information, please see the
Benefits Status Change Guide on My Health.
•
If you are rehired after 31 days of your termination date, you will need to make new benefits elections for most plans in which you
would like to participate.
•
In all cases, the period during which you are not working will result in a break in coverage (unless you elect coverage through COBRA or
plan portability features, as applicable).

45
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Important Definitions
Throughout this brochure, there are references to terms such as “Annual Incentive Compensation,” “Eligible Compensation,” “pay credit
service,” “Total Annual Cash Compensation” and “total service.” These terms are used to determine eligibility for benefits, benefits
contributions and/or coverage levels under certain benefits plans. The definitions below describe these terms.
Annual Incentive Compensation
Annual Incentive Compensation is cash compensation, if any,
awarded under the firm’s Performance-Based Incentive Plan
(generally paid in January) or Branch Profitability Incentive Plan
(generally paid in February).
Eligible Compensation for the 401(k)
Savings Plan
Eligible Compensation includes base salary/regular pay and annual
and non-annual cash incentives. Eligible Compensation does
not include overtime payments, sign-on bonus and similar awards,
referral awards, stipends, non-cash awards (such as equity awards)
and allowances.
Eligible Compensation for the AD&D Plans
and Employee Stock Purchase Plan
Generally your base salary/regular pay, plus applicable job
differential pay (e.g., shift pay). It does not include any annual
bonus, overtime, special recognition or other incentive awards
you might receive. In certain situations, your Eligible Compensation
may include other cash earnings (e.g., commissions, draws and
overrides) paid under certain non-annual incentive plans that
provide compensation in lieu of base salary. Generally, your
Eligible Compensation is updated as changes occur throughout
the year. Please note: Various JPMorgan Chase plans have
different definitions of Eligible Compensation. Separate
definitions may apply to employees in certain sales positions
who are paid on a draw-and-commission basis.
Ongoing Compensation for
the 401(k) Savings Plan
Your base salary/regular pay, plus applicable job differential
pay (e.g., shift pay) and non-annual incentive compensation.
Non-annual incentive compensation includes cash incentives that
are paid throughout the year, such as sales awards and monthly
and quarterly incentives. Ongoing Compensation also includes any
cash incentives paid annually other than Annual Incentive
Compensation (as defined above).
Pay Credit Service
Generally the period beginning on your first business day actively
at work as an employee of JPMorgan Chase or an affiliate and
ending when your employment ends.
Service with a company at the time of its merger generally counts
toward pay credit service. However, only service with the company
employing you at the time of the merger will generally count. (In
other words, if you worked for two companies that later merged,
only service with the company employing you on the merger date
will be recognized.) Service with a company at the time of its
acquisition (as opposed to a merger) may or may not count toward
pay credit service, depending on the terms of the purchase
agreement and the plan.
For a full definition of pay credit service, please see
JPMorgan Chase U.S. Retirement Savings Program — Pay
Credit Service Definition on me@jpmc > Benefits & Rewards
Home > Legally-required Notices.
Total Annual Cash Compensation
Your annual rate of base salary/regular pay plus any applicable job
differential pay (e.g., shift pay) as of each August 1, plus any cash
earnings from any incentive plans (e.g., annual incentive draws,
overrides, and special recognition payments or incentives) that are
paid to or deferred by you for the previous 12-month period ending
each July 31. Overtime is not included. For purposes of determining
your eligibility to receive company matching contributions under the
401(k) Savings Plan, the Medical Plan contribution pay tier level that
applies to you, coinsurance maximum, Long-Term Disability Plan
coverage and eligibility to participate in the Employee Stock
Purchase Plan, your Total Annual Cash Compensation is recalculated
as of each August 1 to take effect the following January 1 and will
remain unchanged throughout the year. For most employees,
Total Annual Cash Compensation will be equal to your annual rate
of base salary/regular pay plus job differentials in the year of hire.
Your Total Annual Cash Compensation will be available on the
Benefits Web Center via My Health > Benefits Web Center > Your
Profile > Personal Information > Personal Details. Separate
definitions may apply to employees in certain sales positions who
are paid on a draw-and-commission basis. If this applies to you,
you will be notified in writing.
Total Service
Generally the period beginning on your first business day actively
at work as an employee of JPMorgan Chase or an affiliate and
ending when your employment ends. This generally includes all
periods of employment with JPMorgan Chase or any of the merged
companies that have become part of JPMorgan Chase.

46
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Notes

47
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
Notes

48
|
Highlights of the 2023 JPMorgan Chase U.S. Benefits Program
For employees living in all states except Arizona and Ohio
259545
